Asthma
Definition
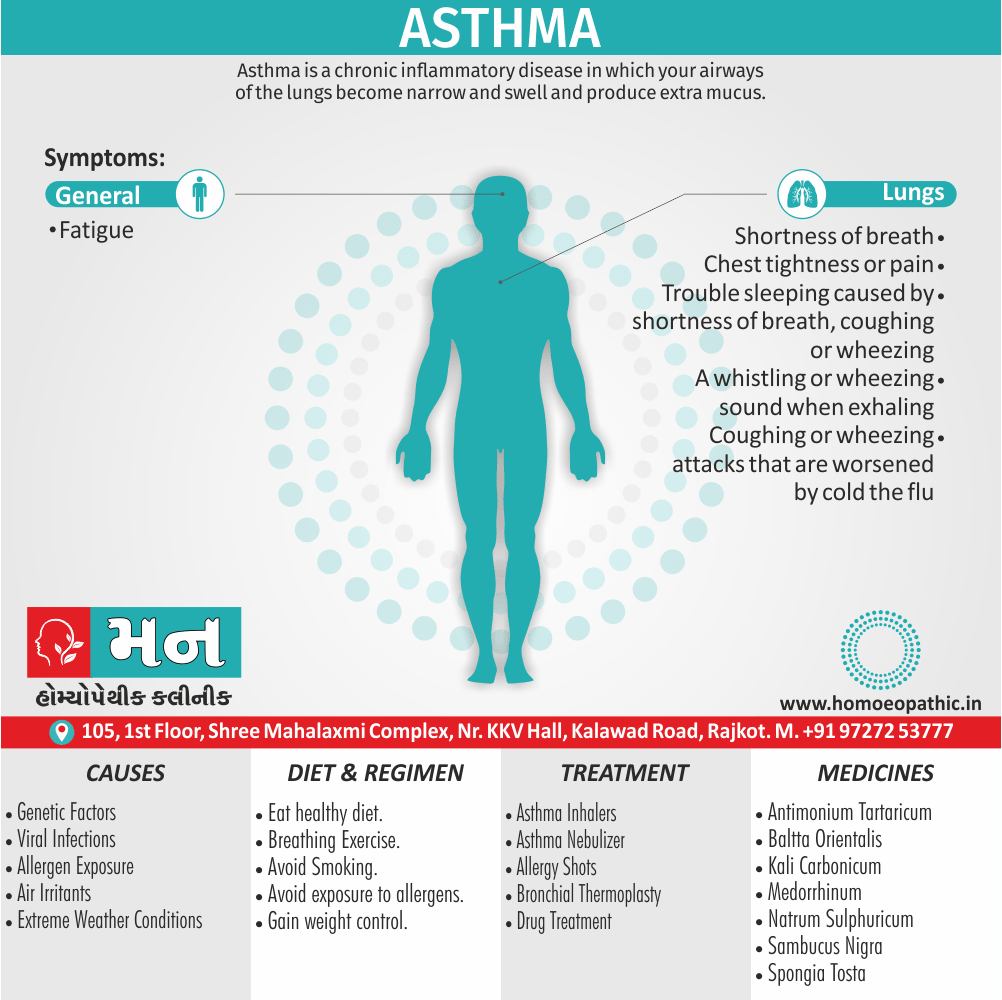
Asthma is a chronic inflammatory disease in which your airways of the lungs become narrow and swell and produce extra mucus. [2]
here are some related terms:
- Bronchial asthma: This term highlights the involvement of the airways (bronchi) in the condition.
- Airway hyperreactivity: This refers to the increased sensitivity of the airways in It, which leads to narrowing and breathing difficulties.
- Asthmatic bronchitis: This is an outdated term that’s not commonly used anymore. It combined asthma and chronic bronchitis, which are now recognized as separate conditions.
Informal terms:
- Wheezing: This is a symptom of It, not the condition itself, but it’s often used colloquially to describe It.
Focus on specific aspects:
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do's & Don'ts
Terminology
References
Also Search As
Overview
Overview of Asthma
- It is a chronic inflammatory disorder of the airways, in which many cells and cellular elements play a role.
- The chronic inflammation is associated with airway hyper-responsiveness that leads to recurrent episodes of wheezing, breathlessness, chest tightness and coughing, particularly at night and in the early morning.
- Current estimates suggest that It affects 300 million people worldwide, with a predicted additional 100 million people affected by 2025.
- Although the development and course of the disease, and the response to treatment, are influenced by genetic determinants, the rapid rise in prevalence implies that environmental factors are critically important in the development and expression of the disease.
Reason of Asthma :
- To date, studies have explored the potential role of indoor and outdoor allergens, microbial exposure, diet, vitamins, breastfeeding, tobacco smoke, air pollution and obesity but no clear consensus has emerged.
- These episodes are usually associated with widespread but variable airflow obstruction within the lung that is often reversible, either spontaneously or with treatment. [1]
- For some people,It is a minor nuisance. For others, it can be a major problem that interferes with daily activities and may lead to a life-threatening asthma attack.
- It can’t be cured, but its symptoms can be controlled.
- Because It often changes over time. [2]
Epidemiology
Epidemiology of Asthama
Several studies have investigated the epidemiology of asthma in India:
Epidemiology of asthma in India (Paramesh, H., 2002): This review article provides an overview of Its prevalence, morbidity, and mortality in India, highlighting the need for improved diagnosis and management strategies. (Indian Journal of Pediatrics, 69(4), 309-312) [10]
Indian Study on Epidemiology of Asthma, Respiratory Symptoms and Chronic Bronchitis in adults (INSEARCH) (2003): This nationwide study estimated the prevalence of asthma in adults to be 2.05%, with variations observed across different regions and socioeconomic groups. [11]
Prevalence, time trends and treatment practices of asthma in India: the Global Asthma Network study (2022): This study found an overall asthma prevalence of 5.06% among adults, with significant variations observed by age, gender, and region. (European Respiratory Society, 8(2), 00528-2021) [12]
Prevalence of asthma among children in India: A systematic review and meta-analysis (2022): This systematic review estimated the pooled prevalence of It among Indian children to be 8.7%, with considerable heterogeneity across studies. [13]
These studies collectively provide valuable insights into the burden of It in India, highlighting the need for continued research and targeted interventions to address this significant public health challenge.
