Amebiasis
Definition
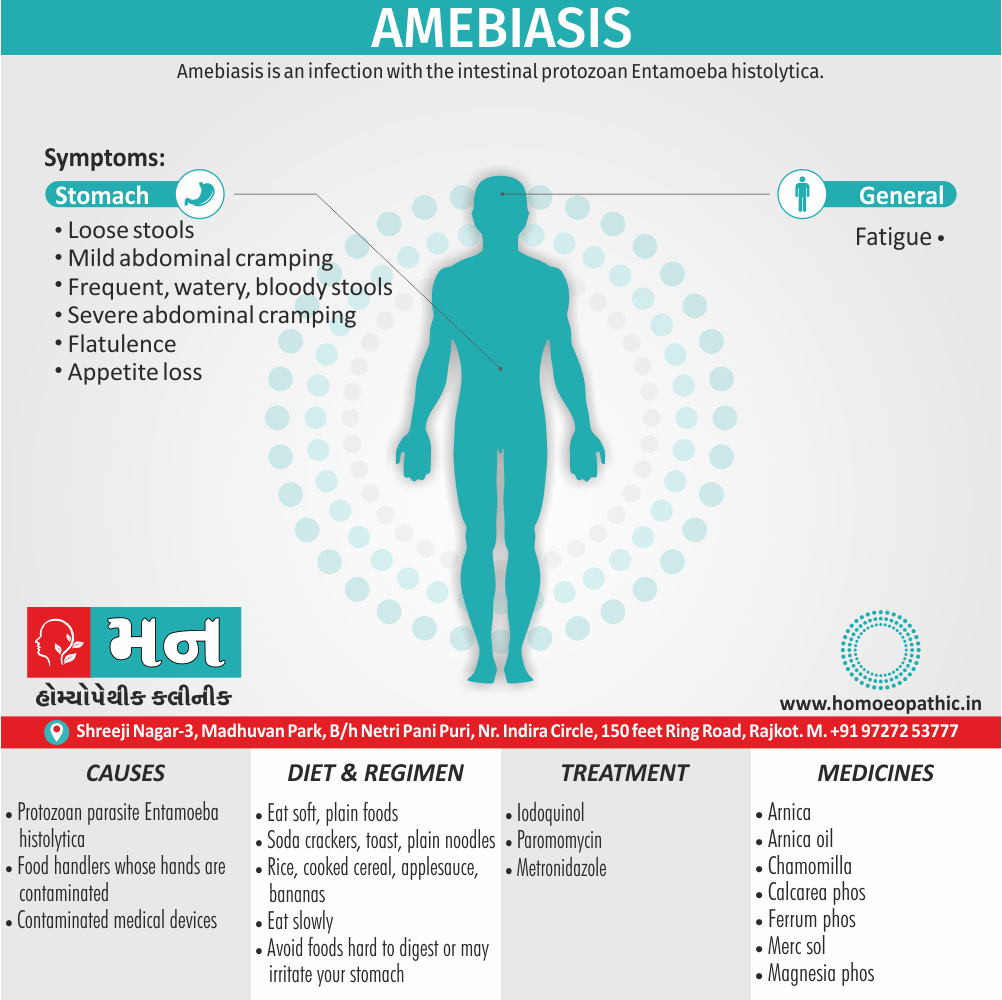
Amebiasis is an infection with the intestinal protozoan Entameba histolytica. About 90% of infections are asymptomatic, and the remaining 10% produce a spectrum of clinical syndromes ranging from dysentery to abscesses of the liver or other organs.[1]
Here are some synonyms of amebiasis:
More specific terms:
Alternative spellings:
- Amoebiasis: This is a common alternative spelling of amebiasis, particularly in British English.
- Amebiosis: This is a less frequent variant, but still encountered occasionally.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do's & Don'ts
Terminology
References
Also Search As
Overview
Overview
About 10% of the world’s population is infected with
Entamoeba, the majority with noninvasive Entamoeba dispar. Amebiasis results from infection with E. histolytica and is the third most common cause of death from parasitic disease (after schistosomiasis and malaria). Invasive colitis and liver abscesses are sevenfold
More common among men than among women; this difference has been attributed to a disparity in complement-mediated killing.
The wide spectrum of clinical disease caused by Entamoeba is due in part to the differences between these two infecting species. E. histolytica has unique isoenzymes, surface antigens, DNA markers, and virulence properties that distinguish it from other genetically related and morphologically identical species, such as E. dispar and E. moshkovskii.[1]
Asymptomatic carriers
Most asymptomatic carriers, including men who have sex with men (MSM) and patients with AIDS, harbor E. dispar and have self-limited infections. In this respect, E. dispar is dissimilar to other enteric pathogens such as Cryptosporidium and Cystoisospora belli, which can cause
Self-limited illnesses in immunocompetent hosts but devastating diarrhea in patients with AIDS. These observations indicate that E. dispar is incapable of causing invasive disease. Unlike E. dispar, E. histolytica can cause invasive disease, as demonstrated in recent reports from Korea, China, and India that suggest higher prevalences of amebic seroconversion, invasive amebiasis, and amebic liver abscesses among HIV-positive than HIV-negative patients.
