Vomiting in Pregnancy
Definition
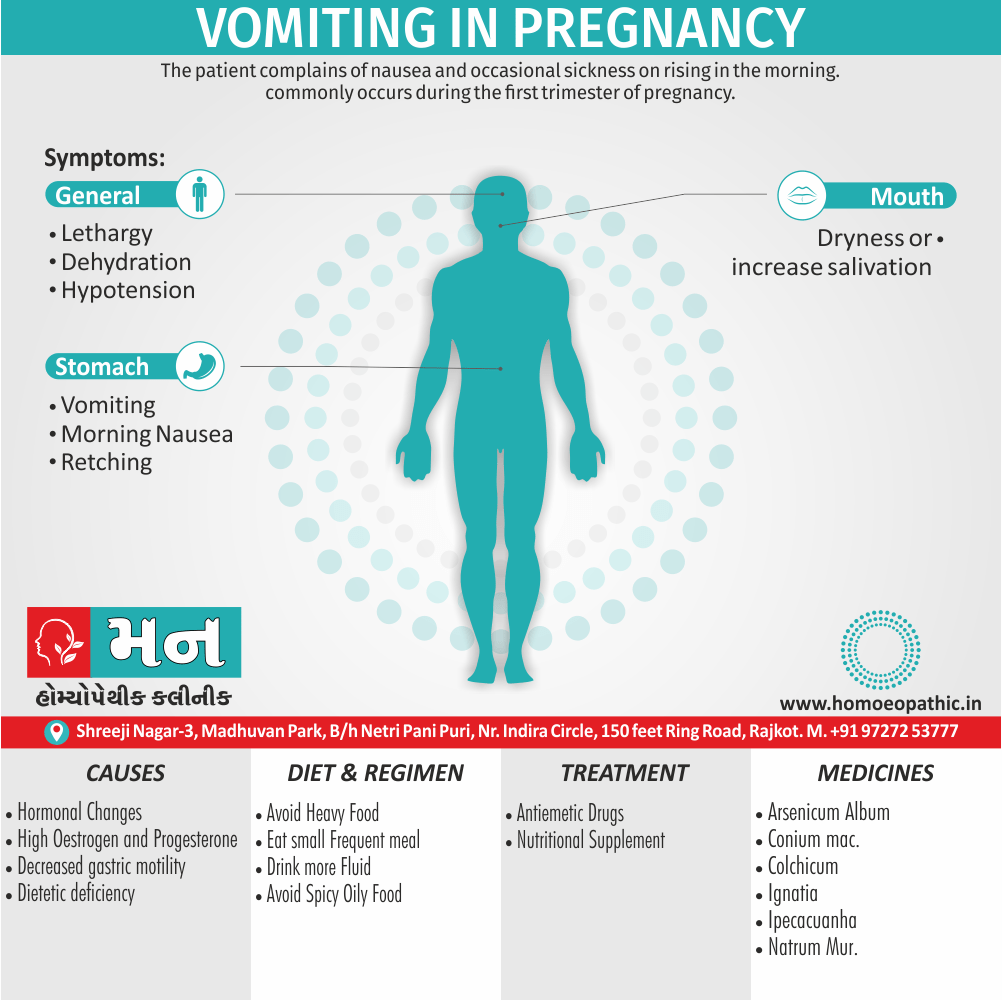
Vomiting in Pregnancy is defined as the complaints of patient about nausea and occasional sickness on rising in the morning, commonly occurs during the first trimester of pregnancy.
Vomiting in pregnancy is a common symptom, especially during the first trimester. While there isn’t a direct synonym, it is often referred to as:
- Morning sickness: Although it can occur at any time of the day or night.
- Nausea and vomiting of pregnancy (NVP): This is the medical term for the condition.
- Emesis gravidarum: Another medical term used for vomiting during pregnancy.
- Pregnancy sickness: A general term for nausea and vomiting during pregnancy.
The severity of vomiting in pregnancy can vary, ranging from mild nausea to severe vomiting that requires medical attention.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview:
Vomiting is a symptom which may be related to pregnancy or may be a manifestation of some medical surgical-gynaecological complications, which can occur at any time during pregnancy. The Former is by far the most common one and is called vomiting of pregnancy.
There has been marked fall in the incidence during the last 30 years.
It is now a rarity in hospital practice (less than 1 in 1,000 pregnancies). The reasons are — (a) Better application of family planning knowledge which reduces the number of unplanned pregnancies, (b) Early visit to the antenatal clinic and (c) Potent antihistaminic and antiemetic drugs. The Causes of vomiting in pregnancy can be classified as follows:[1]
Early Pregnancy
- Simple vomiting (Morning sickness, emesis gravidarum)
- Hyperemesis gravidarum (Pernicious vomiting)
2. Late Pregnancy
- Continuation or reappearance of simple vomiting of pregnancy
- Acute fulminating preeclampsia[1]
Epidemiology
Epidemiology of Vomiting in Pregnancy:
Nausea and vomiting during pregnancy (NVP) is a common occurrence, affecting a significant proportion of pregnant women worldwide. In India, studies have shown a prevalence ranging from 50% to 80%, although there is some variability depending on the specific population and study design.
