Menorrhagia
Definition
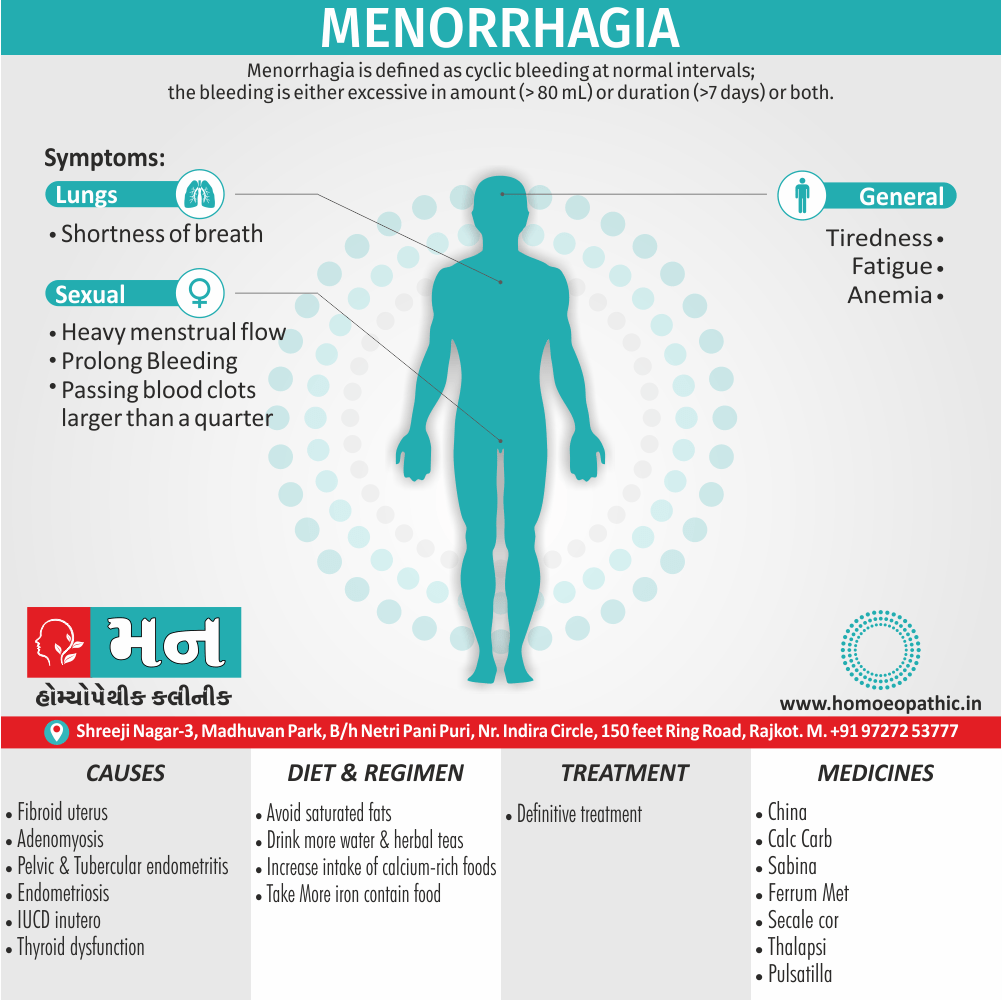
Menorrhagia is defined as cyclic bleeding at normal intervals; the bleeding is either excessive in amount (> 80 mL) or duration (>7 days) or both. [1]
There aren’t any perfect synonyms for menorrhagia in everyday language. However, depending on the context, you could use phrases that capture the meaning:
Formal synonyms:
- Heavy menstrual bleeding (HMB) – This is the most common medical term used interchangeably with menorrhagia.
- Menstruation lasting longer than 7 days.
Informal terms:
- Heavy periods
- Prolonged periods
- Profuse Menses
Remember, the informal terms might be less clear for someone unfamiliar with menstrual issues.
Overview
Epidemiology
Causes
Risk Factors
Pathogenesis
Pathophysiology
Types
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Menorrhagia
Menorrhagia is the medical term for menstrual periods with abnormally heavy or prolonged bleeding. Although heavy menstrual bleeding is a common concern, most women don’t experience blood loss severe enough to be defined as menorrhagia.
