Pneumonia
Definition
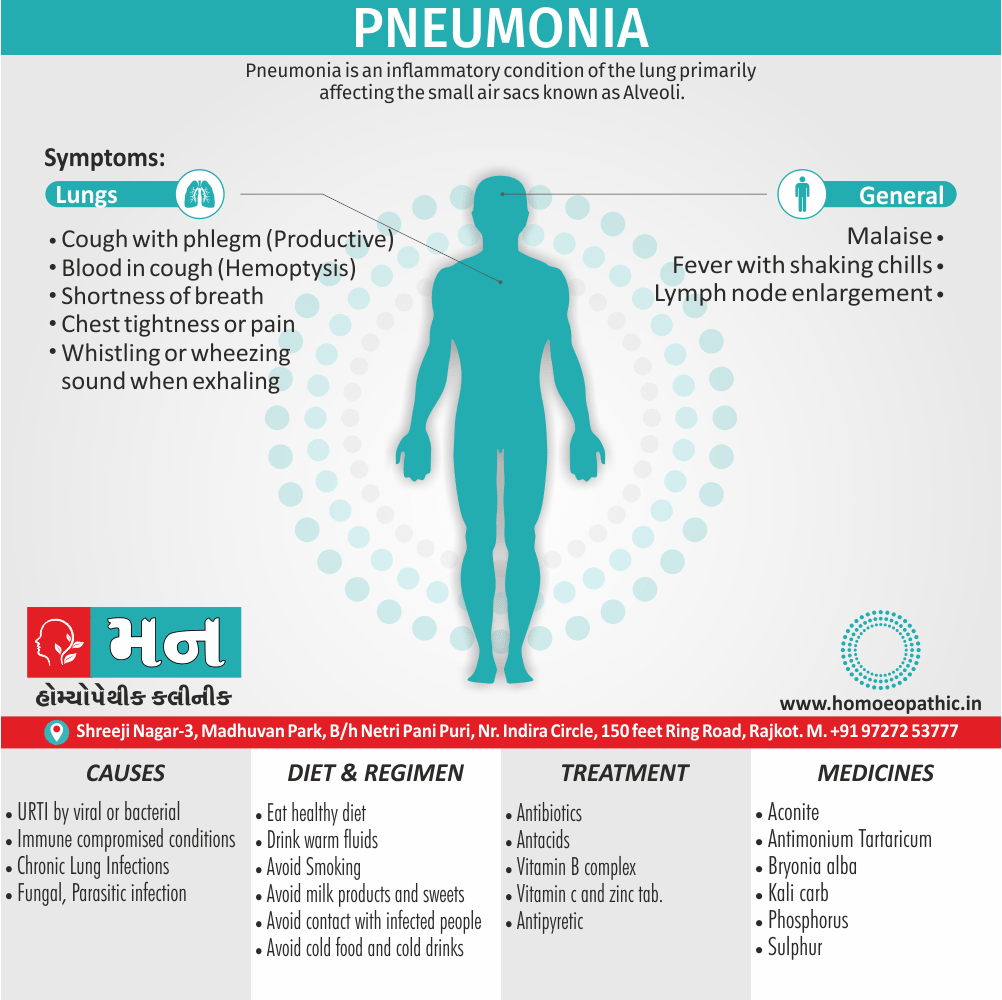
Pneumonia is an inflammatory condition of the lung primarily affecting the small air sacs known as alveoli.[1]
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
Pneumonia is usually caused by infection with viruses or bacteria, and less commonly by other microorganisms. Identifying the responsible pathogen can be difficult. Diagnosis is often based on symptoms and physical examination. Chest X-rays, blood tests, and culture of the sputum may help confirm the diagnosis. The disease may be classified by where it was acquired, such as community- or hospital-acquired or healthcare-associated pneumonia.
Each year, pneumonia affects about 450 million people globally (7% of the population) and results in about 4 million deaths. With the introduction of antibiotics and vaccines in the 20th century, survival has greatly improved. Nevertheless, pneumonia remains a leading cause of death in developing countries, and also among the very old, the very young, and the chronically ill. Pneumonia often shortens the period of suffering among those already close to death and has thus been called "the old man’s friend".[1]
Epidemiology
Epidemiology
- Pneumonia remains a major contributor to illness and death in India, especially among children younger than five. It is estimated that these children experience around 0.28 pneumonia episodes per year, and tragically, 2-3% of these cases result in death.
- When it comes to bacterial pneumonia in Indian children, Streptococcus pneumoniae and Haemophilus influenzae type b (Hib) are the two most prevalent culprits. However, other pathogens like viruses and atypical bacteria also play a role in the overall disease burden.
- The impact of pneumonia in India is not evenly distributed; it’s significantly higher in rural areas and among populations facing socioeconomic challenges. Factors like malnutrition, indoor air pollution, and limited access to healthcare significantly elevate the risk of pneumonia.
References:
Rudan I, et al. Global burden of childhood pneumonia and diarrhoea. Lancet. 2013;381(9875):1405-16. [6]
GBD 2015 Lower Respiratory Infections Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1659-724. [7]
- Walker CLF, et al. Pneumonia in children: causes, risk factors, prevention, and treatment. Lancet. 2013;381(9875):1405-16. [8]
Causes
Causes
[A] Predisposing factors:
Factors that predispose to pneumonia include smoking, immunodeficiency, alcoholism, chronic obstructive pulmonary disease, sickle cell disease (SCD), asthma, chronic kidney disease, liver disease, and biological aging. Additional risks in children include not being breastfed, exposure to cigarette smoke and other air pollution, malnutrition, and poverty. The use of acid-suppressing medications – such as proton-pump inhibitors or H2 blockers – is associated with an increased risk of pneumonia. Approximately 10% of people who require mechanical ventilation develop ventilator-associated pneumonia, and people with a gastric feeding tube have an increased risk of developing aspiration pneumonia. For people with certain variants of the FER gene, the risk of death is reduced in sepsis caused by pneumonia. However, for those with TLR6 variants, the risk of getting Legionnaires’ disease is increased.[2]
[B] Infection:
Bacteria
Bacteria are the most common cause of community-acquired pneumonia (in other words, CAP), with Streptococcus pneumoniae isolated in nearly 50% of cases. Other commonly isolated bacteria include Haemophilus influenzae in 20%, Chlamydophila pneumoniae in 13%, also Mycoplasma pneumoniae in 3% of cases; Staphylococcus aureus; Moraxella catarrhalis; and Legionella pneumophila. A number of drug-resistant versions of the above infections are becoming more common, including drug-resistant Streptococcus pneumoniae (in other words, DRSP) and methicillin-resistant Staphylococcus aureus (MRSA).