Another study published in the Journal of Obstetrics and Gynecology of India in 2012, "Prevalence and Severity of Nausea and Vomiting During Pregnancy" (S. K. Sharma, et al.) reported a slightly lower prevalence of 58.7% in a cohort of pregnant women in Delhi.[3][4]
Causes
Causes of Vomiting in Pregnancy:
The aetiology is obscure but the following are the known facts:
(1) It is mostly limited to the first trimester
(2) It is more common in first pregnancy, with a tendency to recur again in subsequent pregnancies (15%)
(3) Younger age
(4) Low body mass
(5) History of motion sickness or migraine
(6) It has got a familial history — mother and sisters also suffer from the same manifestation
(7) It is more prevalent in hydatidiform mole and multiple pregnancy
(8) It is more common in unplanned pregnancies but much less amongst illegitimate ones. Women with hyperemesis gravidarum, often suffer from transient form of hyperthyroidism (clinical or subclinical).[2]
Types
Classification of Vomiting in Pregnancy:
The vomiting is related to the pregnant state and depending upon the severity, it is classified as:
(i) Simple vomiting of pregnancy or milder type
(ii) Hyperemesis gravidarum or severe type
1] SIMPLE VOMITING (morning sickness, emesis gravidarum)
SIGN AND SYMPTOMS i.e.:
- The patient complains of nausea and occasional sickness on rising in the morning. Slight vomiting is so common in early pregnancy (about 50%) that it is considered as a symptom of pregnancy. It may, however, occur at other times of the day. The vomitus is small and clear or bile stained.
- It does not produce any impairment of health or restrict the normal activities of the women. Besides this, The feature disappears with or without treatment by 12–14th week of pregnancy.
ETIOLOGICAL FACTOR i.e.:
- High level of serum human chorionic gonadotropin, oestrogen also altered immunological states are considered responsible for initiation of the manifestation, which is probably aggravated especially by the neurogenic factor.
DIETARY MEASURE i.e.:
- Taking of dry toast or biscuit and avoidance of fatty also spicy foods are enough to relieve the symptoms in majority.
TREATMENT i.e.:
- Supplementation with vitamin B1 100 mg daily is helpful. In detail, If the simple measures fail, antiemetic drugs trifluoperazine (Espazine) 1 mg twice daily is quite effective.
- Promethazine also ondansetron can be used. Furthermore, Patient is advised to take plenty of fluids (2.5 L in 24 hours) and fruit juice.[1]
2] HYPEREMESIS GRAVIDARUM
- It is a severe type of vomiting of pregnancy which has got deleterious effect on the health of mother and/or incapacitates her in day-to-day activities.
EFFECTS i.e.:
- The adverse effects of severe vomiting are e.g. dehydration, metabolic acidosis (from starvation) or alkalosis (from loss of hydrochloric acid), electrolyte imbalance (hypokalemia) and weight loss.[1]
Risk Factors
Risk factors:
- History of nausea and vomiting in previous pregnancies or with oral contraceptive use: Women who experienced nausea and vomiting in prior pregnancies or while taking oral contraceptives are more likely to have similar symptoms in subsequent pregnancies.
- Multiple gestation: Carrying twins or higher-order multiples increases the risk of severe nausea and vomiting.
- Molar pregnancy: This rare condition, where abnormal tissue grows in the uterus instead of a fetus, can cause severe nausea and vomiting.
- Hyperemesis gravidarum: This condition involves severe and persistent nausea and vomiting that can lead to dehydration, weight loss, and electrolyte imbalances. While the exact cause is unknown, it is believed to be related to hormonal changes during pregnancy.
- Younger maternal age: Studies suggest that younger women may be more susceptible to experiencing nausea and vomiting during pregnancy.
- Obesity: Some research indicates that women with a higher body mass index (BMI) may have an increased risk of severe nausea and vomiting.
- Migraine headaches: Women with a history of migraines may be more likely to experience nausea and vomiting during pregnancy.
- Psychological factors: Stress, anxiety, and depression can contribute to the severity of nausea and vomiting in pregnancy.[5]
Pathogenesis
Pathogenesis:
Hormonal Fluctuations:
- Elevated Human Chorionic Gonadotropin (hCG): Studies have linked high hCG levels, especially during the first trimester, to nausea and vomiting.
