Bronchiectasis
Definition
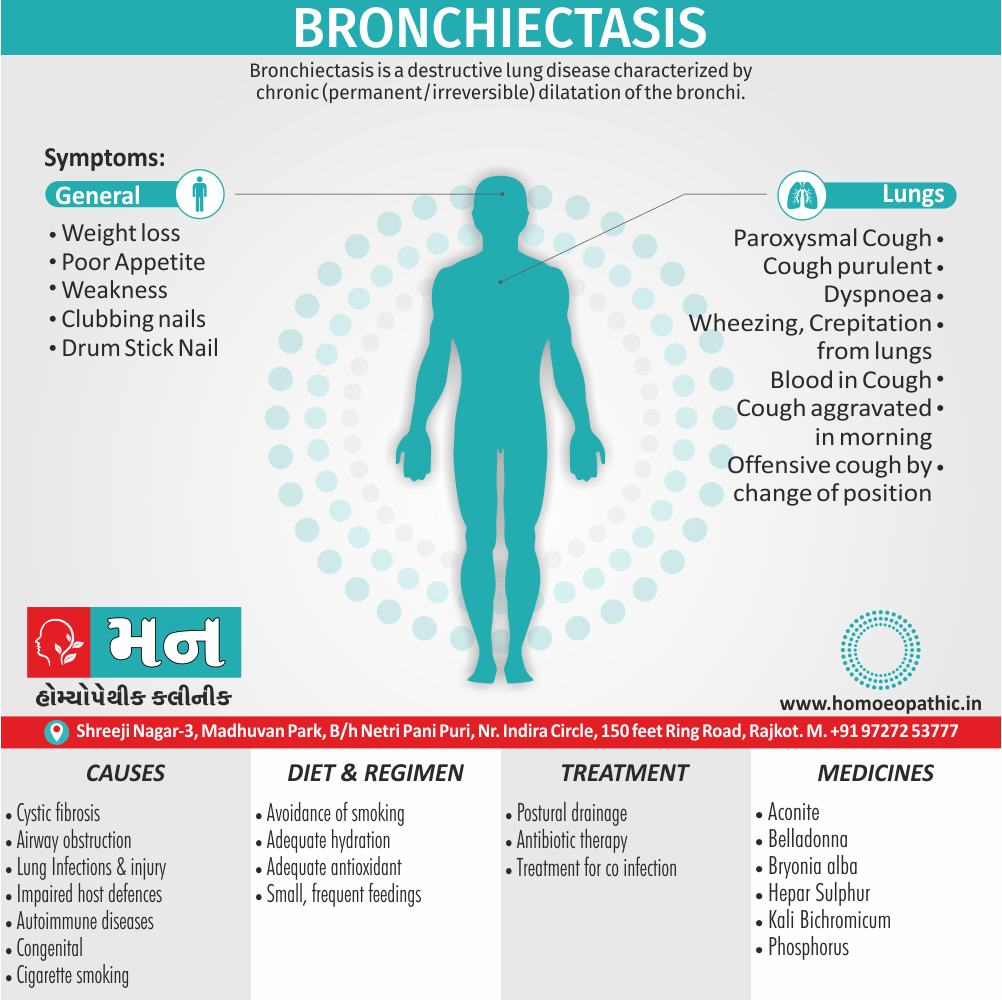
Bronchiectasis a destructive lung disease characterized by chronic (permanent/irreversible) dilatation of the bronchi associated with persistent though variable inflammatory process in the lungs.
Bronchiectasis, unfortunately, doesn’t have any true synonyms in the medical field. It’s a specific lung condition with a unique set of characteristics.
However, depending on the context, here are some related terms you could consider:
- Chronic bronchial dilatation: This is a more descriptive term that explains the chronic nature of the condition and the widening of the airways.
- Cylindrical bronchiectasis, saccular bronchiectasis, varicose bronchiectasis: These are specific types of bronchiectasis based on the appearance of the widened airways.
Important Considerations:
- In a medical setting, "bronchiectasis" is the most precise and widely understood term.
- When discussing the condition in a general context for someone with medical knowledge, "chronic bronchial dilatation" might be an option.
- Avoid using overly simplified terms that might not accurately represent the condition.
Additionally:
- You could describe the symptoms of bronchiectasis, such as "a chronic cough with mucus production." However, this wouldn’t be a synonym for the condition itself.
Remember, clarity and accuracy are crucial when discussing medical conditions. "Bronchiectasis" is the most precise term for most contexts.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Bronchiectasis
The disease affects between 1 per 1000 and 1 per 2,50,000 adults. Moreover, the disease is more common in women and increases as people age. Additionally, Cystic fibrosis identify as a cause in up to half of cases. Bronchiectasis without CF is known as non-CF bronchiectasis. Lastly, Historically, about half of all case of non-CF bronchiectasis were found to be idiopathic, or without a known cause. [1]
Epidemiology
Epidemiology:
The Indian Bronchiectasis Registry (EMBARC-India), established in 2015 in collaboration with the European Multicentre Bronchiectasis Audit and Research Collaboration, provides valuable data on the characteristics and natural history of bronchiectasis in India.
