Prostate Problems
Definition
To understand the Prostate problems, let’s first understand the Prostate Gland.
The prostate is a small gland in men that helps make semen. Located just below the bladder in front of the rectum, it wraps around the tube that carries urine also semen out of the body. It tends to grow larger as you get older. Additionally; If your prostate gets too large, it can cause a number of health issues.[1]
There are several synonyms for prostate problems, depending on the specific condition. Here are some general terms:
- Prostate gland issues
- Prostate conditions
- Lower urinary tract symptoms (LUTS): This is a broad term that refers to any problems with urination, such as difficulty starting or stopping urination, a weak stream, or frequent urination. LUTS can be caused by a variety of conditions, including prostate problems.
- Benign prostatic hyperplasia (BPH): This is the most common prostate problem. It is a noncancerous enlargement of the prostate gland that can cause LUTS.
- Prostatitis : This is inflammation of the prostate gland. It can be caused by a bacterial infection, or it may be nonbacterial. Prostatitis can cause LUTS, as well as pain in the groin, lower abdomen, and genitals.
- Prostate cancer: This is cancer that develops in the prostate gland. It is the most common cancer in men after skin cancer.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
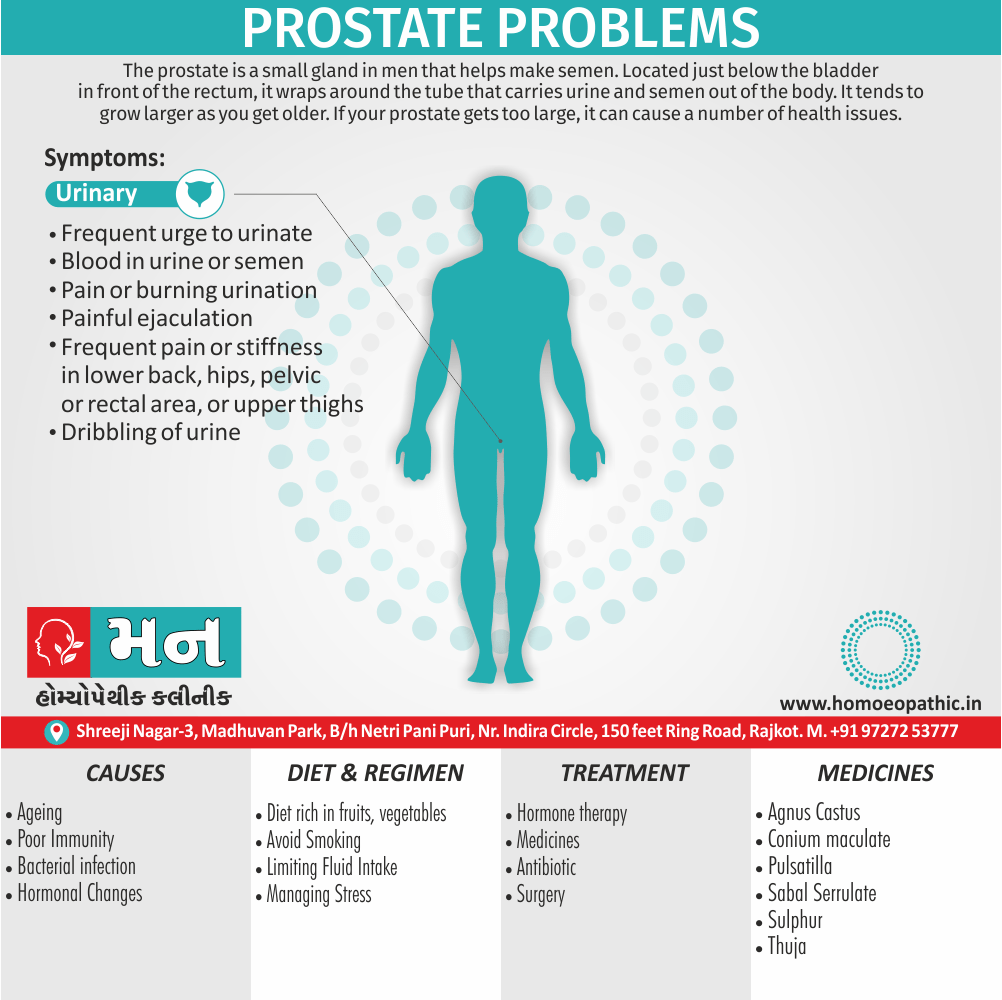
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Prostate Problems
Here are some examples of non-cancer prostate problems i.e.:
Benign prostatic hyperplasia, or BPH, is very common in older men. It means your prostate is enlarged but not cancerous. Treatments for BPH include:
- Watchful waiting, also called active surveillance. If your symptoms are not too bad, your doctor may tell you to wait to see if they get worse before starting treatment. Your doctor will tell you how often to return for check-ups.
- Medications. Medicines can help shrink the prostate or relax muscles near your prostate to ease symptoms.
