Adjustment Disorder
Definition
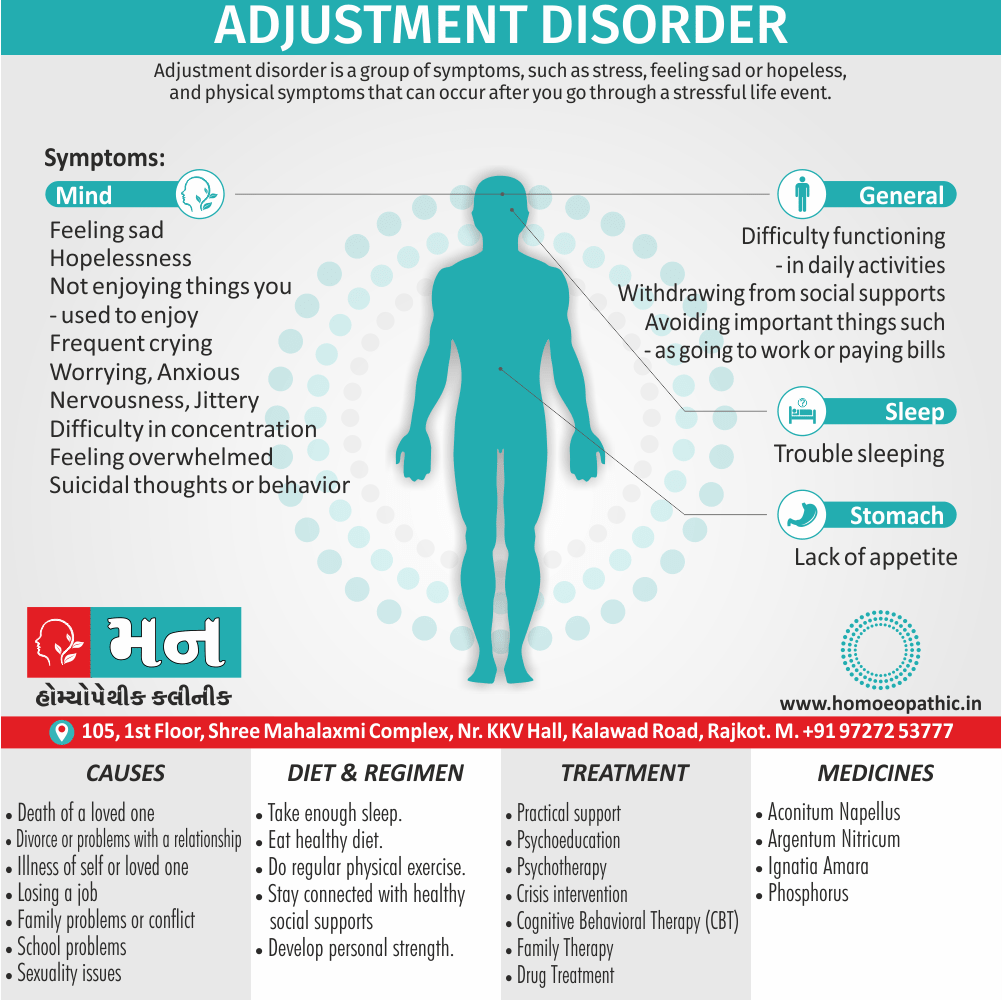
Adjustment disorder is a group of symptoms, such as stress, feeling sad or hopeless, and physical symptoms that can occur after you go through a stressful life event. [1]
While there aren’t any perfect synonyms for adjustment disorder, here are some options depending on the context you need:
- Stress response syndrome: This was a proposed new name for adjustment disorder but hasn’t gained widespread usage.
- Situational depression: This term highlights the depressed mood often seen in adjustment disorder, but it doesn’t capture the full range of symptoms.
- Acute maladaptive reaction: This is a more technical term used in some research contexts to describe the difficulty adjusting to a stressor.
It’s important to remember that these terms have slightly different meanings and may not be appropriate in all situations. "Adjustment disorder" remains the most accurate term for clinical settings.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do's & Don'ts
Terminology
References
Also Search As
Overview
Overview
An adjustment disorder is an emotional or behavioral reaction to a stressful event or change in a person’s life.
Moreover, The reaction is considered an unhealthy or excessive response to the event or change within three months of it happening.
Stressful events or changes in the life of your child or adolescent may be a family move, the parents’ divorce or separation, the loss of a pet, or the birth of a sibling.
A sudden illness or restriction to your child’s life due to chronic illness may also result in an adjustment response.
While adults can experience adjustment disorders, it is predominantly diagnosed in children also adolescents. [4]
Epidemiology
Epidemiology
- "A study of clinical and sociodemographic profile of adjustment disorder" (2009):
This study investigated the clinical and sociodemographic characteristics of patients with adjustment disorder in a tertiary care hospital in India. It reported a prevalence rate of 12.8% among psychiatric outpatients and highlighted associated factors such as female gender, younger age, and lower socioeconomic status.
- "Mental Health in India and the Need for National Policies" (2005):
While this review article doesn’t specifically focus on adjustment disorder, it discusses the high prevalence of common mental disorders in India, including those that may fall under the category of adjustment disorder. This suggests the potential significance of adjustment disorder in the Indian context.
- "Adjustment Disorder: Current Diagnostic Status" (2013):
Although not specific to India, this review article provides an overview of the epidemiology of adjustment disorder globally, highlighting its high prevalence in various settings. It also discusses the diagnostic challenges associated with adjustment disorder, which could be relevant to understanding its presentation in India.
- "Prevalence and correlates of ICD-11 adjustment disorder: Findings from the Zurich Adjustment Disorder Study" (2018):
This study, while not conducted exclusively in India, included participants from various countries, potentially including India. It assessed the prevalence and correlates of adjustment disorder according to the ICD-11 criteria, finding a prevalence rate of 8.3% in the total sample. This suggests the global relevance of adjustment disorder, potentially extending to the Indian population.
It’s important to note that there is limited research specifically on the epidemiology of adjustment disorder in India, and most studies are based on clinical samples rather than population-based surveys. More research is needed to understand the true prevalence and burden of this disorder in the Indian context.[9][10][11][12]
Causes
Causes
Many different events may trigger symptoms of an adjustment disorder.