- Estrogen and Progesterone: Increased levels of these hormones may also play a role in triggering vomiting.
Gastrointestinal Changes:
- Delayed Gastric Emptying: Pregnancy hormones can slow down the movement of food through the digestive tract, leading to nausea and vomiting.
- Heightened Olfactory Sensitivity: Pregnant women often experience a heightened sense of smell, which can trigger nausea in response to certain odors.
Psychological Factors:
- Stress and Anxiety: Emotional stress can exacerbate nausea and vomiting in susceptible individuals.
- Previous History of Motion Sickness or Migraines: Women with a history of these conditions may be more prone to vomiting during pregnancy.[5]
Pathophysiology
Pathophysiology:
(1) Hormonal:
(a) Excess of chorionic gonadotropin or higher biological activity of HCG is associated. This is proved by the frequency of vomiting at the peak level of HCG and also the increased association with hydatidiform mole or multiple pregnancy when the HCG titre is very much raised
(b) High serum level of oestrogen
(c) Progesterone excess leading to relaxation of the cardiac sphincter and simultaneous retention of gastric fluids due to impaired gastric motility. Other hormones involved are: thyroxine, prolactin, leptin and adrenocortical hormones.
(2) Psychogenic:
It probably aggravates the nausea once it begins. But neurogenic element sometimes plays a role, as evidenced by its subsidence after shifting the patient from the home surroundings. Conversion disorder, somatization, excess perception of sensations by the mother are the other theories.
(3) Dietetic deficiency:
Probably due to low carbohydrate reserve, as it happens after a night without food. Deficiency of vitamin B6, vitamin B1 and proteins may be the effects rather than the cause.
(4) Allergic or immunological basis
(5) Decreased gastric motility is found to cause nausea
Whatever may be the cause of initiation of vomiting, it is probably aggravated by the neurogenic element. Unless it is not quickly rectified, features of dehydration and carbohydrate starvation supervene and a vicious cycle of vomiting appears — vomiting → carbohydrate starvation → ketoacidosis → vomiting.[1]
There are no specific morbid anatomical findings. The changes in the various organs as described by Sheehan are the generalized manifestations of starvation and severe malnutrition.
Liver:
Liver enzymes are elevated. There is centrilobular fatty infiltration without necrosis.
Kidneys:
Usually normal with occasional findings of fatty change in the cells of first convoluted tubule,
which may be related to acidosis.
Heart:
A small heart is a constant finding. There may be subendocardial haemorrhage.
Brain:
Small haemorrhages in the hypothalamic region giving the manifestation of Wernicke’s encephalopathy. The lesion may be related to vitamin B1 deficiency.
METABOLIC, BIOCHEMICAL AND CIRCULATORY CHANGES:
The changes are due to the combined effect of dehydration and starvation consequent upon vomiting.
Metabolic:
Inadequate intake of food results in glycogen depletion. For the energy supply, the fat reserve is broken down. Due to low carbohydrate, there is incomplete oxidation of fat and accumulation of ketone bodies in the blood. The acetone is ultimately excreted through the kidneys and in the breath. There is also increase in endogenous tissue protein metabolism resulting in excessive excretion of nonprotein nitrogen in the urine. Water and electrolyte metabolism are seriously affected leading to biochemical and circulatory changes.
Biochemical:
Patients develop acidosis (due to starvation) and alkalosis from loss of hydrochloric acid and hypokalaemia. Loss of water and salts in the vomitus results in fall in plasma sodium, potassium and chlorides. The urinary chloride may be well below the normal 5 g/L or may even be absent. Hepatic dysfunction results in ketosis with rise in blood urea and uric acid. Patient suffers from hypoglycemia, hypoproteinaemia and hypovitaminosis.
Circulatory:
There is haemoconcentration leading to rise in haemoglobin percentage, RBC count and haematocrit values. Slight increase in the white cell count with increase in eosinophils. There is concomitant reduction of extracellular fluid.[1]
Clinical Features
Clinical Features:
- Timing: Typically begins between 4 and 7 weeks’ gestation, peaks at 9 weeks, and usually abates by 16 to 18 weeks.
- Severity: Varies widely, from mild nausea to intractable vomiting requiring hospitalization.
- Symptoms: Nausea, vomiting, food aversions, and occasionally weight loss.
- Complications: Dehydration, electrolyte imbalances, and rarely, Wernicke encephalopathy (due to thiamine deficiency).
- Impact on Quality of Life: Can significantly affect daily activities and well-being.[5]
Sign & Symptoms
Sign & Symptoms of Vomiting in Pregnancy
From the management and prognostic point of view, the cases are grouped into:
- Early
- Late (moderate to severe)
The patient is usually a nullipara, in early pregnancy. The onset is insidious.