- Surgery. If nothing else has worked, your doctor may suggest surgery to help urine flow.
- Other treatments. Sometimes radio waves, microwaves, or lasers are used to treat urinary problems caused by BPH. These methods use different kinds of heat to reduce extra prostate tissue.
Acute bacterial prostatitis
Acute bacterial prostatitis usually starts suddenly from a bacterial infection. See your doctor right away if you have fever, chills, or pain in addition to prostate symptoms. Most cases can cured with antibiotics. You also may need medication to help with pain or discomfort.
Chronic bacterial prostatitis
Chronic bacterial prostatitis is an infection that comes back again and again. This rare problem can be hard to treat. Sometimes, taking antibiotics for a long time may work. Talk with your doctor about other things you can do to help you feel better.
Chronic prostatitis
Chronic prostatitis, also called chronic pelvic pain syndrome, is a common prostate problem. It can cause pain in the lower back, in the groin, or at the tip of the penis. Treatment may require a combination of medicines, surgery, and lifestyle changes.
Be sure to talk with your doctor about the possible side effects of treatment.[1]
Epidemiology
Epidemiology
The epidemiology of prostate problems in India, encompassing both benign prostatic hyperplasia (BPH) and prostate cancer, reveals significant trends.
Benign Prostatic Hyperplasia (BPH)
- Prevalence increases with age: Multiple studies indicate BPH prevalence to be around 25%, 37%, 37%, and 50% for age groups 40-49, 50-59, 60-69, and 70-79 years, respectively. By 60, over 50% of men show some evidence of BPH ("Prostate health in India (BPH & Prostate Cancer)", Archives of Cancer Science and Therapy, no publication year provided).
Prostate Cancer
- Increasing incidence: Prostate cancer is the second leading cancer in large Indian cities like Delhi and Kolkata and among the top ten in other regions ("Epidemiology of prostate cancer in India", ResearchGate, 2014).
- Age-adjusted incidence rates vary: Rates per lakh population in 2009-10 were highest in Delhi (10.2), followed by Bengaluru (8.7), Mumbai (7.3), Chennai (7), and Bhopal (6.1) ("Prostate health in India (BPH & Prostate Cancer)", Archives of Cancer Science and Therapy, no publication year provided).
- Significant increase in some registries: Bangalore, Chennai, Delhi, Mumbai, and Kamrup Urban District recorded statistically significant increasing trends in incidence rates ("Epidemiology of prostate cancer in India", ResearchGate, 2014).
- Rising cases: Approximately 40,000 new cases were reported in 2020, a considerable rise from previous years ("Prostate Cancer Risk Factors: Key Demographic and Statistical Overview", Max Hospital, no publication year provided).
- Average age of incidence is 65 years ("Prostate cancer in India: Current perspectives and the way forward", Journal of Radiation and Health Management, 2023).
Overall
- The burden of prostate problems in India is substantial and growing, particularly with an aging population and increasing life expectancy.
- Both BPH and prostate cancer pose significant health challenges for Indian men.
- Continued research and awareness are essential to address these growing concerns effectively.
Causes
Causes of Prostate Problems
Age: The prostate gland naturally grows with age. This enlargement can lead to benign prostatic hyperplasia (BPH) and increase the risk of other prostate problems.
Hormonal Changes: Imbalances in hormones, particularly the increase in dihydrotestosterone (DHT) with age, can contribute to prostate growth and the development of BPH.
Family History: Men with a family history of prostate problems, particularly prostate cancer, are at an increased risk. Genetic factors can play a significant role in the development of these conditions.
Inflammation: Chronic inflammation of the prostate gland, known as prostatitis, can cause pain and urinary symptoms. The exact cause of inflammation can vary and may include bacterial infections or other factors.
Lifestyle Factors: Unhealthy lifestyle choices, such as a diet high in red meat and fat and lack of exercise, can contribute to prostate problems. Obesity has also been linked to an increased risk of prostate cancer.
Environmental Factors: Exposure to certain environmental toxins and chemicals may also increase the risk of developing prostate problems.
Understanding the causes of prostate problems is crucial for prevention and early detection. By adopting a healthy lifestyle, getting regular checkups, and being aware of risk factors, men can take proactive steps to protect their prostate health.[5]
Types
Types of Prostate Problems
The prostate gland, while essential for male reproductive health, is susceptible to a variety of disorders that can impact quality of life. These problems can range from benign conditions to more serious concerns like cancer. The main types of prostate problems include:
Benign Prostatic Hyperplasia (BPH): This is a non-cancerous enlargement of the prostate gland that is common in older men. It can lead to urinary symptoms like frequent urination, weak stream, and difficulty starting or stopping urination.
Prostate Cancer: This is the most common cancer in men, characterized by the uncontrolled growth of cells in the prostate gland. While it may initially be asymptomatic, advanced prostate cancer can cause symptoms similar to BPH, as well as bone pain, erectile dysfunction, and fatigue.
