Urinary Tract Infection (UTI)
Definition
Urinary Tract Infection (UTI) may be asymptomatic (subclinical infection) or symptomatic (disease). Thus, the term urinary tract infection encompasses a variety of clinical entities, including asymptomatic bacteriuria (ASB), cystitis, prostatitis, and pyelonephritis. [1]
Urinary tract infection (UTI) is a common term, but it can also be referred to as:
- Cystitis: When the infection is specifically in the bladder.
- Bladder infection: A more casual term for cystitis.
- Kidney infection: If the infection spreads to the kidneys, it’s called pyelonephritis.
Please note that UTI is the most common and widely understood term for this condition.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Urinary Tract Infection (UTI)
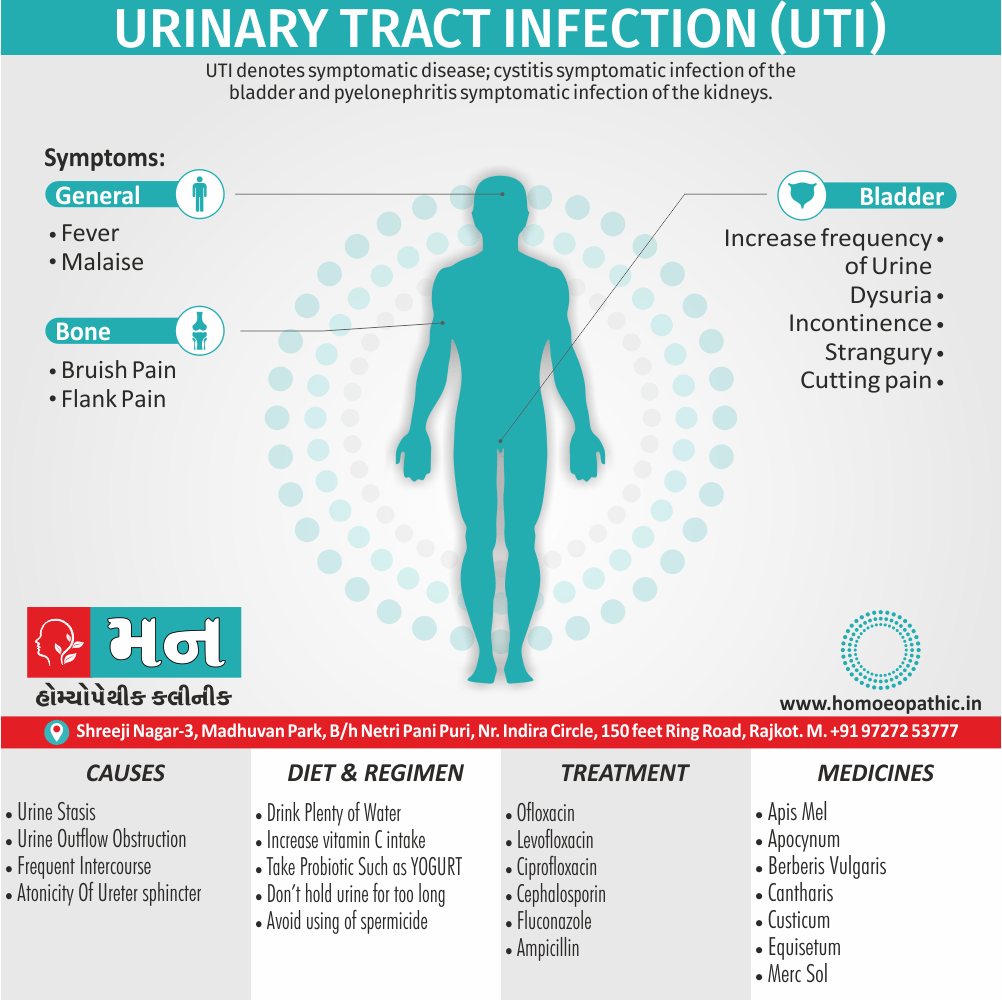
The term UTI denotes symptomatic disease; cystitis, symptomatic infection of the bladder; and pyelonephritis, symptomatic infection of the kidneys.
Uncomplicated UTI refers to acute cystitis or pyelonephritis in nonpregnant outpatient women without anatomic abnormalities or instrumentation of the urinary tract; the term complicated UTI encompasses all other types of UTI.
Recurrent UTI is not necessarily complicated; individual episodes can be uncomplicated and treated as such. Catheter-associated bacteriuria can be either symptomatic (CAUTI) or asymptomatic.
Except among infants and the older people, UTI occurs far more commonly in females than in males.
