Premenstrual syndrome (PMS)
Definition
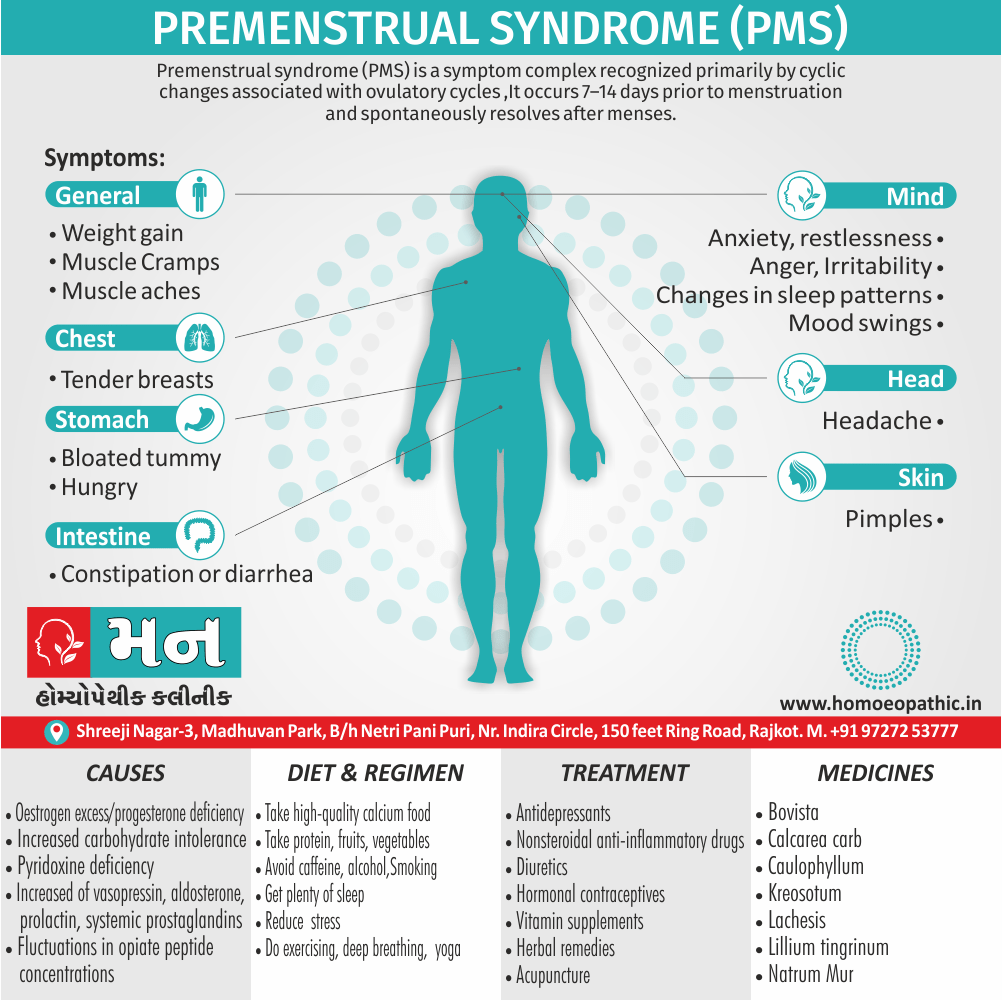
Premenstrual syndrome (PMS also described as premenstrual tension PMT), is a symptom complex recognized primarily by cyclic changes associated with ovulatory cycles. It occurs 7–14 days prior to menstruation and spontaneously resolves after menses. [1]
Here are some synonyms for Premenstrual Syndrome (PMS):
- Premenstrual tension (PMT)
- Premenstrual complaints
- Premenstrual symptoms
- Late luteal phase dysphoric disorder (LLPDD) – a more technical term for a severe form of PMS
- Premenstrual disorders (PMDs) – a broader term encompassing all menstrual-related problems
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
- Most well-adjusted women experience minor psychological and somatic changes for a few days preceding menstruation. [2]
- These menstrual molimina give way to a sensation of relief and well-being once menstruation is established. [2]
- This is extremely common at all ages but especially in women aged 30–45 years, the reported prevalence ranging from 5–95%. [2]
- The age incidence of PMS is said to be due to the fact that stresses are most severe in the third and fourth decades. [2]
- Premenstrual syndrome (PMS) has a wide variety of signs and symptoms, including mood swings, tender breasts, food cravings, fatigue, irritability and depression.[4]
- Still, you don’t have to let these problems control your life. Treatments and lifestyle adjustments can help you reduce or manage the signs and symptoms of premenstrual syndrome.
