Allergic Rhinitis
Definition
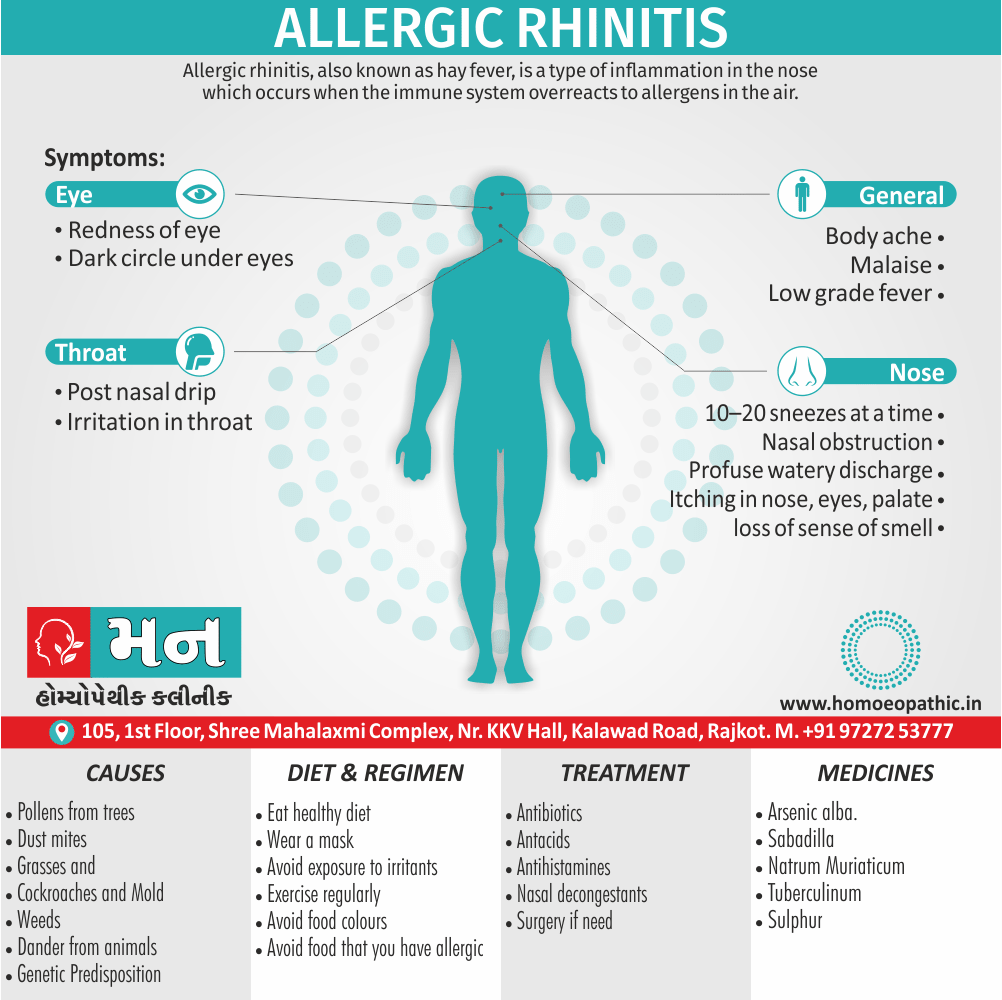
Allergic rhinitis, also knows as hay fever, is a type of inflammation in the nose which occurs when the immune system overreacts to allergens in the air.[1]
Here are some synonyms for allergic rhinitis:
- Hay fever: This is the most common synonym for allergic rhinitis. It refers to the seasonal allergic rhinitis that is triggered by pollen.
- Pollinosis: This is a medical term for allergic rhinitis that is caused by pollen.
- Rose cold: This is an older term for allergic rhinitis that is triggered by pollen from roses.
- Rose fever: This is another older term for allergic rhinitis that is triggered by pollen from roses.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do's & Don'ts
Terminology
References
Also Search As
Overview
Overview
It is an Ig. E Mediated immunologic response of nasal mucosa to airborne allergens and is characterized by watery nasal discharge, nasal obstruction, sneezing also itching in the nose. This may also be associated with symptoms of itching in the eyes, palate and pharynx.
Symptoms onset is often within minutes following allergen exposure and can affect sleep, and the ability to work or study. Some people may develop symptoms only during specific time of the year, often as a result of pollen exposure. Many people with allergic also have asthma, allergic conjunctivitis, or atopic dermatitis [1].
Epidemiology
Epidemiology
Allergic rhinitis (AR) is a prevalent inflammatory condition of the nasal passages in India. Several studies have explored the epidemiology of AR in India, highlighting its significant impact on the population.