Please note that this is not an exhaustive list, and several other studies have been conducted on the epidemiology of asthma in India. You can find more information by searching academic databases or consulting relevant publications.
Causes
Cause of Asthma
No single cause has been identified for It. Instead, researchers believe that the breathing condition is caused by a variety of factors.
Genetics:
- If a parent has asthma, you’re more likely to develop it.
History of viral infections:
- People with a history of viral infections during childhood are more likely to develop the condition.
Hygiene hypothesis:
- This hypothesis proposes that babies aren’t exposed to enough bacteria in their early months and years.
- Therefore, their immune systems don’t become strong enough to fight off asthma and other conditions.
Early allergen exposure:
- Frequent contact with possible allergens and irritants may increase your risk for developing asthma.
Certain conditions and environments may also trigger symptoms of asthma:
illness:
Exercise:
- Increased movement may make breathing more difficult.
Irritants in the air:
- People with asthma may be sensitive to irritants such as chemical fumes, strong odors, also smoke.
Allergens:
- For instance; Animal dander, dust mites, and pollen are just a few examples of allergens that can trigger symptoms.
Extreme weather conditions:
- Conditions such as very high humidity or low temperatures may trigger disease.
Emotions:
- For example; Shouting, laughing, and crying may trigger an attack. [3]
Types
Types of Asthma
The most common type of It is bronchial asthma, which affects the bronchi in the lungs.
Additional forms of It include childhood asthma and adult-onset asthma.
In adult-onset asthma, symptoms don’t appear until at least age 20.
Other types of asthma are described below i.e.
Allergic Asthma (extrinsic asthma):
Allergens trigger this type of asthma.
These might include e.g.:
- Pet dander from animals like cats and dogs
- Food
- Mold
- Pollen
- Dust
Allergic asthma is more likely to be seasonal because it often goes hand-in-hand with seasonal allergies.
Nonallergic Asthma (intrinsic asthma):
Irritants in the air not related to allergies trigger this type of asthma.
Irritants might include e.g.:
- Burning wood
- Cigarette smoke
- Cold air
- Air pollution
- Viral illnesses
- Air fresheners
- Household cleaning products
- Perfumes
Occupational Asthma:
Occupational asthma is a type of asthma induced by triggers in the workplace.
These include e.g.:
- Dust
- Dyes
- Gases and fumes
- Industrial chemicals
- Animal proteins
- Rubber latex
These irritants can exist in a wide range of industries, including farming, textiles, woodworking, also manufacturing.
Exercise-induced bronchoconstriction (EIB):
- Exercise-induced bronchoconstriction (in other words, EIB) usually affects people within a few minutes of starting exercise and up to 10–15 minutes after physical activity.
- This condition was previously known as exercise-induced asthma (EIA).
- Up to 90 percent of people with asthma also experience EIB, but not everyone with EIB will have other types of asthma.
Nocturnal Asthma:
- In this type of asthma, symptoms worsen especially at night.
- Triggers that are thought to bring on symptoms at night include heartburn, pet dander, also dust mites.
- The body’s natural sleep cycle may also trigger nocturnal asthma.
Cough-variant Asthma (CVA):
- Cough-variant asthma doesn’t have classic asthma symptoms of wheezing and shortness of breath.
- CVA is characterized by a persistent, dry cough.
- Cough-variant asthma can lead to full-blown asthma flares that include the other more common symptoms. [3]
Status asthmaticus:
- These prolonged asthma attacks don’t respond to treatment with bronchodilators also are a medical emergency.
- They need immediate treatment.
Asthma in children:
Symptoms can vary from episode to episode in the same child.
Symptoms of asthma i.e.:
- Frequent coughing spells, which may happen during play, at nighttime, or while laughing.
- Moreover, Less energy during play, or pausing to catch breath during play.
- Either Rapid or shallow breathing.
- Complaint of chest tightness or chest "hurting".
- Whistling sound when breathing in or out. Additionally, This sound is called wheezing.
- Seesaw motions in the chest from labored breathing. These motions are called retractions.
- Shortness of breath, loss of breath.
- Tightened neck and chest muscles.
- Weakness or tiredness.
Risk Factors
Risk Factors
A number of factors are thought to increase your chances of developing It.
These include i.e.:
- Having a blood relative (such as a parent or sibling) with same disease.
- Having another allergic condition, such as atopic dermatitis or allergic rhinitis (e.g. hay fever).
- Being higher-weight person,
- Being a smoker or exposure to secondhand smoke.
- Exposure to exhaust fumes or other types of pollution.
- Exposure to occupational triggers, such as chemicals used in farming, hairdressing also manufacturing.
