Ankylosing Spondylitis
Definition
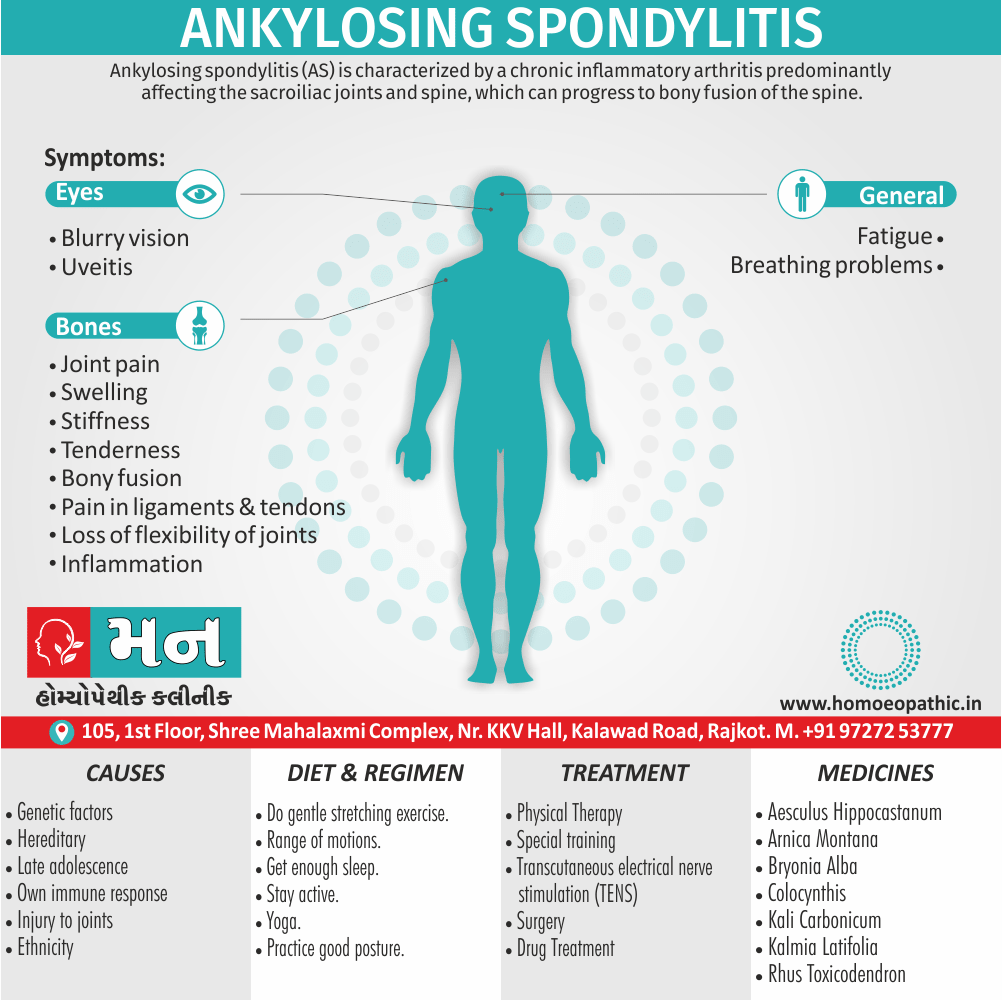
Ankylosing spondylitis (AS) is characterised by a chronic inflammatory arthritis predominantly affecting the sacroiliac joints and spine, which can progress to bony fusion of the spine. [1]
Ankylosing spondylitis has a few synonyms, some of which are more common than others:
- Marie-Strümpell disease: This term is named after the two doctors who first described the condition in the late 19th century, Pierre Marie and Adolph Strümpell.
- Bechterew disease: This term is named after Vladimir Bekhterev, a Russian neurologist who also played a role in identifying the disease.
- Axial spondylitis: This is a broader term that encompasses ankylosing spondylitis as well as other conditions that cause inflammation of the spine.
It’s important to note that "ankylosing spondylitis" is the most widely used and recognized term for this condition
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis.
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do's & Don'ts
Terminology
References
Also Search As
Overview
Overview of Ankylosing spondylitis:
- The Ankylosing Spondylitis onset is typically between the ages of 20 and 30, with a male preponderance of about 3 : 1.
- In Europe, more than 90% of those affected are HLA B27 positive.
- The overall prevalence is less than 0.5% in most populations.
- Over 75% of patients are able to remain in employment and enjoy a good quality of life.
- Even if severe ankylosis develops, functional limitation may not be marked as long as the spine is fused in an erect posture. [1]
- This fusing makes the spine less flexible and can result in a hunched-forward posture.
- If ribs are affected, it can be difficult to breathe deeply. [2]
Epidemiology
Epidemiology of Ankylosing spondylitis:
- Ankylosing spondylitis (AS) is a chronic inflammatory disease primarily affecting the spine. In India, the prevalence of AS has been reported to range between 0.1% and 0.2% in a rural population, as per a study by Malaviya et al. (Indian Rheumatology Association consensus statement on the diagnosis and treatment of axial spondyloarthropathies, 2009). [13]
- However, more recent reports suggest an alarming rise in AS among young Indian adults in their late twenties and early thirties (Alarming rise in Ankylosing Spondylitis amongst young Indian workforce, 2017). [14]
- An estimated 30-40 lakh people in India suffer from AS, with the working population being most commonly affected (Alarming rise in Ankylosing Spondylitis amongst young Indian workforce, 2017). [14]
- A study focusing on the clinical characteristics of AS patients in India found that the trans woman ratio is 5:1, with a mean age of onset of symptoms at 23.6 years and diagnosis at 32.5 years (Clinical characteristics of patients with ankylosing spondylitis in India, 2009). [15]
It is important to note that the epidemiology of AS can vary depending on factors such as geographic location, ethnicity, and socioeconomic status. Therefore, further research is needed to fully understand the prevalence and burden of AS in India.