With menorrhagia, you can’t maintain your usual activities when you have your period because you have so much blood loss and cramping. If you dread your period because you have such heavy menstrual bleeding, talk with your doctor. There are many effective treatments for menorrhagia.[1]
Epidemiology
Epidemiology of Menorrhagia
The epidemiology of menorrhagia in India shows a high prevalence, particularly among women of lower socioeconomic status and those with lower educational levels. It is more prevalent in women over 30, those who are illiterate or have low education levels, and those of low socioeconomic status. It is also more common in housewives than working women, unmarried women, and women who have been married for 20-30 years. Additionally, it is more prevalent in multiparous women and those who have undergone sterilization. These findings are consistent across several studies:
- Inherited bleeding disorders in Indian women with menorrhagia (2003) found that inherited platelet function defects are the most common cause of menorrhagia in Indian women, followed by von Willebrand disease (vWD). [8]
- A Study of Demographic Profile and Evaluation of Menorrhagia (2014) reported that the prevalence of menorrhagia decreases as education status improves and is more common in women of lower socioeconomic status. [9]
- Menstruation and related disorders in Indian adolescent girls: an observational study highlights that the most common cause of menorrhagia in adolescent girls is anovulatory dysfunctional uterine bleeding (DUB). [10]
Please note that these are just a few examples and the epidemiology of menorrhagia in India is complex and multifactorial. It is influenced by a variety of factors, including genetic, hormonal, lifestyle, and socioeconomic factors.
Causes
Causes of Menorrhagia
Menorrhagia is a symptom of some underlying pathology—organic or functional.
Organic
Due to congestion, increased surface area, or hyperplasia of the endometrium
- Fibroid uterus
- Adenomyosis
- Pelvic endometriosis
- IUCD inutero
- Chronic tubo-ovarian mass
- Tubercular endometritis (early cases)
- Retroverted uterus—due to congestion
- Granulosa cell tumor of the ovary
Systemic
- Liver dysfunction—failure to conjugate and thereby inactivates the estrogens
- Congestive cardiac failure
- Severe hypertension
Endocrinal
- Hypothyroidism
- Hyperthyroidism
Hematological
- Idiopathic thrombocytopenic purpura
- Leukemia
- Von Willebrand’s disease
- Platelet deficiency
Emotional upset
Functional
Due to disturbed hypothalamo-pituitary-ovarian endometrial Axis
Dysfunctional uterine bleeding
- Fibroid uterus
- Adenomyosis
- Chronic tubo-ovarian mass [1]
Risk Factors
Risk Factors for Menorrhagia
Several risk factors increase the likelihood of developing menorrhagia. These can be categorized into:
Hormonal Imbalance:
- Ovulatory Dysfunction: Anovulation (absence of ovulation) or irregular ovulation can lead to hormonal imbalances, causing the endometrium (uterine lining) to build up excessively and shed heavily.
- Polycystic Ovary Syndrome (PCOS): This hormonal disorder is characterized by irregular periods, excess androgens (male hormones), and multiple cysts on the ovaries, which can contribute to menorrhagia.
Uterine Conditions:
- Uterine Fibroids: Noncancerous growths in the uterus can cause heavy or prolonged bleeding.
- Adenomyosis: A condition where endometrial tissue grows into the muscular wall of the uterus, leading to heavy periods and pain.
- Endometrial Polyps: Small, benign growths on the lining of the uterus can cause irregular and heavy menstrual bleeding.
Other Medical Conditions:
- Bleeding Disorders: Conditions like von Willebrand disease, a blood clotting disorder, can cause heavy menstrual bleeding.
- Thyroid Disorders: Both hypothyroidism (underactive thyroid) and hyperthyroidism (overactive thyroid) can disrupt the menstrual cycle and contribute to menorrhagia.
- Pelvic Inflammatory Disease (PID): An infection of the female reproductive organs can cause inflammation and scarring, leading to heavy or irregular bleeding.
Medications:
- Anticoagulants: Medications that prevent blood clotting, like warfarin, can increase menstrual flow.
- Hormonal Intrauterine Devices (IUDs): Some hormonal IUDs can cause heavier periods, especially in the first few months after insertion. [11]
Pathogenesis
Pathogenesis of Menorrhagia
Hormonal Imbalance:
- Anovulation: In the absence of ovulation, progesterone levels remain low, leading to unopposed estrogen stimulation of the endometrium. This results in excessive endometrial growth and subsequent heavy shedding during menstruation.
- Progesterone Deficiency: Even in ovulatory cycles, inadequate progesterone production can lead to insufficient endometrial maturation and unstable shedding, contributing to heavy bleeding.
Uterine Abnormalities:
- Uterine Fibroids: These benign tumors can distort the uterine cavity, increase the surface area of the endometrium, and interfere with normal uterine contractions, leading to prolonged and heavy bleeding.
- Adenomyosis: The presence of endometrial tissue within the myometrium (uterine muscle) can cause uterine enlargement, impaired contractility, and increased blood flow, contributing to menorrhagia.
- Endometrial Polyps: These benign growths can increase the endometrial surface area and interfere with normal shedding, leading to heavy or prolonged bleeding.
Coagulation Disorders:
- Von Willebrand Disease: This inherited bleeding disorder affects platelet function and blood clotting, leading to prolonged and heavy menstrual bleeding.
- Other Coagulopathies: Rarely, other inherited or acquired bleeding disorders can contribute to menorrhagia.
Other Factors:
- Chronic Pelvic Inflammation: Inflammation can disrupt normal endometrial shedding and repair, leading to heavy or irregular bleeding.