Epidemiology
Epidemiology
The epidemiology of Premenstrual Syndrome (PMS) in India is characterized by a high prevalence, with studies reporting rates ranging from 18.4% to 65%.
- A systematic review and meta-analysis conducted in 2021 estimated the pooled prevalence of PMS in India to be 43% (95% CI: 0.35-0.50), with the prevalence being higher in adolescents (49.6%; 95% CI: 0.40-0.59). (Kaur et al., 2021)
Specific studies have also reported varying prevalence rates:
- A study among medical students in Bhopal found a PMS prevalence of 65%. (Jiwane et al., 2018)
- A study among college students in Puducherry reported a PMS prevalence of 62.7%. (Bhuvaneswari et al., 2020)
- A study in Gujarat among college students found a PMS prevalence of 18.4%. (Choksi and Shah, 2016)
These findings highlight the significant burden of Premenstrual syndrome (PMS) in India and emphasize the need for further research and targeted interventions to address this prevalent health issue.[10][11][12][13]
Causes
Causes
- The exact cause of Premenstrual syndrome (PMS) is not known. It has been postulated that it represents a syndrome which is the result of multiple biochemical abnormalities. [1]
Amongst these, the following have been implicated:
- Oestrogen excess or progesterone deficiency in the luteal phase.
- Increased carbohydrate intolerance in the luteal phase.
- Pyridoxine deficiency—this vitamin plays a role in oestrogen synthesis and also in dopamine and serotonin production.
- Increased production of vasopressin, Aldosterone, Prolactin and Systemic prostaglandins which adversely affect renal function and contribute to fluid retention and bloating.
- Fluctuations in opiate peptide concentrations affecting endorphin levels. However, biochemical estimations do not bear these out.[1]
- Hence, at present it is not yet clear whether PMS is an abnormal response to normal hormonal fluctuation or a result of hormonal abnormalities.
- A woman with hysterectomy but conservation of ovaries may also suffer from PMT suggesting that the ovarian hormones have a role in PMT.
- Low level of b-endorphins (neurotransmitters) in the brain and low level of serotonin are probably responsible for psychiatric disorders.
- Genetic predisposition is also recognized in a few cases.[1]
Types
Types
Primarily, Premenstrual syndrome (PMS) is categorized into two main types:
Core PMS (formerly PMS-A)
- Characterized by mood symptoms like irritability, tension, depression, and anxiety.
- May also include physical symptoms like bloating, breast tenderness, and headaches.
PMDD (Premenstrual Dysphoric Disorder)
- A more severe form of PMS with significant mood swings, irritability, anger, and depression.
- These symptoms disrupt daily life and relationships.
- Requires a specific diagnosis based on diagnostic criteria.[14]
Risk Factors
Risk Factors
Several factors can increase a woman’s likelihood of experiencing Premenstrual syndrome (PMS):
- Age: PMS is most common in women in their late 20s to early 40s.
- Family history: Women with a family history of PMS or PMDD are at a higher risk.
- Mental health conditions: A history of depression, anxiety, or other mood disorders can increase the risk of PMS.
- Lifestyle factors:
- Smoking
- Lack of physical activity
- Poor diet
- Stress[15].
Pathogenesis
Pathogenesis
The exact cause of Premenstrual syndrome (PMS) remains unclear, but it is believed to be related to hormonal fluctuations during the menstrual cycle. Several factors may contribute:
- Hormonal Fluctuations: Changes in estrogen and progesterone levels, especially the drop in progesterone after ovulation, may trigger symptoms.
- Neurotransmitter Imbalance: Changes in serotonin, a brain chemical that affects mood, may also play a role.
- Genetic Predisposition: Some women may be more genetically susceptible to developing PMS.
- Other Factors: Other potential contributing factors include:
- Changes in brain chemical activity
- Nutritional deficiencies
- Inflammation
- Stress[16].
Pathophysiology
Pathophysiology
The information you provided accurately summarizes the current understanding of the pathophysiology of premenstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD). It highlights the complex interplay of hormonal fluctuations, neurotransmitter activity, and brain circuitry involved in these conditions.
Here’s a breakdown of the key points:
Hormonal influence:
While no specific hormonal abnormality has been identified, PMS/PMDD symptoms are clearly linked to the menstrual cycle and the production of progesterone after ovulation.