Prevalence:
- A systematic review and meta-analysis published in 2019 revealed that the prevalence of AR in India ranges from 20% to 30%. (epidemiology of allergic rhinitis in india: a systematic review, 2019)
- Another study indicated that AR affects a substantial portion of the population, with estimates suggesting that it impacts up to 40% of individuals. (Allergic rhinitis in India: an overview, 2016)
Impact on Quality of Life:
- AR has a considerable impact on individuals’ quality of life, contributing to various complications and associated health issues. (epidemiology of allergic rhinitis in india: a systematic review, 2019)
- It can lead to substantial morbidity, affecting various aspects of daily life. (Allergic rhinitis in India: an overview, 2016)
Comorbidities:
- AR is often associated with other allergic diseases, such as asthma, atopic dermatitis, and conjunctivitis. (Allergic diseases in India – Prevalence, risk factors and current challenges, 2022)
- The unified airway theory suggests that AR is a component of a broader systemic allergic response, potentially affecting multiple organ systems. (epidemiology of allergic rhinitis in india: a systematic review, 2019)
Risk Factors:
- Various environmental and genetic factors contribute to the development of AR in India. (Allergic diseases in India – Prevalence, risk factors and current challenges, 2022)
- The prevalence of AR varies across different geographical locations in India, with unclear reasons for this variation. (Allergic diseases in India – Prevalence, risk factors and current challenges, 2022)
Challenges:
- There is a lack of adequate epidemiological studies in India, particularly in rural and suburban areas, which may misrepresent the true burden of AR. (Allergic rhinitis in India – PubMed, 2023)
- India faces challenges in terms of unmet demand for trained allergy specialists and a poor health service framework, which can hinder effective management of AR. (Allergic diseases in India – Prevalence, risk factors and current challenges, 2022)
In conclusion, AR is a widespread health issue in India, affecting a significant proportion of the population and impacting their quality of life. Further research is needed to better understand the epidemiology of AR in India and to develop effective prevention and treatment strategies.
Causes
Causes
[1] Inhalant allergens
(a) Seasonal allergens for example;
- pollens from trees,
- grasses
(b) Perennial allergens
They are present throughout the year regardless of the season, For example
- Mold
- Dust mites
- Cockroaches
- Dander from animals
Dust includes dust mite, insect parts, fibres and animal dander. Dust Mites live on skin scales also other debris and are found in the beddings, mattresses, pillows, carpets also upholstery.
[2] Genetic Predisposition
It plays an important part.
Chances of children developing allergy are 20 and 47%, respectively, if one or both parents suffer from allergic diathesis [2].
Types
Types
Two clinical types have been recognized:
- Firstly, Seasonal:
Symptoms either appear in or around particular season when the pollens of a particular plant, to which the patient is sensitive, are present on the air.
- Secondly, Perennial:
Symptoms are present throughout the year.
Risk Factors
Risk Factors for Allergic Rhinitis
- The presence of other allergic diseases such as asthma, eczema
- Parental rhinitis
- Allergic sensitization to common household aeroallergens
- higher-weight person
- Elevated exhaled Nitric oxide
- High total serum IgE
- Exposure to parental smoking
- Exposure to pets
- Genetic predisposition
- Exposure to fossil fuel also traffic related pollutants
- Increased dampness also poor ventilation from tightly insulated modern homes (increases sensitization and allergy to molds)
- Early introduction of infants to formula/food[4]
Pathogenesis
Pathogenesis
The pathogenesis of allergic rhinitis (AR) is a complex process involving various immune responses and inflammatory mediators. Several authoritative texts provide detailed explanations of the underlying mechanisms:
Initial Sensitization:
Upon initial exposure to an allergen (e.g., pollen, dust mites), antigen-presenting cells (APCs) capture and process the allergen, presenting it to T helper 2 (Th2) cells.
Th2 cells release cytokines like interleukin-4 (IL-4) and interleukin-13 (IL-13), which stimulate B cells to produce allergen-specific immunoglobulin E (IgE) antibodies.
IgE antibodies bind to high-affinity receptors on mast cells and basophils, priming them for subsequent allergen encounters.[6]
Early-Phase Response:
Upon re-exposure to the same allergen, it cross-links IgE antibodies on mast cells and basophils, triggering their degranulation.
This releases preformed mediators like histamine, tryptase, and leukotrienes, leading to the immediate symptoms of AR, including sneezing, itching, rhinorrhea, and nasal congestion.[7]
Late-Phase Response:
Several hours after the early-phase response, recruited inflammatory cells like eosinophils, basophils, and Th2 cells further contribute to the inflammatory cascade.
These cells release additional mediators like cytokines, chemokines, and lipid mediators, perpetuating the allergic response and contributing to the ongoing symptoms of AR.[8]
Chronic Inflammation and Remodeling:
Repeated allergen exposure and persistent inflammation can lead to structural changes in the nasal mucosa, including epithelial damage, basement membrane thickening, and goblet cell hyperplasia.
