Amphetamine Use Disorder
Definition
Amphetamine use disorder is a chronic, relapsing brain disease characterized by compulsive amphetamine seeking and use, despite the harmful consequences. It is a type of stimulant use disorder that can lead to significant impairment in daily life, including problems with work, school, relationships, and physical and mental health.
Although amphetamine was first synthesized by Edeleanu in 1887, its journey in medicine began in 1932 with the introduction of the Benzedrine inhaler. This inhaler, containing amphetamine, was initially used to treat nasal congestion (coryza and rhinitis) and asthma.
However, its therapeutic applications quickly expanded, and amphetamine was soon recommended for a wide range of conditions. These included narcolepsy (to combat excessive sleepiness), post-encephalitic parkinsonism (to manage motor symptoms), obesity (as an appetite suppressant), and depression (to elevate mood). It was even used to boost energy and enhance work capacity in individuals struggling with fatigue.
Here are some synonyms for Amphetamine Use Disorder:
- Stimulant Use Disorder
- Methamphetamine Use Disorder (often refers to a specific type of amphetamine)
- Speed Addiction
- Upper Addiction
- Crystal Meth Addiction (referring to the crystallized form of methamphetamine)
- Benzedrine Addiction (referring to a brand name of amphetamine)
Please note: These terms are all similar but may have slightly different meanings. It is important to use the most accurate term for the specific situation.
Frequently Asked Questions (FAQ)
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do's & Don'ts
Terminology
References
Also Search As
Overview
Overview
- Amphetamine refers to a unique chemical which is basically phenyl-isopropylamine or methylphenethylamine. It is a powerful CNS stimulant, with peripheral sympathomimetic effects too. The dextro-amphetamine isomer is nearly 3-4 times more potent than the levo-isomer.
- It acts primarily on norepinephrine release in brain, along with an action on the release of dopamine and serotonin.
Although still clinically indicated for narcolepsy and attention deficit hyperactivity disorder (and very rarely for obesity and mild depression), one of the commonest patterns of ‘use’ seen amongst the students and sports-persons to overcome the need for sleep and fatigue. - Tolerance usually develops to the central as well as cardiovascular effects of amphetamines.
- Recently, there has been a resurgence of amphetamine use in USA and Europe, with the availability of ‘designer’ amphetamines, such as MDMA (3,4-methylenedioxyamphetamine; street name: ecstasy or XTC).
Epidemiology
Epidemiology of Amphetamine Use Disorder (AUD):
Amphetamine Type Stimulants (ATS) are used by a small proportion of India’s population. The National Survey on Extent and Pattern of Substance Use in India (2019) found that the prevalence of current ATS use was 0.18% among adults (aged 18-75 years), which translates to an estimated 2 million users. [3]