- Endometrial Hyperplasia: Excessive growth of the endometrium can occur due to prolonged estrogen stimulation, increasing the risk of heavy bleeding.
- Medications: Certain medications, such as anticoagulants and hormonal therapies, can affect menstrual flow and contribute to menorrhagia. [12]
Pathophysiology
Pathophysiology of Menorrhagia
The pathophysiology of menorrhagia, or heavy menstrual bleeding, is complex and multifactorial, involving various hormonal, structural, and coagulation-related factors.
Hormonal Factors:
- Anovulation: In the absence of ovulation, progesterone levels remain low, leading to unopposed estrogen stimulation of the endometrium. This results in excessive endometrial growth and subsequent heavy shedding during menstruation.
- Progesterone Deficiency: Even in ovulatory cycles, inadequate progesterone production can lead to insufficient endometrial maturation and unstable shedding, contributing to heavy bleeding.
Structural Abnormalities:
- Uterine Fibroids: These benign tumors can distort the uterine cavity, increase the surface area of the endometrium, and interfere with normal uterine contractions, leading to prolonged and heavy bleeding.
- Adenomyosis: The presence of endometrial tissue within the myometrium (uterine muscle) can cause uterine enlargement, impaired contractility, and increased blood flow, contributing to menorrhagia.
- Endometrial Polyps: These benign growths can increase the endometrial surface area and interfere with normal shedding, leading to heavy or prolonged bleeding.
Coagulation Disorders:
- Von Willebrand Disease: This inherited bleeding disorder affects platelet function and blood clotting, leading to prolonged and heavy menstrual bleeding.
- Other Coagulopathies: Rarely, other inherited or acquired bleeding disorders can contribute to menorrhagia.
Other Factors:
- Chronic Pelvic Inflammation: Inflammation can disrupt normal endometrial shedding and repair, leading to heavy or irregular bleeding.
- Endometrial Hyperplasia: Excessive growth of the endometrium can occur due to prolonged estrogen stimulation, increasing the risk of heavy bleeding.
- Medications: Certain medications, such as anticoagulants and hormonal therapies, can affect menstrual flow and contribute to menorrhagia. [13]
Types
Types
Menorrhagia, or heavy menstrual bleeding, is primarily categorized based on the underlying cause:
Ovulatory Menorrhagia:
This type is associated with regular menstrual cycles where ovulation occurs. The heavy bleeding is often caused by:
- Hormonal Imbalances: Progesterone deficiency or an imbalance between estrogen and progesterone.
- Uterine Fibroids: Benign tumors that can disrupt normal uterine contractions and increase bleeding.
- Adenomyosis: Endometrial tissue grows into the uterine muscle, causing heavy bleeding and pain.
- Endometrial Polyps: Small growths in the uterine lining can lead to increased bleeding.
- Bleeding Disorders: Conditions like von Willebrand disease can cause prolonged and heavy bleeding.
Anovulatory Menorrhagia:
This type occurs in the absence of ovulation, often due to:
- Hormonal Imbalance: Unopposed estrogen stimulation without progesterone leads to excessive endometrial growth and heavy shedding.
- Polycystic Ovary Syndrome (PCOS): A hormonal disorder characterized by irregular ovulation and often associated with menorrhagia. [14]
Clinical Features
Clinical Features of Menorrhagia
Menorrhagia, or heavy menstrual bleeding, presents with a range of clinical features that can significantly impact a woman’s quality of life. These features include:
Heavy Bleeding:
- Soaking through one or more sanitary pads or tampons every hour for several consecutive hours.
- Needing to use double sanitary protection to control menstrual flow.
- Passing large blood clots, often larger than a quarter.
- Bleeding lasting longer than seven days.
Disruptions in Daily Life:
- Inability to maintain usual activities due to heavy bleeding and associated symptoms.
- Fatigue and tiredness due to blood loss.
- Difficulty sleeping due to discomfort and anxiety.
- Emotional distress, including anxiety and depression, related to the impact on daily life.
Associated Symptoms:
- Painful periods (dysmenorrhea).
- Pelvic pain or pressure.
- Lower back pain.
- Bloating and abdominal discomfort.
- Anemia symptoms, such as shortness of breath, dizziness, and pale skin, due to significant blood loss. [15]
Sign & Symptoms
Sign & Symptoms of Menorrhagia
- Soaking through one or more sanitary pads or tampons every hour for several consecutive hours.
- Needing to use double sanitary protection to control your menstrual flow.
- Needing to wake up to change sanitary protection during the night.
- Bleeding for longer than a week.
- Passing blood clots larger than a quarter.
- Restricting daily activities due to heavy menstrual flow.
- Symptoms of anemia, such as tiredness, fatigue or shortness of breath.[1]
Clinical Examination
Clinical Examination of Menorrhagia
A comprehensive clinical examination is essential for evaluating menorrhagia and determining the underlying cause. The examination typically includes the following components:
1. History Taking:
- Menstrual History: Detailed information about the duration, amount, and frequency of menstrual bleeding, as well as any associated symptoms like pain or fatigue.