These changes contribute to the chronic symptoms of AR and may increase susceptibility to other respiratory conditions like asthma.[9]
Understanding the pathogenesis of AR is crucial for developing effective treatments that target specific mediators and pathways involved in the allergic response. Current therapies focus on allergen avoidance, pharmacotherapy (antihistamines, corticosteroids, leukotriene receptor antagonists), and immunotherapy.
Pathophysiology
Pathophysiology
Inhaled allergens produce specific Ig. E antibody in the genetically Predisposed individuals. This antibody becomes fixed to the blood basophils or tissue mast cells by its Fc end
On subsequent exposure, antigen combines with Ig. E antibody at its Fab end. This reaction produces degranulation of the mast cells with release of several chemical mediators, some of which already exist in the preformed state while others are synthesized afresh.
These mediators are responsible for symptomatology of allergic disease.
Depending on the tissues involved, there may be vasodilation, mucosal oedema, infiltration with eosinophils, excessive secretion from nasal glands or smooth muscle contraction. A “priming affect” has also been described, i.e., mucosa earlier sensitized to an allergen will react to smaller doses of subsequent specific allergen. It also gets “primed” to other nonspecific antigens to which patient was not exposed. Nonspecific Nasal hyper-reactivity is seen in patients of allergic rhinitis.
There is increased nasal response to normal stimuli resulting in sneezing, rhinorrhoea also nasal congestion [2].
Clinically allergic response occurs in two phases i.e.:
1.Acute or early phase
It occurs immediately within 5–30 min, after exposure to the specific allergen and consists of sneezing, rhinorrhoea nasal blockage and/or bronchospasm. It is due to release of vasoactive amines like histamine.
2.Late or delayed phase
It occurs 2–8 h after exposure to allergen without additional exposure. It is due to infiltration of inflammatory cells—eosinophils, neutrophils, basophil, monocytes and CD4 + T cells at the site of antigen deposition causing swelling, congestion and thick secretion.
In the event of repeated or continuous exposure to allergen, acute phase symptomatology overlaps the late phase [2].
Clinical Features
Clinical Features
Allergic rhinitis (AR) presents with a constellation of characteristic clinical features, as described in various authoritative sources:
Nasal Symptoms:
Sneezing: Often paroxysmal and repetitive, especially upon exposure to allergens.
Rhinorrhea: Clear, watery nasal discharge.
Nasal Congestion/Obstruction: Due to mucosal edema and inflammation.
Itching: In the nose, eyes, palate, and throat.[7]
Ocular Symptoms:
Itching: In the eyes, often accompanied by rubbing.
Tearing: Excessive watery discharge from the eyes.
Redness: Conjunctival injection and irritation.[10]
Additional Symptoms:
Postnasal Drip: Sensation of mucus dripping down the back of the throat.
Cough: Due to postnasal drip or associated lower airway inflammation.
Headache: Pressure-like sensation in the frontal or maxillary sinuses.
Fatigue: Due to sleep disturbances and the inflammatory response.[11]
Physical Examination Findings:
Pale/bluish nasal mucosa: Due to venous congestion and edema.
Inferior turbinate hypertrophy: Enlarged and boggy inferior turbinates.
Allergic Shiners: Dark circles under the eyes due to venous congestion.
Allergic Crease: Transverse nasal crease due to frequent upward rubbing of the nose ("allergic salute").[8]
Classification:
Intermittent AR: Symptoms occur <4 days/week or <4 weeks/year.
Persistent AR: Symptoms occur ≥4 days/week and >4 weeks/year.
Mild AR: Symptoms do not impair sleep or daily activities.
Moderate-Severe AR: Symptoms impair sleep, work/school performance, or daily activities.[12]
Understanding the clinical features of AR is essential for accurate diagnosis and appropriate management. If you suspect you have AR, consult a healthcare professional for evaluation and personalized treatmen recommendations.
Sign & Symptoms
Sign and Symptoms:
Symptoms
- There is no age or sex predilection.
- It may start in infants as young as 6 months or older people.
- Usually the onset is at 12–16 years of age.
- The cardinal symptoms of seasonal nasal allergy include paroxysmal sneezing, 10–20 sneezes at a time, nasal obstruction, watery nasal discharge and itching in the nose. Itching May also involve eyes, palate or pharynx. Some may get bronchospasm. The duration and severity of symptoms may Vary with the season.
- Symptoms of perennial allergy are not so severe as that of the seasonal type. They include frequent colds, persistently stuffy nose, loss of sense of smell due to mucosal oedema, postnasal drip, chronic cough and hearing impairment due to eustachian tube blockage or fluid in the middle ear.
Signs
Signs of allergy may be seen in the nose, eyes, ears, pharynx or larynx.
Nasal signs i.e.
include transverse nasal crease—a black line across the middle of dorsum of nose due to constant upward rubbing of nose simulating a salute (allergic salute), pale and oedematous nasal mucosa which may appear bluish. Turbinate’s are swollen. Thin, watery or mucoid discharge is usually present [2].