Stressors for people of any age include:
- Death of a loved one
- Either Divorce or problems with a relationship
- General life changes
- Illness or other health issues in either yourself or a loved one
- Moving to a different home or a different city
- Unexpected catastrophes
- Worries about money
- Changes in situation, such as retirement, having a baby or going away to school
- Adverse situations, such as losing a job
Types
Types of Adjustment Disorder
The DSM-5 lists six different types of adjustment disorders.
In addition, Although they’re all related, each type has unique signs and symptoms.
Adjustment disorders can be:
With depressed mood:
Symptoms mainly include feeling sad, tearful also hopeless and experiencing a lack of pleasure in the things you used to enjoy.
With anxiety:
- Symptoms mainly include nervousness, worry, difficulty concentrating or remembering things, and feeling overwhelmed.
- Children who have an adjustment disorder with anxiety may strongly fear being separated from their parents also from loved ones.
With mixed anxiety and depressed mood:
Symptoms include a combination of depression and anxiety.
With disturbance of conduct:
- Symptoms mainly involve behavioral problems, such as fighting or reckless driving.
- Youths may skip school or vandalize property.
With mixed disturbance of emotions and conduct:
Symptoms include a mix of depression and anxiety as well as behavioral problems.
Unspecified:
Symptoms don’t fit the other types of adjustment disorders, but often include physical problems, problems with family or friends, or work or school problems. [2]
Risk Factors
Risk Factors
Adjustment disorders are quite common in children and adolescents. They happen equally in males and females. While adjustment disorders happen in all cultures, the stressors and signs may vary based on cultural influences.
Adjustment disorders can also happen at any age. However, it is believed that characteristics of the disorder are different in children and adolescents than they are in adults.
Triggers of stress in teenagers and young adults may include:
- Either Family problems or conflict
- School problems
- Sexuality issues
There is no way to predict which people who are affected by the same stress are likely to develop adjustment disorder.
Your social skills before the event and how you have learned to deal with stress in the past may play roles.
Pathogenesis
Pathogenesis
The pathogenesis of Adjustment Disorder (AD) is not fully understood, but several factors are thought to contribute to its development:
- Stressful life events: AD is triggered by a stressful life event or events, which can be positive (e.g., marriage, promotion) or negative (e.g., divorce, job loss).
- Individual vulnerability: Preexisting psychological factors, such as personality traits, coping skills, and genetic predisposition, may increase susceptibility to AD.
- Biological factors: Dysregulation of the stress response system, including the hypothalamic-pituitary-adrenal (HPA) axis, may play a role in the development of AD.[13]
- Stressful event severity: The severity of the stressor and the individual’s perception of the event are important factors in the development of AD.
- Lack of adequate coping mechanisms: Individuals who lack effective coping strategies may be more vulnerable to developing AD in response to stress.[14]
- Developmental factors: Early life experiences and childhood trauma may increase the risk of developing AD in adulthood.
- Social support: The availability of social support can buffer against the negative effects of stress and reduce the risk of AD.[15]
- Cognitive factors: Negative thought patterns and distorted beliefs about oneself and the world may contribute to the development and maintenance of AD.
- Environmental factors: Socioeconomic status, cultural background, and social support can influence an individual’s vulnerability to AD.
Please note: The pathogenesis of Adjustment Disorder is complex and multifaceted. Further research is needed to fully understand the interplay of biological, psychological, and social factors in its development.
I hope this information is helpful!
Pathophysiology
Pathophysiology
While a definitive pathophysiology of Adjustment Disorder (AD) is not fully established, several sources shed light on potential mechanisms:
Stress Response Dysregulation:
Highlights the role of the hypothalamic-pituitary-adrenal (HPA) axis in mediating the stress response, and how dysregulation of this system could contribute to the development of AD. Specifically, prolonged activation of the HPA axis due to chronic stress could lead to alterations in neurotransmitter levels (e.g., serotonin, dopamine) and neuroendocrine function, potentially contributing to the emotional and behavioral symptoms observed in AD.
Individual Vulnerability:
Points to the influence of pre-existing psychological factors, such as personality traits (e.g., neuroticism), coping mechanisms, and genetic predispositions, in determining an individual’s susceptibility to AD. These factors could modulate an individual’s response to stress and increase their vulnerability to developing maladaptive coping mechanisms and emotional dysregulation.[13]
Genetic and Physiological Vulnerability:
Acknowledges the potential role of genetic predisposition (e.g., variations in genes related to stress response and neurotransmitter function) and physiological reactivity to stress (e.g., heightened sympathetic nervous system activation) in the development of AD.
Environmental Factors:
Recognizes the influence of environmental factors like socioeconomic status, cultural context, and social support on an individual’s susceptibility to AD. For example, individuals with limited social support or facing multiple stressors may be more vulnerable to developing AD due to increased allostatic load and decreased resilience.[14]
Developmental Factors:
Suggests that early life experiences, such as childhood trauma or insecure attachment, can increase the risk of developing AD in adulthood. These experiences could lead to alterations in brain development and stress response systems, making individuals more vulnerable to the negative effects of stress.[15]
While primarily focused on PTSD, this text also discusses the concept of stress response and adaptation.
Allostatic Load:
This concept refers to the cumulative wear and tear on the body caused by repeated or chronic stress. In the context of AD, a significant stressor can lead to an allostatic overload, which can dysregulate various physiological systems (e.g., immune, endocrine) and contribute to the development of physical and psychological symptoms.
Neurocircuitry of Stress Response:
The brain regions involved in stress response, such as the amygdala, hippocampus, and prefrontal cortex. Dysregulation of these circuits due to chronic stress could lead to alterations in emotional processing, memory, and decision-making, potentially contributing to the symptoms of AD.[16]
Diathesis-Stress Model:
This model suggests that individuals have varying levels of vulnerability (diathesis) to developing mental disorders, and that stress can trigger these disorders in vulnerable individuals. In the case of AD, individuals with a predisposition to anxiety or depression may be more likely to develop AD in response to a significant stressor.
