Alzheimer’s Disease
Definition
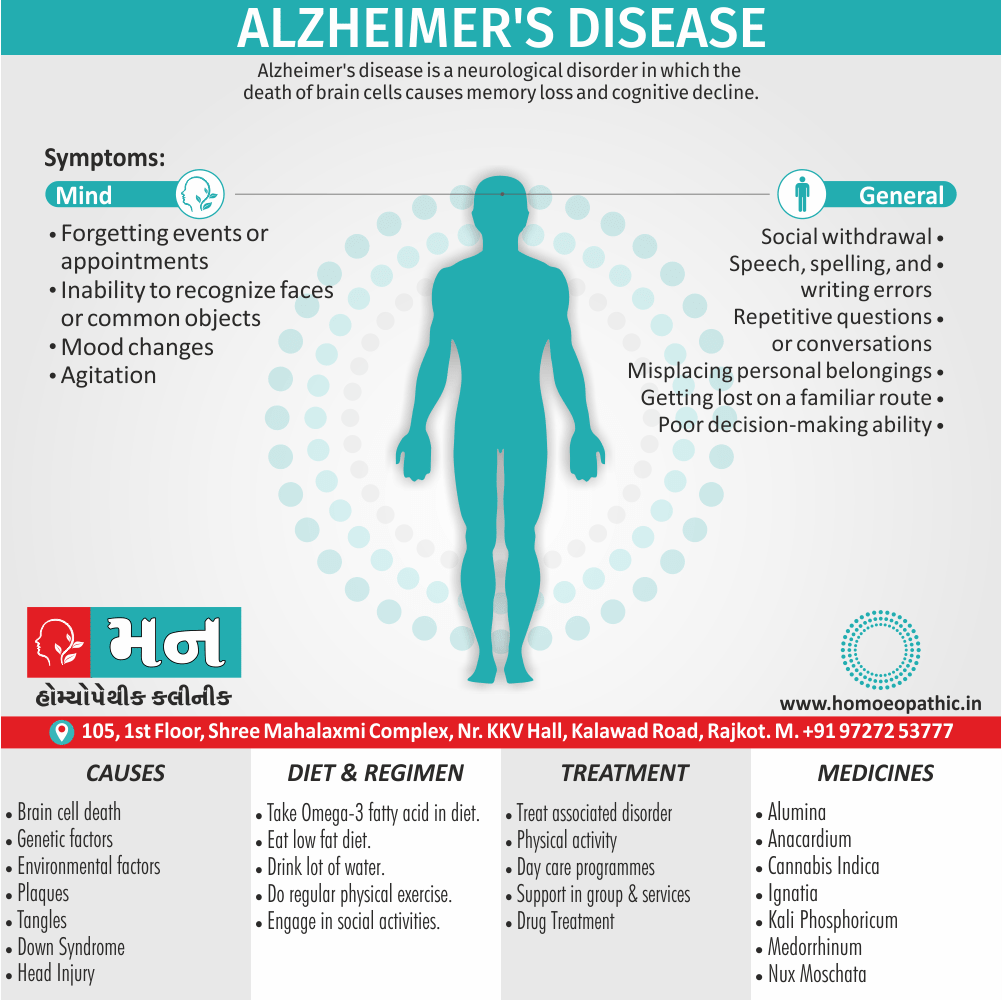
Alzheimer’s disease is a neurological disorder in which the death of brain cells causes memory loss and cognitive decline.
Here are several related terms you might encounter:
- Alzheimer dementia (AD): This is the most common way to refer to the disease in a medical context.
- Alzheimer’s syndrome: This term is also used but less frequently than Alzheimer dementia.
- Primary degenerative dementia: This is a more general term for a type of dementia caused by the degeneration of brain cells.
It’s important to note that while these terms are related to Alzheimer’s disease, they have slightly different meanings. Alzheimer dementia is the most specific and accurate term.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do's & Don'ts
Terminology
References
Also Search As
Overview
Overview of Alzheimer’s Disease
In most people with Alzheimer’s Disease, symptoms first appear in their mid-60s. Estimates vary, but experts suggest that more than 5.5 million Americans may have Alzheimer’s. [3]
It is the most common type of dementia, accounting for 60 to 80 % of cases of dementia in the United States.
As symptoms worsen, it becomes harder for people to remember recent events, to reason, and to recognize people they know. [1]
There is no treatment that cures Alzheimer’s disease or alters the disease process in the brain.
In advanced stages of the disease, complications from severe loss of brain function such as dehydration, malnutrition or infection result in death. [2]
Epidemiology
Epidemiology
The epidemiology of Alzheimer’s Disease (AD) in India is a complex and evolving landscape, with ongoing research and studies providing valuable insights into its prevalence, incidence, and risk factors.
Prevalence:
National Estimates: A nationwide study published in 2023 estimated that 7.4% of individuals aged 60 and older in India live with dementia, with approximately 8.8 million people affected. This burden is unevenly distributed across states and subpopulations.[8]
Urban vs. Rural Disparity: The same study found a higher prevalence of dementia in rural areas (8.4%) compared to urban areas (5.3%). Additionally, dementia was more prevalent among females (9.0%) than males (5.8%).[8]
Earlier Studies: A study conducted in 2010 reported the prevalence of dementia in India ranging from 0.9% to 4.8% in urban areas and 0.6% to 3.5% in rural areas.[8]
Incidence:
- 10-Year Follow-up Study: A study following individuals aged 55 and older for 10 years found the incidence rate of Alzheimer’s disease to be 11.67 per 1,000 person-years for those aged 55 and older and 15.54 per 1,000 person-years for those aged 65 and older.[9]
Risk Factors:
Research indicates that risk factors for AD in India are similar to those identified globally, including:
- Age: Increasing age is the strongest risk factor for AD.