Ocular signs i.e.
include oedema of lids, congestion and cobble- stone appearance of the conjunctiva, and dark circles under the eyes (allergic shiners).
Otologic signs i.e.
include retracted tympanic membrane or serous otitis media as a result of eustachian tube blockage.
Pharyngeal signs i.e.
include granular pharyngitis due to hyperplasia of submucosal lymphoid tissue. A child with perennial allergic rhinitis may show all the features of prolonged mouth breathing as seen in adenoid hyperplasia.
Laryngeal signs i.e.
include hoarseness and oedema of the vocal cords.[2]
Clinical Examination
Clinical Examination
The examination of patients with rhinitis should include an examination of the nose, and assessment for possible comorbidities and complications. The physical examination of a patient with rhinitis may reveal the following i.e.:
General Appearance
- Rhinorrhea may be seen
- Mouth breathing from nasal congestion
- Sniffing
- Allergic shiners: Dark eye shadows beneath the lower eye lid due to blood/fluid accumulation in the infraorbital groove as a result of congestion of the nose/sinuses. It is commonly seen in childhood allergic rhinitis, and the degree of darkness is associated with the chronicity and severity of disease. It can also be seen in nonallergic rhinitis.
- Dennie–Morgan lines: These are wrinkles/ extra skin fold underneath the lower eyelids. It is seen in children with allergic diseases such as allergic rhinitis.
- Allergic salute- A habitual gesture of rubbing the nose upward because of nasal discomfort and pruritus. It sometimes produces a persistent horizontal crease across the nose.
Ocular findings:
Commonly seen in patients with allergic rhinitis. Some of the ocular findings include i.e.:
- Bilateral conjunctival injection, papillae and cobblestones.
- Corneal involvement in severe cases (atopic and vernal keratoconjunctivitis).
- Frequent rubbing of the eyes, irritability, lacrimation, mucus discharge.
- Blepharospasm
- Periorbital edema
Nasal findings:
Examination of the nasal cavity with a speculum or otoscope may reveal the following i.e.:
- Swollen/edematous turbinates
- Pale, bluish or erythematous mucosa. The mucosa is often pale/bluish in allergic rhinitis.
Ear findings:
Otoscopic examination of the ears may reveal signs suggestive of associated co-morbidities such as:
- Otitis media with effusion- common in patients with allergic rhinitis.
- Acute otitis media
Face
- Facial tenderness/discomfort on palpation of the sinuses. This often occurs when the inflammation extends into the sinuses (rhinosinusitis), and it can be as a result of infection or allergy
- Abnormal facial development such as elongated facies may be seen, especially in chronic mouth breathers.
Mouth and Throat
- Coexisting conditions like hypertrophied adenoids may be seen.
- Dental malocclusion frequently occurs in children who are chronic mouth breathers.
- High arch in the palate
- Cobblestoning of the oropharynx
- Posterior drainage of nasal secretions
Skin
- Eczema may be seen in patients with allergic rhinitis if there is coexisting atopic dermatitis.
Chest
- A thorough chest examination is essential, as it may reveal abnormalities suggestive of other pathological conditions or co-morbidities such as respiratory tract infections, asthma.[5]
Diagnosis
Diagnosis
[1] Allergic skin test
[2] CBC shows eosinophilia
Differential Diagnosis
Differential Diagnosis of Allergic Rhinits
- Deviated nasal septum/septal wall anomalies
- Adenoidal hypertrophy
- Nasal tumors (benign and malignant)
- Foreign bodies- Unilateral, mucopurulent rhinorrhea in children could be as a result of insertion of foreign objects into the nostril.
- Trauma
- Anatomical variants in the ostiomeatal complex
- Choanal atresia
- Cleft palate
- Pharyngeal reflux (laryngopharyngo-nasal reflux)
- Metabolic conditions such as acromegaly
Complications
Complications
While often considered a benign condition, allergic rhinitis (AR) can lead to various complications if left untreated or poorly managed. Several authoritative sources highlight potential complications associated with AR:
Sinusitis:
- AR increases the risk of developing sinusitis, an inflammation of the sinuses. The swollen nasal passages can block sinus drainage, leading to mucus accumulation and bacterial infection.[8].
Nasal Polyps:
- These are noncancerous growths in the nasal passages or sinuses that can cause obstruction, loss of smell, and further exacerbate AR symptoms.[7]
Otitis Media:
- AR can predispose to middle ear infections (otitis media), especially in children. The Eustachian tube dysfunction caused by AR can lead to fluid buildup and infection in the middle ear.[11]
Sleep Disturbances:
- Nasal congestion, postnasal drip, and other AR symptoms can disrupt sleep, leading to daytime fatigue, irritability, and decreased cognitive function.[13]
Asthma Exacerbation:
Reduced Quality of Life:
- The persistent symptoms of AR can significantly impair daily activities, work/school performance, and overall well-being.[15]
Other Complications:
- In rare cases, AR may contribute to dental problems (due to mouth breathing), eustachian tube dysfunction, and even mood disorders like anxiety and depression.
