Organic Amnestic Syndrome
Definition
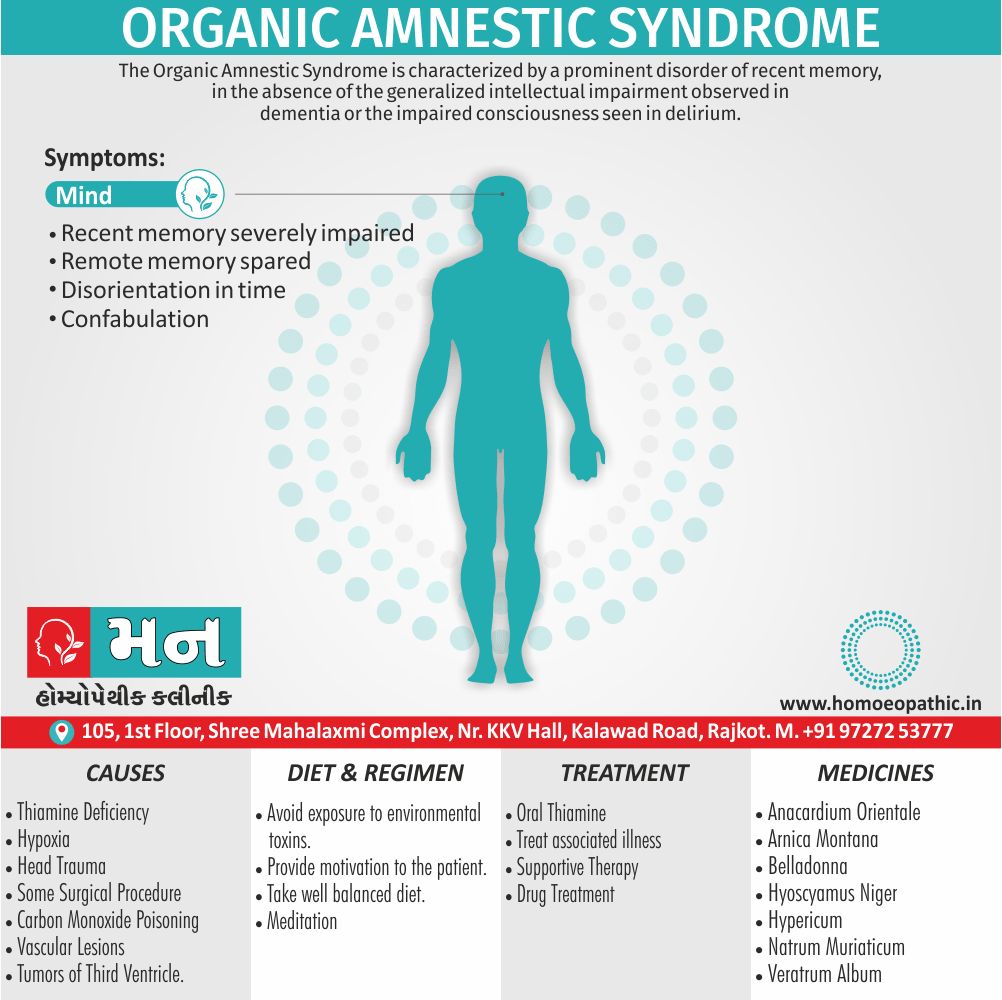
The Organic Amnestic Syndrome is characterize by a prominent disorder of recent memory, in the absence of the generalized intellectual impairment observed in dementia or the impaired consciousness seen in delirium. [1]
There aren’t true synonyms for Organic Amnestic Syndrome, as it’s a specific diagnosis. However, there are some related terms you can use depending on the context:
- Amnestic disorder due to a known medical condition: This is the official diagnostic term used in the ICD-10 coding system, which is another way to describe Organic Amnestic Syndrome. ICD-10 coding system [invalid URL removed]
- Memory disorder caused by a physical illness: This is a more general way to describe the condition for someone unfamiliar with medical terminology.
- Specific diagnosis causing amnesia: If you know the specific cause of the amnesia, you can use that term. For example, "Korsakoff syndrome" is a type of organic amnestic syndrome caused by thiamine deficiency.
Here’s a quick breakdown:
- For medical professionals: Amnestic disorder due to a known medical condition
- For general audience: Memory disorder caused by a physical illness (or specific diagnosis if known)
Remember, it’s always best to use the most precise term possible when discussing medical conditions.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
The condition usually results from lesions in the posterior hypothalamus and nearby mid line structures, but occasionally results from bilateral hippocampal lesions.