Other Studies
In another study, 10% of asymptomatic patients who were colonized with E. histolytica went on to develop amebic colitis, while the rest remained asymptomatic and cleared the infection within 1 year.
The potential of E. moshkovskii to cause diarrhea, weight loss, and colitis was recently demonstrated in a mouse model of cecal infection. However, the pathogenic potential of this species is not clear. A prospective evaluation of children from the Mirpur community of
Dhaka, Bangladesh, found that most children who had diarrheal diseases associated with E. moshkovskii were simultaneously infected with at least one other enteric pathogen.
Areas of highest incidence of Entamoeba infection (due to inadequate sanitation and crowding) include most developing countries in the tropics, particularly Mexico, India, and nations of Central and South America, tropical Asia, and Africa. In a 4-year follow-up study of preschool children in a highly endemic area of Bangladesh, 80% of Children had at least one episode of E. histolytica infection and 53% had more than one episode.
Risk in developed countries
Naturally acquired immunity did develop but usually short-lived and correlated with the presence in the stool of secretory IgA antibody to the major adherence lectin galactose N-acetylgalactosamine (Gal/GalNAc). The main groups at risk for amebiasis in developed countries return travelers, recent immigrants, MSM, military personnel, and inmates of institutions. Data from the GeoSentinel Surveillance Network, which come from tropical medicine clinics on six continents, showed that, among long-term travelers (trip duration, >6 months), diarrhea due to E. histolytica was among the most common diagnoses.
LIFE CYCLE AND TRANSMISSION
- histolytica acquire by ingestion of viable cysts from focally contaminated water, food, or hands. Food-borne exposure is most prevalent and is particularly likely when food handlers are shedding cysts or food being grown with feces-contaminated soil, fertilizer, or water.
Besides the drinking of contaminated water, less common means of transmission include oral and anal sexual practices and—in rare instances—direct rectal inoculation through colonic irrigation devices.
Motile trophozoites are released from cysts in the small intestine and, in most patients, remain as harmless commensals in the large bowel. After encystation, infectious cysts are shed in the stool and can survive for several weeks in a moist environment.
In some patients, the trophozoites invade either the bowel mucosa, causing symptomatic colitis, or the bloodstream, causing distant abscesses of the liver, lungs, or brain. The trophozoites may not encyst in patients with active dysentery, and motile hematophagous trophozoites are frequently present
in fresh stools. Trophozoites are rapidly killed by exposure to air or stomach acid, however, and therefore cannot transmit infection.
Epidemiology
Epidemiology
The epidemiology of amebiasis in India is characterized by high prevalence and significant regional variations.
Prevalence of Amoebiasis and Associated Complications in India: A Systematic Review (2022)
This study found that the prevalence of amebiasis ranges from 3-23% in asymptomatic individuals, 0.64-11% in symptomatic patients, and 1-17.5% in HIV-infected individuals. The highest prevalence was observed in Tamil Nadu, Andaman, and Nicobar Islands, and North East India. The study also reported extraintestinal complications such as amoebic liver abscess, amoebic colitis, colonic perforation, and ameboma.[10]
Molecular Epidemiology of Amoebiasis: A Cross-Sectional Study among North East Indian Population (2015)
This study focused on the North East Indian population and found that the prevalence of Entamoeba histolytica was highest in Assam (18.2%), followed by Manipur (11.7%), Meghalaya (10.2%), and Tripura (8.2%). The study also identified poor living conditions, previous history of infection in family members, and unhygienic toilet facilities as significant risk factors for amoebiasis.[11]
(PDF) Prevalence of Amoebiasis and Associated Complications in India: A Systematic Review (2022)
This study, similar to the first reference, reported a prevalence range of 3-23% in asymptomatic individuals and highlighted the increased healthcare burden and potential fatality of extraintestinal complications.[12]
Epidemiology of amoebiasis | PPT – SlideShare (Year not specified)
This presentation states that amebiasis affects about 15% of the Indian population and emphasizes the role of poor sanitation, socioeconomic status, and contaminated food and water in the transmission of the disease.[13]
These studies collectively demonstrate that amebiasis remains a significant public health concern in India, with a high prevalence and a wide range of clinical manifestations. Further research and targeted interventions are needed to reduce the burden of this disease.
Causes
Cause
The cause of amebiasis is mainly the protozoan parasite Entamoeba histolytica. Some risk factors for amebiasis include consuming contaminated food or water, association with food handlers whose hands contaminate, contact with contaminated medical devices such as colonic irrigation devices, and being pregnant.[2]
Types
Types
Two forms of amoebiasis are recognized:
1.Firstly, Luminal amoebiasis where no clinical signs or symptoms are apparent
2.Secondly, Invasive amoebiasis where the trophozoites invade the intestinal mucosa to produce dysentery or amoeboma, and can spread in blood to give extraintestinal lesions such as liver abscess.[6]
Risk Factors
Risk factors for severe amebiasis include:
- Alcohol use.
