Vaginitis
Definition
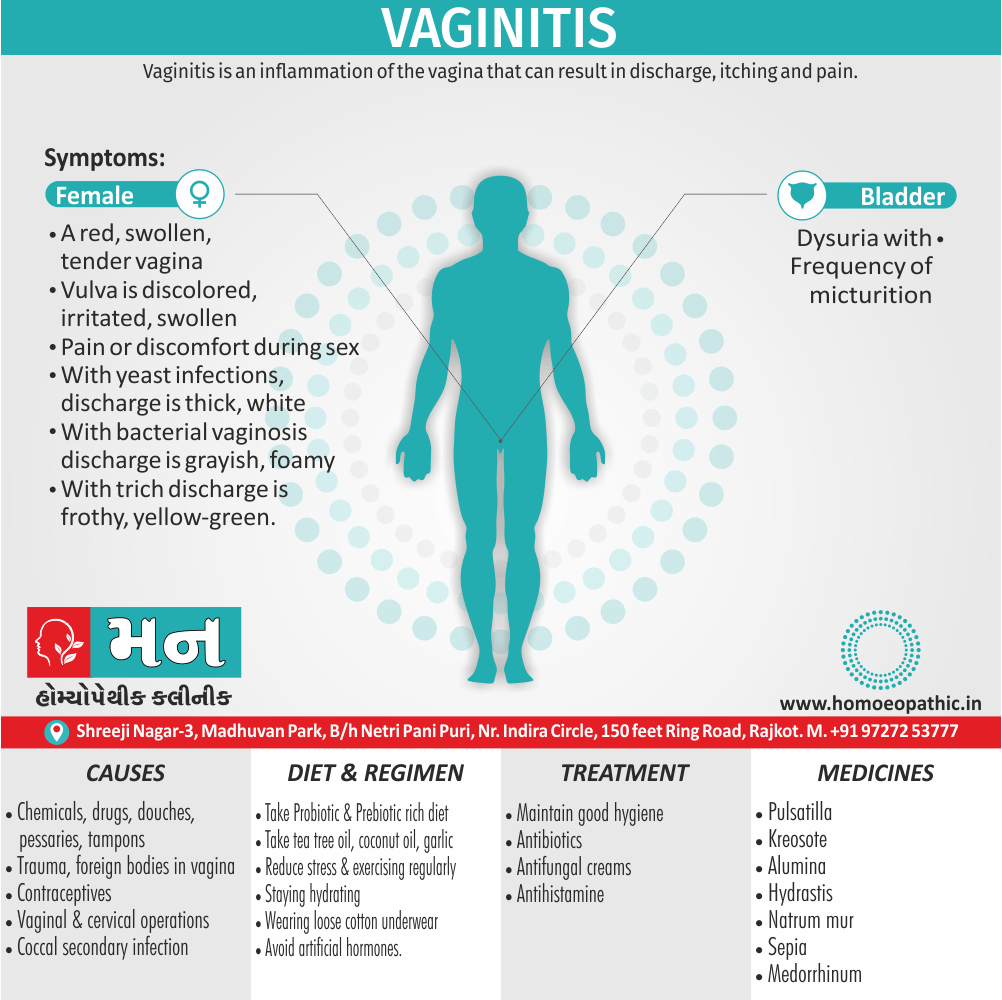
Vaginitis is an inflammation of the vagina that can result in discharge, itching and pain.[2]
Vaginitis is a general term for inflammation of the vagina. There are no direct synonyms for vaginitis, but it can be described in other ways depending on the cause:
- Yeast infection: This is the most common type of vaginitis, caused by an overgrowth of the Candida fungus. Symptoms include itching, burning, and thick, white discharge.
- Bacterial vaginosis: This type of vaginitis is caused by an imbalance of bacteria in the vagina. Symptoms include a fishy odor and thin, grayish-white discharge.
- Trichomoniasis: This is a sexually transmitted infection caused by a parasite. Symptoms include itching, burning, and a frothy, yellow-green discharge.
- Atrophic vaginitis: This type of vaginitis occurs after menopause when estrogen levels decrease, causing vaginal dryness and thinning. Symptoms include pain during sex and increased risk of urinary tract infections.
It’s important to consult with a healthcare professional to determine the cause of vaginitis and get appropriate treatment.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Vaginitis:
Inflammatory conditions of the vulva and vagina. The cause is usually a change in the balance of vaginal bacteria or an infection.
Due to lack of estrogen, the vaginal defense is lost and the infection occurs easily, once introduced inside the vagina.