EARLY:
Vomiting occurs throughout the day. Normal day-to-day activities curtail. Additionally, There is no evidence of dehydration or starvation.
LATE:
(Evidences of dehydration and starvation are present).
Symptoms:
Vomiting increase in frequency with retching. In detail, Urine quantity diminish even to the stage of oliguria. Epigastric pain, constipation may occur. Complications may appear if not treat.
Signs:
Features of dehydration and ketoacidosis: Dry coated tongue, sunken eyes, acetone smell in breath, tachycardia, hypotension, rise in temperature may be noted, jaundice is a late feature. Such late cases rarely seen these days. Vaginal examination and/or ultrasonography done to confirm the diagnosis of pregnancy.
Clinical Examination
Clinical Examination:
Detailed History:
- Onset and duration of vomiting: Establish when the vomiting started and how long it has been ongoing.
- Frequency and severity: Determine how often the vomiting occurs and its intensity.
- Associated symptoms: Inquire about other symptoms such as abdominal pain, fever, diarrhea, or weight loss.
- Dietary intake and fluid intake: Assess the patient’s recent food and fluid consumption.
- Past medical and obstetric history: Review any pre-existing medical conditions or previous pregnancies with similar symptoms.
- Medication and supplement use: Identify any medications or supplements the patient is currently taking.
Physical Examination:
- General appearance: Observe the patient’s overall health and hydration status.
- Vital signs: Measure blood pressure, heart rate, respiratory rate, and temperature.
- Abdominal examination: Palpate the abdomen for tenderness, masses, or organomegaly.
- Pelvic examination: May be performed to rule out other causes of nausea and vomiting, such as ovarian cysts or pelvic inflammatory disease.
- Neurological examination: Assess mental status and reflexes if indicated.[5]
Diagnosis
Diagnosis:
The pregnancy is to be confirmed first.
Thereafter, all the associated causes of vomiting (enumerated before) are to be excluded.
Ultrasonography is useful not only to confirm the pregnancy but also to exclude other, obstetric (hydatidiform mole, multiple pregnancy), gynaecological, surgical or medical causes of vomiting.[1]
Differential Diagnosis
Differential Diagnosis:
- Gastrointestinal causes: gastroenteritis, peptic ulcer disease, gastroesophageal reflux disease (GERD), pancreatitis, cholecystitis, hepatitis, appendicitis, bowel obstruction
- Endocrine causes: hyperthyroidism, diabetic ketoacidosis, adrenal insufficiency
- Neurological causes: migraine, intracranial mass, vestibular disorders
- Urological causes: pyelonephritis, nephrolithiasis
- Other causes: medications, psychiatric disorders (e.g., anxiety, depression)[6]
Complications
Complication:
Maternal:
(1) Neurologic complications:(a) Wernicke’s encephalopathy, beriberi due to thiamine deficiency;(b) Pontine myelinolysis;(c) Peripheral neuritis;(d) Korsakoff’s psychosis.
(2) Stress ulcer in stomach
(3) Oesophageal tear
(4) Jaundice, hepatic failure
(5) Convulsions and coma
(6) Hypoprothrombinaemia due to vitamin K deficiency
(7) Renal failure
Effects on the foetus:
Foetus usually remains unaffected once the problem is resolved.
Foetal risks may be due to low birth weight.[1]
Investigations
Investigation:
Urinalysis:
(1) Firstly, Quantity—small, (2) Secondly, Dark colour, (3) Thirdly, High specific gravity with acid reaction, (4) Fourthly, Presence of acetone, occasional presence of protein and rarely bile pigments and (5) Lastly, Diminished or even absence of chloride.
Biochemical and circulatory changes:
The changes are mentioned previously. Routine and periodic estimation of the serum electrolytes (sodium, potassium and chloride) is helpful in the management of the case.
Serum TSH, T3 and Free T4:
Women may suffer from transient phase of thyroid dysfunction (clinical or subclinical).
Ophthalmoscopic examination is required if the patient is seriously ill. Retinal haemorrhage and detachment of the retina are the most unfavourable signs.
ECG when there is abnormal serum potassium level.[1]
Treatment
Treatment of Vomiting in Pregnancy:
The principles in the management are:
Maintenance of hydration i.e.
- Antiemetic drugs promethazine (Phenergan) 25 mg or prochlorperazine (Stemetil) 5 mg or triflupromazine (Siquil) 10 mg may administer twice or thrice daily intramuscularly. Trifluoperazine (Espazine) 1 mg twice daily intramuscularly is a potent antiemetic therapy. Vitamin B6 and doxylamine are also safe and effective. Metoclopramide stimulates gastric and intestinal motility without stimulating the secretions. It is found useful.