Neurotransmitter involvement:
GABA and serotonin are two key neurotransmitters implicated in PMS/PMDD. Progesterone metabolites can affect GABA receptors, reducing their activity and potentially contributing to symptoms. Serotonin also appears to play a role, as low serotonin levels are associated with PMS-like symptoms, and medications that increase serotonin can be effective in treatment.
Complex brain circuitry:
Brain imaging studies suggest that PMS/PMDD involves complex interactions within brain regions responsible for mood regulation and behavior.
It’s important to remember that PMS/PMDD is likely not caused by a single factor but rather a combination of these elements. Research continues to explore the intricate mechanisms underlying these conditions to develop more effective treatments and improve the quality of life for those affected.[8]
Clinical Features
Clinical Features
Premenstrual syndrome (PMS) is characterized by a wide range of physical and emotional symptoms that typically occur in the luteal phase of the menstrual cycle (between ovulation and the start of menstruation) and resolve with the onset of menses. These symptoms can vary in severity and presentation from one woman to another.
Common clinical features include:
Physical Symptoms:
- Breast tenderness and swelling
- Abdominal bloating
- Headaches
- Fatigue
- Changes in appetite or food cravings
- Sleep disturbances
- Joint or muscle pain
Emotional and Behavioral Symptoms:
- Irritability and mood swings
- Anxiety or tension
- Depression or sadness
- Anger or aggression
- Difficulty concentrating
- Social withdrawal[17]
Sign & Symptoms
Sign & Symptoms
While PMS often involves mild or moderate symptoms that don’t majorly affect daily life, symptoms can be severe enough to impact your everyday activities and overall well-being.[5]
Physical signs
- Bloated tummy
- Cramps
- Tender breasts
- Hunger
- Headache
- Muscle aches
- Joint pain
- Swollen hands and feet
- Pimples
- Weight gain
- Constipation or diarrhea
Emotional and behavioral symptoms
PMS-related changes in your mood, emotions, and behavior might include:
- Anxiety, restlessness
- Unusual anger and irritability
- Changes in appetite, including increased food cravings, especially for sweets
- Changes in sleep patterns, including fatigue and trouble sleeping
- A sad or low mood, which might involve tearfulness or sudden, uncontrollable crying
- Rapid shifts in mood and emotional outbursts
- Decreased sex drive
- Difficulty concentrating or remembering information [5]
- For some, the physical pain and emotional stress are severe enough to affect their daily lives.
- Regardless of symptom severity, the signs and symptoms generally disappear within four days after the start of the menstrual period for most women.[6]
- But a small number of women with premenstrual syndrome have disabling symptoms every month. This form of PMS is called premenstrual dysphoric disorder (PMDD).[6]
- PMDD signs and symptoms include depression, mood swings, anger, anxiety, feeling overwhelmed, difficulty concentrating, irritability and tension.[6]
Clinical Examination
Clinical Examination
The diagnosis of PMS is primarily based on a thorough patient history, focusing on the timing, nature, and severity of symptoms in relation to the menstrual cycle. A physical examination generally does not reveal specific findings for PMS, but it can help to rule out other potential causes of the symptoms.
Here’s what might be involved:
Detailed History: The healthcare provider will inquire about:
- The specific symptoms experienced
- The timing and duration of symptoms in relation to the menstrual cycle
- The severity of symptoms and their impact on daily life
- Any past medical or psychiatric history
- Current medications and supplements
- Lifestyle factors (diet, exercise, stress levels)
Physical Examination: While typically normal, a physical exam may be conducted to exclude other conditions that could mimic PMS. This might include:
- Pelvic examination to rule out gynecological problems
- Breast examination to check for tenderness or lumps
- Thyroid examination to evaluate thyroid function
Symptom Diary: The patient may be asked to keep a daily record of their symptoms for at least two menstrual cycles. This helps to establish a clear pattern of symptom occurrence in relation to the menstrual cycle.[18]
Diagnosis
Diagnosis
- Diagnosis depends on history and careful questioning. Temporal correlation of symptoms with the premenstrual phase of the cycle as documented in a menstrual diary helps to arrive at a rational diagnosis.