- Cancer.
- Malnutrition.
- Older or younger age.
- Pregnancy.
- Recent travel to a tropical region.
- Use of corticosteroid medicine to suppress the immune system[5]
Pathogenesis
Pathgenesis
The pathogenesis of amebiasis is a complex process involving various factors contributing to the parasite’s ability to invade and cause disease in the human host.
The pathogenesis of amebiasis involves the following steps:
- Ingestion of cysts: The infective form of Entamoeba histolytica, the cyst, is ingested through contaminated food or water.
- Excystation: In the small intestine, the cyst wall is digested, releasing the motile trophozoite.
- Colonization: The trophozoites colonize the large intestine, multiplying and feeding on bacteria and tissue debris.
- Invasion: Some trophozoites invade the intestinal mucosa, using their surface lectins to bind to host cells and their proteolytic enzymes to degrade the extracellular matrix.
- Tissue damage: The invading trophozoites cause tissue damage, leading to the formation of characteristic flask-shaped ulcers.
- Extraintestinal spread: In some cases, trophozoites can enter the bloodstream and spread to other organs, most commonly the liver, causing amoebic liver abscess.[14]
The virulence of E. histolytica is determined by its ability to:
- Adhere to host cells: This is mediated by the parasite’s surface lectin, which binds to galactose and N-acetylgalactosamine residues on host cells.
- Lyse host cells: This is achieved by the parasite’s amoebapore, a pore-forming protein that inserts into the host cell membrane, causing cell death.
- Evade the host immune response: The parasite can resist complement-mediated lysis and phagocytosis.[15]
Pathophysiology
Pathophysiology of Amebiasis
Both trophozoites and cysts found in the intestinal lumen, but only trophozoites of E. histolytica invade tissue. The trophozoite is 20–60 μm in diameter also contains vacuoles and a nucleus with a characteristic central nucleolus.
In animals, depletion of intestinal mucus, diffuse inflammation, also disruption of the epithelial barrier precede trophozoite contact with the colonic mucosa. Trophozoites attach to colonic mucus also epithelial cells by their Gal/ GalNAc lectin.
The earliest intestinal lesions are micro ulcerations of the mucosa of the cecum, sigmoid colon, or rectum that release erythrocytes, inflammatory cells, and epithelial cells. Proctoscopy reveals small ulcers with heaped-up margins also normal intervening mucosa. Submucosal extension of ulcerations under viable-appearing surface mucosa causes the classic “flask-shaped” ulcer containing trophozoites at the margins of dead and viable tissues.
Although neutrophilic infiltrates may accompany the early lesions in animals, human intestinal infection mark by a paucity of inflammatory cells, probably in part because of the killing of neutrophils by trophozoites. Treated ulcers characteristically heal with little or no scarring. Occasionally, however, full-thickness necrosis and perforation occur.[2]
Clinical Features
Clinical Features
Amebiasis presents with a wide range of clinical features, from asymptomatic infection to severe invasive disease.
The clinical features of amebiasis can be classified as follows:
Asymptomatic infection: Most individuals infected with Entamoeba histolytica remain asymptomatic, with the parasite residing in the intestinal lumen without causing any symptoms.
Intestinal amebiasis: This manifests as amebic colitis, characterized by abdominal pain, bloody diarrhea, and tenesmus (a feeling of incomplete defecation). In severe cases, it can lead to fulminant colitis with toxic megacolon and perforation.
Extraintestinal amebiasis: This occurs when the parasite spreads beyond the intestines, most commonly to the liver, causing amoebic liver abscess. Symptoms include fever, right upper quadrant pain, and hepatomegaly. Less common sites of extraintestinal spread include the lungs, brain, and skin.[14]
This book adds that the clinical features of amebiasis can also vary depending on the host’s immune status. Immunocompromised individuals, such as those with HIV/AIDS or on immunosuppressive therapy, are at increased risk of severe amebiasis, including extraintestinal spread and complications.[16]
It is important to note that the clinical presentation of amebiasis can be nonspecific and may mimic other gastrointestinal or infectious diseases. Therefore, a thorough history, physical examination, and laboratory tests are essential for accurate diagnosis and timely treatment.
Sign & Symptoms
Clinical Examination
Clinical Examination
Amebiasis clinical examination findings can vary depending on the extent and severity of the infection.