Prostatitis: This is an inflammation of the prostate gland, often causing pain or discomfort in the pelvic area, lower back, or genitals. It can also lead to urinary symptoms and sexual dysfunction.
Other Less Common Conditions: There are also less common prostate problems, such as prostate stones, prostate cysts, and prostate abscesses. These conditions can cause varying symptoms depending on their severity and location.[5]
Risk Factors
Risk Factors of Prostate Problems
While the exact causes of prostate problems like Benign Prostatic Hyperplasia (BPH), prostate cancer, and prostatitis remain an area of ongoing research, several factors have been identified that increase a man’s risk of developing these conditions. Understanding these risk factors is crucial for early detection and prevention strategies.
Key Risk Factors:
- Age: The risk of most prostate problems, especially BPH and prostate cancer, increases significantly with age. Most cases occur in men over 50.
- Family History: Men with a family history of prostate cancer or certain breast cancers have a higher risk of developing prostate cancer themselves.
- Race/Ethnicity: African American men are at a higher risk of developing prostate cancer and are more likely to be diagnosed at a younger age.
- Diet: Diets high in red meat and high-fat dairy products may increase the risk of prostate cancer.
- Obesity: Some studies suggest that obesity may be associated with a higher risk of aggressive prostate cancer.
- Environmental Exposures: Certain chemicals and occupational exposures may increase the risk of prostate cancer.
Other Potential Risk Factors:
- Inflammation of the Prostate (Prostatitis): The link between prostatitis and prostate cancer is still being studied.
- Sexually Transmitted Infections (STIs): Some research suggests a possible association between STIs and an increased risk of prostate cancer.
- Vasectomy: The potential link between vasectomy and prostate cancer remains controversial and inconclusive.[5]
Pathogenesis
Pathogenesis of Prostate Problems
The prostate gland, a crucial part of the male reproductive system, is prone to various disorders, each with its unique underlying mechanisms.
Benign Prostatic Hyperplasia (BPH)
BPH, a non-cancerous enlargement of the prostate, is primarily driven by age-related hormonal changes. The prevailing theory suggests an imbalance between testosterone and dihydrotestosterone (DHT), leading to an increase in prostate cell growth and proliferation. The resulting enlargement compresses the urethra, causing urinary symptoms.
Prostate Cancer
Prostate cancer arises from genetic mutations and alterations in cellular signaling pathways that lead to uncontrolled cell growth and tumor formation. Risk factors include age, family history, and certain genetic mutations.
Prostatitis
Prostatitis, or inflammation of the prostate gland, has multiple potential causes:
- Bacterial Prostatitis: Acute or chronic bacterial infections can trigger inflammation.
- Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS): The exact cause remains unclear, but theories suggest inflammation, nerve irritation, and pelvic muscle dysfunction.
- Non-inflammatory Prostatitis: This category encompasses conditions like prostatodynia, where pain is present without evidence of inflammation.[5]
Pathophysiology
Pathophysiology of Prostate Problems
The prostate gland, an integral part of the male reproductive system, can be subject to a variety of disorders that affect its function and overall health. These disorders stem from a complex interplay of factors, including hormonal imbalances, inflammation, and cellular changes.
Benign Prostatic Hyperplasia (BPH)
BPH, a non-cancerous enlargement of the prostate, is the most common prostate problem in aging men. The exact cause remains unclear, but it is thought to be linked to age-related hormonal changes, specifically the increase in dihydrotestosterone (DHT), a potent androgen that promotes prostate cell growth. This leads to hyperplasia, or an increase in the number of cells, resulting in an enlarged prostate that compresses the urethra, causing urinary symptoms.
Prostate Cancer
Prostate cancer is the second most common cancer in men worldwide. The exact cause is unknown, but it involves genetic mutations and alterations in cellular signaling pathways that lead to uncontrolled cell growth and tumor formation. Risk factors include age, family history, and certain genetic mutations.