- No organic pelvic lesion is detected, and no definite test is available to confirm the diagnosis.[1]
Differential Diagnosis
Differential Diagnosis
PMS can mimic a variety of other conditions, making accurate diagnosis essential. Some common conditions to consider in the differential diagnosis include:
Psychiatric Disorders:
- Major Depressive Disorder
- Bipolar Disorder
- Anxiety Disorders
- Personality Disorders
Gynecological Conditions:
- Endometriosis
- Dysmenorrhea (painful periods)
- Premenstrual Exacerbation (PME) of underlying medical conditions (e.g., asthma, migraines)
Other Medical Conditions:
- Thyroid disorders
- Irritable Bowel Syndrome (IBS)
- Chronic Fatigue Syndrome[19]
Complications
Complications of PMS
While PMS itself is not typically considered a serious medical condition, its symptoms can significantly impact a woman’s quality of life and lead to various complications:
Impaired Daily Functioning: The physical and emotional symptoms of PMS can interfere with work, school, and social activities, leading to decreased productivity and absenteeism.
Strained Relationships: Mood swings, irritability, and emotional instability can negatively affect relationships with partners, family, and friends.
Reduced Quality of Life: The overall emotional and physical discomfort associated with PMS can significantly impact a woman’s sense of well-being and enjoyment of life.
Increased Risk of Mental Health Issues: In some cases, PMS may increase the risk of developing or exacerbating mental health conditions such as depression and anxiety.
Suicidal Thoughts or Behaviors: In rare cases, severe PMS or PMDD (Premenstrual Dysphoric Disorder) may be associated with an increased risk of suicidal ideation or behavior.[20]
Investigations
Investigations of PMS
Primarily, PMS diagnosis relies on a detailed patient history and symptom tracking. However, in some cases, investigations may be necessary to rule out other conditions or confirm the diagnosis. These can include:
Symptom Diary: The cornerstone of PMS diagnosis. Patients are asked to record their symptoms daily for at least two menstrual cycles, noting their severity and timing in relation to their menstrual cycle.
Physical Examination: While usually unremarkable in PMS, a physical exam can help exclude other potential causes of symptoms. This may involve a pelvic examination, breast examination, or thyroid evaluation.
Laboratory Tests: These are not routinely required for PMS diagnosis but may be used to rule out other conditions. These can include:
Thyroid function tests
Blood sugar levels
Complete blood count (CBC)
Hormone levels (occasionally)[21]
Treatment
Treatment of Premenstrual syndrome (PMS)
- For many women, lifestyle changes can help relieve PMS symptoms. But depending on the severity of your symptoms, your doctor may prescribe one or more medications for premenstrual syndrome.
- The success of medications in relieving symptoms varies among women. Commonly prescribed medications for premenstrual syndrome include:
Antidepressants: –
- Selective serotonin reuptake inhibitors (SSRIs) which include fluoxetine (Prozac), paroxetine (Paxil, Pexeva), sertraline (Zoloft) have been reducing mood symptoms.
- SSRIs are the first line treatment for severe PMS or PMDD. These medications are generally taken daily. But for some women with PMS, use of antidepressants may be limited to the two weeks before menstruation begins.[7]
Nonsteroidal anti-inflammatory drugs (NSAIDs): –
- Taken before or at the onset of your period, NSAIDs such as Ibuprofen or Naproxen sodium can ease cramping and breast discomfort.[7]
Diuretics :–
- Taking water pills (diuretics) can help your body shed excess fluid through your kidneys. Spironolactone (Aldactone) is a diuretic that can help ease some of the symptoms of PMS.[7]
Hormonal contraceptives: –
- These prescription medications stop ovulation, which may bring relief from PMS symptoms.[7]
Alternative medicine :-
- Vitamin supplements:-Calcium, magnesium, vitamin E and vitamin B-6 have all been reported to soothe symptoms, but evidence is limited or lacking.
- Herbal remedies:- Some women report relief of PMS symptoms with the use of herbs, such as ginkgo, ginger, chaste berry (Vitex Agnus), evening primrose oil.[7]
Acupuncture
Prevention
Prevention of PMS
While the exact cause of PMS remains elusive, several lifestyle modifications and strategies may help reduce the severity or frequency of symptoms:
Dietary Changes:
- Limit salt intake to minimize fluid retention and bloating.
- Reduce caffeine and alcohol consumption, which can exacerbate mood swings and anxiety.
- Increase intake of complex carbohydrates, fruits, vegetables, and whole grains to stabilize blood sugar levels and improve mood.
- Consider calcium and vitamin D supplementation, as deficiencies may worsen PMS symptoms.
Regular Exercise:
- Engage in moderate-intensity aerobic exercise most days of the week. Exercise releases endorphins, which can boost mood and reduce pain.