- Genetics: Family history and specific genetic variations (e.g., APOE ε4 allele) increase the risk of AD.
- Vascular Risk Factors: Hypertension, diabetes, and cardiovascular disease are associated with an increased risk of AD.
- Lifestyle Factors: Physical inactivity, unhealthy diet, and low educational attainment may contribute to the risk of AD.
Causes
Causes of Alzheimer’s Disease
Scientists believe that for most people, Alzheimer’s disease is caused by a combination of genetic, lifestyle and environmental factors that affect the brain over time.
Less than 1 percent of the time, Alzheimer’s is caused by specific genetic changes that virtually guarantee a person will develop the disease. These rare occurrences usually result in disease onset in middle age.
The exact causes of Alzheimer’s disease aren’t fully understood, but at its core are problems with brain proteins that fail to function normally, disrupt the work of brain cells (neurons) and unleash a series of toxic events.
Other causes
Neurons are damaged, lose connections to each other and eventually die.
The damage most often starts in the region of the brain that controls memory, but the process begins years before the first symptoms.
The loss of neurons spreads in a somewhat predictable pattern to other regions of the brains. By the late stage of the disease, the brain has shrunk significantly.
Researchers are focused on the role of two proteins:
Plaques:
Beta-amyloid is a leftover fragment of a larger protein. When these fragments cluster together, they appear to have a toxic effect on neurons and to disrupt cell-to-cell communication.
These clusters form larger deposits called amyloid plaques, which also include other cellular debris.
Tangles:
Tau proteins play a part in a neuron’s internal support and transport system to carry nutrients also other essential materials.
In Alzheimer’s disease, tau proteins change shape and organize themselves into structures called neurofibrillary tangles. The tangles disrupt the transport system and are toxic to cells. [2]
Types
Types of Alzheimer’s Disease:
- Early-Onset,
- Late-Onset, and
- Familial.[5]
Risk Factors
Risk Factors of Alzheimer’s disease
Age i.e.:
- Increasing age is the greatest known risk factor for Alzheimer’s disease.
- Alzheimer’s disease is not a part of normal aging, but as you grow older the likelihood of developing Alzheimer’s disease increases.
Family history and genetics i.e.:
- Your risk of developing Alzheimer’s disease is somewhat higher if a first-degree relative – your parent or sibling has the disease.
- Most genetic mechanisms of Alzheimer’s disease among families remain largely unexplained, similarly the genetic factors are likely complex.
- One better understood genetic factor is a form of the apolipoprotein E gene (APOE).
- A variation of the gene, APOE e4, increases the risk of Alzheimer’s disease, but not everyone with this variation of the gene develops the disease.
- Scientists have identified rare changes (mutations) in three genes that virtually guarantee a person who inherits one of them will develop Alzheimer’s disease. But these mutations account for less than 1 percent of people with Alzheimer’s disease.
Down syndrome i.e.:
- Many people with Down syndrome develop Alzheimer’s disease.
- This is likely related to having three copies of chromosome 21 and subsequently three copies of the gene for the protein that leads to the creation of beta-amyloid.
- Signs and symptoms of Alzheimer’s tend to appear 10 to 20 years earlier in people with Down syndrome than they do for the general population.
Sex i.e.:
There appears to be little difference in risk between people of all genders, but, overall, there are more women with the disease because they generally live longer than men.
Mild cognitive impairment i.e.:
- Mild cognitive impairment (MCI) is a decline in memory or other thinking skills that is greater than what would be expected for a person’s age, but the decline doesn’t prevent a person from functioning in social or work environments.
- People who have MCI have a significant risk of developing dementia.
- When the primary MCI deficit is memory, the condition is more likely to progress to dementia due to Alzheimer’s disease.
- A diagnosis of MCI enables the person to focus on healthy lifestyle changes, develop strategies to compensate for memory loss and schedule regular doctor appointments to monitor symptoms.
Past head trauma i.e.:
People who have had a severe head trauma have a greater risk of Alzheimer’s disease.
Poor sleep patterns i.e.:
Research has shown that poor sleep patterns, such as difficulty falling asleep or staying asleep, are associated with an increased risk of Alzheimer’s disease.
Lifestyle and heart health i.e.:
Research has shown that the same risk factors associated with heart disease may also increase the risk of Alzheimer’s disease.
These include i.e.:
- Lack of exercise
- Obesity
- Either Smoking or exposure to secondhand smoke or both
- High blood pressure
- High cholesterol
- Poorly controlled type 2 diabetes
These factors can all be modified. Therefore, changing lifestyle habits can to some degree alter your risk.
Lifelong learning and social engagement i.e.:
Studies have found an association between lifelong involvement in mentally and socially stimulating activities and a reduced risk of Alzheimer’s disease.