It is often describe as Korsakov’s syndrome, after the Russian neurologist who first described the clinical features, or as the Wernicke–Korsakov syndrome.
Lastly; The prominent causal factor in most cases appears to thiamine deficiency. [1]
Epidemiology
Epidemiology
General Prevalence: Organic amnestic disorder is relatively rare compared to other mental health conditions. Global estimates suggest a prevalence of around 0.1% to 1% of the general population.
Indian Context: The prevalence of specific neurological and psychiatric conditions in India may differ from global averages due to various factors like genetics, lifestyle, and environmental exposures. Studies focusing on dementia and Alzheimer’s disease in India can offer some insights into the potential burden of organic amnestic disorder, as memory impairment is a significant feature of these conditions.
Potential Resources:
- Research publications from Indian neurological and psychiatric journals.
- Reports and data from the National Mental Health Survey of India.
- Studies conducted by the Indian Council of Medical Research (ICMR) on neurological disorders.
Causes
Causes of Organic Amnestic Syndrome
1. Thiamine deficiency:
In brief; Alcohol abuse is the most frequent cause, and seems to act by causing a deficiency of thiamine.
2. Any other lesion involving bilaterally the inner core of limbic system:
That is mammillary bodies, fornix, hippocampus and parahippocampal structures of medial temporal lobe, posterior hypothalamus and dorsomedial thalamic nuclei.
For example:
- Head trauma,
- Surgical procedure (e.g. bilateral temporal lobectomy),
- Hypoxia,
- Posterior cerebral artery stroke (especially bilateral),
- Herpes simplex encephalitis, and
- Space occupying lesions in the region of III ventricle (e.g. neoplasms) [2]
- Carbon monoxide poisoning,
- Vascular lesions,
- Tumours of the third ventricle. [1]
Types
Types of Organic Amnestic Disorder:
Wernicke-Korsakoff Syndrome: Caused primarily by thiamine (vitamin B1) deficiency, often associated with chronic alcohol abuse. It leads to severe anterograde and retrograde amnesia, confabulation, and other cognitive impairments.
Amnestic Disorder Due to Head Trauma: Memory impairment caused by traumatic brain injury, varying in severity depending on the extent of the damage.
Amnestic Disorder Due to Cerebrovascular Disease: Memory problems resulting from strokes or other disruptions of blood flow to the brain.
Amnestic Disorder Due to Other Medical Conditions: This category encompasses various conditions causing memory impairment, such as infections (e.g., herpes simplex encephalitis), hypoxia, tumors, and neurodegenerative diseases. [3]
Risk Factors
Risk Factors
Several factors increase the risk of developing organic amnestic disorder, primarily by affecting brain health and function. These include:
Chronic Alcohol Abuse: Excessive and prolonged alcohol consumption can lead to thiamine (vitamin B1) deficiency, a significant cause of Wernicke-Korsakoff syndrome, a type of organic amnestic disorder.
Head Trauma: Traumatic brain injuries, such as concussions or severe head injuries, can disrupt memory function and increase the risk of amnestic disorder.
Cerebrovascular Disease: Conditions affecting blood flow to the brain, like strokes or transient ischemic attacks, can damage brain regions crucial for memory and lead to amnestic disorder.
Neurodegenerative Diseases: Conditions like Alzheimer’s disease, Parkinson’s disease, and frontotemporal dementia gradually impair cognitive function, including memory, and can progress to amnestic disorder.
Infections: Certain infections, particularly those causing encephalitis (brain inflammation), such as herpes simplex encephalitis, can damage memory centers and lead to amnestic disorder.
Other Medical Conditions: Other conditions like hypoxia (oxygen deprivation), brain tumors, epilepsy, certain medications, and exposure to toxins can also contribute to the risk of amnestic disorder. [3]
Pathogenesis
Pathogenesis
The pathogenesis of organic amnestic disorder involves damage to brain structures crucial for memory formation, storage, and retrieval. The specific mechanisms can vary depending on the underlying cause, but often involve:
Damage to Medial Temporal Lobe Structures: The hippocampus, entorhinal cortex, and parahippocampal gyrus are key components of the medial temporal lobe memory system. Lesions in these areas, caused by conditions like head trauma, stroke, or neurodegenerative diseases, disrupt the encoding and consolidation of new memories, leading to anterograde amnesia.
