Autonomic Neuropathy
Definition
Autonomic neuropathy occurs when the nerves that control involuntary bodily functions are damaged. [1]
- Dysautonomia: This is a broader term that encompasses various conditions affecting the autonomic nervous system, including autonomic neuropathy.
- Autonomic dysfunction: This term emphasizes the functional impairment of the autonomic nervous system.
- Neurogenic [condition]: This refers to a condition caused by nerve damage, and you could specify the affected system (e.g., neurogenic bladder). However, this wouldn’t be specific to autonomic neuropathy.
Additionally, depending on the specific symptoms, you could use terms related to the affected functions:
- Cardiovascular dysautonomia: This focuses on autonomic dysfunction affecting the heart and blood vessels.
- Gastroparesis: This refers to a specific type of autonomic neuropathy affecting the stomach muscles.
- Neurogenic bowel dysfunction: This describes impaired bowel function due to autonomic nerve damage.
Remember, for clear medical communication, "autonomic neuropathy" is the most precise term.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do's & Don'ts
Terminology
References
Also Search As
Overview
Overview
Autonomic neuropathy is a group of conditions caused by damage to your nerves.
Those nerves are part of your autonomic nervous system. They control many different body functions, i.e.:
- Body temperature
- Blood pressure
- Heart rate
- Digestion
- Urination
- Bowel movements
Damage to those nerves affects the signals between your brain and your organs. [2]
Epidemiology
Epidemiology
The epidemiology of Autonomic Neuropathy (AN) in India varies significantly depending on the underlying cause and the specific population studied. However, several studies have shed light on its prevalence and associated factors:
Diabetic Autonomic Neuropathy (DAN):
- A study published in the Indian Journal of Clinical Practice (2011) found the prevalence of DAN in diabetes mellitus patients visiting a tertiary care center to be 38.5%.[9]
- Another study in the International Journal of Applied and Basic Medical Research (2013) reported a prevalence of 80.39% for cardiac autonomic neuropathy (CAN) in type 2 diabetes mellitus patients[10].
- These studies highlight that DAN is a common complication of diabetes in India.
Fibrocalculous Pancreatic Diabetes (FCPD):
- Research published in the CMC Vellore Department of Endocrinology found a 63.3% prevalence of CAN in patients with FCPD, suggesting a higher risk of autonomic dysfunction in this specific type of diabetes.[10]
Other Causes:
- The epidemiology of AN due to other causes, such as autoimmune diseases, infections, or toxins, is less well-defined in the Indian context. Further research is needed to determine the prevalence and risk factors associated with these forms of AN.
Important Considerations:
- The studies mentioned above represent specific populations and may not be generalizable to the entire Indian population.
- The prevalence of AN likely varies across different regions and socioeconomic groups within India.
- The diagnosis of AN can be challenging, and the availability of specialized testing may be limited in some areas, affecting prevalence estimates.
Recommendations:
- Increased awareness among healthcare professionals about AN and its diverse causes is crucial for early diagnosis and appropriate management.
- Further epidemiological studies with larger, more representative samples are needed to accurately assess the burden of AN in India and identify specific risk factors.
- Improved access to diagnostic tools and specialized care for AN is essential to address this underrecognized condition.
Causes
Causes
Many health conditions can cause autonomic neuropathy. It can also be a side effect of treatments for other diseases, such as cancer. [1]
Some common causes of autonomic neuropathy i.e.:
- Diabetes
- Abnormal protein buildup, called amyloidosis
- Autoimmune diseases e.g. rheumatoid arthritis, Guillain-Barré syndrome, lupus, and Sjogren’s syndrome
- Lyme disease
- HIV
- Parkinson’s disease
- Inherited diseases such as Riley-Day syndrome
- Spinal cord injury
- Surgery
- Medicines, including some chemotherapy drugs used to treat cancer
- Chemicals, like acrylamide, also heavy metals. [2]
Types
Autonomic Neuropathy Types
There are several types of autonomic neuropathy, each affecting different parts of the autonomic nervous system. They include:
- Focal Autonomic Neuropathies: These affect a single nerve or a specific area of the body. Examples include Adie’s tonic pupil, Horner’s syndrome, and diabetic mononeuropathies.