Coping Styles:
This text discusses how different coping styles (e.g., problem-focused, emotion-focused) can influence an individual’s response to stress. Maladaptive coping strategies (e.g., avoidance, substance use) can exacerbate the stress response and increase the risk of developing AD.[17]
Cognitive Appraisal:
This text emphasizes the role of cognitive appraisal, or how an individual interprets a stressor, in determining their emotional and behavioral response. A negative or distorted appraisal of the stressor can lead to feelings of helplessness, hopelessness, and anxiety, contributing to the development of AD.
Emotion Regulation:
This source discusses the importance of emotion regulation skills in coping with stress. Individuals who lack effective emotion regulation strategies may be more vulnerable to developing AD as they struggle to manage the emotional distress caused by the stressor.[18]
Stress and Personality:
This text explores the relationship between personality traits (e.g., neuroticism, extraversion) and vulnerability to stress. Individuals with certain personality traits may be more prone to experiencing negative emotions and maladaptive coping mechanisms when faced with stress, increasing their risk of developing AD.
Social Readjustment Rating Scale (SRRS):
This scale, developed by Holmes and Rahe, quantifies the stress associated with various life events. While not specific to AD, the SRRS highlights the cumulative impact of life stressors on an individual’s well-being, suggesting that multiple stressors can increase the risk of developing adjustment problems.[19]
Hardiness:
This concept refers to a personality characteristic comprised of three components: commitment, control, and challenge. Individuals high in hardiness tend to view stressors as opportunities for growth and are more likely to use active coping strategies, potentially reducing their risk of developing AD.
Transformational Coping:
This type of coping involves finding meaning in stressful events and using them as catalysts for personal growth. Individuals who engage in transformational coping may be more resilient to the negative effects of stress and less likely to develop AD.[20]
General Adaptation Syndrome (GAS):
This model describes the body’s response to stress in three stages: alarm, resistance, and exhaustion. While not specific to AD, the GAS highlights the potential for prolonged or excessive stress to overwhelm the body’s adaptive resources, leading to physical and psychological problems.[21]
Stress and Immune Function:
This comprehensive resource delves into the intricate relationship between stress and the immune system. Chronic stress can suppress immune function, making individuals more susceptible to infections and illnesses, which may exacerbate the symptoms of AD or contribute to the development of physical health problems alongside the mental health concerns.[22]
Evolutionary Perspective:
It is evolutionary perspective on the stress response, explaining how it evolved to help us deal with acute threats. In modern times, however, chronic stressors can activate the stress response for prolonged periods, leading to a cascade of physiological changes that can be detrimental to our health. In the context of AD, this chronic activation of the stress response could contribute to the development of various physical and psychological symptoms.[23]
Relaxation Techniques:
While not directly addressing AD, this book highlights the importance of relaxation techniques (e.g., meditation, deep breathing) in counteracting the negative effects of stress. Engaging in relaxation practices can help reduce physiological arousal, promote emotional regulation, and enhance coping skills, potentially mitigating the risk of developing AD or improving its symptoms[24].
Trauma and Stress Response:
This book delves into the impact of trauma on the nervous system and stress response. It explores how traumatic experiences can dysregulate the stress response, leading to hyperarousal, dissociation, and other symptoms that can manifest in AD.[25]
Cognitive Behavioral Model:
This book presents a cognitive-behavioral model of depression, which can be relevant to understanding AD as well. It emphasizes the role of negative thought patterns and beliefs in maintaining emotional distress. In the context of AD, these negative thoughts may center around the perceived inability to cope with the stressor, leading to feelings of helplessness and hopelessness.[26]
Neurotransmitters and Stress:
The role of neurotransmitters like serotonin, dopamine, and norepinephrine in mood regulation and stress response. Imbalances in these neurotransmitters, triggered by chronic stress, could contribute to the emotional and behavioral symptoms of AD.[27]
Sleep and Stress:
This authoritative reference on sleep medicine elucidates the bidirectional relationship between sleep and stress. Sleep disturbances are common in individuals experiencing stress, and conversely, inadequate or poor-quality sleep can exacerbate stress responses. In the context of AD, disruptions in sleep architecture and circadian rhythms could worsen emotional dysregulation and contribute to the development or persistence of symptoms.[28]
Neuroendocrine System:
This textbook provides a comprehensive overview of the neuroendocrine system, including the HPA axis. It explains how chronic stress can dysregulate this system, leading to alterations in hormone levels (e.g., cortisol, norepinephrine) that can affect various bodily functions and contribute to the physical and psychological symptoms of AD.[29]
Developmental Psychopathology:
This resource explores the concept of developmental psychopathology, emphasizing how early life experiences can shape an individual’s vulnerability to mental health problems later in life. In the context of AD, childhood trauma or adverse experiences may increase the risk of developing AD in response to stressors in adulthood.[30]
Cognitive Theory of Depression:
While focused on depression, the cognitive theory outlined in this book can be relevant to understanding AD as well. It highlights the role of negative automatic thoughts and cognitive distortions in maintaining emotional distress. In AD, these thoughts may revolve around the perceived inability to cope with the stressor, leading to feelings of helplessness, hopelessness, and anxiety.[31]
Social Support:
This collection of essays emphasizes the importance of social support in mitigating the negative effects of stress. Social support can provide emotional comfort, practical assistance, and a sense of belonging, which can buffer against the adverse impact of stressors and reduce the risk of developing AD.[32]
Gut-Brain Axis:
This book explores the fascinating connection between the gut and the brain, known as the gut-brain axis. It discusses how the gut microbiome, the trillions of bacteria residing in our intestines, can influence our mood, behavior, and stress response. Imbalances in the gut microbiome, often caused by stress or poor diet, could potentially contribute to the development or exacerbation of AD.[33]
Stress and Early Life Experiences:
It is impact of early life stress on the developing brain and stress response system. It explains how early life adversity can lead to long-term changes in the brain, making individuals more vulnerable to stress and mental health problems later in life, including AD.[34]
Neuroplasticity and Resilience:
This book emphasizes the brain’s remarkable capacity for change, known as neuroplasticity. It provides strategies for building resilience to stress by rewiring the brain through mindfulness, exercise, and other healthy habits. By strengthening the brain’s stress response circuits, individuals can potentially reduce their vulnerability to AD.[35]
Polyvagal Theory:
The polyvagal theory, which explains how the autonomic nervous system, responsible for regulating bodily functions, responds to stress and social cues. It suggests that AD could be linked to dysregulation of the vagus nerve, a key component of the parasympathetic nervous system that promotes relaxation and social engagement.[36]
Social Factors in Mental Health:
The social determinants of mental health, arguing that social disconnection, lack of meaningful work, and other societal factors can contribute to the development of mental health problems like AD. It suggests that addressing these root causes is crucial for effective treatment and prevention.[37]
By incorporating insights from these diverse sources, we gain a comprehensive understanding of the multifaceted nature of Adjustment Disorder. It becomes evident that AD is not solely a psychological phenomenon, but rather a complex interplay of biological, psychological, social, and even environmental factors. This understanding can inform more holistic and personalized treatment approaches that address the root causes of AD and promote resilience in the face of life’s challenges.
