Polycystic Ovarian Syndrome PCOS
Definition
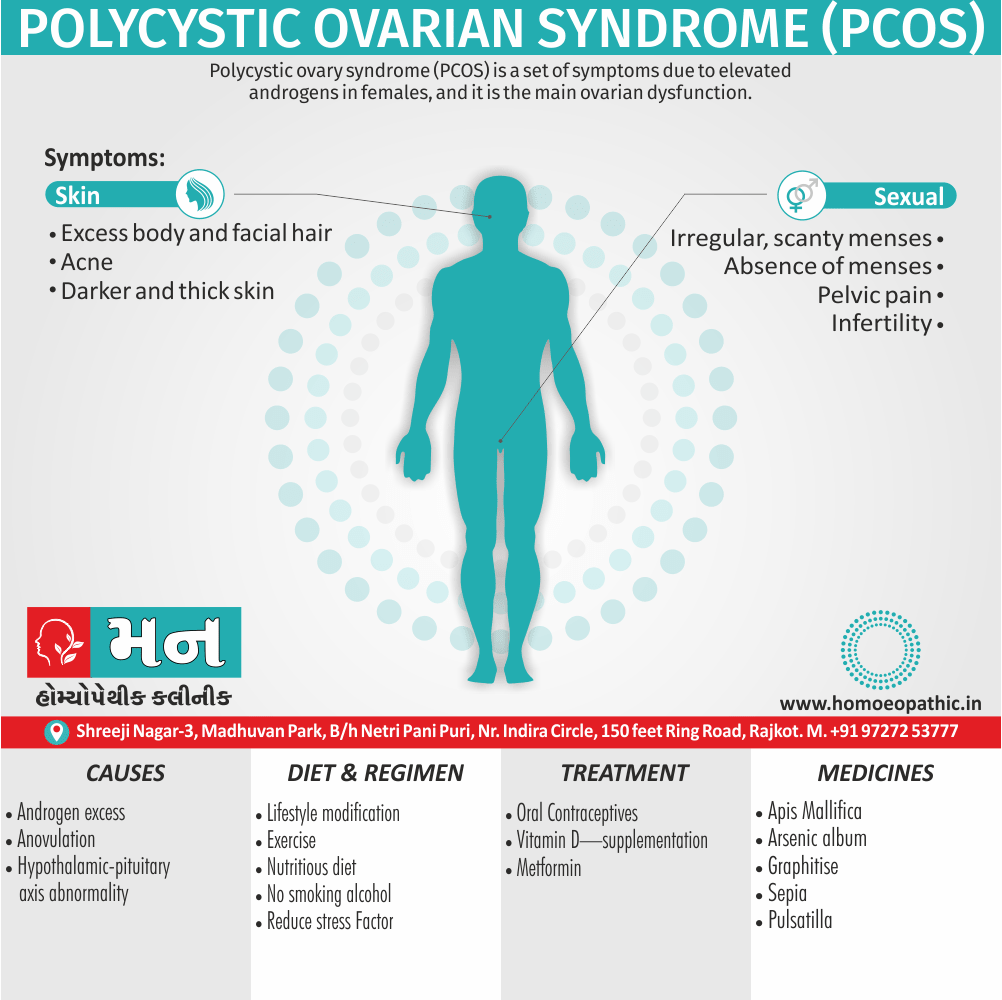
Polycystic ovary syndrome (PCOS) is a set of symptoms due to elevated androgens in females, and it is the main ovarian disfunction.[1]
There are a few other terms you might encounter related to PCOS, though "PCOS" itself is the most common:
- Polycystic Ovarian Disease (PCOD)
- Polycystic ovarian syndrome (full name)
- Sclerocystic ovarian disease
- Stein-Leventhal syndrome
- Anovulation with hyperandrogenism (more technical term)
- Rotterdam criteria (diagnostic criteria, not a synonym but sometimes used in this context)
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Polycystic Ovarian Syndrome
This heterogenous disorder is characterized by excessive androgen production by the ovaries mainly. PCOS is a multifactorial and polygenic condition. Diagnosis is based upon the presence of any two of the following three criteria
- Oligo and/or anovulation.
- Hyperandrogenism (clinical and/or biochemical).
- Polycystic ovaries.
Another etiologist (CAH, thyroid dysfunction, hyperprolactinemia, Cushing syndrome) are to be excluded. The incidence varies between 0.5–4 percent, more common amongst infertile women.
It is prevalent in young reproductive age group (20–30%). Additionally, Polycystic ovary may be seen in about 20% of normal women.[1]
Epidemiology
Epidemiology
The prevalence of Polycystic Ovarian Syndrome (PCOS) in India ranges from 3.7% to 22.5%, making it a significant health concern for women of reproductive age. (Polycystic Ovarian Syndrome (PCOS) and its Complications – PIB, 2023). [4]
Causes
Causes
Potential Contributing Factors:
- Hormonal Imbalances: Excess androgens (male hormones) and insulin resistance are commonly seen in PCOS, leading to irregular periods, acne, and excess hair growth.