Reduced estrogen levels after menopause and some skin disorders also can cause vaginitis.[1]
Epidemiology
Epidemiology of Vaginitis:
Vaginitis, or inflammation of the vagina, is a common condition affecting women worldwide, including India. The epidemiology of vaginitis in India showcases varying prevalence rates depending on the specific type of vaginitis and the population studied.
Bacterial Vaginosis (BV)
- BV is the most common cause of vaginitis in women of reproductive age
- Prevalence rates in India range from 17.8% to 63.7%. (Prevalence and diagnosis of bacterial Vaginosis in tertiary care teaching hospital, 2017)
Vulvovaginal Candidiasis (VVC)
- VVC is the second most common cause of vaginitis.
- Estimated prevalence in India is around 30%. (Prevalence of Vulvovaginal Infections and Species Specific Distribution of)
- (Vulvovaginal Candidiasis in Married Women of North India,2013)
Trichomoniasis
- Trichomoniasis is a sexually transmitted infection that can cause vaginitis.[9][10]
Causes
Causes:
- Chemicals, drugs, douches, pessaries, tampons, trauma, foreign bodies such as rubber ring pessaries, contraceptives and even vaginal and cervical operations are all causative.
- Alteration in the pH towards alkalinity always favors nonspecific infection; hence, its common incidence is in the puerperium.
- The association of coccal secondary infection with trichomoniasis is important, since the isolation of the secondary organism may mask the presence of the Trichomonas, which is really responsible for the discharge.[5]
Types
Classification:
The most common types of vaginitis are i.e.:
- Candida or “yeast” infections.
- Bacterial vaginosis.
- Trichomoniasis vaginitis.
- Either Chlamydia or Gonorrhoea.
- Viral vaginitis (herpes).
- Non-infectious vaginitis.
- Atrophic vaginitis.
Candida or “yeast” infections i.e.:
- Causative Organism Moniliasis is caused by Candida albicans, a gram-positive yeast-like fungus.
- Candida normally lives in your vagina, as well as in the mouth and digestive tract of all people, regardless of gender. An infection occurs when the normally occurring candida increases and cause bothersome symptoms.
- Discharge of Candida infection is white cottage cheese–like discharge.
- Candida infections should alert the health care provider to the patient’s use of antibiotic or immunosuppressive agents, or the presence of diabetes or human immunodeficiency virus (HIV).[3]
Bacterial vaginosis i.e.:
- Bacterial vaginosis (in other words, BV) is actually the most common vaginal infection in women of reproductive age.
- Bacterial vaginosis is caused by a combination of several bacteria that typically live in your vagina. These bacteria seem to overgrow in much the same way candida does when the vaginal pH balance is upset.
- Bacterial vaginosis is not asexually transmitted infection (STI), but it’s seen more often in sexually active people.
- Risk factors for bacterial vaginosis include: – New or multiple sexual partners, Douching, Cigarette smoking.
Trichomoniasis vaginitis i.e.:
- Vaginal trichomoniasis is the most common and important cause of vaginitis in the childbearing period.
- It is caused by Trichomonas vaginalis, a pear-shaped unicellular flagellate protozoon.
- The organism is predominantly transmitted by sexual contact, the male harbors the infection in the urethra and prostate.
- The transmission may also be possible by the toilet articles from one woman to the other or through examining gloves.
- The incubation period is 3–28 days.[1]
Chlamydia or Gonorrhoea i.e.:
- Chlamydia is the most common sexually transmitted infection (in other words, STI).
- Chlamydial vaginitis is most common in young adults aged 15 to 24 who have multiple sexual partners.
- Routine chlamydia screening is recommended by the Centers for Disease Control and Prevention (CDC) annually for sexually active women aged 24 and younger, and also at any age if you have multiple sexual partners, or are at risk.
- Gonorrhea, another bacterial STI, can also cause vaginitis symptoms. It often occurs with chlamydia.
- Sex partners should be tracked and treated appropriately to avoid re-infection.[4]
Viral vaginitis (herpes) i.e.:
Sexually transmitted viruses are a common cause of vaginitis that lead to inflammation of your genitals. The most common type of viral vaginitis is herpes simplex virus (HSV).
- Herpes simplex virus (HSV)- Herpes simplex virus is often just called a herpes infection. These infections are spread by sexual contact and often lead to painful sores. Herpes outbreaks are often associated with stress or emotional distress. You can also get herpes that affects your mouth-pharynx through oral sex.
- Low risk human papillomavirus (HPV) can lead to the development of condyloma, referred to as genital warts, and can be transmitted through vaginal, anal or oral sex.