- Generalized Autonomic Neuropathies: These involve widespread damage to the autonomic nerves. This is often seen in conditions like diabetes, Parkinson’s disease, and autoimmune disorders.
These types can be further classified based on the specific symptoms they cause. For instance, cardiovascular autonomic neuropathy affects the heart and blood vessels, leading to issues with blood pressure and heart rate regulation. Similarly, gastrointestinal autonomic neuropathy affects the digestive system, causing problems like delayed gastric emptying and constipation.[8]
This comprehensive book provides a detailed overview of autonomic nervous system diseases, including various types of autonomic neuropathy. It discusses their causes, diagnosis, and management options, making it a valuable resource for healthcare professionals and researchers.
Risk Factors
Risk Factors
- Alcohol misuse.
- Vitamin deficiencies, particularly B vitamins.
- Infections, such as Lyme disease, shingles, Epstein-Barr virus, hepatitis B and C, and HIV.
- Autoimmune diseases, such as rheumatoid arthritis and lupus, in which your immune system attacks your own tissues.[3]
Pathogenesis
Autonomic Neuropathy Pathogenesis
The pathogenesis of autonomic neuropathy is complex and varies depending on the underlying cause. However, some common mechanisms have been identified:
Metabolic Dysfunction: In conditions like diabetes, elevated blood glucose levels can lead to the formation of advanced glycation end products (AGEs). These AGEs can damage nerve fibers and impair their function. Additionally, diabetes can also disrupt blood flow to the nerves, leading to ischemia and further damage.
Inflammatory Processes: Autoimmune diseases and certain infections can trigger inflammation that targets the autonomic nerves. This inflammation can damage the nerve fibers directly or indirectly through the release of cytokines and other inflammatory mediators.
Neurotoxic Agents: Exposure to certain toxins, such as heavy metals or specific medications, can damage the autonomic nerves. These toxins can interfere with nerve conduction or disrupt cellular processes essential for nerve survival.
Genetic Predisposition: Some individuals may have a genetic predisposition to developing autonomic neuropathy. These genetic factors can affect the structure or function of the nerves, making them more vulnerable to damage.
This comprehensive textbook Peripheral Neuropathy provides a detailed discussion of the pathogenesis of various peripheral neuropathies, including autonomic neuropathy. It explores the underlying mechanisms, risk factors, and potential therapeutic targets, making it a valuable resource for healthcare professionals and researchers.[12]
Pathophysiology
Pathophysiology