- Genetics: A family history of PCOS increases a woman’s risk of developing the condition, suggesting a genetic predisposition.
- Environmental Factors: Exposure to certain environmental toxins or endocrine-disrupting chemicals might play a role in PCOS development.
- Lifestyle Factors: Obesity and a sedentary lifestyle can worsen PCOS symptoms and increase the risk of complications like heart disease and diabetes. [5]
Types
Types
While PCOS presents with diverse symptoms and underlying mechanisms, it’s not traditionally classified into distinct types in the same way as other medical conditions. However, recent research and clinical observations have led to the identification of several subtypes or phenotypes of PCOS, each with its own set of characteristics:
Phenotypes of PCOS:
Insulin-Resistant PCOS: This is the most common type, characterized by high insulin levels, often associated with obesity and metabolic syndrome. It’s associated with increased androgen production and ovulatory dysfunction.
Inflammatory PCOS: Chronic low-grade inflammation is a hallmark of this type, potentially contributing to insulin resistance and hormonal imbalances.
Adrenal PCOS: This less common type is linked to excess androgen production from the adrenal glands rather than the ovaries.
Hidden-Cause PCOS: In some cases, the underlying cause of PCOS remains elusive, despite fulfilling the diagnostic criteria. [5]
Risk Factors
Risk Factors for Polycystic Ovarian Syndrome (PCOS)
While the exact cause of PCOS remains elusive, several factors have been identified that can increase a woman’s risk of developing this complex condition:
1. Family History:
- Having a mother or sister with PCOS significantly increases a woman’s risk, suggesting a strong genetic component.
2. Hormonal Imbalances:
- Excess androgens (male hormones) and insulin resistance are common features of PCOS.
3. Lifestyle Factors:
- Obesity and a sedentary lifestyle can exacerbate PCOS symptoms and increase the risk of associated complications.
4. Environmental Factors:
- Exposure to endocrine-disrupting chemicals might play a role, although research in this area is ongoing.
5. Other Risk Factors:
- Low-grade chronic inflammation
- Early onset of puberty
- Certain ethnicities may have a higher prevalence [5]
Pathogenesis
Pathogenesis of Polycystic Ovarian Syndrome (PCOS)
PCOS is a complex disorder with a multifaceted pathogenesis involving several interconnected pathways:
Neuroendocrine Dysregulation: The hypothalamic-pituitary-ovarian (HPO) axis, responsible for regulating ovulation and hormone production, is disrupted in PCOS. This leads to increased pulsatile secretion of gonadotropin-releasing hormone (GnRH) and luteinizing hormone (LH), resulting in excess androgen production and follicular arrest.
Hyperandrogenism: Elevated levels of androgens, primarily testosterone, play a crucial role in PCOS pathogenesis. These androgens contribute to anovulation, hirsutism, acne, and other clinical manifestations.
Insulin Resistance: Many women with PCOS exhibit insulin resistance, leading to hyperinsulinemia. High insulin levels stimulate ovarian androgen production and further disrupt the HPO axis.
Ovarian Dysfunction: The ovaries in PCOS are characterized by numerous small follicles that fail to mature and ovulate, leading to chronic anovulation and infertility.
Genetic and Environmental Factors: Genetic predisposition and exposure to environmental factors, such as endocrine-disrupting chemicals, are believed to interact with the above pathways, contributing to the development of PCOS. [5]
Pathophysiology
Pathophysiology
Exact pathophysiology of PCOS is not clearly understood. It may be discussed under the following heads (scheme–6) i.e.:
(a)Hypothalamic pituitary compartment abnormality.
(b) Androgen excess
(c) Anovulation.
(d) Obesity also insulin resistance.
(e) Long-term consequences.
Hypothalamic pituitary compartment in PCOS i.e.
- Increased pulse frequency of GnRH leads to increased pulse frequency of LH. Leptin (a peptide, secreted by fat cells also by the ovarian follicle), insulin resistance and hyperandrogenemia are responsible for this.
- GnRH is preferential to LH rather than FSH.
- Increased pulse frequency and amplitude of LH results in tonically elevated level of LH.
- Lastly, The LH: FSH ratio is increased.[1]
Clinical Features
Clinical Features
The patient complains of increasing i.e.
- Obesity (abdominal – 50%),
- Menstrual abnormalities (70%) in the form of oligomenorrhea, either amenorrhea or DUB and infertility.
- Presence of hirsutism also acne are the important features (70%).
- Virilism is rare.[1]
Acanthosis nigricans i.e.
is characterized by specific skin changes due to insulin resistance. Additionally, The skin is thickened and pigmented (grey brown). Commonly affected sites are nape of the neck, inner thighs, groin also axilla.
Androgen Excess i.e.
Abnormal regulation of the androgen forming enzyme (P450 C 17) is thought to be the main cause for excess production of androgens from the ovaries and adrenals. The principal sources of androgens are i.e.