Non-infectious vaginitis i.e.:
- Allergic reaction that causes vaginal irritation without having an infection.
- The most common cause is an allergic reaction or irritation from vaginal sprays, douches or spermicidal products.
- However, the skin around your vagina can also be sensitive to perfumed soaps, feminine products and wipes, lotions, sexual lubricants, detergents and fabric softeners.
Atrophic vaginitis i.e.:
- Vaginitis in postmenopausal women is called atrophic vaginitis. Additionally, The term is preferable to old age vaginitis.
- There is atrophy of the vulvovaginal structures due to estrogen deficiency. The vaginal defense is lost. Vaginal mucosa is thin and is more susceptible to infection and trauma. There may be desquamation of the vaginal epithelium which may lead to formation of adhesions also bands between the walls.
- Either Yellowish or blood-stained vaginal discharge.[1]
Risk Factors
Risk factors of Vaginitis:
- Hormonal changes, such as those associated with pregnancy, birth control pills or menopause
- Sexual activity
- Having a sexually transmitted infection
- Medications, such as antibiotics and steroids
- Use of spermicides for birth control
- Uncontrolled diabetes
- Use of hygiene products such as bubble bath, vaginal spray or vaginal deodorant
- Douching
- Wearing damp or tight-fitting clothing
- Using an intrauterine device (IUD) for birth control. [2]
Pathogenesis
Pathogenesis:
Changes in the vaginal microbiome:
- Decreased lactobacilli: This can occur due to antibiotic use, douching, hormonal changes (menopause), or sexual activity. A decrease in lactobacilli allows other organisms, such as Gardnerella vaginalis (bacterial vaginosis) or Candida species (vulvovaginal candidiasis), to proliferate.
- Overgrowth of pathogenic organisms: Certain bacteria, such as Gardnerella vaginalis or Candida species, can become more prevalent in the vagina, leading to an imbalance and inflammation.
Changes in the vaginal environment:
- Increased pH: An increase in vaginal pH can create a more favorable environment for the growth of certain organisms. This can occur due to menstrual blood, semen, or the use of certain soaps or douches.
- Decreased estrogen: Estrogen plays a crucial role in maintaining the vaginal epithelium and promoting the growth of lactobacilli. During menopause, estrogen levels decline, leading to vaginal atrophy and an increased risk of vaginitis.
Other factors:
- Sexual activity: Sexual activity can introduce new organisms into the vagina, potentially disrupting the microbiome.
- Foreign bodies: Tampons, diaphragms, or other foreign bodies can irritate the vaginal lining and increase the risk of infection.
- Immunosuppression: Women with weakened immune systems are more susceptible to vaginal infections.[11]
Pathophysiology
Pathophysiology:
- Disruption of the vaginal microbiota: The vagina is home to a complex community of microorganisms, known as the vaginal microbiota. This microbiota plays a crucial role in maintaining vaginal health by producing lactic acid, which creates an acidic environment that inhibits the growth of harmful bacteria. Disruption of the vaginal microbiota can lead to an overgrowth of harmful bacteria, which can cause inflammation and infection.
- Inflammation: Inflammation is a natural response to injury or infection. In vaginitis, inflammation can be triggered by various factors, including infections, irritants, and hormonal changes. Inflammation can cause various symptoms, including redness, swelling, itching, and pain.
- Changes in vaginal pH: The normal vaginal pH is acidic, ranging from 3.8 to 4.5. This acidic environment helps to maintain a healthy vaginal microbiota and inhibit the growth of harmful bacteria. Changes in vaginal pH can disrupt the vaginal microbiota and increase the risk of infection.
- Hormonal changes: Hormonal changes, such as those that occur during menopause, can lead to changes in the vaginal epithelium and increase the risk of vaginitis.[11]
Clinical Features
Clinical Features of Vaginitis:
- Abnormal vaginal discharge: This is the most common symptom of vaginitis. The discharge may be thick, thin, white, yellow, green, or gray. It may also have an unpleasant odor.
- Vaginal itching or irritation: This can be mild or severe.
- Vaginal burning or pain: This may be worse during intercourse or urination.
- Vaginal spotting or bleeding: This is less common, but it can occur.
Specific clinical features:
- Bacterial vaginosis (BV): This is the most common cause of vaginitis in women of reproductive age. It is caused by an overgrowth of certain bacteria in the vagina. BV is often associated with a thin, gray discharge that has a fishy odor.
- Yeast infection: This is the second most common cause of vaginitis. It is caused by an overgrowth of yeast in the vagina. Yeast infections are often associated with a thick, white discharge that has a cottage cheese-like appearance.