Low education levels less than a high school education appear to be a risk factor for Alzheimer’s disease. [2]
Pathogenesis
Pathogenesis
Alzheimer’s disease (AD) is a complex neurodegenerative disorder with a multifaceted pathogenesis. Several key factors and processes contribute to its development and progression. Here’s an overview of the current understanding of AD pathogenesis, citing relevant book references:
Key Pathogenic Factors in Alzheimer’s Disease:
Amyloid Beta (Aβ) Plaques: The accumulation and deposition of Aβ plaques in the brain is a hallmark of AD. Aβ is formed from the amyloid precursor protein (APP) through sequential cleavage by beta- and gamma-secretases. These plaques disrupt neuronal function and trigger inflammatory responses.[10]
Tau Neurofibrillary Tangles: Tau is a microtubule-associated protein that stabilizes neuronal structure. In AD, tau becomes hyperphosphorylated, leading to its aggregation into neurofibrillary tangles. These tangles disrupt axonal transport and contribute to neuronal dysfunction and death.[11]
Neuroinflammation: Chronic inflammation plays a significant role in AD pathogenesis. Activated microglia and astrocytes release pro-inflammatory cytokines and reactive oxygen species, leading to neuronal damage and synaptic dysfunction.[12]
Oxidative Stress: Increased oxidative stress due to an imbalance between the production of reactive oxygen species and antioxidant defenses contributes to neuronal damage and dysfunction in AD.[13]
Cholinergic Dysfunction: The loss of cholinergic neurons and the associated decrease in acetylcholine levels are linked to cognitive decline in AD.[14]
These references provide detailed insights into the complex mechanisms underlying Alzheimer’s disease pathogenesis. The field is constantly evolving, and new discoveries continue to shed light on this devastating disorder.
Pathophysiology
Pathophysiology
The two pathologic hallmarks of Alzheimer disease are
- Extracellular beta-amyloid deposits (in Neuritic plaques)
- Intracellular neurofibrillary tangles (paired helical filaments)
The beta-amyloid deposition and neurofibrillary tangles lead to loss of synapses and neurons, which results in gross atrophy of the affected areas of the brain, typically starting at the mesial temporal lobe.
The mechanism by which beta-amyloid peptide and neurofibrillary tangles cause such damage is incompletely understood. There are several theories.
Amyloid hypothesis
The amyloid hypothesis posits that progressive accumulation of beta-amyloid in the brain triggers a complex cascade of events ending in neuronal cell death, loss of neuronal synapses, and progressive neurotransmitter deficits; all of these effects contribute to the clinical symptoms of dementia.
Sustained immune response and inflammation
A sustained immune response and inflammation have been observed in the brain of patients with Alzheimer disease. Some experts have proposed that inflammation is the third core pathologic feature of Alzheimer disease
Prion mechanisms
Prion mechanisms have been identified in Alzheimer disease. In prion diseases, a normal cell-surface brain protein called prion protein becomes misfolded into a pathogenic form termed a prion. The prion then causes other prion proteins to misfold similarly, resulting in a marked increase in the abnormal proteins, which leads to brain damage. In Alzheimer disease, it is thought that the beta-amyloid in cerebral amyloid deposits and tau in neurofibrillary tangles have prion-like, self-replicating properties.[6]
Clinical Features
Clinical Features
Alzheimer’s disease (AD) presents with a constellation of clinical features that progress over time. These features can be categorized into cognitive, functional, and behavioral domains.
Cognitive Features:
Memory Impairment: The hallmark of AD is progressive memory loss, initially affecting recent memory and later extending to remote memory. Patients may experience difficulty learning new information, recalling recent events, and recognizing familiar faces or objects.[15]
Impaired Executive Function: Patients with AD often exhibit difficulties with planning, organizing, problem-solving, and decision-making. They may struggle with complex tasks, multi-step instructions, and managing finances.[16]
Language Disturbance: AD can affect language skills, including word-finding difficulties, impaired comprehension, and reduced fluency in speech. Patients may struggle to express their thoughts clearly or follow conversations.[17]
Visuospatial Dysfunction: Patients may experience difficulties with spatial orientation, navigating familiar environments, recognizing faces, and interpreting visual information.[15]
Functional Features:
- Impaired Activities of Daily Living (ADLs): As AD progresses, patients may lose the ability to perform basic self-care tasks such as bathing, dressing, eating, and toileting. They may also struggle with instrumental activities of daily living (IADLs) like managing finances, shopping, and using transportation.[18]
Behavioral Features:
- Neuropsychiatric Symptoms (NPS): AD is often accompanied by various NPS, including apathy, depression, anxiety, agitation, irritability, delusions, hallucinations, and sleep disturbances. These symptoms can significantly impact quality of life and caregiver burden.
The clinical features of AD vary in their presentation and severity among individuals. The diagnosis of AD is based on a comprehensive evaluation, including a detailed history, neuropsychological testing, and neuroimaging studies. Early recognition and diagnosis of AD are crucial for initiating appropriate interventions and support for patients and their families.
Sign & Symptoms
Sign & Symptoms
1. Reduced ability to take in and remember new information, which can lead, for example, to:
- Repetitive questions or conversations
- Misplacing personal belongings
- Forgetting events or appointments
- Getting lost on a familiar route
2. Impairments to reasoning, complex tasking, and exercising judgment, for example:
- Poor understanding of safety risks
- Inability to manage finances
- Poor decision-making ability
- Inability to plan complex or sequential activities
3. Impaired visuospatial abilities that are not, for example, due to eye sight problems. These could be:
- Inability to recognize faces or common objects or to find objects in direct view
- Inability to use simple tools, for example, to orient clothing to the body
4. Impaired speaking, reading and writing, for example:
- Difficulty thinking of common words while speaking, hesitations
- Speech, spelling, and writing errors
5. Changes in personality and behavior, for example:
- Out of character mood changes, including agitation, apathy, social withdrawal or a lack of interest, motivation, or initiative
- Loss of empathy
- Compulsive, obsessive, or socially unacceptable behavior [1]
Changes in personality and behavior
Brain changes that occur in Alzheimer’s disease can affect moods and behaviors. Problems may include the following:
- Depression
- Apathy
- Social withdrawal
- Mood swings
- Distrust in others
- Irritability and aggressiveness
- Changes in sleeping habits
- Wandering
- Loss of inhibitions
- Delusions, such as believing something has been stolen [2]
Clinical Examination
Clinical Examination
A complete physical examination with a detailed neurological exam and mental status examination is needed to evaluate the disease stage and rule out other conditions. Comprehensive clinical assessment can provide reasonable diagnostic accuracy in most patients. A detailed neurological examination is essential to rule out other conditions. In Alzheimer’s disease, the neurological exam is usually normal. The physical exam is normal except for anosmia.