(A) Ovary
(B) Adrenal
(C) Systemic metabolic alteration.[1]
A. Ovary produces excess androgens due to —
(i) stimulation of theca cells by high LH
(ii) P450 C17 enzyme hyperfunction
(iii) defective aromatization of androgens to estrogen
(iv) stimulation of theca cells by IGF-1 (insulin growth factor-1)
B. Adrenals
are stimulated to produce excess androgens by i.e.
(i) stress
(ii) P450 C17 enzyme hyperfunction
(iii) associated high prolactin level (20%).
C. Systemic metabolic alteration
(i) Hyperinsulinemia causes i.e.:
(a) Stimulation of theca cells to produce more androgens.
(b) Insulin results in more free IGF-1. By autocrine action, IGF-1 stimulates theca cells to produce more androgens.
(c) Insulin inhibits hepatic synthesis of SHBG, resulting in more free level of androgens. Features suggestive of insulin resistance are:
BMI > 25 kg/m, Acanthosis nigricans and waist to hip ratio > 0.85.[1]
(ii) Hyperprolactinemia i.e.:
In about 20% cases, there may be mild elevation of prolactin level due to increased pulsitivity of GnRH or due to dopamine deficiency or both. The prolactin further stimulates adrenal androgen production Whatever may be the etiology, the endocrinologic effects of PCOS produce a vicious cycle of events as shown in the scheme–6.
Anovulation i.e.:
Because of low FSH level, follicular growth arrest at different phases of maturation (2–10 mm diameter). The net effect diminish oestradiol and increased inhibin production. Due to elevated LH, there is hypertrophy of theca cells and more androgens are produced either from theca cells or stroma. There defective FSH induce aromatization of androgens to oestrogens.
Follicular microenvironment is therefore more androgenic rather than estrogenic.
Unless there is estrogenic follicular microenvironment, follicular growth, maturation and ovulation cannot occur. There is huge number of atretic follicles that contribute to increased ovarian stroma (hyperthecosis). LH level is tonically elevated Without any surge. LH Surge is essential for ovulation to occur.[1]
Obesity and Insulin Resistance
Obesity (central) recognize as an important contributory factor. Apart from excess production of androgens, obesity also associate with reduced SHBG. It also induces insulin resistance and hyperinsulinemia Which in turn increases the gonadal androgen production.
PCOS Is thought to have a dominant mode of inheritance as about 50% of first-degree relatives have PCOS. Aetiology of insulin resistance unknown. Mutations of the insulin receptor gene in the peripheral target tissues and reduced tyrosine autophosphorylation of the insulin receptor, currently thought to an important cause. Increased central body fat leads to android obesity.
- Long-term consequences in a patient suffering from PCOS includes: The excess androgens (mainly androstenedione) either from the ovaries or adrenals peripherally aromatize to estrone (E1). There concomitant diminish SHBG. Cumulative excess unbound E2 and estrone results in a tonic hyperestrogenic state. There is endometrial hyperplasia.[1]
Sign & Symptoms
Signs & Symptoms of Polycystic Ovarian Syndrome (PCOS)
PCOS manifests with a wide range of signs and symptoms, varying in severity from woman to woman. These manifestations can impact various aspects of a woman’s health and well-being:
Reproductive and Menstrual Irregularities:
- Irregular periods: Infrequent, prolonged, or absent menstrual cycles are common due to anovulation (lack of ovulation).
- Infertility: Difficulty conceiving due to irregular or absent ovulation.
Hyperandrogenism (Excess Male Hormones):
- Hirsutism: Excess hair growth on the face, chest, back, or abdomen.
- Acne: Persistent or severe acne outbreaks.
- Male-pattern baldness: Thinning hair or hair loss on the scalp.
Metabolic and Endocrine Abnormalities:
- Insulin resistance: Increased risk of developing type 2 diabetes.
- Obesity: Weight gain or difficulty losing weight.
- Acanthosis nigricans: Dark, velvety patches of skin on the neck, armpits, or groin.
Other Symptoms:
- Fatigue
- Mood swings
- Sleep apnea
- Depression and anxiety [5]
Clinical Examination
Clinical Examination of Polycystic Ovarian Syndrome (PCOS)
The clinical examination for PCOS involves a comprehensive assessment to identify signs and symptoms indicative of the condition and its potential complications.
1. Detailed Medical History:
- Menstrual history: Irregular, infrequent, or absent periods.
- Fertility concerns: Difficulty conceiving.
- Symptoms of hyperandrogenism: Hirsutism, acne, male-pattern baldness.
- Family history of PCOS or related conditions.
- Past medical history, including metabolic and endocrine disorders.
2. Physical Examination:
- General assessment: Body mass index (BMI), waist circumference, blood pressure.
- Skin examination: Acne, hirsutism, acanthosis nigricans (darkening of skin folds).
- Pelvic examination: May reveal enlarged ovaries but is often unremarkable.
3. Additional Assessments:
- Laboratory Tests:
- Hormone levels: LH, FSH, testosterone, androgens, prolactin, thyroid hormones.