- Medical History: Any underlying medical conditions, such as bleeding disorders, thyroid problems, or pelvic inflammatory disease, should be noted.
- Medication History: Current medications, including over-the-counter drugs and herbal supplements, should be reviewed to identify potential contributors to heavy bleeding.
- Family History: Any family history of bleeding disorders or gynecological problems should be noted.
2. Physical Examination:
- General Examination: Assessment of vital signs (blood pressure, pulse, temperature) and overall health status.
- Abdominal Examination: Palpation to check for any abdominal masses or tenderness.
- Pelvic Examination:
- Speculum Examination: Visualization of the cervix and vaginal walls to check for any abnormalities.
- Bimanual Examination: Palpation of the uterus and ovaries to assess size, shape, and tenderness.
3. Additional Investigations:
- Laboratory Tests:
- Complete Blood Count (CBC): To check for anemia due to blood loss.
- Thyroid Function Tests: To rule out thyroid disorders.
- Coagulation Profile: To screen for bleeding disorders.
- Hormonal Assays: To evaluate for hormonal imbalances.
- Imaging Studies:
- Ultrasound: To visualize the uterus and ovaries for any structural abnormalities, such as fibroids or polyps.
- Hysteroscopy: To directly visualize the inside of the uterus for any abnormalities. [16]
Diagnosis
Diagnosis
Long duration of flow, passage of big clots, use of increased number of thick sanitary pads, pallor, and low level of hemoglobin give an idea about the correct diagnosis and magnitude of menorrhagia.[1]
Differential Diagnosis
Differential Diagnosis of Menorrhagia
It is important to consider a broad differential diagnosis to ensure accurate identification and appropriate management. Some of the common differential diagnoses for menorrhagia include:
Structural Causes:
- Uterine Fibroids: Benign tumors that can cause heavy or prolonged bleeding.
- Adenomyosis: Endometrial tissue grows into the uterine muscle, leading to heavy periods and pain.
- Endometrial Polyps: Small growths in the uterine lining can cause irregular and heavy menstrual bleeding.
- Endometrial Hyperplasia: Excessive growth of the uterine lining due to hormonal imbalances.
Hormonal Causes:
- Anovulation: Absence of ovulation, often due to polycystic ovary syndrome (PCOS) or thyroid disorders.
- Ovulatory Dysfunction: Irregular ovulation leading to hormonal imbalances.
- Hypothyroidism: Underactive thyroid gland can disrupt the menstrual cycle.
Coagulopathies:
- Von Willebrand Disease: The most common inherited bleeding disorder that can cause heavy menstrual bleeding.
- Other Bleeding Disorders: Rare conditions like factor deficiencies or platelet disorders.
Medications:
- Anticoagulants: Blood thinners can increase menstrual flow.
- Hormonal Contraceptives: Certain types of contraceptives, like IUDs, can cause heavier bleeding.
Other Causes:
- Pelvic Inflammatory Disease (PID): Infection of the reproductive organs can cause inflammation and heavy bleeding.
- Endometriosis: Endometrial tissue grows outside the uterus, potentially causing heavy periods.
- Cervical or Uterine Cancer: Although rare, malignancies can present with abnormal uterine bleeding. [17]
Complications
Complications of Menorrhagia
Menorrhagia, or heavy menstrual bleeding, can lead to several complications if left untreated or inadequately managed. These complications can significantly impact a woman’s physical and emotional well-being. Some of the potential complications include:
Iron-Deficiency Anemia:
- Excessive blood loss during menstruation can lead to a deficiency in iron, an essential component of hemoglobin, the protein responsible for carrying oxygen in the blood.
- Symptoms of anemia include fatigue, weakness, shortness of breath, pale skin, dizziness, and headaches.
Severe Pain and Discomfort:
- Heavy bleeding can be accompanied by severe menstrual cramps (dysmenorrhea) and pelvic pain, interfering with daily activities and quality of life.
- Pain may be due to uterine contractions or underlying conditions like adenomyosis or fibroids.
Reduced Quality of Life:
- Menorrhagia can significantly disrupt a woman’s daily routine, work, social activities, and personal relationships due to heavy bleeding, pain, and associated symptoms like fatigue and mood changes.
Psychological Impact:
- The physical and social limitations caused by menorrhagia can lead to emotional distress, anxiety, depression, and decreased self-esteem.
Rare Complications:
- In some cases, prolonged or severe menorrhagia may require blood transfusions or even surgical interventions like hysterectomy (removal of the uterus) if other treatment options fail. [18]
Investigations
Investigations of Menorrhagia
- Blood tests to check for disorders that cause bleeding, nutritional deficiencies, infections, markers of inflammation, and other findings
- Tests to check your hormone levels also thyroid function
- Urine samples to check for pregnancy, infection, or STIs
- Ultrasounds of your abdomen and pelvis, including transvaginal ultrasounds
Other investigation
- Either CT scans or MRIs
- A pap smear to test for cervical cancer
- Other tissue biopsies to look for other types of cancer
- Surgery (for example; laparoscopy or laparotomy) [7]
Treatment
Treatment of Menorrhagia
The definitive treatment is appropriate to the cause for menorrhagia.[1]
Nonsteroidal anti-inflammatory drugs (NSAIDs) i.e.-
NSAIDs, such as ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve), help reduce menstrual blood loss. NSAIDs have the added benefit of relieving painful menstrual cramps (dysmenorrhea).