References:
Ministry of Social Justice and Empowerment, Government of India. (2019). Magnitude of Substance Use in India. https://socialjustice.gov.in/ writereaddata/UploadFile/ Survey%20Report.pdf
Additional resources:
- National Drug Dependence Treatment Centre (NDDTC), AIIMS. (2019). Magnitude of Substance Abuse in India 2019. https://www.lgbrimh.gov.in/ resources/Addiction_Medicine/ elibrary/ magnitude_substance_abuse_india.pdf
It is important to note that this data represents the prevalence of current ATS use and not specifically Amphetamine Use Disorder (AUD). The prevalence of AUD in India is likely lower than the prevalence of ATS use, as not all individuals who use ATS will develop AUD. Further research is needed to determine the specific prevalence of AUD in India.[2][3]
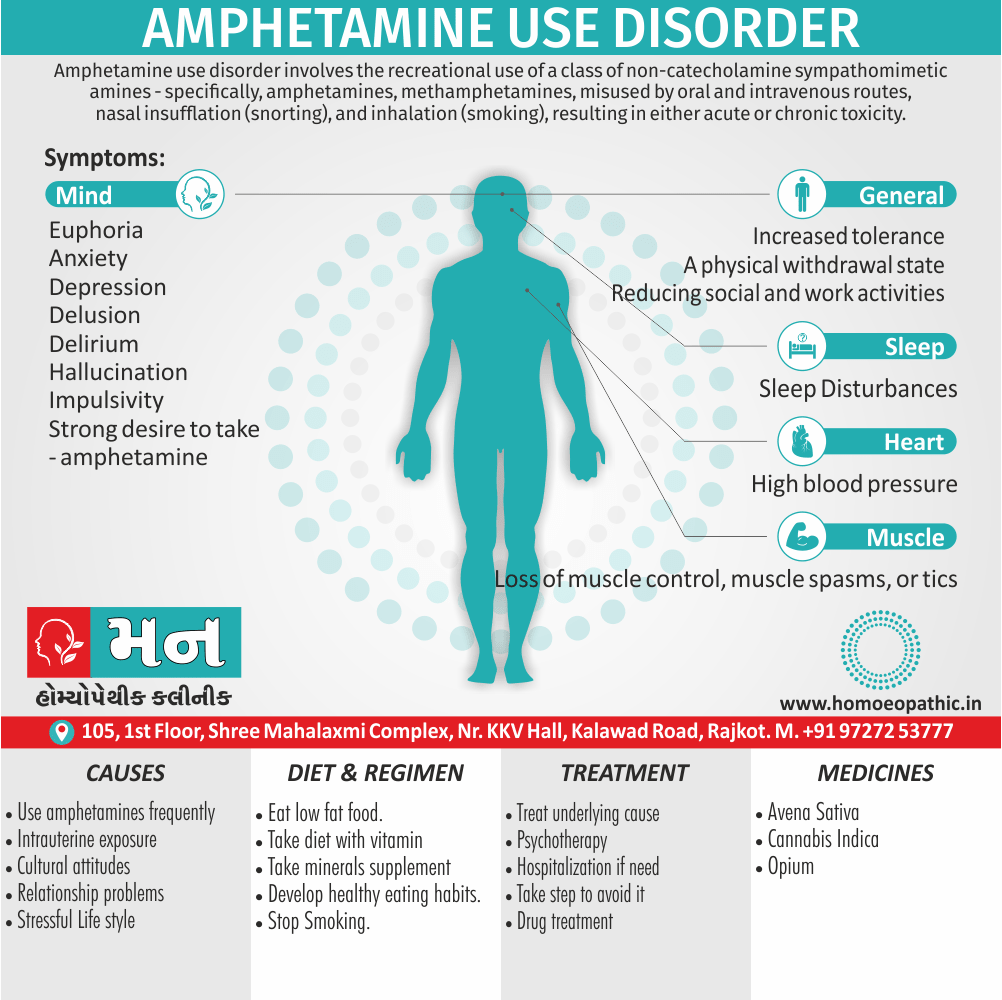
Causes
Causes of Amphetamine Use Disorder (AUD):
Kaplan & Sadock’s Comprehensive Textbook of Psychiatry, 11th Edition (2022) by Benjamin J. Sadock, Virginia A. Sadock, and Pedro Ruiz, details several risk factors and potential causes for Amphetamine Use Disorder (AUD):
Biological Factors:
Genetic predisposition plays a role, with individuals having a family history of substance use disorders being more susceptible. Neurochemical imbalances, particularly involving dopamine and norepinephrine, contribute to the rewarding effects of amphetamines and the development of dependence.
Psychological Factors:
Preexisting mental health conditions like depression, anxiety, ADHD, or personality disorders increase the risk. Individuals may use amphetamines to self-medicate or cope with emotional distress. Impulsivity and sensation-seeking traits also increase vulnerability.
Social and Environmental Factors:
Peer pressure, exposure to drug use in social circles, and easy access to amphetamines can trigger experimentation and escalate into regular use. Stressful life events, trauma, or lack of social support can increase vulnerability. [4]
It’s crucial to note that AUD is a complex disorder with multiple interacting factors. A combination of biological, psychological, and social influences contributes to its development. The specific contribution of each factor may vary from person to person.
Types
Classification of Amphetamine Use Disorder:
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) by the American Psychiatric Association (2013) classifies Amphetamine Use Disorder (AUD) under the category of "Stimulant Use Disorder." This category encompasses disorders related to the use of amphetamines and other stimulant drugs like cocaine.
Furthermore, the DSM-5 specifies that AUD can be classified as:
- Mild: The presence of 2-3 symptoms from a list of criteria related to impaired control, social impairment, risky use, and pharmacological indicators.