spreading of organisms
The spreading of organisms is facilitated by certain risk factors. Alcoholism is associated with Streptococcus pneumoniae, anaerobic organisms, also Mycobacterium tuberculosis; smoking facilitates the effects of Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, and Legionella pneumophila. Additionally, Exposure to birds is associated with Chlamydia psittaci; farm animals with Coxiella burnetti; aspiration of stomach contents with anaerobic organisms; and cystic fibrosis with Pseudomonas aeruginosa and Staphylococcus aureus. Streptococcus pneumoniae is more common in the winter, also it should be suspected in persons aspirating a large number of anaerobic organisms.
Viruses
In adults, viruses account for about one third of pneumonia cases, and in children for about 15% of them. Commonly implicated agents include rhinoviruses, coronaviruses, influenza virus, respiratory syncytial virus (RSV), adenovirus, and parainfluenza. Herpes simplex virus rarely causes pneumonia, except in groups such as newborns, persons with cancer, transplant recipients, and people with significant burns. After organ transplantation or in otherwise immunocompromised persons, there are high rates of cytomegalovirus pneumonia.
secondary infection
Those with viral infections may be secondarily infected with the bacteria Streptococcus pneumoniae, Staphylococcus aureus, or Haemophilus influenzae, particularly when other health problems are present. Different viruses predominate at different times of the year; during flu season, for example, influenza may account for more than half of all viral cases. Outbreaks of other viruses also occur occasionally, including hantaviruses and coronaviruses. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can also result in pneumonia.
Fungi
Fungal pneumonia is uncommon, but occurs more commonly in individuals with weakened immune systems due to AIDS, immunosuppressive drugs, or other medical problems. It is most often caused by Histoplasma capsulatum, Blastomyces, Cryptococcus neoformans, Pneumocystis jiroveci (pneumocystis pneumonia, or PCP), and Coccidioides immitis. Histoplasmosis is most common in the Mississippi River basin, and coccidioidomycosis is most common in the Southwestern United States. The number of cases of fungal pneumonia has been increasing in the latter half of the 20th century due to increasing travel and rates of immunosuppression in the population. For people infected with HIV/AIDS, PCP is a common opportunistic infection.
Parasites
A variety of parasites can affect the lungs, including Toxoplasma gondii, Strongyloides stercoralis, Ascaris lumbricoides, and Plasmodium malariae. These organisms typically enter the body through direct contact with the skin, ingestion, or via an insect vector. Except for Paragonimus westermani, most parasites do not specifically affect the lungs but involve the lungs secondarily to other sites. Some parasites, in particular those belonging to the Ascaris and Strongyloides genera, stimulate a strong eosinophilic reaction, which may result in eosinophilic pneumonia. In other infections, such as malaria, lung involvement is due primarily to cytokine-induced systemic inflammation. In the developed world, these infections are most common in people returning from travel or in immigrants. Around the world, parasitic pneumonia is most common in the immunodeficient.
[C] Noninfectious
Idiopathic interstitial pneumonia or noninfectious pneumonia is a class of diffuse lung diseases. They include diffuse alveolar damage, organizing pneumonia, nonspecific interstitial pneumonia, lymphocytic interstitial pneumonia, desquamative interstitial pneumonia, respiratory bronchiolitis interstitial lung disease, and usual interstitial pneumonia. Lipoid pneumonia is another rare cause due to lipids entering the lung. These lipids can either be inhaled or spread to the lungs from elsewhere in the body.[1]
Types
Types
Pneumonia is most commonly classified by where or how it was acquired:
[A]. community-acquired
[B]. Aspiration
[C]. Healthcare-associated
[D].Hospital-acquired
[E]. Ventilator-associated pneumonia.[1]
Community-acquired pneumonia [CAP]
Community-acquired pneumonia (CAP) acquire in the community, outside of health care facilities. Compared with health care–associated pneumonia, it is less likely to involve multidrug-resistant bacteria. Although the latter are no longer rare in CAP, they are still less likely.[1]
Health care–associated pneumonia (HCAP)
an infection associate with recent exposure to the health care system, including hospitals, outpatient clinics, nursing homes, dialysis centers, chemotherapy treatment, or home care. HCAP sometimes call MCAP (medical care–associated pneumonia).
People may become infected with pneumonia in a hospital; this define as pneumonia not present at the time of admission (symptoms must start at least 48 hours after admission). It likely to involve hospital-acquire infections, with higher risk of multidrug-resistant People in a hospital often have other medical conditions, which may make them more susceptible to pathogens in the hospital.
Ventilator-associated pneumonia [VAP]
occurs in people breathing with the help of mechanical ventilation. Ventilator-associated pneumonia specifically define as pneumonia that arises more than 48 to 72 hours after endotracheal intubation.[1]
It may also classify by the area of the lung affected:
[A]. Lobar pneumonia
[B]. Bronchial pneumonia
[C]. Acute interstitial pneumonia
Pneumonia in children may additionally classify based on signs and symptoms as non-severe, severe, or very severe.
The setting in which pneumonia develops is important to treatment, as it correlates to which pathogens are likely suspects, which mechanisms are likely, which antibiotics are likely to work or fail, and which complications can expect based on the person’s health status [1].
Risk Factors
Risk Factors for Pneumonia
1. Age:
- Infants and young children: Their immune systems are still developing, making them more susceptible to infections.
- Older adults: The immune system weakens with age, increasing the risk of pneumonia.
2. Chronic Diseases:
- Chronic lung diseases: Conditions like COPD (chronic obstructive pulmonary disease) and asthma can make the lungs more vulnerable to infections.
- Heart disease: It can weaken the body’s ability to fight off infections.
- Diabetes: High blood sugar levels can impair the immune system.
- Other chronic conditions: Liver disease, kidney disease, and sickle cell disease can also increase the risk.
3. Lifestyle Factors:
- Smoking: Damages the lungs’ natural defenses against infections.