Pathogenesis
Pathogenesis of asthma
The pathogenesis is a complex process involving multiple factors and pathways. Here are some references from well-known textbooks that delve into the details of Its pathogenesis:
Robbins & Cotran Pathologic Basis of Disease (10th edition, 2021): This book provides a comprehensive overview of the pathophysiologic mechanisms underlying asthma, including airway inflammation, bronchoconstriction, and airway remodeling. It also discusses the role of genetic and environmental factors in Its development. [14]
Harrison’s Principles of Internal Medicine (21st edition, 2022): This textbook offers a detailed discussion of pathogenesis, covering the cellular and molecular mechanisms involved in airway inflammation and hyperresponsiveness. It also highlights the contributions of various inflammatory mediators and cytokines to It pathophysiology. [15]
Murray & Nadel’s Textbook of Respiratory Medicine (7th edition, 2023): This comprehensive textbook provides an in-depth analysis of pathogenesis, exploring the complex interactions between genetic predisposition, environmental triggers, and immune dysregulation. It also discusses the role of airway epithelial cells, smooth muscle cells, and inflammatory cells in asthma pathophysiology. [16]
Middleton’s Allergy: Principles and Practice (9th edition, 2020): This textbook offers a detailed discussion of the allergic mechanisms involved in pathogenesis, including the role of IgE, mast cells, and eosinophils. It also covers the various environmental triggers that can initiate or exacerbate asthma symptoms. [17]
Please note that these are just a few examples, and numerous other textbooks and resources are available that discuss asthma pathogenesis in detail. You can find more information by searching academic databases or consulting relevant publications.
Pathophysiology
Pathophysiology
- Airway hyper-reactivity (AHR) the tendency for airways to narrow excessively in response to triggers that have little or no effect in normal individuals is integral to the diagnosis of asthma and appears to be related, although not exclusively, to airway inflammation.
- Other factors likely to be important in the behavior of airway smooth muscle include the degree of airway narrowing and neurogenic mechanisms.
- Besides this, the relationship between atopy (in other words the propensity to produce IgE) also asthma is well established, and in many individuals there is a clear relationship between sensitization and allergen exposure, as demonstrated by skin prick reactivity or elevated serum specific IgE.
Allergens i.e.:
- Common examples of allergens include house dust mites, pets such as cats and dogs, pests such as cockroaches, and fungi.
- Inhalation of an allergen into the airway is followed by an early and late-phase broncho constrictor response.
- Allergic mechanisms of an array of cytokines, chemo-kines and growth factors.
- Examination of the inflammatory cell profile in induced sputum samples demonstrates that, although It is predominantly characterized by airway eosinophilia, neutrophilic inflammation predominates in some patients, while, in others, scant inflammation is observed: so-called ‘pauci-granulocytic’ asthma.
- With increasing severity and chronicity of the disease, remodeling of the airway may occur, leading to fibrosis of the airway wall, fixed narrowing of the airway additionally a reduced response to bronchodilator medication. [1]
Clinical Features
Clinical Features of Asthama
The clinical features are well-described in various medical textbooks. Here are a few references:
Harrison’s Principles of Internal Medicine (21st edition, 2022, McGraw Hill): This comprehensive textbook details the classic triad of asthma symptoms: wheezing, breathlessness, and cough. It also discusses the variability of these symptoms, their nocturnal worsening, and the triggers that can exacerbate them. [15]
Murray and Nadel’s Textbook of Respiratory Medicine (7th edition, 2023, Elsevier): This textbook provides an in-depth overview of the clinical manifestations, including the characteristic patterns of airflow obstruction, the physical examination findings, and the use of spirometry for diagnosis and monitoring. [16]
Global Initiative for Asthma (GINA) guidelines (2023 update): While not a textbook, these guidelines offer a comprehensive overview of asthma symptoms and their assessment, emphasizing the importance of recognizing the variability and periodicity of symptoms, as well as the impact on quality of life. [18]
Middleton’s Allergy: Principles and Practice (9th edition, 2020, Elsevier): This textbook focuses on the allergic aspects of It, detailing the clinical presentation of allergic asthma and the relationship between asthma and other allergic conditions like allergic rhinitis and atopic dermatitis. [17]
These references collectively provide a comprehensive overview of the clinical features of It, emphasizing the importance of recognizing the variability and complexity of the disease presentation.
Sign & Symptoms
Sign and Symptoms of Asthma
Asthma symptoms vary from person to person.
You may have infrequent asthma attacks, have symptoms only at certain times such as when exercising or have symptoms all the time.
Asthma signs and symptoms i.e.:
- Shortness of breath.
- Chest tightness or pain.
- Trouble sleeping caused by shortness of breath, coughing or wheezing.
- A whistling or wheezing sound when exhaling (generally wheezing is a common sign of asthma in children).
- Either Coughing or wheezing attacks that are worsened by a respiratory virus, such as a cold or the flu.
Signs that your asthma is probably worsening i.e.:
- It’s signs and symptoms that are more frequent and bothersome.
- Increasing difficulty breathing (especially, measurable with a peak flow meter, a device used to check how well your lungs are working).
- The need to use a quick-relief inhaler more often.
For some people, asthma signs and symptoms flare up in certain situations i.e.:
- Exercise-induced asthma, which may be worse when the air is cold also dry.
- Occupational asthma, triggered by workplace irritants such as chemical fumes, gases or dust.
- Allergy-induced asthma, triggered by airborne substances, such as pollen, mold spores, cockroach waste or particles of skin and dried saliva shed by pets (specifically pet dander) [2]
Asthma is commonly mistaken for a cold or chest infection which is taking time to resolve (e.g. longer than 10 days).
Classical precipitants include exercise, particularly in cold weather, exposure to airborne allergens or pollutants, and viral upper respiratory tract infections.
Wheeze apart, there is often very little to find on examination.
An inspection for nasal polyps and eczema should be performed.
Occasionally, a vasculitic rash may suggest Churg– Strauss syndrome.
Patients with mild intermittent asthma are usually asymptomatic between exacerbations.
Individuals with persistent asthma report ongoing breathlessness and wheeze, but these are variable, with symptoms fluctuating over the course of one day, or from day to day or month to month.
Asthma characteristically displays a diurnal pattern, with symptoms and lung function being worse in the early morning. [1]
Clinical Examination
Physical Examination
Physical examination may be normal or can be characteristically present with a loud polyphonic expiratory wheeze.