Stress Management:
- Incorporate stress-reduction techniques such as yoga, meditation, deep breathing exercises, or mindfulness practices.
Adequate Sleep:
- Aim for 7-8 hours of quality sleep each night. Sleep deprivation can exacerbate mood swings and fatigue.
Supplements and Medications:
- Certain supplements like vitamin B6, magnesium, and chasteberry may be beneficial in reducing PMS symptoms.
- In severe cases, medications like oral contraceptives, antidepressants, or diuretics may be prescribed by a healthcare professional.[22]
Homeopathic Treatment
Homeopathic Treatment of Premenstrual syndrome (PMS)
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Premenstrual syndrome (PMS):
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Medicines:
Bovista
- Premenstrual problems with puffiness in the extremities, fluid retention and a bloated feeling often indicate a need for this remedy.
- The woman may feel very awkward and clumsy, and may constantly be dropping things because of swollen-feeling hands.
- Diarrhea occurring around the time of the menstrual period strongly indicates this remedy.[9]
Calcarea carbonica
- PMS with fatigue, anxiety, and a feeling of being overwhelmed suggest a need for this remedy.
- The woman may have problems with water-retention and weight gain, tender breasts, digestive upsets, and headaches.
- Periods often come too early and last too long, sometimes with a flow of bright red blood.
- A general feeling of chilliness, with clammy hands and feet and cravings for sweets and eggs are other indications for Calcarea.[9]
Lachesis
- Women who need this remedy are usually intense, with a tremendous need for an outlet, both physically and mentally.
- Symptoms of PMS include congestion, headaches, flushing, surges of heat, and an intense outspoken irritability often with strong feelings of suspicion or jealousy.
- When the flow arrives, it may be heavy, but brings relief of tension. Intolerance of restrictive clothing around the waist or neck is another indication for Lachesis.[9]
Lycopodium
- PMS with a craving for sweets and a ravenous appetite suggests a need for this remedy.
- Digestive upsets with abdominal bloating and flatulence often seen, with the person feeling worst in the late afternoon and evening.
- Menstrual periods may delay, follow by a heavy flow that goes on for extra days.
- A woman who needs this remedy often wears a worried look and lacks self-confidence although she may irritable and bossy to pets and family members.
- A desire to alone, but with someone in the other room, is another indication for Lycopodium.[9]
Natrum Muriaticum
- A person who needs this remedy usually seems reserved to others, but is deeply emotional inside.
- She may feel extremely sad and lonely, but gets affronted or angry if others try to console her or sympathize.
- Depression, anger over minor things, and a need to be alone to cry are often seen when Natrum mur is needed.
- Menstrual problems can be accompanied by migraines, or a backache that feels better from lying on something either hard or pushing a solid object against the painful place.
- Lastly, A craving for salt, strong thirst, and a tendency to feel worse from being in the sun are other indications for this remedy.[9]
Pulsatilla
- Generally, This remedy can be helpful during many conditions involving hormonal changes and is often helpful to girls who have recently started having periods.
- PMS with irritability, moodiness, and weepiness is typical.
- Either Delay or suppression of the menstrual flow can be accompanied by queasy feelings, nausea, and faintness. Additionally Being too warm or in a stuffy room makes things worse, and fresh air can bring relief.
- The timing, amount, and nature of the menstrual flow are changeable as are the woman’s moods when Pulsatilla is the remedy.
- The woman usually is emotional also needy, wanting a lot of attention and comforting.[9]
Sepia
- In brief, This remedy relieves mood swings from PMS associated with irritability and poor venous circulation.[9]
Veratrum album
- Menstrual periods with very heavy flow and cramping, with a feeling of exhaustion also icy coldness suggest a need for this remedy.
- Furthermore, Vomiting and diarrhea are often seen.
- Periods may start too early and go on too long. In detail, The woman feels worse at night, from exercise, and from drinking things that are warm.
- Cold drinks, small meals, and wrapping up in warm clothes or covers may help to bring improvement.[9]
Caulophyllum
- This remedy is often helpful to women with a history of irregular periods, difficulty becoming pregnant or slow childbirth due to weak muscle tone of the uterus.
- Symptoms include discomfort during periods and a heavy flow of blood or other discharge.
- Drawing pains may feel in the pelvic region, thighs, and legs.