Causes
Causes of Ankylosing spondylitis
Several things make AS more likely:
Age:
- It tends to start between your teens and 30s.
Gender:
- Men are two to three times more likely to get the disease than women.
Genetics:
- You can inherit it from your parents.
- One gene, called HLA-B27, is common in people with AS.
Ethnicity:
- AS appears more often among native groups in the U.S. and Canada. [4]
Types
Types of Ankylosing spondylitis
- Nonradiographic axial spondyloarthritis (nr-axSpA). This is the less severe form of spondyloarthritis. “Nonradiographic” means that something is not easily visible on an X-ray. .
- Radiographic axial spondyloarthritis. This is the first phase of ankylosing spondylitis. It happens when nr-axSpA gradually gets worse and affects the sacroiliac joints and the bones of the spine.[7]
Risk Factors
Risk Factors
Family history and HLA-B27 gene
Age.
About 80 percent Trusted Source of people first develop ankylosing spondylitis symptoms under age 30.
Sex.
Ankylosing spondylitis tends to develop about twice as often in men than in women.
Ethnicity.
The prevalence of the HLA-B27 gene seems to vary between ethnic groups. According to one studyTrusted Source, its incidence rate was 7.5 percent in non-Hispanic whites, 4.6 percent among Mexican-Americans, and 1.1 percent among non-Hispanic blacks.
Gut inflammation.
Up to 70 percent Trusted Source of people with ankylosing spondylitis have gut inflammation, suggesting a potential origin in the gut. It’s thought disruption to the microbiome in your gut may play a role in its development.
Smoking.
Some research Trusted Source has found an association between the development of ankylosing spondylitis and smoking, but the association still is not clear.
Childhood infections.
A 2016 study Trusted Source found an association between childhood respiratory infections and the later development of ankylosing spondylitis. Childhood appendicitis was linked to a decreased risk.[10]
Pathogenesis
Pathogenesis:
The pathogenesis of Ankylosing Spondylitis (AS) is a complex interplay of genetic and environmental factors. While the exact mechanisms are not fully understood, several key elements have been identified:
Genetic Predisposition:
- HLA-B27: The strongest genetic association with AS is the presence of the HLA-B27 gene. This gene is present in over 90% of AS patients but only 5-8% of the general population. However, having the HLA-B27 gene does not guarantee the development of AS.
- Other Genes: Genome-wide association studies have identified other genes associated with AS, including IL23R, ERAP1, and RUNX3. These genes are involved in immune regulation and inflammatory responses.
Environmental Factors:
- Gut Microbiome: Alterations in the gut microbiome have been linked to AS. Dysbiosis, an imbalance of gut bacteria, may trigger an inflammatory response that contributes to the development of AS.
- Infections: Some studies suggest that certain infections may trigger AS in genetically susceptible individuals.
Immunological Mechanisms:
- Inflammation: Chronic inflammation plays a central role in the pathogenesis of AS. The immune system mistakenly attacks the joints and entheses (the sites where tendons and ligaments attach to bone), leading to inflammation and tissue damage.
- Bone Remodeling: Inflammation triggers excessive bone formation, leading to the fusion of vertebrae and other joints. [16]
Pathophysiology
Pathophysiology
- Ankylosing spondylitis is thought to arise from an as yet ill defined interaction between environmental pathogens and the host immune system in genetically susceptible individuals.
- Increased faecal carriage of Klebsiella aerogenes occurs in patients with established AS and may relate to exacerbation of both joint and eye disease.
- Wider alterations in the human gut microbial environment are increasingly implicated, which could lead to increased levels of circulating cytokines such as IL 23 that can activate entheseal or synovial T cells.
- The HLA B27 molecule itself is implicated through its antigen presenting function (it is a class I MHC molecule) or because of its propensity to form homodimers that activate leukocytes.
- HLA B27 molecules may also misfold, causing increased endoplasmic reticulum stress.
- This could lead to inflammatory cytokine release by macrophages and dendritic cells, thus triggering inflammatory disease. [1]
Clinical Features
Clinical Features:
The clinical features of Ankylosing Spondylitis (AS) can vary significantly between individuals, but common manifestations include:
Axial Features:
- Inflammatory Back Pain: This is often the first symptom, characterized by insidious onset, morning stiffness lasting over 30 minutes, and improvement with exercise. Pain typically affects the lower back and buttocks.
- Reduced Spinal Mobility: Progressive stiffness and reduced range of motion in the spine, particularly in the lumbar and thoracic regions.
- Chest Pain: Inflammation of the costovertebral joints can cause chest pain, which may worsen with deep breathing.
- Enthesitis: Inflammation at the sites where tendons and ligaments attach to bone, commonly affecting the Achilles tendon, plantar fascia, and iliac crest.
Peripheral Features:
- Peripheral Arthritis: Inflammation of joints outside the spine, typically affecting the hips, shoulders, and knees.
- Dactylitis: Swelling of an entire finger or toe, often referred to as "sausage digit."
- Uveitis: Inflammation of the uvea, the middle layer of the eye, causing pain, redness, and blurred vision.
