Cluster Headache
Definition
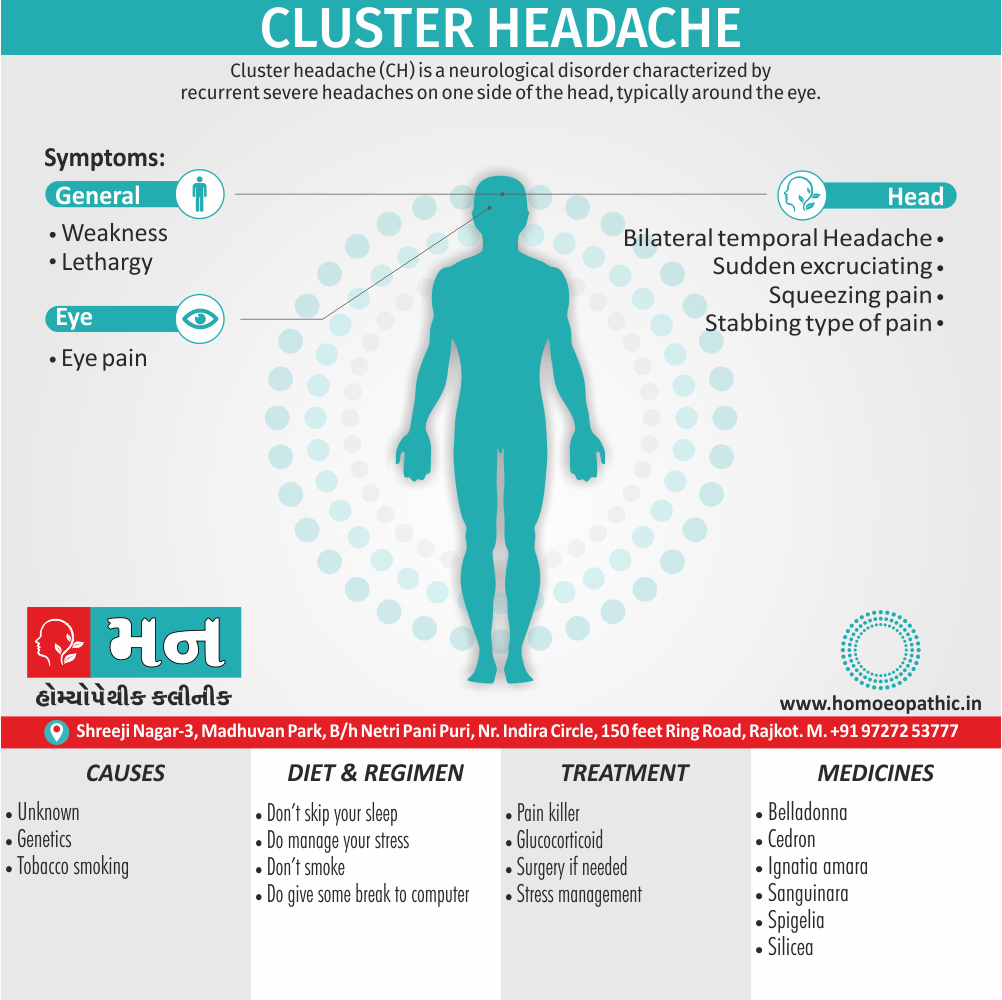
Cluster headache (CH) is a neurological disorder characterized by recurrent severe headaches on one side of the head, typically around the eye. There is often accompanying eye watering, nasal congestion, or swelling around the eye on the affected side. These symptoms typically last 15 minutes to 3 hours.[1]
Cluster headaches have a few lesser-known synonyms you might encounter:
- Paroxysmal nocturnal cephalgia: This term emphasizes the sudden, severe nature of the attacks and their tendency to occur at night.
- Histamine headache: This name refers to the possible role of histamine, a chemical in the body, in triggering cluster headaches.
- Horton headache (or Horton syndrome): These terms are named after Dr. Dudley Joy Horton, who first described cluster headaches in detail.