Key findings from the EMBARC-India registry published in 2022 include:
- High Prevalence: Bronchiectasis is a significant health problem in India.
- Distinct Phenotypes: Besides aetiological phenotypes, the study identified distinct ‘frequent exacerbator’ and ‘Pseudomonas aeruginosa’ phenotypes.
- Severity: Indian patients wereyounger and showed greater disease severity, higher prevalence of ‘frequent exacerbators’ and ‘P. aeruginosa’ phenotypes compared to European cohorts.
- Management Gaps: There were significant gaps in adherence to guideline-based bronchiectasis management. [9]
Causes
Causes
In detail, there are many causes that can induce or contribute to the development of bronchiectasis. The frequency of these different causes varies with geographic location. Additionally, Cystic fibrosis identifies as a cause in up to half of cases. Bronchiectasis without CF is known as non-CF bronchiectasis. Historically, about half of all case of non-CF bronchiectasis were found to be idiopathic, or without a known cause. However, more recent studies with a more thorough diagnostic work-up have found an etiology in 60 to 90% of patients.
Cystic fibrosis
Cystic fibrosis is the most common life-threatening autosomal recessive disease in the United States and Europe. It is a genetic disorder that affects the lungs, but also the pancreas, liver, kidneys, and intestine. In general, It cause by mutations in the CFTR protein, a chloride channel expressed in epithelial cells. Lung disease results from clogging of the airways due to mucus build-up, decreased muco-ciliary clearance, also resulting inflammation. In later stages, changes to the structure of the lung, such as bronchiectasis, occur. Around 5 to 10% of all patients with cystic fibrosis develop bronchiectasis.
Airway obstruction
An airway obstruction can cause by either an intraluminal mass such as a tumor or a foreign body. Furthermore, the presence of an airway obstruction leads to a cycle of inflammation. It is important to identify the presence of an obstruction because surgical resection is often curative if obstruction is the cause. In adults, foreign body aspiration often associate with an altered state of consciousness. The foreign body often unchewed food, or part of a tooth or crown. In conclusion, Bronchiectasis that results from foreign body aspiration generally occurs in the right lung in the lower lobe or posterior segments of the upper lobe.
Lung infections
A range of bacterial, mycobacterial, also viral lung infections are associated with the development of bronchiectasis. Bacterial infections commonly associated with bronchiectasis i.e. P. aeruginosa, H. influenzae, and S. pneumoniae. Gram-negative bacteria more commonly implicate than gram-positive bacteria. A history of mycobacterial infections such as tuberculosis can lead to damage of the airways that predisposes to bacterial colonization. In brief, Severe viral infections in childhood can also lead to bronchiectasis through a similar mechanism. Nontuberculous mycobacteria infections such as Mycobacterium avium complex found to be a cause in some patients. Lastly, Recent studies have also shown Nocardia infections to implicated in bronchiectasis.
Impaired host defences
Impairments in host defenses that lead to bronchiectasis may be congenital, such as with primary ciliary dyskinesia, or acquired, such as with the prolonged use of immunosuppressive drugs. Additionally, these impairments may localized to the lungs, or systemic throughout the body. In these states of immunodeficiency, there a weakened or absent immune system response to severe infections that repeatedly affect the lung and eventually result in bronchial wall injury. HIV/AIDS an example of an acquired immunodeficiency that can lead to the development of bronchiectasis.
Aspergillosis
Allergic bronchopulmonary aspergillosis (ABPA) an inflammatory disease caused by hypersensitivity to the fungus Aspergillus fumigatus. It suspected in patients with a long history of asthma also symptoms of bronchiectasis such as a productive, mucopurulent cough. Imaging often shows peripheral and central airway bronchiectasis, which unusual in patients with bronchiectasis caused by other disorders.
Autoimmune diseases
Several autoimmune diseases have associated with bronchiectasis. Specifically, individuals with rheumatoid arthritis and Sjogren syndrome have increased rates of bronchiectasis. In these diseases, the symptoms of bronchiectasis usually present later in the disease course. Other autoimmune diseases such as ulcerative colitis and Crohn’s disease also have an association with bronchiectasis. Additionally, graft-versus-host disease in patients who have underwent stem cell transplantation can lead to bronchiectasis as well.
Lung injury
Bronchiectasis could caused by: inhalation of ammonia and other toxic gases, chronic pulmonary aspiration of stomach acid from esophageal reflux or a hiatal hernia.
Congenital
Bronchiectasis may result from congenital disorders that affect either cilia motility or ion transport. A common genetic cause cystic fibrosis, which affects chloride ion transport. Another genetic cause is primary ciliary dyskinesia, a rare disorder that leads to immotility of cilia and can lead to situs inversus. When situs inversus accompanied by chronic sinusitis and bronchiectasis, this known as Kartagener’s syndrome. Other rare genetic causes include Young’s syndrome and Williams-Campbell syndrome.