Disruption of Diencephalic Structures: The thalamus and mammillary bodies play a vital role in memory processing and retrieval. Damage to these structures, often seen in Wernicke-Korsakoff syndrome and other conditions affecting the diencephalon, can result in both anterograde and retrograde amnesia.
Neurotransmitter Imbalance: Neurotransmitter systems, particularly those involving acetylcholine, play a crucial role in memory function. Disruptions in these systems, caused by conditions like Alzheimer’s disease or certain medications, can contribute to memory impairment.
Neuronal Loss and Synaptic Dysfunction: Conditions like neurodegenerative diseases lead to progressive loss of neurons and disruption of synaptic connections in critical brain regions, impairing memory function.
Other Mechanisms: Specific underlying conditions may have unique pathogenic mechanisms contributing to amnestic disorder. For instance, in Wernicke-Korsakoff syndrome, thiamine deficiency leads to neuronal damage and gliosis in specific brain regions. [4]
Pathophysiology
Pathophysiology
Organic amnestic disorder arises from damage to brain structures crucial for memory processing. The specific mechanisms depend on the underlying cause, but often involve:
Damage to Medial Temporal Lobe Structures: The hippocampus, entorhinal cortex, and parahippocampal gyrus are essential for memory encoding and consolidation. Lesions in these areas disrupt the formation of new memories, causing anterograde amnesia. This damage can occur due to head trauma, stroke, or neurodegenerative diseases like Alzheimer’s.
Disruption of Diencephalic Structures: The thalamus and mammillary bodies play a vital role in memory retrieval and consolidation. Damage to these structures, often seen in Wernicke-Korsakoff syndrome and other conditions, can lead to both anterograde and retrograde amnesia.
Neurotransmitter Imbalance: Neurotransmitters like acetylcholine are crucial for memory function. Disruptions in these systems, caused by Alzheimer’s disease or certain medications, can contribute to memory impairment.
Neuronal Loss and Synaptic Dysfunction: Neurodegenerative diseases lead to progressive neuron loss and synaptic dysfunction in critical brain regions, impairing memory.
Other Mechanisms: Specific underlying conditions may have unique pathogenic mechanisms. For instance, in Wernicke-Korsakoff syndrome, thiamine deficiency leads to neuronal damage and gliosis in specific brain regions. [3]
Clinical Features
Clinical Features
Organic amnestic disorder presents with a core set of clinical features primarily affecting memory function, but it can also impact other cognitive domains.
Key Features:
Anterograde Amnesia: The hallmark feature, this refers to significant difficulty learning and retaining new information after the onset of the disorder. Individuals may struggle to remember recent events, conversations, or appointments.
Retrograde Amnesia: This involves difficulty recalling memories from the past, especially for events closer to the onset of the disorder. Older, more remote memories are often better preserved.
Impaired Short-Term Memory: Individuals may have trouble holding information in their minds for short periods, impacting their ability to follow conversations, complete tasks, or solve problems.
Preserved Immediate Recall: Immediate recall of information, such as repeating a short list of words or numbers, is usually intact.
Confabulation: In some cases, individuals may unintentionally fill in memory gaps with fabricated or distorted information, often without awareness that they are doing so. This is more common in Wernicke-Korsakoff syndrome.
Other Cognitive Impairments: While memory impairment is the primary feature, individuals with organic amnestic disorder may also experience difficulties with attention, concentration, executive function, and visuospatial skills.
Emotional and Behavioral Changes: The memory loss and associated cognitive impairments can lead to frustration, anxiety, depression, irritability, or apathy. [5]
Sign & Symptoms
Sign & Symptoms
Recent memory severely impaired:
The impairment of memory is characterise by a severe impairment of recent memory or short-term memory (inability to learn new material). This is associate with impaired remote memory or long-term memory (inability to recall previously learned material). There is however no impairment of immediate memory (i.e. immediate retention and recall). Recent memory impairment also leads to disorientation in time and place. [2]
Remote memory spared
Disorientation in time:
One consequence of the profound disorder of memory is an associate disorientation in time. [1]
Confabulation:
Gaps in memory are often filled by confabulation. [1] With the progression of the disease, confabulation often disappears. [2]
Other cognitive functions preserved:
It including remote memory, are relatively well preserve. [1]
Unlike the patient with dementia, the patient with an amnesic syndrome seems alert and able to reason or hold an ordinary conversation, so that the interviewer may at first be unaware of the extent of the memory disorder. [1]
Clinical Examination
Clinical Examination of organic amnestic disorder
The clinical examination of organic amnestic disorder involves a comprehensive assessment to identify memory impairment, its severity, and associated cognitive or neurological deficits. The process typically includes the following components:
Detailed History:
A thorough medical and psychiatric history is crucial to identify potential risk factors, such as alcohol abuse, head trauma, stroke, or other medical conditions. Information about the onset, duration, and progression of memory problems is also essential.
