Cryptomenorrhea
Definition
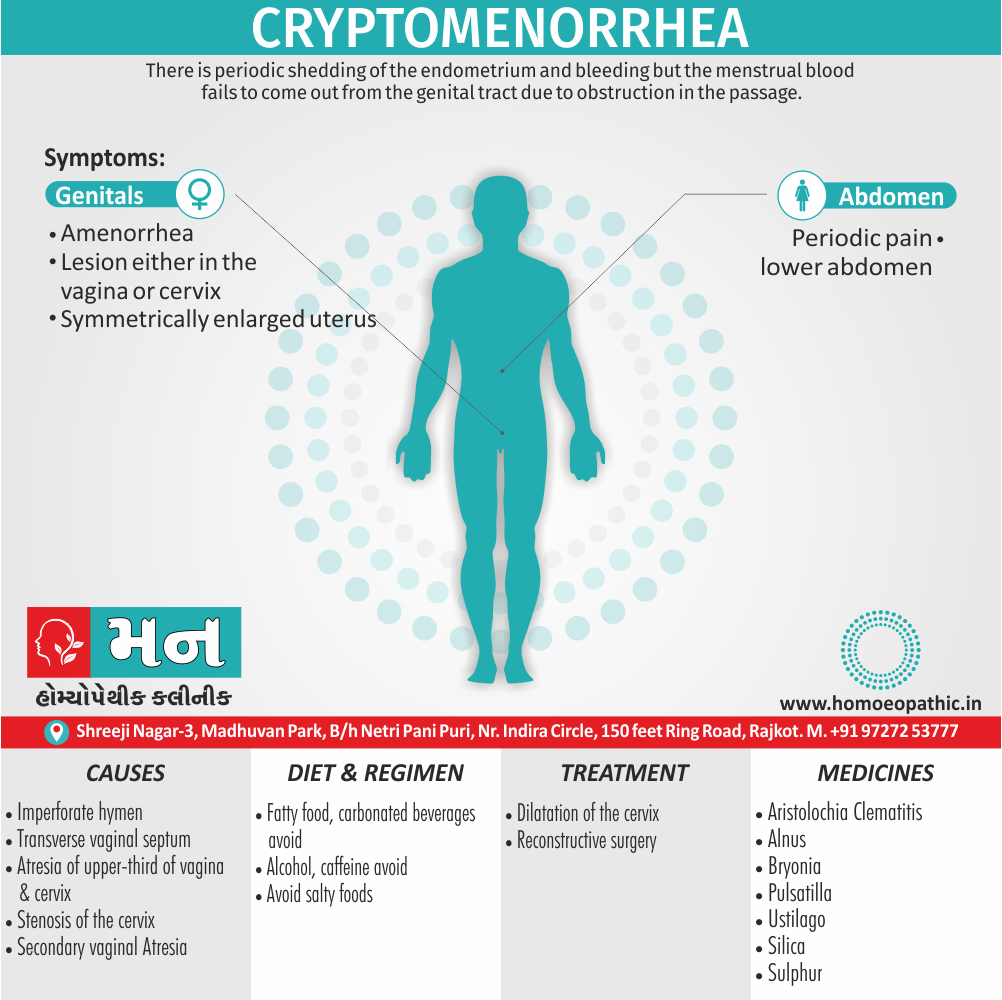
In cryptomenorrhea, there is periodic shedding of the endometrium and bleeding but the menstrual blood fails to come out from the genital tract due to obstruction in the passage.[1]
There aren’t any true synonyms for cryptomenorrhea because it’s a specific medical term. However, depending on the context, here are some ways to describe it:
- Hidden menstruation: This is a more general way to describe the condition.
- Internal menstruation: This emphasizes that the bleeding happens internally but doesn’t go into the specifics.
- Blocked menstruation: This focuses on the cause of the hidden bleeding.
If you need to be more precise in a medical context, you can simply use "cryptomenorrhea."