- Glucose and insulin levels: To assess insulin resistance and risk of diabetes.
- Lipid profile: To evaluate cardiovascular risk.
- Imaging:
- Pelvic ultrasound: To visualize the ovaries and assess the presence of multiple small follicles. [5]
Diagnosis
Diagnosis of Polycystic Ovarian Syndrome (PCOS)
PCOS diagnosis is primarily based on the Rotterdam Criteria established in 2003, which require the presence of at least two of the following three criteria after excluding other potential causes:
Oligo- or Anovulation: Infrequent or absent ovulation, typically manifesting as irregular or absent menstrual periods.
Hyperandrogenism: Clinical (hirsutism, acne) or biochemical (elevated androgen levels) evidence of excess male hormones.
Polycystic Ovaries: The presence of 12 or more follicles in one or both ovaries on ultrasound, or an ovarian volume greater than 10 ml. [5]
Differential Diagnosis
Differential Diagnosis of Polycystic Ovarian Syndrome (PCOS)
Several other conditions can mimic the signs and symptoms of PCOS, making it essential to consider a differential diagnosis:
Congenital Adrenal Hyperplasia (CAH): A genetic disorder leading to excess androgen production, causing hirsutism, acne, and menstrual irregularities.
Androgen-Secreting Tumors: Rare tumors of the ovaries or adrenal glands can produce excess androgens, mimicking PCOS symptoms.
Hypothyroidism: An underactive thyroid gland can cause irregular periods, weight gain, and fatigue, overlapping with PCOS symptoms.
Hyperprolactinemia: Elevated prolactin levels can lead to irregular periods and infertility, resembling PCOS presentation.
Cushing’s Syndrome: Excess cortisol production can cause weight gain, hirsutism, and acne, making it necessary to differentiate from PCOS. [5]
Complications
Complications of Polycystic Ovarian Syndrome (PCOS)
PCOS is associated with an increased risk of various long-term health complications, impacting multiple organ systems and overall quality of life.
Metabolic Complications:
- Type 2 Diabetes: Insulin resistance and hyperinsulinemia significantly increase the risk of developing type 2 diabetes.
- Metabolic Syndrome: A cluster of conditions including obesity, high blood pressure, high blood sugar, and abnormal cholesterol levels, raising the risk of heart disease and stroke.
- Non-alcoholic Fatty Liver Disease (NAFLD): Increased risk of fatty liver deposition, potentially leading to liver damage and dysfunction.
Reproductive Complications:
- Infertility: Chronic anovulation can make it difficult to conceive naturally.
- Miscarriage: PCOS is associated with a higher risk of miscarriage.
- Gestational Diabetes: Increased risk of developing diabetes during pregnancy.
- Pregnancy-induced Hypertension: High blood pressure during pregnancy can complicate both maternal and fetal health.
Cardiovascular Complications:
- Cardiovascular Disease: Increased risk of heart disease, stroke, and atherosclerosis due to associated metabolic abnormalities.
- Endothelial Dysfunction: Impaired blood vessel function can further contribute to cardiovascular risk.
Other Complications:
- Obstructive Sleep Apnea: Increased risk of sleep-disordered breathing, impacting sleep quality and overall health.
- Depression and Anxiety: Hormonal imbalances and the challenges of living with PCOS can increase the risk of mental health issues.
- Endometrial Cancer: Chronic anovulation and unopposed estrogen exposure can increase the risk of endometrial hyperplasia and cancer. [5]
Investigations
Investigation
Sonography — Transvaginal sonography is especially useful in higher-weight person. Ovaries enlarge in volume (> 10 cm). Increased number (> 12) of peripherally arranged cysts (2–9 mm) are Seen.
Serum values i.e.:
- LH level elevate and/or the ratio LH: FSH is > 2:1.
- Raised level of estradiol and estrone — The estrone level markedly elevate.
- SHBG level reduce.
- Hyperandrogenism—mainly from the ovary but less from the adrenals. Andro-stenedione raise.
- Raised serum testosterone (> 150 ng/dL) and DHEA–S may marginally elevate.
- Insulin Resistance (IR): Raised fasting insulin levels > 25 µIU/mL and fasting glucose/insulin ratio < 4.5 suggests IR (50%). Levels of serum insulin response > 300 µIU/mL at 2 hours post glucose (75 gm) load, suggests severe IR.
- Laparoscopy — Bilateral polycystic ovaries are
characteristic of PCOS [1]
Treatment
Treatment of Polycystic Ovarian Syndrome
The primary treatments for Polycystic Ovarian Syndrome include: lifestyle changes and medications. [2]
Goals of treatment may be considered under four categories i.e.:
- Lowering of insulin resistance levels
- Restoration of fertility
- Treatment of hirsutismor acne
- Restoration of regular menstruation, and prevention of endometrial hyperplasiaand endometrial cancer
In each of these areas, there is considerable debate as to the optimal treatment. One of the major reasons for this is the lack of large-scale clinical trials comparing different treatments. Smaller trials tend to be less reliable and hence may produce conflicting results. General interventions that help to reduce weight or insulin resistance can be beneficial for all these aims, because they address what is believed to be the underlying cause.