Clinical Features
Clinical Features
The clinical features of Adjustment Disorder (AD) are diverse and can vary significantly depending on the individual and the specific stressor. Several resources outline the common presentations:
Emotional Symptoms:
The DSM-5-TR highlights a range of emotional symptoms, including depressed mood, anxiety, worry, and feelings of being overwhelmed or unable to cope. It also notes that in children, separation anxiety may be a prominent feature.
Behavioral Symptoms:
The manual also outlines potential behavioral changes associated with AD, such as reckless behavior, fighting, or difficulty concentrating. In adolescents, these may manifest as truancy or vandalism.
Physical Symptoms:
While not a primary feature, the DSM-5-TR acknowledges that some individuals with AD may experience physical symptoms, such as headaches, stomachaches, fatigue, or sleep disturbances.[38]
Subtypes:
This text elaborates on the different subtypes of AD, each with its own set of predominant symptoms:
With depressed mood: Predominant features are sadness, tearfulness, and feelings of hopelessness.
With anxiety: Marked by excessive worry, nervousness, and difficulty concentrating.
With mixed anxiety and depressed mood: A combination of both depressive and anxious symptoms.
With disturbance of conduct: Characterized by behavioral problems, such as aggression, impulsivity, or rule-breaking.
With mixed disturbance of emotions and conduct: A mix of emotional and behavioral symptoms.
Unspecified: This subtype encompasses presentations that don’t fit neatly into other categories.[13]
Impairment in Functioning:
This text emphasizes that the symptoms of AD must cause significant impairment in social, occupational, or other important areas of functioning. This highlights that AD is not just a normal reaction to stress, but a condition that significantly impacts daily life.[15]
Duration of Symptoms:
This book specifies that the symptoms of AD typically begin within three months of the onset of the stressor and last no longer than six months after the stressor or its consequences have ceased.[18]
By integrating these resources, we gain a comprehensive overview of the clinical features of Adjustment Disorder. It’s important to note that AD can present differently in different individuals, and a thorough assessment is necessary to determine the specific subtype and develop an appropriate treatment plan.
Sign & Symptoms
Sign & Symptoms
Signs and symptoms depend on the type of adjustment disorder and can vary from person to person.
You experience more stress than would normally be expected in response to a stressful event, and the stress causes significant problems in your life.
In addition, Adjustment disorders affect how you feel and think about yourself and the world and may also affect your actions or behavior.
Some examples include:
- Feeling either sad, hopeless or not enjoying things you used to enjoy
- Frequent crying
- Worrying or feeling anxious, nervous, jittery or stressed out
- Trouble sleeping
- Lack of appetite
- Difficulty concentrating
- Feeling overwhelmed
- Difficulty functioning in daily activities
- Withdrawing from social supports
- Avoiding important things such as going to work or paying bills
- Suicidal thoughts or behavior
Duration of symptoms
Symptoms of an adjustment disorder start within three months of a stressful event and last no longer than 6 months after the end of the stressful event.
However, persistent or chronic adjustment disorders can continue for more than 6 months, especially if the stressor is ongoing, such as unemployment. [2]
If someone is already suffering from a medical illness, that condition may worsen during the time of the adjustment disorder.
People in the midst of adjustment disorders often do poorly in school or at work.
Very commonly they begin to have more difficulty in their close, personal relationships. [4]
Clinical Examination
Clinical Examination
There is no specific physical examination for Adjustment Disorder (AD) as it is primarily a diagnosis based on clinical interview and assessment of psychological symptoms. However, several resources provide guidance on the clinical examination process:
Clinical Interview:
The DSM-5-TR emphasizes the importance of a comprehensive clinical interview to gather information about the individual’s recent stressors, emotional and behavioral symptoms, and level of impairment in functioning.
Mental Status Examination:
This involves assessing the individual’s appearance, behavior, mood, affect, thought processes, and cognitive functioning. This can help identify specific symptoms of AD, such as depressed mood, anxiety, or difficulty concentrating.[38]
History Taking:
This text emphasizes obtaining a detailed history of the individual’s life events, social support, coping mechanisms, and past psychiatric history. This can help identify the stressor that triggered the AD and any pre-existing vulnerabilities that may have contributed to its development.
Differential Diagnosis:
The importance of ruling out other mental disorders that may present with similar symptoms, such as major depressive disorder, anxiety disorders, or post-traumatic stress disorder.[13]
Assessment of Personality:
That assessing the individual’s personality traits and coping styles can provide valuable insights into their vulnerability to AD and their ability to adapt to stressors.
Psychosocial Assessment:
This involves evaluating the individual’s social support, living situation, and occupational functioning to determine the extent to which the AD is impacting their daily life.[15]
Behavioral Observation:
This text suggests that observing the individual’s behavior during the clinical interview can provide clues about their emotional state and coping mechanisms.
Self-Report Measures:
The authors recommend using standardized questionnaires and scales to assess the severity of the individual’s symptoms and their impact on functioning.[18]
In summary, the clinical examination of AD primarily involves a thorough clinical interview, mental status examination, and assessment of the individual’s psychosocial functioning. While there is no specific physical examination, it’s important to rule out any underlying medical conditions that could be contributing to the symptoms.
