Chikungunya
Definition
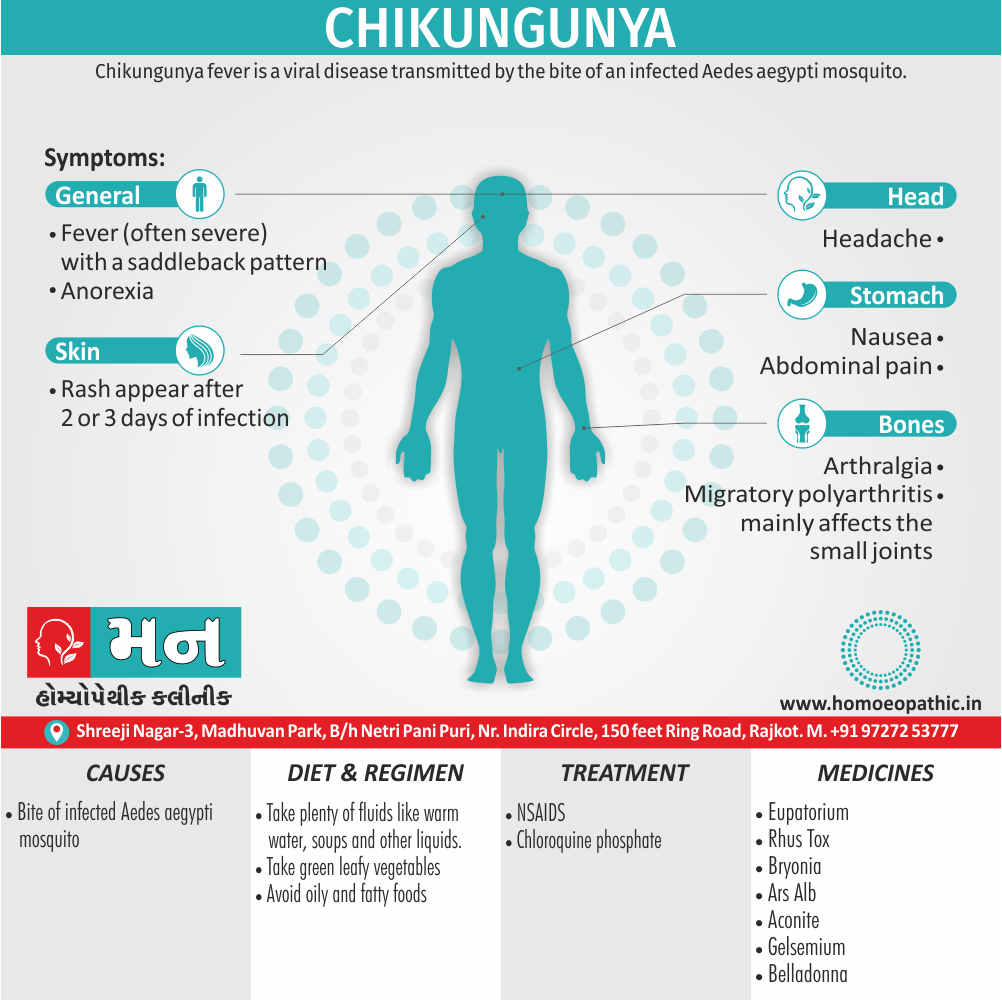
Chikungunya fever is a viral disease transmitted by the bite of infected Aedes aegypti mosquito. (1)
Chikungunya doesn’t have true synonyms in the medical field, as it’s a specific viral disease. However, depending on the context, here are some related terms you can consider:
- Chikungunya fever: This emphasizes the fever as a prominent symptom.
- CHIK: This is a common abbreviation for chikungunya used in medical contexts.
- CK: This is a less common abbreviation for chikungunya.
Informal Terms (use with caution):
- O’nyong-nyong fever: This is a similar viral disease that can cause confusion, so it’s best to avoid unless you’re specifically referring to that condition.
- Mayaro virus: This is another related virus, but it causes a different disease with distinct symptoms.
Important Considerations:
- In a medical setting, "chikungunya" is the most precise and recognized term.
- "Chikungunya fever" or "CHIK" might be used depending on the context, but prioritize clarity, especially for a general audience.
- Avoid informal terms or terms for similar diseases to prevent confusion.