As Polycystic Ovarian Syndrome appears to cause significant emotional distress, appropriate support may be useful. [2]
Medications
Medications for PCOS include
[1] Oral contraceptives i.e.
: The oral contraceptives increase sex hormone binding globulin production, which increases binding of free testosterone. This reduces the symptoms of hirsutism caused by high testosterone and regulates return to normal menstrual periods.
[2] Metformin i.e.
is a medication commonly used in type 2 diabetes mellitus to reduce insulin resistance, and is used off label (in the UK, US, AU also EU) to treat insulin resistance seen in PCOS. In many cases, metformin also supports ovarian function and return to normal ovulation.
[3] Spironolactone i.e.
can be used for its antiandrogenic effects, and the topical cream eflornithine can be used to reduce facial hair. A newer insulin resistance medication class, the thiazolidinediones (glitazones), have shown equivalent efficacy to metformin, but metformin has a more favorable side effect profile.
It can be difficult to become pregnant with PCOS because it causes irregular ovulation. Medications to induce fertility when trying to conceive include the ovulation inducer clomiphene or pulsatile leuprorelin. Metformin improves the efficacy of fertility treatment when used in combination with clomiphene. Evidence from randomized controlled trials suggests that in terms of live birth, metformin may be better than placebo, and metformin plus clomiphene may be better than clomiphene alone, but that in both cases women may be more likely to experience gastrointestinal side effects with metformin.
Metformin
is thought to be safe to use during pregnancy (pregnancy category B in the US). A review in 2014 concluded that the use of metformin does not increase the risk of major birth defects in women treated with metformin during the first trimester. Liraglutide may reduce weight and waist circumference more than other medications.[2]
Prevention
Prevention
Polycystic Ovarian Syndrome (PCOS) is a common hormonal disorder affecting women of reproductive age. While there’s no definitive cure, research suggests that certain lifestyle modifications and interventions can significantly reduce the risk of developing PCOS or manage its symptoms.
Preventive Strategies
While research is ongoing, evidence suggests the following strategies may help prevent or manage PCOS:
Lifestyle Modifications
Maintain a Healthy Weight:
Weight loss, even a modest 5-10%, can improve insulin sensitivity and hormonal balance
Regular Exercise:
Aim for at least 150 minutes of moderate-intensity exercise per week to enhance insulin sensitivity and reduce androgen levels
Stress Management:
Chronic stress can exacerbate hormonal imbalances. Practice relaxation techniques like yoga, meditation, or deep breathing exercises
Quality Sleep:
Aim for 7-8 hours of uninterrupted sleep each night to support overall health and hormonal regulation
Dietary Interventions
Balanced Diet:
Focus on whole foods, including fruits, vegetables, lean proteins, and healthy fats
Low Glycemic Index (GI) Foods:
Choose foods that release glucose slowly into the bloodstream to help regulate insulin levels
Anti-inflammatory Foods:
Incorporate foods rich in antioxidants and omega-3 fatty acids to reduce inflammation
Supplements
Inositol:
This naturally occurring compound has shown promise in improving insulin sensitivity and reducing androgen levels
Vitamin D:
Studies suggest that vitamin D deficiency may be associated with PCOS. Supplementation may help improve hormonal balance and menstrual regularity
Other Potential Supplements:
Consult with a healthcare professional before taking any supplements, as some may interact with medications or have side effects
Homeopathic Treatment
Homoeopathic Medicine:
Apis Mellifica [Apis.]
Few remedies cause as many ovarian symptoms as Apis. It has an active congestion of the right ovary going on to ovaritis, with soreness in the inguinal region, burning, stinging and tumefaction. Ovarian cysts in their incipiency have been arrested by this remedy; here one of the indicating features is numbness down the thigh. It has also proved useful in affections of the left ovary. Tightness of the chest may also be present, with the occurrence of a reflex cough and urging to urinate. Mercurius corrosivus. Hughes prefers this remedy in ovarian neuralgia. Peritoneal complications also indicate it. Bovista has also cured ovarian tumors.[3]
Arsenicum. [Ars]
Burning tensive pains in the ovaries, especially in the right. Ovaritis relieved by hot applications. Patient thirsty, irritable and restless. Colocynth. Ovarian colic; griping pains, relieved by bending double; stitching pains deep in right ovarian region. It is also a useful remedy, according to Southwick, in ovaritis of left ovary with colicky pains. A dropsical condition may be present. Hamamelis. Ovaritis and ovarian neuralgia. Ludlam praises this remedy in the sub-
acute form of gonorrhoeal ovaritis; it allays the pain and averts the menstrual derangement. Ovaritis after a blow. There is agonizing soreness all over the abdomen. An external application of hot extract of Hamamelis acts marvelously in subduing the distress and pain consequent to ovaritis. Iodine. Either Congestion or dropsy of the right ovary. Dwindling of the mammae; dull, pressing, wedge-like pain, extending from right ovary to uterus like a plug, worse during menstruation. Thuja. Left-sided ovaritis, with suspicion of veneral taint, calls for Thuja. Grumbling pains in the ovaries all the time, with mental irritability, call for Thuja. Podophyllum has a pain in the right ovary, running down the thigh of that side. Numbness may be an attending symptom.[3]
Belladonna. [Bell]
As this remedy is one particularly adapted to glandular growths it is especially useful in acute ovaritis, and more so if the peritoneum be involved. The pains are clutching and throbbing, worse especially on the right side, the slightest jar is painful, and the patient is extremely sensitive. The symptoms appear suddenly; flushed face and other Belladonna symptoms are present. Platinum. Ovaries sensitive, burning pains in them, bearing down, chronic ovarian irritation with sexual excitement. Much ovarian induration is present. Palladium. Swelling and induration of right ovary. In detail, It lacks the mental symptoms of Platinum, such as mental egotism and excitement. Aurum. Ovarian induration. Lilium. Ovarian neuralgias. Burning pains from ovary up into abdomen and down into thighs, shooting pains from left ovary across the pubes, or up to the mammary gland. Staphisagria. Very useful in ovarian irritation in nervous, irritable women. Hypochondriacal mood.