- Excessive alcohol consumption: Weakens the immune system.
4. Environmental Factors:
- Exposure to air pollution: Irritates the lungs and makes them more susceptible to infection.
- Secondhand smoke: Increases the risk, especially in children.
5. Weakened Immune System:
- HIV/AIDS: Compromises the body’s ability to fight off infections.
- Organ transplant: Requires immunosuppressive medications, increasing the risk.
- Cancer treatment: Chemotherapy and radiation therapy can weaken the immune system.
6. Other Factors:
Pathogenesis
Pathogenesis of Pneumonia
Pneumonia develops when microorganisms overcome the host’s defense mechanisms and establish an infection in the lung parenchyma. The process generally involves the following stages:
Entry of Pathogens:
Microbes can enter the lungs through several routes:
- Inhalation: Most common, with pathogens entering through the respiratory tract.
- Aspiration: Inhalation of oropharyngeal or gastric contents into the lungs.
- Hematogenous spread: From a distant infection site via the bloodstream.
- Direct spread: From an adjacent infected area (e.g., empyema).
Evasion of Host Defenses:
To establish an infection, pathogens must evade various host defense mechanisms:
- Mucociliary clearance: The movement of mucus by cilia that traps and removes inhaled particles.
- Cough reflex: A protective mechanism to expel irritants and secretions.
- Alveolar macrophages: Phagocytic cells that engulf and destroy microorganisms.
- Immune system: Humoral (antibodies) and cellular (T cells) responses.
Colonization and Inflammation:
Pathogens that successfully evade host defenses can adhere to and colonize the respiratory epithelium. This triggers an inflammatory response, leading to:
- Recruitment of neutrophils: Neutrophils migrate to the infection site to phagocytose pathogens.
- Release of inflammatory mediators: Cytokines and chemokines promote inflammation and immune cell activation.
- Fluid accumulation in the alveoli: This impairs gas exchange and can cause respiratory distress.
Consolidation and Resolution:
- Consolidation: In some cases, the affected lung tissue becomes filled with inflammatory exudate (pus), leading to consolidation.
- Resolution: If the infection is controlled, the inflammatory response resolves, and the lung tissue heals. [9]
Pathophysiology
Pathophysiology
Pneumonia fills the lung’s alveoli with fluid, hindering oxygenation. The alveolus on the left is normal, whereas the one on the right is full of fluid from pneumonia.[1]
Mode of infection:
- Droplet infection
- Aspiration
- Blood
- Systemic
Pneumonia frequently starts as an upper respiratory tract infection that moves into the lower respiratory tract. It is a type of pneumonitis (lung inflammation). The normal flora of the upper airway give protection by competing with pathogens for nutrients. In the lower airways, reflexes of the glottis, actions of complement proteins and immunoglobulins are important for protection. Micro-aspiration of contaminated secretions can infect the lower airways and cause pneumonia. The progress of pneumonia is determined by the virulence of the organism; the amount of organism required to start an infection; and the body’s immune response against the infection.
Bacterial
Most bacteria enter the lungs via small aspirations of organisms residing in the throat or nose. Half of healthy people have these small aspirations during sleep. While the throat always contains bacteria, potentially infectious ones reside there only at certain times and under certain conditions. A minority of types of bacteria such as Mycobacterium tuberculosis and Legionella pneumophila reach the lungs via contaminated airborne droplets.
Bacteria can also spread via the blood. Once in the lungs, bacteria may invade the spaces between cells and between alveoli, where the macrophages and neutrophils (defensive white blood cells) attempt to inactivate the bacteria. The neutrophils also release cytokines, causing a general activation of the immune system. This leads to the fever, chills, and fatigue common in bacterial pneumonia. The neutrophils, bacteria, and fluid from surrounding blood vessels fill the alveoli, resulting in the consolidation seen on chest X-ray.[1]
Viral
Viruses may reach the lung by a number of different routes. Respiratory syncytial virus is typically contracted when people touch contaminated objects and then they touch their eyes or nose. Other viral infections occur when contaminated airborne droplets are inhaled through the nose or mouth. Once in the upper airway, the viruses may make their way into the lungs, where they invade the cells lining the airways, alveoli, or lung parenchyma. Some viruses such as measles and herpes simplex may reach the lungs via the blood.
Lung invasion
The invasion of the lungs may lead to varying degrees of cell death. When the immune system responds to the infection, even more lung damage may occur. Primarily white blood cells, mainly mononuclear cells, generate the inflammation. As well as damaging the lungs, many viruses simultaneously affect other organs and thus disrupt other body functions. Viruses also make the body more susceptible to bacterial infections; in this way, bacterial pneumonia can occur at the same time as viral pneumonia.[1][2]
Clinical Features
Clinical Features of Pneumonia
The presentation of pneumonia can vary depending on factors like the causative agent, the patient’s age and overall health, and the severity of the infection. However, some common clinical features include:
- Cough: Often productive, with sputum that may be clear, yellow, green, or even blood-tinged.
- Fever: Typically present, but may be absent in older adults or immunocompromised individuals.
- Chills: Shaking chills may accompany fever.
- Shortness of breath: Can range from mild to severe, depending on the extent of lung involvement.
- Chest pain: Sharp or pleuritic (worsens with breathing), localized to the area of infection.
- Fatigue: A common symptom, especially in severe cases.
- Muscle aches and headaches: May be present.
- Nausea, vomiting, and diarrhea: More common in children and with certain pathogens.
- Confusion or changes in mental status: May occur, particularly in older adults.
Additional features in specific populations:
- Infants and young children: May present with non-specific symptoms like irritability, poor feeding, and lethargy.
- Older adults: May have atypical presentations, with confusion, falls, or worsening of underlying chronic conditions.
- Immunocompromised individuals: May experience a more severe or prolonged illness. [9]
Sign & Symptoms
Sign & Symptoms
- Productive cough, fever accompanied by shaking chills, shortness of breath, sharp or stabbing chest pain during deep breaths, and an increased rate of breathing. In older people, confusion may be the most prominent sign.
- In children under five are fever, cough, and fast or difficult breathing
- Cough is frequently absent in children less than 2 months old
- More severe signs and symptoms in children may include blue-tinged skin, unwillingness to drink, convulsions, ongoing vomiting, extremes of temperature, or a decreased level of consciousness.