- Moderate: The presence of 4-5 symptoms.
- Severe: The presence of 6 or more symptoms.
This classification system helps mental health professionals assess the severity of the disorder and develop appropriate treatment plans.
Risk Factors
Risk Factors of Amphetamine Use Disorder (AUD):
- Genetic Predisposition: Family history of substance use disorders, particularly involving stimulants, increases the risk of AUD.
- Co-occurring Mental Health Disorders: Individuals with pre-existing conditions like depression, anxiety, ADHD, bipolar disorder, or personality disorders are more vulnerable to developing AUD.
- Impulsivity and Sensation-Seeking: Personality traits characterized by impulsivity, risk-taking behavior, and a need for novel experiences increase the likelihood of experimenting with and abusing amphetamines.
- Environmental Factors: Exposure to drug use within social circles, peer pressure, and easy access to amphetamines contribute to the risk.
- Stressful Life Events: Trauma, major life changes, or chronic stress can trigger or exacerbate substance use as a coping mechanism.
- Early Initiation of Drug Use: Starting amphetamine use at a younger age significantly increases the risk of developing AUD later in life. [4]
Pathogenesis
Pathogenesis of Amphetamine Use Disorder (AUD)
The exact pathogenesis of Amphetamine Use Disorder (AUD) is complex and multifactorial, involving a combination of genetic, neurobiological, and environmental factors.
Koob, G. F., & Volkow, N. D. (2016). Neurobiology of addiction: A neurocircuitry analysis. The Lancet Psychiatry, 3(8), 760-773.
- This reference explains that the primary neurobiological mechanism underlying AUD is the dysregulation of the brain’s reward system, particularly the mesolimbic dopamine pathway.
- Amphetamines increase the release of dopamine in the nucleus accumbens, a key brain region involved in reward processing. Repeated exposure to amphetamines can lead to long-term changes in the brain’s structure and function, including alterations in dopamine receptors and transporters.
- These changes contribute to the development of tolerance, dependence, and withdrawal symptoms associated with AUD. [5]
Stahl’s Essential Psychopharmacology, 5th Edition (2017) by Stephen M. Stahl
- This book further elaborates on the neurobiological mechanisms, emphasizing the role of glutamate and other neurotransmitters in the development of AUD.
- It highlights the concept of "hypofrontality," a decrease in activity in the prefrontal cortex, which is involved in decision-making and impulse control.
- This hypofrontality can contribute to the compulsive drug-seeking behavior seen in individuals with AUD. [6]
It’s important to note that the pathogenesis of AUD is still an area of active research, and new insights are emerging constantly.
Pathophysiology
The pathophysiology of Amphetamine Use Disorder (AUD):
Neurotransmitter Dysregulation:
- Amphetamines primarily affect the dopamine system by increasing the release and blocking the reuptake of dopamine in the brain’s reward pathway.
- This leads to excessive dopamine signaling, which reinforces drug-seeking behavior and contributes to the development of addiction.
- Other neurotransmitters like norepinephrine and serotonin are also implicated, playing a role in the stimulant effects and mood-related aspects of AUD.
Structural and Functional Brain Changes:
- Chronic amphetamine use can induce long-term changes in the brain’s structure and function.
- These changes include reduced gray matter volume in regions involved in decision-making and impulse control, as well as alterations in receptor sensitivity and neurotransmitter signaling pathways.
- These changes can perpetuate cravings and make it difficult for individuals to control their drug use.
Neuroadaptations and Tolerance:
With repeated use, the brain adapts to the presence of amphetamines by reducing dopamine receptor sensitivity and downregulating other neurotransmitter systems.
This leads to tolerance, where higher doses are needed to achieve the same desired effects, further driving the cycle of addiction.
Withdrawal and Dependence:
When amphetamine use is abruptly stopped, the brain’s altered neurochemistry can result in withdrawal symptoms such as fatigue, depression, anxiety, and intense cravings.
These withdrawal symptoms can be severe and contribute to relapse.
Genetic and Environmental Factors:
While the neurobiological mechanisms are central to AUD, genetic and environmental factors also play a role.