- Cranial autonomic syndrome 3 (CAS 3): This is a more technical term used in the medical field to classify cluster headaches.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Cluster Headache
Cluster Headache are a primary headache disorder Of Trigeminal autonomic cephalgia (in other words, TAC) type.
The condition usually first occurs between 20 and 40 years of age. Men are affected about four times more often than women. Cluster headaches are named for the occurrence of groups of headache attacks (e.g. clusters). They have also been referred to as "suicide headaches".
Epidemiology
Epidemiology of Cluster Headache:
The epidemiology of cluster headache (CH) in India is not as well-established as in some Western countries, but several studies have provided valuable insights:
Neuroepidemiology study of headache in the region of Jammu of north Indian population: A cross-sectional study (2022):
- This study found a prevalence rate of 53.84% for headaches overall, but did not specifically report on the prevalence of CH. [10]
Prevalence of Primary Headache Disorders in a Population of Semi-Urbanized Area of South India: A Cross-Sectional Study (Year not explicitly mentioned in the reference):
- This study found a prevalence of 14.04% for CH in the studied population. [11]
Cluster Headache – Incidence and Its Association with Age, Gender and Triggers (2021):
- This study focused on the incidence of CH in a hospital setting and found it to be 1% in the studied population. [12]
The burden attributable to headache disorders in India: estimates from a community-based study in Karnataka State (2015):
- This study focused on the broader burden of headache disorders but did not specifically report on the prevalence of CH. [13]
(PDF) EHMTI-0333. The prevalence and burden of migraine in India: results of a population-based study in Karnataka state (Year not explicitly mentioned in the reference):
- This study focused on migraine and did not specifically report on the prevalence of CH. [14]
These studies suggest that while CH is not as common as other headache disorders in India, it still affects a significant number of people. Further research is needed to establish a more precise estimate of the prevalence and to better understand the factors that contribute to CH in the Indian population.
Causes
Causes
The cause of cluster headache is unknown.
Nerves
- Two nerves are thought to play an important role in CH: the trigeminal nerve and the facial nerve.
Genetics
- Cluster headache may run in some families in an autosomal dominants inheritance pattern.
- People with a first degree relative with the condition are about 14–48 times more likely to develop it themselves, and around 8 to 10% of persons with CH have a positive family history.
- Several studies have found a higher number of relatives affected among female. Others have suggested these observations may be due to lower numbers of females in these studies.
- Possible genetic factors warrant further research, current evidence for genetic inheritance limit.
Tobacco smoking
- About 65% of persons with CH are, or have tobacco smokers.
- People with CH may predispose to certain traits, including smoking or other lifestyle habits.
Hypothalamus
- A review suggests that the suprachiasmatic nucleus of the hypothalamus, which is the major biological clock in the human body, may involve in cluster headaches, because CH occurs with diurnal and seasonal rhythmicity.
- Positron emission tomography (in other words, PET) scans indicate the brain areas which are activated during attack only, compared to pain free periods.
- These pictures show brain areas that are active during pain in yellow/orange color (called "pain matrix").
- The area in the center (in all three views) specifically activate during CH only.
- The bottom row voxel-based morphometry (in other words, VBM) shows structural brain differences between individuals with and without CH; only a portion of the hypothalamus is different.
Types
Types
There are two types of cluster headaches: episodic and chronic.
- Episodic cluster headaches occur regularly between one week and one year, followed by a headache-free period of one month or more.
- Chronic cluster headaches occur regularly for longer than one year, followed by a headache-free period that lasts for less than one month. (6)
Risk Factors
Risk factor
- Exposure to tobacco smock
- Positive family History
Exciting or triggering factors i.e.:
- Nitroglycerine
- Alcohol
- Histamine
Pathogenesis
Pathogenesis of Cluster Headache:
The exact pathogenesis of cluster headache (CH) remains elusive, but current understanding points towards a complex interplay of several factors:
Hypothalamic Involvement:
- The hypothalamus, a brain region crucial for regulating circadian rhythms, appears to play a central role. The strict periodicity and circannual rhythm of CH attacks suggest a dysregulation of the hypothalamic-pituitary-adrenal axis.