- Hydrocortisone 100 mg IV in the drip give in a case with hypotension or in intractable vomiting. Oral method prednisolone also use in severe cases.
- Nutritional supplementation— with vitamin B1 (100 mg daily), vitamin B6, vitamin C and vitamin B12 are given.
To correct the fluids and electrolytes imbalance
To correct metabolic disturbances (acidosis or alkalosis)
To prevent the serious complications of severe vomiting
Care of pregnancy
Hospitalization
Nursing care: Sympathetic but firm handling of the patient is essential. Social and psychological support should extend.
Hyperemesis progress chart is helpful to assess the progress of patient while in hospital. Daily record of pulse, temperature, blood pressure at least twice daily, intake-output, urine for acetone, protein, bile, blood biochemistry and ECG (when serum potassium is abnormal) are important.
Clinical features of improvement are evidenced by i.e.—
(a) Subsidence of vomiting
(b) Feeling of hunger
(c) Better look
(d) Normalization of blood biochemistry (electrolytes)
(e) Disappearance of acetone from the breath and urine
(f) Normal pulse and blood pressure
(g) Normal urine output.
Prevention
Prevention:
Dietary Adjustments
- Small, Frequent Meals: Consuming smaller meals more frequently throughout the day helps to prevent an empty stomach, which can trigger nausea.
- Bland Foods: Avoiding greasy, spicy, or strongly flavored foods is recommended.
- Carbohydrate-Rich Snacks: Crackers, toast, or plain rice cakes can help settle the stomach.
- Ginger: Consuming ginger in various forms, such as tea, candies, or capsules, has been shown to be effective in reducing nausea.
- Vitamin B6: Supplementing with vitamin B6 can also help alleviate symptoms.
Lifestyle Modifications
- Adequate Rest: Fatigue can worsen nausea, so ensuring adequate rest is important.
- Stress Management: Techniques such as meditation, yoga, or deep breathing can help manage stress, which can contribute to nausea.
- Avoiding Triggers: Identifying and avoiding specific triggers, such as certain smells or foods, can be helpful.
- Hydration: Staying well-hydrated is important, although it’s best to sip fluids slowly throughout the day rather than drinking large amounts at once.
Acupressure and Acupuncture
- P6 Point: Applying pressure to the P6 point on the wrist (inner forearm, three finger widths below the wrist crease) has been shown to be effective in reducing nausea.
- Acupuncture: Consult a licensed acupuncturist for potential relief.
Medications
- When dietary and lifestyle modifications are insufficient, medications may be considered. Consult your healthcare provider to discuss appropriate options.[7]
Homeopathic Treatment
Homeopathic Treatment of Vomiting in Pregnancy :
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness are also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can be greatly improved with homeopathic medicines.
Homeopathic Medicines for Vomiting in Pregnancy
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications are also taken into account for selecting a remedy.
Homeopathic Medicine:
Acitic Acid
- Sour belching and vomiting during pregnancy, with profuse water brash and salivation, day and night, sensation as if an ulcer were in the stomach, giving great uneasiness.
- intense thirst, passing a large quantity of urine and great prostration.
Arsenicum Album
- Vomiting after eating and drinking, and at night, of green or black matter; cold water seems to lie on stomach, although great desire for it; burning pains in precordium and anguish; burning pains in stomach.
- Bowels and breasts; great weakness and exhausting diarrhoea; (>) by motion.
- Food relish but leaves a bitter taste in mouth; aversion to meats and desire for fruits and vegetables; coldness and restlessness.
Colchicum
- Great sensitiveness to the smell of food; indifferent to surroundings, fretful; face flushed, faint aching about navel as if she must eat, but with loathing and disgust for food at the thought, sight or smell of it.
- All attempts to eat cause violent nausea and vomiting. Albuminuria, cannot stand erect or lie down with stretched out legs without vomiting, has to flex knees crouch together for relief.
Conium
- Nausea only or worse while lying down; terrible nausea in vomiting in women suffering from scirrhosities, the vomited matter white and frothy or looking like coffee-grounds.
- Swelling or soreness of breasts, especially when it has been habitual during menses; intermittent urination; eructations and heartburn.[2]
Cyclamen
- Wants no breakfast; after eating the least quantity, nausea and disgust for food in mouth and throat; feels as if brain were in motion when leaning against something.
- Vertigo, objects turn in a circle about her; dimness of vision, with fiery sparks before eyes;
- Intermittent thirst; greasy taste, and fat food disagrees; nocturnal flatulency from atony of bowels, causing distention, (<) by getting up and walking about.
Ferrum Phos
- Vomiting of food undigested, sooner or later after eating, vomiting of food, with sour fluid; vomiting of bright-red blood, with tendency to from a gelatinous mass.