- Other Extra-articular Manifestations: Less common features include cardiovascular complications (aortitis, conduction abnormalities), pulmonary involvement (apical fibrosis), and gastrointestinal issues (inflammatory bowel disease). [17]
Sign & Symptoms
Sign & Symptoms
Pain and stiffness:
- You may have constant pain and stiffness in the low back, buttocks, and hips that continues for more than 3 months.
- Ankylosing spondylitis often starts around the sacroiliac joints, where the sacrum (the lowest major part of the spine) joins the ilium bone of the pelvis in the lower back region.
- It might hurt more at night and get better when you wake up.
- You might also feel pain in other joints such as your knees, shoulders, and jaw.
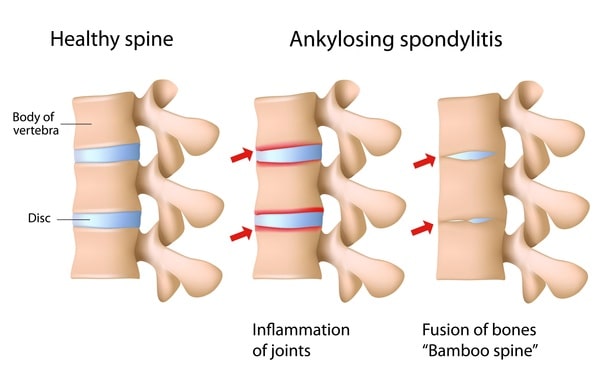
Fusion Of Bones
Bony fusion:
- Ankylosing spondylitis can cause an overgrowth of the bones, which may lead to abnormal joining of bones, called "bony fusion."
- Fusion affecting bones of the neck, back, or hips may affect your ability to perform everyday things.
- Fusion of the ribs to the spine or breastbone may limit your ability to expand your chest when taking a deep breath.
Pain in ligaments and tendons:
- Spondylitis also may affect some of the ligaments and tendons that attach to bones.
- Tendinitis (inflammation of the tendon) may cause pain and stiffness in the area behind or beneath the heel, such as the Achilles tendon.
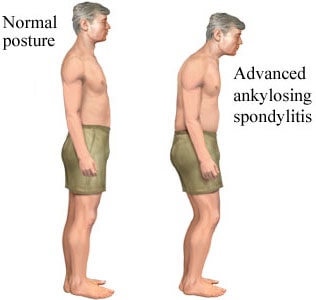
Bent Posture
Bent posture:
- If AS has gone undiagnosed and untreated, you might have a stooped posture from changes to your vertebrae.
Breathing problems:
- Changes in posture can lead to changes in your lungs that make it hard to breath.
Heart trouble:
- The inflammation can also affect your heart.
Eye problem:
- AS is linked to uveitis, a condition that causes inflammation in your eyes.
- Symptoms include pain, light sensitivity, and blurry vision.
Inflammatory bowel disease:
- The inflammation can also affect your digestive system.
- You might notice diarrhea, belly pain and cramps, bloody poop, less appetite, and weight loss without trying.
Psoriasis:
- About 10% of people with AS have this immune system disease that causes scaly, itchy red patches on their skin.
Fatigue:
- You could feel run down because of lack of sleep due to pain or as a part of the disease process itself.
Dactylitis:
- You may get swollen toes or fingers.
Fever:
- Person might have a mild fever.
Over many years, AS can cause new bone to grow on your spine, fusing the vertebrae and making it harder to move.
Generally, This can cause severe stiffness.
About half the people who have AS get either osteoporosis, or brittle bones. [4]
Clinical Examination
Clinical Examination of Ankylosing spondylitis
Appearance of the Patient
- Patients with ankylosing spondylitis usually appear normal.
Vital Signs
- Vital signs are within normal limits in patients with AS.
Cervical spine
- Forward stooping of the thoracic and cervical spine.
- The degree of flexion deformity is measured by asking the patient to stand erect with heels and buttocks against a wall and to extend the neck while keeping the mandible in the horizontal position and ask the patient to touch the wall.
- The degree of flexion deformity is measured by the distance between the occiput and the wall.
Thoracic spine
- The degree of chest expansion is measured by the range of motion of the costovertebral joints and is measured at the level of the xiphoid process.
- The physician must ask the patient to raise their arms beyond their heads and then ask the patient to maximal forced expiration how much they can and that is followed by a maximal inspiration.
- In normal individuals the expansion is usually >2 cm.
- In normal individuals it is greater than 10 cm.
Lateral spinal flexion
- Physician must ask the patient with AS to standing erect with heel and back against a wall and knees and hands extended and measure the distance between the tip of the middle finger and the floor.
- Then ask the patient to bend sideways without bending the knees.
Schober test
- In patients with AS Schober test is used to measure forward flexion of the lumbar spine.
- Physician must ask the patient to stands erect then a point is placed at the middle of a line joining the posterior superior iliac spines, another mark is made above 10 cm in the midline then ask the patient to bends forward how much they can without bending the knees and measure the distance.
- In normal individuals should exceed 2 cm.
Sacroiliac joint tenderness
- In AS patients to bring out sacroiliac pain apply direct pressure over the sacroiliac joint.
- Sacroiliac joint tenderness is also elicit by the following
- Ask the patient to be supine position, then apply direct pressure on the anterior superior iliac spine and, at the same time physician must apply force on iliac spine laterally.
- Ask the patient to be on the side, then physician must apply pressure to compress the pelvis.