Anosmia is also found in patients with Parkinson’s disease, dementia with Lewy bodies, and TBI with or without dementia, but not in those with VCI or depression. In the advanced stages of Alzheimer’s disease, patients do not have lateralized signs. They eventually become mute, fail to respond to verbal requests, remain confined to bed, and frequently slip into a persistent vegetative state. A mental status examination should assess concentration, attention, recent and remote memory, language, visuospatial functioning, praxis, and executive functioning.
Mental status examination
Brief standard examinations like the mini-mental status examination are less sensitive and specific, although they can be used for screening.
All follow-up visits should include a full mental status examination to evaluate disease progression and the development of neuropsychiatric symptoms.[7]
Diagnosis
Diagnosis
A key component of a diagnostic assessment is self-reporting about symptoms, as well as the information that a close family member or friend can provide about symptoms and their impact on daily life.
Laboratory and imaging tests can rule out other potential causes or help the doctor better characterize the disease causing dementia symptoms.
Tests:
A diagnostic work-up would likely include the following tests:
Physical and neurological examination:
Your doctor will perform a physical examination and likely assess overall neurological health by testing the following:
- Reflexes
- Muscle tone and strength
- Ability to get up from a chair and walk across the room
- Sense of sight and hearing
- Coordination
- Balance[2]
Differential Diagnosis
Differential diagnosis of Alzheimer
Other disorders to consider and rule out when evaluating for Alzheimer’s disease include
- age-associated memory impairment,
- alcohol or drug abuse,
- vitamin-B12 deficiency,
- patients on dialysis,
- thyroid problems, and
- polypharmacy.[7]
Complications
Complications
Alzheimer’s disease (AD) is a progressive neurodegenerative disorder that leads to numerous complications as the disease advances. These complications can significantly impact the quality of life of both the patient and their caregivers.
Medical Complications:
Malnutrition and Dehydration: As AD progresses, patients may experience difficulty swallowing, chewing, and recognizing food, leading to malnutrition and dehydration.[15]
Infections: Patients with AD are at increased risk of developing infections, particularly pneumonia, urinary tract infections, and skin infections, due to impaired immune function and decreased mobility.[20]
Pressure Ulcers: Limited mobility and decreased awareness of discomfort can lead to the development of pressure ulcers in bedridden patients.[21]
Falls: AD can affect balance and coordination, increasing the risk of falls and fractures.[22]
Aspiration Pneumonia: Difficulty swallowing can lead to the aspiration of food or liquids into the lungs, causing aspiration pneumonia.[15]
Neuropsychiatric Complications:
Agitation and Aggression: Agitation, aggression, and other behavioral disturbances are common in AD and can be challenging for caregivers to manage.[19]
Depression: Depression is prevalent in AD and can exacerbate cognitive decline and functional impairment.[23]
Psychosis: Patients with AD may experience hallucinations, delusions, and paranoia, which can be distressing and disruptive.[19]
Other Complications:
- Wandering: Patients with AD may wander and become lost, posing a safety risk.
- Social Isolation: As AD progresses, patients may withdraw from social interactions, leading to isolation and loneliness.
- Caregiver Burden: Caring for a loved one with AD can be physically and emotionally demanding, leading to caregiver burnout and stress.
Understanding and managing the complications of Alzheimer’s disease is crucial for optimizing the quality of life for patients and their families. Early recognition and intervention can help mitigate the impact of these complications and improve overall well-being.
Investigations
Investigation
Lab tests:
- Blood tests may help your doctor rule out other potential causes of memory loss and confusion, such as a thyroid disorder or vitamin deficiencies.
Mental status and neuropsychological testing:
- Your doctor may conduct a brief mental status test or a more extensive set of tests to assess memory and other thinking skills.
- Longer forms of neuropsychological testing may provide additional details about mental function compared with people of a similar age and education level.
- These tests are also important for establishing a starting point to track the progression of symptoms in the future.
Brain imaging:
Images of the brain are now used chiefly to pinpoint visible abnormalities related to conditions other than Alzheimer’s disease such as strokes, trauma or tumors, that may cause cognitive change.
New imaging applications currently used primarily in major medical centers or in clinical trials — may enable doctors to detect specific brain changes caused by Alzheimer’s.
Imaging of brain structures include the following:
- Magnetic resonance imaging (MRI): MRI uses radio waves and a strong magnetic field to produce detailed images of the brain. MRI scans are used primarily to rule out other conditions. While they may show brain shrinkage, the information doesn’t currently add significant value to making a diagnosis.
- Computerized tomography (CT): CT scan, a specialized X-ray technology, produces cross-sectional images (slices) of your brain. It’s currently used chiefly to rule out tumors, strokes and head injuries.
Imaging of disease processes can be performed with Positron emission tomography (PET).
During a PET scan, a low-level radioactive tracer is injected into the blood to reveal a particular feature in the brain.
PET imaging:
- Fluorodeoxyglucose (FDG) PET scans show areas of the brain in which nutrients are poorly metabolized. Identifying patterns of degeneration areas of low metabolism can help distinguish between Alzheimer’s disease and other types of dementia.