Additionally:
- You could describe the symptoms of chikungunya, such as "a mosquito-borne viral illness causing fever, joint pain, and rash." This wouldn’t be a synonym but could be helpful in some contexts.
Remember, accurate communication is crucial when discussing diseases. "Chikungunya" or "chikungunya fever" are the most precise terms for most contexts.
Overview
Epidemiology
Causes
Risk Factors
Types
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Chikungunya
- Disease caused by chikungunya virus is endemic in rural areas of Africa.
- Intermittent epidemics take place in towns and cities of both Africa and Asia.
- Aedes aegypti mosquitoes are the usual vectors for the disease in urban areas.
- In 2004, a massive epidemic began in the Indian Ocean region (in particular on the islands of Réunion and Mauritius) and was most likely spread by travelers.
- Aedes albopictus was identified as the major vector of chikungunya virus during that epidemic.
- Between 2013 and 2014, several thousand chikungunya virus infections were reported (and several tens of thousands of cases were suspected) from Caribbean islands.
- The virus was imported to Italy, France, also the United States by travelers from the Caribbean.
- Chikungunya virus poses a threat to the continental United States as suitable vector mosquitoes are present in the southern states.
- Besides this, The disease is most common among adults, in whom the clinical presentation may be dramatic.
- Lastly, The abrupt onset of chikungunya virus disease follows an incubation period of 2–10 days. (2)
Epidemiology
Epidemiology
Chikungunya virus (CHIKV) is a significant public health concern in India, with a history of outbreaks and sporadic cases. The following provides an overview of the epidemiology of chikungunya in India, citing relevant references and their publication years:
Early outbreaks:
- The first recorded CHIKV outbreak in India occurred in Kolkata in 1963, followed by outbreaks in other cities in the 1960s and 1970s (Facts about the Chikungunya, n.d.).
- Retrospective serological tests suggest CHIKV was present in India before 1963 (Parida et al., 2022).
Sporadic cases and resurgences:
- Sporadic cases were reported in Maharashtra during the 1980s and 2000s (Facts about the Chikungunya, n.d.).
- CHIKV resurfaced in India in 2005, affecting several South Indian states (Mohan et al., 2012).
Recent trends:
- CHIKV outbreaks have become more frequent and widespread since 2004, partly due to viral adaptations (Chikungunya fact sheet, n.d.).
- In 2019, there were 81,914 clinically suspected cases of CHIKV in India, with 12,205 laboratory-confirmed cases across 21 states and 3 Union territories (Parida et al., 2022).
- As of July 2020, there were 18,533 clinically suspected CHIKV cases, with 2812 laboratory-confirmed cases (Parida et al., 2022).
- CHIKV remains endemic in 22 Indian states and 4 Union territories (Parida et al., 2022).
Causes
Causes
- CHIK virus is an alphavirus in the Semliki Forest complex (Togaviridae) and most closely related to o’nyong nyong (ONN) virus. (4)
Risk Factors
Risk Factors
the risk factors for Chikungunya are:
- Geographical location: Living in or traveling to areas where Chikungunya virus is endemic or experiencing an outbreak. The Aedes aegypti and Aedes albopictus mosquitoes, which transmit the virus, thrive in tropical and subtropical climates.
- Time of day: Chikungunya transmission is highest during daylight hours when Aedes mosquitoes are most active.
- Environmental factors: Areas with stagnant water, such as open containers, tires, or flower pots, provide breeding sites for Aedes mosquitoes, increasing the risk of transmission.
- Lack of protective measures: Not using mosquito repellents, wearing protective clothing, or using bed nets can increase the risk of mosquito bites and Chikungunya infection.
- Age: While people of all ages can be infected, older adults may be at higher risk of severe disease.
- Underlying medical conditions: Individuals with chronic illnesses, such as diabetes or heart disease, may be more susceptible to complications from Chikungunya. [10]
Types
Types
According to the book "Hunter’s Tropical Medicine and Emerging Infectious Diseases (11th Edition)" by Strickland G.T. (Editor) published in 2020 by Elsevier, there are not distinct "types" of Chikungunya in the traditional sense of different strains or variants. However, the book describes varying clinical presentations of Chikungunya infection, ranging from asymptomatic or mild cases to severe cases with prolonged joint pain and other complications.