Trigeminovascular Activation:
- The trigeminal nerve, responsible for facial sensation, becomes activated in CH. This leads to the release of inflammatory neuropeptides, such as calcitonin gene-related peptide (CGRP) and pituitary adenylate cyclase-activating polypeptide (PACAP), which cause vasodilation and neurogenic inflammation.
Autonomic Dysfunction:
- CH is associated with prominent autonomic symptoms, such as lacrimation, rhinorrhea, and ptosis. This suggests an imbalance in the parasympathetic and sympathetic nervous systems.
Genetic Predisposition:
- Although no single gene has been identified, familial clustering suggests a genetic component to CH susceptibility.
Environmental Triggers:
- Certain triggers, like alcohol, nicotine, and nitroglycerin, can provoke attacks in susceptible individuals. This suggests an interaction between genetic predisposition and environmental factors.
Imaging Studies:
- Functional imaging studies have shown activation of the posterior hypothalamus during CH attacks, further supporting the role of the hypothalamus.
Novel Therapeutic Targets:
- Recent research has focused on developing new therapies targeting CGRP and PACAP, highlighting their importance in CH pathophysiology.
It emphasizing the complex interplay of hypothalamic dysregulation, trigeminovascular activation, autonomic dysfunction, genetic predisposition, and environmental triggers. [15]
Pathophysiology
Pathophysiology
- The pathophysiology of cluster headache is not fully understood. Current theories implicate mechanisms such as vascular dilation, trigeminal nerve stimulation, and circadian effects.
- Histamine release, an increase in mast cells, genetic factors, and autonomic nervous system activation may also contribute.
- Acute cluster headache has been shown to involve activation of the posterior hypothalamic gray matter, and is inherited as an autosomal dominant condition in about 5% of patients.
- Having a first-degree relative with cluster headache increases the risk 14- to 39-fold.
- One study showed an association between cluster headache and the HCRTR2 gene.
- Disturbed circadian rhythms have been suggested as a possible contributor because headaches often begin during sleep. (5)
Clinical Features
Clinical Features of Cluster Headache:
The clinical features of cluster headache (CH) are characteristic and often striking:
Severe Unilateral Pain:
- Excruciating pain, often described as sharp, stabbing, or burning, localized around one eye or temple.
Short Duration Attacks:
- Attacks typically last 15-180 minutes but can be shorter or longer.
Frequency:
- Attacks occur in clusters, often multiple times per day, for weeks or months, followed by remission periods.
Circadian/Circannual Rhythmicity:
- Attacks often occur at the same time each day and may follow seasonal patterns.
Ipsilateral Autonomic Symptoms:
- Cranial: Lacrimation, conjunctival injection, nasal congestion or rhinorrhea, forehead and facial sweating, miosis, ptosis, eyelid edema
- Extracranial: Partial Horner syndrome (miosis and ptosis)
Agitation and Restlessness:
- Patients are often restless and unable to lie still during attacks.
Triggers:
- Attacks may be triggered by alcohol, nitroglycerin, or histamine.
Premonitory Symptoms:
- Some patients experience premonitory symptoms, such as mild discomfort or aura, hours before an attack.
Pain Characteristics:
- The pain is usually not aggravated by routine physical activity.
Sex Distribution:
- CH is more common in men than women.
Age of Onset:
- Typically occurs between 20 and 50 years of age.
A detailed account of the clinical features of CH, emphasizing its unique combination of severe unilateral pain, short duration attacks, cluster periods, rhythmicity, and accompanying autonomic symptoms. This distinct clinical presentation often allows for a clear diagnosis, facilitating appropriate management and treatment. [15]
Sign & Symptoms
Sign & Symptoms of Cluster Headache
Nature of Cluster Headache
- Onset: Sudden, rapid
- Duration: 50- 180 min
- Character: Recurrent, unilateral
- Location: Around or above or behind eye also temporal region
- Pain: e.g. Stabbing, Excruciating, Burning, Drilling, Squeezing type
- A core feature of cluster headache is periodicity. At least one of the daily attacks of pain recurs at about the same hour each day for the duration of a cluster bout.