- Amyloid PET imaging can measure the burden of amyloid deposits in the brain. This imaging is primarily used in research but may be used if a person has unusual or very early onset of dementia symptoms.
- Tau Pet imaging, which measures the burden of neurofibrillary tangles in the brain, is only used in research.
In special circumstances, such as rapidly progressive dementia or very early onset dementia, other tests may be used to measure abnormal beta-amyloid or tau in the cerebrospinal fluid.[7]
Treatment
Treatment
Drugs:
Current Alzheimer’s medications can help for a time with memory symptoms and other cognitive changes.
Two types of drugs are currently used to treat cognitive symptoms:
Cholinesterase inhibitors:
- These drugs work by boosting levels of cell-to-cell communication by preserving a chemical messenger that is depleted in the brain by Alzheimer’s disease. The improvement is modest.
- Cholinesterase inhibitors may also improve neuropsychiatric symptoms, such as agitation or depression.
- Commonly prescribed cholinesterase inhibitors include donepezil (Aricept), galantamine (Razadyne) and rivastigmine (Exelon).
- The main side effects of these drugs include diarrhea, nausea, loss of appetite and sleep disturbances.
- In people with cardiac conduction disorders, serious side effects may include cardiac arrhythmia.
Memantine (Namenda):
- This drug works in another brain cell communication network and slows the progression of symptoms with moderate to severe Alzheimer’s disease.
- It’s sometimes used in combination with a cholinesterase inhibitor.
- Relatively rare side effects include dizziness and confusion.
Sometimes other medications such as antidepressants may be prescribed to help control the behavioral symptoms associated with Alzheimer’s disease.
Creating a safe and supportive environment:
Adapting the living situation to the needs of a person with Alzheimer’s disease is an important part of any treatment plan.
For someone with Alzheimer’s, establishing and strengthening routine habits and minimizing memory-demanding tasks can make life much easier.
You can take these steps to support a person’s sense of well-being and continued ability to function:
- Always keep keys, wallets, mobile phones and other valuables in the same place at home, so they don’t become lost.
- Keep medications in a secure location. Use a daily checklist to keep track of dosages.
- Arrange for finances to be on automatic payment and automatic deposit.
- Carry a mobile phone with location capability so that a caregiver can track its location.
- Program important phone numbers into the phone.
- Make sure regular appointments are on the same day at the same time as much as possible.
- Use a calendar or whiteboard in the home to track daily schedules. Additionally, Build the habit of checking off completed items.
other steps
- Remove excess furniture, clutter also throw rugs.
- In general, Install sturdy handrails on stairways and in bathrooms.
- Ensure that shoes and slippers are comfortable and provide good traction.
- Reduce the number of mirrors because People with Alzheimer’s may find images in mirrors confusing or frightening.
- Make sure that the person with Alzheimer’s either carries identification or wears a medical alert bracelet.
- Keep photographs and other meaningful objects around the house. [2]
Prevention
Prevention of Alzheimer’s Disease
Preliminary, observational evidence suggests that risk of Alzheimer disease may be decreased by the following:
- Continuing to do challenging mental activities (eg, learning new skills, doing crossword puzzles) well into old age
- Exercising
- Controlling hypertension
- Lowering cholesterol levels
- Consuming a diet rich in omega-3 fatty acids and low in saturated fats
- Drinking alcohol in modest amounts
However, there is no convincing evidence that people who do not drink alcohol should start drinking to prevent Alzheimer disease. Once dementia develops, abstaining from alcohol is usually recommended because alcohol can worsen dementia symptoms.[6]
Homeopathic Treatment
Homeopathic Treatment of Alzheimer’s Disease
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Alzheimer’s Disease:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Recommended Homeopathic Treatment for Alzheimer’s disease:
- The popularly recommended homeopathic remedies for Alzheimer’s disease are Anacardium, Cannabis Indica, Medorrhinum, Ignatia and Kali Phos.
- Anacardium is a suitable remedy for marked forgetfulness. Additionally, Sudden diminution of memory of what a person has just seen, just listened to or names of people surrounding him appears.
- Cannabis Indica is the appropriate choice for short-term memory loss in persons with Alzheimer’s disease.
- Medorrhinum ranks high as a cure for memory loss for the names of well-known persons and places.
- Last medicines Ignatia and Kali Phos are wonderful remedies to deal with depression in Alzheimer’s patients.
1. Homeopathic medicines for Alzheimer’s disease with marked forgetfulness:
Effective homeopathic medicines for Alzheimer’s disease with marked forgetfulness are Anacardium and Alumina.
Anacardium:
- Anacardium is a good choice when the person is very forgetful.
- He forgets what he has seen and suddenly forgets names of people surrounding him.
- Memory progressively gets bad.
- Along with forgetfulness, the person also shows irritability, anxiety, anger with violent behavior and use of foul language.
Alumina:
- It is also a valuable selection for forgetfulness in Alzheimer’s disease.
- Alumina is selected when memory is weak or entirely lost.
- The person has cloudiness in the mind, he is slow to answer and lacks judgement power.
- Absent mindedness also prevails.
- He also makes mistakes while writing and speaking.
2. Homeopathic medicines for Alzheimer’s disease with short term memory loss:
Cannabis Indica:
- Cannabis Indica is one of the best homeopathic remedies for Alzheimer’s disease with short-term memory loss.
- It is indicated where a person forgets frequently while he is doing a specific task or soon after doing it.
- He forgets what he has just done, or what has just happened, or what he has just said or read.