To prevent these complications, prompt diagnosis and effective management of AR are crucial. Consultation with a healthcare professional is recommended to develop a personalized treatment plan and address any underlying or associated conditions.
Investigations
Investigation of Allergic Rhinitis
To measure your antibodies to specific allergens, your provider may take a blood sample also send it to a lab for testing. Additionally, This blood test is called an immunoglobulin E (IgE) test.
It can detect all types of allergies, including food allergies.
Your provider may recommend a skin prick test to determine what allergens are causing your symptoms.
Skin prick test
This common test is painless and accurate, though it may be a little uncomfortable. Your provider places a small sample of different allergens on your skin (usually on your forearm or back) also scratches or pricks the skin with a needle. Scratching the skin allows the allergen to get under the surface.
If you’re allergic to the allergen, the area will become red, itchy also irritated in 15 to 30 minutes. You may develop raised, hive-like welts called wheals that show an allergic reaction. A skin prick test is a safe, effective way to determine which allergens are causing your symptoms.[6]
Treatment
Treatment of Allergic Rhinitis:
it’s can be divided into:
1. Avoidance of allergen i.e.
This is most successful if the antigen involved is single. Moreover, Removal of a pet from the house, encasing the pillow or mattress with plastic sheet, change of place of work or sometimes change of job may require.
A particular food article to which the patient is found allergic can eliminate from the diet.
2. Drugs:
(a) Antihistaminic i.e.
They control rhinorrhoea, sneezing and nasal itch. All antihistaminic have the side effect of drowsiness; some more than the other. The dose and type of the antihistaminic has to be individualized. If one antihistaminic is not effective, another may try from a different class [2]
(b) Sympathomimetic drugs (oral or topical) i.e.
Alpha-adrenergic drugs constrict blood vessels and reduce nasal congestion and oedema. They also cause central nervous system stimulation and are often giving in combination with antihistaminic to counteract drowsiness. Pseudoephedrine and phenylephrine are often combining with antihistaminics for oral administration. Additionally, Topical use of sympathomimetic drugs causes nasal decongestion.
Phenylephrine, oxymetazoline and xylometazoline Are often used to relieve nasal obstruction, but are notorious to cause severe rebound congestion. Patient Resorts to using more and more of them to relieve nasal obstruction. This vicious cycle leads to rhinitis medicamentosa.
(c)Corticosteroids i.e.
Oral corticosteroids are very effective in controlling the symptoms of allergic rhinitis but their use should limit to acute episodes which have not controlled by other measures.
3. Immunotherapy i.e.
Immunotherapy or hyposensitization is used when drug treatment fails to control symptoms or produces intolerable side effects [2].
Prevention
Prevention of Allergic Rhinitis
Allergic rhinitis cannot be prevented. You can help your symptoms especially by avoiding the things that cause your symptoms.
- Keep windows closed. This is especially important during high-pollen seasons.
- Wash your hands after petting animals.
- Use dust- also mite-proof bedding and mattress covers.
- Wear glasses outside to protect your eyes.
- Shower before bed to wash off allergens from hair and skin.
You can also avoid things that can make your symptoms worse, such as:
- Aerosol sprays
- Air pollution
- Cold temperatures
- Humidity
- Irritating fumes
- Tobacco smoke
- Wind
- Wood smoke[5]
Homeopathic Treatment
Homeopathic management of Allergic Rhinitis:
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Allergic Rhinitis:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
1. Allium Cepa:
- Action: Primarily targets acrid nasal discharge that irritates the nostrils, accompanied by bland (non-irritating) eye discharge. Think of the symptoms you get from cutting an onion.
- Symptoms: Watery eyes, sneezing, burning sensation in the nose, and a runny nose that worsens in a warm room and improves in open air.
2. Arsenicum album:
- Action: Suitable for rhinitis with thin, watery, and burning nasal discharge, often accompanied by sneezing and restlessness.
- Symptoms: Burning and itching in the nose, sneezing, watery discharge, and a general feeling of chilliness. Symptoms often worsen at midnight or with changes in temperature.
3. Natrum muriaticum:
- Action: Addresses allergic rhinitis with excessive sneezing, often as the initial symptom.
- Symptoms: Dry mucous membranes, loss of taste and smell, watery nasal discharge, and a craving for salt.
4. Euphrasia:
- Action: Focuses on profuse, acrid tears with bland nasal discharge.
- Symptoms: Burning and redness of the eyes, sensitivity to light, and a constant need to wipe the eyes.
5. Pulsatilla:
- Action: Often used for allergic rhinitis with thick, yellow-greenish discharge and a lack of thirst.