- Trichomoniasis: This is a sexually transmitted infection (STI) that is caused by a parasite. Trichomoniasis is often associated with a yellow-green discharge that has a foul odor.[12]
Sign & Symptoms
Sign & Symptoms :
- A red, swollen, tender vagina with irritation and burning.
- Dysuria with frequency of micturition [5]
- Our vagina and/or vulva is discolored, irritated, swollen, or uncomfortable.
- Pain or discomfort during sex.
- Vaginal discharge that isn’t normal for you:
- With yeast infections, discharge is usually thick, white, and odorless. You may also have a white coating in and around your vagina.
- With bacterial vaginosis, you may have vaginal discharge that’s grayish, foamy, and smells fishy.
- With trich, discharge is often frothy, yellow-green, smells bad, and may have spots of blood in it. [6]
Clinical Examination
Clinical Examination of Vaginitis :
- The clinical examination for vaginitis includes a careful inspection of the external genitalia, vagina, and cervix.
- The presence of vulvar erythema, edema, excoriation, or discharge should be noted.
- A speculum examination is performed to visualize the vaginal walls and cervix.
- The characteristics of any vaginal discharge, such as color, consistency, and odor, should be documented.
- A cotton swab is used to collect a sample of the discharge for microscopic examination and culture.
- The cervix should be inspected for signs of inflammation or infection, such as erythema, friability, or discharge.
- Bimanual examination is performed to assess for cervical motion tenderness or adnexal masses, which may suggest pelvic inflammatory disease.[11]
Diagnosis
Diagnosis of Vaginitis :
- Review your medical history- This includes your history of vaginal or sexually transmitted infections.
- Perform a pelvic exam- During the pelvic exam, your health care provider might use an instrument (speculum) to look inside your vagina for inflammation and discharge.
- Collect a sample for lab testing- Your health care provider might collect a sample of cervical or vaginal discharge for lab testing to confirm what kind of vaginitis you have.
- Perform pH testing- Your health care provider might test your vaginal pH by applying a pH test stick or pH paper to the wall of your vagina. An elevated pH can indicate either bacterial vaginosis or trichomoniasis. However, pH testing alone is not a reliable diagnostic test.[2]
Differential Diagnosis
Complications
Complications:
Pregnancy complications: Certain types of vaginitis, such as bacterial vaginosis (BV), have been associated with an increased risk of premature rupture of membranes, preterm labor, and low birth weight.
Increased risk of STIs: The presence of vaginitis can disrupt the vaginal microbiome, making women more susceptible to acquiring or transmitting STIs like HIV.
Sexual dysfunction: The discomfort and pain associated with vaginitis can lead to decreased sexual desire and painful intercourse, impacting a woman’s intimate relationships.
Emotional distress: The chronic nature of some vaginitis cases and the impact on sexual health can lead to anxiety, depression, and decreased self-esteem.[13]
Investigations
Investigations:
Microscopic Examination of Vaginal Discharge:
- A sample of vaginal discharge is collected and examined under a microscope.
- This helps to identify the presence of specific microorganisms, such as bacteria, yeast, or trichomonads, which can indicate the cause of vaginitis.
pH Testing:
- The pH of the vaginal discharge is measured using a pH strip.
- A normal vaginal pH is typically between 3.8 and 4.5.
- An elevated pH can suggest bacterial vaginosis or trichomoniasis.
Whiff Test:
- A small amount of potassium hydroxide is added to a sample of vaginal discharge.
- A fishy odor, known as a positive whiff test, is characteristic of bacterial vaginosis.
Culture:
- A sample of vaginal discharge is cultured in a laboratory to identify specific microorganisms, particularly when the initial microscopic examination is inconclusive.
Nucleic Acid Amplification Tests (NAATs):
- These tests detect the genetic material of specific microorganisms, such as Chlamydia trachomatis and Neisseria gonorrhoeae, which can cause sexually transmitted infections (STIs) often associated with vaginitis.
Other Investigations:
- Depending on the patient’s symptoms and medical history, additional investigations may be warranted. These can include:
- Allergy testing
- Blood tests to assess hormone levels or check for underlying medical conditions
- Colposcopy to examine the cervix and vagina for any abnormalities
- Biopsy of vaginal tissue for microscopic examination[7]
- Depending on the patient’s symptoms and medical history, additional investigations may be warranted. These can include:
Treatment
Treatment :
- The cause of the infection determines the appropriate treatment. It may include oral or topical antibiotics and/or antifungal creams, antibacterial creams, or similar medications.