- Pneumonia caused by Legionella may occur with abdominal pain, diarrhea, or confusion
- It caused by Streptococcus pneumoniaeis associated with rusty colored sputum.
Other symptoms
- Pneumonia caused by Klebsiella may have bloody sputum often described as "currant jelly".
- Bloody sputum (known as hemoptysis) may also occur with tuberculosis, Gram-negative pneumonia, lung abscesses and more commonly acute bronchitis.
- Pneumonia caused by Mycoplasma pneumoniae may occur in association with swelling of the lymph nodes in the neck, joint pain, or a middle ear infection
- Viral pneumonia presents more commonly with wheezing than bacterial pneumonia.
Clinical Examination
Clinical Examination of Pneumonia
The clinical examination of a patient with suspected pneumonia typically involves a thorough assessment of various systems, with particular focus on the respiratory system.
General Appearance
- Patient may appear ill, with fever, sweating, and signs of respiratory distress (tachypnea, use of accessory muscles).
Vital Signs
- Fever is often present.
- Tachycardia (rapid heart rate) and tachypnea (rapid breathing) are common.
- Hypotension (low blood pressure) may be seen in severe cases.
- Pulse oximetry may reveal decreased oxygen saturation (hypoxemia).
Respiratory System
Inspection:
- Increased respiratory rate.
- Use of accessory muscles of respiration (e.g., sternocleidomastoid, intercostal muscles).
- Chest wall retractions (inward movement of the chest wall during inspiration).
- Nasal flaring (especially in children).
Palpation:
- Decreased chest expansion on the affected side.
- Increased tactile fremitus (vibrations felt on the chest wall during speech) over areas of consolidation.
Percussion:
- Dullness to percussion over areas of consolidation.
Auscultation:
- Crackles (rales): Discontinuous, popping sounds heard during inspiration, suggesting fluid in the alveoli.
- Bronchial breath sounds: Loud, high-pitched breath sounds heard over areas of consolidation.
- Egophony: Increased resonance of the spoken "E" sound, heard as "A" over areas of consolidation.
- Whispered pectoriloquy: Increased clarity of whispered words heard over areas of consolidation.
- Pleural friction rub: A grating sound heard during inspiration and expiration, suggesting pleural inflammation.
Other Systems
- Cardiovascular: May reveal tachycardia and signs of right heart strain in severe cases.
- Abdominal: May show tenderness in the right upper quadrant if there is associated liver congestion.
- Neurological: May show signs of confusion or altered mental status, particularly in older adults or those with severe hypoxemia. [12]
Diagnosis
Diagnosis
Physical examination
Physical examination may sometimes reveal low blood pressure, high heart rate, or low oxygen saturation. The respiratory rate may be faster than normal, and this may occur a day or two before other signs. Examination of the chest may be normal, but it may show decreased expansion on the affected side. Harsh breath sounds from the larger airways that are transmitted through the inflamed lung are termed bronchial breathing and are heard on auscultation with a stethoscope. Crackles (rales) may be heard over the affected area during inspiration. Percussion may be dulled over the affected lung, and increased, rather than decreased, vocal resonance distinguishes pneumonia from a pleural effusion.[1]
Diagnosis in children
The World Health Organization has defined pneumonia in children clinically based on either a cough or difficulty breathing and a rapid respiratory rate, chest indrawing, or a decreased level of consciousness.
- A rapid respiratory rate is defined as greater than 60 breaths per minute in children under 2 months old,
- Greater than 50 breaths per minute in children 2 months to 1 year old,
- Greater than 40 breaths per minute in children 1 to 5 years old.
In children, low oxygen levels and lower chest indrawing are more sensitive than hearing chest crackles with a stethoscope or increased respiratory rate. Grunting and nasal flaring may be other useful signs in children less than five years old.
Lack of wheezing is an indicator of Mycoplasma pneumoniae in children with pneumonia, but as an indicator it is not accurate enough to decide whether or not macrolide treatment should be used.
The presence of chest pain in children with pneumonia doubles the probability of Mycoplasma pneumoniae.[1]
Diagnosis in adults
In general, in adults, investigations are not needed in mild cases. There is a very low risk of pneumonia if all vital signs and auscultation are normal.
C-reactive protein (CRP)
may help support the diagnosis. For those with CRP less than 20 mg/L without convincing evidence of pneumonia, antibiotics are not recommended.
Procalcitonin
may help determine the cause and support decisions about who should receive antibiotics. Antibiotics are encouraged
if the procalcitonin level reaches 0.25 μg/L, strongly encouraged
it reaches 0.5 μg/L, and strongly discouraged
if the level is below 0.10 μg/L.
In people requiring hospitalization,
- Pulse oximetry,
- Chest radiography
- Blood tests– including a complete blood count, serum electrolytes,
- C-reactive protein level, and possibly
- Liver function tests– are recommended.
The diagnosis of influenza-like illness can be made based on the signs and symptoms; however, confirmation of an influenza infection requires testing. Thus, treatment is frequently based on the presence of influenza in the community or a rapid influenza test.[1]
Differential Diagnosis
Differential Diagnosis
Several diseases can present with similar signs and symptoms to pneumonia, such as:
- Chronic obstructive pulmonary disease,
- Asthma,
- Pulmonary edema,
- Bronchiectasis,
- Lung cancer, and
- Pulmonary emboli.[2]
Complications
Complications of Pneumonia
While most cases of pneumonia resolve with appropriate treatment, the infection can sometimes lead to serious complications. These complications can be broadly classified into:
1. Respiratory Complications:
- Pleurisy: Inflammation of the pleura (the lining of the lungs and chest cavity), causing sharp chest pain that worsens with breathing.
- Pleural effusion: Fluid buildup in the pleural space, which may require drainage if it impairs breathing.
- Empyema: Collection of pus in the pleural space, often requiring drainage and antibiotics.
- Lung abscess: A localized collection of pus within the lung tissue, usually requiring drainage or prolonged antibiotic therapy.
- Acute respiratory distress syndrome (ARDS): A severe lung injury characterized by widespread inflammation and fluid buildup in the lungs, requiring intensive care management.
2. Systemic Complications:
- Sepsis: A life-threatening condition caused by the body’s overwhelming response to infection, leading to organ dysfunction.
- Bacteremia: Presence of bacteria in the bloodstream, which can spread to other organs and cause infections.