Prostatitis
Prostatitis refers to inflammation of the prostate gland, which can be caused by bacterial infections, chronic inflammation, or non-inflammatory conditions. Bacterial prostatitis can be acute or chronic, while chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) is a complex condition with unclear etiology, possibly involving inflammation, nerve irritation, and pelvic muscle dysfunction.[5]
Clinical Features
Clinical Features of Prostate Problems
Prostate problems can manifest in a variety of ways, depending on the underlying cause and severity. Here’s an overview of the common clinical features associated with various prostate disorders:
Benign Prostatic Hyperplasia (BPH)
BPH primarily affects the lower urinary tract, leading to:
- Obstructive Symptoms:
- Weak urine stream
- Hesitancy and straining to urinate
- Intermittent urine flow
- Sensation of incomplete bladder emptying
- Dribbling after urination
- Irritative Symptoms:
- Increased frequency of urination
- Urgency to urinate
- Nocturia (waking up at night to urinate)
Prostate Cancer
Early-stage prostate cancer often presents with no symptoms. However, as the tumor grows, it can cause similar symptoms to BPH, along with:
- Blood in urine or semen
- Painful ejaculation
- Bone pain (in advanced cases)
- Unexplained weight loss
- Erectile dysfunction
Prostatitis
Prostatitis can cause a range of symptoms, including:
- Pain or discomfort:
- In the lower abdomen, groin, or back
- During or after ejaculation
- During bowel movements
- Urinary symptoms:
- Similar to BPH
- Burning or painful urination
- General symptoms:
- Fever and chills (in acute bacterial prostatitis)
- Fatigue
It’s important to note that these are just some of the possible clinical features of prostate problems. If you’re experiencing any concerning symptoms, consult a healthcare professional for proper evaluation and diagnosis. Early detection and treatment can significantly improve outcomes for many prostate conditions.[5]
Sign & Symptoms
Sign & Symptoms
See your doctor right away if you have any of these symptoms:
- Frequent urge to urinate
- Need to get up many times during the night to urinate
- Blood in urine or semen
- Pain or burning urination
- Painful ejaculation
- Frequent pain or stiffness in lower back, hips, pelvic or rectal area, or upper thighs
- Dribbling of urine
Clinical Examination
Clinical Examination of Prostate Problems
The clinical examination of the prostate is a crucial step in diagnosing and managing various prostate problems. It typically involves a combination of a digital rectal examination (DRE) and assessment of lower urinary tract symptoms (LUTS).
Digital Rectal Examination (DRE)
- Procedure: The physician inserts a gloved, lubricated finger into the rectum to palpate the prostate gland.
- Assessment: The DRE allows the physician to evaluate:
- Size and shape of the prostate
- Consistency (soft, firm, hard, or nodular)
- Tenderness or pain
- Presence of any abnormalities, such as nodules or asymmetry
Lower Urinary Tract Symptoms (LUTS) Assessment
History taking: The physician inquires about the patient’s urinary symptoms, including:
- Frequency of urination
- Urgency
- Nocturia (waking up at night to urinate)
- Hesitancy or difficulty initiating urination
- Weak or intermittent urinary stream
- Straining to urinate
- Incomplete emptying of the bladder
- Dribbling after urination
Questionnaires: Standardized questionnaires, such as the International Prostate Symptom Score (IPSS), may be used to quantify the severity of LUTS.
Additional Tests
Depending on the clinical findings and suspected diagnosis, the physician may recommend additional tests, such as:
- Prostate-specific antigen (PSA) blood test
- Urinalysis and urine culture
- Uroflowmetry
- Post-void residual urine measurement
- Transrectal ultrasound (TRUS)
- Prostate biopsy[6]
Diagnosis
Diagnosing Prostate Cancer
To find out if prostate symptoms are caused by cancer, your doctor will ask about your past medical problems and your family’s medical history. Your doctor also will perform a physical exam. During the exam, your doctor will put a gloved finger into your rectum to examine your prostate to check for:
- The size, firmness, and texture of the prostate
- Any hard areas, lumps, or growth spreading beyond the prostate
- Any pain caused by touching or pressing on the prostate
You may ask to give a urine sample for testing. Your doctor also may do a blood test to check the prostate-specific antigen (PSA) level. PSA levels can be high in men with an enlarged prostate gland or with prostate cancer. You may also need an ultrasound exam that takes computer pictures of the prostate.
If tests show that you might have cancer, your doctor will refer you to a specialist (a urologist) for a prostate biopsy. The doctor will take small tissue samples from several areas of the prostate gland to look for cancer cells.
Differential Diagnosis
Differential Diagnosis of Prostate Problems
Accurate diagnosis of prostate problems is essential for effective management and treatment. However, various conditions can present with similar symptoms, making the differential diagnosis challenging.
Benign Prostatic Hyperplasia (BPH)
- Differential diagnoses:
- Prostate cancer
- Bladder neck obstruction
- Urethral stricture
- Neurogenic bladder
- Overactive bladder
- Urinary tract infection (UTI)
Prostate Cancer
- Differential diagnoses:
- BPH
- Prostatitis
- Bladder cancer
Prostatitis
- Differential diagnoses:
- BPH
- Prostate cancer
- UTI
- Sexually transmitted infections (STIs)
- Interstitial cystitis
- Chronic pelvic pain syndrome[6]
Complications
Complications of an enlarged prostate:
- Sudden inability to urinate (urinary retention).You might need to have a tube (catheter) inserted into your bladder to drain the urine. Some men with an enlarged prostate need surgery to relieve urinary retention.
- Urinary tract infections (in other words; UTIs).Inability to fully empty the bladder can increase the risk of infection in your urinary tract. If UTIs occur frequently, you might need surgery to remove part of the prostate.
- Bladder stones. These generally cause by an inability to completely empty the bladder. Bladder stones can cause infection, bladder irritation, blood in the urine also obstruction of urine flow.