- A cream containing cortisone may also use to relieve some of the irritation. If an allergic reaction involve, an antihistamine may also prescribe. For women who have irritation and inflammation caused by low levels of estrogen (postmenopausal), a topical estrogen cream might prescribe.
The following are typical treatments for trichomoniasis, bacterial vaginosis, and yeast infections i.e.:
- Trichomoniasis: Oral treatment with either metronidazole or tinidazole.
- "Sexual partner(s) should be treated simultaneously.
- Patients should advise to avoid sexual intercourse for at least 1 week and until they and their partner(s) have completed treatment and follow-up."
- Bacterial vaginosis: The most commonly used antibiotics are metronidazole, available in both pill and gel form, and clindamycin available in both pill and cream form.
- Yeast infections: Local azole, in the form of ovula and cream. All agents appear to be equally effective.
- These anti-fungal medications, which are available in over-the-counter form, are generally used to treat yeast infections.
- Treatment may last anywhere between one, three, or seven days.
- Trichomoniasis- Your health care provider may prescribe metronidazole (Flagyl) or tinidazole (Tindamax) tablets.
- Genitourinary syndrome of menopause (vaginal atrophy)- Estrogen — in the form of vaginal creams, tablets or rings — can treat this condition. This treatment is available by prescription from your health care provider, after other risk factors and possible complications reviewed.
- Noninfectious vaginitis– To treat this type of vaginitis, you need to pinpoint the source of the irritation and avoid it. Possible sources include new soap, laundry detergent, sanitary napkins or tampons.[2]
Prevention
Prevention:
- Good hygiene might prevent some types of vaginitis from recurring and relieve some symptoms:
- Avoid baths, hot tubs and whirlpool spas.
- Avoid irritants – These include scented tampons, pads, douches and scented soaps. Rinse soap from your outer genital area after a shower and dry the area well to prevent irritation. Don’t use harsh soaps, such as those with deodorant or antibacterial action, or bubble bath.
- Wipe from front to back after using the toilet. Doing so avoids spreading fecal bacteria to your vagina.
- Avoid douching – Your vagina doesn’t require cleansing other than regular showering. Repetitive douching disrupts the good organisms that live in the vagina and can increase your risk of vaginal infection. Douching won’t clear up a vaginal infection.
- Practice safer sex – Using a condom and limiting the number of sex partners can help.
- Wear cotton underwear – Also wear pantyhose with a cotton crotch. Consider not wearing underwear to bed. Yeast thrives in moist environments.[2]
Homeopathic Treatment
Homeopathic Treatment:
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Vaginitis:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
Pulsatilla – For vaginitis with Thick Vaginal Discharge
- Pulsatilla is a natural homeopathic medicine derived from a plant named Pulsatilla Nigricans or Wind-flower of the natural order Ranunculaceae.
- Pulsatilla is helpful for vaginitis when vaginal discharges are thick like cream.
- They are white (like milk) and get worse on lying down.
- There may be a burning felt in the vagina along with a backache.
Kreosote – For Itching in Vagina
- Kreosote is a natural medicine especially for itching in the vagina in cases of vaginitis.
- The itching is quite intense also violent.
- There may be soreness also burning in the vagina after scratching.
- Furthermore, The genitals are swollen too.
- The vaginal discharge may be either white or yellow and smells putrid.[4]
- Besides this, Standing and walking worsens the discharge.
- Weakness may appear with the discharges.
- Lastly, There is a frequent urge to urinate.
Alumina – For Vaginitis Vaginal Discharges Causing Burning in Vagina
- Alumina offers a natural cure for burning in the vagina due to vaginitis.
- The discharges are worse during the daytime and may be transparent or light yellow.
- They are also highly acrid, corrosive, excoriating.
- Cold washing tends to relieve the symptoms.
- In some cases, stitching and throbbing pain in the vagina is also felt.
Natrum Mur – For Vaginitis with White Vaginal Discharge
- Natrum Mur is an effective natural medicine for vaginitis cases with white vaginal discharges.
- The discharges are thick and profuse and tend to get worse at night.
- They also tend to acrid and are attended with itching and a smarting pain in genitals.
- General weakness may also be present.
Merc Sol – For Greenish Vaginal Discharge in Vaginitis
- Merc Sol a homeopathic medicine used to treat vaginitis with greenish vaginal discharges.
- A night aggravation of the discharges may present.
- The discharges may blood-stained, corrosive and itchy, leading to scratching.
- Scratching often followed by burning.
- A smarting and biting sensation in genitals is also present.
- The genitals may also swollen.