- Symptoms: Changeable symptoms, tearful disposition, and a desire for open air. Symptoms often worsen in warm rooms and improve with cold applications.
6. Kali bichromicum:
- Action: Targets cases with thick, stringy, and yellow or greenish nasal discharge.
- Symptoms: Nasal blockage, post-nasal drip, and a loss of smell.
7. Sabadilla:
- Action: Helpful when there’s intense itching in the nose and violent sneezing, often triggered by specific odors.
- Symptoms: Sneezing attacks, watery nasal discharge, and a dry mouth.
8. Wyethia:
- Action: Addresses intense itching in the nose, roof of the mouth, and behind the ears.
- Symptoms: Dryness of the nose and throat, constant need to swallow, and a feeling of a lump in the throat.
Diet & Regimen
Diet and Regimen
Regimen and Diet
Diet for Managing Allergic Rhinitis
Focus on:
- Omega-3 rich foods: Fatty fish, flaxseeds, chia seeds for anti-inflammatory benefits.
- Vitamin C rich foods: Citrus fruits, berries, leafy greens for natural antihistamine properties.
- Probiotics: Yogurt, kefir, sauerkraut to support gut health and immune function.
- Quercetin-rich foods: Apples, onions, berries for antihistamine and anti-inflammatory effects.
Limit or avoid:
- Dairy products: May increase mucus production for some.
- Processed foods: Often contain additives and preservatives that trigger inflammation.
- Alcohol: Can worsen nasal congestion and inflammation.
- Your specific food allergens: Crucial to identify and avoid!
Regimen for Managing Allergic Rhinitis
Reduce Allergen Exposure:
- Identify and avoid your triggers (pollen, dust mites, pet dander, mold).
- Nasal irrigation with saline solution to remove allergens and irritants.
- Maintain clean indoor air (air filters, vacuuming, hot water wash for bedding).
Symptom Management:
- Manage stress through relaxation techniques (yoga, meditation).
- Use over-the-counter relief (antihistamines, decongestants, nasal corticosteroids) as needed.
- Consider immunotherapy (allergy shots) for long-term desensitization.
Important: Always consult a doctor or allergist for personalized advice and treatment options. They can help you identify your triggers and create a tailored management plan.
Do's & Don'ts
Do’s & Don’ts
Managing allergic rhinitis (AR) effectively involves a combination of lifestyle modifications, allergen avoidance, and appropriate medical treatment. Here are some essential do’s and don’ts based on authoritative references:
Do’s:
Identify and Avoid Triggers:
- Keep a diary to track your symptoms and potential allergens.
- Minimize exposure to identified allergens like pollen, dust mites, pet dander, and molds.[10]
Maintain a Clean Environment:
- Use dust mite covers for bedding and pillows.
- Vacuum regularly with a HEPA filter.
- Keep indoor humidity low to discourage mold growth.[11]
Use Medications as Prescribed:
- Follow your doctor’s instructions for using antihistamines, decongestants, nasal corticosteroids, or other prescribed medications.[7]
Consider Allergen Immunotherapy:
- If allergen avoidance and medications are insufficient, discuss immunotherapy (allergy shots or sublingual tablets) with your doctor.[16]
Don’ts:
Don’t Smoke or Be Around Smoke:
- Smoking worsens AR symptoms and can trigger asthma attacks.[14]
Don’t Overuse Decongestants:
- Prolonged use can lead to rebound congestion.[17]
Don’t Ignore Worsening Symptoms:
- Consult your doctor if your symptoms are not well-controlled or if you develop new symptoms.[8]
Don’t Self-Medicate:
- Always consult with your doctor before starting any new medications or supplements, as some may interact with your existing treatment plan.
By following these do’s and don’ts and working closely with your healthcare professional, you can effectively manage allergic rhinitis and improve your quality of life.
Terminology
Key Terminologies and Meanings:
Allergic Rhinitis:Inflammation of the nasal mucosa caused by an allergic reaction to airborne allergens.
Hay Fever: A common synonym for allergic rhinitis, particularly when triggered by pollen during specific seasons.
Pollinosis: A medical term specifically referring to allergic rhinitis caused by pollen.
- IgE-Mediated: Refers to the type of immune response involved in allergic rhinitis, where immunoglobulin E (IgE) antibodies play a central role in triggering the allergic reaction.
- Allergens: Substances that trigger allergic reactions, such as pollen, dust mites, animal dander, and mold spores.
- Rhinorrhea: A runny nose, often watery and clear, characteristic of allergic rhinitis.
Nasal Obstruction/Congestion:
Blockage or stuffiness in the nose due to swelling of the nasal lining.
- Pruritus: Itching, a common symptom in allergic rhinitis affecting the nose, eyes, palate, and throat.
- Paroxysmal Sneezing: Sudden and repeated episodes of sneezing, often triggered by allergen exposure.