- Endocarditis: Infection of the heart valves, often requiring prolonged antibiotic treatment and sometimes surgery.
- Meningitis: Inflammation of the meninges (membranes surrounding the brain and spinal cord), a serious condition requiring prompt treatment.
- Pericarditis: Inflammation of the pericardium (the sac surrounding the heart), causing chest pain and potentially affecting heart function.
3. Other Complications:
- Respiratory failure: Inability of the lungs to adequately oxygenate the blood or remove carbon dioxide, requiring mechanical ventilation.
- Pneumonia recurrence: Some individuals may experience recurrent episodes of pneumonia, especially if they have underlying lung diseases or weakened immune systems. [9]
Investigations
Investigations
- X-Ray chest
- CT-Scan
- Lung ultrasound
Treatment
Treatment
Antibiotics by mouth, rest, simple analgesics, and fluids usually suffice for complete resolution.
However, those with other medical conditions, the older people, or those with significant trouble breathing may require more advanced care. If the symptoms worsen, the pneumonia does not improve with home treatment, or complications occur, hospitalization may require.
Bacterial
- Antibiotics improve outcomes in those with bacterial pneumonia. The first dose of antibiotics should give as soon as possible. Increased use of antibiotics, however, may lead to the development of antimicrobial resistant strains of bacteria.
- Antibiotic use also associate with side effects such as nausea, diarrhea, dizziness, taste distortion, or headaches
Worldwide spread
- In the UK, treatment before culture results with results with amoxicillin recommend as the first line for community-acquired pneumonia, with doxycycline or clarithromycin as alternatives.
- In North America, amoxicillin, doxycycline, and in some areas a macrolides(such as azithromycin or erythromycin) is the first-line outpatient treatment in adults.
- In children with mild or moderate symptoms, amoxicillin taken by mouth is the first line.
- The use of fluoroquinolones in uncomplicated cases discourage due to concerns about side-effects and generating resistance in light of there being no greater benefit.
- Recommendations for hospital-acquired pneumonia include third- and fourth-generation cephalosporins, carbapenems, fluoroquinolones, aminoglycosides, and vancomycin.
Viral
- Neuraminidase inhibitors may use to treat viral pneumonia caused by influenza viruses (influenza A and influenza B).[1]
- No specific antiviral medications recommend for other types of community acquired viral pneumonias including SARS coronavirus, adenovirus, hantavirus, and parainfluenza virus.
- Influenza A may treat with rimantadine or amantadine, while influenza A or B may treat with oseltamivir, zanamivir or peramivir.
- These are of most benefit if they start within 48 hours of the onset of symptoms. Many strains of H5N1 influenza A, also known as avian influenza or "bird flu", have shown resistance to rimantadine and amantadine. The use of antibiotics in viral pneumonia recommend by some experts, as it is impossible to rule out a complicating bacterial infection. The British Thoracic Society recommends that antibiotics withheld in those with mild disease. The use of corticosteroids is controversial.
Aspiration
- In general, aspiration pneumonitis treat conservatively with antibiotics indicated only for aspiration pneumonia. The choice of antibiotic will depend on several factors, including the suspected causative organism and whether pneumonia acquire in the community or developed in a hospital setting. Common options include clindamycin, a combination of a beta-lactam antibiotic and metronidazole, or an aminoglycoside. Corticosteroids sometimes use in aspiration pneumonia, but there is limited evidence to support their effectiveness.[1]
Prevention
Prevention of Pneumonia
Pneumonia prevention strategies aim to reduce the risk of acquiring the infection and its potential complications. Key preventive measures include:
1. Vaccination
- Pneumococcal vaccines: Protect against Streptococcus pneumoniae, a common cause of bacterial pneumonia. Recommended for infants, young children, older adults, and individuals with certain chronic conditions.
- Influenza vaccine: Reduces the risk of influenza, which can predispose individuals to pneumonia. Recommended annually for everyone 6 months and older.
- COVID-19 vaccine: Reduces the risk of COVID-19, which can lead to severe pneumonia.
- Haemophilus influenzae type b (Hib) vaccine: Protects against Hib, another common cause of bacterial pneumonia, particularly in young children.
2. Hygiene Practices
- Frequent handwashing: Helps prevent the spread of respiratory germs.
- Covering coughs and sneezes: Prevents the transmission of respiratory droplets containing infectious agents.
- Avoiding close contact with sick individuals: Reduces exposure to respiratory pathogens.
3. Lifestyle Modifications
- Quitting smoking: Significantly reduces the risk of pneumonia and other respiratory infections.
- Limiting alcohol consumption: Excessive alcohol use can weaken the immune system.
- Maintaining a healthy diet: Adequate nutrition supports a strong immune system.
- Regular exercise: Enhances overall health and immune function.
4. Other Preventive Measures
- Managing chronic conditions: Keeping underlying health conditions like diabetes, heart disease, and lung diseases well-controlled helps reduce the risk of complications from pneumonia.
- Breastfeeding: Provides infants with antibodies that protect against infections, including pneumonia.
- Reducing exposure to indoor air pollution: Minimizing exposure to smoke, dust, and other irritants can help protect the lungs. [10]
Homeopathic Treatment
Homeopathic Treatment
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Plantar fasciitis
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Homeopathy a form of alternative medicine used for the treatment of pneumonia, is based on the theory of individualization. It takes into account the lifestyle, hereditary factors, personality as well as the medical history of a person & aims to treat the person as a whole including their psychological & physiological health.
Some of the homeopathic remedies that are effective against pneumonia are [4],
Medicines:
1. Ferrum phosphoricum
- This, like Aconite, is a remedy for the first stage before exudation takes place, and, like Aconite, if there be any expectoration it is thin, watery and blood streaked.
- It is a useful remedy for violent congestions of the lungs, whether appearing at the onset of the diseases or during its course, which would show that the inflammatory action was extending; it thus corresponds to what term secondary pneumonias, especially in the age and debilitated.
- There high fever, oppress and hurry breathing, and bloody expectoration, very little thirst; there are extensive rales, and perhaps less of that extreme restlessness and anxiety that characterizes Aconite.
- This remedy, with kali muriaticum, forms the Schuesslerian treatment of this disease.