Elements of the autonomic examination include variations in the pulse, postural measurements of blood pressure and heart rate, pupillary light reactions, skin coloration and temperature, patterns of sweating, and other organ-specific physical findings relevant to the individual patient’s presentation.
Especially important is the often neglected practice of measuring the blood pressure standing up, for orthostatic hypotension cannot be diagnosed by symptoms alone and is a common source of potential morbidity.
The examination should be carried out in the context of understanding the syndromic nature of abnormalities of components of the autonomic nervous system.[5]
Clinical Features
Autonomic Neuropathy: Clinical Features
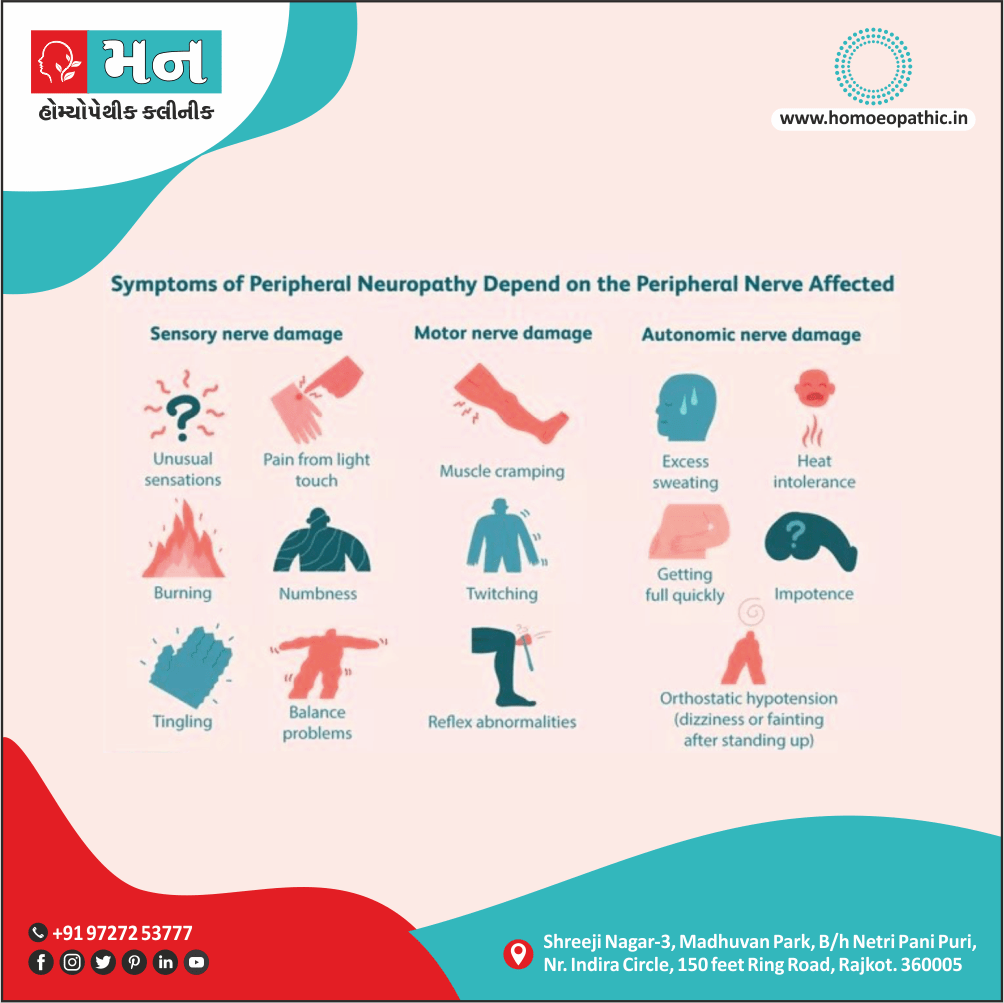
The clinical features of autonomic neuropathy are diverse and depend on the specific nerves affected. Common symptoms include:
- Cardiovascular: Orthostatic hypotension (drop in blood pressure upon standing), dizziness, lightheadedness, palpitations, and exercise intolerance.
- Gastrointestinal: Gastroparesis (delayed gastric emptying), nausea, vomiting, constipation, diarrhea, and difficulty swallowing.
- Genitourinary: Erectile dysfunction, ejaculatory problems, urinary incontinence or retention, and decreased vaginal lubrication.
- Sudomotor: Anhidrosis (lack of sweating) or hyperhidrosis (excessive sweating), often localized to specific body regions.
- Pupillary: Impaired pupillary reflexes, leading to difficulty adjusting to changes in light and impaired night vision.
- Metabolic: Hypoglycemia unawareness, where the body fails to produce the usual warning signs of low blood sugar.
This comprehensive textbook Principles of Neurology covers the full spectrum of neurological disorders, including autonomic neuropathy. The chapter on autonomic disorders provides a detailed description of the clinical features, diagnosis, and management of autonomic neuropathy, making it an essential resource for medical professionals and students.[13]
Sign & Symptoms
SIgn & Symptoms
It depend on the nerves affected.
They might include:
Dizziness and fainting:
When standing, caused by a sudden drop in blood pressure (orthostatic hypertension).
Urinary problems:
Such as difficulty starting urination, incontinence, difficulty sensing a full bladder and inability to completely empty the bladder, which can lead to urinary tract infections.
Sexual difficulties:
This including problems achieving or maintaining an erection (in other words, erectile dysfunction) or ejaculation problems in men. Specifically, In women, problems include vaginal dryness, low libido and difficulty reaching orgasm.
Difficulty digesting food:
Such as feeling full after a few bites of food, loss of appetite, diarrhea, constipation, abdominal bloating, nausea, vomiting, difficulty swallowing and heartburn, above all due to changes in digestive function.
Inability to recognize:
Low blood sugar (hypoglycemia), because of the warning signals, such as getting shaky, aren’t there.