- Bladder damage.A bladder that hasn’t emptied completely can stretch and weaken over time. As a result, the muscular wall of the bladder no longer contracts properly, making it harder to fully empty your bladder.
- Kidney damage.Pressure in the bladder from urinary retention can directly damage the kidneys or allow bladder infections to reach the kidneys.
Most men with an enlarged prostate don’t develop these complications. However, acute urinary retention and kidney damage can be serious health threats.[4]
Having an enlarged prostate is not believed to increase your risk of developing prostate cancer.
Investigations
Investigation
PSA Testing
Until recently, many doctors encouraged yearly PSA testing for all men beginning at age 50, or even earlier for men at high risk of prostate cancer. As doctors have learned more about the benefits and harms of prostate cancer screening, they have begun to caution against annual PSA testing. Talk with your doctor about what is best for you.
Yearly PSA testing in men without symptoms is generally not recommended. However, in men who report prostate symptoms, PSA testing (along with digital rectal examination) can help doctors determine the nature of the problem. In men who have been treated for prostate cancer, the PSA test may be used to see if the cancer has come back.[1]
Treatment
Treatment
It depends on whether cancer is in part or all of the prostate, or if it has spread to other parts of the body. It also depends on your age and overall health. Talk with your doctor about the best treatment choice for you and the possible side effects of treatment. You may want to ask another doctor for a second opinion.
Treatment for prostate cancer may be:
- Watchful waiting, also called active surveillance. If the cancer is not causing problems, you may decide not to get treated right away. Instead, your doctor will check regularly for changes in your condition. Treatment may start if the cancer begins to grow.
- Surgery. The most common type of surgery removes the whole prostate also some nearby tissue.
- Radiation therapy. This treatment uses radiation to kill cancer cells and shrink tumors. Additionally, the radiation may come from an X-ray machine or from tiny radioactive pellets placed inside or near the tumor.
- Hormone therapy. Men having other treatments, like radiation therapy, also may treat with drugs to stop the body from making testosterone. This is done if it seems likely that the cancer will come back. Hormone therapy also can use for prostate cancer that has spread beyond the prostate.
Prevention
Prevention of Prostate Problems
While some prostate problems, like those related to genetics, may be unavoidable, there are steps men can take to reduce their risk or promote early detection:
Lifestyle Modifications:
- Healthy Diet:
- Emphasize fruits, vegetables, and whole grains.
- Limit red meat and high-fat dairy products.
- Consider incorporating foods rich in lycopene (tomatoes, watermelon), selenium (Brazil nuts, fish), and zinc (oysters, beans).
- Regular Exercise: Maintain a healthy weight and stay physically active.
- Limit Alcohol and Avoid Smoking: These habits can negatively impact overall health, including prostate health.
Screening and Early Detection:
- Prostate-Specific Antigen (PSA) Test: Discuss with your doctor the appropriate age to start and frequency of PSA testing.
- Digital Rectal Exam (DRE): Your doctor may recommend this exam as part of your prostate screening.
Specific Recommendations for Certain Conditions:
- BPH:
- Maintain a healthy weight.
- Limit caffeine and alcohol, especially before bedtime.
- Avoid medications that can worsen urinary symptoms.
- Prostate Cancer:
- Consider genetic testing if you have a strong family history.
- Discuss with your doctor about chemoprevention options if you are at high risk.[5]
Homeopathic Treatment
Homeopathic Treatment for Prostate Problems
Homeopathy is a safe and natural alternative and plays a vital role in reducing the size of the prostate if administered timely.
This line of treatment can be taken alone when the symptoms are mild to moderate, and along with any other alternative treatment when the symptoms are severe. Homeopathic medicines have no side effects or contraindications and can benefit most individuals if started timely.[4]
HRD’s Homeopathic treatment is offered only to the following individuals:
- Individuals having no strong indication for surgery, ascertained by the severity of complaints and clinical examination by your physician
- Recently diagnosed cases or those with infrequent and/or mild to moderated symptoms
- Patients refusing surgery or cannot be operated on due to other medical conditions
Mild to moderate symptoms of urinary retention, increased frequency at night and a weak stream should strongly consider homeopathic treatment for duration of 4-6 months.
Homoeopathic Approach
- Homeopathic remedies having anti-tumorproperties are prescribed.
- The prescribed remedy helps in: reducing the sizeof the enlarged Prostate, counteracts infection in the urinary tract and improves sphincter control.
- The treatment outcome does depend on the extent of prostatic hypertrophy. Individuals experiencing mild symptoms with marginal hypertrophy experience greater reliefas compared to chronic, advanced cases with severe retention.[4]
Homoeopathic Medicines
Aconite nep [Acon]
Prostatitis with great urging to urinate and great pain during micturition, or where in milder cases there is great pain in walking, especially down stairs.