- Stiffness or arthritis, especially in the finger-joints, often seen when this remedy needed.[9]
Lillium tigrinum
- This remedy may helpful if a woman is inclined toward rage during PMS, makes other people "walk on eggs," and is extremely sensitive and irritable.
- Pressure in the rectum and in the pelvic region, with a sensation that the uterus is pushing out, may make her feel a frequent need to sit or cross her legs.
- Emotions and excitement aggravate the symptoms, and fresh air will often bring relief.[9]
Nux vomica
- When a woman with PMS is extremely impatient, pushy, and intolerant, this remedy may of use.
- Uncomfortable, irregular menstrual periods can experience, often with a nagging urge to move the bowels before the flow begins.
- Constipation is common, and constricting pains may extend to the rectum or tailbone region.
- Anger, mental strain, physical exertion, and overindulgence in coffee, alcohol, or food can aggravate the problems.[9]
- Woman often feels chilly and improves from warmth and rest.[9]
Kreosotum
- Headache, nausea, and a heavy flow that makes the genitals and surrounding skin feel irritated and swollen are indications for this remedy.
- Kreosotum often indicate for women with PMS who feel irritable and uncomfortable, and have a strong dislike of sexual activity.[9]
Diet & Regimen
Diet & Regimen
For Premenstrual syndrome (PMS)
Dietary Strategies for PMS Relief:
- Focus on Whole Foods: Emphasize a balanced diet rich in fruits, vegetables, whole grains, and lean protein.
- Limit Processed Foods: Explain the negative impact of processed foods, sugary snacks, and excessive caffeine and alcohol on PMS symptoms.
- Micronutrients Matter: Highlight the importance of specific nutrients:
- Calcium and Vitamin D: Explain their role in mood regulation and reducing cramps. Recommend sources like dairy, leafy greens, and fortified foods.
- Magnesium: Discuss its benefits in easing anxiety, irritability, and muscle cramps. Suggest incorporating magnesium-rich foods like nuts, seeds, and dark chocolate.
- B Vitamins: Explain their role in mood and energy regulation. Recommend sources like whole grains, legumes, and leafy greens.
- Omega-3 Fatty Acids: Discuss their anti-inflammatory effects and potential to improve mood. Suggest sources like fatty fish, flaxseeds, and walnuts.
- Calcium and Vitamin D: Explain their role in mood regulation and reducing cramps. Recommend sources like dairy, leafy greens, and fortified foods.
Regimen
- Regular Exercise: Explain the mood-boosting and stress-reducing benefits of exercise. Recommend activities like yoga, walking, and swimming.
- Stress Management: Discuss the impact of stress on PMS symptoms. Suggest stress-reducing techniques like meditation, deep breathing exercises, and spending time in nature.
- Sleep Hygiene: Emphasize the importance of quality sleep for hormonal balance and mood regulation. Offer tips for improving sleep habits.
- Hydration: Explain the role of hydration in reducing bloating and water retention. Encourage adequate water intake throughout the day.
- Focus on Whole Foods: Emphasize a balanced diet rich in fruits, vegetables, whole grains, and lean protein.
Do’s and Don'ts
Do’s & Don’ts
Premenstrual Syndrome do’s & Don’ts
Do’s:
The Diet:
- Eat a balanced diet rich in fruits, vegetables, and whole grains.
- Limit salt intake to reduce bloating.
- Reduce caffeine and alcohol consumption, which can worsen symptoms.
- Increase your intake of calcium-rich foods or consider a supplement.
- Consider taking vitamin B6 and magnesium supplements, after consulting your doctor.
Lifestyle:
- Engage in regular exercise, even light activity can help.
- Get enough sleep (7-8 hours per night).
- Manage stress through relaxation techniques like yoga, meditation, or deep breathing.
- Track your symptoms with a diary to identify patterns and triggers.
- Seek support from friends, family, or a therapist if needed.
- Consult your doctor if symptoms are severe or interfering with your life.
Don’ts:
The Diet:
- Don’t skip meals, especially breakfast.
- Don’t overindulge in sugary or processed foods.
- Not consume excessive amounts of salt.
Lifestyle:
- Don’t smoke, as it can worsen PMS symptoms.
- Don’t neglect self-care. Take time for yourself to relax and recharge.
- Not hesitate to seek professional help if you’re struggling to manage your symptoms.
Remember, these are general guidelines. It’s essential to listen to your body and find what works best for you. If you have concerns about PMS or PMDD, talk to your healthcare provider. They can offer personalized advice and treatment options to help you manage your symptoms and improve your quality of life.