- Ask the patient to be supine position, physician must ask the patient to flex one of the knees and then to abduct as well as externally rotate the corresponding hip, then apply pressure on the knee which is flexed and this elicit pain on the sacroiliac joint.
Hip joint
- When a patient with AS is exhibiting abnormal gait hip involvement should be suspected.
- In AS patients hip involvement lead to flexion deformities and can be assessed by internal and external rotation of the hip.
Dactylitis
- Dactylitis also called as sausage digits. In AS patients the fingers looks like in appearance.
Lungs
- Restrictive lung disease
- Upper lobe fibrosis
Cardiovascular
- Patients with AS present with following cardiovascular features
- Valvular heart disease
- Aortitis
- Conduction disturbance[8]
Diagnosis.
Diagnosis
- In established AS, radiographs of the sacroiliac joint show irregularity and loss of cortical margins, widening of the joint space and subsequently sclerosis, joint space narrowing and fusion.
- Lateral thoracolumbar spine X rays may show anterior ‘squaring’ of vertebrae due to erosion and sclerosis of the anterior corners and periostitis of the waist.
- Bridging syndesmophytes may also be seen.
- Basically, these are areas of calcification that follow the outermost fibres of the annulus.
- In advanced disease, ossification of the anterior longitudinal ligament and facet joint fusion may also be visible.
- The combination of these features may result in the typical ‘bamboo’ spine.
- Erosive changes may be seen in the symphysis pubis, the ischial tuberosities and peripheral joints.
- Osteoporosis and atlantoaxial dislocation can occur as late features.
- Patients with early disease can have normal X Rays, but if clinical suspicion is high, MRI should be performed.
- This is much more sensitive for detection of early sacroiliitis than X ray and can also detect inflammatory changes in the lumbar spine.
Criteria for diagnosing Ankylosing Spondylitis:
Imaging e.g. |
|
History |
|
Clinical Examination such as, |
|
Investigations such as, |
|
[1]
The features include i.e.:
- Pain that does not improve with rest.
- Pain that causes sleep disturbance.
- Back pain that starts gradually, before the age of 40 years, and is not caused by injury.
- Symptoms that persist for over 3 months.
- Spinal stiffness in the mornings, which improves with exercise and motion. [3]
Differential Diagnosis
Differential Diagnosis of Ankylosing spondylitis
- Chronic Lower Back Pain
- Reactive Arthritis
- Fibromyalgia
- Psoriatic Arthritis
- Enteropathic Arthritis
- DISH[11]
Complications
Complications:
Ankylosing Spondylitis (AS) can lead to various complications over time, affecting multiple organ systems:
Spinal Complications:
- Spinal Fusion: Progressive inflammation and ossification can lead to fusion of the vertebrae, resulting in a rigid spine and limited mobility.
- Spinal Fractures: Weakened vertebrae due to chronic inflammation are more prone to fractures, even with minor trauma.
- Cauda Equina Syndrome: A rare but serious complication involving compression of nerve roots at the base of the spinal cord, causing bowel/bladder dysfunction, sensory loss, and weakness in the lower extremities.
Extraspinal Complications:
- Peripheral Arthritis: Inflammation of joints outside the spine, typically affecting the hips, shoulders, and knees.
- Uveitis: Inflammation of the uvea, the middle layer of the eye, causing pain, redness, and blurred vision.
- Cardiovascular Disease: AS is associated with an increased risk of aortitis (inflammation of the aorta) and other cardiovascular complications.
- Osteoporosis: Chronic inflammation can lead to decreased bone density, increasing the risk of fractures.
- Pulmonary Involvement: Restrictive lung disease and apical fibrosis can occur due to limited chest expansion. [18]
Investigations
Investigation of Ankylosing spondylitis
Blood tests
If your GP suspects AS, they may arrange blood tests to check for signs of inflammation in your body. Inflammation in your spine and joints is a main symptom of the condition.
If your results suggest you do have inflammation, you’ll be referred to a rheumatologist for further tests. A rheumatologist is a specialist in conditions that affect muscles and joints.
Further tests
Your rheumatologist will carry out imaging tests to examine the appearance of your spine and pelvis, as well as further blood tests.
These may include:
- an X-ray
- a MRI scan
- an ultrasound scan
Genetic testing
A genetic blood test may sometimes be carried out to see if you carry the HLA-B27 gene, which is found in most people with AS.
This can contribute towards a diagnosis of AS, but it’s not entirely reliable as not everyone with the condition has this gene and some people have the gene without ever developing AS.[9]
Treatment
Treatment of Ankylosing spondylitis
The goal of treatment is to relieve your pain and stiffness, because prevent or delay complications and spinal deformity.
Moreover, Ankylosing spondylitis treatment is most successful before the disease causes irreversible damage to your joints.
Medications:
Nonsteroidal anti-inflammatory drugs (NSAIDs) such as naproxen (Naprosyn) and indomethacin (Indocin) are the medications doctors most commonly use to treat ankylosing spondylitis.
They can relieve your inflammation, pain and stiffness. However, these medications might cause gastrointestinal bleeding.
If NSAIDs aren’t helpful, your doctor might suggest starting a biologic medication, such as a tumor necrosis factor (TNF) blocker or an interleukin 17 (IL-17) inhibitor.
TNF blockers target a cell protein that causes inflammation in the body.
IL-17 plays a role in your body’s defense against infection and also has a role in inflammation.
TNF blockers help reduce pain, stiffness, and tender or swollen joints.
They are administered by injecting the medication under the skin or through an intravenous line.