The severity and duration of symptoms can vary depending on individual factors, such as age and underlying health conditions, but there are no distinct types of Chikungunya virus identified based on clinical presentation alone. [10]
Pathogenesis
Pathogenesis
The pathogenesis of Chikungunya involves the following steps:
Entry and Replication: After a bite from an infected mosquito, the Chikungunya virus (CHIKV) enters the skin and infects fibroblasts, the cells responsible for producing collagen and other structural components of tissues. The virus replicates within these cells.
Dissemination: The virus then spreads from the skin to other tissues, particularly the liver and joints, through the bloodstream.
Immune Response and Inflammation: The immune system recognizes the virus and mounts a response, but this response also contributes to the disease symptoms. The immune cells release inflammatory molecules that cause fever, rash, and joint pain. The virus can also infect macrophages, which are immune cells that normally engulf and destroy pathogens. This may contribute to the persistence of the virus in the body and the chronic joint pain that some people experience.
Joint Involvement: The virus has a particular affinity for the synovium, the tissue that lines the joints. Infection of the synovium leads to inflammation and damage, causing the severe joint pain and swelling that are characteristic of Chikungunya. In some cases, the joint pain can persist for months or even years after the initial infection. [10]
The exact mechanisms underlying the chronic joint pain and other complications of Chikungunya are still being investigated, but it is believed that the virus may persist in the joints or other tissues, causing ongoing inflammation and damage. [10]
Pathophysiology
Pathophysiology
- In India Aedes aegypti mosquito is the main vector.
- Aedes albopictus is also implicated.
- In Africa there is a sylvian cycle involving forest mosquitoes, humans and possibly other mammals.
- In Asia, sylvatic viral reservoirs have not been defined. (4)
Clinical Features
Clinical Features
Incubation Period:
Typically 3-7 days (range 1-12 days).
Acute Phase:
- Fever: High fever (>39°C or 102°F), often with abrupt onset.
- Arthralgia (Joint Pain): Severe, debilitating, and often symmetrical, affecting multiple joints. Commonly involves the hands, wrists, ankles, and feet.
- Arthritis (Joint Inflammation): Swelling, redness, and tenderness of the affected joints.
- Rash: Maculopapular (flat or raised red spots) rash, typically appearing a few days after the onset of fever.
- Other Symptoms: Headache, myalgia (muscle pain), fatigue, nausea, vomiting, and conjunctivitis (redness of the eyes).
Chronic Phase (Post-Chikungunya Chronic Inflammatory Rheumatism – PCCIR):
- Persistent or Recurrent Joint Pain: In some cases, joint pain can persist for months or even years after the initial infection.
- Other Symptoms: Fatigue, arthritis, tenosynovitis (inflammation of the tendon sheaths), and neurological manifestations (rare). [10]
Sign & Symptoms
Signs and Symptoms
- Fever (often severe) with a saddleback pattern and
- Severe arthralgia is accompanied by chills
- Abdominal pain
- Anorexia
- Conjunctival injection
- Headache
- Nausea
- Photophobia
- Migratory polyarthritis mainly affects the small 1313 joints of the ankles, feet, hands, and wrists, but the larger joints are not necessarily spared.
- Rash may appear at the outset or several days into the illness; its development often coincides with defervescence, which occurs around day either 2 or 3 of the disease.
- The rash is most intense on the trunk and limbs also may desquamate.
- Young children develop less prominent signs also are therefore less frequently hospitalized.
- Besides this, Children also often develop a bullous rather than a maculopapular/ petechial rash.
- Maternal–fetal transmission has reported and, in some cases, has led to fetal death. (2)
Clinical Examination
Clinical examination
Fever
The disease is characterized by an acute onset of high fever, typically more than 39°C (102°F).
Skin
- Maculopapular rash
- Nasal blotchy erythema
- Freckle-like pigmentation over centro-facial area
- Flagellate pigmentation on face and extremities
- Lichenoid eruption and hyperpigmentation in photodistributed areas
- Multiple aphthous-like ulcers over scrotum, crural areas and axilla.
- Lymphedema in acral distribution (bilateral/unilateral)
- Multiple ecchymotic spots (children)
- Vesiculobullous lesions (infants)
- Subungual hemorrhage
- Photo urticaria
- Acral urticaria
Joints
- Polyarthralgia usually symmetric and often occur in hands and feet
- Periarticular swelling and joint effusion in knees. (5)
Diagnosis
Diagnosis of Chikungunya
- Routine laboratory investigations are not specific. The ESR may be elevated to 20-50 mm/hr and CRP may also be elevated.