During the neonatal period, the incidence of UTI is slightly higher among males than among females because male infants more commonly have congenital urinary tract anomalies.
After 50 years of age, obstruction from prostatic hypertrophy becomes common in men, and the incidence of UTI is almost as high among men as among women.
Between 1 year and ~50 years of age, UTI and recurrent UTI are predominantly diseases of females.
The prevalence of ASB is ~5% among women between ages 20 and 40 and may be as high as 40–50% among older people of all genders
As many as 50–80% of women in the general population acquire at least one UTI during their lifetime—uncomplicated cystitis in most cases.[1]
Epidemiology
Epidemiology
Urinary tract infections (UTIs) are a common health concern in India, affecting individuals across various age groups and genders. However, the epidemiology can vary based on factors such as geographical location, socioeconomic conditions, and healthcare access.
Reference:
- Christy VR (2019) Epidemiology of urinary tract infection in south India. Biomed Res Clin Prac, 2019 doi: 10.15761/BRCP.1000190 Volume 4: 2-5.
This study, conducted in South India in 2019, offers insights into the prevalence and patterns of UTIs in that region.
Key findings from the study:
- Prevalence: UTIs were found to be prevalent across all age groups, including infants and the older.
- Gender: The study observed a higher prevalence of UTIs in females, particularly in the reproductive age group and post-menopausal stage.
- Risk factors: Lifestyle changes, poor personal hygiene, nutritional deficiencies, catheter use, unclean baby napkins, and immune deficiency were identified as contributing factors to UTIs in the study area.
Additional points to consider:
- While this study provides valuable data on the epidemiology of UTIs in South India, further research is needed to understand the nationwide prevalence and variations across different regions.
- Factors such as antibiotic resistance patterns and the impact of UTIs on public health also require ongoing investigation.
Please note:
- It’s important to remember that the epidemiology of UTIs can evolve over time, and the findings from this 2019 study may not fully reflect the current situation.
- Always consult with a healthcare professional for personalized advice and treatment regarding UTIs.
Remember, I cannot provide medical advice. If you have any concerns about UTIs, please consult a healthcare professional.
Causes
Causes of Urinary Tract Infection (UTI)
- Urinary tract infections are caused by microorganisms — usually bacteria — that enter the urethra and bladder, causing inflammation and infection.
- Though a UTI most commonly happens in the urethra and bladder, bacteria can also travel up the ureters and infect your kidneys.
- More than 90% of bladder infection (cystitis) cases are caused by E. coli, a bacterium normally found in the intestines.
- Some women are more likely to get UTIs because of their genes.
- The shape of their urinary tracts makes others more likely to be infected.
- Women with diabetes may be at higher risk because their weakened immune systems make them less able to fight off infections.
- Other conditions that can boost your risk include hormone changes, multiple sclerosis, and anything that affects urine flow, such as kidney stones, a stroke, and a spinal cord injury.[3]
Types
Types
Classification of Urinary Tract Infection (UTI)
An infection can happen in different parts of your urinary tract.
Each type has a different name, based on where it is.
Infection of the bladder (cystitis) i.e.:
- This type of UTI is usually caused by Escherichia coli (E. coli), a type of bacteria commonly found in the gastrointestinal (GI) tract.
- However, sometimes other bacteria are responsible.
- Sexual intercourse may lead to cystitis, but you don’t have to be sexually active to develop it.
- All women are at risk of cystitis because of their anatomy — specifically, the short distance from the urethra to the anus and the urethral opening to the bladder.
- You might also have lower belly pain and cloudy or bloody urine.
Infection of the urethra (urethritis) i.e.:
- This type of UTI can occur when GI bacteria spread from the anus to the urethra.
- Also, because the female urethra is close to the vagina, sexually transmitted infections, such as herpes, gonorrhoea, chlamydia and mycoplasma, can cause urethritis.
- This can cause a discharge and burning when you pee.
Pyelonephritis i.e.:
Risk Factors
Risk factor of Urinary Tract Infection (UTI)
Urinary tract infections are common in women, and many women experience more than one infection during their lifetimes. Risk factors specific to women for UTIs include:
- Female anatomy- A woman has a shorter urethra than a man does, which shortens the distance that bacteria must travel to reach the bladder.
- Sexual activity- Sexually active women tend to have more UTIs than do women who aren’t sexually active. Having a new sexual partner also increases your risk.
- Certain types of birth control- Women who use diaphragms for birth control may be at higher risk, as well as women who use spermicidal agents.