The five TNF blockers approved by the Food & Drug Administration to treat ankylosing spondylitis are i.e.:
- Adalimumab (Humira)
- Certolizumab pegol (Cimzia)
- Etanercept (Enbrel)
- Golimumab (Simponi; Simponi Aria)
- Infliximab (Remicade)
Secukinumab (Cosentyx) is the first IL-17 inhibitor approved by the FDA for the treatment of ankylosing spondylitis.
TNF blockers and IL-17 inhibitors can reactivate latent tuberculosis and make you more prone to infection.
Therapy:
- Physical therapy is an important part of treatment and can provide a number of benefits, from pain relief to improved strength and flexibility.
- A physical therapist can design specific exercises for your needs.
- Range-of-motion and stretching exercises can help maintain flexibility in your joints and preserve good posture.
- Proper sleep and walking positions and abdominal and back exercises can help maintain your upright posture.
Surgery:
Most people with ankylosing spondylitis don’t need surgery.
However, your doctor might recommend surgery if you have severe pain or joint damage, or if your hip joint is so damaged that it needs to be replaced. [2]
Prevention
Prevention of Ankylosing Spondylitis
- Stay physically active.
- Use good posture.
- Prevent neck injuries by always using the right equipment and the right form when exercising or playing sports.
- Avoid trauma to your neck.[12]
Homeopathic Treatment
Homeopathic Treatment of Ankylosing Spondylitis
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Ankylosing Spondylitis:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
1. Aesculus Hippocastanum
- Generally, Aesculus Hippocastanum is a top listed medicine for ankylosing spondylitis.
- This medicine is prepared from a plant commonly called ‘horse chestnut.’
- The natural order of this plant is Sapindaceae.
- The prominent symptom indicating the use of Aesculus Hippocastanum is a pain in the sacrum and the hips.
- Along with this, there is marked stiffness in the lower back.
- The symptoms get worse from rising from the seat, also the person has to make repeated efforts.
- At the same time, there is a sensation as if the back would break.
- Aching pains in the lumbar, sacral also the pelvic region are treated well with homeopathic medicine Aesculus Hippocastanum.
Key indications for using aesculus hippocastanum i.e.:
- Pain in sacrum and hips due to inflammation.
- Besides this, Marked stiffness in the lower back.
- Back pain worse rising from a seat and on stooping.
2. Kalmia Latifolia
- Kalmia Latifolia is specifically a highly beneficial medicine for ankylosing spondylitis.
- This medicine is prepared from the fresh leaves of a plant i.e. ‘Mountain Laurel.’
- The natural order of this plant is Ericaceae.
- It is indicated when there is a constant pain in the spine.
- Pain in the lumbar area and a burning/heat sensation in the lumbar spine is present.
- A feeling of lameness in the back is present.
- Sometimes there is a sensation as if the back would break.
- There is also an intense pain in the neck (cervical spine) along with stiffness.
- The neck feels tender to the touch.
- Kalmia Latifolia is an effective homeopathic remedy for the pain in the neck (cervical spine) which then radiates to the shoulders.
- Early morning worsening of neck pain and stiffness is also present.
Key indications for using kalmia latifolia i.e.:
- Constant pain in the spine.
- Pain in lumbar back attended with heat / burning in the spine.
- Neck pain and stiffness.
3. Rhus Toxicodendron
- Rhus Tox is especially a well indicated medicine for ankylosing spondylitis.
- It helps in reducing the stiffness of the back.
- The stiffness is most intense in the morning.
- Sitting also aggravates the stiffness.
- Rhus Tox also works wonders in reducing back stiffness that gets worse from taking rest.
- Here lying or sitting still worsens the stiffness.
- The person requiring Rhus Tox gets relief by walking.
- Pain in the lower back is also severe along with stiffness.
- Rhus Tox is also a natural medicine for managing back pain which gets relieved by the application of hard pressure.
Key indications for using Rhus Tox:
- Intense stiffness in the back.
- Back stiffness that is worse in the morning or due to inactivity.
- Back pain and stiffness that is reduced by walking.
4. Colocynthis
- Colocynthis is a medicine especially, for ankylosing spondylitis with marked hip pain. Additionally, It is prepared from a plant named ‘bitter cucumber.’
- Moreover, This plant belongs to the family Cucurbitaceae.
- For using Colocynthis hip pain may be cramping, drawing or tearing in nature.
- The pain from hip may also extend down to the knee, leg or even to the feet in a few cases.
- Sensitivity to touch the affected hip is also seen in many cases.
- Colocynthis is also a useful remedy for hip pain that gets better by lying on the affected side.
- In some cases, pressure on the affected hip offers comfort.
- Hip pain that gets better by warmth also indicates the use of homeopathic medicine Colocynthis.
- The person needing Colocynthis also experiences an aggravation of hip pain by sitting, standing, being in motion, and gets relief from rest.
5. Bryonia Alba
- Bryonia Alba is another well-indicated medicine for treating ankylosing spondylitis.
- This medicine is prepared from a plant commonly named ‘Wild Hops.’
- The natural order of this plant is Cucurbitaceae.
- A backache that is worse from motion or walking is the guiding feature to use Bryonia Alba.
- In a few cases, stooping, standing and sitting also worsen the backache.
- The relief in back pain is afforded only with absolute complete rest.
- Stiffness is also present along with a backache.
- The stiffness is so intense that a person has to sit and walk in a stooped posture.
- Maintaining an upright posture while sitting/walking is difficult.
6. Agaricus Muscarius
- Agaricus Muscarius is majorly used in ankylosing spondylitis when the spine is sensitive to touch, along with pain.