- Isolating the virus or identifying genomic products by PCR in acute phase blood specimens can confirm the diagnosis.
- Serologically specific IgM or other antibodies can be demonstrated by IgM capture ELISA test.
- This test will distinguish the condition form dengue which is also transmitted by the same vector.
- During the prevailing epidemic in south Kerala a few cases of co-infection by chikungunya and dengue have been observed. (4)
Differential Diagnosis
Differential Diagnosis of Chikungunya
Complications
Complications of Chikungunya
- Chronic Arthralgia/Arthritis: Persistent or recurrent joint pain affecting multiple joints, lasting for months or even years.
- Neurological Complications: Rare but can include encephalitis (inflammation of the brain), meningitis (inflammation of the membranes surrounding the brain and spinal cord), myelopathy (damage to the spinal cord), Guillain-Barré syndrome (immune system attacks the nerves), and other neurological manifestations.
- Cardiovascular Complications: Myocarditis (inflammation of the heart muscle) and other cardiac abnormalities.
- Ocular Complications: Uveitis (inflammation of the uvea, the middle layer of the eye), retinitis (inflammation of the retina), and optic neuritis (inflammation of the optic nerve).
- Other Complications: Hepatitis (inflammation of the liver), nephritis (inflammation of the kidneys), and skin manifestations (e.g., bullous lesions, vasculitis). [10]
Investigations
Investigations of Chikungunya
- Chikungunya virus diagnosed on the basis of serological test such as enzyme linked immunosorbent assays (ELISA) may presence of IgM and IgG anti- Chikungunya antibodies.
- IgM antibody levels are highest 3 to 5 weeks after the onset of illness and persist for about 2 months. (1)
Treatment
Treatment of Chikungunya
- Treatment is symptomatic with relief of pain with ibuprofen, naproxen, aceclofenac or paracetamol.
- Aspirin should avoid. (1)
- Chloroquine phosphate 250mg/day has found useful.
- Nonsteroidal anti-inflammatory drugs
- Sometimes chloroquine for refractory arthritis. (2)
Prevention
Prevention of Chikungunya
- An experimental live attenuated vaccine has shown to produce high levels of neutralizing antibody in human volunteers but efficacy has not tested.
- Anti-mosquito measures and personal protection with mosquito repellants will reduce the spread. (4)
Homeopathic Treatment
Homeopathic Treatment of Chikungunya
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Chikungunya:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
Eupatorium:
- The leading characteristic is violent aching, bone breaking pains.
- Muscles of chest, back and limbs feel bruised, sore aching.
- Patient is restless, chilly also nauseated.
- Colds, Influenza, Dengue.
- Sluggishness of all organs also functions.
- Useful in broken down constitutions of inebriate.
- Weakness
- Burning heat.
- Sweat; relieves all the symptoms except the headache.
- Sweat scanty (3)
Bryonia:
- Chill with hot head and red face, aggravation especially in warm room.
- Dry burning heat, with agg. of all the symptoms.
- Blood seems hot.
- Painful continued fevers.
- Sweat, either sour or oily
- Complaints from taking cold drinks, in hot weather. (3)
Gelsemium:
- Generally, Chill with aching and languor, mixed with heat or alternating with heat, chill up and down back.
- Cold hands also feet.
- Heat with drowsiness.
- Thirst absent, with trembling.
- Cold sweat.
- Bilious remittent, malarial, typhoid, cerebro-spinal fevers.
- Nervous, shuddering, chill, preceded especially by visual disturbances.
- Lastly, Inco-ordination of muscles, which do not obey the will (3)
Rhus Tox:
- Easily chilled aggravation specifically by least uncovering; with pain in limbs.
- Chill as if dashed with cold water or cold water in the veins; additionally preceded by cough; alternating with heat.
- Chill in single parts.
- Furthermore, Heat, with busy delirium.
- Typhoid.
- Sweat; aggravation especially during and pain; with sleepiness.
- Urticaria during fever.
- Wants to yawn also stretch during chill (3)
Arsenic Alb.:
- Externally cold, with internal burning heat.
- Coldness; in spots.
- Sensitive to cold, yet amel. in open air.