Tracheobronchomegaly, or Mourner-Kuhn syndrome a rare condition characterize by significant tracheobronchial dilation and recurrent lower respiratory tract infections. Individuals with alpha 1-antitrypsin deficiency have found to be particularly susceptible to bronchiectasis, due to the loss of inhibition to enzyme elastase which cleaves elastin. This decreases the ability of the alveoli to return to normal shape during expiration.
Cigarette smoking
A causal role for tobacco smoke in bronchiectasis has not demonstrated. Nonetheless, tobacco smoking worse pulmonary function and accelerate the progression of disease that is already present
Types
Types
1. Cystic Fibrosis Bronchiectasis (CFB):
- Cystic fibrosis (CF) is a genetic condition that causes thick, sticky mucus to build up in the patient’s lungs, resulting in repeated pulmonary infections. Like bronchiectasis, each cycle of inflammation and infection further damages the bronchi, causing patients to exhibit signs of bronchiectasis. According to the Cystic Fibrosis Foundation, there are more than 30,000 people living with CF in the United States today.
2. Non-Cystic Fibrosis Bronchiectasis (NCFB):
- Patients can also develop bronchiectasis outside of CF. For instance, if a patient is living with COPD (chronic obstructive pulmonary disease); has damaged cilia (tiny hair-like structures inside the bronchial tube that help clear mucus in the lungs); experiences asthma; or has impaired muscular and nervous system functions that prevent them from clearing mucus naturally, they may develop bronchiectasis-related symptoms.(5)
- Reid categorized bronchiectasis as having three main phenotypes:
- 1) tubular characterized by smooth dilation of the bronchi.
- 2) varicose in which the bronchi are dilated with multiple indentations; and
- 3) cystic in which dilated bronchi terminate in blind ending sacs.
Risk Factors
Risk factors
- Cystic fibrosis, which causes almost half of the cases of bronchiectasis in the United States.
- Immunodeficiency disorders, such as common variable immunodeficiency and, less often, HIV and AIDS.
- Allergic bronchopulmonary aspergillosis, which is an allergic reaction to a fungus called aspergillus that causes swelling in the airways.
- Disorders that affect cilia function, such as primary ciliary dyskinesia, can cause bronchiectasis. Cilia are small, hair-like structures that line your airways. They help clear mucus (a slimy substance) out of your airways.
- Chronic (long-term) pulmonary aspiration, which can inflame the airways
- Connective tissue diseases, such as rheumatoid arthritis, Sjögren’s syndrome external link, and Crohn’s disease. (4)
Pathogenesis
Pathogenesis:
The pathogenesis of bronchiectasis involves a vicious cycle of infection, inflammation, and structural damage to the airways.
Here’s an explanation from a reputable medical source:
"Bronchiectasis results from a cycle of infection and inflammation, leading to progressive airway destruction and remodeling. The process begins with an initial insult to the airways, such as infection, aspiration, or airway obstruction. This triggers an inflammatory response, leading to the recruitment of neutrophils and other inflammatory cells. These cells release proteases and other inflammatory mediators that damage the bronchial wall and impair mucociliary clearance. The impaired clearance leads to mucus accumulation, which further promotes bacterial colonization and perpetuation of the cycle."
Additionally:
- The vicious cycle: The damaged bronchial walls become dilated and deformed, creating pockets where mucus and bacteria can accumulate. This leads to further inflammation and damage, perpetuating the cycle.
- Key mediators: Neutrophils play a crucial role in the pathogenesis of bronchiectasis by releasing proteases that degrade the structural components of the bronchial wall.
- Other factors: Additional factors that can contribute to the development of bronchiectasis include impaired host defense mechanisms, genetic predisposition, and environmental exposures. [10]
Please note: This is a simplified explanation of a complex process. The pathogenesis of bronchiectasis can vary depending on the underlying cause and individual patient factors.
Pathophysiology
Pathophysiology of Bronchiectasis
The diagnostic feature of bronchiectasis dilate bronchi. The Reid classification differentiates between pathological and radiological appearances of bronchiectasis.
Cylindrical bronchiectasis i.e.
- Bronchial dilatation is mild and the bronchi retain their regular relatively straight outline.
- Varicose bronchiectasis
- Bronchial dilatation is greater and local constrictions are present, giving the airway an irregular appearance.
Saccular/cystic bronchiectasis i.e.
–is the most severe form and characterize by large areas of distal ‘grape-like’ bronchial dilatation and loss of bronchial subdivision.
Atelectatic bronchiectasis i.e.
-is a localized form related to proximal bronchial distortion or occlusion.
Clinical Features
The Clinical Features:
Cardinal Symptoms:
- Chronic cough: Persistent cough is the most common symptom and is usually productive of mucopurulent sputum.
- Sputum production: Daily production of thick, often discolored (yellow or green) sputum is characteristic.
- Hemoptysis: Coughing up blood can occur due to airway inflammation and fragility.
Additional Symptoms:
- Dyspnea (shortness of breath): This can vary in severity depending on the extent of lung involvement.