Aesculus Hip [Ascu]
Desire to urinate often, but passes little at a time, scanty and dark-yellow, with scalding in passing through the urethra, some- times deep-red, with strong odor; amorous dreams and seminal emissions; blind piles, with shooting pains up back.[3]
Agnus Castus
When pressing at stool, discharge of prostatic fluid; pollutions from irritable weakness with prostatorrhoea; red, turbid urine, with burning and pressure in urethra.
Aloe
Sensation as if a plug were wedged between symphysis and coccyx, pressing downward; incontinence of urine from enlarged prostate; intense pain and soreness in rectum after stool with protrusion of piles, (<) from touch and temporarily (>) by cold water.
Apis Mell
Excessive pain in vesical region, frequent desire and pressing down in region of sphincter, not only during day, but has to get up often at night; AGONY IN PASSING URINE; retention of urine or dark, scanty urine.
Baryta Carb
HYPERTROPHY OF PROSTATE; after urinating renewed straining with dribbling of urine; numbness in genitals for several minutes; frequent micturition, no stool, in old men.
Causticum
PULSATIONS IN PERINEUM; after passing a few drops pain in urethra, bladder and spasms in rectum, with renewed desire; must pass water every few minutes at night with extremely painful pressing and urging; additionally chronic prostatitis; contraction of sphincter, with excoriating serous discharge from anus.[3]
Chimaphila
Sensation of swelling in perineum, as if on sitting down a ball were pressing against it; inability to urinate without standing with the feet wide apart and the body inclined forward. ACUTE PROSTATITIS from sitting on a cold damp stone, excessive itching and painful irritation of urethra from the end of penis to neck of bladder, which dysuria may increase to complete retention from swelling of prostate; great quantities of thick, ropy, bloody mucus in urine; prostatic disease with waste of prostatic fluid.
Copiva
INDURATION OF PROSTATE, in old men, with no increase in size or slight augmentation with extreme hardness; burning and sensation of dryness in region of prostate gland and in urethra, with great pain while urinating, urine emitted by drops; mucous discharge from bowels with much rumbling and rolling in abdomen.
Cyclamen
Prostatic troubles, with stitches and pressure, urging to stool and micturition; in and near anus and in perineum drawing- pressing pain, as from subcutaneous ulceration of a small spot, while walking or sitting; frequent desire to urinate, with scanty discharge; while urinating, pricking pain at the end of the urethra.
Digitalis
HYPERTROPHY OF PROSTATE, CARDIAC SYMPTOMS MARKED; dribbling discharge of urine and continued fullness after micturition or fruitless effort to urinate; throbbing pain in region of neck of bladder during the straining efforts to pass water; increased desire to urinate after a few drops have passed, causing the old man to walk about in distress though motion increases desire to urinate; frequent desire to defaecate at the same time; very small, soft stool passed without relief, urine pale, slightly cloudy, looking smoky.
Kali Bichrom
STITCHES IN PROSTATE when walking, must stand still; prostatic fluid escapes at stool; painful drawing from perineum into urethra; after micturition burning in back part of urethra as if a drop had remained, with unsuccessful effort to pass it; stitches in urethra.
Magnesia Carb
DISCHARGE OF PROSTATIC FLUID WHEN PASSING FLATUS; involuntary urination while walking or rising from a seat.
Pulsatilla
Continued dull stitches in neck of bladder, with a pressure of urine, while lying upon his back; AFTER MICTURITION SPASMODIC PAINS IN NECK OF BLADDER, EXTENDING TO PELVIS AND THIGHS; prostatic troubles of older people, faeces flat, small in size.[3]
Selenium
Prostatic juice oozes while sitting, during sleep, when walking and at stool; involuntary urination while walking, drips after stool or micturition; additionally stool hard also impacted that it requires mechanical aid; (<) in hot weather, after sleep, from anything which causes relaxation.
Staphysagria
Frequent and copious urination; burning the whole length of urethra; frequent urging with scanty discharge of a thin stream of red-looking urine; urging as if bladder were not empty; In detail; discharge of dark urine by drops; pain extending from anus along urethra, coming on after either walking or riding.
Sulphur
Offensive sweat around genitals; stools hard, knotty, insufficient; urine foetid, with greasy-looking pellicle on it; painful desire, with discharge of bloody urine, requiring great effort; besides this; mucous discharge from urethra.
Thuja
Syphilis and sycosis, especially suppressed or badly treated gonorrhoea; stitches in urethra from behind, also from rectum into bladder; rectal tenesmus, deep perineal pains; dysuria, retained urine; cutting at beginning of passing water, the pain descending the urethra to a point just above the external meatus; urine squirts either out or slowly drops; besides this scalding also cutting at the close of urination; stream interrupted several times before bladder is entirely emptied; frequent desire to urinate in the evening, (>) by lying down.
Sabal Serrulata:
Sabal Serrulata is one of the most popular homeopathic medicines for prostate gland enlargement with many patients having consumed it reported great results. It works for most causes of prostate gland enlargement as well.[3]
Diet & Regimen
Diet & Regimen
Foods to eat
Specific foods known to benefit the prostate include i.e.:
- Salmon: Salmon is rich in healthy fats that contain omega-3 fatty acids, which help prevent and reduce inflammation within the body. Other cold-water fish, such as sardines and trout, are also rich in these types of fats.