The clinical examination of a patient with amebiasis may reveal the following:
- Intestinal amebiasis (amebic colitis):
- Abdominal tenderness, especially in the right lower quadrant
- Signs of peritoneal irritation (rebound tenderness, guarding)
- Hepatomegaly (enlarged liver) in some cases
- Amoebic liver abscess:
- Tender hepatomegaly with pain on percussion
- Fever
- Jaundice (yellowing of the skin and eyes) in a minority of cases[14]
The physical examination in amebiasis may also include:
- Digital rectal examination: May reveal tenderness and blood or mucus in the stool.
- Other findings: Depending on the site of extraintestinal involvement, may include lung findings (rales, decreased breath sounds), neurological deficits, or skin lesions.[16]
It’s important to note that these findings are not specific to amebiasis and can be seen in other gastrointestinal and infectious diseases. Therefore, a comprehensive evaluation, including laboratory tests (stool microscopy, serology) and imaging studies (ultrasound, CT scan), is necessary for a definitive diagnosis.
Diagnosis
Diagnosis
Entamoeba histolytica must be differentiated from other intestinal protozoa. Microscopic identification of cysts and trophozoites in the stool is the common method for diagnosing E. histolytica. Differentiation is based on morphologic characteristics of the cysts and trophozoites.
In addition, E. histolytica trophozoites can also be identified in aspirates or biopsy samples obtained during colonoscopy or surgery.
Immunodiagnosis -Antibody Detection-
a) Enzyme immunoassay (EIA) is most useful in patients with extra-intestinal disease (i.e., amoebic liver abscess) when organisms are not generally finding on stool examination.
b) Indirect hemagglutination (IHA).
If antibodies are not detectable in patients with an acute presentation of suspected amoebic liver abscess, a second specimen should be drawn 7-10 days later. If the second specimen does not show sero-conversion, other tests should be considered.
Detectable E. histolytica-specific antibodies may persist for years after successful treatment, so the presence of antibodies does not necessarily indicate acute or current infection.
Antigen Detection-
Antigen detection may be useful as an adjunct to microscopic diagnosis in detecting parasites and to distinguish between pathogenic and nonpathogenic infections.
Molecular Diagnosis-
Conventional Polymerase chain reaction (PCR)-In reference diagnosis laboratories, molecular analysis by PCR-based assays is the method of choice for discriminating between the pathogenic species (E. histolytica) also the nonpathogenic species (E. dispar).
Radiography, Ultrasonography, Computed tomography (in other words, CT) and Magnetic resonance imaging (MRI) can used for detection of liver abscess, cerebral amoebiasis.
Rectosigmoidoscopy and colonoscopy can provide diagnostic information in intestinal amoebiasis.[7]
Differential Diagnosis
Differential Diagnosis
The differential diagnosis for E. histolytica intestinal amebiasis includes i.e.:
- Bacterial pathogens i.e.: Shigella, Escherichia coli, Salmonella, Campylobacter, and Clostridioides difficile
- Inflammatory bowel disease
- Ischemic bowel disease
The differential diagnosis for E. histolytica extraintestinal amebiasis includes i.e.:
- Pyogenic liver abscess
- Echinococcal disease
- Malignancy[9]
Complications
Complications
Amebiasis, if left untreated or in severe cases, can lead to various complications.
The complications of amebiasis can be categorized as follows:
- Intestinal complications:
- Fulminant colitis: A severe form of colitis characterized by extensive inflammation and tissue destruction, which can lead to toxic megacolon (dilation of the colon) and perforation.
- Ameboma: A rare complication where a mass of inflammatory tissue forms in the colon, mimicking a tumor.
- Extraintestinal complications:
- Amoebic liver abscess: The most common extraintestinal complication, occurring when the parasite spreads to the liver and forms an abscess. This can cause fever, right upper quadrant pain, and hepatomegaly.
- Other extraintestinal abscesses: Less commonly, abscesses can form in other organs, such as the lungs, brain, and skin.
- Other complications:
- Peritonitis: Inflammation of the peritoneum (lining of the abdominal cavity), which can occur if an amebic abscess ruptures.
- Anemia: Due to blood loss from the intestines in cases of amebic colitis.[14]
That amebiasis can also lead to the following complications:
- Intussusception: A condition where one segment of the intestine telescopes into another, causing obstruction.
- Stricture: Narrowing of the intestinal lumen due to scarring from chronic inflammation.
- Pericarditis: Inflammation of the pericardium (the sac surrounding the heart), which can occur if an amoebic liver abscess ruptures into the pericardium.[16]
It is crucial to recognize and manage these complications promptly to prevent further morbidity and mortality associated with amebiasis.
Investigations
Investigation
- stool antigen detection
- PCR or qPCR of stool or liver abscess pus for E histolytica DNA
- serum antibody test
- stool microscopy
- colonoscopy
- liver ultrasound
- CXR[8]
Treatment
Treatment of Amebiasis
The drugs used to treat amebiasis can be classified according to their primary site of action. Luminal amebic ides poorly absorbed; they reach high concentrations in the bowel, but their activity limited to cysts and trophozoites close to the mucosa.