Genetic predisposition can influence an individual’s susceptibility to addiction, while environmental factors like stress, trauma, and social influence can trigger or exacerbate drug use. [6]
Clinical Features
Clinical Features of Amphetamine Use Disorder (AUD):
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) by the American Psychiatric Association (2013) outlines the clinical features of Amphetamine Use Disorder (AUD):
Impaired Control:
- Taking larger amounts or over a longer period than intended.
- Persistent desire or unsuccessfulefforts to cut down or control use.
- Spending a great deal of time obtaining, using, or recovering from the effects of amphetamines.
- Craving or strong desire to use amphetamines.
Social Impairment:
- Failure to fulfill major role obligations at work, school, or home.
- Continued use despite persistent or recurrent social or interpersonal problems caused or exacerbated by amphetamine use.
- Giving up important social, occupational, or recreational activities because of amphetamine use.
Risky Use:
- Recurrent use in situations where it is physically hazardous.
- Continued use despite knowledge of having a persistent or recurrent physical or psychological problem likely caused or exacerbated by amphetamine use.
Pharmacological Indicators:
- Tolerance: Needing increased amounts to achieve intoxication or desired effect.
- Withdrawal: Characteristic withdrawal syndrome for amphetamines or using amphetamines to relieve or avoid withdrawal symptoms. [7]
Sign & Symptoms
Sign & Symptoms
- The withdrawal syndrome is typically seen on an abrupt discontinuation of amphetamines after a period of chronic use. Moreover, The syndrome is characterized by depression (especially it may present with suicidal ideation), marked asthenia, apathy, fatigue, hypersomnia alternating with insomnia, agitation also hyperphagia.
Clinical Examination
Clinical Examination
While the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition) by the American Psychiatric Association (2013) primarily focuses on diagnostic criteria for AUD, it doesn’t explicitly outline a clinical examination procedure. However, the following book can offer guidance on assessment:
1. Thorough History Taking:
Eliciting information about the pattern and duration of amphetamine use, route of administration, quantity used, history of prior treatment attempts, co-occurring medical and psychiatric conditions, and social and environmental factors contributing to drug use.
2. Physical Examination:
Assessing for signs of amphetamine intoxication (e.g., dilated pupils, tachycardia, elevated blood pressure) or withdrawal (e.g., fatigue, depression, agitation).
3. Mental Status Examination:
Evaluating for cognitive impairments, mood disturbances, and psychotic symptoms that may be associated with AUD.
4. Laboratory Tests:
Screening for amphetamines in urine or blood, as well as other relevant tests to assess for medical complications related to amphetamine use.
5. Psychosocial Assessment:
Exploring the patient’s social support network, living situation, occupational functioning, and legal issues related to drug use.
6. Screening Tools and Questionnaires:
Utilizing validated instruments like the Addiction Severity Index (ASI) or the Drug Abuse Screening Test (DAST) to assess the severity of the disorder and identify areas needing intervention. [8]
Diagnosis
Diagnosis
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) by the American Psychiatric Association (2013) provides the criteria for diagnosing Amphetamine Use Disorder (AUD):
A problematic pattern of amphetamine use leading to clinically significant impairment or distress, as manifested by at least two of the following, occurring within a 12-month period:
Clinical Significant
- Amphetamine is often taken in larger amounts or over a longer period than was intended.
- There is a persistent desire or unsuccessful efforts to cut down or control amphetamine use.
- A great deal of time is spent in activities necessary to obtain amphetamine, use amphetamine, or recover from its effects.
- Craving, or a strong desire or urge to use amphetamine.
- Recurrent amphetamine use resulting in a failure to fulfill major role obligations at work, school, or home.
- Continued amphetamine use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of amphetamine.
- Important social, occupational, or recreational activities are given up or reduced because of amphetamine use.
- Recurrent amphetamine use in situations in which it is physically hazardous.
- Amphetamine use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by amphetamine.
- Tolerance, as defined by either of the following: a. A need for markedly increased amounts of amphetamine to achieve intoxication or desired effect. b. A markedly diminished effect with continued use of the same amount of amphetamine.
- Withdrawal, as manifested by either of the following: a. The characteristic withdrawal syndrome for amphetamine. b. Amphetamine (or a closely related substance) is taken to relieve or avoid withdrawal symptoms.
Specify current severity:
- Mild: Presence of 2-3 symptoms.
- Moderate: Presence of 4-5 symptoms.