Vitals
Pulse Rate
- Increased heart rate in acute severe episode
Strength
- Pulsus paradoxus (a fall of SBP between 10-20mmHg during inspiration) in moderately severe episode
- Pulsus paradoxus (a fall of SBP greater than 20-40 mmHg during inspiration) in acute severe episode and imminent respiratory failure
Respiratory Rate
- Increased respiratory rate greater than 30 cycles per minute in moderately severe and acute severe episodes
Skin
- Profuse sweating in imminent respiratory failure
- Severe hypoxia resulting in central cyanosis and hypoventilation in imminent respiratory failure
Eyes
- Conjunctival congestion as a consequence of constant rubbing are suggestive of associated allergic rhinitis.
Nose
- Nasal examination is mandatory to rule out associated conditions such as, aspirin sensitivity or allergic rhinitis.
- Transverse crease on nose as a consequence of constant rubbing and pale swollen nasal mucosa are suggestive of associated allergic rhinitis.
Lungs
Mild Episode
- Prolong end-expiratory wheeze
- In between attacks, chest is clear and no abnormal physical signs may be detectable.
Moderately Severe Episode
- Use of accessory muscles of respiration such as sternocleidomastoid and scalene muscles
- Hyper-resonant lungs
- Loud prolonged expiratory wheeze with a reduced inspiration to expiration ratio
- Vesicular breath sounds with prolonged respiration
Acute Severe Episode
- Patient has to sit upright with arms extended to support the upper chest (tripod position) that assist the use of accessory muscles of respiration
- Use of accessory muscles of respiration
Imminent Respiratory Failure
- Paradoxical thoraco-abdominal breathing
- Wheeze and breath sounds are typically absent secondary to severe airway obstruction, representing a silent chest which is an ominous sign.
Chronic Asthma
- Persistent scattered rhonchi
Other Associated Findings
Diagnosis
Diagnosis of Asthma
Physical examination:
To rule out other possible conditions such as a respiratory infection or chronic obstructive pulmonary disease (in other words, COPD); physical examination & history of symptoms is necessary.
Tests to measure lung functions:
You may also be given lung (in other words, pulmonary) function tests to determine how much air moves in and out as you breathe.
These tests may i.e.:
Spirometry:
- This test estimates the narrowing of your bronchial tubes by checking how much air you can exhale after a deep breath and how fast you can breathe out.
- A spirometry test can provide an indication of lung function.
- A spirometry can help assess lung function.
- Spirometry is a non-invasive test that requires deep breaths and forceful exhalation into a hose.
- The hose links to a machine called a spirometer that displays two key measurements:
- Forced vital capacity (FVC), or the maximum amount of air a person can both inhale and exhale.
- Forced expiratory volume (FEV-1), the maximum amount of air a person can exhale in one second.
- The doctor then compares these measurements against what would be normal for another person of the same age.
- In general, Measurements below normal indicate obstructed airways and probable It.
- A doctor will often administer a bronchodilator drug to open air passages before retesting with the spirometer to confirm the diagnosis.
- If results improve after using the drug, the risk of an asthma diagnosis increases.
- Besides this, Children under 5 years of age are difficult to test using spirometry, so asthma diagnoses will rely mostly on symptoms, medical histories, and other parts of the physical examination process.
- In younger children, doctors commonly prescribe asthma medicines for 4 to 6 weeks to gauge physical response.
Peak flow:
- A peak flow meter is a simple device that measures how hard you can breathe out.
- Lower than usual peak flow readings are a sign your lungs may not be working as well and that your asthma may be getting worse.
- Your doctor will give you instructions on how to track and deal with low peak flow readings.
- Lung function tests often are done before and after taking a medication called a bronchodilator, such as albuterol, to open your airways.
- If your lung function improves with use of a bronchodilator, it’s likely you have It.
Other tests to diagnose include:
Methacholine challenge:
- Methacholine is a known trigger that, when inhaled, will cause mild constriction of your airways.
- If you react to the methacholine, you likely have It.
- This test may be used even if your initial lung function test is normal.
Nitric oxide test:
- This test, though not widely available, measures the amount of the gas, nitric oxide, that you have in your breath.
- When your airways are inflamed a sign you may have higher than normal nitric oxide levels.
Imaging tests:
- A chest X-ray and high-resolution computerized tomography (CT) scan of your lungs and nose cavities (sinuses) can identify any structural abnormalities or diseases (such as infection) that can cause or aggravate breathing problems.
Allergy testing:
- This can be performed by a skin test or blood test.
- Allergy tests can identify allergy to pets, dust, mold and pollen.
- If important allergy triggers are identified, this can lead to a recommendation for allergen immunotherapy.
Sputum eosinophils:
- This test looks for certain white blood cells (eosinophils) in the mixture of saliva and mucus (sputum) you discharge during coughing.
- Eosinophils are present when symptoms develop and become visible when stained with a rose-colored dye (eosin).
Provocative testing for exercise and cold-induced asthma:
- In these tests, your doctor measures your airway obstruction before and after you perform vigorous physical activity or take several breaths of cold air.
How asthma is classified ?
To classify your severity, your doctor considers your answers to questions about symptoms (such as how often you have asthma attacks and how bad they are), along with the results of your physical exam and diagnostic tests.
Determining your asthma severity helps your doctor choose the best treatment.
severity often changes over time, requiring treatment adjustments.
It is classified into four general categories:
Asthma classification | Signs and symptoms |
|---|---|
| Mild intermittent | This symptoms up to two days a week and up to two nights a month |
| Mild persistent | Symptoms more than twice a week, but no more than once in a single day |
| Moderate persistent | Symptoms once a day and more than one night a week |
| Severe persistent | Symptoms throughout the day on most days and frequently at night |
[2]
Differential Diagnosis
Differential Diagnosis of Asthma
- Chronic obstructive pulmonary disease (COPD),
- Congestive heart failure,
- Gastroesophageal reflux disease,
- Mechanical obstruction of the airways (e.g., tumors, foreign bodies), and
- Vocal cord dysfunction.