Sweating abnormalities:
Such as sweating too much or too little, which affect the ability to regulate body temperature.
Sluggish pupil reaction:
Making it difficult to adjust especially from light to dark and seeing well when driving at night.
Exercise intolerance:
Which can occur if your heart rate stays the same instead of adjusting to your activity level. [1]
Clinical Examination
Autonomic Neuropathy Clinical Examination
The clinical examination for autonomic neuropathy involves a comprehensive assessment of various body systems potentially affected by the disorder. It typically includes:
Cardiovascular Assessment:
- Orthostatic Hypotension: Measure blood pressure and heart rate while the patient is lying down, sitting, and standing. A significant drop in blood pressure upon standing is indicative of orthostatic hypotension.
- Heart Rate Variability: Assess heart rate response to deep breathing and Valsalva maneuver. Reduced variability suggests autonomic dysfunction.
Gastrointestinal Assessment:
- Gastric Emptying: Assess symptoms like early satiety, bloating, and nausea, which may suggest gastroparesis.
- Bowel Function: Inquire about bowel habits, constipation, and diarrhea.
Genitourinary Assessment:
- Erectile Dysfunction: Inquire about erectile function in men.
- Bladder Function: Assess for urinary incontinence or retention.
Sudomotor Assessment:
- Sweat Test: Quantitative sudomotor axon reflex test (QSART) or thermoregulatory sweat test (TST) can be used to assess sweat production.
Pupillary Assessment:
- Pupil Size and Reactivity: Check pupil size and response to light and accommodation.
This comprehensive textbook Autonomic Failure: A Textbook of Clinical Disorders of the Autonomic Nervous System provides a detailed guide to the clinical assessment of autonomic disorders, including autonomic neuropathy. It describes various tests and procedures used to evaluate autonomic function and interpret the findings, making it an essential resource for clinicians involved in the diagnosis and management of autonomic disorders.[14]
Diagnosis
Diagnosis
Breathing tests i.e.:
- These tests measure how your heart rate and blood pressure respond during exercises such as forcefully exhaling (in other words, Valsalva maneuver).
Tilt-table test i.e.:
- Generally, This test monitors the response of blood pressure and heart rate to changes in posture and position, simulating what occurs when you stand up after lying down.
- You lie flat on a table, which is then tilted to raise the upper part of your body. Additionally, normally your body narrows blood vessels and increases heart rate to compensate for the drop in blood pressure.
- This response either may be slowed or abnormal if you have autonomic neuropathy.
- A simpler test for this response involves standing for a minute, then squatting for a minute and then standing again while blood pressure and heart rate are monitored.
Gastrointestinal tests i.e.:
- In brief, Gastric-emptying tests are the most common tests to check for digestive abnormalities such as slow digestion and delayed emptying of the stomach (gastroparesis).
Quantitative pseudomotor axon reflex test i.e.:
- This test evaluates how the nerves that regulate your sweat glands respond to stimulation.
- A small electrical current passes through capsules placed on your forearm, upper and lower leg and foot, while a computer analyzes the response of your nerves also sweat glands.
- You might feel warmth or a tingling sensation during the test.
Thermoregulatory sweat test i.e.:
- You’re coated with a powder that changes color when you sweat.
- While lying in a chamber with a slowly increasing temperature, digital photos document the results as you begin to sweat.
- Your sweat pattern might help confirm a diagnosis of autonomic neuropathy or suggest other causes for decreased or increased sweating.
Urinalysis and bladder function (urodynamic) tests i.e.:
- If you have bladder or urinary signs and symptoms, a series of urine and bladder tests can evaluate bladder function.
Ultrasound i.e.:
- If you have bladder signs and symptoms, your doctor might do an ultrasound in which high-frequency sound waves create an image of the bladder and other parts of the urinary tract. [1]
Differential Diagnosis
Differential Diagnosis
- Botulism
- Porphyria
- Amyloidosis, and
- Para carcinomatous neuropathies.
Complications
Autonomic Neuropathy Complications
Autonomic neuropathy can lead to various complications due to the dysfunction of the autonomic nervous system. These complications can affect multiple organ systems and significantly impact the patient’s quality of life. Some common complications include:
Cardiovascular Complications:
- Orthostatic Hypotension: This can cause dizziness, lightheadedness, falls, and syncope (fainting).