Mental Status Examination:
This evaluates various cognitive domains, including:
- Memory: Assessing immediate recall, short-term memory, and long-term memory using standardized tests or tasks (e.g., recalling a list of words, recalling past events).
- Attention and Concentration: Assessing the ability to focus and sustain attention through tasks like digit span or serial sevens.
- Language: Evaluating comprehension, fluency, naming, and repetition to identify any language deficits.
- Visuospatial Skills: Assessing the ability to perceive and manipulate visual information through tasks like drawing or copying figures.
- Executive Function: Evaluating planning, organization, problem-solving, and decision-making abilities through tasks like the Trail Making Test or the Wisconsin Card Sorting Test.
Neurological Examination:
This assesses cranial nerves, motor function, sensory function, reflexes, and coordination to identify any neurological signs suggestive of an underlying cause for memory impairment.
Laboratory and Imaging Studies:
- Blood tests: To assess for nutritional deficiencies (e.g., thiamine), infections, or other metabolic abnormalities.
- Neuroimaging: Brain imaging techniques like MRI or CT scan can help identify structural abnormalities, such as brain atrophy, lesions, or vascular changes. [6]
Diagnosis
Diagnosis of Organic Amnestic Syndrome
According to ICD-10, the following features are required for the diagnosis:
- Recent memory impairment (in other words; anterograde and retrograde amnesia)
- No impairment of immediate retention also recall
- Attention, consciousness
- Global intellectual functioning
- Historical or objective evidence of brain disease or injury (occurs particularly with bilateral involvement of diencephalic and medial temporal structures). [2]
Furthermore, the patient may give a vivid and detailed account of recent activities that, on checking, turn out to be inaccurate.
It is as though he cannot distinguish between true memories and the products of his imagination or recollection of events from times other than those he is trying to recall.
Such a patient is often suggestible; in response to a few cues from the interviewer, he may give an elaborate account of taking part in events that never happened. [1]
Differential Diagnosis
Differential Diagnosis
Several conditions can mimic the memory impairment seen in organic amnestic disorder. It’s crucial to distinguish between these conditions to ensure accurate diagnosis and appropriate management. Some of the key differential diagnoses include:
Dementia: While memory impairment is a core feature of dementia, it typically involves broader cognitive deficits, including language, executive function, and visuospatial skills. The onset is usually gradual, and progression is often relentless.
Mild Cognitive Impairment (MCI): MCI represents a transitional stage between normal aging and dementia. It involves cognitive decline beyond what is expected for age but doesn’t significantly impair daily functioning. Memory impairment is often a prominent feature.
Depression: Memory problems, particularly difficulty concentrating and recalling information, can occur in depression. However, they typically improve with treatment for depression.
Anxiety Disorders: Anxiety can also interfere with memory and concentration. However, the memory problems are usually less severe and improve with anxiety management.
Dissociative Amnesia: This involves a sudden loss of memory for personal information, often triggered by a traumatic event. It typically doesn’t affect the ability to learn new information.
Substance-Induced Amnesia: Memory problems can be caused by the use of certain medications or substances, such as benzodiazepines or alcohol. The memory impairment usually improves with abstinence.
Normal Aging: Some degree of memory decline is a normal part of aging. However, it typically doesn’t significantly interfere with daily functioning or involve other cognitive deficits. [3]
Complications
Complications
Organic amnestic disorder can lead to several complications affecting various aspects of an individual’s life. These complications can stem directly from memory impairment or indirectly from the emotional and psychological impact of the condition. Some of the major complications include:
Functional Impairment: The inability to learn and retain new information can severely affect daily functioning, including difficulty managing personal care, performing household tasks, maintaining employment, or participating in social activities.
Safety Risks: Memory impairment can increase the risk of accidents and injuries, such as forgetting to turn off appliances, getting lost, or mismanaging medications.