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Cryptomenorrhea
Basically, there is only accumulation of blood in the uterine cavity resulting in hematometra. On the other hand, In neglected cases, the blood may enter the tubes whose fimbrial ends get blocked resulting in distension of the tubes by blood → hematosalpinx[1]
Epidemiology
Epidemiology of Cryptomenorrhoea
There is limited epidemiological data on cryptomenorrhoea (also known as hematocolpos) specifically for India. However, several studies and case reports from India have documented the occurrence of this condition, suggesting it is not uncommon but accurate prevalence rates are not available.
Cryptomenorrhoea is often associated with imperforate hymen or other obstructive genital anomalies. Studies investigating the prevalence of these anomalies in India could provide some indirect insights into the potential frequency of cryptomenorrhoea. For example, a study published in the Indian Journal of Pediatrics in 2009 reported a prevalence of 0.06% for imperforate hymen among adolescent girls in a rural Indian population.
Additionally, several case reports of cryptomenorrhoea in Indian patients have been published in various medical journals over the years. While these case reports don’t offer population-level data, they do highlight the presence of this condition within the country.
Please note that due to the lack of dedicated epidemiological studies on cryptomenorrhoea in India, it is challenging to provide precise figures or specific references on its prevalence. [4]
Causes
Causes of Cryptomenorrhea
Congenital e.g.:
[1] Imperforate hymen
[2] Transverse vaginal septum
[3] Atresia of upper-third of vagina also cervix.
Acquired e.g.:
[1] Stenosis of the cervix following amputation, deep
[2] cauterization and conization.
[3] Secondary vaginal Atresia following neglected also
[4] difficult vaginal delivery. [1]
Types
Types of Cryptomenorrhoea
Cryptomenorrhoea itself is not categorized into different types, as it is a symptom rather than a disease itself. It refers to the condition where menstrual bleeding occurs but is not visible due to an obstruction in the genital tract.
However, the underlying causes of cryptomenorrhoea can be varied and can lead to different presentations of the condition. These causes can be classified as:
Congenital:
- Imperforate hymen (most common)
- Transverse vaginal septum
- Vaginal atresia
Acquired:
- Cervical stenosis (scarring or narrowing of the cervix)
- Uterine synechiae (Asherman’s syndrome)
- Rarely, tumors obstructing the outflow tract [5]
Risk Factors
Risk Factors of Cryptomenorrhea
The primary risk factor for cryptomenorrhoea is the presence of an obstruction in the genital tract. However, certain factors can increase the likelihood of developing these obstructions, particularly congenital ones:
Family History: A family history of imperforate hymen or other genital anomalies can increase the risk of a female child developing similar conditions.
Certain Genetic Syndromes: Some rare genetic syndromes, such as Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome, are associated with congenital absence or malformation of the vagina, uterus, or both.
Prenatal Exposure to Certain Medications or Substances: In rare cases, prenatal exposure to certain medications or substances may increase the risk of developing congenital genital anomalies. [6]
Pathogenesis
Pathogenesis of Cryptomenorrhea
Cryptomenorrhoea is a consequence of an obstruction in the female genital tract, preventing the outflow of menstrual blood. The pathogenesis varies depending on the underlying cause:
Imperforate Hymen: This is the most common cause. The hymen, a thin membrane partially covering the vaginal opening, fails to perforate during fetal development. As menstruation begins, blood accumulates behind the hymen (hematocolpos), causing it to bulge and create a bluish discoloration. If left untreated, the blood can back up into the uterus (hematometra) and even the fallopian tubes (hematosalpinx).
Transverse Vaginal Septum: This is a less common congenital anomaly where a fibrous band of tissue divides the vagina into two segments. Menstrual blood accumulates in the upper segment, leading to hematocolpos and potentially hematometra.
Vaginal Atresia: In this rare condition, the vagina is completely absent or severely underdeveloped, preventing menstrual outflow entirely.
Acquired Causes: Cervical stenosis and uterine synechiae are acquired conditions that can obstruct menstrual flow. Cervical stenosis is often caused by scarring from previous procedures or infections. Uterine synechiae (Asherman’s syndrome) are adhesions within the uterus, usually resulting from trauma during surgery or infection. [7]
Pathophysiology
Pathophysiology of Cryptomenorrhea
If the site of obstruction is low down in the vagina, the accumulated blood results Firstly in hematocolpos → Then hematometra → After that, hematosalpinx.