- Cardiac Arrhythmias: Irregular heart rhythms can lead to palpitations, chest pain, and even sudden cardiac death.
- Silent Myocardial Ischemia: This is a dangerous condition where the heart doesn’t receive enough blood flow, but the patient experiences no symptoms.
Gastrointestinal Complications:
- Gastroparesis: This can lead to chronic nausea, vomiting, abdominal pain, early satiety, and malnutrition.
- Constipation or Diarrhea: Disruption of bowel function can cause significant discomfort and affect nutrient absorption.
- Fecal Incontinence: This can be embarrassing and socially isolating.
Genitourinary Complications:
- Erectile Dysfunction: This can significantly affect sexual function and quality of life for men.
- Neurogenic Bladder: This can lead to urinary incontinence, retention, and recurrent urinary tract infections.
Thermoregulatory Complications:
- Hypothermia or Hyperthermia: Impaired sweating can make it difficult to regulate body temperature, increasing the risk of heatstroke or hypothermia.
Metabolic Complications:
- Hypoglycemia Unawareness: This can lead to severe low blood sugar episodes without warning symptoms, increasing the risk of seizures, coma, and even death.
This comprehensive bookTreatment of Autonomic Disorders provides a detailed overview of autonomic disorders, including the complications associated with autonomic neuropathy. It discusses the pathophysiology, clinical manifestations, and management strategies for various autonomic complications, making it a valuable resource for healthcare professionals involved in the care of patients with autonomic dysfunction.[15]
Investigations
Investigations
- Breathing tests
- Tilt-table test
- Gastrointestinal tests
- Quantitative pseudomotor axon reflex test
- Thermoregulatory sweat test
- Urinalysis and bladder function (urodynamic) tests
- Ultrasound[1]
Treatment
Treatment
Your doctor mainly will treat the disease that caused your nerve damage.
For example, if you have diabetes, you’ll need to control your blood sugar with diet, exercise, and possibly medicine.
For autoimmune diseases, like Sjogren’s syndrome, you’ll get medicine to control your immune system and bring down inflammation in your body.
digestive symptoms i.e.:
- Change your diet.
- Eat smaller meals so you don’t feel too full.
- Add fluid and fiber to your diet to prevent bloating and constipation.
- Laxatives can help with constipation, and other medicines can treat diarrhea and belly pain.
- Sleep with the head of your bed raised to prevent heartburn.
urinary symptoms i.e.:
- Drink fluids and empty your bladder at set times during the day. This can help your bladder hold more fluid.
- Oxybutynin (Ditropan XL) and tolterodine (Detrol) stop your bladder muscle from squeezing too often.
- Bethanechol helps you empty your bladder all the way.
- Use a catheter. This tube goes into your bladder to help empty it.
To treat sweating problems i.e.:
- A few drugs can help you make less sweat, including glycopyrrolate (Robinul, Robinul Forte) and botulinum toxin.
- If you don’t sweat enough, stay inside when it’s hot outdoors.
To treat heart and blood pressure symptoms i.e.:
- Take a medicine that raises your blood pressure, such as fludrocortisone or midodrine and pyridostigmine (Mestinon).
- Take medicine to control your heart rate.
- Beta-blockers can help bring your heart back into a normal rhythm.
- Stand up slowly so you don’t get dizzy.
- Get extra salt and fluid in your diet to help raise your blood pressure.
- Only do this if your doctor recommends it. In some cases, it can raise your blood pressure too high or cause swelling.
sexual symptoms i.e.:
- Drugs like sildenafil (e.g. Revatio, Viagra), tadalafil (e.g. Cialis), and vardenafil (e.g. Levitra, Staxyn) can help men get and keep an erection.
- Women can try a water-based lubricant to make sex more comfortable. [2]
Prevention
Prevention
While certain inherited diseases that put you at risk of developing autonomic neuropathy can’t be prevented, you can slow the onset or progression of symptoms by taking care of your health in general and managing your medical conditions.