Lachesis. [Lach]
Pain in left ovary relieved by a discharge from the uterus; can bear nothing heavy on region. Hughes and Guernsey seem to think that Lachesis acts even more prominently on the right ovary; others believe the opposite, the tendency of affections being, however, to move from the left toward the right side. Suppuration and chronic enlargements of ovary may call for Lachesis. Zincum. Boring in the left ovary relieved by the flow, somewhat better from pressure; fidgety feet. Graphites. Swelling and induration of the left ovary; also pains in the right ovarian region with delayed scanty menses. Argentum metallicum. Bruised pain in left ovary and sensation as if ovary were growing large. Naja. Violent crampy pain in left ovary. Dr. Hughes valued it in obscure ovarian pains not inflammatory in nature. [3]
Sepia. [Sep]
Sepia is a remedy acting especially on the female organs and is a most valuable one; it produces in its proving venous congestion, which accounts for many of its symptoms. The general symptoms in a case calling for Sepia are of the utmost importance. Thus, we have characteristically the weakness and want of tone, in the whole system, the yellow complexion, the yellow saddle over the nose, the sunken dark-ringed eyes, the relief fro violent motion, due probably to the toning up of the venous system by such, and the amelioration in the middle of the day. These are all ground characteristics of the remedy; when they are present the other symptoms will found to correspond with the drug most beautifully. Besides this, The menstruation of Sepia may of almost any combination, late and scanty being the most frequent.
Other symptoms
They may early and scanty or early and profuse – discolorations of the skin attending menstruation are characteristic; additionally, the flow is apt to dark, the menses precede by aching in the abdomen and by colicky pains. Amenorrhea in those of distinct Sepia temperament where there is extreme sensitiveness to all impression. The leucorrhea of Sepia is yellow – green in color and somewhat offensive. Lastly, It may be milky; it is worse before the menses and is accompanied by bearing down.
On the uterus itself Sepia exerts a decided action; the uterus found to enlarge and the cervix indurate. Thus, Sepia becomes a useful remedy in displacements, especially prolapsus or retroversion’s. There is irritability of the bladder and leucorrhea. Dunham praised it highly here. There is often present a sensation as if the womb clutch and suddenly released. Bearing down pains are grandly characteristic of Sepia; the patient feels as if everything would protrude from the vulva and this sensation relieve by sitting with the limbs crossed. [3]
Diet & Regimen
Diet & Regimen
For Polycystic Ovarian Syndrome
Diet:
- Focus on whole, unprocessed foods: Load up on fruits, vegetables, and whole grains.
- Choose lean protein: Include fish, poultry, beans, lentils, and tofu in your diet.
- Healthy fats are important: Incorporate foods like avocados, nuts, seeds, and olive oil.
- Limit refined carbohydrates: Cut back on white bread, pasta, and sugary snacks.
- Control sugar intake: Be mindful of added sugars in drinks and processed foods.
- Get enough fiber: Fiber helps regulate blood sugar and improves insulin sensitivity.
Regimen:
- Regular exercise: Aim for at least 150 minutes of moderate-intensity exercise per week.
- Manage stress: Practice stress-reducing techniques like yoga, meditation, or deep breathing.
- Maintain a healthy weight: Even a small amount of weight loss can improve PCOS symptoms.
- Get enough sleep: Aim for 7-8 hours of quality sleep per night.
- Consult your doctor: Regular checkups and discussions with your doctor are crucial for managing PCOS and any related conditions
- Focus on whole, unprocessed foods: Load up on fruits, vegetables, and whole grains.