- Menopause– After menopause, a decline in circulating estrogen causes changes in the urinary tract that make you more vulnerable to infection.
- Urinary tract abnormalities- Babies born with urinary tract abnormalities that don’t allow urine to leave the body normally or cause urine to back up in the urethra have an increased risk of UTIs.
- Blockages in the urinary tract- Kidney stones or an enlarged prostate can trap urine in the bladder and increase the risk of UTIs.
- A suppressed immune system
- Catheter use- People who can’t urinate on their own and use a tube (catheter) to urinate have an increased risk of UTIs.[3]
- A recent urinary procedure.Urinary surgery or an exam of your urinary tract that involves medical instruments can both increase your risk of developing a urinary tract infection.[3]
Pathogenesis
Pathogenesis
Urinary tract infections (UTIs) arise from a complex interplay of host and bacterial factors, involving several key steps:
- Colonization: Uropathogenic bacteria, predominantly Escherichia coli, colonize the periurethral area and ascend the urethra.
- Adherence: Bacterial adhesins, such as fimbriae and pili, bind to specific receptors on uroepithelial cells, enabling attachment and resisting urine flow.
- Invasion: Bacteria invade uroepithelial cells, causing tissue damage and inflammation. Intracellular bacterial communities may form, contributing to recurrent infections.
- Ascension: Bacteria ascend to the bladder, causing cystitis. Further ascension to the kidneys can result in pyelonephritis, a more severe infection.
- Host response: The host immune system responds to infection, but excessive inflammation can worsen tissue damage.
Please note: I cannot provide medical advice. If you have any concerns about UTIs, consult a healthcare professional.[5]
Pathophysiology
Pathophysiology of Urinary Tract Infection (UTI)
- The urinary tract can be viewed as an anatomic unit united by a continuous column of urine extending from the urethra to the kidneys.
- In the majority of UTIs, bacteria establish infection by ascending from the urethra to the bladder.
- Continuing ascent up the ureter to the kidney is the pathway for most renal parenchymal infections.
- However, introduction of bacteria into the bladder does not inevitably lead to sustained and symptomatic infection.
- The interplay of host, pathogen, and environmental factors determines whether tissue invasion and symptomatic infection will ensue.
- Any foreign body in the urinary tract, such as a urinary catheter or stone, provides an inert surface for bacterial colonization.
- Abnormal micturition and/or significant residual urine volume promotes true infection. In the simplest of terms, anything that increases the likelihood of bacteria entering the bladder and staying there increases the risk of UTI.
- Bacteria can also gain access to the urinary tract through the blood stream.
- However, hematogenous spread accounts for <2% of documented UTIs and usually results from bacteremia caused by relatively virulent organisms, such as Salmonella and S. aureus.
- Indeed, the isolation of either of these pathogens from a patient without a catheter or other instrumentation warrants a search for a bloodstream source.
- Hematogenous infections may produce focal abscesses or areas of pyelonephritis within a kidney and result in positive urine cultures.
- The pathogenesis of candiduria is distinct in that the hematogenous route is common.
- The presence of Candida in the urine of a non-instrumented immunocompetent patient implies either genital contamination or potentially widespread visceral dissemination.[1]
Clinical Features
Clinical Features
The clinical presentation of urinary tract infections (UTIs) can vary depending on the site of infection and the patient’s age and underlying health conditions. However, some common symptoms include:
Lower UTI (cystitis):
- Dysuria (painful urination)
- Frequency (increased urge to urinate)
- Urgency (strong, sudden urge to urinate)
- Suprapubic pain (discomfort in the lower abdomen)
- Hematuria (blood in the urine)
- Cloudy or foul-smelling urine
Upper UTI (pyelonephritis):
Please note:
- I cannot provide medical advice.
- If you experience any of these symptoms, please seek professional medical evaluation.[5]
Sign & Symptoms
Sign & Symptoms of Urinary Tract Infection (UTI)
- A strong, persistent urge to urinate
- A burning sensation when urinating
- Passing frequent, small amounts of urine
- Urine that appears cloudy
- Urine that appears red, bright pink or cola-coloured — a sign of blood in the urine
- Strong-smelling urine
- Pelvic pain, in women — especially in the center of the pelvis and around the area of the pubic bone. [3]
Clinical Examination
Clinical Examination
The clinical examination for suspected urinary tract infections (UTIs) typically involves:
- Vital signs: Measuring temperature, blood pressure, and pulse rate to assess for signs of systemic infection (fever, tachycardia).