Follow your doctor’s advice on healthy living to control diseases and conditions, which might include these recommendations e.g.:
- Control your blood sugar if you have diabetes.
- Avoid alcohol and smoking.
- Get appropriate treatment if you have an autoimmune disease.
- Take steps to prevent or control high blood pressure.
- Achieve and maintain a healthy weight.
- Exercise regularly. [1]
Homeopathic Treatment
Homeopathic Treatment of Autonomic Neuropathy
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines of Autonomic Neuropathy:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Causticum:
- It is useful when involuntary urination is worse in the winter and better in the summer.
- Various fears and apprehensions accompany the urination, especially fears that something bad will happen to them.
- They have a fear of going to bed in the dark.
- These people also tend to wet their pants when they cough or sneeze or even laugh.
Equisetum:
- This is for people who wet their pants or their bed for no known reason other than out of habit.
- It should be considered when the person has no other obvious symptoms.
- It should also be given when the person experiences wild dreams or nightmares when bedwetting.
- Besides this, they tend to dream of crowds of people.
Gelsemium:
- This medicine especially indicated in Autonomic Neuropathy.
- Centers its action on nervous system, causing various degrees of motor paralysis.
- Dizziness, drowsiness, dullness and trembling are the hallmark of this remedy.
- Trembling ranks the highest in this remedy, weakness and paralysis, especially of the muscles of the head.
- Paralysis of various groups of muscles like eyes, throat, chest, sphincters and extremities.
- Head remedy for tremors.
- Mind sluggish and muscular system relaxed.
- Staggering gait.
- Loss of power of muscular control.
- Cramps in muscles of forearm.
- Excessive trembling and weakness of all limbs.
- Worse by dampness, excitement, bad news. On the other hand, Better by bending forwards, profuse urination, continued motion and open air.
Agnus Castus:
- Homeopathic medicine Agnus Castus is used in cases where there is complete inability to attain penile erection during the sexual act.
- Homeopathic medicine Agnus Castus can be used in cases of erectile dysfunction and sexual weakness where the male has a mental aversion to indulge in sex, along with decreased physical strength.
Caladium:
- Good medicine for Autonomic Neuropathy.
- Homeopathic medicine Caladium is of great help for treatment of erectile dysfunction when the male is unable to have an erection despite having a sexual desire or urge.
Acid Phos & Selenium:
- Acid Phos and Selenium can both help the males with Erectile Dysfunction when the erections last only for a short time with early or premature emissions.
- Both these medicines can be used if men attempting the sexual act experience relaxation of the sex organs.
- However, if there is involuntary semen discharge during sleep or while passing stool or during short erections, then Selenium can be of great help.
- Males requiring Selenium also suffer from lack of complete gratification from sex due to early emissions.
Diet & Regimen
Diet and Regimen
- Control Your Blood Sugar to Avoid Diabetic Neuropathy
- Get Enough Vitamin B12 and Other Nutrients
- Watch Your Intake of Vitamin B6
- Avoid Mercury and Other Toxins in Your Food That Are Linked to Neuropathy
- Limit or Avoid Alcohol to Help Prevent or Stop the Progress of Neuropathy
- Understand Your Relationship to Gluten if Celiac Disease Caused Your Nerve Damage[7]
Do's & Don'ts
The Do’s & Don’ts
Do’s:
- Do manage underlying conditions: If autonomic neuropathy is caused by a condition like diabetes or an autoimmune disorder, proper management of that condition is crucial. This may involve medication, lifestyle changes, and regular checkups with your doctor.
- Do monitor blood pressure regularly: Orthostatic hypotension is a common complication of autonomic neuropathy. Regularly monitoring your blood pressure, especially upon standing, can help identify drops and guide treatment.
- Do adjust your diet: Eating smaller, more frequent meals can help with gastroparesis. Increasing fiber and fluid intake can help with constipation.
- Do stay hydrated: Dehydration can worsen orthostatic hypotension. Aim to drink plenty of fluids throughout the day.
- Do exercise regularly: Exercise can improve cardiovascular health and help regulate blood pressure. Choose low-impact activities and consult your doctor before starting a new exercise program.
- Do maintain a healthy weight: Obesity can worsen autonomic neuropathy symptoms. Talk to your doctor about a weight loss plan if needed.