- Chills irregular, shaking, craves hot drinks during chill, Dyspnoea during chill.
- Besides this, Heat as of hot water in veins; or they burn like lines of fire.
- High fever, hectic fever.
- Sweat, with great thirst, either Dyspnoea or exhaustion.
- Sweat cold.
- Waves of icy coldness either in blood vessels or intense boiling heat.
- Intermittent fever, yellow fever. (3)
Aconite:
- Chill passes through him in waves.
- Either Chill or coldness alternating with heat.
- High fever, dry burning heat, in eyelids, nose, mouth, throat, lungs also palms, must uncover.
- Sweat drenching, wants to uncover.
- Sweat especially on uncovered parts or affected parts. (3)
Diet & Regimen
Diet and Regimen for Chikungunya
- Take plenty of fluids like warm water, soups also other liquids.
- Additionally, Take green leafy vegetables
- Take vit C rich fruits like orange, amla, lime.
- Avoid oily also fatty foods.
Do’s and Don'ts
The Do’s & Don’ts
Here are some general Dos and Don’ts for Chikungunya, combining information from various reliable sources:
Do’s:
- Do seek medical attention: If you experience symptoms like high fever, severe joint pain, or rash, consult a doctor promptly for diagnosis and treatment.
- Do rest: Get plenty of rest to help your body recover.
- Do stay hydrated: Drink plenty of fluids like water, juices, and oral rehydration solutions to prevent dehydration caused by fever and sweating.
- Do manage pain and fever: Use over-the-counter pain relievers like paracetamol (acetaminophen) as directed by your doctor. Avoid aspirin and non-steroidal anti-inflammatory drugs (NSAIDs) unless specifically prescribed, as they may increase the risk of bleeding.
- Do protect yourself from mosquito bites: Use mosquito repellents, wear long-sleeved shirts and pants, and use bed nets, especially during the daytime when Aedes mosquitoes are most active.
- Do eliminate mosquito breeding sites: Remove stagnant water from containers around your home, such as flower pots, tires, and buckets, to prevent mosquito breeding.
- Do get vaccinated: If available in your area, consider getting the Chikungunya vaccine for added protection.
Don’ts:
- Don’t self-medicate: Avoid taking any medications without consulting a doctor, as some drugs may interact with Chikungunya treatment or worsen symptoms.
- Don’t ignore symptoms: If you experience persistent or worsening symptoms, seek medical attention promptly.
- Don’t travel: If you have Chikungunya, avoid traveling to prevent spreading the virus to other areas.
- Don’t allow mosquito bites: Take preventive measures to avoid mosquito bites, as Chikungunya is primarily spread through infected mosquitoes.
Remember, these are general guidelines, and specific recommendations may vary depending on your individual circumstances. Always consult with a healthcare professional for personalized advice and treatment.
Terminology
Terminologies:
- Aedes aegypti/albopictus: Species of mosquitoes that are the primary vectors (transmitters) of the Chikungunya virus.
- Alphavirus: A type of virus to which the Chikungunya virus belongs.
- Arthralgia: Joint pain, a hallmark symptom of Chikungunya.
- Arthritis: Inflammation of the joints, which can occur in Chikungunya.
- Chikungunya fever: The full name of the disease, emphasizing the fever as a key symptom.
- CHIKV/CHIK: Abbreviations commonly used for the Chikungunya virus.
Chronic Phase (Post-Chikungunya Chronic Inflammatory Rheumatism – PCCIR):
- The phase of the illness after the acute symptoms subside, but where some patients experience long-term joint pain.
- ELISA: Enzyme-linked immunosorbent assay, a type of blood test used to detect Chikungunya antibodies.
- Endemic: A disease that is regularly found among particular people or in a certain area.
- Epidemic: A widespread occurrence of an infectious disease in a community at a particular time.
- Fibroblasts: Cells in connective tissue that are targeted by the Chikungunya virus.
- IgM/IgG: Types of antibodies produced by the immune system in response to Chikungunya infection.
- Incubation Period: The time between infection and the appearance of symptoms.
- Maculopapular rash: A type of rash with both flat and raised spots.
- Myalgia: Muscle pain.
- Pathogenesis: The manner in which a disease develops.
- Pathophysiology: The disordered physiological processes associated with disease or injury.
- PCR: Polymerase chain reaction, a test used to detect the genetic material of the Chikungunya virus.