Only two luminal drugs are available in the United States i.e.:
Iodoquinol and paromomycin.
Indications for the use of luminal agents include eradication of cysts in patients with colitis or a liver abscess and treatment of asymptomatic asymptomatic individuals who pass cysts colonize with E. dispar, which does not warrant specific therapy. However, it is prudent to treat asymptomatic individuals who pass cysts unless E. dispar
Colonization can definitively demonstrated by specific antigen detection tests carriers.
The majority of Tissue amebic ides reach high concentrations in the blood and tissue after oral or parenteral administration. The development of nitroimidazole compounds, especially metronidazole, was a major advance in the treatment of invasive amebiasis. Patients with amebic colitis should treat with IV or oral metronidazole. Side effects include nausea, vomiting, abdominal discomfort, and a disulfiram- like reaction.
Another longer-acting imidazole compound, tinidazole, is also effective and available in the United States. All patients should also receive a full course of therapy with a luminal agent, since metronidazole does not eradicate cysts.
Resistance to metronidazole has selected in the laboratory but has not found in clinical isolates. Relapses are not uncommon and probably represent reinfection or failure to eradicate amebas from the bowel because of an inadequate dosage or duration of therapy.
AMEBIC LIVER ABSCESS
Metronidazole is the drug of choice for amebic liver abscess. Longer acting nitroimidazoles (tinidazole and ornidazole) have been effective as single-dose therapy in developing countries. With early diagnosis and therapy, mortality rates from uncomplicated amebic liver abscess are <1%. There is no evidence that combined therapy with two drugs is more effective than the single-drug regimen. Studies of South Africans with liver abscesses demonstrated that 72% of patients without intestinal symptoms had bowel infection with E. histolytica; thus, all treatment regimens should include a luminal agent to eradicate cysts and prevent further transmission. Amebic
Liver abscess recurs rarely.
More than 90% of patients respond dramatically to metronidazole therapy with decreases in both pain and fever within 72 h. Indications for aspiration of liver abscesses are (1) the need to rule out a pyogenic abscess, particularly in patients with multiple lesions; (2) the lack of a clinical response in 3–5 days; (3) the threat
of imminent rupture; and (4) the need to prevent rupture of left-lobe abscesses into the pericardium. There is no evidence that aspiration, even of large abscesses (up to 10 cm), accelerates healing. Percutaneous drainage may be successful even if the liver abscess has already ruptured. Surgery should reserve for instances of bowel perforation and rupture into the pericardium.
Prevention
Amebic infection spread by ingestion of food or water contaminated with cysts. Since an asymptomatic carrier may excrete up to 15 million cysts per day, prevention of infection requires adequate sanitation and eradication of cyst carriage. In high-risk areas, infection can minimized by the avoidance of unpeeled fruits and vegetables and the use of bottled water. Because cysts are resistant to readily attainable levels of chlorine, disinfection by iodination (tetraglycine hydroperiodide) recommend. There is no effective prophylaxis. [1]
Prevention
Prevention
Amoebiasis can be prevented and controlled both by non-specific and specific measures.
Non-specific measures are concerned with-
- Improved water supply– The cysts are not kill by chlorine in amount used for water disinfection. Water filtration and boiling are more effective than chemical treatment of water against amoebiasis.
- Sanitation–Safe disposal of human excreta coupled with the sanitary practice of washing hands after defecation and always before handling and consuming food.
- Food safety– Uncooked fruits and vegetables should wash thoroughly with safe water, peel fruits, and boil vegetables prior to eating.Measures should also include the protection of food and drink from flies and cockroaches and the control of these insects. Carriers, who pass cysts and involve in handling food, whether at home, at street stalls, or in catering establishments, should actively detect and treat since they are major transmitters of amoebiasis.
- Health education of the public as well as health personnel at all levels about sanitation and food hygiene-Elementary hygienic practices should propagate and constantly reinforced in schools, health care units, and the home through periodic campaigns using the mass media.
- General social and economic development-The implementation of individual and community preventive measures (e.g., washing of hands, proper excreta disposal) should be an essential part of these activities.
Specific measures that should be undertaken when possible are-
- community surveys to monitor the local epidemiological situation with regard to amoebiasis;
- improvement of case management, i.e., rapid diagnosis and adequate treatment of patients with invasive amoebiasis at all levels of the health services, including the community and health centre levels;
- surveillance and control of situations that may encourage the further spread of amoebiasis, e.g., refugee camps, contaminated public water sources.[7]
Homeopathic Treatment
Homeopathic Treatment of Amebiasis
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines are selected after a full individualizing examination and case-analysis,
which includes
- the medical history of the patient,
- physical and mental constitution,
- family history,
- presenting symptoms,
- underlying pathology,
- possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) is also often taken into account for the treatment of chronic conditions. A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’. The disease diagnosis is important but in homeopathy, the cause of disease is not just probed to the level of bacteria and viruses.