- Severe: Presence of 6 or more symptoms.
Differential Diagnosis
Differential Diagnosis of AUD:
Other Substance Use Disorders:
It’s crucial to determine if the patient is using other substances concurrently or has a history of other substance use disorders. Cocaine, methamphetamine, and other stimulant use disorders can share similar clinical features with AUD.
Primary Psychiatric Disorders:
Several psychiatric conditions can mimic or co-occur with AUD. These include:
- Bi-polar Disorder: Manical episodes can present with increased energy, decreased need for sleep, and impulsivity, which can be mistaken for amphetamine intoxication.
- Attention-Deficit/Hyperactivity Disorder (ADHD): Restlessness, inattention, and impulsivity are common in both ADHD and AUD.
- Anxiety Disorders: Agitation, insomnia, and restlessness can be symptoms of both anxiety disorders and amphetamine use.
- Schizophrenia and Other Psychotic Disorders: Amphetamine use can induce or exacerbate psychotic symptoms like hallucinations and delusions.
Medical Conditions:
Certain medical conditions can cause symptoms that overlap with AUD. These include:
- Hyperthyroidism: Can present with weight loss, tremors, and increased heart rate, similar to amphetamine intoxication.
- Neurological Disorders: Some neurological conditions can cause agitation, restlessness, and mood changes. [4]
Complications
Acute intoxication and Complications:
The signs and symptoms of acute amphetamine intoxication are primarily;
Cardiovascular: e.g. Tachycardia, Hypertension, Haemorrhage, Cardiac failure and Cardiovascular shock)
Central: Seizures, Hyperpyrexia, Tremors, Ataxia, Euphoria, Pupillary dilatation, Tetany and Coma).
Additionally, the neuro psychiatric manifestations include anxiety, panic, insomnia, restlessness, irritability, hostility and bruxism.
Acute intoxication may present as a suspicious hallucinatory syndrome which closely mimics schizophrenia. The distinguishing features include rapidity of onset, prominence of visual hallucinations, absence of thought disorder, appropriateness of affect, fearful emotional reaction, also presence of confusion.
However, a confident diagnosis requires an estimation of the recent urinary amphetamine levels. Amphetamine-induced psychosis usually resolves within seven days of urinary clearance of amphetamines.
Generally, Chronic amphetamine intoxication leads to severe and compulsive craving for the drug. A high degree of tolerance is characteristic, with the dependent individual needing up to 15-20 times the initial dose, in order to obtain the pleasurable effects.
A common pattern of chronic use is a cycle of runs (in other words, heavy use for several days) followed by crashes (stopping the drug use). Besides this, Tactile hallucinations, in clear consciousness, may sometimes occur in chronic amphetamine intoxication.
Investigations
Investigations for individuals suspected of having Amphetamine Use Disorder (AUD):
Urine Drug Screening: This is the most common and readily available test for detecting amphetamines in the system. Amphetamines can be detected in urine for up to 48-72 hours after use.
Blood Test: While less common than urine tests, blood tests can provide a more accurate measure of recent amphetamine use. They can also be used to detect other substances that may be used concurrently with amphetamines.
Hair Follicle Test: This test can detect amphetamine use for a longer duration, up to 90 days, but is less commonly used due to its higher cost and longer turnaround time.
Psychological Evaluation: A comprehensive psychological evaluation can help assess the severity of AUD, identify co-occurring mental health disorders, and guide treatment planning.
Medical Evaluation: This may include a physical examination, laboratory tests (such as liver and kidney function tests), and electrocardiogram (ECG) to assess for any medical complications related to amphetamine use.[9]
Treatment
Treatment of Intoxication:
Acute intoxication is treated by symptomatic measures i.e.;
- Hyperpyrexia (cold sponging, parenteral antipyretics),
- Seizures (e.g. parenteral diazepam),
- Psychotic symptoms (e.g. anti psychotics),
- Hypertension (e.g. anti hypertensives).
Acidification of urine (with oral NH4Cl; 500 mg every 4 hours) facilitates the elimination of amphetamines.
Treatment of Withdrawal Symptoms:
The presence of severe suicidal depression may necessitate hospitalization. The treatment includes symptomatic management, use of antidepressants also supportive psychotherapy. Furthermore, the management of withdrawal syndrome is usually the first step towards successful management of amphetamine dependence.