- Wheezing and chest tightness: These can occur due to airway obstruction and inflammation.
- Recurrent respiratory infections: Individuals with bronchiectasis are prone to frequent infections due to impaired mucociliary clearance.
- Fatigue and weight loss: These can be signs of chronic infection and inflammation.
Physical Examination Findings:
- Crackles on auscultation: Crackles (rales) are often heard over the affected lung areas due to secretions in the airways.
- Digital clubbing: This is a painless enlargement of the fingertips and toes and is a sign of chronic lung disease.
Other Clinical Features:
- Exacerbations: Acute worsening of symptoms, often triggered by respiratory infections.
- Sinusitis and rhinosinusitis: These conditions are often associated with bronchiectasis due to similar underlying mechanisms.
Please note: The clinical presentation of bronchiectasis can vary depending on the underlying cause, the extent of lung involvement, and individual patient factors. Some individuals may have mild symptoms, while others may experience more severe complications. [11]
Sign & Symptoms
Sign & Symptoms
Bronchitis i.e.
Attacks of recurrent bronchitis, more common in winter. Clubbing of fingers diagnostic.
Hemorrhagic (bronchiectasis sicca) –
Recurrent hemoptysis with good health in-between, or attacks of bronchitis.
Suppurative –
For instances; Chronic cough, copious purulent expectoration, general toxemia, clubbing of fingers varying from slight parrot beak curvature of finger nails to bulbous drum stick enlargement (pulmonary osteoarthropathy).
During exacerbations, Dyspnoea and wheezing occur in 75% of patients and pleuritic chest pain in 50%. Pleuritic chest pain cause by distended peripheral airways and inflammation adjacent to the visceral pleura. Pyrexia rare during exacerbations; if it is present, pneumonia should exclud.
With relatively rapid onset –
Symptoms developing with comparative suddenness, as a sequel to partial bronchial obstruction by a foreign body or after anesthesia. In early stages paroxysmal cough with occasional offensive sputum which may provoke by change of position. Later large amounts of foetid sputum. Signs mostly limited to auscultation and depend on the size of the affected bronchi, patency of the airways and viscosity of secretions. There may signs of (a) bronchitis, or (b) fibrosis, or (c) consolidation, or (d) collapse, or (e) of cavitation’s.
Early stages –
Fine crackles or sticky rhonchi and slight alteration in character of breath sounds.
Late stages –
Bronchial breathing, coarse crept and perhaps signs of a cavity. Changing character of physical signs after a long bout of cough when air entry may become louder and bronchial in character or from day to day. Sharp metallic or “leathery” rales characteristic. Recurrent pneumonia in the same area of the lung classically associate with bronchiectasis. [1]
Clinical Examination
Clinical examination of Bronchiectasis
Subjective assessment:
- History of childhood infection or childhood respiratory symptoms
- Family history of bronchiectasis, especially cystic fibrosis
Smoking history - Presence of symptoms to suggest a systemic inflammatory disorder (joint problems, skin rash, muscle pain)
- Duration and severity of symptoms
- Frequency of infective exacerbations.
· Objective clinical examination:
- Peripheral examination for signs of chronic lung disease e.g nail changes (clubbing) occur in some forms of bronchiectasis
- Cough quality, strength and sputum production
- Signs to suggest a systemic inflammatory disorder (joints, skin, muscles, eyes)
- Listening to the chest. Bronchiectasis is characterised by focal or generalised noises (crepitations, wheeze) heard with the stethoscope. (6)
Diagnosis
Diagnosis of Bronchiectasis
SPUTUM EXAMINATION –
To exclude diagnosis of underlying pulmonary tuberculosis. Culture and sensitivity of infecting organism as a guide to chemotherapy.
RADIOLOGY:
Sinus radiographs – for chronic sinusitis.
Chest radiography – for changes suggestive or associated with the diagnosis.
Collapse (either segmental or lobar)
Crowding of pulmonary vessels, indicating area of damage or consolidation that may become infected. • ‘Tramline shadows’ suggesting bronchial wall oedema.
Cystic lesions suggesting saccular bronchiectasis
Evidence of previous tuberculosis.
Evidence of previous heart surgery.
HRCT–
High-resolution CT has replaced bronchography and is the preferred investigation. CT findings include the following: – The ‘signet ring’ sign (end-on dilated bronchi that are larger than the accompanying pulmonary artery) seen in all form of bronchiectasis
Tramlines (in other words, non-tapering bronchi) seen in cylindrical bronchiectasis – Varicose bronchiectasis has a beaded (tree-imbued) appearance – ‘Cysts’ with air-fluid levels in dilated bronchi characteristic of cystic bronchiectasis SPIRAL CT may aid diagnosis by reducing motion artefact and identifying subtle bronchiectatic changes.
SPECIAL INVESTIGATIONS:
may indicate the cause of bronchiectasis in some patients.
Immunoglobulins –
Most patients with bronchiectasis have raised plasma concentrations of immunoglobulins (especially IgA).