- Tomatoes: Tomatoes are packed with lycopene, an antioxidant that may benefit prostate gland cells. Cooking tomatoes, such as in tomato sauce or soup, helps to release the lycopene and make it more readily available to the body.
- Berries: For example; Strawberries, blueberries, raspberries, and blackberries are excellent sources of antioxidants, which help to remove free radicals from the body. Free radicals are the by products of reactions that occur within the body and can cause damage and disease over time.[2]
- Broccoli: Broccoli and other cruciferous vegetables, including bok choy, cauliflower, Brussels sprouts, also cabbage, contain a chemical known as sulforaphane. Additionally, This is thought to target cancer cells and promote a healthy prostate.
- Nuts: Nuts are rich in zinc, a trace mineral. Zinc is found in high concentrations in the prostate also is thought to help balance testosterone and DHT. Besides nuts, shellfish and legumes are also high in zinc.
- Citrus: Oranges, lemons, limes, and grapefruits are all high in vitamin C, which may help to protect the prostate gland.
- Onions and garlic: One study found that men with BPH tended to eat less garlic also onions that men without BPH. More research is needed to confirm these results, but onions and garlic are healthful additions to most diets.
Some foods to avoid include:
- Red meat: Research suggests that going red meat-free may help improve prostate health. In fact, daily meat consumption believed to triple the risk of prostate enlargement.
- Dairy: Similarly to meat, regular consumption of dairy increased risk of BPH. Cutting out or reducing butter, cheese, and milk may help reduce BPH symptoms.
- Caffeine: Caffeine may act as a diuretic, which means that it increases how much, how often, and how urgently a person has to urinate. Cutting back on coffee, tea, soda, and chocolate may improve urinary symptoms of BPH.
- Alcohol: Alcohol can also stimulate urine production. Men with BPH may find that their symptoms improved by giving up alcohol.
- Sodium: A high salt intake may increase the urinary tract symptoms associated with BPH. Following a low-sodium diet by not adding salt to meals and avoiding processed foods may be helpful for some men. [2]
Do’s and Don'ts
The Do’s & Don’ts
Do’s:
Maintain a Healthy Diet:
- Emphasize fruits, vegetables, and whole grains.
- Limit red meat and high-fat dairy products.
- Incorporate foods rich in lycopene (tomatoes, watermelon), selenium (Brazil nuts, fish), and zinc (oysters, beans).
Exercise Regularly:
- Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Exercise helps maintain a healthy weight and improves overall well-being.
Get Regular Checkups:
- Talk to your doctor about the appropriate age to start prostate screenings (PSA test and DRE).
- Early detection is crucial for successful treatment of prostate problems.
Practice Good Hygiene:
- Maintain proper hygiene to prevent urinary tract infections, which can sometimes lead to prostatitis.
Don’ts:
Smoke or Use Tobacco Products:
- Smoking increases the risk of many health problems, including prostate cancer.
Drink Excessive Amounts of Alcohol:
- Excessive alcohol consumption can negatively impact prostate health.
Ignore Urinary Symptoms:
- Difficulty urinating, frequent urination, or pain during urination can be signs of prostate problems. Seek medical attention if you experience these symptoms.
Delay Seeking Medical Attention:
- If you are concerned about your prostate health or have any symptoms, don’t hesitate to talk to your doctor. Early diagnosis and treatment can make a significant difference.
Terminology
Terminology
- Prostate: A walnut-sized gland in men, located below the bladder and in front of the rectum. It produces fluid that nourishes and protects sperm.
- Benign Prostatic Hyperplasia (BPH): A non-cancerous enlargement of the prostate gland, common in older men. It can cause urinary symptoms due to pressure on the urethra.
- Prostate Cancer: The most common cancer in men, characterized by the uncontrolled growth of cells in the prostate gland.
- Prostatitis: Inflammation of the prostate gland, often causing pain or discomfort in the pelvic area.
- Prostate-Specific Antigen (PSA): A protein produced by the prostate gland. Elevated PSA levels in the blood can indicate prostate problems, including cancer.
- Digital Rectal Exam (DRE): A physical exam where a doctor inserts a gloved finger into the rectum to feel the prostate for abnormalities.
- Transurethral Resection of the Prostate (TURP): A surgical procedure to remove excess prostate tissue that is blocking urine flow.
- Brachytherapy: A type of radiation therapy where radioactive seeds are implanted directly into the prostate gland to treat cancer.
- Prostatectomy: Surgical removal of the prostate gland, usually to treat prostate cancer.
- Erectile Dysfunction (ED): The inability to get or maintain an erection firm enough for sexual intercourse.
- Incontinence: The inability to control the bladder or bowels, leading to leakage of urine or stool.