Other factors like mental, emotional and physical stress that could predispose a person to illness are also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition. The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology is not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can be greatly improved with homeopathic medicines.
Homeopathic remedies
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications are also taken into account for selecting a remedy.
Medicines of Amebiasis:
Aloe Socotrina :
frequent stools of bloody water; bloody, jellylike mucus involuntary while passing flatus, Shooting of boring pains in the region of the navel, Increased by pressure; the lower part of the abdomen swollen and sensitive of pressure the digestion and movements in the abdomen are more in the left side and along the track of the colon, Increased after food; Fainting whilst at stool or after[5]
Arsenic Album:
Watery stools at the beginning of the disease very offensive, stools containing more or less pus, sometimes fluid faecal matter, nearly always fluid or coagulated blood; evacuation of dark blood preceded by violent screaming; sensation as of the abdomen would burst before stool; sensation of contraction just above the anus, during stool; tenesmus and burning in rectum, with trembling of limbs, after stool. Great exhaustion after stool; face sunken, pale and features distorted; burning thirst and yet intolerance of water; foetid, greenish urine; sticky perspiration.
Colchicum:
Very painful urging to stool, at first only a little faeces pass, afterwards transparent, gelatinous and very membranous mucous ,with some relief of a pain in abdomen watery, jellylike mucus passes from anus with violent spasms in sphincter; bloody stools, with scrapings from intestines and protrusion of anus; forcing, pressing pain in rectum with frequent scanty discharge; long- lasting agonizing pain in rectum and anus after stool, causing screams and crying; Bloody stool with deathly nausea from smelling cooking; great weakness and exhaustion as after exertion, cannot move head from pillow without help; keeps legs bent on abdomen to avoid move head from pillow without help; keeps legs bent on abdomen to avoid distress when straightening them out; frequent shuddering down the back: cramps in calves of legs; burning or icy coldness of stomach. Autuminal Dysentery.
Colocynth:
Dysenteric diarrhoea, (<) after least food or drink, with compressive, griping pains, commencing at navel and passing down to rectum; stools bloody, full of mucus, passing even half hour, with great straining and burning of anus, temporarily ceasing after stool and by warmth in bed; weakness, paleness and prostration after stool; colicky cutting and squeezing pains (>) by bending forward and accompanied by disposition to stool; burning along urethra during stool; chills proceeding from abdomen[5]
Ferrum phos.:
Aggravation Day and night–Bloody, mucous stools mixed with watery discharges.
Chamomilla:
Swelling of the body, pinching about the navel, passage of offensive flatus without relief.[3]
Nux vom:
Stools, small, slimy, bloody, with urging.. Tenesmus ceasing after stool. Like pitch with blood; pressing in loins and upper part of sacral region, with sensations if broken. Longing for brandy. Milky sours on stomach
Sulphur:
Dysenteric stools at night with colic and violent tenesmus; blood in mucus in thready streaks; frequent unsuccessful desire for stool; with the stool tenesmus ceases, but mucus and blood are still being discharged; prolapses ani at night; cutting pains while urging at stool, (>) by dry heat; chills on lower part of body and lassitude.
Merc :
Excoriating discharges. Cutting in the lower part of the abdomen, at night, the pains increase before the stool and during the stool, with violent tenesmus. The pains rather increase after a stool. Additionally, sometimes they extend to the back, during the stool, hot sweat on the forehead, which soon becomes cold and sticky. Frequent discharge of pure blood or bloody green mucus, like stirred eggs, screams during stool (in children).
Merc core:
Almost constant cutting pains in abdomen and intolerable, almost ineffectual pressing, straining and tenesmus; only frequent scanty discharges of blood slime, day and night; severe pains in rectum continue after stool burning and tenesmus conjointly of rectum and bladder[5]
Diet & Regimen
Diet & Regimen
Regimen ad diet for amebiasis:
Diet for Amebiasis
During the acute phase of amebiasis (when symptoms like diarrhea are present), the focus is on supporting your body and gut while it fights the infection.
What to eat:
- Bland, easily digestible foods: This includes things like white rice, bananas, applesauce, toast, and clear broths. These are gentle on your digestive system.
- Cooked vegetables: Well-cooked carrots, potatoes, and squash are good options.
- Lean protein: Chicken, fish, or tofu (ensure they are well-cooked).
- Hydration: It’s crucial to stay hydrated, especially if you have diarrhea. Drink plenty of water, oral rehydration solutions (like those with electrolytes), and clear broths.
- Bland, easily digestible foods: This includes things like white rice, bananas, applesauce, toast, and clear broths. These are gentle on your digestive system.
What to avoid:
- Dairy products: Milk and cheese can be hard to digest when you have amebiasis.
- Spicy foods: These can irritate your digestive system.
- Fatty foods: Avoid fried foods, greasy meats, and rich sauces.
- Raw fruits and vegetables: These may carry a risk of contamination. Stick to cooked options.