Tranexamic acid i.e.-
Tranexamic acid helps reduce menstrual blood loss and only needs to be taken at the time of the bleeding.
Oral contraceptives i.e.-
A side from providing birth control, oral contraceptives can help regulate menstrual cycles and reduce episodes of excessive or prolonged menstrual bleeding.
Oral progesterone i.e.-
The hormone progesterone can help correct hormone imbalance and reduce menorrhagia.
Hormonal IUD (e.g. Liletta, Mirena) i.e.-
This intrauterine device releases a type of progestin called levonorgestrel, which makes the uterine lining thin and decreases menstrual blood flow and cramping.[6]
Procedures-
You may need surgical treatment for menorrhagia if medical therapy is unsuccessful.
Treatment options include:
- Dilation also curettage (D&C)
- Uterine artery embolization
- Myomectomy
- Focused ultrasound surgery
- Endometrial ablation
- Endometrial resection
- Hysterectomy [6]
Prevention
Prevention of Menorrhagia
While not all cases of menorrhagia can be prevented, certain lifestyle modifications and proactive measures may help reduce the risk or severity of heavy menstrual bleeding:
Maintain a Healthy Weight: Obesity is associated with an increased risk of menorrhagia. Maintaining a healthy weight through a balanced diet and regular exercise can help regulate menstrual cycles and reduce bleeding.
Exercise Regularly: Regular physical activity can help regulate hormonal balance and promote overall health, potentially reducing the risk of menorrhagia. However, excessive exercise can disrupt the menstrual cycle, so moderation is key.
Manage Stress: Chronic stress can disrupt hormonal balance and worsen menstrual symptoms, including heavy bleeding. Practicing stress-reducing techniques like yoga, meditation, or deep breathing exercises may be beneficial.
Avoid Smoking: Smoking has been linked to irregular periods and increased menstrual bleeding. Quitting smoking can improve overall health and potentially reduce the risk of menorrhagia.
Consider Hormonal Contraceptives: In some cases, hormonal contraceptives like birth control pills or hormonal intrauterine devices (IUDs) can help regulate menstrual cycles and reduce heavy bleeding. However, it’s essential to discuss the potential risks and benefits with a healthcare provider before starting any hormonal therapy. [19]
Homeopathic Treatment
Homeopathic Treatment for Menorrhagia
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Menorrhagia:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicine:
Cal-c
- Menses too early, too profuse, too long-lasting; over-exertion or least excitement causes return of menses. Additionally, Inward coldness.
- Lastly, Sensation if she had on cold, damp stockings.
China
- Menses too early, too profuse; discharge especially dark, clotted; ringing in ears; loss of sight, fainting.
Ferr-m
- Menses too early, too profuse, too long-lasting; fiery red face; cease for a day or two and then return; flow pale, watery also debilitating.
- In detail, Metrorrhagia with red, flushed face partly fluid also partly clotted blood; labour-like pains.
Secale
- Generally, Best adapted to thin, scrawny women. In detail, Copious dark fluid, flow may come in gushes and is preceded by strong bearing down pains.
- Continuous, bloody, watery discharge between two periods or rather prolonged periods, so that it is practically speaking a continuous flooding.
- Thin, black, horribly offensive flow. Additionally, Great debility.
- Flow or hemorrhage of the aforesaid character after either delivery or abortion.
Thalspi
- Basically, Uterine hemorrhage with violent uterine colic also cramps; consequent on abortion or labor; at menopause.
- In detail, Premature menstruation; on the first day she hardly had a show, second day, hemorrhage with severe colic, vomiting and expulsion of large clots.[3]
Sabina
- Retained placenta; intense after-pains. Additionally, Menorrhagia in women who aborted readily. Inflammation of ovaries and uterus after abortion.
- Menses profuse, bright. Uterine pains extend into thighs. In detail, Threatened miscarriage.
- Sexual desire increased.
- Besides this, Leucorrhea after menses, corrosive, offensive. Discharge of blood between periods, with sexual excitement. Promotes expulsion of moles especially from uterus.
- Pain from sacrum to pubis, also from below upwards shooting up the vagina.
- All in all, Hemorrhage; partly clotted; worse from least motion.[5]
Pulsatilla
- Hemorrhage ceases for a little while also then recommences with redoubled force.