If the obstruction is at the cervix, it will produce hematometra → hematosalpinx. Hematocolpos produces marked elongation of the urethra → retention of urine.[1]
Clinical Features
Clinical Features of Cryptomenorrhea
The clinical presentation of cryptomenorrhoea varies depending on the underlying cause and the duration of obstruction. However, some common features include:
Primary Amenorrhea or Oligomenorrhea: Young girls who have reached puberty but have not started menstruating (primary amenorrhea) or have infrequent periods (oligomenorrhea) may have cryptomenorrhoea.
Cyclic Pelvic Pain: This is often the most prominent symptom. The pain typically coincides with the expected timing of menstruation and is caused by the accumulation of blood behind the obstruction. The pain can be crampy and similar to menstrual cramps or a dull, constant ache.
Pelvic Mass: In some cases, a pelvic mass can be palpated on physical examination. This is due to the accumulation of blood in the vagina (hematocolpos), uterus (hematometra), or fallopian tubes (hematosalpinx).
Bulging Hymen: In cases of imperforate hymen, the hymen may appear bluish and bulging due to the trapped blood.
Urinary Symptoms: If the obstruction is large enough, it can compress the bladder or urethra, leading to urinary frequency, urgency, or difficulty voiding.
Constipation: Rarely, a large pelvic mass can compress the rectum, causing constipation. [8]
Sign & Symptoms
Sign & Symptoms of Cryptomenorrhea
The patients with history of any of the etiological factors mentioned earlier, Complain of i.e.:
- Amenorrhea dated back from the events.
- Periodic pain lower abdomen
Pelvic examination reveals the offending lesion either in the vagina or cervix. The uterus is symmetrically enlarged.[1]
Clinical Examination
Clinical Examination of Cryptomenorrhea
A thorough clinical examination is crucial in diagnosing cryptomenorrhoea. Key aspects include:
Abdominal Examination: Palpation may reveal a suprapubic mass if there is significant hematocolpos or hematometra. Tenderness may be present, particularly during the expected time of menstruation.
Inspection of External Genitalia: In cases of imperforate hymen, the hymen may appear bluish and bulging due to the accumulated blood. Other anomalies, such as vaginal agenesis or a transverse vaginal septum, may also be visible on inspection.
Speculum Examination: This is not usually performed in adolescent girls with suspected cryptomenorrhoea due to the risk of causing pain and trauma. However, it may be considered in older women after other diagnostic modalities have been exhausted.
Bimanual Palpation (Rectal or Rectovaginal): This examination helps assess the size and consistency of the uterus and the presence of any pelvic masses. A bulging vaginal wall may be palpable in cases of hematocolpos.
Neurological Examination: Assessing for neurological deficits is important, especially if there are urinary symptoms or constipation, as these could indicate spinal cord compression from a large pelvic mass. [5]
Diagnosis
Diagnosis of Cryptomenorrhea
In brief, Cryptomenorrhea can be easily diagnosed using ultrasound. The vagina is commonly seen filled with blood whereas the uterus usually appears pushed upward.[1]
Differential Diagnosis
Differential Diagnosis of Cryptomenorrhoea
While the classic presentation of cryptomenorrhoea is relatively straightforward, it is essential to consider other conditions that can mimic its symptoms, especially in cases where the diagnosis is less clear:
Primary Amenorrhea (Without Obstruction): Several conditions can cause primary amenorrhea without an outflow tract obstruction. These include:
Gonadal Dysgenesis (Turner Syndrome): This genetic condition affects females and is characterized by absent or non-functional ovaries.
Hypothalamic-Pituitary Disorders: Conditions affecting the hypothalamus or pituitary gland, which regulate the menstrual cycle, can lead to primary amenorrhea.
Müllerian Agenesis (Mayer-Rokitansky-Küster-Hauser Syndrome): This congenital disorder involves the absence or underdevelopment of the uterus and vagina.
Other Causes of Cyclic Pelvic Pain:
Endometriosis: This condition involves the growth of endometrial tissue outside the uterus and can cause cyclic pelvic pain.
Pelvic Inflammatory Disease (PID): This infection of the female reproductive organs can cause pelvic pain, but it is usually not strictly cyclic.