- The sensitivity of the spine is severe in the morning.
- Other symptoms pointing towards the use of Agaricus Muscarius are back pain getting worse from stooping, a burning sensation in the spine, and a feeling of tightness in the back muscles.
- A lumbosacral backache that is worse during daytime exertion is also treated well with Agaricus Muscarius.
- A marked stiffness in the back is present along with pain.
- There is a sensation as if the back would break.
- Another sensation that may appear is that of a cold or hot needle piercing the back.
7. Kali Carbonicum
- Kali Carb is a medicine is especially used to treat ankylosing spondylitis where weakness in the lower back accompanies back pain.
- The pain is present in the lower back, hips, also thighs.
- Besides this, The person feels better by lying down.
- It is also helpful when there is difficulty in turning in bed from a backache.
- Another chief indication to use kali carb is a sharp pain in back extending up and down.
8. Natrum Muriaticum
- Natrum Mur is specifically, another valuable medicine used to treat ankylosing spondylitis.
- The characteristic feature to use natrum mur is relief from back pain upon lying down, especially on a hard surface.
- Other symptoms include difficulty in stooping, a pulsating sensation in the back and pain in the sacrum.
- The person needing homeopathic medicine Natrum Mur may also need firm support on the back.
9. Cimicifuga Racemosa
- It is prepared from a plant i.e. black cohosh of natural order Ranunculaceae.
- Cimicifuga Racemosa is used to treat neck (cervical back) pain and stiffness in cases of ankylosing spondylitis.
- A contracted sensation in the neck is present, because the neck is sensitive to touch.
- Pressure seems to worsen the pain in the neck.
- Any motion of the head and hands also aggravates the neck pain.
- Worsening of neck pain from exposure to cold air is also treated well with homeopathic medicine Cimicifuga Racemosa.
10. Calcarea Fluorica
- Calcarea Fluor is a especially indicated medicine for dissolving osteophytes (bony outgrowths appearing in the spine) in cases of ankylosing spondylitis.
- Another symptom that suggests the use of Calcarea Fluor is a back pain that is worse from rest conversely, better from motion.
- Application of warmth may also relieve back pain in a few cases.
- Restlessness along with back pain is also present.
11. Tellurium Met
- Tellurium Met is a medicine for ankylosing spondylitis with marked sacral pain radiating down the thigh.
- The back is sensitive, so that the pain gets worse from touch.
- A feeling of weakness in the back, and cervical back pain spreading to the shoulder and between the scapulae are other symptoms that indicate the need for this medicine.
- The cervical spine is also sensitive to pressure and touch.
12. Conium Maculatum
- Conium Maculatum is especially indicated when there is a severe aching in the sacral region from walking a short distance.
- Stitching pain in the sacrum when standing, weakness also lameness in the small of the back, tightness in the nape of the neck with pain and stiffness and soreness in the lower cervical spine are also present.
- Pain in the dorsal back between both the shoulders and the lumbar region also indicates the need for this medicine.
13. Guaiacum
- Guaiacum is a significant medicine for ankylosing spondylitis with a stiff neck.
- It is a plant-based medicine especially, prepared from the plant ‘Guaiacum Officinale.’ Additionally, The natural order of this family is Zygophyllaceae.
- Marked stiffness in the neck is the key feature to use this medicine.
- Pain in the neck and the back (between scapulae) is also treated well with this medicine.
- It is also indicated in some cases where neck pain radiates down the sacrum. [5]
Diet & Regimen
Diet & Regimen

Exercises Of Ankylosing Spondylitis
Back Against a Wall i.e.:
- Firstly, Stand against a wall, with your heels and buttocks touching the wall.
- Secondly, Squeeze your shoulder blades together.
- Then, Hold for 5 seconds, then relax.
- At last, Repeat.
Prone Lying i.e.:
- Lie on your stomach.
- Slowly prop yourself up on your elbows so that your chest is off the ground.
- If you’re able, straighten your arms.
- Hold for 10 to 20 seconds, then return to start position.
- Repeat.
Seated Thoracic Extension i.e.:
- Sit upright in a chair, with your feet flat on the floor.
- Place your hands behind your head for support, with your elbows out to the sides.
- Keeping your head still, slowly roll the top of your spine over the back of the chair.
- Hold for 5 to 10 seconds, then return to start position.
- Repeat.
Quadricep Stretch i.e.:
- Lie on your stomach.
- Loop a strap, belt, or sheet around the top of one foot.
- Gently pull the strap over your shoulder until you feel a stretch through the muscle.
- Hold for 10 to 20 seconds, then return to start position.
- Repeat on the other side.
Seated Figure Four Stretch i.e.:
- Firstly, Sit upright in a chair, with your feet flat on the floor.
- Secondly, Lift your right leg and place your right foot on top of your left thigh, just above your knee.
- After that, Keeping your spine as straight as possible, slowly hinge forward.
- For a deeper stretch, apply gentle pressure on the right thigh.
- Hold for 10 to 20 seconds, then return to start position.
- Similarly, repeat on the other side.
Plank i.e.:
- Lie on your stomach with your forearms on the floor also elbows directly below your shoulders.
- Tighten your stomach muscles additionally, lift your hips off the floor.
- Squeeze your buttock muscles, also left your knees off the floor.
- Keep your body straight, but without letting your pelvis sag toward the floor.
- Hold for 10 to 20 seconds, then return to start position.