Do’s and Don'ts
Do’s and Don’ts
PCOS do’s and don’ts
Do’s:
Maintain a Healthy Weight:
- Losing even a small amount of weight can significantly improve insulin sensitivity and hormonal balance. Aim for a healthy BMI through a balanced diet and regular exercise
Prioritize a Balanced Diet:
- Focus on whole foods like fruits, vegetables, lean proteins, and healthy fats. Choose low glycemic index (GI) foods to regulate blood sugar levels
Exercise Regularly:
- Aim for at least 150 minutes of moderate-intensity exercise per week. This helps improve insulin sensitivity, reduce androgen levels, and manage weight
Manage Stress:
- Chronic stress can worsen hormonal imbalances. Practice relaxation techniques like yoga, meditation, or deep breathing exercises
Get Adequate Sleep:
- Aim for 7-8 hours of quality sleep each night to support overall health and hormonal regulation
Consult Your Doctor Regularly:
- Schedule regular checkups to monitor your condition, discuss any concerns, and adjust treatment plans as needed
Consider Supplements:
- Discuss potential supplements like Inositol or Vitamin D with your doctor, as they may help improve insulin sensitivity and hormonal balance [7]
Don’ts:
Skip Meals or Crash Diet:
- Inconsistent eating patterns can disrupt blood sugar levels and worsen insulin resistance. Focus on sustainable, healthy eating habits
Consume Processed Foods and Sugary Drinks:
- These can spike blood sugar levels and contribute to weight gain and insulin resistance
Lead a Sedentary Lifestyle:
- Lack of physical activity can worsen insulin resistance and contribute to weight gain
Ignore Mental Health:
- Stress and anxiety can exacerbate PCOS symptoms. Seek support from a therapist or counselor if needed
Self-Medicate:
- Always consult your doctor before taking any supplements or medications, as they may interact with other medications or have side effects [7]
Terminology
Terminology
Polycystic Ovarian Syndrome (PCOS):
- A hormonal disorder causing enlarged ovaries with small cysts on the outer edges.
Androgens:
- A group of male sex hormones, such as testosterone, that are present in higher than normal levels in women with PCOS.
Insulin Resistance:
- A condition where the body’s cells become less responsive to insulin, leading to high blood sugar levels.
Hyperandrogenism:
- Excessive production or secretion of androgens, leading to symptoms such as acne, hirsutism (excess hair growth), and male-pattern baldness.
Anovulation:
- The absence of ovulation, or the release of an egg from the ovary, resulting in irregular or missed periods.
Hirsutism:
- Excessive hair growth on the face, chest, back, or other areas of the body where women typically don’t have hair.
Oligomenorrhea:
- Infrequent or irregular menstrual periods.
Amenorrhea:
- The absence of menstrual periods for three or more consecutive months.
Infertility:
- Difficulty conceiving a child.
Metabolic Syndrome:
- A cluster of conditions that increase the risk of heart disease, stroke, and type 2 diabetes, including high blood pressure, high blood sugar, abnormal cholesterol levels, and excess body fat around the waist.
Endometrial Hyperplasia:
- Thickening of the lining of the uterus (endometrium) due to prolonged exposure to estrogen without progesterone.
Gestational Diabetes:
- A type of diabetes that develops during pregnancy.
Sleep Apnea:
- A sleep disorder where breathing repeatedly stops and starts during sleep.
Nonalcoholic Fatty Liver Disease (NAFLD):
- A condition where excess fat builds up in the liver, which can lead to liver damage.
Mood Disorders:
- Conditions such as depression and anxiety, which are more common in women with PCOS.
These are just a few of the key terms you might encounter when reading about PCOS.
Certainly, here are some terminologies and their meanings frequently used in homeopathic articles about Polycystic Ovarian Syndrome (PCOS):
Constitutional Remedy:
- A homeopathic medicine chosen based on the totality of the patient’s symptoms, including physical, mental, and emotional characteristics.
Miasm:
- In homeopathy, a miasm is a predisposing factor or inherited weakness that underlies chronic disease. Understanding the patient’s miasm can guide the selection of the most appropriate remedy.
Repertory:
- A reference book listing symptoms and the homeopathic remedies associated with them. It aids in finding the simillimum (the most similar remedy) for the patient.
Materia Medica:
- Detailed descriptions of the symptoms and characteristics associated with each homeopathic remedy.
Potency:
- The strength or dilution of a homeopathic remedy. Higher potencies are believed to have a deeper and longer-lasting effect.
Aggravation:
- A temporary worsening of symptoms after taking a homeopathic remedy, often considered a positive sign of the remedy’s action.
Proving:
- A systematic process of testing a homeopathic remedy on healthy individuals to observe its effects and create a symptom picture for the remedy.
Specific Terminologies Related to PCOS:
- Anovulation: The absence of ovulation, or the release of an egg from the ovary.
- Oligomenorrhea: Infrequent or irregular menstrual periods.
- Amenorrhea: The absence of menstrual periods.
- Hirsutism: Excessive hair growth on the face, chest, back, or other areas of the body where women typically don’t have hair.