- Pain, itching, and burning during urination in the genitals upon contact with urine is also present.
Hydrastis – For Yellow Vaginal Discharges in Vaginitis
- Homeopathic medicine Hydrastis prepare from the fresh root of a plant Hydrastis Canadensis.
- Use of Hydrastis consider in cases of vaginitis with a yellow discharge from the vagina.
- The discharges are profuse, thick, tenacious, and highly viscid.
- The discharges may stringy and ropy in some cases.
- Occasionally, they may offensive.
- Itching in the vagina appears from discharges.
Sepia – For Vaginitis with Painful Coition
- Sepia is a natural remedy for vaginitis with very painful coition.
- In cases where Sepia works effectively, the vaginal discharges are clear, watery or yellowish-greenish.
- They may also be blood-stained.
- They get worse after urinating.
- The discharges are excoriating with severe vaginal itching and burning pain.
- It may also have a fetid odor.
- Along with the above features, there is an increased frequency of urination.
Graphites – To Manage Profuse, Gushing Vaginal Discharges in Vaginitis
- Homeopathic medicine Graphites is very beneficial for managing profuse, gushing vaginal discharges in vaginitis.
- The discharge is mainly white or yellowish-white.
- It flows through the day and night.
- The discharges are acrid and excoriate the skin.
- They also cause a biting pain in the vagina.
- The back feels weak due to these copious discharges.
Nitric Acid – For Vaginitis with Foul Vaginal Discharge
- Nitric Acid is a natural medicine for vaginitis with vaginal discharges that are offensive.
- In cases needing Nitric Acid, the color of vaginal discharge varies.
- It may be green, brown, flesh-colored or clear like water.
- The discharge is acrid and causes burning in the vulva and vagina.
- Stitching pain in the vagina may also be felt.
Natrum Phos – For Sour-Smelling Vaginal Discharges in Vaginitis
- Natrum Phos is an effective medicine for sour-smelling vaginal discharges in cases of vaginitis.
- The discharges from the vagina may be creamy or watery, and often honey-colored.
- They are often acidic.
Medorrhinum – For Vaginal Discharge with Fish-like Odours
- Medorrhinum is a natural remedy for vaginitis where the vaginal discharges have a peculiar fishy odor.
- The discharges are acrid, excoriating with excessive itching.
- Washing with lukewarm water relieves the itching.
- The discharges are also very thick.
- An attending gonorrhea infection may be present in cases needing Medorrhinum.
Diet & Regimen
Diet & Regimen:
for Vaginitis
Diet
While diet alone can’t cure vaginitis, certain foods can help support vaginal health and potentially reduce the risk of infections:
- Probiotic-rich foods: Yogurt, kefir, sauerkraut, and kimchi contain "good" bacteria (like Lactobacillus) that can help maintain a healthy vaginal pH balance and fight off harmful bacteria.
- Cranberries: Cranberries (especially unsweetened cranberry juice or extract) may help prevent urinary tract infections (UTIs), which sometimes occur alongside vaginitis.
- Fruits and vegetables: A diet rich in fruits and vegetables provides essential nutrients and antioxidants that support overall health, including 1 vaginal health. 1. blog.medzell.netblog.medzell.net
- Foods high in vitamin C: Vitamin C boosts the immune system, which can help fight off infections.
- Omega-3 fatty acids: Found in fatty fish, flaxseeds, and walnuts, omega-3s have anti-inflammatory properties.
Foods to Limit or Avoid:
- Sugary foods and drinks: Sugar can promote the growth of yeast, which can worsen yeast infections (a common cause of vaginitis).
- Processed foods: These often lack nutritional value and may contribute to inflammation.
- Alcohol: Excessive alcohol consumption can weaken the immune system.
Regimen for Vaginitis
In addition to diet, these practices can help prevent and manage vaginitis:
- Good hygiene:
- Wipe from front to back after using the toilet to prevent bacteria from spreading from the rectum to the vagina.
- Wash the vulva (external genital area) with mild, unscented soap and water. Avoid douching, as it can disrupt the natural balance of bacteria in the vagina.
- Cotton underwear and loose-fitting clothes: This allows for better air circulation and reduces moisture, which can discourage the growth of harmful bacteria and yeast.
- Safe sex practices: Use condoms to reduce the risk of sexually transmitted infections (STIs), which can cause vaginitis.
- Avoid irritants: Scented soaps, bubble baths, feminine hygiene products, and tight-fitting clothing can irritate the vagina.
Do’s and Don'ts
Do’s & Don’ts of Vaginitis :
Vaginitis Do’s & Don’ts
Do’s:
Maintain good hygiene:
- Wash your external genitals (vulva) daily with mild, unscented soap and water.