Ovarian Cysts: Some ovarian cysts can cause pain that might coincide with the menstrual cycle.
Other Causes of Pelvic Masses:
Uterine Fibroids: These noncancerous growths in the uterus can cause pelvic pain and pressure.
Ovarian Tumors: Both benign and malignant ovarian tumors can present as pelvic masses. [9]
Complications
Complications of Cryptomenorrhea
If left untreated, cryptomenorrhoea can lead to several complications, including:
Hematosalpinx and Hematometra: The accumulation of blood can extend beyond the vagina, filling the uterus (hematometra) and even the fallopian tubes (hematosalpinx). This can cause significant pain and may impair fertility.
Endometriosis: Retrograde menstruation, where menstrual blood flows back through the fallopian tubes into the pelvic cavity, can occur in cases of cryptomenorrhoea. This can lead to the development of endometriosis, a painful condition where endometrial tissue grows outside the uterus.
Infection: The accumulated blood can become infected, leading to pelvic inflammatory disease (PID). This can cause fever, pelvic pain, and potentially damage the reproductive organs.
Infertility: Long-term obstruction and the associated complications can damage the fallopian tubes and uterus, leading to infertility.
Urinary Retention: In severe cases, a large hematocolpos can compress the urethra, leading to difficulty urinating or complete urinary retention. [7]
Investigations
Investigations for Cryptomenorrhea
A combination of clinical assessment and imaging studies are employed to diagnose cryptomenorrhoea and identify the underlying cause of the obstruction:
Ultrasound: This is often the first-line imaging modality. Transabdominal ultrasound can visualize the hematocolpos (blood-filled vagina), hematometra (blood-filled uterus), or hematosalpinx (blood-filled fallopian tubes). It can also identify anatomical anomalies like an imperforate hymen or transverse vaginal septum.
Magnetic Resonance Imaging (MRI): MRI provides more detailed anatomical information than ultrasound. It is particularly useful for visualizing complex anomalies or differentiating between different types of pelvic masses.
Laboratory Tests: While not diagnostic, certain laboratory tests can be helpful:
- Complete Blood Count (CBC): To assess for anemia, which can occur with prolonged or heavy menstrual bleeding.
- Pregnancy Test: To rule out pregnancy as a cause of amenorrhea.
- Hormone Levels: To evaluate the function of the ovaries and other endocrine glands involved in menstruation.
Other Tests: In some cases, additional tests may be needed:
- Hysterosalpingogram (HSG): This involves injecting contrast dye into the uterus and fallopian tubes to visualize their anatomy and identify any blockages.
- Laparoscopy: This minimally invasive surgery allows direct visualization of the pelvic organs and can be used to diagnose and treat certain conditions causing cryptomenorrhoea. [8]
Treatment
Treatment of Cryptomenorrhea
Simple dilatation of the cervix so as to drain the collected blood is enough. Additionally, In cases of secondary atresia of the vagina, reconstructive surgery is to be performed, to maintain the patency.[1]
Prevention
Prevention of Cryptomenorrhea
Primary prevention of cryptomenorrhoea is not always possible, as most cases are due to congenital anomalies that occur during fetal development. However, early detection and intervention can prevent complications and long-term consequences.
Newborn Examination: A thorough examination of female newborns can identify some genital anomalies, such as an imperforate hymen, allowing for early intervention.
Health Education: Educating parents and adolescents about the signs and symptoms of puberty, including the onset of menstruation, can help identify potential issues early on.
Regular Pediatric Check-ups: Routine check-ups allow healthcare providers to monitor the development of female children and adolescents and identify any concerns related to puberty or menstruation. [10]
Homeopathic Treatment
Homeopathic Treatment of Cryptomenorrhea
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Medicine of Cryptomenorrhea:
Clematis:
Brown discharge, watery flow. In detail, Eczema of the vulva. Sensual itching, aggravated before menses, on the other hand, ameliorated during menses, aggravated after menses. Menses absent, late or short, Blood especially, black, with clotting. Varicocele. Dysmenorrhea. Infrequent menses. Amenorrhea. Metritis. After-pains with laryngitis. Lastly, Vaginitis.