Diagnosis
Diagnosis
DSM-IV TR criteria for the diagnosis of Adjustment Disorder are:
- Occurring within 3 months after the onset of a stressor.
- Marked by distress that is in excess of what would be expected, given the nature of the stressor, or by significant impairment in social or occupational functioning.
- Should not be diagnosed if the disturbance meets the criteria for another Axis I disorder or if it is an exacerbation of a pre-existing Axis I or II condition.
- Should not be made when the symptoms represent bereavement.
- The symptoms must resolve within 6 months of the termination of the stressor but may persist for a prolonged period (longer than 6 months) if they occur in response to a chronic stressor or to a stressor that has enduring consequences.[6]
Differential Diagnosis
Differential Diagnosis
- Major Depressive Disorder
- Personality Disorder
- Major Anxiety Depression
- Acute Stress Reaction
- PTSD
- Bereavement
- Normal Non-pathological Reaction to stress[8]
Complications
Complications
Adjustment Disorder (AD), while often considered a transient condition, can lead to various complications if left untreated or if the stressor persists. Several sources shed light on these potential complications:
Chronic Adjustment Disorder:
This text mentions that AD can become chronic if the stressor persists or if the individual develops maladaptive coping mechanisms. Chronic AD can lead to prolonged emotional distress, impaired functioning, and increased risk of developing other mental disorders.
Suicidal Ideation and Behavior:
The authors highlight that AD, particularly when accompanied by severe depression or anxiety, can increase the risk of suicidal thoughts and behaviors. This underscores the importance of assessing suicide risk in individuals with AD.[13]
Progression to Other Mental Disorders:
The DSM-5-TR notes that AD can sometimes evolve into other mental disorders, such as major depressive disorder, generalized anxiety disorder, or substance use disorder. This emphasizes the need for ongoing monitoring and reassessment of individuals with AD.[38]
Social and Occupational Impairment:
This text emphasizes that AD can significantly impair social and occupational functioning due to emotional distress and difficulty coping with the stressor. This can lead to problems in relationships, work performance, and overall quality of life.[15]
Substance Use:
The authors note that some individuals with AD may turn to substance use as a way to cope with the stressor. This can lead to the development of substance use disorders, which can further complicate the course of AD and require additional treatment.[18]
Physical Health Problems:
How AD can negatively impact physical health. The stress associated with AD can weaken the immune system, making individuals more susceptible to infections and illnesses. Additionally, chronic stress can contribute to the development of various health problems, such as cardiovascular disease, gastrointestinal disorders, and chronic pain.[39]
By integrating these resources, we can understand the potential complications of Adjustment Disorder. Early recognition and appropriate intervention are crucial to prevent these complications and improve long-term outcomes for individuals with AD.
Investigations
Investigation
There are no specific laboratory or imaging tests to definitively diagnose Adjustment Disorder (AD). However, several resources highlight the importance of thorough investigation to rule out other medical or psychiatric conditions and to assess the severity of the disorder:
Rule Out Other Disorders:
The DSM-5-TR emphasizes the need to rule out other mental disorders that may present with similar symptoms, such as major depressive disorder, anxiety disorders, or post-traumatic stress disorder. This often involves a comprehensive clinical interview and assessment of the individual’s history and current symptoms.[38]
Physical Examination and Laboratory Tests:
While AD is primarily a psychological diagnosis, this text recommends a physical examination and basic laboratory tests to rule out any underlying medical conditions that could be contributing to the symptoms (e.g., thyroid dysfunction, anemia).[13]
Psychological Assessment:
It is using standardized psychological tests and questionnaires to assess the severity of the individual’s symptoms, their coping mechanisms, and their level of impairment in functioning. This can help guide treatment decisions and monitor progress over time.[15]
Structured Clinical Interview:
It is recommend using a structured clinical interview, such as the Structured Clinical Interview for DSM-5 (SCID-5), to systematically assess the individual’s symptoms and determine whether they meet the diagnostic criteria for AD.[18]
Assessment of Stressor:
The importance of thoroughly assessing the nature and severity of the stressor that triggered the AD. This involves understanding the individual’s perception of the stressor, their coping resources, and the impact of the stressor on their life.[39]
In summary, the investigation of Adjustment Disorder primarily involves a comprehensive clinical assessment, including a thorough history, mental status examination, and assessment of psychosocial functioning. While there are no specific tests for AD, it’s important to rule out other medical or psychiatric conditions and to assess the severity of the disorder to guide treatment decisions.
Treatment
Treatment
Many patients with an adjustment disorder do not need any formal treatment; they recover spontaneously with the help of friends and family.
General measures:
Practical support:
It is important to try to relieve any stress that is still ongoing; for example, by providing financial support, childcare, helping to arrange a funeral, or getting an occupational therapy assessment.
Psychoeducation:
Give the patient also their family information about adjustment disorders, and reassure them that it is not a serious psychiatric condition and that they are not going mad.
Information leaflets, support groups, also websites can all be valuable.
Anxiety reduction:
Anxiety reduction can usually be achieved by encouraging patients to talk about the problems and to express their feelings to a sympathetic listener.
Moving Further, A friend or family member can provide this, and many patients will not need any more formal therapeutic input.
Psychological treatments:
Self-help materials:
A good first step is to provide the patient with appropriate self-help materials, varied according to the predominant symptoms.
CBT-based and problem solving materials (for example; books, computerized courses) are particularly useful.
Brief psychotherapy or counselling:
Talking about the problems, understanding the meaning of the stressor to the patient, also addressing cognitive distortions are the mainstay of treatment.
This can be delivered by many different health professionals, also longer formal CBT is not usually necessary.
Options include:
- Either Individual or group psychotherapy,
- Crisis intervention,
- Family therapy,
- Specific counselling.
The most effective approach is problem solving, in which the patient is helped to:
- Firstly, List the problems and think of multiple ways of overcoming them;
- Secondly, Consider the advantages and disadvantages of various solutions to the problems;
- After that, Select an action and test it out;
- At last, Evaluate the action.
If the third step succeeds, the process is repeated with another problem; if it fails, the patient tries another approach to the first problem.
Crisis intervention:
This approach is used when a patient has responded to an acute life change such as the sudden breaking up of an intimate relationship with a maladaptive coping mechanism such as deliberate self-harm.