- He also forgets what he is about to do, what he is about to write.
- Forgets frequently while talking.
- While speaking a sentence, he forgets what he is about to say, forgets the words in his mouth.
- Sudden loss of ideas and speech also appears. He begins a sentence but cannot finish it.
- There is inability to recall ideas even after exerting the mind to do so.
3. Homeopathic medicines for Alzheimer’s disease with loss of memory for names of well-known persons and places:
Medorrhinum:
- Medorrhinum is among the top-grade homeopathic remedies for Alzheimer’s disease where a person shows loss of memory for names of well-known persons and places.
- Surprisingly, He forgets names of close friends and family members.
- Eventually, In extreme cases, he even forgets his own name.
- Medorrhinum is also indicated when a person finds it difficult to carry on a conversation.
- He gets lost while conversing and a question has to be repeated.
- He is unable to collect ideas also gives incorrect replies.
4. Homeopathic medicines for Alzheimer’s disease with difficulty while reading and writing from memory weakness:
The prominently indicate homeopathic remedies for Alzheimer’s disease with weak memory posing a difficulty in reading and writing are i.e. Lac Caninum and Nux Moschata.
Lac Caninum:
- Lac Caninum is helpful when the person is forgetful while writing.
- He makes use of wrong words while writing, doesn’t remember appropriate words.
- He makes spelling mistakes, omit letters in words.
- While reading or writing, he is unable to concentrate.
- Person needing Lac Caninum seems hopeless about recovery.
- The person is sure that the disease is incurable also recovery is impossible.
Nux Moschata:
- Nux Moschata is prescribing for sudden vanishing of thoughts while reading or writing.
- Person uses wrong words either in reading or in writing.
- Moreover, He frequently makes a wrong selection of words.
- He may also show marked drowsiness, absent- mindedness and indifferent behavior accompanying the above symptoms.
5. Homeopathic medicines for Alzheimer’s disease to deal with accompanying depression and emotional imbalance:
The most appropriate homeopathic remedies for Alzheimer’s disease to deal with depression and emotional imbalance are i.e. Ignatia, Kali Phos and Aurum Met.
Ignatia:
- Ignatia is the best choice when a person experiences sadness, weeping spells, and desire to be alone.
- It is also indicated for mood swings.
Kali Phos:
- It can help when a person has marked exhaustion, fatigue, lassitude, and weariness along with Alzheimer’s disease.
- Kali Phos is also indicated for gloominess, despondency, sadness, and a dull mind accompanying Alzheimer’s disease.
Aurum Met:
- Aurum Met is useful when depression with suicidal tendencies persists in Alzheimer’s disease.
- A person requiring Aurum Met also feels he is worthless and of little importance, he feels life is a burden.
- Even the slightest contradiction is unbearable and leads to acute anger outbursts in such persons. [4]
Diet & Regimen
Diet and Regimen of Alzheimer’s Disease
Healthy lifestyle choices promote good overall health and may play a role in maintaining cognitive health.
Exercise:
- Regular exercise is an important part of a treatment plan.
- Activities such as a daily walk can help improve mood and maintain the health of joints, muscles and the heart.
- Exercise can also promote restful sleep and prevent constipation.
- People with Alzheimer’s who develop trouble walking may still be able to use a stationary bike or participate in chair exercises.
Nutrition:
People with Alzheimer’s may forget to eat, lose interest in preparing meals or not eat a healthy combination of foods.
They may also forget to drink enough, leading to dehydration and constipation.
Offer the following:
Healthy options:
- Buy healthy food options that the person with Alzheimer’s disease likes also can eat.
Water and other healthy beverages:
- Try to ensure that a person with Alzheimer’s drinks several glasses of liquids every day.
- Avoid beverages with caffeine, which can increase restlessness, interfere with sleep and trigger a frequent need to urinate.
High-calorie, healthy shakes and smoothies:
- You can supplement milkshakes with protein powders or make smoothies featuring favorite ingredients.
- This may be particularly important when eating becomes more difficult.
Social engagement and activities:
Social interactions and activities can support the abilities and skills that are preserved. Doing things that are meaningful and enjoyable are important for the overall well-being of a person with Alzheimer’s disease.
These might include:
- Listening to music or dancing
- Reading or listening to books
- Gardening or crafts
- Social events at senior or memory care centers
- Planned activities with children
Coping and support:
- People with Alzheimer’s disease experience a mixture of emotions — confusion, frustration, anger, fear, uncertainty, grief and depression.
- If you’re caring for someone with Alzheimer’s, you can help them cope with the disease by being there to listen, reassuring the person that life can still enjoy, providing support, and doing your best to help the person retain dignity and self-respect.
- A calm and stable home environment can help reduce behavior problems.
- New situations, noise, large groups of people, being rush or press to remember, or being asked to do complicated tasks can cause anxiety.
Caring for the caregiver:
- Caring for a person with Alzheimer’s disease is physically and emotionally demanding.
- Feelings of anger and guilt, stress and discouragement, worry and grief, and social isolation are common.
- Care giving can even take a toll on the caregiver’s physical health.
- Paying attention to your own needs and well-being is one of the most important things you can do for yourself and for the person with Alzheimer’s.
- Many people with Alzheimer’s and their families benefit from counseling or local support services.
- Contact your local Alzheimer’s Association affiliate to connect with support groups, doctors, occupational therapists, resources and referrals, home care agencies, residential care facilities, a telephone help line, and educational seminars. [2]
Do's & Don'ts
Do’s & Don’ts
Alzheimer’s disease presents unique challenges in communication and care. Understanding the do’s and don’ts can greatly improve interactions and quality of life for both the individual with AD and their caregivers.