- Blood may be dark also mixed with coagulated lumps. [4]
Diet & Regimen
Diet & Regimen
For menorrhagia
Diet:
- Iron-rich foods: Heavy bleeding can lead to iron deficiency anemia. Prioritize:
- Red meat, poultry, and fish
- Leafy green vegetables (spinach, kale)
- Legumes (lentils, beans)
- Fortified cereals and bread
- Vitamin C: Enhances iron absorption. Include:
- Citrus fruits
- Berries
- Tomatoes
- Peppers
- Vitamin K: Plays a role in blood clotting. Good sources include:
- Leafy green vegetables
- Broccoli
- Brussels sprouts
- Omega-3 fatty acids: May help reduce inflammation and cramping. Find them in:
- Fatty fish (salmon, tuna)
- Flaxseeds
- Walnuts
- Hydration: Drink plenty of water to replenish fluids lost during heavy bleeding.
- Limit: Alcohol and caffeine, which can worsen symptoms.
Regimen:
- Stress management: Stress can exacerbate menstrual symptoms. Practice relaxation techniques like yoga, meditation, or deep breathing.
- Regular exercise: Moderate exercise can improve blood circulation and reduce cramping.
- Maintain a healthy weight
- Avoid smoking: Smoking can worsen menstrual cramps and increase the risk of heavy bleeding.
- Herbal remedies: Some herbs like ginger and chamomile may help with pain and inflammation. Consult a healthcare professional before using herbal remedies.
Do’s and Don'ts
Do’s and Don’ts
Menorrhagia do’s and don’ts
Do’s:
- Seek Medical Attention: Consult a healthcare professional for proper diagnosis and to rule out any underlying medical conditions.
- Track Your Periods: Keep a record of your menstrual cycle, noting the duration, flow, and any associated symptoms. This information can help your doctor assess the severity of your condition and determine the best course of treatment.
- Maintain a Healthy Lifestyle: Eat a balanced diet rich in iron, exercise regularly, and manage stress to promote overall health and potentially reduce the severity of menorrhagia.
- Take Iron Supplements: If you have iron-deficiency anemia due to heavy bleeding, your doctor may recommend iron supplements to replenish iron stores.
- Use Appropriate Menstrual Products: Choose sanitary pads or tampons with higher absorbency to manage heavy flow. Consider using menstrual cups or period underwear for added protection and comfort.
- Manage Pain: Over-the-counter pain relievers like ibuprofen or naproxen can help alleviate menstrual cramps. Warm compresses or a heating pad on the lower abdomen may also provide relief.
- Consider Hormonal Therapy: In some cases, hormonal contraceptives like birth control pills or hormonal IUDs can help regulate menstrual cycles and reduce heavy bleeding.
Don’ts:
- Ignore Heavy Bleeding: Heavy menstrual bleeding is not normal and should not be ignored. Seek medical attention if your periods are consistently heavy or interfere with your daily life.
- Self-Medicate: Avoid taking over-the-counter medications or herbal supplements without consulting your doctor, as they may interact with other medications or worsen the condition.
- Overexert Yourself: During heavy bleeding episodes, avoid strenuous activities and prioritize rest to conserve energy and reduce fatigue.
- Neglect Your Emotional Well-being: Menorrhagia can take a toll on your emotional health. Don’t hesitate to seek support from friends, family, or a therapist if you are feeling stressed, anxious, or depressed.
- Delay Seeking Help: If your symptoms worsen or if you experience any unusual bleeding patterns, consult your doctor promptly for further evaluation and treatment.
Terminology
Terminology
- Menorrhagia: Excessive menstrual bleeding in terms of duration (more than 7 days) or volume (more than 80 ml per cycle).
- Metrorrhagia: Bleeding between periods or irregular uterine bleeding.
- Menometrorrhagia: A combination of both menorrhagia and metrorrhagia, characterized by heavy and irregular bleeding.
- Dysmenorrhea: Painful menstruation, often accompanied by cramping in the lower abdomen.
- Oligomenorrhea: Infrequent menstrual periods, occurring less often than every 35 days.
- Amenorrhea: Absence of menstruation for three or more consecutive cycles.
- Polymenorrhea: Frequent menstrual periods, occurring more often than every 21 days.
- Hypermenorrhea: Increased menstrual flow without a change in the cycle’s length.
- Hypomenorrhea: Decreased menstrual flow with a regular cycle.
- AUB (Abnormal Uterine Bleeding): A broad term encompassing any deviation from normal menstrual bleeding patterns, including variations in frequency, duration, or volume.
- DUB (Dysfunctional Uterine Bleeding): Abnormal uterine bleeding not caused by a structural abnormality or systemic disease, often related to hormonal imbalances.
- PCOS (Polycystic Ovary Syndrome): A hormonal disorder characterized by irregular periods, excess androgens (male hormones), and multiple cysts on the ovaries.
- Endometriosis: A condition where tissue similar to the lining of the uterus grows outside the uterus.
- Fibroids: Benign tumors that grow in the uterus.
- Adenomyosis: A condition where the lining of the uterus grows into the muscular wall of the uterus.
- Endometrial Polyps: Small, benign growths on the lining of the uterus.