Agnus:
Clinical This drug has been used especially for strumous disorders, enlarged submaxillary glands, leucorrhoeas, with erosions of cervix, which bleed easily, amenorrhoea, burning pain from back to pubis.
Bryonia:
Sticking pains in the region of the liver on touch, coughing or breathing. Specifically, Symptoms of inflammation of the liver and of the diaphragm. Abdomen distended. Additionally, A feeling of something heavy lying in the abdomen. Movements. loud either rumbling or a gurgling and soreness and dragging downward.
Pulsatilla:
Suited to patients of a mild also easy disposition. In detail, Pain in lower part of abdomen and across the small of the back; giddiness, fullness about the head and eyes; chilliness, cold hands and feet; sour taste in the mouth after eating; nausea also vomiting; loss of appetite, with desire for acids, and palpitation; disinclination for exercise, alternate laughing and crying, sadness, melancholy, painfulness of the head; the symptoms are worse in the afternoon and before midnight; whereas symptoms are better in the open air while exercising. pains frequently change from one place to another.
Ustilago:
It is specifically indicated in Cryptomenorrhea. Tenderness of the left ovary, with pain and swelling. Basically, A distress referred to the mouth of the uterus. Yellow, offensive leucorrhoea. Menstruation free, bright, not coagulated. Uterine hemorrhage, bright, thin, with soft, spongy uterus, pain extending to the knees; with tenderness especially, of left ovary. Ovarian neuralgia, left. Membranous dysmenorrhoea. Pain shooting down the legs. Persistent uterine hemorrhage, with oozing of dark blood in clots. All in all, Pain in the left mammary region between periods, with ovarian congestion and burning pains.
Silica:
Colicky pains in the lower abdomen, with straining and increased pain during stool. Constantly hard, greatly distended. Feels thick and heavy like a weight.
Sulphur:
After Puls, when the latter has been insufficient, and in all cases which drag, especially if the patient complains of heat in the head, giddiness, and palpitation, short breath, loss of appetite, sickness after eating, loss of flesh, and depression.[3]
Diet & Regimen
Diet & Regimen
It’s a good idea to avoid foods that cause bloating and water retention. Some of the biggest culprits include:
- fatty foods
- alcohol
- carbonated beverages
- caffeine
- salty foods
Reducing or cutting out these foods can help alleviate cramps and decrease tension. [2]
Do’s and Don'ts
Do’s & Don’ts
Cryptomenorrhea Do’s & Don’ts
Do’s:
- Seek medical attention promptly: If a young girl has reached puberty age but hasn’t started menstruating, or experiences cyclic pelvic pain without visible bleeding, consult a doctor immediately.
- Schedule regular gynecological checkups for adolescent girls: This can help in early detection of any anatomical abnormalities causing cryptomenorrhoea.
- Educate yourself about the signs and symptoms of cryptomenorrhoea: Early recognition of the condition can lead to prompt treatment and prevent complications.
- Follow the doctor’s advice regarding treatment: This may involve surgery to correct the underlying anatomical abnormality.
- Maintain good hygiene practices: This is important to prevent infections in case of hematocolpos (accumulation of blood in the vagina).
- Seek emotional support: Dealing with a diagnosis of cryptomenorrhoea can be emotionally challenging. Talking to a counselor or therapist can be beneficial.
Don’ts:
- Ignore the symptoms: Delaying diagnosis and treatment can lead to serious complications.
- Self-medicate: Do not attempt to treat cryptomenorrhoea with over-the-counter medications or home remedies.
- Hesitate to ask questions: If you have any concerns or questions about the diagnosis or treatment, do not hesitate to discuss them with your doctor.
- Engage in strenuous physical activity: If experiencing pelvic pain, avoid activities that could worsen the discomfort.
- Feel ashamed or embarrassed: Cryptomenorrhoea is a medical condition, and there is no reason to feel ashamed or embarrassed about it.
Terminology
Terminology
Key Terminologies:
- Cryptomenorrhoea: A condition where menstruation occurs but the blood fails to exit the body due to an obstruction in the genital tract.
- Hematocolpos: Accumulation of menstrual blood in the vagina.