- Repeat. [6]
Do's & Don'ts
Do’s & Don’ts
Do’s:
- Exercise Regularly: Engage in regular physical activity, including stretching, aerobic exercises, and strengthening exercises. This helps maintain flexibility, reduce pain, and improve posture.
- Maintain Good Posture: Practice standing and sitting with proper posture to prevent spinal deformities. Consider using ergonomic chairs and pillows.
- Quit Smoking: Smoking can worsen inflammation and disease progression. Seek help to quit if needed.
- Take Medications as Prescribed: Follow your doctor’s instructions for medications, including NSAIDs, DMARDs, or biologics.
- Eat a Healthy Diet: A balanced diet rich in fruits, vegetables, and whole grains can help manage inflammation and maintain a healthy weight.
- Get Enough Sleep: Aim for 7-8 hours of sleep per night to allow your body to rest and repair.
Don’ts:
- Avoid High-Impact Activities: Limit activities that put excessive stress on your joints, such as running or jumping.
- Don’t Ignore Pain: If you experience new or worsening pain, consult your doctor. Early intervention can prevent complications.
- Avoid Excessive Alcohol Consumption: Alcohol can interfere with medications and worsen inflammation.
- Don’t Slouch or Hunch Over: Poor posture can exacerbate spinal stiffness and pain.
- Avoid Overexertion: Listen to your body and rest when needed. Pushing yourself too hard can worsen symptoms. [19]
Terminology
Terminology Of Ankylosing Spondylitis:
Ankylosing Spondylitis (AS):
- A chronic inflammatory disease primarily affecting the spine, causing pain, stiffness, and potential fusion of the vertebrae.
Sacroiliac Joints:
- The joints connecting the base of the spine (sacrum) to the pelvic bones (ilium). These are often the first to be affected in AS.
HLA-B27:
- A gene strongly associated with AS, present in most people with the condition.
Prevalence:
- The proportion of a population found to have a particular condition.
Ankylosis:
- Stiffening or fusion of a joint due to abnormal bone growth, a common feature of advanced AS.
Inflammatory Arthritis:
- Arthritis characterized by inflammation of the joints, causing pain, swelling, and stiffness.
Miasmatic Tendency:
- In homeopathy, a predisposition to certain types of diseases based on inherited or acquired factors.
Potency:
- In homeopathy, refers to the strength or dilution of a remedy.
Repetition of Dose:
- How often a homeopathic remedy is taken.
Insidious Onset:
- Gradual onset of a disease without obvious initial symptoms.
Morning Stiffness:
- Stiffness experienced in the morning, often a characteristic feature of inflammatory arthritis.
Enthesitis:
- Inflammation at the sites where tendons or ligaments attach to bone.
Uveitis:
- Inflammation of the uvea, the middle layer of the eye.
Extra-Articular Manifestations:
- Symptoms or conditions occurring outside of the joints.
Dactylitis:
- Inflammation of an entire finger or toe, often referred to as "sausage digit."
Lumbar:
- Relating to the lower back.
Sacral:
- Relating to the sacrum, the bone at the base of the spine.
Pelvic:
- Relating to the pelvis, the bony structure that supports the lower spine and connects the legs.
Lumbosacral:
- Relating to the lumbar spine and sacrum.
Osteophytes:
- Bony outgrowths that develop on bone edges, often seen in AS.
NSAIDs:
- Nonsteroidal anti-inflammatory drugs, commonly used to manage pain and inflammation in AS.
DMARDs:
- Disease-modifying antirheumatic drugs, used to slow the progression of inflammatory arthritis.
Biologics:
- Targeted therapies that suppress the immune system’s response, used in moderate to severe AS.
This list aims to clarify the medical and homeopathic terms used in the article, enhancing your understanding of Ankylosing Spondylitis and its homeopathic treatment approaches.
References
References
- Davidson’s Principles and Practice of Medicine (22nd edition) Ch. 25
- https://www.mayoclinic.org/diseases-conditions/ankylosing-spondylitis/symptoms-causes/syc-20354808
- https://www.medicalnewstoday.com/articles/248217.php
- https://www.webmd.com/arthritis/what-is-ankylosing-spondylitis#1
- https://www.drhomeo.com/ankylosing-spondylitis/ankylosing-spondylitis-homeopathic-remedies/
- https://creakyjoints.org/diet-exercise/ankylosing-spondylitis-stretches-exercises/
- https://www.webmd.com/ankylosing-spondylitis/guide/types-stages-ankylosing-spondylitis
- https://www.wikidoc.org/index.php/Ankylosing_spondylitis_physical_examination
- https://www.nhs.uk/conditions/ankylosing-spondylitis/diagnosis/
- https://www.healthline.com/health/ankylosing-spondylitis/ankylosing-spondylitis-causes#whos-at-risk
- https://creakyjoints.org/about-arthritis/axial-spondyloarthritis/axspa-overview/ankylosing-spondylitis-misdiagnosis/
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/cervical-spondylosis
- Indian Rheumatology Association consensus statement on the diagnosis and treatment of axial spondyloarthropathies, 2009.
- Alarming rise in Ankylosing Spondylitis amongst young Indian workforce, 2017.
- Clinical characteristics of patients with ankylosing spondylitis in India, 2009.