Infrequent causes of wheezing include i.e.
- Pulmonary embolism,
- Pulmonary infiltrates with eosinophilia, and
- Some medications (e.g., angiotensin-converting enzyme (ACE) inhibitors)[8]
Complications
Complications
Several textbooks detail the potential complications of asthma:
Harrison’s Principles of Internal Medicine (21st edition, 2022, McGraw Hill): This comprehensive textbook discusses the complications of severe asthma, including status asthmaticus, respiratory failure, pneumothorax, pneumomediastinum, and atelectasis. It also mentions the long-term consequences of poorly controlled asthma, such as airway remodeling and fixed airflow obstruction. [15]
Murray and Nadel’s Textbook of Respiratory Medicine (7th edition, 2023, Elsevier): This textbook provides an in-depth overview of the potential complications of asthma, including acute exacerbations, respiratory failure, and the development of chronic obstructive pulmonary disease (COPD) in some patients. It also discusses the psychological and social impact of It. [16]
Asthma: Clinician’s Desk Reference (1st edition, 2014, Routledge): This practical guide for clinicians outlines the acute and chronic complications of It, including status asthmaticus, respiratory acidosis, and the development of bronchiectasis. It also discusses the impact of asthma on growth and development in children. [19]
Global Initiative for Asthma (GINA) guidelines (2023 update): While not a textbook, these guidelines provide a comprehensive overview of the potential complications of It, including exacerbations, hospitalizations, and the development of comorbidities such as anxiety and depression. [18]
These resources emphasize that while asthma is a manageable condition for most patients, it can lead to serious complications if not properly controlled. Early recognition and treatment of exacerbations are crucial to prevent these complications and improve long-term outcomes for patients with asthma.
Investigations
Investigation of Asthma
The main tests used to help diagnose asthma are:
- FeNO test – you breathe into a machine that measures the level of nitric oxide in your breath, which is a sign of inflammation in your lungs
- spirometry – you blow into a machine that measures how fast you can breathe out and how much air you can hold in your lungs
- peak flow test – you blow into a handheld device that measures how fast you can breathe out, and this may be done several times over a few weeks to see if it changes over time
After you’re diagnosed with It, you may also have a chest X-ray or allergy tests to see if your symptoms might be triggered by an allergy.[7]
Treatment
Treatment
It is is a chronic condition but may be controlled with appropriate treatment in the majority of patients.
The goal of treatment should be to obtain and maintain complete control, but aims may be modified according to the circumstances and the patient.
A variety of tools/questionnaires have been validated to assist in assessing control.
Written action plans can be helpful in developing self management skills.
Avoidance of aggravating factors:
- This is particularly important in the management of occupational asthma but may also be relevant in atopic patients, when removing or reducing exposure to relevant antigens, such as a pet, may effect improvement.
- House dust mite exposure may be minimised by replacing carpets with floorboards and using mite impermeable bedding.
- So far, improvements in control following such measures have been difficult to demonstrate.
- Many patients are sensitised to several ubiquitous aeroallergens, making avoidance strategies largely impractical.
- Measures to reduce fungal exposure and eliminate cockroaches may be applicable in specific circumstances, and medications known to precipitate or aggravate It should be avoided.
- Smoking cessation is particularly important, as smoking not only encourages sensitisation, but also induces a relative corticosteroid resistance in the airway. [1]
Rescue Inhalers (or Quick-Relief Inhalers):
Asthma & Inhaler
- These are medications you breathe in.
- You use them to ease symptoms when they happen.
- They relax the muscles that tighten around the airways.
- This helps to open them up so you can breathe easier.
- If you’re using this type of medication more than 2 days a week, see your doctor.
These medications include:
- Short-acting beta-agonists, which are the first choice for quick relief of symptoms.
- Anticholinergics to reduce mucus in addition to opening your airways. Additionally, They take longer to work than short-acting beta-agonists.
- Oral corticosteroids to lower swelling in your airways
- Combination quick-relief medicines contain both an anticholinergic and a short-acting beta-agonist. If you can’t use an inhaler, you might get them from a nebulizer, a machine that helps you breathe in medicine.
Preventative, Long-Term Medications:
These medications work over the long term to treat symptoms and prevent attacks.
Furthermore, they reduce swelling and mucus in your airways.
As a result, the airways are less sensitive and less likely to react to triggers.
They include:
Inhaled corticosteroids i.e.:
- To prevent swelling.
- They also reduce mucus in your lungs.
- They’re the most effective long-term control medicines.
- Corticosteroids aren’t the same as anabolic steroids people use to grow muscle.
Inhaled long-acting beta-agonists i.e.:
- To open your airways by relaxing the smooth muscles around them.
- You’ll take this medication along with an inhaled corticosteroid.
Combination inhaled medicine i.e.:
- This medicine pair an inhaled corticosteroid with a long-acting beta-agonist.
- This is an easy way to take them together.
Biologics i.e.:
- That target a cell or protein in your body to prevent airway inflammation.
- They can either be shots or infusions you get every few weeks.
- They’re expensive, so that you usually get them if other medications don’t work.
Leukotriene modifiers i.e.:
- For relax the smooth muscles around your airways and ease swelling.
- You can take them either as pills or liquids.
Cromolyn i.e.:
- It prevents your airways from swelling when they come into contact with an trigger.
- It’s a non-steroid medicine that comes in an inhaler.
Theophylline i.e.:
- To relax the smooth muscles that narrow your airways.
- It comes as a tablet, capsule, solution, or syrup to take by mouth.