- Abdominal examination: Palpation of the abdomen for tenderness over the suprapubic area (suggestive of cystitis) or costovertebral angle tenderness (suggestive of pyelonephritis).
- Pelvic examination (in women): May be performed to assess for signs of vaginal or cervical infection that could contribute to UTI symptoms.
- Rectal examination (in men): May be performed to assess for prostate tenderness or enlargement, which could contribute to UTI symptoms.
- Neurological examination: May be performed to assess for neurological deficits that could contribute to voiding dysfunction and increase the risk of UTIs.[5]
Please note:
- I cannot provide medical advice.
- The specific components of the clinical examination may vary depending on the patient’s presentation and the clinician’s judgment.
- If you have any concerns about UTIs, consult a healthcare professional.
Diagnosis
Diagnosis of Urinary Tract Infection (UTI)
Tests and procedures used to diagnose urinary tract infections include:
Analyzing a urine sample i.e.
- Your doctor may ask for a urine sample for lab analysis to look for white blood cells, red blood cells or bacteria.
- To avoid potential contamination of the sample, you may be instructed to first wipe your genital area with an antiseptic pad and to collect the urine midstream.
- The Urine Dipstick Test, Urinalysis, and Urine Culture Useful diagnostic tools include the urine dipstick test and urinalysis, both of which provide point-of-care information, and the urine culture, which can retrospectively confirm a prior diagnosis.
Growing urinary tract bacteria in a lab i.e.
- Lab analysis of the urine is sometimes followed by a urine culture.
- This test tells your doctor what bacteria are causing your infection and which medications will be most effective.
Creating images of your urinary tract i.e.
- If you are having frequent infections that your doctor thinks may be caused by an abnormality in your urinary tract, you may have an ultrasound, a computerized tomography (in other words, CT) scan or magnetic resonance imaging (MRI).
- Your doctor may also use a contrast dye to highlight structures in your urinary tract.
Using a scope to see inside your bladder i.e.
- If you have recurrent UTIs, your doctor may perform a cystoscopy, using a long, thin tube with a lens (cystoscope) to see inside your urethra and bladder.
- The cystoscope is inserted in your urethra and passed through to your bladder.[3]
Differential Diagnosis
Differential Diagnosis
When evaluating a patient with suspected UTI, it is important to consider other conditions that can present with similar symptoms. These differential diagnoses may include:
- Vaginitis: Inflammation of the vagina, often caused by fungal or bacterial infections, can cause dysuria and vaginal discharge.
- Urethritis: Inflammation of the urethra, often caused by sexually transmitted infections, can cause dysuria and urethral discharge.
- Interstitial cystitis/painful bladder syndrome: A chronic bladder condition causing bladder pain and urinary urgency/frequency, often without evidence of infection.
- Urolithiasis (kidney stones): Stones in the urinary tract can cause flank pain, hematuria, and sometimes dysuria.
- Pyelonephritis: While an upper UTI, pyelonephritis may present with more systemic symptoms like fever, chills, and flank pain, requiring prompt evaluation and treatment.
- Prostatitis: Inflammation of the prostate gland can cause dysuria, pelvic pain, and sometimes fever.
Please note: I cannot provide medical advice. If you’re experiencing any symptoms, please seek professional medical evaluation.[5]
Complications
Complications of Urinary Tract Infection (UTI)
- Recurrent infections, especially in women who experience two or more UTIs in a six-month period or four or more within a year.
- Permanent kidney damage from an acute or chronic kidney infection (pyelonephritis) due to an untreated UTI.
- Increased risk in pregnant women of delivering low birth weight or premature infants.
- Urethral narrowing (stricture) in men from recurrent urethritis, previously seen with gonococcal urethritis.
- Sepsis, a potentially life-threatening complication of an infection, especially if the infection works its way up your urinary tract to your kidneys.[3]
Investigations
Investigations
The diagnosis of urinary tract infections (UTIs) typically involves a combination of clinical assessment and laboratory investigations. These investigations may include:
- Urinalysis: A dipstick test and microscopic examination of the urine can detect the presence of white blood cells (pyuria), red blood cells (hematuria), nitrites (indicating the presence of certain bacteria), and leukocyte esterase (an enzyme released by white blood cells).
- Urine culture: A urine sample is cultured in a laboratory to identify the specific bacteria causing the infection and determine its antibiotic susceptibility.
- Blood tests: May be performed in cases of suspected pyelonephritis or in patients with severe symptoms to assess for signs of systemic infection (elevated white blood cell count, C-reactive protein).