2. Bryonia Alba
- It is the remedy for pneumonia; it furnishes a better pathological picture of the disease than any other, and it comes in after Bryonia is looser and moister than that of Aconite, and there are usually sharp stitching pleuritic pains, the cough of Bryonia is also hard and dry at times and the sputum is scanty and rust colored, so typical of pneumonia.
- There may circumscribe redness of the cheeks, slight delirium and apathy; the tongue will most likely dry, and the patient will most likely dry, l and the patient will want to keep perfectly quiet.
- It a right-side remedy and attacks the parenchyma of the lung, and perhaps more strongly indicate in the croupous form of pneumonia.
- The patient dreads to cough and holds his breath to prevent it on account of the pain it causes; it seems as though the chest walls would fly to pieces.
- The pains in the chest, besides being worse by motion and breathing, are relieved by lying on the right or painful side, because this lessens the motions; of that side.
- Coughs which hurt distant parts of the body call for Bryonia.
- Phosphorus most commonly follows Bryonia in pneumonia, and is complementary.
- In pneumonias complicated by pleurisy Bryonia is the remedy, par excellence.
- Halbert believes that Cantharis relieves the painful features of the early development of the exudate better than any other remedy, a hint which comes from Dr.Jousset, who used the remedy extensively.[3]
3. Kali muriaticum
- Since the advent of Schussler’s this has been a favorite remedy with some physicians, and not without a good ground for its favoritism.
- Clinical experience has proved that this drug in alternation with Ferrum Phosphoricum constitutes a treatment of pneumonia which has been very successful in many hands.
- The symptoms calling for Kali muriaticum as laid down by Schussler are very meager, it given simply because there is a fibrinous exudation in the lung substance.
- There is a white, viscid expectoration and the tongue coated white.
- It better suited to the second stage, for when the third stage appears with its thick, yellowish expectoration it replace by Kali Sulphuricum in the biochemic nomenclature.[3]
4. Phosphorus
- It is "the great mogul of lobar pneumonia." It should remembered that Phosphorus is not, like Bryonia, the remedy when the lungs completely hepatized, although it is one of the few drugs which have known to produce hepatization.
- When bronchial symptoms are present it is the remedy, and cerebral symptoms during pneumonia often yield better to Phosphorus than to Belladonna.
- There is cough; with pain under sternum, as if something torn loose; there is pressure across the upper part of the chest and constriction of the larynx; there pressure across the upper part of the chest and constriction of the larynx; there are mucous rales, labored breathing, sputa yellowish mucus, with blood streaks therein, or rust colored, as under Bryonia.
Relationship of Phosphorus
- After Phosphorus, Hepar Sulphur. naturally follows as the exudate begins to often; it is the remedy of the third stage, the fever is; of a low character. Tuberculinum. In lobular pneumonia this remedy surpasses Phosphorus or Antimonium tartaricum, and competent observers convinced that it has an important place in the treatment of pneumonia; some using it in very case intercurrently; doses varying from 6x to 30x. When typhoid symptoms occur in the course of pneumonia then Phosphorus will come in beautifully.
- Phosphorus follows Bryonia well, being complementary to it. There is also a sensation as if the chest were full of blood, which causes an oppression; of breathing, a symptom met with commonly enough in pneumonia.
- Hughes maintains that Phosphorus should give in preference to almost any medicine in acute chest affections in young children.
- Lilienthal says Phosphorus is our great tonic to the heart and lungs. Hyoscyamus. Dr. Nash considers this remedy one; of the best in typhoid pneumonia, meaning that it is more frequently indicated than any other.[3]
5. Chelidonium
- Bilious pneumonia is, perhaps more often indicative of Chelidonium than of any other remedy. there are stitching pains under the right scapula, loose rattling cough and difficult expectoration, oppression; of chest, as under Antimonium tartaricum, and fan-like motions of the alae nasi, as under Lycopodium.
- Mercurius is quite similar in bilious pneumonia; the stools will decide, those of Mercurius being slimy and accompan by tenesmus; the expectoration is also apt to blood-streak.
- With Chelidonium there is an excess of secretion in the tubes, which; is similar to Antimonium tartaricum, and an inability to raise the same.
- It has greatly praise in catarrhal pneumonia of young children where there is plentiful secretion and inability to raise it.
- The right lung more often affect in cases calling for Chelidonium.[3]
6. Antimonium tartaricum
- This drug especially indicated in pneumonia and pleuro-pneumonia at the stage of resolution.
- There are fine moist rales heard all over the hepatized portion of the lungs; these are different from the Ipecac rales; they are fine, while those of Ipecac are coarse.
- With Antimonium tartaricum there is great oppression of breathing, worse towards morning, compelling the patient to sit up to breath.
- There are also sharp, stitching pains and high fever, as under Bryonia, and it, perhaps, more closely corresponds to the catarrhal form than it does to the croupous.
- Bilious symptoms, if present, do not contra-indicate, as there are many of these in its pathogenesis.
- There is one peculiar symptom, the patient feels sure that the next cough will raise the mucus, but it does not. When there is deficient reaction, as in the old age or; in very young children, this remedy particularly indicated.
7. Kali carbonicum
- Kali Carb. is, perhaps, more similar to Bryonia than any drug in the symptom of sharp, stitching pains in the chest.
- These are worse by motion, but, unlike Bryonia they come whether the patient moves or not, and are more in the lower part of the right lung.
- In pneumonia with intense dyspnoea and a great deal of mucus on the chest, which, like in all of the Kalis, raise with difficulty, wheezing and whistling breathing,
- Kali carbonicum is the remedy, especially if the cough tormenting. It comes in with benefit ofttimes where Antimonium tartaricum and Ipecac have failed to raise the expectoration.
- Kali bichromicum may indicate by its well-known tough, stringy expectoration.[3]
8. Sulphur
- A remedy to use in any stage of pneumonia.
- It will prevent, if given in the beginning, if the symptoms indicate it.
- It will prevent hepatization and cause imperfect and slow resolution to react. When the case has a typhoid tendency and the lung and the lung tends to break down, where there are rales, muco-purulent expectoration slow speech, dry tongue and symptoms of hectic, Sulphur is the remedy.
- Weakness and faintness are characteristic symptoms. Dr. G. J. Jones says a dyspnoea occurring at night between 12 and 2 causing the patient to sit up in bed is a valuable symptom.