- Von Willebrand Disease: An inherited bleeding disorder that can cause heavy menstrual bleeding.
- Hysteroscopy: A procedure that allows a doctor to look inside the uterus using a thin, lighted tube.
- Endometrial Ablation: A procedure that destroys the lining of the uterus to reduce menstrual bleeding.
- Hysterectomy: Surgical removal of the uterus.
Remedies:
These are substances derived from plants, minerals, or animals, diluted and potentized to stimulate the body’s healing response. Examples for menorrhagia include:
- Phosphorus: For bright red, profuse bleeding with a tendency to clot.
- Sabina: For heavy bleeding with pain extending from the back to the pubic bone.
- Calcarea carbonica: For heavy bleeding with a feeling of coldness and bloating.
- Secale cornutum: For prolonged, dark, offensive bleeding with a weak and exhausted feeling.
- Ipecacuanha: For bright red, gushing bleeding with nausea and vomiting.
References
References
- DC DUTTA’s GYNECOLOGY
- https://www.thewomens.org.au/health-information/periods/healthy-periods/exercise-diet-periods#:~: text=Avoid%20saturated%20 fats%20such%20as,tofu%2C%20 broccoli%20and%20bok%20choy.
- The Homoeopathic Prescriber By K. C. Bhanja
- The Homoeopathic Prescriber By K. C. Bhanja
- Materia Medica By Boericke W.
- https://www.mayoclinic.org/diseases-conditions/menorrhagia/diagnosis-treatment/drc-20352834
- https://www.verywellhealth.com/an-overview-of-metrorrhagia-4584380#toc-diagnosis
- Balgir RS. Inherited bleeding disorders in Indian women with menorrhagia. Platelets. 2003 Mar;14(2):83-8. doi: 10.1080/0953710031000090695. PMID: 12614371.
- Prajapati VP, Patel PR. A Study of Demographic Profile and Evaluation of Menorrhagia. Indian Journal of Applied Research. 2014 January; Volume : 4 | Issue : 1 | Page : 83-85.
- Sharma S, Sharma P, Tyler LN, Kapoor S. Menstruation and related disorders in Indian adolescent girls: an observational study. Indian J Endocrinol Metab. 2021 Nov-Dec;25(6):582-588. doi: 10.4103/ijem.ijem_806_21. PMID: 34900540; PMCID: PMC8653880.
- Menorrhagia and Dysmenorrhea: Risk Factors, Diagnosis, and Management by Charles S. Debrovner, Ilaria Erasmo, Simone Ferrero (2018)
- Clinical Disorders of the Endometrium and Menstrual Cycle (1997) by Iain T. Cameron, Ian S. Fraser, Stephen K. Smith
- Clinical Gynecologic Endocrinology and Infertility (2019) Marc A. Fritz, Leon Speroff (9th edition, Lippincott Williams & Wilkins)
- Practical Manual of Menstrual Disorders (2016) by David F. Archer
- Management of Menstrual Disorders by Elizabeth A. Stewart, Paula J. Adams Hillard, 2014
- Clinical Gynecology (3rd Edition, 2011) by Eric J. Bieber, Arthur L. Herbst. Elsevier.
- Comprehensive Gynecology (7th Edition, 2017) William’s Gynecology. McGraw Hill Professional.
- Yen & Jaffe’s Reproductive Endocrinology (8th Edition, 2019) Jerome F. Strauss III, Robert L. Barbieri. Elsevier.
- The Period Repair Manual: Natural Treatment for Better Hormones and Better Periods (2018) Lara Briden
Also Search As
Also Search As
People can search for homeopathic articles on menorrhagia using various online resources and strategies, including:
Search engines:
- Use specific keywords: Try searches like "homeopathy for menorrhagia," "homeopathic remedies for heavy periods," or "homeopathic treatment for excessive menstrual bleeding."
- Include additional terms: To refine your search, add terms like "case studies," "research," "clinical trials," or "reviews" to find specific types of articles.
- Utilize advanced search options: Most search engines offer advanced search features, allowing you to filter results by date, language, or file type (e.g., PDF).
Homeopathic websites and databases:
- Explore dedicated websites: Many homeopathic organizations and clinics have websites with articles, blogs, and case studies related to menorrhagia and other women’s health issues.
- Search homeopathic databases: Some online databases, like Hompath or RadarOpus, allow you to search for homeopathic remedies and case studies related to specific conditions.
Social media and online forums:
- Follow homeopathic groups and pages: Many social media platforms have groups and pages dedicated to homeopathy, where you can find articles, discussions, and recommendations for resources on menorrhagia.
- Participate in online forums: Join online forums related to homeopathy or women’s health to connect with others who may have experience with homeopathic treatment for menorrhagia.
Libraries and bookstores:
- Visit your local library: Many libraries have a collection of books and journals on homeopathy, including resources on specific conditions like menorrhagia.
- Browse homeopathic bookstores: Specialty bookstores dedicated to homeopathy may carry a wider selection of books and publications on this topic.