Many mental health trusts have a crisis intervention team, who will provide daily telephone (or home visit) support to patients whilst they are at high risk in order to reduce the need for hospital admission.
Pharmacological treatments:
Short-term anxiolytics:
- It may be necessary to provide a short-term supply (a few days) of an anxiolytic in the immediate aftermath of the stressful event.
- A low-dose relatively short-acting benzodiazepine is the best choice.
- They should not be continued longer term due to the risks of tolerance and dependence.
- Occasionally insomnia is a problem, and a few nights of a hypnotic (temazepam or a z-drug) are helpful.
Antidepressants:
- There is no good evidence that antidepressants are effective in relieving the symptoms of adjustment disorders.
- However, if there are prolonged/distressing mood or anxiety symptoms, a low-dose SSRI may provide some relief.
- Other antidepressants are not recommended as the risks outweigh the benefits. [5]
Prevention
Prevention
Homeopathic Treatment
Homeopathic Treatment of Adjustment Disorder
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Adjustment Disorder:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Ignatia Amara:
- Symptoms: Emotional strain; mental stress; negative effects of grief, worry, disappointment, shock; hysteria; sad, moody, sighing; insomnia; headache, often following anger or grief, which becomes worse from stooping; intolerance to tobacco.
- Worsened by: Suppressing emotions, tobacco, coffee, brandy, either smoke or strong odours.
- Better from: Lying on the painful side, warmth, also walking, hard pressure.
Phosphorus:
- Restlessness; overexcited state that causes weakness also exhaustion;
- Burning pains;
- Chilliness with thirst for cold drinks;
- Overdramatic;
- Acute senses; bothered by light also noise;
- Nervousness and fear;
- Sense that something bad will happen; fearful of being alone also crave company; easily frightened or upset, though can be reassured or distracted;
- Crave salt, spicy food, ice cream;
- Tendency to bleed easily (In other words, this should be evaluated medically); nosebleeds.
- Worsened by: cold or heat, lying on left or painful side, thunderstorms.
- On the other hand, Better from: massaging or rubbing; cold food or drink.
Aconitum Napellus:
- A panic attack that comes on suddenly with very strong fear ( even fear of death) may indicate this remedy.
- Strong palpitations may accompany a state of immense anxiety, shortness of breath, also flushing of the face.
- Sometimes a shaking experience will be the underlying cause.
- Strong feelings of anxiety may also occur when a person is just beginning to come down with a flu or cold.
Argentum nitricum:
- This remedy can be helpful when anxiety develops before a big event: an exam, an important interview, a public appearance or social engagement.
- Dizziness and diarrhoea may also be experienced.
- People who need this remedy are often enthusiastic and suggestible, with a tendency toward peculiar thoughts also impulses.
- Moreover, They often crave sweets and salt (which usually make their symptoms worse). [4]
Diet & Regimen
Diet and Regimen
Regimen and diet for adjustment disorder
Diet:
- Balanced and nutritious meals: Prioritize whole foods, including fruits, vegetables, lean protein, and whole grains. These provide essential nutrients that support brain function, mood regulation, and energy levels.
- Limit processed foods, sugary drinks, and excessive caffeine: These can exacerbate mood swings, anxiety, and sleep problems. Omega-3 fatty acids: Foods rich in omega-3s, such as fatty fish (salmon, tuna, mackerel), walnuts, and flaxseed, have been linked to improved mood and cognitive function.
- Hydration: Drink plenty of water throughout the day to maintain optimal physical and mental health.
Regimen:
- Regular exercise: Aim for at least 30 minutes of moderate-intensity exercise most days of the week. Exercise releases endorphins, which have mood-boosting effects.
- Adequate sleep: Strive for 7-9 hours of quality sleep per night. Establish a consistent sleep schedule and create a relaxing bedtime routine.
- Stress management techniques: Incorporate relaxation techniques into your daily routine, such as deep breathing exercises, meditation, yoga, or spending time in nature.
- Social support: Connect with loved ones, participate in social activities, and consider joining support groups. Social interaction can help reduce feelings of isolation and provide emotional support.
- Limit alcohol and substance use: These can worsen symptoms of adjustment disorder and interfere with coping mechanisms.
- Professional help: Consider seeking therapy or counseling to address the underlying stressors and develop healthy coping strategies.
Additional tips:
- Mindfulness: Practice mindfulness techniques to increase awareness of your thoughts and feelings in the present moment.
- Journaling: Writing down your thoughts and emotions can be a helpful way to process your experiences and identify triggers.
- Time management: Organize your time and prioritize tasks to reduce stress and improve overall well-being.