- Sylvatic cycle: A transmission cycle of a disease that involves wild animals (such as monkeys) and mosquitoes.
- Vector: An organism, typically a biting insect or tick, that transmits a disease or parasite from one animal or plant to another.
- Viral reservoir: The long-term host of a virus.
Homeopathic-Specific Terms:
- Miasmatic tendency: A predisposition or susceptibility to certain types of diseases in homeopathic theory.
- Repertory: A book used by homeopaths to look up symptoms and find corresponding remedies.
- Rubric: A symptom category in a homeopathic repertory.
- Potency: The strength or dilution of a homeopathic remedy.
- Aggravation: A temporary worsening of symptoms after taking a homeopathic remedy, often considered a sign of the body’s healing response.
- Amelioration: An improvement in symptoms after taking a homeopathic remedy.
References
References of Chikungunya
- Textbook of Medicine by Golwala
- Harrisons Textbook of medicine
- Phatak materia medica
- Textbook of Medicine
- https://www.wikidoc.org/index.php/Chikungunya_differential_diagnosis, clinical examination
- Facts about the Chikungunya (n.d.). National Center for Vector Borne Diseases Control (NCVBDC). https://ncvbdc.mohfw.gov.in/index4.php?lang=1&level=0&linkid=488&lid=3764
- Chikungunya fact sheet (n.d.). World Health Organization (WHO). https://www.who.int/news-room/fact-sheets/detail/chikungunya
- Mohan, A., Kiran, K., Manohar, C., & Valli, T. (2012). Chikungunya Infection in India: Results of a Prospective Hospital Based Multi-Centric Study. PLoS ONE, 7(3).
- Parida, M., Dash, P. K., & Saxena, S. K. (2022). An Overview of Indian Biomedical Research on the Chikungunya Virus with Particular Reference to Its Vaccine, an Unmet Medical Need. Pathogens, 11(6), 1102.
- Hunter’s Tropical Medicine and Emerging Infectious Diseases (11th Edition) by Strickland G.T. (Editor) published in 2020 by Elsevier
Also Search As
Also Search As
Specific terms related to the homeopathic remedies mentioned in the article:
- Eupatorium perfoliatum for Chikungunya
- Bryonia alba for Chikungunya
- Rhus toxicodendron for Chikungunya
Broader search terms:
- Mosquito-borne illness homeopathic treatment
- Viral fever homeopathic remedies
- Joint pain homeopathic medicine
1. Search Engines (Google, Bing, etc.):
Specific Keywords:
People can search using the terms you’ve already listed, like "Chikungunya homeopathic remedies" or "homeopathic treatment for Chikungunya joint pain."
Broader Keywords:
They can also use more general terms like "homeopathy for viral infections" or "natural remedies for Chikungunya."
2. Homeopathic Websites and Forums:
Dedicated Websites:
Many websites focus on homeopathic medicine. These sites often have articles, blogs, or resource sections where your article could be featured.
Forums and Communities:
Online communities of homeopathic practitioners and patients are great places for sharing and finding information.
3. Social Media:
Sharing on Relevant Groups:
If the article is published online, share it on social media platforms like Facebook, Twitter, or LinkedIn. Target groups and pages that are focused on homeopathy, natural health, or even Chikungunya awareness.
4. Professional Associations:
Homeopathic Organizations:
Contact national or regional homeopathic associations. They might share your article in their newsletters, on their websites, or through their social media channels.
5. Direct Links:
Your Website/Blog:
If you have a personal platform, publish the article there and share the link directly.
Additional Tips:
- Title Optimization: Make sure the article’s title includes relevant keywords to improve its visibility in search results.
- Meta Description: Write a concise and informative meta description that summarizes the article’s content and entices people to click.
- Hashtags: Use relevant hashtags when sharing on social media to increase its reach.
1. Search Engines (Google, Bing, DuckDuckGo):
Direct Keyword Searches:
Use the most relevant terms from the article, such as:
- "Chikungunya homeopathic remedies"
- "Homeopathic treatment for Chikungunya"
- "Homeopathic medicine for Chikungunya fever"
- "Chikungunya homeopathy"
- If the article has a unique title, try searching for the exact title.