- Do seek medical attention for any new or worsening symptoms: Promptly reporting any changes can help identify potential complications early and prevent further damage.
Don’ts:
- Don’t ignore symptoms: Early detection and treatment are crucial for managing autonomic neuropathy and preventing complications.
- Don’t skip meals or eat large meals: This can worsen gastroparesis symptoms.
- Don’t drink excessive alcohol or caffeine: These substances can dehydrate you and worsen orthostatic hypotension.
- Don’t stand up quickly: Rise slowly from a lying or sitting position to prevent dizziness and falls.
- Don’t use over-the-counter medications without consulting your doctor: Some medications can interact with treatments for autonomic neuropathy or worsen symptoms.
- Don’t hesitate to seek support: Living with autonomic neuropathy can be challenging. Talking to a therapist or joining a support group can help you cope with the emotional and physical impact of the condition.
This comprehensive textbook Autonomic Neurology: Basic and Clinical Principles provides a detailed overview of autonomic neurology, including the diagnosis, management, and prognosis of autonomic neuropathy. It offers practical advice on lifestyle modifications and coping strategies for patients living with this condition, making it a valuable resource for healthcare professionals and patients alike.[16]
Terminology
Terminology
- Autonomic Neuropathy: A condition where nerves of the autonomic nervous system (responsible for involuntary bodily functions) are damaged.
- Dysautonomia: A broader term encompassing various disorders affecting the autonomic nervous system, including autonomic neuropathy.
- Autonomic Dysfunction: Emphasizes the functional impairment of the autonomic nervous system.
- Cardiovascular Autonomic Neuropathy: Autonomic neuropathy specifically affecting the heart and blood vessels.
- Gastroparesis: A type of autonomic neuropathy causing delayed stomach emptying.
- Neurogenic Bowel Dysfunction: Impaired bowel function due to autonomic nerve damage.
- Diabetic Autonomic Neuropathy (DAN): Autonomic neuropathy caused by diabetes.
- Cardiac Autonomic Neuropathy (CAN): DAN affecting the heart’s autonomic nerves.
- Fibrocalculous Pancreatic Diabetes (FCPD): A specific type of diabetes with a higher risk of autonomic neuropathy.
- Orthostatic Hypotension: A sudden drop in blood pressure upon standing, a common symptom of autonomic neuropathy.
- Hypoglycemia Unawareness: Impaired ability to recognize low blood sugar levels due to autonomic neuropathy.
- Miasmatic Tendency: A homeopathic concept referring to an individual’s predisposition to certain disease patterns.
This list provides definitions for key terms used in the article, helping readers better understand the complex topic of autonomic neuropathy and its various aspects.
References
Reference
- https://www.mayoclinic.org/diseasesconditions/autonomicneuropathy/symptoms-causes/syc-20369829
- https://www.webmd.com/diabetes/autonomic-neuropathy-overview#1
- https://www.mayoclinic.org/disease-conditions/peripheralneuropathy/symptoms-causes/syc-20352061
- https://www.healthline.com/health/autonomic-dysfunction#treatments
- https://pubmed.ncbi.nlm.nih.gov/29294184
- https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/614171
- https://www.everydayhealth.com/neuropathy/diet-understanding-connection/
- Autonomic Nervous System Diseases: Advances in Research and Treatment ,Editors: Christopher J. Mathias and Phillip A. Low (2014), Publisher: Springer Science & Business Media ,Edition: 1st Edition.
- Indian Journal of Clinical Practice (2011).
- International Journal of Applied and Basic Medical Research (2013).
- CMC Vellore Department of Endocrinology.
- Peripheral Neuropathy ,Editors: John W. Griffin, Anthony A. F. Sima, Jerry R. Mendell, and Robert E. Lovelace ,(2019), Publisher: Elsevier ,Edition: 6th Edition.
- Principles of Neurology, Author: Allan H. Ropper and Martin A. Samuels,(2019) Publisher: McGraw-Hill Education,Edition: 11th Edition.
- Autonomic Failure: A Textbook of Clinical Disorders of the Autonomic Nervous System, Author: Christopher J. Mathias, David J. Goldstein, Lucy Norcliffe-Kaufmann, and Roland D. Thijs,(2010) ,Publisher: Oxford University Press,Edition: 5th Edition.