- Suddenly leaves table and with one effort vomit up the and then sets down and eats again.
Gossypium
- Great distress, weakness and marked prostration; nausea before breakfast; useful in very bad cases where miscarriage threaten.
- Nausea from least motion in morning soon after waking, with distress in pit of stomach; and immediately on raising head,
- Retching and violent efforts to vomit at first very little comes up, except wind, with a loud noise, soon saliva and some thick fluids discharge and occasionally a little bilious matter, but rarely and ingesta, followed by faintness.
Ignatia
- Great emptiness; qualmishness also weakness in region of stomach, with flat taste; additionally, distention of abdomen after eating; hiccough; sour eructations;
- Frequent regurgitation of food also of bitter liquid; vomiting at night of food taken in the evening.
- Empty retching relieved especially by eating, salivation, copious lemon- colored urine; clavus hysterics.
Ipecacuanha
- One continual sense of nausea all the time. In detail, vomiting fluids and solids in an undigested state; vomiting of large quantities of mucus; bilious vomiting; diarrhoea and colic;
- Desire for dainties and sweets or averse to all food; stomach feels relaxed; nausea with salivation also hiccough; foul breath; distended abdomen; sleepy after vomiting.[2]
Lobelia Inflata
- Vomiting with profuse flow of saliva; additionally frequent gulping up of burning sour fluid.
- Nausea (<) at night and after sleeping, (>) by a little food or drink and in some cases (<) from food and drink; faintness.
- After vomiting breaks out in a sweat, followed especially by a sensation as of needles pricking her all over; asthmatic sufferings.
Natrum Muriaticum
- Morning nausea; vomiting of food; profuse, constant Waterbrash, like limpid mucus.
- Obstinate cases, with loss of appetite and taste; great hunger, as if stomach were empty, but no appetite; heartburn after eating;
- Headache on awaking in the morning; palpitation; dreams of robbers in house, which must search for to satisfy her whim.
Nux Vomica
- Nausea in early morn, with fainting; vomiting after eating or thinks she would feel better if she could vomit; food and drink smell bad to her, cannot bear the smell of tobacco.
- Bitter or sour taste, belching, eructations, hiccough and heartburn; vomiting of a sticky mucus and a sour fluid; restless sleep, particularly after 3 A.M.
- Great depression and irritability, wants to left alone; longing for alcoholic stimulants; constipation.
Petroleum
- Applicable to all gastric troubles of pregnant women, vomiting of bile; aversion to fat food also meat: (<) when riding in carriage; besides this dizziness and stupefaction after a slight meal.
- Dimness of sight; additionally constant and profuse collection of fluid in mouth, with frequent spitting and nausea; diarrhoea only in daytime.
Sepia
- Vomiting of either milky water or mucus; sense of emptiness in pit of stomach; thought of food sickens her; taste as of manure; aversion to meat and bread; morning nausea.
- Vomiting of either food or bile, finally even blood; before pregnancy uterine anomalies, with either yellowish or purulent; leucorrhea; morning sickness, reflex hard, tumefied cervix.
Silicea
- Qualmishness also vomiting in women whose menses were always accompanied by palpitation. Additionally, taste of blood in the morning; nausea, with palpitation of heart after every exercise that raises the temperature of body; aversion to meat; constipation;
- Great weakness at night; pressure at pit of stomach; nausea specifically after lying down; frequent sour or loud eructation; vomiting after every drink; NERVOUS exhaustion.[2]
Diet & Regimen
Diet & Regimen:
for Pregnancy Vomiting
Diet
- Bland is Best: Think the BRAT diet: Bananas, Rice, Applesauce, Toast. These are easy on the stomach and provide energy.
- Small, Frequent Meals: Grazing throughout the day keeps your blood sugar stable and your stomach from getting too empty (a major nausea trigger!).
- Hydration Heroes: Sip on fluids constantly, even if you’re vomiting. Good choices include:
- Water
- Ginger ale (flat)
- Electrolyte drinks
- Clear broths
- Ginger Power: Ginger is a natural nausea fighter. Try ginger tea, ginger candies, or even ginger ale.
- Protein Boost: Protein helps keep nausea at bay. Include lean meats, eggs, yogurt, and nuts in your diet.
- Vitamin B6: Some studies suggest B6 can help with morning sickness. Find it in foods like bananas, chicken, and spinach.
Foods to Avoid:
- Greasy, Fatty Foods: These are harder to digest and can worsen nausea.
- Spicy Foods: Can irritate the stomach.
- Strong Smells: Even the smell of certain foods can trigger nausea. Avoid cooking or being around strong odors.
Regimen for Pregnancy Vomiting
- Rest: Fatigue can worsen nausea. Get plenty of sleep and rest when you need to.