Long-acting bronchodilators i.e.:
- You might use these along with corticosteroids if you have ongoing symptoms despite treatment with a daily inhaled steroid.
- Never use long-acting bronchodilators alone as a long-term asthma treatment.
Oral corticosteroids i.e.:
- If no other medicine can get your attacks under control, your doctor might have you take these medications for a couple of weeks.
- They come either in pills or liquids.
How Do You Take Medications?
Inhalers:
- Inhalers are the most common and effective way to deliver medicine to the lungs.
- Moreover, they’re available in several types that work in different ways.
- Some deliver one medication.
- Others contain two different medications.
Nebulizer:
- If you’re having trouble using small inhalers, your doctor may prescribe an nebulizer.
- This machine changes asthma medications from a liquid to a mist so it’s easier to get the medicine into your lungs.
- It also has a mouthpiece or mask that makes it a good option for infants, small children, older adults, or anyone who has trouble using inhalers with spacers.
- It does take a few more minutes than using an inhaler.
Bronchial thermoplastic:
- People with asthma often have extra smooth muscle in their airway walls.
- Generally, In this procedure, the doctor uses a small tube known as a bronchoscope to send heat to the walls also reduce the smooth muscle.
Alternative Treatments:
Breathing exercises:
- These can lower the amount of medication you need to control your symptoms.
Herbal and natural remedies:
- Black seed oil (in other words, Nigella sativa): Some studies have shown it can help open airways.
- Caffeine: It’s a mild bronchodilator (meaning it can open your airways), but it doesn’t work as fast as medications. Avoid if for several hours before any doctor’s appointment that might include a lung function test.
- Choline: This substance helps with bodily functions. You can get it in meat, liver, eggs, poultry, fish, shellfish, peanuts, also cauliflower or from a supplement.
- Pycnogenol: You can get this pine bark extract as a supplement. [4]
Prevention
Homeopathic Treatment
Homeopathic Treatment of of Asthma
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines of Asthma:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Homeopathic remedies
Natrum Sulphuricum:
- It is aggravated by damp weather, the severe cough that makes a person hold his chest while coughing.
- Greenish expectoration.
Ipecac:
Antimonium Tartaricum:
- It is associated with a lot of rattling in the chest especially with little expectoration.
Sambucus Nigra:
- Childhood asthma.
- The attack is generally worse at midnight making child wake up from sleep.
Blatta Orientalis :
- It is from a damp environment.
- There can be an allergy to mildew, rotting leaves, mounds.
- Aggravation especially from exertion also ascending.
Senega:
- Wheeze also cough end in a sneeze.
- Furthermore, There is a pain in back on coughing.
- Rattling in the chest.
Ocimum sanctum:
- Generally, Pain in the chest while coughing sneezing, can’t be quiet in bed during the attack.
Lobelia inflata:
- It is without cough also expectoration.
- It is worse after any exertion.
Medorrhinum:
- It is better by bending his head on a pillow and the patient desires fast fan even in winter especially with a craving for ice.
Lycopodium:
- Flapping of alae nasi also rapid abdominal movement.
Some Postures:
- Bending head backward ameliorates: i.e. Spongia Tosta
- Must rise up and bend the head backward: i.e. Hepar Sulph
- Sitting with head bend forward on knees, amel: i.e. Kali Carbonicum
- Sitting with head bend forward and rocking: i.e. Kali Carbonicum
- Leaning backward, agg: Psorinum
- Bending forward, amel: e.g. Arsenicum Album, Cinchona, Kali Bichromicum, Kali Carbonatum, Lachesis, Spongia Tosta
- Difficult sitting bend forwards: e.g. Digitalis, Rhus Toxicodendron, Sepia
- Lying on back ameliorates: Cactus Grandiflorus
- Better lying on the right side: e.g. Spigelia, Colchicum [5]
Diet & Regimen
Diet And Regimen
Regimen and diet for asthma
Diet for Asthma
Eat plenty of:
- Fruits and vegetables
- Vitamin D-rich foods (fatty fish, fortified milk, eggs)
- Omega-3 fatty acids (salmon, tuna, flaxseeds, walnuts)
Be mindful of:
Regimen for Asthma
- Medication: Strictly follow your doctor’s prescribed asthma medication plan.
- Avoid triggers: Identify and minimize exposure to allergens (pollen, dust mites), irritants (smoke, pollution), and other triggers like exercise, cold air, and infections.
- Monitor your breathing: Use a peak flow meter as directed by your doctor to track lung function.
- Asthma action plan: Have a written plan from your doctor outlining steps to take when symptoms worsen or during an attack.
- Manage stress: Practice relaxation techniques to reduce stress, which can trigger asthma.
- Exercise regularly: Engage in suitable physical activity to improve lung function (consult your doctor for guidance).
- Clean indoor air: Reduce allergens and irritants in your home with regular cleaning, dust mite covers, and humidity control.
Important:
- Individualized approach: Work with your doctor to create a personalized asthma management plan.
- Medical advice: Always consult your doctor for diagnosis, treatment, and ongoing management of asthma.
- Emergency preparedness: Know how to recognize and respond to an asthma attack. Keep your rescue inhaler accessible and seek emergency care if needed
Do's & Don'ts
Do’s & Don’ts
Managing asthma effectively involves following specific dos and don’ts to prevent and control symptoms, reduce the risk of exacerbations, and maintain a good quality of life.
DO’s for Asthma:
- Take medications as prescribed: Use your preventer inhaler regularly as directed, even when you feel well, to reduce inflammation and prevent asthma attacks. Use your reliever inhaler immediately during an attack to relieve symptoms.
- Identify and avoid triggers: Keep a diary to track your symptoms and identify triggers such as pollen, dust mites, pet dander, smoke, or cold air. Avoid these triggers as much as possible.