- Imaging studies: May be indicated in certain cases, such as recurrent UTIs, suspected complications (e.g., kidney stones, abscess), or atypical presentations. These may include ultrasound, CT scan, or MRI.[5]
Please note:
- I cannot provide medical advice.
- The specific investigations required may vary depending on the patient’s presentation and the clinician’s judgment.
- If you have any concerns about UTIs, consult a healthcare professional.
Treatment
Treatment of Urinary Tract Infection (UTI)
Antibiotics usually are the first line treatment for urinary tract infections.
Simple infection
Drugs commonly recommended for simple UTIs include i.e.:
- Trimethoprim/sulfamethoxazole (e.g. Bactrim, Septra, others)
- Fosfomycin (Monurol)
- Nitrofurantoin (e.g. Macrodantin, Macrobid)
- Cephalexin (Keflex)
- Ceftriaxone
The group of antibiotic medicines known as fluoroquinolones — such as ciprofloxacin (Cipro), levofloxacin and others — isn’t commonly recommended for simple UTIs, as the risks of these medicines generally outweigh the benefits for treating uncomplicated UTIs.
In some cases, such as a complicated UTI or kidney infection, your doctor might prescribe a fluoroquinolone medicine if there are no other treatment options.
Often, UTI symptoms clear up within a few days of starting treatment. But you may need to continue antibiotics for a week or more. Take the entire course of antibiotics as prescribed.
For an uncomplicated UTI that occurs when you’re otherwise healthy, your doctor may recommend a shorter course of treatment, such as taking an antibiotic for one to three days. But whether this short course of treatment is enough to treat your infection depends on your particular symptoms and medical history.
Your doctor may also prescribe a pain medication (analgesic) that numbs your bladder and urethra to relieve burning while urinating, but pain usually is relieved soon after starting an antibiotic.
Frequent infections
If you have frequent UTIs, your doctor may make certain treatment recommendations, such as:
- Low-dose antibiotics, initially for six months but sometimes longer
- Self-diagnosis and treatment, if you stay in touch with your doctor
- A single dose of antibiotic after sexual intercourse if your infections are related to sexual activity
- Vaginal estrogen therapy if you’re postmenopausal
Severe infection
For a severe UTI, you may need treatment with intravenous antibiotics in a hospital. [3]
Prevention
Prevention of Urinary Tract Infection (UTI)
You can take these steps to reduce your risk of urinary tract infections:
- Drink plenty of liquids, especially water
- Drink cranberry juice
- Wipe from front to back
- Empty your bladder soon after intercourse
- Avoid potentially irritating feminine products
- Change your birth control method. [3]
Homeopathic Treatment
Homeopathic Treatment of Urinary Tract Infection (UTI)
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Urinary Tract Infection (UTI)
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Medicines:
Apis mellifica
- The symptoms of scanty urine always lead one to consider whether Apis is or is not the remedy, for although Apis produces scanty urine there are number of other drugs that will do the same thing.
- The keynotes for Apis in urinary affections are scanty or suppressed urine, drowsiness, oedema in in various parts, thirstlessness and suffocation on lying down.
- The urine is dark, highly albuminous, and contains casts, so it is readily seen how Apis may correspond to any form of Bright’s disease.
- In difficult micturition of children Apis is often a useful remedy. It has frequent desire, with the passage of a few drops at a time.
- Among other symptoms are great irritation at the neck of the bladder and incontinence of urine. It is also the remedy to be thought of in retained urine or inflamed bladder after abuse of Cantharis.
Apocynum cannabinum
- Apocynum seems to act somewhat on the kidneys and give rise to various dropsical conditions. It produces a scanty urine, which is light in Color, or, as it is given, sherry-coloured.
- Its first effect is to produce a copious diuresis; this is followed by the scantiness of urine which results in dropsy.
- It also produces an incontinence and may be useful in enuresis.
- A sinking bruised feeling at the stomach is an indication for its use.
Berberis vulgaris
- Burning sensation in the urinary bladder.
- A feeling as if the urine has not completely passed after urinating.
- Thick, bright red urine.
- Presence of mucus in the urine.
- Soreness in kidney area especially while stooping.
- Pain in bladder, thighs and loins on urinating.
- Frequent urge to urinate.
- Stitching pain in testicles.
- Shooting pain in urethra, which extends upward.
- A feeling of pressure on the bladder on urinating.
- Presence of slimy sediment in the urine.
Cantharis
- An intolerable urge to urinate.
- Presence of blood in the urine.
- Cutting and burning pain in the renal region.
- Emission of urine in drops, cutting pain after passing urine.
- Presence of membranous scales in the urine.