- Alcohol and caffeine: These can dehydrate you and irritate your gut.
- Dairy products: Milk and cheese can be hard to digest when you have amebiasis.
Regimen for Amebiasis
Medical Treatment:
- Consult a doctor: Amebiasis requires medical treatment with antibiotics to kill the parasite. Do not self-treat.
- Complete the full course of medication: Even if you start feeling better, it’s important to finish all your medication as prescribed to ensure the infection is completely cleared.
- Consult a doctor: Amebiasis requires medical treatment with antibiotics to kill the parasite. Do not self-treat.
Hygiene:
- Handwashing: Wash your hands thoroughly with soap and water after using the bathroom, changing diapers, and before eating or preparing food.
- Water safety: Drink bottled or boiled water, especially when traveling to areas where amebiasis is common.
- Food safety: Wash fruits and vegetables thoroughly, and avoid eating raw or undercooked foods.
- Handwashing: Wash your hands thoroughly with soap and water after using the bathroom, changing diapers, and before eating or preparing food.
Important Notes
Do's & Don'ts
Do’s & Don’ts
Amebiasis is a preventable disease. Here are some do’s and don’ts to reduce the risk of infection and complications:
Do’s:
- Practice good hygiene: Wash your hands thoroughly with soap and water after using the toilet, changing diapers, and before handling food.
- Drink safe water: Drink boiled or bottled water, especially when traveling to areas where amebiasis is endemic.
- Cook food thoroughly: Ensure that all food is cooked thoroughly and served hot. Avoid raw or undercooked vegetables and fruits that cannot be peeled.
- Wash fruits and vegetables carefully: Wash fruits and vegetables thoroughly under running water, especially if they are to be eaten raw.
- Seek medical attention if you have symptoms: If you experience symptoms such as diarrhea, abdominal pain, or blood in the stool, consult a doctor promptly for diagnosis and treatment.
- Follow the prescribed treatment regimen: If you are diagnosed with amebiasis, take all medications as prescribed by your doctor to ensure complete eradication of the parasite.
- Educate others about amebiasis: Spread awareness about the disease, its transmission, and preventive measures to your family, friends, and community.
Don’ts:
- Do not drink untreated water: Avoid drinking water from rivers, lakes, or wells that have not been boiled or treated.
- Do not eat raw or undercooked food: Avoid eating raw or undercooked meat, fish, seafood, and vegetables that cannot be peeled.
- Do not share personal items: Avoid sharing towels, utensils, or other personal items with someone who is infected with amebiasis.
- Do not defecate in the open: Use toilets and latrines to prevent contamination of the environment with the parasite.
- Do not ignore symptoms: If you experience any symptoms, do not self-medicate or delay seeking medical advice.
- Do not stop treatment prematurely: Even if you feel better, continue taking medications as prescribed until the full course is completed to ensure complete eradication of the parasite.[17]
By following these do’s and don’ts, you can significantly reduce your risk of contracting amebiasis and prevent its complications.
Terminology
Terminology
- Amebiasis: An infection of the intestines caused by the parasite Entamoeba histolytica.
- Protozoan: A single-celled microscopic organism. Entamoeba histolytica is a type of protozoan.
- Asymptomatic: Showing no symptoms of disease, even though the infection is present.
- Dysentery: A type of gastroenteritis that results in bloody diarrhea.
- Abscess: A swollen area within body tissue, containing an accumulation of pus.
- Trophozoite: The active, feeding stage of the Entamoeba histolytica life cycle.
- Cyst: The dormant, infective stage of Entamoeba histolytica that is passed in feces.
- Luminal Amebiasis: An infection where the parasite remains in the intestine without invading tissues.
- Invasive Amebiasis: An infection where the parasite invades the intestinal wall or other organs.
- Tenesmus: A feeling of constantly needing to pass stools, even if the bowels are empty.
- Hepatomegaly: An enlarged liver.
- Homeopathic Aggravation: A temporary worsening of symptoms after taking a homeopathic remedy, often followed by improvement.
- Miasmatic Tendency: In homeopathy, a predisposition to certain types of diseases based on inherited or acquired factors.
References
References
- Harrison-s_Principles_of_Internal_Medicine-_19th_Edition-_2_Volume_Set
- Medicine Golwala
- A Primer of Materia Medica by T. F. Allen.
- https://hhma.org/healthadvisor/aha-gastameb-crs/#:~:text=You%20may%20eat%20soft%2C%20plain,%2C%20meats%2C%20and%20raw%20vegetables.