Prevention
Prevention of Amphetamine Use Disorder:
Universal Prevention:
These strategies target the general population, aiming to reduce the overall risk factors and increase protective factors for substance use. They include:
- School-based programs: Providing education about the risks of drug use, developing social and emotional skills, and promoting healthy alternatives to drug use.
- Public awareness campaigns: Raising awareness about the dangers of amphetamines and promoting healthy lifestyles.
- Policy interventions: Implementing stricter regulations on the availability and marketing of amphetamines.
Selective Prevention:
These strategies focus on individuals or groups at higher risk of developing AUD, such as those with a family history of substance abuse or those experiencing significant life stressors. Interventions may include:
- Family-based programs: Enhancing family communication and problem-solving skills, and providing support for parents.
- Targeted interventions for high-risk youth: Providing education and support to young people who are experimenting with drugs or engaging in risky behaviors.
Indicated Prevention:
These strategies aim to prevent the progression of AUD in individuals who are already showing early signs of problematic amphetamine use. Interventions may include:
- Brief interventions: Providing feedback and advice about reducing or stopping amphetamine use.
- Motivational enhancement therapy: Helping individuals develop the motivation and skills to change their behavior.
- Referral to specialized treatment: Connecting individuals with appropriate treatment resources if needed.
By implementing a comprehensive prevention strategy that combines universal, selective, and indicated approaches, it is possible to reduce the incidence and prevalence of AUD in the population. [8]
Homeopathic Treatment
Homeopathic Treatment of Amphetamine Use Disorder (AUD):
- Homeopathy treats the person as a whole.
- It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition.
- The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’? The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition. The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Amphetamine Use Disorder (AUD) :
The homeopathic remedies (medicines) given below indicate the therapeutic affinity, but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor. So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines for Amphetamine Use Disorder (AUD):
- Nux vomica: Often considered for individuals with irritability, anxiety, and sleep disturbances associated with stimulant use.
- Avena sativa: May be used to address exhaustion, anxiety, and insomnia related to withdrawal.
- Coffea cruda: Might be considered for individuals experiencing heightened sensitivity, restlessness, and sleep difficulties due to stimulant use.
Hyoscyamus niger: For individuals experiencing delirium, hallucinations, or manical behavior associated with amphetamine intoxication.
Stramonium: May be considered for extreme agitation, confusion, and fearfulness related to amphetamine use.
Cannabis indica: This remedy might be used to address withdrawal symptoms like apathy, depression, and sleep disturbances.
Zincum metallicum: May be considered for individuals experiencing restlessness, fidgeting, and nervous exhaustion due to stimulant use.
Diet & Regimen
Diet & Regimen for Amphetamine Use Disorder (AUD):
While there is no specific diet or regimen solely for Amphetamine Use Disorder (AUD) outlined in major medical textbooks, a balanced and nutritious diet can play a supportive role in recovery.
Substance Abuse:
- Replenish Nutrient Deficiencies: Chronic amphetamine use often leads to poor dietary habits and nutrient deficiencies. A balanced diet rich in fruits, vegetables, whole grains, and lean protein can help restore essential vitamins and minerals.
- Support Brain Health: Certain nutrients like omega-3 fatty acids, B vitamins, and antioxidants are crucial for brain function and can aid in recovery from the neurotoxic effects of amphetamines.
- Stabilize Blood Sugar: Fluctuations in blood sugar levels can trigger cravings and mood swings. Regular meals and snacks that include complex carbohydrates and protein can help maintain stable blood sugar levels.
- Improve Overall Health: A healthy diet can boost energy levels, improve sleep quality, and support the immune system, all of which are important for recovery from AUD.
- Limit Caffeine and Sugar: These substances can exacerbate anxiety, insomnia, and other withdrawal symptoms.
- Stay Hydrated: Adequate water intake is essential for detoxification and overall health.
- Avoid Processed Foods: Processed foods are often high in sugar, unhealthy fats, and artificial ingredients, which can hinder recovery.