- Pelvic Floor Muscles: Muscles that support the bladder, rectum, and other pelvic organs. Strengthening these muscles can help improve urinary control.
- Active Surveillance: A monitoring approach for low-risk prostate cancer, involving regular PSA tests and biopsies to watch for signs of progression.
- Hormone Therapy: Treatment that reduces the levels of male hormones (androgens) in the body, often used to treat prostate cancer.
References
Referances use For Article Prostate Problems
- https://www.nia.nih.gov/health/prostate-problems
- https://www.medicalnewstoday.com/articles/321079#managing-an-enlarged-prostate
- Homoeopathic Therpeutics By Lilienthal
- https://www.mayoclinic.org/diseases-conditions/benign-prostatic-hyperplasia/symptoms-causes/syc-20370087
- Kumar, V., Abbas, A. K., & Aster, J. C. (2021). Robbins and Cotran pathologic basis of disease (10th ed.). Elsevier.
- Campbell-Walsh Urology (12th ed.), Alan J. Wein, Louis R. Kavoussi, Andrew C. Novick, Alan W. Partin, Craig A. Peters, 2021, Elsevier.
Also Search As
Prostate Problems Also Search As
Online Search Engines:
- Use specific keywords:
- "homeopathy prostate problems"
- "homeopathic remedies for BPH"
- "homeopathic treatment for prostatitis"
- "homeopathy and prostate cancer"
- Include additional terms to narrow down the search:
- "research articles"
- "clinical trials"
- "case studies"
- "specific homeopathic remedies" (e.g., "Sabal serrulata", "Thuja occidentalis")
Homeopathic Websites and Databases:
- Visit websites of reputable homeopathic organizations and institutions.
- Search databases specifically dedicated to homeopathic research and literature.
- Look for articles published in peer-reviewed homeopathic journals.
Libraries:
- Consult librarians for assistance in finding relevant books and journals on homeopathy and prostate health.
- Check the library catalog for books and articles on the topic.
Homeopathic Practitioners:
- Ask your homeopathic practitioner for recommendations on reliable sources of information.
- Inquire about any specific research or case studies they may be aware of.
Tips for Effective Searching:
- Use a variety of search terms and combinations.
- Filter search results by date to find the most recent information.
- Pay attention to the credibility and source of the information.
- Look for articles published in reputable journals and websites.
- Consult with a qualified homeopathic practitioner to discuss any findings and get personalized advice.
By using these strategies, individuals can access a wealth of information on the homeopathic approach to prostate problems and make informed decisions about their health and treatment options.
Frequently Asked Questions (FAQ)
What is Prostate Problems?
Definition
The prostate is a small gland in men that helps make semen. In detail; It tends to grow larger as you get older. If your prostate gets too large, it can cause a number of health issues.
What are common Prostate Problems?
Common Prostate Problems:
Benign prostatic hyperplasia
Acute bacterial prostatitis
Chronic bacterial prostatitis
What are the symptoms of Prostate Problems?
Symptoms
Frequent urge to urinate
Need to get up many times during the night to urinate
Blood in urine or semen
Pain or burning urination
. When should I see a doctor about prostate problems?
Any of the symptoms mentioned above
Changes in your urinary habits
Blood in your urine or semen
Pain in your lower back, pelvis, or hips
How are prostate problems diagnosed?
Diagnosis can made on given criteria:
Medical history and physical exam, including a digital rectal exam (DRE)
Urine tests to check for infection or blood
Blood tests, such as a prostate-specific antigen (PSA) test
Imaging tests, such as ultrasound or MRI
What are the treatment options for prostate problems?
Treatment
Watchful waiting: Monitoring the condition for changes.
Medications: To shrink the prostate, relax the bladder muscles, or treat infections.
minimally invasive therapies: To destroy excess prostate tissue or widen the urethra.
Surgery: To remove part or all of the prostate gland.
How does homeopathy approach prostate problems?
Homeopathic Approach:
Homeopathy aims to stimulate the body’s natural healing abilities.
A homeopath will conduct a detailed consultation to understand your specific symptoms, medical history, and overall health.
Based on this, they’ll prescribe a personalized remedy aimed at addressing the root cause of your prostate issues.
Can homeopathy cure prostate problems?
Yes,
Homeopathy aims to support the body’s healing process and manage symptoms.
While some individuals may experience significant improvement, the effectiveness of homeopathy for prostate problems varies from person to person.
It’s crucial to have realistic expectations and continue any conventional treatments recommended by your doctor.
How long does it take to see results with homeopathy?
The response time to homeopathic treatment varies depending on the individual and the severity of the condition.
Some individuals may experience relief within a few weeks, while others may require a longer duration of treatment.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Prostate Problems?
Homoeopathic Medicines For Prostate Problems
Aesculus
Agnus Castus
Aloe
Baryta Carb
Causticum
Copiva
Chimaphila
Cyclamen
Kali Bichrom
Magnesia Carb
Selenium
Staphysagria