- Its field especially in neglect pneumonias in psoric constitutions, with tendency to develop into tuberculosis.
- In purulent expectoration Sanguinaria is the better remedy, especially where it is offensive even to the patient himself.
- If the lung hepatize, the patient at night restless and feverish, ulceration threatened, and there is no tendency to recuperation then one may depend upon Sulphur.
- Lycopodium also; a most useful remedy in delay or partial resolution.
- There is a tightness across the chest, aching over lungs, general weakness.
- Hughes says it is the best remedy where the case threatens to run into acute phthisis.[3]
Diet & Regimen
Diet & Regimen
- Drink plenty of fluids and fresh juice of fruits and vegetables.
- Consume hot vegetable soups – tomato, sweet corn etc.
- Add a pinch of turmeric to your diet as it has anti-inflammatory properties.
- Initially diet should consist of fresh fruits and vegetables, when better can start with grains and little of protein in diet.
- Milk and milk products and sweets should be avoided to decrease mucus production.
- Onion and garlic should be consumed it is beneficial.
- Boil a mixture of Bishops weed (Ajwain), tea leaves and water and inhale the steam, helps to decongest. Do this at least 2-3 times a day.
- Gargle with warm water, a pinch of salt and turmeric to sooth your throat.
- Consume lots of vitamin A, maintains the integrity of the respiratory mucosa: Liver oils of fish like cod, shark, and halibut are richest source of vitamin A.
Other dietary measures
- Egg, milk and milk products, meat, fish, kidney and liver.
- Yellow orange-colored fruits and vegetables, dark green leafy vegetables.
- Increase intake of vitamin C, it has antioxidant property: foods of animal origin are poor in vitamin C.
- Citrus fruits, green vegetables.
- Include zinc in your diet, it boosts up your immunity:
- Meat, poultry and milk, sea food – shell fish, crab, shrimp, and sea plants etc.
- Plant foods are low in zinc, Whole wheat grains provide good amount of zinc.
- Avoid sharing things such as towels, beverages with infected people.
- Avoid contact with infected people.
- Avoid crowded places.
- Avoid smoking and alcohol.[5]
Do’s and Don'ts
Do’s and Don’ts
Pneumonia do’s and don’ts
Do’s
- Seek Medical Attention: If you suspect pneumonia, see a doctor promptly for diagnosis and treatment.
- Complete the Full Course of Antibiotics: If prescribed antibiotics, take them exactly as directed and finish the entire course, even if you feel better sooner.
- Get Plenty of Rest: Rest is essential for your body to fight the infection and recover.
- Stay Hydrated: Drink plenty of fluids to help thin mucus and make it easier to cough up.
- Use a Humidifier: Moist air can help soothe irritated airways and make breathing easier.
- Control Fever: Use over-the-counter medications like acetaminophen or ibuprofen to reduce fever and manage discomfort, as directed by your doctor.
- Practice Good Hygiene: Wash your hands frequently, cover your coughs and sneezes, and avoid close contact with sick people to prevent spreading the infection.
- Get Vaccinated: Get vaccinated against pneumococcal pneumonia, influenza, and COVID-19 to reduce your risk of these infections and their potential complications.
- Quit Smoking: If you smoke, quitting is one of the best things you can do for your lung health and reduce the risk of pneumonia.
- Manage Chronic Conditions: If you have underlying health conditions like asthma, diabetes, or heart disease, work with your doctor to manage them effectively and reduce your risk of pneumonia.
Don’ts
- Don’t Ignore Symptoms: If you experience symptoms like persistent cough, fever, chest pain, or shortness of breath, seek medical attention promptly.
- Don’t Self-Medicate: Don’t take antibiotics or other medications without a doctor’s prescription.
- Don’t Overexert Yourself: Avoid strenuous activity while recovering from pneumonia.
- Don’t Smoke: Smoking damages the lungs and makes them more susceptible to infections.
- Don’t Drink Alcohol: Alcohol can weaken the immune system and interfere with medications.
- Don’t Ignore Follow-up Appointments: Attend all follow-up appointments with your doctor to ensure complete recovery and monitor for any complications.
Terminology
Terminology
1. Pneumonia:
- Meaning: An infection that inflames the air sacs in one or both lungs. The air sacs may fill with fluid or pus, causing cough, fever, chills, and difficulty breathing.
2. Pathogens:
- Meaning: Microorganisms that cause disease, such as bacteria, viruses, or fungi. In the context of pneumonia, these are the agents responsible for the infection.
3. Consolidation:
- Meaning: A region of the lung where the air sacs are filled with fluid or inflammatory material, making the lung tissue denser and less able to exchange oxygen and carbon dioxide effectively.
4. Community-Acquired Pneumonia (CAP):
- Meaning: Pneumonia acquired outside of a hospital or healthcare setting.
5. Hospital-Acquired Pneumonia (HAP):
- Meaning: Pneumonia that develops 48 hours or more after admission to a hospital or other healthcare facility.
6. Ventilator-Associated Pneumonia (VAP):
- Meaning: Pneumonia that develops in people who are on a mechanical ventilator to help them breathe.
7. Aspiration Pneumonia:
- Meaning: Pneumonia that occurs when food, liquid, or vomit is inhaled into the lungs.
8. Walking Pneumonia:
- Meaning: A milder form of pneumonia with less severe symptoms. People with walking pneumonia may continue their usual activities but may experience a prolonged recovery.
9. Lobar Pneumonia:
- Meaning: Pneumonia that affects one or more lobes (sections) of the lung.
10. Bronchopneumonia:
- Meaning: Pneumonia that affects the patches of tissue around the bronchi (the airways that lead to the lungs).
11. Pleural Effusion:
- Meaning: A buildup of fluid in the pleural space, the area between the lungs and the chest wall.
12. Empyema:
- Meaning: A collection of pus in the pleural space.
13. Lung Abscess:
- Meaning: A localized collection of pus within the lung tissue.
14. Sepsis:
- Meaning: A life-threatening condition caused by the body’s overwhelming response to an infection.
15. Hypoxemia:
- Meaning: Low levels of oxygen in the blood.
16. Dyspnea:
- Meaning: Shortness of breath or difficulty breathing.
17. Tachypnea:
- Meaning: Rapid breathing.
18. Tachycardia:
- Meaning: Rapid heart rate.