- Kelley’s Textbook of Rheumatology, 11th Edition (2023) by Gary S. Firestein, et al. (Editors)
- Harrison’s Principles of Internal Medicine, 21st Edition (2022) by Dennis L. Kasper, et al. (Editors)
- Oxford Textbook of Rheumatology, 5th Edition (2018) by David A. Isenberg, et al. (Editors)
- The Spondylitis Association of America’s Guide to Ankylosing Spondylitis (2019) by Spondylitis Association of America (Author)
Also Search As
Also Search As
There are several ways people can search for information on Ankylosing Spondylitis (AS):
Online Search Engines:
- Google: The most popular search engine, simply type "Ankylosing Spondylitis" or related terms like "AS symptoms," "AS treatment," etc.
- Bing: Another major search engine with a similar approach to Google.
- DuckDuckGo: A privacy-focused search engine that doesn’t track your searches.
Medical Websites & Organizations:
- Mayo Clinic: Provides comprehensive information on diseases and conditions, including AS.
- Versus Arthritis: A UK-based charity with information on various forms of arthritis, including AS.
- Spondylitis Association of America: A patient advocacy organization dedicated to providing information and support for people with AS.
- Arthritis Foundation: Offers resources and information on arthritis, including AS.
Online Medical Libraries & Databases:
- PubMed: A free database of biomedical literature, including research articles on AS.
- Google Scholar: Another source for scholarly articles on AS.
Social Media:
- Facebook Groups & Forums: Many online communities exist where people with AS can connect, share experiences, and learn from each other.
- Twitter: Following relevant hashtags (e.g., #AnkylosingSpondylitis) can lead to news, research updates, and personal stories about AS.
Additional Tips:
- Use Specific Search Terms: For more targeted results, use specific terms like "ankylosing spondylitis diagnosis," "ankylosing spondylitis complications," etc.
- Consult with a Healthcare Professional: If you have specific questions or concerns about AS, it’s always best to consult with a doctor or rheumatologist for personalized advice.
Remember, while online resources can provide valuable information, always verify the information from reputable sources and consult with a healthcare professional for any medical concerns.
There are several methods to search for an article on Ankylosing Spondylitis (AS):
1. Online Search Engines:
- Keywords: Use specific keywords like "Ankylosing Spondylitis," "AS symptoms," "AS treatment," or "AS causes."
- Search Operators: Refine your search using operators like quotation marks (""Ankylosing Spondylitis"") for exact phrases or minus sign (-review) to exclude certain types of results.
2. Academic Databases:
- PubMed: A free resource for biomedical and life sciences literature. Use keywords or MeSH terms (Medical Subject Headings) to find relevant articles.
- Google Scholar: Search for scholarly articles and books on AS. Filter by date, relevance, or publication type.
3. Medical Websites & Organizations:
- Reputable Sources: Look for information on websites of trusted organizations like the Mayo Clinic, Arthritis Foundation, Spondylitis Association of America, or Versus Arthritis.
- Specific Sections: Check for sections on research, publications, or news to find articles related to AS.
4. Social Media:
- Hashtags: Search for relevant hashtags on platforms like Twitter (e.g., #AnkylosingSpondylitis, #AS) to find news, discussions, and potentially links to articles.
- Groups & Communities: Join online forums or groups dedicated to AS. Members often share links to articles or research findings.
5. Libraries:
- Medical Libraries: If you have access to a medical library, ask a librarian for assistance in finding relevant articles in medical journals or databases.
- Public Libraries: Many public libraries offer access to online databases and resources where you might find articles on AS.
Tips:
- Look for Peer-Reviewed Articles: Prioritize articles published in reputable medical journals for accurate and reliable information.
- Check References: Look at the reference list of the article you find. This can lead you to other relevant articles.
- Consult with a Healthcare Professional: If you need help interpreting research findings or have questions about AS, talk to your doctor or a rheumatologist.
Frequently Asked Questions (FAQ)
Can AS be cured?
There is currently no cure for AS, but early diagnosis and proper management can significantly improve quality of life.
How is AS diagnosed?
Diagnosis involves a combination of medical history, physical examination, imaging studies (X-ray, MRI), and blood tests.
What are the symptoms of AS?
- Common symptoms include inflammatory back pain, stiffness, reduced spinal mobility, chest pain, and fatigue.
What is Ankylosing Spondylitis (AS)?
AS is a chronic inflammatory disease that primarily affects the spine, causing pain, stiffness, and potentially leading to spinal fusion.
Is homeopathic treatment safe for AS?
Homeopathic remedies are generally considered safe when prescribed by a qualified practitioner. However, it is essential to consult with a healthcare professional before starting any new treatment, especially if you are already taking conventional medications.
What are the treatment options for AS?
Treatment aims to manage pain, improve mobility, and prevent complications. Options include medications (NSAIDs, DMARDs, biologics), physical therapy, and lifestyle modifications.
Can homeopathy help with Ankylosing Spondylitis (AS)?
Homeopathy aims to treat AS by addressing the underlying causes of inflammation and pain through individualized remedies. While some anecdotal evidence suggests potential benefits, scientific research on homeopathy for AS is limited.
What homeopathic remedies are commonly used for AS?
Homoeopathic Medicine For Ankylosing Spondylitis
Common remedies include Rhus Toxicodendron, Bryonia Alba, Calcarea Carbonica, and Kali Carbonicum. However, the selection of a specific remedy depends on individual symptoms and overall health condition.
Are there any side effects of homeopathic treatment for AS?
Homeopathic remedies are generally safe and have minimal side effects. However, some people may experience a temporary worsening of symptoms before improvement, known as a homeopathic aggravation.
How long does it take to see results with homeopathic treatment for AS?
Theresponse to homeopathic treatment varies for each individual. Some people may experience improvement in symptoms within weeks, while others may take longer.