Seasonal Allergic Rhinitis:
Allergic rhinitis that occurs during specific seasons, usually due to pollen from trees, grasses, or weeds.
- Perennial Allergic Rhinitis: Allergic rhinitis that persists throughout the year, often caused by indoor allergens like dust mites, pet dander, or mold.
- Allergic Salute: A characteristic upward rubbing of the nose in response to nasal itching and discomfort.
- Allergic Shiners: Dark circles under the eyes due to venous congestion in the sinuses, often seen in allergic rhinitis.
- Cobblestone Mucosa: An appearance of the conjunctiva (lining of the eyelids) with small bumps or follicles, often associated with allergic rhinitis.
- Edema: Swelling of tissues due to fluid accumulation, often seen in the nasal passages during an allergic reaction.
- Homeopathy: A system of alternative medicine that uses highly diluted substances to stimulate the body’s healing response.
- Homeopathic Remedies: Substances used in homeopathy, selected based on the individual’s specific symptoms and constitution.
- Miasm: A concept in homeopathy referring to a predisposing factor or inherited tendency towards certain diseases.
Additional Notes:
- You might want to add terms like "antihistamines," "corticosteroids," and "immunotherapy" in the terminology section as they are mentioned in the treatment section of the article.
- For SEO purposes, consider adding a section on "homeopathic remedies for allergic rhinitis" to the article to further optimize for relevant keywords.
References
Reference
- https://en.wikipedia.org/wiki/Allergic_rhinitis
- Disease of EAR, NOSE, AND THROAT&HEAD AND NECK SURGERY 6TH EDITIONS BY P.L Dhingra, Shruti Dhingra.
- https://www.multicarehomeopathy.com/diseases/6-best-homeopathic-medicines-for-allergic-rhinitis-treatment
- https://www.wikidoc.org/index.php/Rhinitis_risk_factors
- https://familydoctor.org/condition/allergic-rhinitis/
- Abbas, A. K., Lichtman, A. H., & Pillai, S. (2020). Cellular and Molecular Immunology (9th ed.). Elsevier.
- Holgate, S. T., Pawankar, R., Akdis, C. A., & Canonica, G. W. (2015). Middleton’s Allergy: Principles and Practice (8th ed.). Elsevier Saunders.
- Bachert, C., Akdis, C. A., & Gevaert, P. (2019). Allergic Rhinitis and Chronic Rhinosinusitis: A Practical Guide (2nd ed.). Springer.
Galli, S. J., Tsai, M., & Piliponsky, A. M. (2008). The development of allergic inflammation. Nature, 454(7203), 445-454.
- Bielory, L., & Friedlaender, M. H. (2019). Allergic Diseases: Diagnosis and Management (5th ed.). Little, Brown and Company.
- Corren, J., Baroody, F. M., & Togias, A. (2018). Allergic Rhinitis and Its Impact on Asthma (ARIA) 2016 Revision. Journal of Allergy and Clinical Immunology, 142(4), 984-991.
- World Health Organization. (2016). Allergic Rhinitis and its Impact on Asthma (ARIA) Guidelines.
- Kern, R. C., & Conley, D. B. (2016). Clinical Otolaryngology: Head and Neck Surgery (2nd ed.). Elsevier.
- Pawankar, R. (2011). Allergic rhinitis and asthma: The united airway disease concept. Asian Pacific Journal of Allergy and Immunology, 29(1), 1-6
- Bousquet, J., Schünemann, H. J., Zuberbier, T., & Bachert, C. (2012). ARIA guidelines—2012 revision. Allergy, 67(8), 969-1000.
- Cox, L., Nelson, H., Lockey, R., & Calabria, C. (2011). Allergen immunotherapy: A practice parameter third update. Journal of Allergy and Clinical Immunology, 127(1), S1-S55.
Also Search As
Also Search as
Online Resources:
- Search Engines: Using search engines like Google, Bing, or DuckDuckGo with keywords like "allergic rhinitis," "hay fever," or "pollen allergy" can lead to a vast array of information, including articles, research studies, and medical websites.
- Reputable Websites: Organizations like the American Academy of Allergy, Asthma & Immunology (AAAAI) and the Asthma and Allergy Foundation of America (AAFA) provide comprehensive information on AR, including symptoms, causes, diagnosis, and treatment options.
- Health Websites: Websites like Mayo Clinic, WebMD, and Healthline offer detailed information on AR, including potential complications and tips for managing the condition.
Healthcare Professionals:
- Primary Care Physician: A primary care physician can assess for AR, provide a diagnosis, and recommend appropriate treatment options or referrals to specialists.
- Allergist/Immunologist: These specialists focus on allergies and immune system disorders and can provide comprehensive diagnosis and treatment for AR.
Support Groups and Forums:
Libraries and Bookstores:
- Books and resources on allergies and AR can be found in libraries and bookstores.