- The typical cluster headache patient has daily bouts of one to two attacks of relatively short-duration unilateral pain for 8 to 10 weeks a year; this is usually followed by a pain-free interval that averages a little less than 1 year.
- Cluster headache is characterized as chronic when there is less than 1 month of sustained remission without treatment. Patients are generally perfectly well between episodes.
- Onset is nocturnal in about 50% of patients, and men are affected three times more often than women.
- Patients with cluster headache tend to move about during attacks, pacing, rocking, or rubbing their head for relief; some may even become aggressive during attacks.
- This is in sharp contrast to patients with migraine, who prefer to remain motionless during attacks.[1]
Cluster headache attack is accompanied by at least one of the following autonomic symptoms:
- Drooping eyelid
- Pupil constriction
- Redness of the conjunctiva
- Tearing
- Runny nose and less commonly
- Facial blushing ,swelling, or sweating, typically appearing on the same side of the head as the pain.
- Similar to a migraine, sensitivity to light (photophobia) or noise (phonophobia) may occur during a CH. Nausea is a rare symptom although it has been reported.
- Restlessness (for example, pacing or rocking back and forth) may occur. Secondary effects may include the inability to organize thoughts and plans, physical exhaustion, confusion, agitation, aggressiveness, depression, and anxiety.
- People with CH may dread facing another headache and adjust their physical or social activities around a possible future occurrence. Likewise, they may seek assistance to accomplish what would otherwise be normal tasks. T
- hey may hesitate to make plans because of the regularity, or conversely, the unpredictability of the pain schedule.
- These factors can lead to generalized anxiety disorder, panic disorder, serious depressive disorder social withdrawal and isolation.
- Cluster headaches have been recently associated with obstructive sleep apnea.
Recurrence
- Cluster headaches may occasionally be referred to as "alarm clock headache" because of the regularity of their recurrence.
- CH attacks often awaken individuals from sleep; attacks typically striking at a precise time of day each morning or night.
- The recurrence of headache cluster grouping may occur more often around solstices, or seasonal changes, sometimes showing circannual periodicity. Conversely, attack frequency may be highly unpredictable, showing no periodicity at all. These observations have prompted researchers to speculate an involvement or dysfunction of the hypothalamus.
- The hypothalamus controls the body’s "biological clock" and circadian rhythm. In episodic cluster headache, attacks occur once or more daily, often at the same time each day for a period of several weeks, followed by a headache-free period lasting weeks, months, or years.
- Approximately 10–15% of cluster headaches are chronic, with multiple headaches occurring every day for years, sometimes without any remission.
- The frequency, severity, and duration of headache attacks experienced by people during these cycles varies between individuals and does not demonstrate complete remission of the episodic form. The condition may change unpredictably from chronic to episodic and from episodic to chronic. [1]
Clinical Examination
Clinical examination of Cluster Headache
- Examination findings in cluster headache are usually autonomic related; suggesting parasympathetic hyperactivity and sympathetic impairment.
- Exam findings may include ptosis, lacrimation, conjunctival injection, miosis, nasal congestion, rhinorrhea, neck stiffness and photophobia. (7)
Diagnosis
Diagnosis of Cluster Headache
- Cluster-like head pain may be diagnosed as secondary headache rather than cluster headache.
- A detailed oral history aids practitioner in correct differential diagnosis, as there are no confirmatory tests for CH.
- A headache diary can be useful in tracking when and where pain occurs, how severe it is, and how long the pain lasts.
- A record of coping strategies used may help distinguish between headache type; data on frequency, severity and duration of headache attacks are a necessary tool for initial and correct differential diagnosis in headache conditions. [1]
In accordance with the International Headache Society (IHS) diagnostic criteria,
- Cluster headaches occurring in two or more cluster periods, lasting from 7 to 365 days with a pain-free remission of one month or longer between the headache attacks may be classified as episodic.