Terminology
Terminologies
Premenstrual Syndrome (PMS): A collection of physical and emotional symptoms that occur in the luteal phase of the menstrual cycle (between ovulation and menstruation) and typically resolve with the onset of menses.
Premenstrual Dysphoric Disorder (PMDD): A more severe form of PMS characterized by significant mood disturbances, such as irritability, depression, and anxiety, that significantly impact daily life and relationships.
Luteal Phase: The second half of the menstrual cycle, after ovulation, when progesterone levels rise and then fall if pregnancy does not occur. PMS symptoms typically occur during this phase.
Symptom Diary: A tool used to track the timing and severity of PMS symptoms over several menstrual cycles, aiding in diagnosis and treatment planning.
Additional Terms
Mood Swings: Fluctuations in mood, often including irritability, sadness, anxiety, or anger.
Bloating: A feeling of abdominal fullness or tightness often associated with fluid retention.
Breast Tenderness: Soreness or discomfort in the breasts.
Fatigue: A feeling of tiredness or lack of energy.
Cravings: Intense desires for specific foods, often salty or sweet.
Insomnia: Difficulty falling or staying asleep.
Concentration Difficulties: Trouble focusing or paying attention.
Social Withdrawal: A tendency to avoid social interaction.
Selective Serotonin Reuptake Inhibitors (SSRIs): A class of antidepressants sometimes used to treat PMDD.
Terminologies Related To Homoeopathy
- Pulsatilla: Indicated for mood swings, irritability, tearfulness, and a craving for sweets.
- Sepia: Helpful for women experiencing indifference, irritability, sadness, and a sense of bearing down in the pelvis.
- Lachesis: Suggested for women with premenstrual headaches, irritability, and bloating.
- Natrum Muriaticum: Indicated for emotional PMS symptoms like sadness, irritability, and a tendency to dwell on past hurts.
- Calcarea Carbonica: Considered for women with bloating, water retention, fatigue, and a craving for sweets.
- Cyclamen: Often used for premenstrual headaches, dizziness, and mood swings.
- Folliculinum: Sometimes used for PMS symptoms that follow a cyclical pattern and are closely linked to hormonal fluctuations.
Disclaimer:
- Always consult a qualified healthcare professional for diagnosis and treatment of PMS.
- Never self-treat, especially if you have other health conditions or are taking medications.
References
References use for Article Premenstrual syndrome (PMS)
Textbook of Gynacology VG Padubidri (1)
Textbook of Jeffcoate’s Principles of Gynecology (2)
https://en.wikipedia.org/wiki/ Premenstrual_syndrome(3)
https://www.mayoclinic.org/diseases-conditions/premenstrual-syndr(4)
https://www.webmd.com/women/pms/what-is-pms(5)
https://www.mayoclinic.org/diseases-conditions/premenstrual-synd(6)
https://wwwS.mayoclinic.org/diseases-conditions/premenstrual-syndrome/diagnosi (7)
https://pubmed.ncbi.nlm.nih.gov/22611222/(8)
https://www.peacehealth.org/medical-topics/id/hn-2241003(9)
https://www.webmd.com/women/pms/ features/diet-and-pms(10)
Bhuvaneswari K, Selvaraj K, Kumar SG, et al. Prevalence of premenstrual syndrome and its impact on quality of life among selected college students in Puducherry. NMJI. 2020;32(1).(11)
Choksi S, Shah V. Prevalence of premenstrual syndrome and premenstrual dysphoric disorder among medical students in Gujarat. Indian J Physiol Pharmacol. 2016;60(3):328-332.(12)
Jiwane R, Sachan A, Jain R, et al. Prevalence of premenstrual syndrome and premenstrual dysphoric disorder among medical students and its impact on their academic and social performance. J Midlife Health. 2018;9(2):68-72.(13)
Kaur H, Aggarwal A, Dalal PK. Prevalence of premenstrual syndrome and premenstrual dysphoric disorder in India: A systematic review and meta-analysis. Health Promot Perspect. 2021;11(2):129-141.(14)
The Complete Guide to PMS, 2nd Edition, Katharina Dalton, 1994, Wellingborough: Thorsons Publishers.(15)
Fast Facts: Premenstrual Syndrome, 1st Edition, Nick Panay, 2005, Abingdon, Oxon: Health Press.(16)
Clinical Gynecologic Endocrinology and Infertility, 8th Edition, Leon Speroff, Marc A. Fritz, 2011, Lippincott Williams & Wilkins(17).