Tips for Effective Searching:
- Use specific keywords: Instead of just searching for "allergies," use more specific terms like "allergic rhinitis," "hay fever triggers," or "seasonal allergies treatment."
- Use quotation marks: Enclosing search terms in quotation marks will yield results that include the exact phrase.
- Use Boolean operators: Words like "AND," "OR," and "NOT" can help refine your search. For example, searching for "allergic rhinitis AND treatment" will show results that include both terms.
- Be mindful of the source: Ensure the information comes from reputable sources like medical organizations, government agencies, or well-established health websites.
There are numerous ways to search for information on Allergic Rhinitis (AR):
1. Online Resources:
- Search Engines: Google, Bing, DuckDuckGo, etc., are excellent starting points. Use keywords like "allergic rhinitis," "hay fever," "pollen allergy," or specific symptom terms like "sneezing" or "runny nose."
- Reputable Medical Websites: Websites like the Mayo Clinic, WebMD, Healthline, the American Academy of Allergy, Asthma & Immunology (AAAAI), and the Asthma and Allergy Foundation of America (AAFA) offer comprehensive, medically accurate information on AR.
- Government Health Agencies: Organizations like the National Institutes of Health (NIH) or the Centers for Disease Control and Prevention (CDC) can have resources and research on AR.
2. Academic Databases:
- PubMed: A free resource from the National Library of Medicine that allows you to search for scholarly articles and research publications on AR.
- Google Scholar: Another free search engine specifically for academic literature, including research papers, theses, and books on AR.
3. Healthcare Professionals:
- Your Doctor or Allergist: These are the best resources for personalized diagnosis and treatment recommendations.
- Pharmacists: They can provide information on over-the-counter and prescription medications for AR.
4. Libraries:
- Local libraries often have books and resources on allergies and AR. Librarians can help you navigate their collections and find relevant materials.
5. Social Media & Online Communities:
- Support Groups & Forums: Many online communities and forums are dedicated to discussing allergies, including AR. They can be a valuable source of support and shared experiences. Be sure to choose reputable groups and forums moderated by healthcare professionals or experienced patients.
Tips for Effective Searching:
- Use Specific Keywords: Be as specific as possible in your search terms. For example, instead of "allergies," use "allergic rhinitis treatment options" or "allergic rhinitis causes."
- Combine Keywords: Use Boolean operators (AND, OR, NOT) to refine your search. For example, search for "allergic rhinitis AND children" to find information specifically for children.
- Check the Source: Always verify the information you find online. Look for credible sources like medical organizations, government agencies, or well-respected health websites.
By using a combination of these methods and tips, you can easily find reliable and comprehensive information on allergic rhinitis to help you understand, manage, and treat your condition effectively.
Frequently Asked Questions (FAQ)
What is Allergic rhinitis?
Allergic rhinitis, also knows as hay fever, is a type of inflammation in the nose which occurs when the immune system overreacts to allergens in the air.
Homeopathic Medicines used by Homeopathic Doctors in Treatment of Allergic rhinitis?
Medicine For Allergic Rhinitis
- Arsenic album
- Sulphur
- Natrum muriaticum
- Sabadilla
- Allium cepa
- Tuberculinum
What are the causes of Hay Fever?
Cause
- Pollens
- Mould
- Dust mites
- Cockroaches
- Dander from animals
- Genetic Predisposition
Describe the symptoms of Allergic rhinitis?
Symptoms
- Paroxysmal sneezing
- Nasal obstruction
- Watery nasal discharge
- Itching in the nose
- Frequent colds
- Persistently stuffy nose
- Loss of sense of smell
- Chronic cough
- Oedema of lids
- Hoarseness
- Oedema of the vocal cords
What are the common triggers for allergic rhinitis?
Triggers For Allergic Rhinitis
Common triggers include pollen from trees, grasses, and weeds (seasonal allergies), dust mites, pet dander, mold spores, and cockroaches (perennial allergies).
How is allergic rhinitis diagnosed?
Diagnosis
Diagnosis involves a medical history review, physical examination, and possibly allergy testing (skin prick test or blood test) to identify specific allergens triggering the symptoms.
What are the treatment options for allergic rhinitis?
Treatment
Treatment options include allergen avoidance, over-the-counter or prescription antihistamines, decongestants, nasal corticosteroids, leukotriene modifiers, and immunotherapy (allergy shots).
Can homeopathy really help with allergic rhinitis?
Yes!
Homeopathy has a long history of successfully treating allergic rhinitis. It works by stimulating the body’s own healing abilities to reduce sensitivity to allergens and alleviate symptoms like sneezing, itching, and congestion.
Is homeopathy safe for allergic rhinitis?
Yes,
homeopathic remedies are prepared through a process of extreme dilution, making them safe for people of all ages, including pregnant and breastfeeding women. There are no known side effects or interactions with conventional medications.