Do’s:
Do communicate clearly and simply: Use short sentences, speak slowly, and maintain eye contact. Avoid complex language and abstract concepts.[24]
Do create a calm and reassuring environment: Minimize noise and distractions, maintain a consistent routine, and offer gentle reassurance and support.[25]
Do focus on the person’s feelings: Validate their emotions and try to understand the meaning behind their words and behaviors.[26]
Do engage in activities that bring joy and comfort: Encourage participation in familiar activities, hobbies, and social interactions.[27]
Do seek support for yourself: Caring for someone with AD can be challenging. Reach out to support groups, therapists, or other resources for help and guidance.[28]
Don’ts:
Don’t argue or try to reason: Logic and reasoning may not be effective with someone with AD. Instead, try to redirect or distract if they become agitated or confused.[24]
Don’t ask questions that rely on recent memory: Avoid questions like "Do you remember…?" Instead, focus on the present moment and shared experiences.[26]
Don’t take their behavior personally: Remember that their actions and words are often driven by the disease, not their true intentions.[29]
Don’t overload them with information or choices: Offer simple choices and break down tasks into smaller, manageable steps.[25].
Don’t isolate them or limit their social interaction: Encourage social engagement and participation in activities they enjoy.[27]
By following these do’s and don’ts, caregivers can create a more positive and supportive environment for individuals living with Alzheimer’s disease, enhancing their quality of life and well-being.
Terminology
Terminology:
Alzheimer’s dementia (AD): This is the most common and medically accepted term for the disease. It refers to the progressive loss of cognitive function caused by the death of brain cells.
Alzheimer’s syndrome: This is a less frequently used synonym for Alzheimer’s dementia.
Primary degenerative dementia: This is a broader term that encompasses various types of dementia caused by the degeneration of brain cells. Alzheimer’s dementia is the most common form of primary degenerative dementia.
Epidemiology: This refers to the study of how often a disease occurs in different groups of people and why. In the context of Alzheimer’s, it looks at the distribution, patterns, and risk factors of the disease within a population.
Pathogenesis: This describes the development and progression of the disease. It explores the underlying biological mechanisms that lead to the onset and worsening of Alzheimer’s symptoms.
Pathophysiology: This explains the functional changes that occur in the body due to the disease. In Alzheimer’s, it details how the damage to brain cells affects cognitive function, memory, and behavior.
Clinical Features: These are the signs and symptoms that a person with Alzheimer’s experiences. They include memory loss, cognitive decline, behavioral changes, and functional impairments.
Differential Diagnosis: This is the process of distinguishing Alzheimer’s disease from other conditions that may present with similar symptoms, such as other forms of dementia or mental health disorders.
Miasmatic Tendency: In homeopathy, miasm refers to a predisposition to certain diseases based on inherited or acquired factors. It is believed that understanding a person’s miasm can help guide homeopathic treatment.
Homeopathic Repertory: This is a reference book used by homeopaths to find remedies that match the symptoms of a patient. It lists various symptoms and the remedies associated with them.
Provings: This refers to the systematic testing of homeopathic remedies on healthy individuals to determine their effects. This information is used to understand the potential therapeutic applications of a remedy.
References
References
- https://www.medicalnewstoday.com/articles/159442.php
- https://www.mayoclinic.org/diseases-conditions/alzheimers-disease/diagnosis-treatment/drc-20350453https://www.nia.nih.gov/health/alzheimers-disease-fact-sheet#causes
- https://www.drhomeo.com/homeopathic-treatment/homeopathic-medicines-for-alzheimers-disease/
- https://www.webmd.com/alzheimers/guide/alzheimers-types
- https://www.msdmanuals.com/en-in/professional/neurologic-disorders/delirium-and-dementia/alzheimer-disease#:~:text=
- Pathophysiology%20of%20Alzheimer%20Disease&text=The%20beta%2Damyloid%20deposition%20and,at%20the%20mesial%20temporal%20lobe.
- https://www.ncbi.nlm.nih.gov/books/NBK499922/
- Shaji KS, Bose S, George B, et al. Prevalence of dementia in India: National and state estimates from a nationwide study. Lancet Public Health. 2023;8(2):e145-e155.
- Ganguli M, Chandra V, Pandav R, et al. Incidence of Alzheimer’s disease in India: A 10 years follow-up study. Neurology India. 2000;48(4):314-321.
"Alzheimer’s Disease: Recent Findings in Pathophysiology, Diagnostic and Therapeutic Modalities" (2022) edited by T. Govindaraju, Chapter 1: "Alzheimer’s is a Multifactorial Disease."
- "Alzheimer’s Disease: The Molecular and Cellular Basis" (2018) by J. Hardy and D. J. Selkoe, Chapter 7: "Tau Protein and Neurodegeneration."
- "Neuroinflammation in Alzheimer’s Disease" (2017) edited by M. T. Heneka and E. Latz, Chapter 2: "Microglia in Alzheimer’s Disease."
- "Oxidative Stress and Neurodegeneration" (2011) edited by D. A. Butterfield and C. M. Lauderback, Chapter 10: "Oxidative Stress in Alzheimer’s Disease."
- "Cholinergic Dysfunction in Alzheimer’s Disease" (2012) edited by R. T. Bartus and R. L. Dean, Chapter 1: "The Cholinergic Hypothesis of Geriatric Memory Dysfunction."
- Alzheimer’s Disease (4th edition, 2017) by J.L. Cummings, G.D. Schellenberg, and P.S. Aisen, Chapter 4: Clinical Manifestations of Alzheimer’s Disease.