- https://medlineplus.gov/ency/article/000298.htm
- https://pubmed.ncbi.nlm.nih.gov/15462926/
- https://www.aimu.us/2016/07/10/amoebiasis-diagnosis-symptoms-complications-and-management/
- https://bestpractice.bmj.com/topics/en-us/553
- https://www.ncbi.nlm.nih.gov/books/NBK557718/
- Prevalence of Amoebiasis and Associated Complications in India: A Systematic Review (2022)
- Molecular Epidemiology of Amoebiasis: A Cross-Sectional Study among North East Indian Population (2015)
- (PDF) Prevalence of Amoebiasis and Associated Complications in India: A Systematic Review (2022)
- Epidemiology of amoebiasis | PPT – SlideShare (Year not specified)
- Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases,9th Edition,John E. Bennett, Raphael Dolin, Martin J. Blaser (2020), Elsevier
- Medical Microbiology, 8th Edition ,Patrick R. Murray, Ken S. Rosenthal, Michael A. Pfaller(2016),Elsevier
- Harrison’s Principles of Internal Medicine,20th Edition,Dennis L. Kasper, Anthony S. Fauci, Stephen L. Hauser, Dan L. Longo, J. Larry Jameson, Joseph Loscalzo (2018),McGraw Hill Professional
- The Manual of Tropical Medicine,5th edition,G. Thomas Strickland, Jay S. Keystone, Thomas B. Nutman, Alan J. Magill, Martin S. Wolfe, Peter Hotez, Sir Brian Greenwood (2021),Elsevier.
Also Search As
Also Search As
People can search for information on Amebiasis using a variety of methods:
Online Search Engines:
- Use search terms like "amebiasis", "amebiasis symptoms", "amebiasis treatment", "amebiasis prevention", or "amebiasis complications".
- Search for specific book titles mentioned in this article, such as "Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases" or "Harrison’s Principles of Internal Medicine".
- Include the names of the authors and publishers to narrow down the search.
Online Medical Resources:
- Visit reputable medical websites like the World Health Organization (WHO), Centers for Disease Control and Prevention (CDC), or MedlinePlus.
- Look for articles, fact sheets, or guidelines on amebiasis.
Libraries:
- Search the library catalog for books on infectious diseases or parasitology.
- Consult with a librarian for assistance in finding relevant resources.
Healthcare Professionals:
- Consult with your doctor or a healthcare professional specializing in infectious diseases for the most accurate and up-to-date information on amebiasis.
Additional Tips:
- Look for articles published in peer-reviewed medical journals for reliable and evidence-based information.
- Be wary of information found on personal blogs or websites that are not affiliated with reputable medical organizations.
- Cross-reference information from different sources to ensure accuracy and completeness.
- Pay attention to the date of publication to ensure the information is current.
By utilizing these resources and strategies, individuals can easily access comprehensive and accurate information on amebiasis, its prevention, symptoms, diagnosis, and treatment options.
There are several ways to search for this article on amebiasis, depending on the specific information you are seeking and the resources available to you:
Keyword Search:
- Use relevant keywords like "amebiasis," "Entamoeba histolytica," "intestinal infection," "parasitic disease," or specific terms mentioned in the article (e.g., "amebic colitis," "liver abscess").
- Combine keywords for more targeted results (e.g., "amebiasis symptoms," "amebiasis treatment").
- Utilize search engines like Google, Bing, or DuckDuckGo to search the web for articles, research papers, and other resources.
Academic Databases:
- If you have access to academic databases like PubMed, Google Scholar, or Web of Science, use them to search for scholarly articles and publications on amebiasis.
- Use advanced search options to filter by publication date, author, or journal.
Medical Websites and Resources:
Library Catalogs:
- If you have access to a library, search the catalog for books or journals related to infectious diseases, parasitology, or tropical medicine.
- Ask a librarian for assistance in finding relevant materials.
Specific Book References:
- If you are looking for information from the books mentioned in this article, you can search for them directly by title, author, or ISBN.
- Check online retailers like Amazon or Barnes & Noble, or visit your local bookstore or library.
Social Media:
- Follow relevant organizations or experts on social media platforms like Twitter or Facebook to stay updated on the latest research and news on amebiasis.
By using a combination of these methods, you can effectively search for and find comprehensive information on amebiasis from various credible sources.
Frequently Asked Questions (FAQ)
What is Amebiasis?
What causes Amebiasis?
- Consuming contaminated food or water
- Association with food handlers whose hands are contaminated
- Contact with contaminated medical devices
- Being pregnant
Can amebiasis be prevented?
Yes, amebiasis can be prevented by:
- Practicing good hygiene (washing hands frequently)
- Drinking safe water (bottled or boiled)
- Eating cooked foods that are hot
- Avoiding raw fruits and vegetables that cannot be peeled
What are the 4 signs of Amebiasis?
- Loose stools
- Mild abdominal cramping,
- Frequent, watery, and/or bloody stools with severe abdominal cramping
- Flatulence
- Appetite loss
- Fatigue
Are there any complications of amebiasis?
Can homeopathy treat amebiasis effectively?
How does a homeopath choose the right remedy for Amebiasis?
Homeopathic treatment is highly individualized. A homeopath will conduct a detailed case taking, considering the patient’s unique symptoms, medical history, and overall constitution to select the most appropriate remedy.