Aspergillus precipitins –
Recurrent mucus plugging of major airways and development of proximal bronchiectasis occurs in allergic bronchopulmonary aspergillosis.
Barium studies –
For gastro-esophageal reflux, since association of basal bronchiectasis is well recognized.
a1-antitrypsin deficiency associate with premature pulmonary emphysema though rarely in association with bronchiectasis.
Detection of cystic fibrosis –
By sweat test and/or genetic analysis
Differential Diagnosis
Differential diagnosis of Bronchiectasis
- COPD
- Asthma
- Pneumonia
- Tuberculosis
- Chronic sinusitis
- Lung cancer
- Postnasal drip
- Inhaled foreign body. (7)
Complications
Complications of bronchiectasis
Investigations
Investigations:
The following investigations are recommended for diagnosing and evaluating bronchiectasis, as outlined in a reputable medical source:
Imaging:
- High-resolution computed tomography (HRCT): The gold standard for diagnosing bronchiectasis. It can visualize the characteristic bronchial wall thickening, airway dilation, and mucus plugging.
- Chest X-ray: May show nonspecific findings like increased bronchovascular markings or atelectasis, but it is less sensitive than HRCT.
Microbiology:
- Sputum culture: Identifies the bacteria or other pathogens causing the infection in the airways.
- Blood tests: May be used to look for signs of inflammation or infection.
Pulmonary Function Tests (PFTs):
- Spirometry: Assesses lung function and can detect airflow obstruction, which is common in bronchiectasis.
- Lung volumes: Measures the total lung capacity and residual volume, which can be increased in severe cases.
Additional Investigations:
- Bronchoscopy: May be performed to visualize the airways directly, obtain samples for culture, or remove mucus plugs.
- Immunologic tests: May be indicated to assess for underlying immune deficiencies or connective tissue disorders that can predispose to bronchiectasis.
- Genetic testing: May be considered in cases with a suspected genetic cause, such as cystic fibrosis.[12]
Please note: The specific investigations recommended for a patient with suspected or confirmed bronchiectasis will depend on the individual’s clinical presentation, medical history, and the suspected underlying cause. Always consult with a healthcare professional for appropriate guidance on diagnosis and management.
Treatment
Treatment of Bronchiectasis
Postural drainage–
Since bronchiectasis usually affects the lower lobes the prone position with the head tilted downwards is the most useful. Deep breathing or coughing, assisted by percussion of the affected part (clapping) helps to dislodge the secretions. It should carried out at least twice daily for 15–20 minutes at a time. Expectoration facilitate by cough mixtures, or better inhalation of nebulized bronchodilator isoproterenol followed by inhalation of nebulized water or steam, followed by postural drainage. This should done on arising in the morning since the patient with bronchiectasis tends to pool secretions during the night. [1]
Antibiotic therapy –
Antibiotics can delay progression in patients with cystic fibrosis. Antibiotics penetration into the bronchial mucosa and secretions impair and the dose needs to be higher and duration longer. H. influenzae, H. parainfluenza, Str. pneumonia and Moraxella catarrhalis are the most common organisms in exacerbations,
- β-lactam antibiotics (e.g. amoxicillin 500 mg t.d.s. for 10–14 days) remain the first line therapy.
- Alternatives include quinolones and macrolides. Chronic colonization with Ps. aeruginosa is common in severe disease.
- Choice of antibiotic guide by sensitivities, but oral quinolones (e.g. ciprofloxacin 500 mg b.d. for 2 weeks) is the first time therapy. Development of resistance is common, and iv antibiotics e.g. ceftadizime 2 g t.d.s. for 14 days, gentamicin (in accordance with plasma levels), and piperacillin 4.5 g t.d.s. for 14 days require. Nebulized antibiotics allow maximal concentrations of antibiotics in the airways with reduced systemic effects. Amoxicillin 500 mg b.d., gentamicin 80 mg b.d., and tobramycin solution for inhalation 300 mg b.d. can be used.
Acute exacerbations –
Hospitalization in all severely ill patients, when chest pain limits coughing and sputum clearance (this increases risk of pneumonia) and iv antibiotics are required.
Prophylactic therapy –
One guideline for therapy is when there are exacerbations every 2 months that prevent participation in normal activities of 2 weeks or more during the exacerbation. Continuous therapy considere in patients who persistently expectorate purulent sputum. Aggressive treatment warrant because persistent infection causes tissue destruction. Bilateral lung transplantation has use when respiratory failure develops despite optimal medical management.
Intravenous immunoglobulin replacement
Intravenous immunoglobulin replacement thought to be effective in pan hypogammaglobulinemia, but given only to patients with established, widespread lung damage.
α-antitrypsin replacement therapy by inhaled route has the potential to neutralize damaging processes that are released as part of the airways inflammatory response.