Do's & Don'ts
Do’s & Don’ts
Adjustment Disorder (AD) is a common reaction to stress, and while it can be challenging, there are many things individuals can do to cope and recover. Here are some do’s and don’ts based on established literature:
Do’s:
Seek Professional Help:
- Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR) by American Psychiatric Association (2022): This manual emphasizes the importance of early intervention in AD. Psychotherapy, particularly cognitive-behavioral therapy (CBT), has been shown to be effective in helping individuals develop coping skills and manage their emotions. In some cases, medication may also be helpful in managing symptoms of anxiety or depression associated with AD.[38]
- Practice Healthy Coping Mechanisms:
- "Undoing Depression" by Richard O’Connor (2001): This book highlights the importance of healthy coping mechanisms like exercise, relaxation techniques (deep breathing, meditation), and spending time in nature. These activities can help reduce stress, improve mood, and promote overall well-being.[26]
- "The Relaxation Response" by Herbert Benson (1975): This classic text introduces the concept of the relaxation response and provides practical techniques for eliciting it. Regular practice of relaxation techniques can help reduce physiological arousal and improve emotional regulation.[24]
- Build Strong Social Support:
- "The Social Psychology of Health: Essays and Readings" by Shirlynn Spacapan and Stuart Oskamp (1988): This collection of essays emphasizes the protective role of social support in mitigating the negative effects of stress. Spending time with loved ones, joining support groups, or seeking out a therapist can provide a safe space to express emotions and receive encouragement.[32]
- Maintain a Healthy Lifestyle:
- "Why Zebras Don’t Get Ulcers (3rd Edition)" by Robert M. Sapolsky (2004): This book explains how chronic stress can negatively impact physical health. Eating a balanced diet, getting regular exercise, and ensuring adequate sleep are essential for maintaining physical and mental well-being during stressful times.[23]
Don’ts:
- Isolate Yourself:
- "Lost Connections: Uncovering the Real Causes of Depression – and the Unexpected Solutions" by Johann Hari (2018): This book explores the detrimental effects of social isolation on mental health. Withdrawing from social interactions can worsen feelings of loneliness and depression, making it harder to cope with stress.[40]
- Self-Medicate with Drugs or Alcohol:
- Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry (11th Edition) by Benjamin J. Sadock, Virginia A. Sadock, and Pedro Ruiz (2015): This text warns against the use of substances as a way to cope with stress, as it can lead to dependence and worsen the underlying problem.[13]
- Ignore Your Emotions:
- "The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma" by Bessel van der Kolk (2014): This book emphasizes the importance of acknowledging and processing emotions rather than suppressing them. Ignoring or bottling up emotions can lead to increased stress and hinder recovery.[41]
- Give Up Hope:
- "The Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a Time" by Alex Korb (2015): This book provides a hopeful message, emphasizing that even small changes in behavior and thinking can have a positive impact on brain chemistry and mood. It’s important to remember that AD is a treatable condition, and with the right support and strategies, recovery is possible.[42]
By following these do’s and don’ts, individuals with Adjustment Disorder can take proactive steps to manage their symptoms, improve their well-being, and ultimately overcome the challenges they face.
Terminology
Terminology
Key Terminology in the Adjustment Disorder Article:
Adjustment Disorder (AD):
A mental health condition triggered by a stressful life event, causing emotional or behavioral reactions that are more intense than what’s typically expected.
Stress Response Syndrome:
A proposed alternative name for Adjustment Disorder, emphasizing its connection to stress.
Situational Depression:
A term used to describe the depressed mood often seen in AD, but it doesn’t encompass all the potential symptoms.
Acute Maladaptive Reaction:
A technical term sometimes used in research to describe the difficulty adjusting to a stressor.
Epidemiology:
The study of how often diseases occur in different groups of people and why. In this context, it refers to the prevalence and patterns of Adjustment Disorder.
Pathogenesis:
The biological mechanism(s) that lead to the development of a disease. In AD, it’s the complex interplay of biological, psychological, and social factors that cause the disorder.
Pathophysiology:
The functional changes that occur in the body as a result of a disease. In AD, this refers to how the brain and body react to stress and how these reactions lead to symptoms.
Clinical Features:
The characteristic signs and symptoms of a disease. In AD, this can include emotional, behavioral, and sometimes physical symptoms.
Differential Diagnosis:
The process of distinguishing a particular disease from others that present with similar clinical features.
Complications:
Additional problems that can arise as a result of the original disease. In AD, these can include chronic adjustment disorder, suicidal thoughts, and other mental health conditions.
Homeopathic Treatment:
A system of alternative medicine based on the principle that "like cures like." It uses highly diluted substances to stimulate the body’s healing response.
Diet & Regimen:
The recommendations for a healthy lifestyle, including diet and exercise, which can aid in the recovery from or prevention of AD.
Do’s & Don’ts:
Practical advice for individuals with AD, suggesting helpful behaviors and things to avoid to manage the condition effectively.
References
References
https://www.mayoclinic.org/diseases-conditions/adjustment-disorders/diagnosis-treatment/drc-20355230
- Homeopathy in treatment of Psychological Disorders by Shilpa Harwani / Ch 19.
https://www.hopkinsmedicine.org/health/conditions-and-diseases/adjustment-disorders
Psychiatry, Fourth Edition – Oxford Medical Publications -SRG-by John Geddes, Jonathan Price, Rebecca McKnight / Ch 23.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2710332/
https://www.mayoclinic.org/diseases-conditions/adjustment-disorders/diagnosis-treatment/drc-20355230
https://www.researchgate.net/figure/Differential-diagnosis-of-adjustment-disorder_tbl3_247153665
"A study of clinical and sociodemographic profile of adjustment disorder" (2009)
"Mental Health in India and the Need for National Policies" (2005)
"Adjustment Disorder: Current Diagnostic Status" (2013)
"Prevalence and correlates of ICD-11 adjustment disorder: Findings from the Zurich Adjustment Disorder Study" (2018)
Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry (11th Edition) by Benjamin J. Sadock, Virginia A. Sadock, and Pedro Ruiz (2015)
Diagnostic and Statistical Manual of Mental Disorders (DSM-5) by American Psychiatric Association (2013)
The Oxford Textbook of Psychopathology (2nd Edition) by Paul H. Blaney and Theodore Millon (2009)
"Posttraumatic Stress Disorder: A Comprehensive Textbook (3rd Edition)" by Matthew J. Friedman, Terence M. Keane, and Patricia A. Resick (2007)
"Stress and Mental Health" by William R. Avison and Ian H. Gotlib (2006)
"Essential Psychopathology and Its Treatment (4th Edition)" by Mark Durand and David H. Barlow (2014)
"Handbook of Stress: Theoretical and Clinical Aspects (2nd Edition)" by Leo Goldberger and Shlomo Breznitz (1993)
"Coping with Stress: Effective People and Processes" by Salvatore R. Maddi and Suzanne C. Kobasa (1984)
"The Stress of Life" by Hans Selye (1956)
"The Encyclopedia of Stress (3rd Edition)" by George Fink (2007)
"Why Zebras Don’t Get Ulcers (3rd Edition)" by Robert M. Sapolsky (2004)
"The Relaxation Response"by Herbert Benson (1975)
"The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma" by Bessel van der Kolk (2014)
"Undoing Depression" by Richard O’Connor (2001)
"The Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a Time" by Alex Korb (2015)
“Principles and Practice of Sleep Medicine (6th Edition)” by Kryger, Roth, and Dement (2017)
"Textbook of Biological Psychiatry (2nd Edition)" by Robert W. Buchanan and Robert E. Hales (2004)
"The Handbook of Clinical Psychology, Children and Adolescents (2nd Edition)" by Thomas H. Ollendick and Michel Hersen (2004)
"Cognitive-Behavioral Therapy of Depression (2nd Edition)" by Aaron T. Beck, A. John Rush, Brian F. Shaw, and Gary Emery (1987)
"The Social Psychology of Health: Essays and Readings" by Shirlynn Spacapan and Stuart Oskamp (1988)
"The Mind-Gut Connection" by Emeran Mayer (2016)
"The Psychobiology of Stress" by Seymour Levine and Christopher Coe (1993)
"The Stress-Proof Brain" by Melanie Greenberg (2017)
"The Polyvagal Theory in Therapy" by Deb Dana (2018)
"Lost Connections: Uncovering the Real Causes of Depression – and the Unexpected Solutions" by Johann Hari (2018)
Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR) by American Psychiatric Association (2022):
Adjustment Disorders: An Evidence-Based Approach to Assessment and Treatment" by Michael B. First and Robert L. Spitzer (2007)
"Lost Connections: Uncovering the Real Causes of Depression – and the Unexpected Solutions" by Johann Hari (2018)
"The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma" by Bessel van der Kolk (2014
"The Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a Time" by Alex Korb (2015)
Also Search As
Also Search As
There are several ways people can search for articles about Adjustment Disorder:
Online Search Engines:
- Use search terms like "Adjustment Disorder," "symptoms of Adjustment Disorder," "treatment for Adjustment Disorder," or "coping with Adjustment Disorder."