- Burning and stinging pain in the kidney region.
- Pressing pain in the kidneys which is relived by pressing on the head of penis.
- Inflammation of the kidney and urethra.
- Symptoms get worse on touching the affected are and on urinating.
Clematis Erecta
- Frequent urination with low urine output and interrupted flow of urine so the urine falls in drops.
- Inability to pass all the urine.
- A tingling sensation in the urethra after urinating.
- Constriction in the urethra.
- Post void dribbling.
- Pain in urethra, which gets worse at night.
- Milky or frothy urine.
- Stitching pain in urethra and abdomen.
- Itching in the genitals.
- Symptoms get worse with warmth and at night.
Sarsaparilla
- Scanty and sandy urine.
- Severe pain in the urethra at the end of urination.
- Dribbling of urine while sitting.
- Tenderness in the bladder.
- Pain in the right kidney.
- Passing urine in a thin and feeble stream.
- Low urine output and frequent urination along with passing hard stools.
- Presence of thread like flakes in the urine.
- Burning sensation in the urethra after urination.
- Presence of stones in the bladder.
- Symptoms get worse after urinating and damp weather.
Pulsatilla
- Increased desire to urinate, which gets worse at night and while lying down.
- Burning pain in the urethra during and after urination.
- Involuntary emission of urine at night.
- Involuntary discharge of urine while coughing or passing wind.
- Pain in bladder after urination.
- Presence of blood and mucus in the urine.
- Weakness in the loins while urinating.
- Feeling pressure in urethra and bladder.
- Symptoms get worse from warmth and after eating anything, better with use of cold applications. [2]
Diet & Regimen
Diet & Regimen of Urinary Tract Infection (UTI)
- Drink Plenty of Water
- Increase vitamin C intake
- Take a healthy diet and try to consume nutritious and fibre rich food items.
- Avoid food items which are too salty, spicy or sugary.
- Take Probiotic Such as Yogurt, Fermented Food
- Good Bathroom & Hygiene habit
- Don’t hold urine for too long
- Peeing after sexual intercourse
- Avoid using of spermicide
- When you use the toilet wipe front to back.[3]
Do’s and Don'ts
Do’s & Don’ts
UTI Do’s and Don’ts:
Do’s:
- Drink plenty of fluids: Water is best, but unsweetened cranberry juice may also help. Fluids flush bacteria from your system.
- Urinate frequently: Don’t hold your urine. Frequent urination helps to wash bacteria out of the urinary tract.
- Wipe front to back: After using the toilet, wipe from front to back to prevent bacteria from the anus from entering the urethra.
- Urinate after sex: This helps flush out bacteria that may have entered the urethra during intercourse.
- Take the full course of antibiotics: If prescribed, complete the entire course of antibiotics even if you start to feel better.
- Consider over-the-counter pain relief: Acetaminophen or ibuprofen can help relieve pain and fever associated with UTIs.
- Wear loose-fitting cotton underwear: This allows air circulation and helps keep the area dry.
- Practice good hygiene: Wash the genital area daily with mild soap and water.
Don’ts:
- Don’t delay treatment: See a doctor if you suspect you have a UTI. Untreated UTIs can lead to serious complications.
- Don’t drink alcohol or caffeine: These can irritate the bladder and worsen symptoms.
- Don’t use feminine hygiene products: Douching, feminine sprays, and scented soaps can disrupt the natural balance of bacteria in the vagina and increase the risk of UTIs.
- Don’t wear tight-fitting clothes: Tight clothes can trap moisture and create a breeding ground for bacteria.
- Don’t hold your urine: Holding urine allows bacteria to multiply in the bladder.
- Don’t have sex until the infection is cleared: Sex can irritate the urethra and worsen symptoms.
Note: These are general guidelines. If you have concerns about a UTI, consult a healthcare professional for personalized advice and treatment.
Terminology
Terminology
Common terminologies
- UTI (Urinary Tract Infection): An infection that can occur anywhere along the urinary tract, which includes the kidneys, ureters, bladder, and urethra.
- Cystitis: Inflammation of the bladder, often caused by a bacterial infection.
- Pyelonephritis: A more serious type of UTI that affects the kidneys.
- Urethritis: Inflammation of the urethra, often caused by a sexually transmitted infection.
- Bacteriuria: The presence of bacteria in the urine.
- Dysuria: Painful or burning sensation during urination.
- Frequency: Increased need to urinate.
- Urgency: A sudden, strong urge to urinate.
- Hematuria: Blood in the urine.
- Pyuria: The presence of white blood cells (pus) in the urine, indicating inflammation or infection.