Regimen:
In addition to a healthy diet, a regular regimen that includes exercise, stress management techniques (such as yoga or meditation), and adequate sleep can also be beneficial in supporting recovery from AUD. [8]
Do's & Don'ts
The Do’s & Don’ts:
Do’s:
- Seek professional help: AUD is a complex condition best managed with professional guidance. Reach out to a doctor, therapist, or addiction specialist for assessment and treatment.
- Build a strong support system: Surround yourself with supportive friends and family who understand your struggles and encourage your recovery.
- Attend therapy: Individual and group therapy can provide valuable tools for managing cravings, developing coping skills, and addressing underlying issues contributing to substance use.
- Engage in healthy activities: Exercise, hobbies, and spending time in nature can boost mood, reduce stress, and provide healthy alternatives to drug use.
- Be patient and persistent: Recovery is a journey, not a destination. It takes time and effort, but with persistence and support, lasting recovery is possible.
Don’ts:
- Don’t try to quit alone: Withdrawal symptoms can be challenging, and professional support can make a significant difference.
- Don’t isolate yourself: Social connection is crucial for recovery. Avoid withdrawing from loved ones and supportive communities.
- Don’t give up on treatment: If one treatment approach doesn’t work, try another. There are various effective treatments for AUD, and finding the right fit is essential.
- Don’t be afraid to ask for help: Reaching out for support is a sign of strength, not weakness.
- Don’t give up on yourself: Recovery is a process filled with ups and downs. Remember that setbacks are normal and don’t define your journey.
Additional Considerations:
- Avoid triggers: Identify and avoid people, places, or situations that trigger cravings.
- Manage stress: Develop healthy coping mechanisms for stress, such as relaxation techniques or mindfulness.
- Prioritize self-care: Get enough sleep, eat a nutritious diet, and engage in activities that bring joy and fulfillment.
Terminology
Terminologies used in the article Amphetamine Use Disorder (AUD):
General Terminology
- Amphetamine: A central nervous system (CNS) stimulant drug that increases alertness, energy, and focus.
- CNS Stimulant: A drug that speeds up the activity of the brain and nervous system.
- Sympathomimetic: A substance that mimics the effects of the sympathetic nervous system, responsible for the "fight or flight" response.
- Tolerance: The need for increasing amounts of a substance to achieve the desired effect, or a diminished effect with continued use of the same amount.
- Withdrawal: The unpleasant physical and psychological symptoms experienced when a person stops using a substance they have become dependent on.
- Hypersomnia: Excessive daytime sleepiness.
- Hyperphagia: Increased appetite or excessive eating.
- Intoxication: The state of being affected by a drug, often leading to impaired judgment, behavior, and coordination.
- Psychotic Symptoms: Hallucinations (false perceptions) and delusions (false beliefs) are examples of psychotic symptoms.
Medical Terminology
- Coryza: Inflammation of the mucous membrane in the nose, causing symptoms like a runny nose and congestion (common cold).
- Rhinitis: Inflammation of the nasal mucosa, leading to sneezing, congestion, and a runny nose (allergies or infections).
- Narcolepsy: A sleep disorder characterized by excessive daytime sleepiness and sudden sleep attacks.
- Postencephalitic Parkinsonism: Parkinsonism (tremor, rigidity, slowness of movement) that occurs as a result of brain inflammation (encephalitis).
- Tachycardia: Abnormally rapid heart rate.
- Hypertension: High blood pressure.
- Hyperpyrexia: Extremely high fever.
- Ataxia: Lack of muscle coordination.
- Pupillary Dilatation: Enlargement of the pupil (the black center of the eye).
- Tetany: Involuntary muscle contractions caused by low calcium levels or other factors.
- Bruxism: Teeth grinding or clenching.
Homeopathic Terminology
- Individualized Treatment: Tailoring treatment to the specific needs and symptoms of each individual.
- Miasmatic Tendency: A predisposition to certain disease patterns or groups of symptoms, considered in homeopathic treatment selection.
- Psychosomatic: Physical symptoms caused or aggravated by mental factors.
References
References
- A Short Textbook of Psychiatry by Niraj Ahuja / Ch 4.