Comprehensive Gynecology, 7th Edition, Gretchen M. Lentz, Andrea Dunaif, Elizabeth A. Stewart, et al., 2017, Elsevier.(18)
Williams Gynecology, 4th Edition, Barbara L. Hoffman, John O. Schorge, Joseph I. Schaffer, et al., 2020, McGraw Hill Professional.(19)
Yen & Jaffe’s Reproductive Endocrinology, 8th Edition, Jerome F. Strauss III, Robert L. Barbieri, 2019, Elsevier.(20)
Premenstrual Syndrome and Premenstrual Dysphoric Disorder, 1st Edition, Peter J. Schmidt, David R. Rubinow, 1992, American Psychiatric Press, Inc.(21)
Novak’s Textbook of Gynecology, 16th Edition, Jonathan S. Berek, 2016, Lippincott Williams & Wilkins.(22)
Our Bodies, Ourselve, 9th Edition, The Boston Women’s Health Book Collective, 2011, Touchstone.(23)
Also Search As
PMS Also Search As
Search Engines
Specific Keywords: Use precise search terms like:
- "homeopathy for PMS"
- "homeopathic remedies for premenstrual syndrome"
- "natural treatment for PMS"
- "alternative medicine for PMS"
Advanced Search Operators: Refine your search further by:
- Using quotation marks for exact phrases (e.g., "homeopathic treatment of PMS")
- Excluding specific terms with the minus sign (e.g., "PMS -conventional medicine")
- Searching within specific websites (e.g., "PMS site:nationalcenterforhomeopathy.org")
Specialized Websites & Databases
Homeopathic Organizations: Check websites of national or international homeopathic associations.
- The National Center for Homeopathy (NCH)
- The British Homeopathic Association (BHA)
- The Homeopathic Research Institute (HRI)
Homeopathic Journals & Publications: Search databases like:
- PubMed (filter for "Complementary Therapies" or "Homeopathy")
- The American Journal of Homeopathic Medicine
- Homeopathy
Online Homeopathic Libraries & Resources: Explore websites that offer collections of homeopathic articles and information.
Additional Tips:
- Consult a Homeopath: A qualified homeopath can provide personalized recommendations and information based on your specific symptoms and needs.
- Be Critical of Information: Evaluate the source and credibility of any information you find. Look for articles published in peer-reviewed journals or from reputable homeopathic organizations.
Frequently Asked Questions (FAQ)
What is Premenstrual syndrome?
Premenstrual syndrome is a symptom complex recognized primarily by cyclic changes associated with ovulatory cycles.
What are the symptoms of Premenstrual syndrome?
- Bloated tummy
- Cramps
- Tender breasts
- Hunger
- Headache
- Muscle aches
- Joint pain
- Swollen hands and feet
- Pimples
What are the causes of Premenstrual syndrome?
- There’s no specific test for PMS. Diagnosis is usually based on your symptoms and their timing in relation to your menstrual cycle. Keeping a symptom diary can help identify patterns and confirm the diagnosis.
How is PMS diagnosed?
- Oestrogen excess or progesterone deficiency in the luteal phase.
- Increased carbohydrate intolerance in the luteal phase.
- Pyridoxine deficiency
- Fluctuations in opiate peptide concentrations
How can I manage PMS symptoms?
- Lifestyle changes like regular exercise, stress management techniques, and a healthy diet can help alleviate PMS symptoms. Over-the-counter pain relievers, hormonal birth control, and certain supplements may also be beneficial.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Premenstrual syndrome?
- Bovista
- Calcarea carbonica
- Lachesis
- Lycopodium
- Natrum Muriaticum
- Pulsatilla
Can homeopathy help with PMS?
- Yes, homeopathy can offer a natural approach to managing PMS symptoms by addressing the underlying hormonal imbalances and individual sensitivities.
Is it safe to use homeopathy for PMS?
- Homeopathic remedies are generally considered safe and well-tolerated when prescribed by a qualified practitioner.
How long does it take to see improvement with homeopathy for PMS?
- The response time to homeopathic treatment varies depending on the individual and the severity of symptoms. Some women may experience relief within a few cycles, while others may require longer-term treatment.
How does a homeopath choose the right remedy for PMS?
- A qualified homeopath conducts a detailed case analysis, considering the woman’s physical, emotional, and mental symptoms, menstrual history, and overall health to select the most appropriate remedy.