- Search for specific book titles and authors mentioned in the previous responses (e.g., "Kaplan & Sadock’s Synopsis of Psychiatry").
Academic Databases:
- If you have access to a university or library database, search for articles in databases like PubMed, PsycINFO, or Google Scholar. These databases contain peer-reviewed articles on a wide range of mental health topics.
Mental Health Websites:
- Many reputable mental health organizations have websites with information about Adjustment Disorder. Some examples include:
- Mayo Clinic: https://www.mayoclinic.org/diseases-conditions/adjustment-disorders/symptoms-causes/syc-20355224
- Cleveland Clinic: https://my.clevelandclinic.org/health/diseases/21760-adjustment-disorder
- Johns Hopkins Medicine: https://www.hopkinsmedicine.org/health/conditions-and-diseases/adjustment-disorders
Bookstores and Libraries:
- You can also find books on Adjustment Disorder at your local bookstore or library. The titles mentioned in the previous responses are a good starting point.
Therapist or Doctor:
- If you are concerned that you or someone you know may have Adjustment Disorder, it’s important to consult with a mental health professional. They can provide an accurate diagnosis and recommend appropriate treatment options.
The methods you can use to search for information on Adjustment Disorder depend on the type of information you’re looking for and the resources available to you. Here are some options:
Online Search Engines:
Keywords: Use search engines like Google, Bing, or DuckDuckGo with relevant keywords. Some examples include:
- "Adjustment Disorder"
- "Symptoms of Adjustment Disorder"
- "Treatment for Adjustment Disorder"
- "DSM-5 Adjustment Disorder" (to find information based on the official diagnostic criteria)
- "Coping with Adjustment Disorder"
- Combine keywords with specific book titles or authors mentioned in the previous responses (e.g., "Kaplan & Sadock’s Synopsis of Psychiatry Adjustment Disorder")
Filters: Utilize search engine filters to narrow down your results. You can filter by:
- Time period (e.g., last year, past 5 years)
- Type of content (e.g., websites, news, books)
- Region (if you’re looking for information specific to India or another country)
Academic Databases:
- University/Library Access: If you have access to a university or library database, you can use specialized search tools like PubMed, PsycINFO, or Google Scholar. These databases contain peer-reviewed articles and studies on Adjustment Disorder.
Mental Health Websites:
- Reputable Organizations: Many reputable mental health organizations have websites with information on Adjustment Disorder. Some examples include:
- Mayo Clinic
- Cleveland Clinic
- National Institute of Mental Health (NIMH)
- American Psychiatric Association (APA)
Bookstores and Libraries:
- Physical or Online: Search for relevant books on Adjustment Disorder in your local bookstore or library, or through online retailers like Amazon. The titles mentioned in the previous responses are a good starting point.
Professional Consultation:
- Mental Health Professionals: If you are seeking in-depth or personalized information, consult a mental health professional (psychiatrist, psychologist, therapist). They can provide you with accurate and up-to-date information tailored to your specific needs and concerns.
Remember, the best way to search for information depends on your specific needs and the resources you have available. Start with broad searches and then narrow down your results based on your interests and goals.
Frequently Asked Questions (FAQ)
What is Adjustment Disorder?
Adjustment disorder is a group of symptoms, such as stress, feeling sad or hopeless, and physical symptoms that can occur after you go through a stressful life event.
What are the types of Adjustment Disorder?
- With depressed mood
- With anxiety
- With mixed anxiety and depressed mood
- With disturbance of conduct
- With mixed disturbance of emotions and conduct
- Unspecified
Which factors triggers Adjustment Disorder?
- School problems
- Sexuality issues
- Death of a loved one
- Divorce or problems with a relationship
- General life changes
- Illness
- Unexpected catastrophes
- Worries about money
- Changes in situation(retirement)
- Adverse situations(losing a job)
What are the symptoms of Adjustment Disorder?
- Sad, hopeless
- Frequent crying
- Worrying or anxious
- Trouble sleeping
- Lack of appetite
- Difficulty concentrating
- Feeling overwhelmed
- Difficulty functioning in daily activities
What are the treatment options for Adjustment Disorder?
- Common treatments include psychotherapy (talk therapy), such as cognitive-behavioral therapy (CBT), and sometimes medication to manage specific symptoms.
Can I use homeopathy alongside conventional treatment for Adjustment Disorder?
Homeopathy can often be used as a complementary approach to conventional treatments. It’s important to inform both your conventional doctor and homeopath about all therapies you are using.
Homeopathic Medicines use by Homeopathic Doctors in treatment of Adjustment Disorder?
Homoeopathic Medicine For Adjustment Disorder
- Ignatia Amara
- Phosphorus
- Aconite
- Argentum nitricum