19. Crackles (Rales):
- Meaning: Abnormal lung sounds heard with a stethoscope, often described as crackling or rattling sounds.
Homeopathic Remedies Commonly Used in Pneumonia Cases:
- Aconitum napellus: Often considered for early stages of pneumonia, especially when accompanied by high fever, restlessness, anxiety, and dry cough.
- Bryonia alba: May be indicated when there’s a dry, painful cough, stitching chest pain that worsens with movement, and a desire for complete stillness.
- Phosphorus: Can be useful when the cough is loose and productive with rust-colored sputum, accompanied by chest tightness and shortness of breath.
- Antimonium tartaricum: Often considered for cases with rattling cough, difficulty expectorating mucus, and drowsiness.
- Ipecacuanha: May be helpful when there’s a persistent cough with nausea and vomiting, and a sensation of constriction in the chest.
- Kali carbonicum: Can be considered for cases with stitching chest pain, shortness of breath, and a tendency to catch cold easily.
References
References
- https://en.wikipedia.org/wiki/Pneumonia
- Harrison’s Principles of Internal Medicine 19Th Edition.
- Therapeutics from Zomeo Ultimate LAN
- https://www.myupchar.com/ en/disease/pneumonia/homeopathy
- http://specialityclinic.com/homeopathic-treatment/diet-and-nutrition/Pneumonia
Rudan I, et al. Global burden of childhood pneumonia and diarrhoea. Lancet. 2013;381(9875):1405-16.
GBD 2015 Lower Respiratory Infections Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1659-724.
- Walker CLF, et al. Pneumonia in children: causes, risk factors, prevention, and treatment. Lancet. 2013;381(9875):1405-16.
- Harrison’s Principles of Internal Medicine, 21st Edition (2022) by Dennis L. Kasper, Anthony S. Fauci, Stephen L. Hauser, Dan L. Longo, J. Larry Jameson, Joseph Loscalzo. Published by McGraw Hill Professional
- Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases, 9th Edition (2020), By John E. Bennett, Raphael Dolin, Martin J. Blaser. Published by Elsevier
- Nelson Textbook of Pediatrics, 21st Edition (2020). by Robert M. Kliegman, Bonita F. Stanton, Joseph St. Geme, Nina F Schor, Richard E. Behrman. Published by Elsevier.
Also Search As
Also Search As
People can search for homeopathic articles on pneumonia using various online methods, including:
Search Engines
- Use specific keywords:
- Include additional terms:
- "case studies"
- "research"
- "clinical trials"
- specific homeopathic remedies (e.g., "Aconitum napellus pneumonia")
- Use quotation marks:
- Enclose phrases in quotation marks (e.g., "homeopathic medicine for pneumonia") to search for exact matches.
Homeopathic Websites and Journals
- Visit reputable homeopathic websites: Search for well-established homeopathic organizations or journals that publish research articles and case studies.
- Use their search function: Many homeopathic websites have a search bar where you can enter keywords like "pneumonia" to find relevant articles.
Social Media
- Follow homeopathic organizations and practitioners: Stay updated on the latest research and articles by following relevant accounts on social media platforms.
- Search relevant hashtags: Search for hashtags like #homeopathy, #pneumonia, and #homeopathicremedies to find discussions and articles shared by others.
There are several ways to search for information about pneumonia, depending on the specific information you are seeking and the resources available to you. Here are some common approaches:
Online Search Engines:
- Keyword searches: Use search engines like Google, Bing, or DuckDuckGo to search for general information about pneumonia or specific aspects you are interested in. Use keywords like "pneumonia symptoms," "pneumonia causes," "pneumonia treatment," or "pneumonia prevention."
- Image search: Use image search on search engines to find images of chest X-rays with pneumonia or illustrations of the respiratory system affected by pneumonia.
Medical Websites and Databases:
- Reputable medical websites: Visit websites like Mayo Clinic, WebMD, or the Centers for Disease Control and Prevention (CDC) to access reliable information about pneumonia, its causes, symptoms, treatment, and prevention.
- Medical databases: If you are conducting research or looking for in-depth information, access medical databases like PubMed or MEDLINE to find scientific articles and research papers on pneumonia.
Libraries:
- Medical books: Visit your local library or university library to access medical textbooks or reference books on pneumonia. These resources can provide detailed information on the pathophysiology, diagnosis, and treatment of pneumonia.
- Medical journals: Libraries often have subscriptions to medical journals that publish research articles and clinical studies on pneumonia.
Healthcare Professionals:
- Consult your doctor: If you have concerns about pneumonia or are experiencing symptoms, the best way to get personalized information is to consult your doctor or another qualified healthcare professional.
- Ask a pharmacist: Pharmacists can provide information about pneumonia medications, their side effects, and interactions with other medications.
Frequently Asked Questions (FAQ)
What is Pneumonia?
Pneumonia is an inflammatory condition of the lung primarily affecting the small air sacs known as alveoli.
What causes Pneumonia?
What are the symptoms of Pneumonia?
Give the types of Pneumonia?
- Community-acquired
- Aspiration
- Healthcare-associated
- Hospital-acquired
- Ventilator-associated pneumonia
Homeopathic Medicines used by Homeopathic Doctors in treatment of Pneumonia?
Homoeopathic medicine for pneumonia
- Bryonia Alba
- Kali Muriaticum
- Phosphorus
- Chelidonium
- Antimonium tartaricum
- Kali carbonicum
- Sulphur
Can homeopathy help with pneumonia?
Yes, homeopathy can offer supportive care for pneumonia by addressing the individual’s symptoms and stimulating the body’s natural healing response. It aims to reduce the severity and duration of the illness.
How does a homeopath select the right remedy for pneumonia?
A homeopath will conduct a detailed case analysis, considering the patient’s physical, mental, and emotional symptoms along with their medical history. This helps to identify the most suitable remedy.
Is it safe to use homeopathy for pneumonia?
Homeopathic remedies are generally safe and well-tolerated when prescribed by a qualified practitioner. However, it’s crucial to consult a doctor for proper diagnosis and treatment of pneumonia, especially in severe cases.
How long does it take to see improvement with homeopathy for pneumonia?
The response time varies depending on the individual’s condition and the severity of the illness. Some may experience relief within a few days, while others may require a longer duration of treatment.