- Acupressure: Wristbands that apply pressure to the P6 acupressure point (inner wrist) may provide relief for some women.
- Morning Routine: Keep crackers or dry toast by your bed and eat a few before getting up in the morning.
- Fresh Air: Open a window or take a short walk outside for some fresh air.
- Avoid Triggers: Identify and avoid anything that seems to trigger your nausea, whether it’s a certain food, smell, or activity.
- Prenatal Vitamins: If your prenatal vitamins seem to trigger nausea, try taking them at night or with a snack.
- Bland is Best: Think the BRAT diet: Bananas, Rice, Applesauce, Toast. These are easy on the stomach and provide energy.
Do’s and Don'ts
Do’s & Don’ts :
Vomiting in Pregnancy Do’s & Don’ts
Do’s:
Stay hydrated
- Dehydration is a concern with frequent vomiting. Sip fluids throughout the day, even if you can only tolerate small amounts at a time. Water, clear broths, electrolyte drinks, and diluted fruit juices are good options.
Eat small, frequent meals:
- An empty stomach can worsen nausea. Aim for 5-6 small meals or snacks throughout the day instead of three large meals.
- Choose bland, easily digestible foods:
- Crackers, toast, rice, bananas, and applesauce are typically gentle on the stomach.
Rest:
- Fatigue can exacerbate nausea. Get plenty of rest and avoid overexertion.
Try ginger:
- Ginger has been shown to help alleviate nausea. You can consume it in various forms such as ginger tea, ginger ale, ginger candies, or ginger capsules (consult your doctor before taking any supplements).
Consult your doctor:
- If vomiting is severe, persistent, or accompanied by other symptoms like fever, abdominal pain, or weight loss, seek medical advice immediately.
Don’ts:
Not lie down immediately after eating:
- This can increase the likelihood of reflux and vomiting. Wait at least 30 minutes before lying down.
Don’t skip meals:
- An empty stomach can worsen nausea. Even if you don’t feel like eating, try to have something small and bland.
Don’t consume spicy, greasy, or fried foods:
- These can irritate the stomach and trigger nausea and vomiting.
Must Not expose yourself to strong odors:
- Certain smells can trigger nausea. Avoid cooking strong-smelling foods or using harsh cleaning products.
Don’t take any medications without consulting your doctor.
Terminology
Terminology:
Nausea and Vomiting of Pregnancy (NVP)
Meaning: The medical term encompassing the common experience of nausea and/or vomiting during pregnancy, often referred to as "morning sickness."
Significance: Affects a large majority of pregnant women, typically starting around the 6th week and subsiding by the second trimester.
Hyperemesis Gravidarum (HG)
Meaning: A severe form of NVP characterized by persistent and excessive vomiting, leading to dehydration, weight loss, and electrolyte imbalances.
Significance: Requires medical attention and may necessitate hospitalization to manage symptoms and complications.
Morning Sickness
Meaning: A colloquial term for NVP, although symptoms can occur at any time of the day or night.
Significance: While commonly used, it can be misleading as it doesn’t accurately reflect the potential severity or timing of symptoms.
Dehydration
Meaning: A condition resulting from excessive fluid loss, often caused by persistent vomiting.
Significance: Can lead to serious complications like electrolyte imbalances, kidney problems, and preterm labor.
Electrolyte Imbalances
Meaning: Disruptions in the normal levels of minerals like sodium, potassium, and chloride in the body, often caused by dehydration.
Significance: Can affect various bodily functions, including muscle contractions, nerve signaling, and heart rhythm.
Prenatal Vitamins
Meaning: Supplements containing essential vitamins and minerals to support the health of both mother and developing baby during pregnancy.
Significance: While crucial for a healthy pregnancy, iron in prenatal vitamins can sometimes worsen nausea and vomiting.
Food Aversions
Meaning: Strong dislikes or disgust towards certain foods or smells, commonly experienced during pregnancy.
Significance: Can make it challenging to maintain a balanced diet and obtain necessary nutrients.
Dry Heaves/Retching
Meaning: Involuntary spasms of the diaphragm and abdominal muscles without vomiting, often preceding or accompanying nausea.
Significance: Can be distressing and contribute to the overall discomfort of NVP.
General Homeopathic Terms:
Remedy: A substance used in homeopathy to treat a specific set of symptoms.
Potency: The strength or dilution of a homeopathic remedy.
Proving: A process in which healthy volunteers take a remedy and record their symptoms, helping to establish the remedy’s picture.
Similia Similibus Curentur: The foundational principle of homeopathy, translated as "like cures like." It means that a substance that can cause symptoms in a healthy person can be used to treat similar symptoms in a sick person.
Vital Force: The innate healing energy of the body.
Constitutional Remedy: A remedy that matches the overall physical and mental characteristics of an individual.