- Have an asthma action plan: Work with your doctor to create a personalized plan outlining steps to take during an asthma attack, including when to use rescue medication and when to seek medical attention.
- Exercise regularly: Regular physical activity can help improve lung function and reduce asthma symptoms. However, consult your doctor before starting a new exercise program.
- Get vaccinated: Get vaccinated against influenza and pneumococcal disease to reduce the risk of respiratory infections that can trigger Its attacks.
- Monitor your peak flow: Use a peak flow meter to measure how well your lungs are working and track changes in your asthma control.
DON’Ts for Asthma:
- Don’t smoke: Smoking and exposure to secondhand smoke can worsen Its symptoms and increase the risk of attacks.
- Don’t ignore worsening symptoms: If your symptoms worsen or your rescue medication isn’t working, seek medical attention promptly.
- Don’t stop medication without consulting your doctor: Even if you feel well, don’t stop taking your preventer medication without your doctor’s approval, as this could lead to a flare-up.
- Don’t expose yourself to excessive pollution: Air pollution can trigger asthma symptoms. Avoid spending time in areas with high levels of pollution, especially on days with poor air quality.
- Don’t neglect stress management: Stress can trigger asthma attacks in some people. Find healthy ways to manage stress, such as exercise, meditation, or yoga.
By following these dos and don’ts, you can effectively manage your asthma and minimize the impact it has on your life. Remember to consult your doctor for personalized advice and guidance on managing your asthma.
Terminology
Terminology
The homeopathic article on It includes several medical and homeopathic-specific terms. Here’s a breakdown of some key terms and their meanings:
Medical Terms:
- Asthma: A chronic inflammatory lung disease characterized by airway narrowing, swelling, and mucus production, leading to difficulty breathing.
- Bronchial: This emphasizes the involvement of the bronchi (airways) in the lungs.
- Airway hyperreactivity: Increased sensitivity of the airways to triggers, causing them to narrow easily.
- Allergens: Substances that trigger allergic reactions, such as pollen, dust mites, or pet dander.
- Triggers: Factors that initiate or worsen asthma symptoms.
- Pathogenesis: The biological mechanism that leads to the development of a disease.
- Pathophysiology: The functional changes associated with a disease.
- Spirometry: A lung function test that measures how much and how quickly air can be exhaled.
- Peak flow: A measure of how fast you can forcefully exhale air.
- Bronchodilator: A medication that relaxes the muscles in the airways, making breathing easier.
- Status asthmaticus: A severe, prolonged It’s attack that doesn’t respond to usual treatment.
Homeopathic Terms:
- Homeopathy: A system of alternative medicine based on the principle of "like cures like."
- Miasmatic tendency: A predisposition to certain types of diseases, according to homeopathic theory.
- Homeopathic remedies: Substances used in homeopathy to treat various conditions.
- Potency: The number of times a homeopathic remedy has been diluted and succussed (shaken).
- Repetition of dose: How often a homeopathic remedy is taken.
- Aggravation: Worsening of symptoms after taking a homeopathic remedy (considered a positive sign in some cases).
- Amelioration: Improvement of symptoms after taking a homeopathic remedy.
Additional Terms in the Article:
- Epidemiology: The study of how often diseases occur in different groups of people and why.
- Clinical features: The signs and symptoms of a disease.
- Differential diagnosis: The process of distinguishing a particular disease from others with similar symptoms.
- Complications: New or additional problems that arise as a result of a disease.
References
References
- Davidson’s Principles and Practice of Medicine (22nd edition) Ch. 19
- https://www.mayoclinic.org/diseases-conditions/asthma/symptoms-causes/syc-20369653
- https://www.medicalnewstoday.com/articles/323523.php
- https://www.healthline.com/health/asthma
- https://hompath.com/blog/10-homeopathic-medicines-asthma/
- https://www.wikidoc.org/index.php/Asthma_physical_examination
- https://www.nhs.uk/conditions/asthma/diagnosis/
- https://www.atsdr.cdc.gov/csem/asthma/differential_diagnosis_of_asthma.html
- https://www.healthline.com/health/asthma/asthma-diet#foods-to-avoid
- Epidemiology of asthma in India (Paramesh, H., 2002)
- Indian Study on Epidemiology of Asthma, Respiratory Symptoms and Chronic Bronchitis in adults (INSEARCH) (2003)
- Prevalence, time trends and treatment practices of asthma in India: the Global Asthma Network study (2022)
- Prevalence of asthma among children in India: A systematic review and meta-analysis (2022)
- Robbins & Cotran Pathologic Basis of Disease (10th edition, 2021)
- Harrison’s Principles of Internal Medicine (21st edition, 2022)
- Murray & Nadel’s Textbook of Respiratory Medicine (7th edition, 2023)
- Middleton’s Allergy: Principles and Practice (9th edition, 2020)
- Global Initiative for Asthma (GINA) guidelines (2023 update)
- Asthma: Clinician’s Desk Reference (1st edition, 2014, Routledge)
Also Search As
Asthma Also Search As :
- Homeopathic remedies for It.
- Homeopathic asthma management
- Its treatment in homeopathy
- Natural remedies for asthma (homeopathic focus)
- Homeopathy for wheezing and breathlessness
- Homeopathic approach to allergic asthma
- Homeopathic medicines for childhood asthma
- Asthma and miasmatic treatment (homeopathic)
- Individualized homeopathic treatment for It
- Constitutional homeopathy for asthma
Allopathic Perspective Also Search As :
- Bronchial asthma treatment guidelines
- Medications and inhalers
- Prevention strategies
- Triggers and management
- Dagnosis and testing
- Severe asthma complications
- Latest research on asthma
- Action plan
- Pulmonary function tests for asthma
- Allergen immunotherapy for asthma
- Asthma in children and adults (differentiating factors)
There are several ways to search for articles on It, depending on the resources and tools you have access to. Here are some methods:
1. Academic Databases
- PubMed: A free search engine accessing primarily the MEDLINE database of references and abstracts on life sciences and biomedical topics.