- Hematometra: Accumulation of menstrual blood in the uterus.
- Hematosalpinx: Accumulation of menstrual blood in the fallopian tubes.
- Imperforate Hymen: A condition where the hymen (a membrane that partially covers the vaginal opening) is completely closed or has a very small opening.
- Transverse Vaginal Septum: A horizontal band of tissue dividing the vagina into upper and lower segments.
- Atresia: Absence or closure of a normal body opening.
- Cervical Stenosis: Narrowing of the cervical opening.
- Uterine Synechiae (Asherman’s Syndrome): Formation of scar tissue or adhesions within the uterus.
- Primary Amenorrhea: Absence of menstruation in a person who has reached puberty.
- Oligomenorrhea: Infrequent or irregular menstrual periods.
- Miasmatic Tendency: A predisposition to certain types of diseases in homeopathic theory.
Homeopathic Remedies Mentioned:
- Clematis: Used for brown or watery discharge, eczema of the vulva, irregular menstruation, and pelvic inflammation.
- Agnus Castus: Used for menstrual irregularities, burning pain, and scrofulous conditions.
- Bryonia: Used for inflammation of the liver, abdomen distension, and pain.
- Pulsatilla: Used for individuals with mild dispositions, mood swings, and changeable symptoms.
- Ustilago: Specifically indicated for cryptomenorrhoea with tenderness of the left ovary and uterine hemorrhage.
- Silicea: Used for colicky pains in the lower abdomen and constipation.
- Sulphur: Used when other remedies fail, and for symptoms like heat in the head, giddiness, and palpitation.
References
References
- DC DUTTA’s GYNECOLOGY
- https://www.thewomens.org.au/health-information/periods/healthy-periods/exercise-diet-periods
- A Complete Repertory Of The Tissue Remedies Of Schussler By S. F. Shannon
- Indian Journal of Pediatrics in 2009
- Novak’s Gynecology, 16th Edition by Jonathan S. Berek, Evelyn Nicole F. Berek (2020) published by Wolters Kluwer
- Comprehensive Gynecology, 7th Edition by William’s Gynecology (2017) published by McGraw Hill Professional
- Te Linde’s Operative Gynecology, 13th Edition, byJohn O. Schorge, Joseph I. Schaffer, Marlene M. Corton (2020) published by Wolters Kluwer
- Clinical Gynecologic Endocrinology and Infertility, 9th Edition by Marc A. Fritz, Leon Speroff (2019) published by Wolters Kluwer
- Williams Gynecology, 4th Edition, by Barbara L. Hoffman, John O. Schorge, Joseph I. Schaffer, et al. (2020) published by McGraw Hill Professional
- Practical Pediatric and Adolescent Gynecology (2nd Edition) by Veronica Gomez-Lobo (2018) published by Cambridge University Press
Also Search As
Also Search As
- Hematocolpos: The accumulation of menstrual blood in the vagina due to an obstruction.
- Hidden Menstruation: A general term for menstruation that is not visible due to obstruction.
- Imperforate Hymen: A common cause of cryptomenorrhoea where the hymen is fully closed or has a very small opening.
- Menstrual Obstruction: A broader term encompassing various conditions that obstruct menstrual flow.
- Obstructed Menses: Another term for menstruation that is blocked due to an obstruction.
- Primary Amenorrhea Causes: Cryptomenorrhoea can be a cause of primary amenorrhea, so searching for this broader term might be helpful.
- Teenage Amenorrhea: As cryptomenorrhoea often affects adolescents, searching for "teenage amenorrhea" could lead to relevant information.
General Terms:
- Cryptomenorrhoea
- Hidden menstruation
- Internal menstruation
- Blocked menstruation
- Hematocolpos
- Hematometra
- Hematosalpinx
Medical Terms:
- Primary amenorrhea
- Oligomenorrhea
- Imperforate hymen
- Transverse vaginal septum
- Vaginal atresia
- Cervical stenosis
- Uterine synechiae
- Asherman’s syndrome
Homeopathic Terms:
- Homeopathic treatment for cryptomenorrhoea
- Homeopathic remedies for menstrual obstruction
- Clematis for cryptomenorrhoea
- Pulsatilla for cryptomenorrhoea
- Ustilago for cryptomenorrhoea
Specific Phrases:
- Causes of cryptomenorrhoea
- Symptoms of cryptomenorrhoea
- Diagnosis of cryptomenorrhoea
- Treatment of cryptomenorrhoea
- Complications of cryptomenorrhoea
- Prevention of cryptomenorrhoea
Additional Tips:
- Combine different search terms for more specific results (e.g., "homeopathic treatment cryptomenorrhoea").