Tips for Effective Searching:
- Be specific: Use clear and concise keywords to describe your search query.
- Use multiple search terms: Try different combinations of keywords to broaden your search.
- Evaluate sources critically: Consider the credibility and expertise of the author or publication before relying on the information presented.
- Consult a homeopath: For personalized advice and treatment recommendations, consult a qualified homeopath.
By utilizing these resources and strategies, you can find valuable information and insights into the homeopathic approach to managing menorrhagia.
People can search for information on menorrhagia in various ways, utilizing different resources and search strategies:
Online resources:
- Search engines: Using popular search engines like Google, Bing, or DuckDuckGo, people can enter keywords such as "menorrhagia," "heavy menstrual bleeding," or "causes of heavy periods" to find relevant articles, websites, and medical information.
- Medical websites: Reputable medical websites like Mayo Clinic, WebMD, or the National Institutes of Health (NIH) provide reliable information on menorrhagia, including its symptoms, causes, diagnosis, and treatment options.
- Online health forums and communities: Online forums and communities dedicated to women’s health can offer support and shared experiences from individuals dealing with menorrhagia. These platforms may also provide insights into alternative therapies and coping mechanisms.
- Social media: Social media platforms like Facebook, Twitter, or Instagram can be used to connect with support groups and organizations that provide information and resources related to menorrhagia.
Offline resources:
- Healthcare professionals: Consulting a doctor, gynecologist, or other healthcare professionals is crucial for accurate diagnosis and personalized treatment recommendations for menorrhagia.
- Medical libraries: Medical libraries in hospitals or universities offer access to a vast collection of medical textbooks, journals, and research papers on menorrhagia and related topics.
- Support groups: Local support groups for women with menstrual disorders can provide a safe space for sharing experiences, receiving emotional support, and learning about coping mechanisms for menorrhagia.
- Books and publications: Various books and publications on women’s health and menstrual disorders can provide detailed information on menorrhagia, including its causes, symptoms, and treatment options.
Tips for Effective Searching:
- Use specific keywords: Using precise keywords like "menorrhagia treatment options" or "causes of heavy periods during menopause" can help refine search results.
- Consider trusted sources: Rely on information from reputable medical websites, healthcare professionals, and peer-reviewed medical journals.
- Be mindful of potential biases: When seeking information online, be aware of potential biases in blogs, forums, or social media posts. Always cross-reference information with reliable sources.
- Consult a healthcare professional: For personalized advice and treatment recommendations, always consult a qualified healthcare professional.
Remember, seeking information from reliable sources and consulting a healthcare professional is crucial for understanding and managing menorrhagia effectively.
Frequently Asked Questions (FAQ)
What is Menorrhagia?
Menorrhagia is defined as cyclic bleeding at normal intervals; the bleeding is either excessive in amount (> 80 mL) or duration (>7 days) or both.
What causes Menorrhagia?
- Fibroid uterus
- Adenomyosis
- Pelvic endometriosis
- IUCD inutero
- Liver dysfunction
- Congestive cardiac failure
- Severe hypertension
- Hypothyroidism, Hyperthyroidism
- Leukemia
- Emotional upset
How is menorrhagia diagnosed?
Menorrhagia is diagnosed through a combination of medical history review, physical examination, and additional tests like blood tests, ultrasound, or hysteroscopy.
What are the symptoms of Menorrhagia?
- Soaking through one or more sanitary pads or tampons every hour for several consecutive hours.
- Needing to use double sanitary protection to control your menstrual flow.
- Needing to wake up to change sanitary protection during the night.
- Bleeding for longer than a week.
- Passing blood clots larger than a quarter.
- Restricting daily activities due to heavy menstrual flow.
- Symptoms of anemia, such as tiredness, fatigue or shortness of breath
When should I see a doctor for menorrhagia?
If you experience heavy menstrual bleeding that interferes with your daily life, lasts longer than seven days, or is accompanied by severe pain or other unusual symptoms, consult a doctor for diagnosis and treatment.
Can homeopathy treat menorrhagia?
Yes, homeopathy offers a holistic approach to managing menorrhagia by addressing the underlying causes and individualizing treatment based on specific symptoms.
Is homeopathic treatment for menorrhagia safe?
Homeopathic remedies are generally considered safe when prescribed by a qualified practitioner.
However, it is essential to consult a homeopath before self-treating.
How does homeopathic treatment for menorrhagia work?
Homeopathic remedies aim to stimulate the body’s self-healing mechanisms and restore balance to the vital force, thereby reducing heavy bleeding and associated symptoms.
How long does it take to see results with homeopathic treatment for menorrhagia?
The duration of treatment varies depending on individual factors, but some women may experience improvement in their symptoms within a few weeks or months of starting homeopathic treatment.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Menorrhagia?
Homoeopathic Medicines for Menorrhagia
- Cal carb
- China
- Ferr met
- Secale
- Thalspi
- Sabina
- Pulsatilla