- Google Scholar: Provides a simple way to broadly search for scholarly literature across many disciplines and sources.
- Cochrane Library: A collection of high-quality, independent evidence to inform healthcare decision-making.
- Scopus: A large abstract and citation database of peer-reviewed literature.
- Web of Science: Another comprehensive research database providing access to multiple databases that reference cross-disciplinary research.
2. Library Resources
- University Libraries: Many university libraries provide access to a range of databases and journals, often accessible through the library’s website.
- Public Libraries: Some public libraries offer access to databases and journals through their online portals.
3. Medical Websites and Journals
- American Thoracic Society (ATS): Offers articles and guidelines on respiratory health.
- Journal of Asthma: A peer-reviewed journal dedicated to the study of It.
- British Thoracic Society (BTS): Provides guidelines and articles on respiratory conditions, including It.
4. Government and Health Organizations
- Centers for Disease Control and Prevention (CDC): Offers a wealth of information on It, including statistics, guidelines, and research articles.
- World Health Organization (WHO): Provides global health data and publications on asthma.
- National Heart, Lung, and Blood Institute (NHLBI): Offers information and research articles on It.
5. General Internet Search
- Google Search: You can use specific keywords to find articles and information on asthma. For example, search for "asthma research articles" or "latest asthma treatment guidelines."
6. Professional Networks and Social Media
- ResearchGate: A social networking site for scientists and researchers to share papers and results.
- LinkedIn: Professionals and experts in the field often share articles and insights on medical topics, including asthma.
7. Medical Conferences and Seminars
- Attending conferences and seminars can provide access to the latest research and articles presented by experts in the field.
8. Direct Subscriptions
- Subscribing to specific journals or publications that focus on respiratory health and asthma can provide regular updates and access to articles.
People can search for information on asthma in various ways:
Online Resources:
- Search engines: Use Google, Bing, DuckDuckGo, or other search engines to search for terms like "asthma," "asthma symptoms," "asthma treatment," "homeopathic asthma treatment," or other relevant terms.
- Health websites: Consult reputable health websites such as the Mayo Clinic (https://www.mayoclinic.org/diseases-conditions/ asthma/symptoms-causes/syc-20369653), Cleveland Clinic (https://my.clevelandclinic.org/ health/diseases/6424-asthma), WebMD, or healthline.com for comprehensive information on asthma.
- Specific organizations: Look for information from organizations specializing in asthma, such as the Asthma and Allergy Foundation of America (AAFA) or the Global Initiative for Asthma (GINA).
- Academic databases: If you need more in-depth, scientific information, search academic databases like PubMed or Google Scholar for research articles and studies on asthma.
Offline Resources:
- Books: Consult medical textbooks, health encyclopedias, or books specifically focused on asthma.
- Libraries: Visit your local library for books and resources on asthma.
- Healthcare professionals: Talk to your doctor, allergist, or respiratory therapist for personalized information and advice on asthma.
Tips for Effective Searching:
- Use specific keywords: Instead of just searching for "asthma," use more specific terms like "asthma triggers," "asthma in children," or "natural remedies for asthma."
- Consider the source: Make sure the information you find comes from reputable sources, such as medical organizations or trusted health websites.
- Consult a professional: If you have specific questions or concerns about asthma, always consult a qualified healthcare professional for personalized advice.
Frequently Asked Questions (FAQ)
What is Asthma?
Definition
Asthma is a chronic lung disease that inflames and narrows the airways, making breathing difficult. It’s characterized by recurrent episodes of wheezing, breathlessness, chest tightness, and coughing.
What are the symptoms of Asthma?
- Shortness of breath.
- Chest tightness or pain
- Trouble sleeping
- Coughing or wheezing
- Whistling or wheezing sound when exhaling
- Difficulty breathing
What are the causes of Asthma?
Causes
- Genetics
- History of viral infections
- Early allergen exposure
- Illness
- Exercise
- Irritants in the air
- Allergens
- High humidity or low temperatures
- Shouting, laughing, also crying
How is asthma diagnosed?
Asthma diagnosis involves a review of your medical history, physical examination, and lung function tests like spirometry and peak flow measurement. These tests help assess how well your lungs are working.
What are some common asthma triggers?
Asthma triggers vary from person to person, but common ones include allergens (pollen, dust mites, pet dander), respiratory infections, exercise, cold air, smoke, and strong odors.
Are there different types of asthma?
Can homeopathy cure asthma?
Homeopathy aims to treat the whole person, including their individual symptoms and constitution, rather than just the disease itself. In some cases, homeopathic remedies may provide relief from asthma symptoms and improve overall well-being. However, the effectiveness of homeopathy in curing asthma lacks scientific consensus.
How does a homeopathic doctor select a remedy for asthma?
Homeopathic practitioners consider a wide range of factors when selecting a remedy, including the patient’s medical history, physical and mental constitution, family history, presenting symptoms, and potential triggers. They aim to address the root cause of the condition and restore overall health.
Is homeopathic treatment safe for asthma?
Homeopathic remedies are generally considered safe when prescribed by a qualified practitioner. However, it’s crucial to inform your healthcare providers about any homeopathic treatment you’re undergoing, especially if you’re also using conventional asthma medications.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Asthma?
Homoeopathic Medicines for Asthma
Several homeopathic remedies are often considered for asthma, each chosen based on the individual’s specific symptoms and constitution. Some of these remedies include Natrum Sulphuricum, Ipecac, Antimonium Tartaricum, Sambucus Nigra, Blatta Orientalis, Senega, and more. It’s important to consult a qualified homeopathic practitioner to determine the most suitable remedy for your specific case.