- Pat the area dry gently; avoid rubbing.
- Wipe from front to back after using the toilet to prevent bacteria from the anus from entering the vagina.
Practice safe sex:
- Use condoms to reduce the risk of sexually transmitted infections that can lead to vaginitis.
- Limit the number of sexual partners.
Wear breathable clothing:
- Choose cotton underwear and loose-fitting clothes to allow air circulation and keep the area dry.
- Avoid tight-fitting pants, nylon underwear, and pantyhose without a cotton crotch.
Change tampons and pads regularly
Manage underlying conditions:
- If you have diabetes, keep your blood sugar levels under control, as high blood sugar can increase the risk of yeast infections.
Eat a balanced diet:
- Include yogurt with live cultures in your diet, as it may help maintain a healthy balance of bacteria in the vagina.
Don’ts:
Should’t douche:
- Douching disrupts the natural balance of bacteria in the vagina, increasing the risk of infection.
Avoid harsh soaps and scented products:
- Scented soaps, bubble baths, feminine hygiene sprays, and scented toilet paper can irritate the vagina.
Don’t wear wet or damp clothing:
- Change out of wet swimsuits or sweaty workout clothes promptly, as moisture can promote the growth of yeast and bacteria.
Don’t scratch:
- Scratching can further irritate the area and potentially lead to skin breakdown and infection.
Never have sex if you have symptoms:
- Avoid sexual intercourse until your symptoms have cleared up to prevent spreading the infection to your partner.
Terminology
Terminology:
Vaginitis
- Meaning: Inflammation of the vagina, often accompanied by discomfort, discharge, and changes in vaginal odor.
- Significance: A broad term encompassing various conditions affecting the vaginal tissues, often requiring diagnosis to pinpoint the specific cause.
Bacterial Vaginosis (BV)
- Meaning: A common type of vaginitis caused by an imbalance in the natural vaginal bacteria, leading to an overgrowth of certain bacteria.
- Significance: Often characterized by a thin, gray or white discharge with a fishy odor, especially after intercourse.
Yeast Infection (Candidiasis)
- Meaning: A vaginal infection caused by an overgrowth of the fungus Candida albicans, commonly known as yeast.
- Significance: Typically associated with thick, white, curd-like discharge, along with itching and burning.
Trichomoniasis
- Meaning: A sexually transmitted infection caused by the parasite Trichomonas vaginalis.
- Significance: May cause a frothy, yellow-green discharge, itching, and discomfort during urination or intercourse.
Atrophic Vaginitis
- Meaning: Vaginal inflammation due to thinning and drying of the vaginal tissues, often associated with decreased estrogen levels after menopause.
- Significance: Can lead to dryness, burning, itching, and painful intercourse.
Leukorrhea
- Meaning: A normal white or clear vaginal discharge, typically occurring in increased amounts during ovulation or pregnancy.
- Significance: Distinguishing normal leukorrhea from abnormal discharge is crucial for identifying potential vaginal infections.
pH
- Meaning: A measure of the acidity or alkalinity of the vaginal environment, normally slightly acidic (pH 3.8-4.5).
- Significance: An elevated pH can indicate certain infections, such as bacterial vaginosis.
Discharge
- Meaning: Fluid secreted from the vagina, which can vary in color, consistency, and odor depending on the underlying cause.
- Significance: Observing changes in discharge can provide valuable clues for diagnosing vaginal infections.
Dyspareunia
- Meaning: Painful sexual intercourse.
- Significance: Can be a symptom of various vaginal conditions, including infections and atrophic vaginitis.
Pruritus
- Meaning: Itching.
- Significance: A common symptom of many vaginal infections, including yeast infections and trichomoniasis.
Homoeopathic Terminology:
- Miasm: In homeopathy, a miasm is a predisposing factor or inherited taint that can contribute to disease susceptibility.
- Constitutional Remedy: A homeopathic remedy chosen based on the individual’s overall physical, mental, and emotional characteristics, rather than just the specific symptoms of the disease.
- Potency: The strength or dilution of a homeopathic remedy.
- Repertory: A reference book used by homeopaths to find remedies based on specific symptoms.
- Materia Medica: A collection of detailed descriptions of the properties and effects of homeopathic remedies.