- Include the word "article" or "information" in your search to find relevant articles or web pages.
- Search on homeopathic websites or forums for discussions and information specific to homeopathic treatment.
People can find this article on Cryptomenorrhoea in several ways:
Directly through the website or platform:
- URL: If they know the exact web address (URL) of the article, they can simply type or paste it into their browser’s address bar.
- Site Search: Most websites and platforms have an internal search bar. Users can type relevant keywords like "cryptomenorrhoea," "hidden menstruation," or "homeopathic treatment for cryptomenorrhoea" into the search bar to find the article within that specific website.
By using search engines (like Google, Bing, DuckDuckGo):
- Keywords: Use the terms mentioned previously in "Also Search As" and "How people can search this article."
- Specific Phrases: Try phrases like "homeopathic remedies for cryptomenorrhoea," "causes of cryptomenorrhoea," or "treatment options for hidden menstruation."
- Combinations: Combine different search terms for more refined results (e.g., "cryptomenorrhoea homeopathy India").
Through social media:
- Hashtags: Search for relevant hashtags on platforms like Twitter or Instagram (e.g., #cryptomenorrhoea, #homeopathy, #womenshealth).
- Groups and Communities: Join online groups or forums focused on women’s health or homeopathy and ask for information or resources on cryptomenorrhoea.
Through medical databases or directories:
- PubMed: If the article has been published in a medical journal, it might be indexed in PubMed, a database of medical literature.
- Homeopathic Directories: Look for the article in directories of homeopathic articles or resources.
Frequently Asked Questions (FAQ)
What is Cryptomenorrhea?
In cryptomenorrhea, there is periodic shedding of the endometrium and bleeding but the menstrual blood fails to come out from the genital tract due to obstruction in the passage.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Cryptomenorrhea?
Homoeopathic Treatment For Cryptomenorrhea
- Clematis
- Bryonia
- Pulsatilla
- Ustilago
- Silicea
- Sulphur
What are the symptoms of Cryptomenorrhea?
- Amenorrhea dated back from the events.
- Periodic pain lower abdomen
What are the causes of Cryptomenorrhea?
- Imperforate hymen
- Transverse vaginal septum
- Atresia of upper-third of vagina and cervix
- Stenosis of the cervix following amputation, deep
- Cauterization and conization
- Secondary vaginal Atresia following neglected
- Difficult vaginal delivery
Is cryptomenorrhoea dangerous?
Yes, if left untreated, cryptomenorrhoea can lead to complications like hematosalpinx, hematometra, endometriosis, infection, and even infertility.
What are the treatment options for cryptomenorrhoea?
Treatment typically involves surgery to correct the underlying obstruction. Homeopathic remedies might be considered as a complementary approach, but always consult a qualified healthcare professional.
Can homeopathy treat cryptomenorrhoea?
While homeopathy is a complementary therapy, some practitioners believe it can help manage the symptoms of cryptomenorrhoea and potentially address underlying imbalances. However, consulting with a qualified healthcare professional for diagnosis and treatment is crucial.
What are the common homeopathic remedies for cryptomenorrhoea?
Some homeopathic remedies suggested for cryptomenorrhoea include Pulsatilla, Clematis, Bryonia, Ustilago, Silicea, and Sulphur. The choice of remedy depends on individual symptoms and constitution.
Is it safe to use homeopathy alongside conventional treatment for cryptomenorrhoea?
It’s important to inform your doctor about any homeopathic remedies you’re considering, as some remedies might interact with conventional medications.
How can I find a qualified homeopathic practitioner for cryptomenorrhoea?
Look for certified homeopaths with experience in treating women’s health issues. Referrals from trusted sources can also be helpful.