- Treatment of Autonomic Disorders, Editors: Phillip A. Low and Christopher J. Mathias, (2010) ,Publisher: Springer Science & Business Media, Edition: 1st Edition
- Autonomic Neurology: Basic and Clinical Principles, Editors: Phillip A. Low and Aaron I. Vinik,(2018), Publisher: Elsevier, Edition: 2nd Edition
Also Search As
Also Search As
People can search for the article on Autonomic Neuropathy using a variety of methods:
Search Engines:
- Use keywords related to the topic and homeopathy, such as:
- "homeopathic treatment for autonomic neuropathy"
- "homeopathic remedies for autonomic neuropathy"
- "autonomic neuropathy natural treatment"
- Include the specific homeopathic remedies mentioned in the article if known, like:
- "Aconitum Napellus for autonomic neuropathy"
- "Arsenicum Album for autonomic neuropathy"
Homeopathic Websites and Forums:
- Search within homeopathic websites or forums that discuss health conditions.
- Look for specific sections or categories related to neuropathy or neurological disorders.
Social Media:
- Follow homeopathic practitioners or organizations on social media platforms.
- Look for relevant hashtags like #homeopathy, #autonomicneuropathy, #naturalhealth.
Additional Tips:
- Specify the type of autonomic neuropathy if relevant (e.g., diabetic autonomic neuropathy).
- Use synonyms or related terms (e.g., "dysautonomia" or "nerve damage").
- Check the author’s name or the website where the article was originally published for more targeted searches.
By utilizing these search strategies, individuals interested in learning about the homeopathic approach to autonomic neuropathy can easily find relevant information and resources.
There are several ways to search for an article on autonomic neuropathy, depending on the specific information you are looking for and the resources available to you:
Online Search Engines:
- Use search engines like Google, Bing, or DuckDuckGo.
- Enter relevant keywords, such as "autonomic neuropathy," "symptoms," "treatment," or "homeopathy."
- Refine your search using filters like "news articles," "scholarly articles," or "blogs."
Academic Databases:
- If you need scholarly or research-based articles, use academic databases like PubMed, Google Scholar, or ScienceDirect.
- Search using specific medical terms (e.g., "dysautonomia," "peripheral neuropathy") for more precise results.
Homeopathic Resources:
- Explore websites or blogs dedicated to homeopathy.
- Look for articles or case studies on autonomic neuropathy or related conditions.
- Consult homeopathic journals or publications for in-depth information.
Social Media:
- Search for relevant hashtags on platforms like Twitter or Facebook (e.g., #autonomicneuropathy, #homeopathy).
- Follow homeopathic practitioners or organizations for updates and discussions.
Libraries:
- Visit your local library or university library.
- Consult librarians for assistance in finding relevant books or journals.
Remember to use specific keywords and phrases to narrow down your search and find the most relevant articles. Additionally, consider the credibility and source of the information you find, especially when it comes to health-related topics.
Frequently Asked Questions (FAQ)
What is Autonomic Neuropathy?
Autonomic neuropathy occurs when the nerves that control involuntary bodily functions are damaged.
What are the causes of Autonomic Neuropathy?
- Diabetes
- Amyloidosis
- Autoimmune diseases
- HIV
- Parkinson’s disease
- Inherited diseases
- Spinal cord injury
- Surgery
- Chemotherapy drugs
- Chemicals (acrylamide)
How does homeopathic treatment work for autonomic neuropathy?
Homeopathic remedies aim to stimulate the body’s self-healing mechanisms and restore balance to the autonomic nervous system.
What are the symptoms of Autonomic Neuropathy?
- Dizziness and fainting
- Urinary problems
- Sexual difficulties
- Difficulty digesting food
- Inability to recognize
- Sweating too much or too little
- Sluggish pupil reaction
Homeopathic Medicines used by Homeopathic Doctors in treatment of Autonomic Neuropathy?
Homoeopathic Medicines for Autonomic Neuropathy
- Causticum
- Equisetum
- Gelsemium
- Agnus Castus
- Caladium
- Acid Phos
- Selenium