Social Isolation: The challenges associated with memory loss and the potential for embarrassment or frustration can lead to social withdrawal and isolation.
Psychological Distress: Memory impairment can cause significant emotional and psychological distress, including anxiety, depression, frustration, low self-esteem, and feelings of helplessness.
Caregiver Burden: The need for constant supervision and assistance can place a significant burden on caregivers, leading to stress, exhaustion, and potential health problems.
Financial Difficulties: The impact on employment and the potential need for specialized care or assisted living can create financial strain.
Increased Risk of Other Health Problems: Individuals with organic amnestic disorder may be at increased risk of other health problems, such as malnutrition, falls, infections, and further cognitive decline. [7]
Investigations
Investigations
The primary goal of investigations is to identify the underlying cause of memory impairment and rule out other potential diagnoses. The specific tests and procedures may vary based on the individual’s clinical presentation and suspected etiology. Common investigations include:
Neuropsychological Testing: A comprehensive neuropsychological assessment helps to characterize the nature and severity of memory impairment and other cognitive deficits. It may include standardized tests evaluating various cognitive domains, such as memory, attention, language, visuospatial skills, and executive function.
Laboratory Tests: Blood tests can assess for potential causes of memory impairment, such as:
- Nutritional deficiencies: Thiamine (vitamin B1) deficiency is a crucial marker for Wernicke-Korsakoff syndrome.
- Infections: Testing for infections like syphilis or HIV, which can affect the brain.
- Metabolic abnormalities: Evaluating thyroid function, liver function, and electrolyte levels.
- Neuroimaging: Brain imaging techniques can visualize structural or functional abnormalities contributing to memory impairment. Common modalities include:
- Magnetic Resonance Imaging (MRI): Provides detailed images of brain structures and can reveal lesions, atrophy, or vascular changes.
- Computed Tomography (CT) Scan: Less detailed than MRI but useful for detecting acute bleeding or large structural abnormalities.
Electroencephalography (EEG): EEG records brain electrical activity and can help identify seizures or other abnormal brain patterns associated with memory impairment.
Lumbar Puncture (Spinal Tap): This procedure may be performed in specific cases to analyze cerebrospinal fluid for signs of infection or inflammation. [6]
Treatment
Treatment
- For cases that may be due to thiamine deficiency, this vitamin should prescribe in the hope of limiting further damage.
- Oral thiamine is sufficient in non-urgent situations, but patients admitted to hospital should give parenteral B vitamins (Pabrinex®). [1]
- Supportive care for general condition and treatment of the associated medical illness. [2]
Prevention
Prevention
Preventing organic amnestic disorder primarily focuses on mitigating the risk factors associated with the condition. While some causes, like neurodegenerative diseases, are less preventable, others can be significantly reduced through lifestyle modifications and medical interventions.
Preventive Strategies:
Reduce Alcohol Consumption: Excessive alcohol intake is a major risk factor for Wernicke-Korsakoff syndrome, a type of organic amnestic disorder. Moderating or abstaining from alcohol can prevent this complication.
Prevent Head Injuries: Wearing helmets during activities like cycling, motorcycling, or contact sports can reduce the risk of traumatic brain injury and subsequent memory impairment.
Manage Cardiovascular Health: Controlling blood pressure, cholesterol levels, and diabetes can minimize the risk of stroke and other vascular conditions affecting brain health.
Promptly Treat Infections: Early diagnosis and treatment of infections, especially those that can affect the brain (e.g., encephalitis), can prevent long-term neurological complications.
Healthy Lifestyle: Maintaining a healthy lifestyle with regular exercise, a balanced diet, adequate sleep, and stress management can promote overall brain health and cognitive function.
Cognitive Stimulation: Engaging in activities that challenge the brain, such as learning new skills, reading, playing games, and social interaction, can help maintain cognitive reserve and potentially delay the onset of memory problems. [3]
Homeopathic Treatment
Homeopathic Treatment for Organic Amnestic Syndrome
Homeopathy is one of the most popular holistic systems of medicine. Additionally, The selection of remedy is based upon the theory of individualization and symptoms similarity by using holistic approach.
There are some specific homeopathic remedies which are quite helpful in amnesia treatment.
Belladonna, Anacardium, Hyoscyamus, Digitalis, Arnica Montana, Plumbum Met, Mercurius, Kali Phos, Natrum Mur, Natrum Carb, Zincum Met, Hypericum, Veratrum Album also many other medicines.