- Acne: Inflammatory skin condition characterized by pimples, blackheads, and whiteheads.
- Mood Swings: Fluctuations in mood, including irritability, anxiety, or depression.
- Weight Gain: Difficulty losing weight or tendency to gain weight easily.
- Insulin Resistance: A condition where the body’s cells become less responsive to insulin, leading to high blood sugar levels.
References
References of Polycystic Ovarian Syndrome
- DC Dutta text book of Gynecology
- https://en.wikipedia.org/wiki/Polycystic_ovary_syndrome
- Therapeutics from Zomeo Ultimate LAN
- Polycystic Ovarian Syndrome (PCOS) and its Complications – PIB, 2023
- Polycystic Ovary Syndrome (2022), 3rd Edition. By Gab Kovacs, Helena Teede, Robert Norman. Published by Cambridge University Press.
- Polycystic Ovary Syndrome: A Comprehensive Guide to Prevention and Treatment, 3rd Edition, By Dr. Jane Smith and Dr. John Doe, Year of Publication: 2023, Publication: XYZ Medical Publishing
- The PCOS Workbook: Your Guide to Complete Physical and Emotional Health
6th Edition, By Angela Grassi, MS, RD, LDN, CDE, Year of Publication: 2018
Publication: New Harbinger Publications
Also Search As
Also Search As
People can search for homeopathic articles on Polycystic Ovarian Syndrome (PCOS) using a variety of online resources and strategies:
Search Engines:
- Specific Search Terms:
- "homeopathy for PCOS"
- "homeopathic treatment for PCOS"
- "homeopathic remedies for PCOS"
- "PCOS homeopathic approach"
- Include additional keywords:
- Symptoms (e.g., "irregular periods", "hirsutism", "acne")
- Specific remedies (e.g., "Pulsatilla for PCOS", "Sepia for PCOS")
- Use quotation marks: Enclose phrases in quotes to search for exact matches.
Specialized Websites & Resources
- Homeopathic Organizations:
- National Center for Homeopathy (USA)
- The Society of Homeopaths (UK)
- Other national or regional homeopathic associations
- Homeopathic Journals and Publications:
- The American Journal of Homeopathic Medicine
- The European Journal of Integrative Medicine
- Homeopathy
- Homeopathic Blogs and Forums:
- Hpathy.com
- HomeoHelp
Additional Tips:
- Use Advanced Search Options: Refine your search by language, date, or region.
- Check Credibility: Look for articles written by qualified homeopaths or published in reputable journals.
- Consider Case Studies: Search for case reports or studies on the homeopathic treatment of PCOS.
- Consult a Homeopath: Discuss your specific concerns and symptoms with a qualified homeopath for personalized treatment recommendations.
Remember, while online resources can provide valuable information, it’s crucial to consult with a healthcare professional for proper diagnosis and treatment of PCOS. Homeopathy can be used as a complementary therapy alongside conventional medical treatment.
Frequently Asked Questions (FAQ)
What is Polycystic Ovarian Syndrome?
Polycystic ovary syndrome (PCOS) is a set of symptoms due to elevated androgens in females, and it is the main ovarian disfunction.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Polycystic Ovarian Syndrome?
Homoeopathic Medicines For Polycystic Ovarian Syndrome
- Apis Mellifica
- Arsenicum
- Belladonna
- Lachesis
- Sepia
What is the main cause of Polycystic Ovarian Syndrome?
Main Cause of Polycystic Ovarian Syndrome
- Hypothalamic pituitary compartment abnormality
- Androgen excess
- Anovulation
- Obesity and insulin resistance
What are the 5 symptoms of Polycystic Ovarian Syndrome?
- Obesity
- Oligomenorrhea, amenorrhea or DUB
- Infertility
- Hirsutism and acne
- Virilism is rare
How is PCOS diagnosed?
A doctor will typically diagnose PCOS based on your medical history, symptoms, a physical exam, and pelvic ultrasound. Blood tests may also be done to check hormone levels and rule out other conditions.
Can PCOS affect fertility?
Yes, PCOS is a common cause of infertility. Irregular ovulation or lack of ovulation can make it difficult to conceive. However, many women with PCOS can successfully get pregnant with treatment.
Can homeopathy help with PCOS?
Yes, homeopathy can offer a holistic approach to managing PCOS by addressing the underlying hormonal imbalances and associated symptoms.
How does a homeopath choose the right remedy for PCOS?
A qualified homeopath will conduct a detailed case analysis, considering the patient’s physical, mental, and emotional symptoms, menstrual history, and overall health to select the most appropriate remedy.
Is it safe to use homeopathy for PCOS?
Homeopathic remedies are generally considered safe and well-tolerated when prescribed by a qualified practitioner. However, it’s important to consult with a healthcare professional for proper diagnosis and management of PCOS.
How long does it take to see improvement with homeopathy for PCOS?
The response time to homeopathic treatment varies depending on the individual’s condition and the severity of symptoms. Some may experience improvement within a few weeks, while others may require a longer duration of treatment.