General supportive treatment – (a) Adequate nutrition. (b) Eradication of chronic nocturnal post-nasal discharge and treatment of sinusitis. (c) Avoidance of smoking. (d) Adequate hydration
Complications of bronchiectasis
Pulmonary – recurrent pneumonia, lung abscess, haemoptysis
Pleural – pleurisy, pleural effusion or empyema Corpulmonale Cerebral abscess Amyloidosis Seronegative arthropathy. [1]
Prevention
Prevention of Bronchiectasis
Bronchiectasis is a long-term condition with symptoms that need to be managed over many years. Patients should work closely with a doctor to determine healthy habits that will limit flare-ups. Some suggestions may be:
- Quit smoking and avoid secondhand smoke.
- Maintain a healthy diet, low in sodium, added sugars, saturated fats and refined grains.
- Stay hydrated, drinking plenty of water to help prevent mucus build-up.
- Be diligent about taking oral and inhaled medications and performing mucus clearance techniques daily.
- Staying up to date on vaccinations.
- Take antibiotics for one to two weeks during flare-ups.
- Despite maintaining a healthy lifestyle, occasional flare-ups may occur . This often happens because of a new respiratory infection or overgrowth of bacteria. Symptoms such as increased mucus (sputum) production that is bloody or a different color, fever, fatigue, weight loss and worsening shortness of breath may be a sign you’re experiencing a flare-up. In these instances, you should contact your doctor immediately. (8)
Homeopathic Treatment
Homoeopathic treatment
Homeopathic Treatment of Bronchiectasis
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Bronchiectasis:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
1. ACONITUM NAPELLUS:
The first remedy that is often indicated at the onset of the infection. It is effective only within the first twenty four hours. Useful when there is a short, dry cough, a temperature and an irritation of the throat, chest and trachea. The cause is usually exposure to cold. There is a chilly restlessness, anxiety and a full, bounding pulse, with general weakness.
2. ANTIMONIUM TARTARICUM:
Useful when there is a accumulation of considerable loose, rattling, moist mucus in the chest. For children breathing and a loose cough, but little phlegm is expectorated. There may be vomiting and laboured breathing. Pronounced physical and mental exhaustion.
3. BELLADONNA:
A high temperature, dry cough, a pounding, pulsating headache and a flushed face with a dry, hot skin. The cough is worse at night and when lying down.[2]
4. BRYONIA ALBA:
A painful, violent, dry, stitching cough with a headache and pain in the chest wall. Worse with coughing and better when supporting the area with both hands. The expectoration is yellow and often blood streaked. The cough is worse after meals. Patient drinks large quantities of fluids at long intervals.
5. KALI BICHROMIUM:
For less acute cases. The phlegm is tough, thick and stringy and cannot easily be expectorated. There is a tightness of the chest and a troublesome cough.
Worse in the evenings. (about 4 pm to 5 pm).
6. PHOSPHORUS:
Useful for tall, pale patients with little natural resistance. They are bright-eyed, very anxious and need constant reassurance. Breathing is often difficult with wheezing; with a dry, tickling cough and a sore chest. Worse when talking and in fresh air.
7. BACILLINUM:
Repeated infections.[2]
Diet & Regimen
Diet & Regimen of Bronchiectasis
- Use a diet with 1.0–1.25 g protein/kg and sufficient calories to meet elevated metabolic requirements appropriate for age and sex.
- Small, frequent feedings may better tolerate.
- Fluid intake of 2–3 L daily may offer, unless contraindicated.
- Intravenous fat emulsions may indicate (eicosanoids are inflammatory modulators, and thromboxane and leukotrienes tend to be potent mediators of inflammation). Omega-3 fatty acids should enhance in the oral diet by including salmon, tuna, sardines, walnuts, and flaxseed. Supplements may also useful.
- Adequate antioxidant use with vitamins C and E and selenium may beneficial. Ensure adequate potassium intake, depending on medications used.[3]
Do’s and Don'ts
Do’s and Don’ts
Here are some do’s and don’ts for managing bronchiectasis, based on recommendations from a reputable medical source:
Do’s:
- Do practice good airway clearance techniques: Regularly perform techniques like postural drainage, percussion, and positive expiratory pressure (PEP) devices to help clear mucus from the airways.
- Do adhere to prescribed medications: Take antibiotics, bronchodilators, and other medications as directed by your doctor.
- Do get vaccinated: Stay up-to-date on vaccinations for influenza, pneumococcus, and COVID-19 to reduce the risk of infections.
- Do maintain a healthy lifestyle: Eat a balanced diet, exercise regularly, get enough sleep, and avoid smoking and secondhand smoke.
- Do seek medical attention for exacerbations: Promptly contact your doctor if you experience a worsening of symptoms, such as increased cough, sputum production, or shortness of breath.
- Do consider pulmonary rehabilitation: This program can help improve your exercise capacity, lung function, and quality of life.
Don’ts:
- Don’t smoke or be exposed to secondhand smoke: Smoking is a major risk factor for bronchiectasis and can worsen symptoms.
- Don’t ignore respiratory infections: Promptly treat any respiratory infections to prevent them from worsening and triggering exacerbations.