References
References :
- DC Dutta’s Textbook of Gynecology: Including Contraception (6th edition)
- https://www.mayoclinic.org › vaginitis
- Clinical_Gynecology.pdf
- https://my.clevelandclinic.org/health/diseases/9131-vaginitis
- Gynacology VG Padubidri.pdf
- https://www.plannedparenthood.org/learn/health-and-wellness/vaginitis
- https://www.ncbi.nlm.nih.gov/books
- https://www.medicalnewstoday.com/articles/327507
- Prevalence and diagnosis of bacterial Vaginosis in tertiary care teaching hospital, 2017
Prevalence of Vulvovaginal Infections and Species Specific Distribution of Vulvovaginal Candidiasis in Married Women of North India,2013
- Comprehensive Gynecology, 7th Edition. By Lobo RA, Gershenson DM, Lentz GM, Valea FA. Elsevier, 2017.
- Clinical Gynecologic Endocrinology and Infertility, 8th Edition
- Hacker, Neville F., and Joseph C. Gambone. Essentials of Obstetrics and Gynecology. 6th ed. Elsevier Saunders, 2016.
Also Search As
Also Searched As:
Online Search Engines
- This is the most common method. Use specific keywords such as:
Homeopathic Websites and Forums
Many homeopathic organizations and practitioners have websites with articles and resources. Search on sites like:
The National Center for Homeopathy (NCH)
The American Institute of Homeopathy (AIH)
The British Homeopathic Association (BHA)
Homeopathic Educational Services (HES)
You can also explore online forums dedicated to homeopathy, where practitioners and patients share information.
Homeopathic Journals and Publications
- Search databases of homeopathic journals for peer-reviewed articles on vaginitis. Some reputable journals include:
- The American Journal of Homeopathic Medicine
- Homeopathy
- The European Journal of Integrative Medicine
Using search engines like Google:
- This is the most common and accessible method. Simply type "vaginitis" into the search bar, and you’ll get a plethora of information, including articles, images, and videos. You can refine your search by adding specific keywords, such as "vaginitis symptoms," "vaginitis causes," or "vaginitis treatment."
Homeopathic Libraries
- If you have access to a homeopathic library, browse their collection or consult a librarian for assistance.
Homeopathic Practitioners
- Ask your homeopathic practitioner for recommendations on articles or resources. They may have their own publications or be able to guide you to reliable sources.
Using medical websites and databases:
Reputable medical websites like Mayo Clinic, Cleveland Clinic, and WebMD offer reliable and detailed information on vaginitis. Medical databases like PubMed provide access to scientific articles and research papers.
Consulting healthcare professionals:
- The most reliable way to get information about vaginitis is to talk to your doctor or a qualified healthcare professional. They can provide personalized advice based on your specific symptoms and medical history.
Using health forums and online communities:
- While these platforms can offer support and shared experiences, it’s important to be cautious about the information you find there. Always verify any information you find on forums with reliable sources.
Using mobile apps:
- Several health apps offer information and resources on various health conditions, including vaginitis. These apps can be convenient for accessing information on the go.
Frequently Asked Questions (FAQ)
What is Vaginitis?
Vaginitis is an inflammation of the vagina that can result in discharge, itching and pain.
What causes Vaginitis?
- Chemicals
- Drugs
- Douches
- Pessaries
- Tampons
Give the types of Vaginitis?
- Candida or “yeast” infections.
- Bacterial vaginosis.
- Trichomoniasis vaginitis.
- Chlamydia or Gonorrhoea.
- Viral vaginitis (herpes).
- Non-infectious vaginitis.
- Atrophic vaginitis.
Can vaginitis be prevented?
- Practicing good hygiene
- Avoiding douching
- Wearing cotton underwear
- Using condoms during sexual activity
- Managing stress
- Eating a healthy diet
What are the symptoms of Vaginitis?
- A red, swollen, tender vagina with irritation and burning.
- Dysuria with frequency of micturition
- Vagina and/or vulva is discolored, irritated, swollen, or uncomfortable.
- Pain or discomfort during sex.
Can homeopathy cure vaginitis completely?
- Homeopathy aims to address the underlying cause of vaginitis, potentially leading to complete resolution of symptoms. However, the effectiveness can vary depending on individual factors and the severity of the condition.
Can homeopathy prevent recurrent vaginitis?
- By addressing the underlying susceptibility and strengthening the immune system, homeopathy may help reduce the frequency and severity of recurrent vaginitis.
How long does it take to see results with homeopathy for vaginitis?
- The response time can vary depending on the individual and the severity of the condition. Some people may experience relief within a few days, while others may require a longer duration of treatment.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Vaginitis?
Homeopathic Medicines
- Pulsatilla
- Kreosote
- Alumina
- Natrum Mur
- Merc Sol
- Hydrastis
- Sepia