- Nitrites: A byproduct of certain bacteria that can be detected in the urine.
- Leukocyte esterase: An enzyme produced by white blood cells that can be detected in the urine.
- Antibiotics: Medications used to treat bacterial infections.
- Uropathogens: Bacteria that cause UTIs.
- Catheter-associated UTI (CAUTI): A UTI that develops in a person who has a urinary catheter.
- Recurrent UTI: Multiple UTIs occurring within a certain period of time.
- Complicated UTI: A UTI that occurs in a person with an underlying medical condition or structural abnormality of the urinary tract.
- Uncomplicated UTI: A UTI that occurs in a healthy individual with a normal urinary tract.
Remember, these are just some of the common terminologies used in articles about UTIs. The specific terms used may vary depending on the focus of the article and the intended audience.
Here are some common terminologies and their meanings used in homeopathic articles about UTIs, along with some additional terms that might be encountered:
Basic Terminology:
- Cystitis: Inflammation of the bladder, the most common type of UTI.
- Urethritis: Inflammation of the urethra, often associated with STIs but can also be caused by other factors.
- Nephritis/Pyelonephritis: Inflammation of the kidneys, a more serious form of UTI that can lead to complications if untreated.
- Tenesmus: A painful, persistent urge to urinate even when the bladder is empty.
- Strangury: Slow and painful urination with a feeling of incomplete emptying.
- Dysuria: Painful or burning sensation during urination.
- Haematuria: Blood in the urine.
Homeopathic Concepts:
- Repertory: A reference book used by homeopaths to find remedies based on specific symptoms.
- Materia Medica: A collection of descriptions of homeopathic remedies and their effects on the body.
- Constitutional Remedy: A remedy chosen based on the patient’s overall physical and mental characteristics, not just the specific symptoms of the UTI.
- Acute Prescribing: Selecting a remedy based on the immediate and intense symptoms of the UTI.
- Miasm: A predisposition to certain types of diseases, believed to be inherited or acquired, and influencing the choice of remedies.
- Potency: The strength or dilution of a homeopathic remedy.
- Aggravation: A temporary worsening of symptoms after taking a remedy, sometimes seen as a positive sign of healing.
- Proving: A process where healthy individuals take a substance to observe its effects and create a symptom picture for the remedy.
Specific Remedies Often Mentioned in UTI Articles:
- Cantharis: Burning pain, intense urgency, and frequent urination with small amounts.
- Sarsaparilla: Painful urination, especially at the end, with sand-like sediment in the urine.
- Staphysagria: UTI after sexual intercourse or suppressed emotions.
- Nux vomica: Irritable, impatient individuals with frequent urging and ineffectual urination.
- Pulsatilla: Gentle, emotional individuals with changeable symptoms and a desire for company.
- Apis mellifica: Stinging, burning pains with scanty urine and swelling.
- Mercurius solubilis: Frequent urination with offensive odor and a tendency to profuse sweating.
- Equisetum: Constant urging with much urine but little relief.
Remember, this is not an exhaustive list and the specific terminologies used may vary depending on the article.
Disclaimer: Homeopathy is a complementary therapy and should not be used as a replacement for conventional medical treatment for UTIs. Always consult a qualified healthcare professional for diagnosis and treatment.
References
References use for Article Urinary Tract Infection (UTI)
- Harrisons_Principles_of_Internal_Medicine-_19th_Edition-_2_Volume
- Therapeutic Pocket Book
- https://www.mayoclinic.org/diseases-conditions/urinary-tract-infection/symptoms-causes/syc
Christy VR (2019) Epidemiology of urinary tract infection in south India. Biomed Res Clin Prac, 2019 doi: 10.15761/BRCP.1000190 Volume 4: 2-5.
- Urinary Tract Infections: Molecular Pathogenesis and Clinical Management
Edition: 1st Edition
Writers: Matthew A. Mulvey, PhD; Scott J. Hultgren, PhD; and Ann E. Stapleton, MD
(2014), Publication: ASM Press
Also Search As
Also Search As
People can search for homeopathic articles on UTIs in several ways:
Online Search Engines:
Using specific keywords:
- "homeopathy UTI treatment"
- "homeopathic remedies for cystitis"
- "homeopathic medicine for urinary tract infection"
- "homeopathic approach to UTIs"
- Include specific remedy names if known (e.g., "Cantharis for UTI")
Specifying the type of information they need:
- "homeopathic case studies on UTIs"
- "homeopathic research on UTIs"
- "homeopathic self-care for UTIs"
- "homeopathic FAQs on UTIs"
Using advanced search options:
- Specify file type (e.g., PDF) to find downloadable articles
- Use quotation marks to search for exact phrases
- Exclude certain words with the minus sign (e.g., "homeopathy UTI -allopathy")
Homeopathic Websites and Resources:
- Visit websites of homeopathic organizations and clinics.