Organic Amnestic Syndrome
Organic amnestic syndrome, also known as Korsakoff’s syndrome, is a memory disorder caused by damage to the brain, often due to thiamine (vitamin B1) deficiency associated with chronic alcohol misuse.
Homeopathic Medicine
Homeopathy emphasizes individualized treatment based on the person’s unique symptoms and constitution. Here are some remedies commonly considered for organic amnestic syndrome:
- Nux Vomica: For individuals with irritability, impatience, and digestive complaints along with memory issues.
- Avena Sativa: For nervous exhaustion, weakness, and difficulty concentrating.
- Kali Phosphoricum: For mental fatigue, memory loss, and anxiety.
- Anacardium Orientale: For forgetfulness, confusion, and a sense of duality.
- Phosphorus: For individuals with a lively and sensitive nature, experiencing memory problems and difficulty concentrating.
Important Note:
- Consult a Qualified Homeopath: It’s crucial to consult a qualified homeopathic practitioner for proper diagnosis and individualized treatment. Self-treatment is strongly discouraged.
- Conventional Treatment: Conventional treatment for organic amnestic syndrome primarily involves thiamine supplementation and addressing any underlying alcohol misuse or nutritional deficiencies. Homeopathy may be considered as a complementary therapy.[8]
Diet & Regimen
Diet & Regimen
While there is no specific diet or regimen that can cure organic amnestic disorder, a healthy lifestyle and diet can play a supportive role in managing symptoms and potentially slowing further cognitive decline, depending on the underlying cause.
Dietary Considerations:
Focus on Brain-Healthy Foods:
Include plenty of fruits, vegetables, and whole grains in your diet.
Choose healthy fats, such as those found in fatty fish, nuts, and olive oil.
Limit saturated and trans fats, found in processed foods and fried foods.
Ensure adequate intake of B vitamins, especially thiamine (vitamin B1), which is crucial for brain health.
Hydration: Drink plenty of water throughout the day to maintain optimal brain function.
Limit Alcohol: Alcohol can worsen memory problems and interfere with medications. If the amnestic disorder is related to alcohol abuse, complete abstinence is crucial.
Dietary Supplements: Consult with a healthcare professional before taking any supplements. They may recommend specific supplements like vitamin B12 or omega-3 fatty acids, depending on individual needs and underlying causes.
Lifestyle Regimen:
Regular Exercise: Engaging in regular physical activity can improve blood flow to the brain and promote cognitive function.
Cognitive Stimulation: Participating in mentally stimulating activities, like puzzles, games, reading, and learning new things, can help maintain cognitive abilities.
Stress Management: Chronic stress can negatively impact memory and overall health. Practices like meditation, deep breathing exercises, or yoga can help manage stress levels.
Social Engagement: Staying connected with friends and family can provide emotional support and help maintain cognitive function.
Sleep Hygiene: Getting adequate sleep is essential for memory consolidation and overall cognitive health. [3]
Do’s and Don'ts
Do’s & Don’ts
Organic Amnestic Syndrome do’s & don’ts
Do’s:
Seek Professional Help: Consult a doctor or mental health professional for proper diagnosis and management. Early intervention is key.
Establish Routines: Consistent daily routines and schedules can help individuals with memory impairment feel more secure and in control.
Use Memory Aids: Utilize tools like calendars, reminders, notes, and alarms to assist with memory recall.
Create a Safe Environment: Minimize fall risks and remove potential hazards at home.
Encourage Social Engagement: Maintaining social connections and participating in activities can help with cognitive stimulation and emotional well-being.
Communicate Clearly and Patiently: Use simple language, repeat information as needed, and avoid overwhelming the individual with too much information at once.
Provide Emotional Support: Be understanding, patient, and reassuring. Memory loss can be frustrating and anxiety-inducing.
Care for the Caregiver: Caregivers need to take care of their own physical and mental health. Seek support groups or respite care when needed.
Don’ts:
- Don’t Argue or Correct: Avoid arguing about forgotten events or trying to force memories. This can lead to frustration and distress.
- Don’t Overload with Information: Keep conversations and instructions simple and concise.
- Don’t Rush or Pressure: Give the individual ample time to process information and respond.
- Don’t Isolate: Encourage social interaction and participation in activities within the individual’s capabilities.
- Don’t Neglect Safety: Be mindful of potential safety risks, such as wandering or forgetting to take medications.