References
References:
- DC Dutta’s Textbook of Obstetrics Eight edition
- Homoeopathic Therapeutics by Lilienthal
- "Prevalence and Severity of Nausea and Vomiting in Pregnancy and its Impact on the Quality of Life in Pregnant Women"
- "Prevalence and Severity of Nausea and Vomiting During Pregnancy"
- Williams Obstetrics, 26th Edition
- Obstetrics by Ten Teachers, 20th Edition
- Cunningham, F. Gary, et al. Williams Obstetrics, 26th Edition. McGraw Hill Medical, 2021.
Also Search As
Also Search As:
Online:
Search engines: Use search engines like Google, DuckDuckGo, or Bing. Try specific search terms like:
"homeopathy for vomiting in pregnancy"
"homeopathic remedies for morning sickness"
"nausea and vomiting in pregnancy homeopathic treatment"
Homeopathic websites: Visit websites of reputable homeopathic organizations or practitioners. These sites often have articles or blogs on various health topics, including pregnancy-related issues.
Medical databases: Search medical databases like PubMed or Google Scholar for scientific articles on homeopathy and pregnancy.
Offline:
Libraries: Visit your local library and search their catalog or ask a librarian for help finding books or journals on homeopathy and pregnancy.
Homeopathic practitioners: Consult a qualified homeopathic practitioner. They can provide you with information and resources on homeopathic treatment options for vomiting in pregnancy.
Tips for Effective Searching:
Use specific keywords: Be as specific as possible in your search terms. Include words like "homeopathy," "pregnancy," "vomiting," "nausea," and "morning sickness."
Check the source: Make sure the information you find comes from a reliable source, such as a reputable homeopathic organization, a qualified practitioner, or a peer-reviewed medical journal.
Consider the date: Medical information can change over time. Look for articles that are relatively recent to ensure the information is up-to-date.
Consult a professional: If you have questions about homeopathic treatment for vomiting in pregnancy, talk to a qualified homeopathic practitioner. They can assess your individual needs and recommend the most appropriate treatment.
Specific search terms: Use precise keywords to target your search, such as:
"Morning sickness"
"Nausea and vomiting during pregnancy"
"Causes of vomiting in pregnancy"
"Treatment for vomiting in pregnancy"
Reliable sources: Focus your search on reputable websites and organizations, such as:
Medical websites: Mayo Clinic, WebMD, Cleveland Clinic, etc.
Government health organizations: Centers for Disease Control and Prevention (CDC), National Institutes of Health (NIH), etc.
Professional organizations: American College of Obstetricians and Gynecologists (ACOG)
Question format: Phrase your search as a question to get more targeted results, for example:
"When should I see a doctor for vomiting in pregnancy?"
"What are the safe medications for morning sickness?"
"Can vomiting in pregnancy harm my baby?"
Image search: Use image search to find visual aids and infographics that explain the causes, symptoms, and treatment options for vomiting in pregnancy.
Frequently Asked Questions (FAQ)
What is Vomiting in Pregnancy?
It Is define as the complaints of patient about nausea and occasional sickness on rising in the morning, commonly occurs during the first trimester of pregnancy.
What causes Vomiting in Pregnancy?
- Mostly limited to the first trimester
- More common in first pregnancy
- Younger age
- Low body mass
- History of motion sickness or migraine
- Familial history
Give the types of Vomiting in Pregnancy?
- Simple vomiting of either pregnancy or milder type
- Hyperemesis gravidarum or severe type
How can I manage morning sickness at home?
Some tips to manage morning sickness include eating small, frequent meals, avoiding trigger foods, staying hydrated, and getting plenty of rest.
What are the symptoms of Vomiting in Pregnancy?
- Vomiting increased in frequency with retching
- Urine quantity diminish even to the stage of oliguria
- Epigastric pain, constipation may occur
- Complications may appear if not treated
Are homeopathic remedies safe during pregnancy?
- Homeopathic remedies are generally considered safe during pregnancy when prescribed and administered by a qualified homeopathic practitioner. They are highly diluted and do not typically interact with conventional medications.
When does morning sickness usually start and end?
Morning sickness typically starts around the 6th week of pregnancy and peaks between weeks 8-12. For most women, it subsides by the second trimester, around week 14.
How long does it take for homeopathic remedies to work?
- The response to homeopathic remedies can vary depending on the individual and the severity of symptoms. Some women may experience relief within a few hours or days, while others may require a longer duration of treatment.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Vomiting in Pregnancy?
Homeopathic Medicines
- Acitic Acid
- Arsenicum Album
- Colchicum
- Conium
- Cyclamen
- Ferrum Phos
- Gossypium
- Ignatia
- Ipecacuanha
- Lobelia Inflata