Related Searches:
Expand your search with related terms:
- "Natural remedies for Chikungunya"
- "Homeopathic remedies for joint pain"
- "Homeopathic treatment for viral fever"
Author Name:
If you know the author of the article, search for their name along with "Chikungunya homeopathy."
2. Homeopathic Websites and Databases:
- National Center for Homeopathy (NCH): Check the NCH website for publications or articles.
- Homeopathic Educational Services (HES): Search their online resources.
- Homeopathy World Community: Look for articles in their online library.
- Other Reputable Homeopathic Websites: Several websites specialize in homeopathy information and may have published your article.
3. Social Media Platforms:
- Facebook: Search in homeopathy groups or pages.
- Twitter: Use hashtags like #homeopathy, #chikungunya, or #naturalremedies.
- LinkedIn: If the article has a professional focus, it might be shared on LinkedIn groups related to homeopathy or healthcare.
4. Academic Databases (If applicable):
- If the article was published in a peer-reviewed journal, search databases like PubMed or Google Scholar.
5. Direct Links and Recommendations:
- If you know the website or platform where the article is published, go directly to it.
- Ask friends, colleagues, or online communities interested in homeopathy if they’ve come across the article and for the link.
Important Considerations:
- Publication Location: Where the article was published will heavily influence how you search for it.
- SEO: The website or platform’s search engine optimization (SEO) practices will affect how easily the article is found on search engines.
- Promotion: If the author or publisher actively promotes the article, it will be easier to find through various channels.
Frequently Asked Questions (FAQ)
What is Chikungunya?
Chikungunya is a viral disease transmitted to humans through the bite of infected Aedes mosquitoes. It’s characterized by sudden high fever, severe joint pain, headache, muscle pain, joint swelling, and rash.
How is Chikungunya transmitted?
The virus is spread by the bite of an infected Aedes aegypti or Aedes albopictus mosquito. It’s not transmitted directly from person to person.
How can I prevent Chikungunya?
- Protect yourself from mosquito bites by using insect repellent, wearing long sleeves and pants, and using bed nets.
- Eliminate mosquito breeding sites around your home by removing standing water.
Is there a treatment for Chikungunya?
There is no specific antiviral treatment. Management focuses on relieving symptoms with pain relievers, rest, and fluids.
Can homeopathy prevent Chikungunya?
While there’s no specific preventative remedy, homeopathy aims to strengthen the immune system and enhance overall well-being, potentially making individuals less susceptible to infections.
What are the symptoms of Chikungunya?
Symptoms of Chikungunya
- High fever (often over 102°F)
- Severe joint pain (often symmetrical, affecting multiple joints)
- Joint swelling
- Muscle pain
- Headache
- Rash
- Fatigue
- Nausea
What is the homeopathic approach to Chikungunya?
Homeopathy views Chikungunya as an imbalance in the body’s vital force. Treatment aims to stimulate the body’s natural healing abilities, addressing both the physical symptoms and the underlying susceptibility.
Can homeopathy help with Chikungunya symptoms?
Yes, homeopathic remedies can help manage the fever, joint pain, rash, and fatigue associated with Chikungunya. Remedies like Eupatorium Perfoliatum, Bryonia Alba, and Rhus Toxicodendron are often considered for their potential to relieve specific symptoms.
Are there specific homeopathic remedies for Chikungunya?
Yes, several remedies may be helpful, depending on the individual’s unique symptom presentation. A qualified homeopath will conduct a detailed consultation to select the most suitable remedy for each person.
- Eupatorium Perfoliatum: Known for its effectiveness in relieving intense, bone-breaking pain and fever.
- Bryonia Alba: Often used for dry, burning fever, headache, and joint pain aggravated by movement.
- Gelsemium Sempervirens: May be helpful for symptoms like fever with chills, weakness, and muscle aches.
- Rhus Toxicodendron: Commonly used for joint pain and stiffness that improves with movement, and restlessness.
- Arsenicum Album: Can be beneficial for burning pains, restlessness, and anxiety associated with the illness.
- Aconitum Napellus: Often used in the early stages of the illness for sudden onset of high fever and anxiety.
How does homeopathic treatment for Chikungunya differ from conventional medicine?
Conventional medicine primarily focuses on symptom relief using pain medications and anti-inflammatory drugs. Homeopathy aims to address the root cause of the illness and strengthen the body’s overall defenses, potentially reducing the duration and severity of symptoms.