- Don’t Overlook Emotional Needs: Address feelings of anxiety, depression, or frustration that may accompany memory loss.
Terminology
Terminology
Organic:
Refers to a physical or biological cause, distinguishing it from psychological or functional causes. In the context of amnestic disorder, it indicates that the memory impairment is due to an underlying medical condition affecting brain function.
Amnestic Disorder:
A clinical condition characterized by significant memory impairment, particularly the inability to learn new information (anterograde amnesia) or recall past events (retrograde amnesia), impacting daily functioning.
Anterograde Amnesia:
The inability to form new memories after the onset of the disorder.
Retrograde Amnesia:
The inability to recall memories from the past, typically affecting events closer to the onset of the disorder.
Confabulation:
The unintentional fabrication or distortion of memories, often to fill in gaps in recall.
Medial Temporal Lobe:
A brain region crucial for memory processing, including the hippocampus, entorhinal cortex, and parahippocampal gyrus. Damage to this area often leads to anterograde amnesia.
Diencephalon:
Another brain region important for memory, including the thalamus and mammillary bodies. Damage here can result in both anterograde and retrograde amnesia.
Wernicke-Korsakoff Syndrome:
A type of organic amnestic disorder caused by thiamine (vitamin B1) deficiency, often associated with chronic alcohol abuse. It is characterized by severe memory impairment, confabulation, and other neurological symptoms.
Neurodegenerative Diseases:
Progressive conditions affecting brain function, such as Alzheimer’s disease, Parkinson’s disease, and frontotemporal dementia, which can lead to memory impairment and other cognitive deficits.
Cerebrovascular Disease: Conditions affecting blood flow to the brain, such as strokes or transient ischemic attacks, which can damage brain areas involved in memory.
Traumatic Brain Injury (TBI): Injury to the brain caused by external force, which can disrupt memory and other cognitive functions.
Homoeopathic Key Principles and Remedies:
Individualization:
Homeopathic treatment is highly individualized, considering the person’s unique symptoms, personality, and medical history.
Holistic Approach:
Homeopathy aims to treat the whole person, not just the memory impairment, considering emotional and mental aspects as well.
Remedies:
Various homeopathic remedies may be considered based on the individual’s specific symptoms and underlying cause of the amnestic disorder. Some commonly used remedies include:
Anacardium:
For memory weakness, forgetfulness, and confusion.
Baryta Carbonica:
For slowness of thought, difficulty concentrating, and childish behavior.
Conium:
For memory loss associated with vertigo, dizziness, and difficulty focusing.
Hyoscyamus:
For memory loss with restlessness, agitation, and delirium.
Lycopodium:
For memory loss with anxiety, low self-confidence, and digestive issues.
Phosphorus:
For memory loss with weakness, exhaustion, and sensitivity to external stimuli.
References
References
- Psychiatry, Fourth Edition- Oxford Medical Publications – SRG- by Geddes, Jonathan Price, Rebecca McKnight / Ch 26.
- A Short Textbook of Psychiatry by Niraj Ahuja / Ch 3.
- Kaplan & Sadock’s Comprehensive Textbook of Psychiatry (10th Edition) by Benjamin J. Sadock, Virginia A. Sadock, Pedro Ruiz., 2017. Published by Wolters Kluwer
- Principles of Behavioral and Cognitive Neurology (3rd Edition), by M.-Marsel Mesulam., 2014. Published by Oxford University Press
- Diagnostic and Statistical Manual of Mental Disorders (DSM-5) (5th Edition), American Psychiatric Association., 2013.
- The American Psychiatric Association Practice Guidelines for the Treatment of Psychiatric Disorders: Compendium 2006., by American Psychiatric Association.
- The American Psychiatric Association Publishing Textbook of Neuropsychiatry and Behavioral Neurosciences.(6th Edition), by Stuart C. Yudofsky, Robert E. Hales., 2015 Published by American Psychiatric Publishing, Inc.