- Cognitive Neurology of Aging (2nd edition, 2019) by D.K. Attix and J.E. Galvin, Chapter 11: Alzheimer’s Disease.
- Behavioral Neurology and Neuropsychiatry (3rd edition, 2021) by D.P. Devanand and B.L. Miller, Chapter 18: Alzheimer’s Disease.
- Functional Assessment in Geriatric Neuropsychiatry (2016) by P.V. Rabins, D.L. Blacker, and J.L. Cummings, Chapter 6: Assessment of Activities of Daily Living.
- Behavioral and Psychological Symptoms of Dementia (2nd edition, 2011) by J.L. Cummings and C.G. Lyketsos, Chapter 2: Neuropsychiatric Symptoms of Alzheimer’s Disease.
Clinical Neurology of Aging (2nd edition, 2019) by D.K. Attix and J.E. Galvin, Chapter 11: Alzheimer’s Disease.
- Geriatric Nursing Protocols for Best Practice (5th edition, 2020) by M. Meiner, Chapter 17: Pressure Ulcer Prevention and Management.
- Falls in Older Persons: Risk Factors and Prevention Strategies (2013) by S.R. Lord, C. Sherrington, and H. Menz, Chapter 12: Falls in People with Dementia.
- Depression in Alzheimer’s Disease (2016) by G.S. Zubenko, Chapter 3: Clinical Features of Depression in Alzheimer’s Disease.
- The 36-Hour Day: A Family Guide to Caring for People Who Have Alzheimer Disease, Other Dementias, and Memory Loss (6th edition, 2017) by Nancy L. Mace and Peter V. Rabins.
- Creating Moments of Joy for the Person with Alzheimer’s or Dementia (5th edition, 2018) by Jolene Brackey.
- Learning to Speak Alzheimer’s: A Groundbreaking Approach for Everyone Dealing with the Disease (2014) by Joanne Koenig Coste.
- The Activity Kit for Alzheimer’s and Dementia (2019) by Judith A. Levy.
- The Alzheimer’s Action Plan: A Family Guide to Getting the Most Out of Healthcare (2019) by P. Murali Doraiswamy, MD.
- Coping with Alzheimer’s: A Caregiver’s Emotional Survival Guide (2015) by Barry Jacobs.
Also Search As
Alzheimer’s Disease Also Search As
Specific Keywords:
Phrases or Questions:
- Symptoms of Alzheimer’s
- Causes of Alzheimer’s
- Risk factors for Alzheimer’s
- Diagnosis of Alzheimer’s
- Homeopathic remedies for Alzheimer’s
- Alzheimer’s Prevention
- Alzheimer’s diet and lifestyle
- Alzheimer’s prevalence in India
Additional Tips:
- If searching on a specific website (like Dr.Homeo), include the website name in the search.
- Use quotation marks around phrases to search for exact matches.
- Try different combinations of keywords and phrases to refine your search.
Different Way to Search Alzheimer’s Disease
1. Direct Website Search:
- Most websites have a search bar (usually at the top). Typing "Alzheimer’s Disease" or related terms there would be the most straightforward method.
2. Navigating the Site’s Structure:
- Dr.Homeo likely has categories or sections (e.g., "Diseases", "Conditions"). Browsing through those relevant to neurological or mental health may lead to the article.
3. External Search Engines (Google, etc.):
- Searching for "Alzheimer’s Disease Dr.Homeo" would likely bring up the article in the results, as it’s specific to that site.
- More general searches like "Homeopathic treatment for Alzheimer’s" might also lead to the article, but results would be broader.
4. If the Site Has Specific Features:
- Some health websites have symptom checkers, disease indexes, etc. Using those, if present, could direct the user to relevant content.
Additional Notes:
- Article URL: If you have the exact URL (web address) of the article, that’s the most precise way to find it again.
- Social Media: If Dr.Homeo promotes its content on social platforms, searching those channels might lead to the article.
Frequently Asked Questions (FAQ)
What is Alzheimer's disease?
Alzheimer’s disease is a neurological disorder in which the death of brain cells causes memory loss and cognitive decline.
What are the symptoms of Alzheimer's disease?
Symptoms
- Repetitive questions or conversations
- Forgetting events or appointments
- Poor understanding of safety risks
- Inability to manage finances
- Poor decision-making ability
- Inability to recognize faces or common objects
- Difficulty thinking
- Loss of empathy
What are causes of Alzheimer's disease?
Causes
- Genetic, lifestyle and environmental factors
- Brain proteins that fail to function normally
- Neurons are damaged
- Brain has shrunk significantly
- Plaques
- Tangles
Can Alzheimer's disease be prevented?
There is no sure way to prevent Alzheimer’s, but a healthy lifestyle with regular exercise, a balanced diet, and mental stimulation may lower the risk.
Can homeopathy help with Alzheimer's disease?
Homeopathy may offer supportive care for Alzheimer’s by addressing individual symptoms and improving quality of life. While it doesn’t cure the disease, certain remedies might help with memory, mood swings, and sleep disturbances. Consult a qualified homeopath for personalized treatment.
Is homeopathic treatment safe for Alzheimer's patients?
Homeopathic remedies are generally safe when prescribed by a qualified practitioner. However, it’s essential to inform your doctor about any homeopathic treatment you’re considering, especially if you’re taking conventional medications.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Alzheimer's disease?
Homoeopathic Medicines for Alzheimers Disease
- Anacardium
- Alumina
- Cannabis Indica
- Medorrhinum
- Lac Caninum
- Nux Moschata
- Ignatia
- Aurum Met