- Ministry of Social Justice and Empowerment, Government of India. (2019). Magnitude of Substance Use in India. https://socialjustice.gov.in/ writereaddata/UploadFile/ Survey%20Report.pdf
- National Drug Dependence Treatment Centre (NDDTC), AIIMS. (2019). Magnitude of Substance Abuse in India 2019. https://www.lgbrimh.gov.in/ resources/Addiction_Medicine/ elibrary/magnitude_substance_abuse_india.pdf
- Kaplan & Sadock’s Comprehensive Textbook of Psychiatry, 11th Edition (2022) by Benjamin J. Sadock, Virginia A. Sadock, and Pedro Ruiz
Koob, G. F., & Volkow, N. D. (2016). Neurobiology of addiction: A neurocircuitry analysis. The Lancet Psychiatry, 3(8), 760-773.
Stahl’s Essential Psychopharmacology, 5th Edition (2017) by Stephen M. Stahl
The clinical features of Amphetamine Use Disorder (AUD) are detailed in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), published by the American Psychiatric Association in 2013.
A Comprehensive Textbook, 5th Edition (2019) by David A. Fiellin, Robert P. Schwartz, and Richard A. Rawson
Also Search As
Also Search As:
This article can also be searched as:
- Amphetamine addiction
- Stimulant addiction
- Methamphetamine addiction
- Speed addiction
- Crystal meth addiction
- Benzedrine addiction
- Substance use disorder involving amphetamines
- Stimulant use disorder
- Drug addiction
- Substance abuse
- Addictive disorders
- Mental health and addiction
- Effects of amphetamines
- Symptoms of amphetamine withdrawal
- Treatment for amphetamine addiction
- Prevention of amphetamine abuse
What is Amphetamine Use Disorder?
Definition
In Amphetamine Use Disorder, it was introduced as benzedrine inhaler, for the treatment of coryza, rhinitis and asthma. Later, it recommended for a variety of conditions such as narcolepsy, postencephalitic parkinsonism, obesity, depression, and even to heighten energy and capacity to work
What is the treatment of acute intoxication of Amphetamine Use Disorder?
Treatment:
Hyperpyrexia (cold sponging, parenteral antipyretics),
Seizures (parenteral diazepam),
Psychotic symptoms (anti psychotics),
Hypertension (anti hypertensives)
Give the complications of Amphetamine Use Disorder?
What are the withdrawal symptoms of Amphetamine Use Disorder?
Withdrawal Symptoms:
Depression (may present with suicidal ideation)
Marked asthenia
Apathy
Fatigue
Hypersomnia alternating with insomnia
Agitation
Hyperphagia.
What are the signs and symptoms of AUD?
Common signs & symptoms
Physical: Increased heart rate, dilated pupils, weight loss, sleep disturbances.
Psychological: Anxiety, agitation, irritability, paranoia, depression, hallucinations.
Behavioral: Neglecting responsibilities, financial difficulties, social isolation, risky behavior.
How is AUD diagnosed?
Diagnosis is based on a thorough evaluation by a healthcare professional. It includes:
Clinical interview: Assessing symptoms, drug use history, and social impact.
Physical examination: Checking for physical signs of drug use and related complications.
Laboratory tests: Urine or blood tests to confirm amphetamine presence.
Psychological assessment: To rule out other mental health disorders.
Can homeopathy help with Amphetamine Use Disorder (AUD)?
While conventional medicine focuses on managing symptoms and withdrawal, homeopathy aims to address the underlying causes of AUD, considering the individual’s unique physical and emotional state.
Can homeopathy replace conventional treatment for AUD?
Yes,
Homeopathy can be a complementary approach to conventional treatment for AUD. It’s essential to work with a healthcare team that includes both conventional and homeopathic practitioners to develop a comprehensive treatment plan.
Is homeopathic treatment for AUD safe?
Yes,
Homeopathic remedies are generally safe when prescribed by a qualified practitioner. However, it’s important to consult with a healthcare professional to discuss the best approach for your individual needs and to ensure there are no contraindications with other medications you may be taking.
Which homeopathic remedies are commonly used for AUD?
Homoeopathic medicines for Amphetamine use disorder
Nux vomica: For irritability, anxiety, and sleep disturbances.
Avena sativa: For exhaustion, anxiety, and insomnia during withdrawal.
Coffea cruda: For heightened sensitivity, restlessness, and sleep difficulties.
Hyoscyamus niger: For delirium, hallucinations, or manical behavior.
Stramonium: For extreme agitation, confusion, and fearfulness.