- Don’t neglect airway clearance: Skipping airway clearance techniques can lead to mucus buildup and increased risk of infection.
- Don’t hesitate to seek medical advice: If you have any concerns about your condition or treatment, talk to your doctor.
- Don’t be exposed to air pollution or irritants: Avoid exposure to environmental triggers that can worsen symptoms, such as dust, fumes, and strong odors.[13]
Remember: These are general guidelines, and your individual treatment plan may vary depending on the severity of your condition and other factors. Always consult with your doctor for personalized advice on managing bronchiectasis.
Terminology
Terminology:
Homeopathic Terminology
- Miasmatic Tendency: This refers to the concept of inherited predispositions or tendencies towards certain disease patterns. Homeopaths believe that understanding a person’s miasm can guide treatment selection.
- Constitutional Indications: These are the physical, mental, and emotional characteristics of an individual that are considered when choosing a homeopathic remedy.
- Therapeutic Affinity: This means a remedy’s specific attraction or relationship to certain organs, tissues, or systems in the body.
- Potency: This indicates the strength or dilution of a homeopathic remedy. Higher potencies are believed to have a deeper and longer-lasting effect.
- Repetition of Dose: Refers to how often a homeopathic remedy is taken. This can vary depending on the individual, the remedy, and the severity of the condition.
- Psychosomatic: The idea that the mind (psyche) and body (soma) are interconnected, and emotional or mental factors can influence physical health.
Key Points from the Article
- Holistic Approach: Homeopathy emphasizes treating the whole person, not just the disease. This means considering their physical, mental, and emotional well-being.
- Individualized Treatment: Homeopathic treatment is tailored to the specific symptoms and characteristics of each individual.
- Symptom Picture: The complete set of symptoms a person experiences is crucial in selecting the right homeopathic remedy.
- Remedies: Homeopathic remedies are natural substances (often derived from plants, minerals, or animals) that are highly diluted. They are selected based on their similarity to the patient’s symptoms.
Important Note: The article correctly emphasizes that these remedies are provided for informational purposes only. It’s crucial to consult with a qualified homeopathic practitioner for proper assessment and treatment.
References
References
- Golwalla’s MEDICINE for Students 25th Edition
- Homoeopathic Body-System Prescribing – A Practical Workbook of Sector Remedies
- Nutrition and Diagnosis-Related Care (Nutrition and Diagnosis-Related Care (Escott-Stump)
- https://www.nhlbi.nih.gov/health/bronchiectasis/causes
- https://smartvest.com/blog/understanding-types-bronchiectasis/#:~:text=According%20to%20the%20CHEST%20Foundation,cystic%20fibrosis%20bronchiectasis%20(NCFB)
- https://bronchiectasis.com.au/assessment/medical/clinical-examination
- https://www.google.com/search?q=bronchiectasis+differential+diagnosis&newwindow
- https://www.lung.org/lung-health-diseases/lung-disease-lookup/bronchiectasis/treating-and-managing
- Chalise, P., et al. (2022). Characteristics and Natural History of Bronchiectasis in India: Results From the Indian Bronchiectasis Registry (EMBARC-India). Chest, 162(3), 892-903.
- Harrison’s Principles of Internal Medicine" (20th Edition, 2018)
- Murray and Nadel’s Textbook of Respiratory Medicine" (7th Edition, 2021)
- Fishman’s Pulmonary Diseases and Disorders" (5th Edition, 2015)
- BTS Guideline for Bronchiectasis" (British Thoracic Society, 2019)
Also Search As
Bronchiectasis Also Search As
Online Search Engines:
Google, Bing, DuckDuckGo:
Simply type "bronchiectasis" in the search bar. This will bring up a wide range of articles, websites, and resources on the topic. You can further refine your search by adding specific keywords like "symptoms," "causes," "treatment," or "bronchiectasis in India."
Health and Medical Websites:
Reputable Health Websites:
Many well-known health websites like Mayo Clinic, Cleveland Clinic, WebMD, and Healthline have detailed articles on bronchiectasis. You can search their websites directly or use a search engine with the website name (e.g., "bronchiectasis Mayo Clinic").
Organizations Dedicated to Lung Health:
Look for information on websites like the American Lung Association or the British Lung Foundation. They often have resources specifically tailored to bronchiectasis.
Medical Databases:
PubMed:
This is a database of scientific articles, including many research papers on bronchiectasis. You can use it to find in-depth medical information and studies.
Google Scholar:
Another source for academic articles and research on bronchiectasis.
Libraries:
Public Libraries:
Many public libraries have books and resources on health topics, including bronchiectasis.
Medical Libraries:
If you have access to a medical library (e.g., at a university or hospital), they will have a wider range of specialized resources on bronchiectasis.
Additional Tips:
Use Specific Keywords:
Instead of just searching for "bronchiectasis," use more specific terms to find the information you need. For example, you could search for "bronchiectasis symptoms," "bronchiectasis treatment options," or "bronchiectasis guidelines."