"Homeopathic Psychology: Personality Profiles of the Major Constitutional Remedies", Edition: 1st Edition, Writer: Philip M. Bailey
(1995, Publication: North Atlantic Books
Also Search As
Also Search As
People can search for homeopathic articles on organic amnestic disorder using the following methods:
Online Resources:
Search Engines: Utilizing search engines like Google, DuckDuckGo, or Bing with specific search terms is the most common method. Effective search terms include:
- "homeopathy for organic amnestic disorder"
- "homeopathic treatment for memory loss due to brain injury"
- "homeopathic remedies for amnesia"
- "organic amnesia and homeopathy"
Homeopathic Journals and Websites: Reputable homeopathic journals and websites often publish articles on various health conditions, including organic amnestic disorder. Some notable resources include:
- The American Journal of Homeopathic Medicine
- The European Journal of Integrative Medicine
- The National Center for Homeopathy
- The British Homeopathic Association
Homeopathic Databases: Online databases like Hompath or RadarOpus offer a vast collection of homeopathic literature, including articles and cases related to organic amnestic disorder.
Offline Resources:
- Homeopathic Libraries: Homeopathic libraries, often associated with homeopathic colleges or associations, can provide access to books, journals, and other publications related to the topic.
- Homeopathic Practitioners: Consult with a qualified homeopathic practitioner who may have access to relevant articles or case studies.
There are several ways to search for information on organic amnestic disorder, using both online and offline resources:
Online Search Methods:
Search Engines: Use popular search engines like Google, Bing, DuckDuckGo, etc. with specific keywords like:
- "organic amnestic disorder"
- "causes of memory loss"
- "amnesia due to brain injury"
- "Wernicke-Korsakoff syndrome"
- "memory disorders"
Medical Websites & Databases: Reputable medical websites and databases can provide reliable information. Some valuable resources include:
- PubMed: A database of biomedical literature
- MedlinePlus: A consumer health information resource from the U.S. National Library of Medicine
- Mayo Clinic website
- WebMD
- National Institutes of Health (NIH) website
Online Medical Journals: Look for articles in online medical journals specializing in neurology, psychiatry, or geriatrics.
Offline Search Methods:
- Libraries: Visit your local library or a medical library to access books, journals, and other resources on the topic.
- Bookstores: Look for books on neurology, psychiatry, or memory disorders in bookstores.
- Healthcare Professionals: Consult with your doctor, a neurologist, or a psychiatrist for information and guidance.
Frequently Asked Questions (FAQ)
What is Organic Amnestic Syndrome?
What causes Organic Amnestic Syndrome?
- Thiamine deficiency
- Head trauma,
- Surgical procedure
- Hypoxia,
- Posterior cerebral artery stroke (especially; bilateral),
- Herpes simplex encephalitis, and
- Space occupying lesions in the region of III ventricle
- Carbon monoxide poisoning,
- Vascular lesions,
How is organic amnestic disorder diagnosed?
Diagnosis involves a thorough medical history, physical examination, neuropsychological testing, and potentially brain imaging or laboratory tests to identify the underlying cause.
What is the prognosis for organic amnestic disorder?
The prognosis varies depending on the underlying cause. Some causes, like reversible infections or nutritional deficiencies, may lead to full recovery. In cases of neurodegenerative diseases, memory impairment may progress over time.
What are the symptoms of Organic Amnestic Syndrome?
- Recent memory severely impaired
- Short-term memory (inability to learn new material)
- Long-term memory (inability to recall previously learned material). There is however no
- Impairment of immediate memory
- Remote memory spared
- Disorientation in time
- Confabulation
- Other cognitive functions preserved
How do I find a qualified homeopathic practitioner?
You can search for registered homeopaths in your area through professional organizations like the National Center for Homeopathy or the North American Society of Homeopaths.
Can homeopathy help with organic amnestic disorder?
Homeopathy may offer supportive treatment for individuals with organic amnestic disorder by addressing the underlying imbalances and promoting overall well-being. It aims to stimulate the body’s self-healing abilities and may help manage symptoms associated with memory impairment.
Is homeopathic treatment safe for organic amnestic disorder?
Homeopathic remedies are generally considered safe when prescribed and monitored by a qualified homeopathic practitioner.
It’s essential to disclose all current medications and health conditions to avoid potential interactions.
What should I expect during a homeopathic consultation for organic amnestic disorder?
The practitioner will conduct a detailed case-taking, including questions about your medical history, symptoms, lifestyle, and emotional well-being. Based on this information, they will recommend an individualized treatment plan.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Organic Amnestic Syndrome?
Homoeopathic Medicines for Organic Amnestic Syndrome
- Belladonna
- Anacardium
- Digitalis
- Arnica Montana
- Plumbum Met
- Mercurius
- Kali Phos
- Natrum Mur
- Natrum Carb
- Zincum Met