- Search databases of homeopathic journals and publications.
- Check blogs and articles written by homeopathic practitioners.
Social Media and Forums:
- Follow homeopathic groups and pages on social media.
- Participate in online forums and discussions about homeopathy.
- Ask questions and seek recommendations from other users.
Libraries and Bookstores:
- Look for books on homeopathy and UTIs.
- Browse the health and wellness sections for relevant magazines and journals.
Additional tips:
- Use reliable sources: Look for information from reputable homeopathic organizations, practitioners, and publications.
- Cross-reference information: Consult multiple sources to get a well-rounded understanding of the topic.
- Be specific in your search terms: The more specific your keywords, the more relevant the search results will be.
- Consult a homeopath: For personalized advice and treatment recommendations, it’s always best to consult a qualified homeopathic practitioner.
By utilizing these search strategies, people can find valuable homeopathic information on UTIs that suits their specific needs and interests.
There are several ways to search for information about UTIs (Urinary Tract Infections), catering to different needs and preferences:
Online Search Engines:
- Using Specific Keywords: Search with phrases like "UTI symptoms," "UTI treatment," "UTI prevention," "UTI causes," "UTI in women," "UTI in men," or "UTI in children" to find general information.
- Adding Specific Details: Refine your search by including additional details like "UTI during pregnancy," "UTI with diabetes," "UTI antibiotics," or "UTI home remedies" to find information relevant to your situation.
- Using Medical Websites: Search on reputable websites like Mayo Clinic, WebMD, NHS, or Healthdirect for reliable and evidence-based information.
- Searching for Images: Use image search to find visual representations of UTI symptoms, anatomy, or diagnostic tests.
- Using Videos: Search for educational videos on platforms like YouTube to understand UTI visually.
Medical Databases and Journals:
- PubMed: Search for scholarly articles and research papers on UTIs.
- Other Medical Databases: Consider using databases like Cochrane Library or Embase for specific research purposes.
Healthcare Professionals:
- Consulting Your Doctor: Talk to your doctor or a healthcare professional for personalized advice, diagnosis, and treatment options.
- Asking a Pharmacist: Pharmacists can provide information about over-the-counter medications and answer questions about prescription medications for UTIs.
Books and Libraries:
- Medical Textbooks: Consult medical textbooks or reference books for in-depth information about UTIs.
- Libraries: Visit your local library to find books and articles on UTIs.
Support Groups and Online Communities:
- Online Forums and Groups: Connect with others who have experienced UTIs to share experiences, ask questions, and find support.
- Social Media: Follow health organizations or patient advocacy groups on social media for updates and information.
Remember:
- Use Reliable Sources: Make sure the information you find comes from reputable sources.
- Be Specific: The more specific your search terms, the more relevant the results will be.
- Consult a Professional: If you have any concerns about UTIs, always consult a healthcare professional for personalized advice and treatment recommendations.
By utilizing these various search methods, you can access a wide range of information about UTIs and make informed decisions about your health.
Frequently Asked Questions (FAQ)
What is Urinary Tract Infection?
UTI may be asymptomatic (subclinical infection) or symptomatic (disease). Thus, the term urinary tract infection encompasses a variety of clinical entities, including asymptomatic bacteriuria (ASB), cystitis, prostatitis, and pyelonephritis.
Give the types of Urinary Tract Infection?
- Infection of the bladder (cystitis)
- Infection of the urethra (urethritis)
- Pyelonephritis
What causes Urinary Tract Infection?
- Microorganisms usually bacteria
- Genes
- Shape of their urinary tracts
- Women with diabetes
- Hormone changes
- Multiple sclerosis
What are the symptoms of Urinary Tract Infection?
- A strong, persistent urge to urinate
- A burning sensation when urinating
- Passing frequent, small amounts of urine
- Urine that appears cloudy
- Urine that appears red, bright pink or cola-coloured
- Strong-smelling urine
- Pelvic pain
Homeopathic Medicines used by Homeopathic Doctors in treatment of Urinary Tract Infection?
Homeopathic Medicines
- Apis mellifica
- Apocynum cannabinum
- Berberis vulgaris
- Cantharis
- Clematis Erecta
- Sarsaparilla
- Pulsatilla