Check Credibility:
Ensure the information you find comes from reliable sources, such as reputable health organizations, medical professionals, or peer-reviewed research articles. Be wary of information from unknown or unverified sources.
There are several ways to search for information on bronchiectasis, depending on the type of information you’re seeking and the resources available to you:
Online Search Engines:
General Search Engines (Google, Bing, DuckDuckGo):
Simply type "bronchiectasis" into the search bar. This will bring up a wide range of articles, websites, and resources related to the topic.
Specialized Search Engines (Google Scholar, PubMed):
These search engines focus on academic and scientific literature. Use them if you need research articles, clinical studies, or scholarly information about bronchiectasis.
Health and Medical Websites:
Reputable Health Websites:
Many organizations and websites provide reliable information on bronchiectasis. Some examples include:
- Mayo Clinic
- Cleveland Clinic
- American Lung Association
- National Heart, Lung, and Blood Institute (NHLBI)
- British Lung Foundation
Websites of Medical Journals:
Journals like the New England Journal of Medicine, The Lancet, and Chest often publish articles about bronchiectasis.
Libraries:
Public Libraries:
Many public libraries have books and resources on health topics, including bronchiectasis.
Medical Libraries:
University or hospital libraries often have a more extensive collection of medical resources, including textbooks, journals, and databases with information on bronchiectasis.
Other Resources:
- Patient Support Groups: Online or in-person support groups for people with bronchiectasis can provide valuable information and connect you with others who share similar experiences.
- Medical Professionals: Consult with your doctor or a pulmonologist for personalized information and recommendations about bronchiectasis.
Tips for Effective Searching:
- Use specific keywords: Instead of just searching for "bronchiectasis," try using more specific terms like "bronchiectasis causes," "bronchiectasis treatment," or "bronchiectasis living with."
- Combine keywords: Use Boolean operators like AND, OR, and NOT to refine your search. For example, "bronchiectasis AND cystic fibrosis" will find articles that discuss both conditions.
- Check the date of publication: Ensure the information is up-to-date, as medical knowledge and treatments can evolve.
- Evaluate the source: Be sure to use reliable sources, such as reputable health organizations, medical journals, and healthcare professionals.
- Read multiple sources: Don’t rely on just one article or website. Gather information from various sources to get a comprehensive understanding of bronchiectasis.
By using these various methods, you can find a wealth of information on bronchiectasis to learn about its causes, symptoms, diagnosis, treatment, and management.
Frequently Asked Questions (FAQ)
What is Bronchiectasis?
Bronchiectasis is a destructive lung disease characterized by chronic (permanent/irreversible) dilatation of the bronchi associated with persistent though variable inflammatory process in the lungs.
What are the symptoms of bronchiectasis?
Common symptoms include:
- Persistent cough with thick mucus (often yellow or green)
- Shortness of breath, especially during physical activity
- Wheezing or chest tightness
- Frequent respiratory infections
- Fatigue and weight loss
What causes bronchiectasis?
Several factors can contribute to its development, including:
- Recurrent lung infections
- Cystic fibrosis
- Immune system disorders
- Blockages in the airways
- Aspiration of foreign objects
Can bronchiectasis be cured?
There is no cure for bronchiectasis, but it can be effectively managed with treatment to improve symptoms, reduce flare-ups, and prevent complications.
Can bronchiectasis be prevented?
While not always preventable, you can reduce your risk by:
- Getting vaccinated against respiratory infections
- Managing underlying lung conditions
- Avoiding smoking and secondhand smoke
- Practicing good hygiene to prevent infections
Can homeopathy help with bronchiectasis?
Yes, homeopathy can offer supportive care for bronchiectasis by addressing the underlying causes of the condition and managing its symptoms. While it’s not a replacement for conventional medicine, homeopathy can work alongside it to improve overall well-being.
Which homeopathic remedies are commonly used for bronchiectasis?
The choice of remedy depends on individual symptoms and underlying causes. Some commonly used remedies include:
- Pulsatilla: For thick, yellow-green mucus and emotional sensitivity.
- Antimonium tartaricum: For rattling cough with difficulty expectorating mucus.
- Phosphorus: For bleeding tendencies, hoarseness, and chest tightness.
- Kali bichromicum: For stringy, sticky mucus and sinusitis.
- Carbo vegetabilis: For extreme fatigue and difficulty breathing.
Always consult with a qualified homeopath for a proper assessment and personalized treatment plan.
How does homeopathy work for bronchiectasis?
Homeopathy aims to stimulate the body’s innate healing abilities to address the root causes of the condition. Remedies are selected based on the individual’s unique symptom picture.
What are the benefits of using homeopathy for bronchiectasis?
Homeopathy may help:
- Reduce the frequency and severity of exacerbations
- Improve mucus clearance and cough
- Boost the immune system
- Enhance overall respiratory health
- Address emotional and mental well-being related to the condition
Can I use homeopathy alongside conventional treatments for bronchiectasis?
Yes, homeopathy can be used as a complementary therapy alongside conventional treatments. Discuss with your healthcare providers to ensure there are no interactions or contraindications.