- If headache attacks occur for more than a year without pain-free remission of at least one month, the condition is classified as chronic.
- Chronic CH both occurs and recurs without any remission periods between cycles; there may be variation in cycles, meaning the frequency and severity of attacks may change without predictability for a period of time.
- The frequency, severity, and duration of headache attacks experienced by people during these cycles varies between individuals and does not demonstrate complete remission of the episodic form. The condition may change unpredictably from chronic to episodic and from episodic to chronic. [1]
Differential Diagnosis
Differential Diagnosis of Cluster Headache
Complications
Complications of Cluster Head:
While cluster headache (CH) itself is not typically associated with serious or life-threatening complications, it can lead to significant morbidity and negatively impact a patient’s quality of life.
Potential Complications and Consequences:
Suicide Risk:
- The intense pain and debilitating nature of CH can lead to depression and, in severe cases, suicidal ideation or attempts. This is a serious concern and requires prompt evaluation and intervention.
Medication Overuse Headache (MOH):
- Frequent use of acute medications (e.g., opioids, triptans) to manage CH attacks can paradoxically lead to a rebound headache, exacerbating the problem.
Sleep Disturbance:
- CH attacks often disrupt sleep, leading to chronic sleep deprivation, fatigue, and impaired cognitive function.
Anxiety and Mood Disorders:
- The unpredictable and recurrent nature of CH can trigger anxiety and mood disturbances, further impacting quality of life.
Social and Occupational Impairment:
- The frequent and intense attacks can significantly disrupt work, social activities, and personal relationships.
Substance Abuse:
- Some individuals may turn to alcohol or other substances to cope with the pain and distress of CH, leading to potential addiction issues.
Horner Syndrome:
- While not a direct complication, a partial Horner syndrome (miosis and ptosis) is a common associated feature of CH.
Rare Complications:
- In rare cases, CH has been associated with more severe complications, such as stroke or intracranial hemorrhage, though the causal link is not well-established. [15]
Timely diagnosis, appropriate management, and addressing psychosocial factors are crucial for mitigating the negative impact of this debilitating condition.
Investigations
Investigation of Cluster Headache
- Investigation studies include neuroimaging, cerebrospinal fluid (CSF) examination, and blood tests, which are selected depending on the patient’s history and findings.
- For most patients, the diagnostic test of choice is a magnetic resonance imaging (MRI) brain scan. (8)
Treatment
Treatment of Cluster Headache
- Cluster headache attacks peak rapidly, and thus a treatment with quick onset require.
- Many patients with acute cluster headache respond very well to oxygen inhalation. This should give as 100% oxygen at 10–12 L/min for 15–20 min. It appears that high flow and high oxygen content are important.
- Sumatriptan 6 mg SC is rapid in onset and will usually shorten an attack to 10–15 min; there is no evidence of tachyphylaxis.
- Sumatriptan (20 mg) and zolmitriptan (5 mg) nasal sprays are both effective in acute cluster headache, offering a useful option for patients who may not wish to self-inject daily.
- Oral sumatriptan is not effective for prevention or for acute treatment of cluster headache.[1]
- The recommended first-line preventive therapy is verapamil, a calcium channel blocker. Verapamil was previously underused in people with cluster headache.
- There is little evidence to support a long-term benefit from glucocorticoids, but they may use until other medications take effect as they appear to be effective at three days.
- Nerve stimulators may an option in the small number of people who do not improve with medications. Two procedures, deep vein stimulation or occipital nerve stimulation may useful; early experience shows a benefit in about 60% of cases.
Prevention
Prevention of Cluster Headache
- Stick to a regular sleep schedule. Cluster periods can begin when there are changes in your normal sleep schedule. During a cluster period, follow your usual sleep routine.
- Avoid alcohol. Alcohol consumption, including beer and wine, can quickly trigger a headache during a cluster period. (9)
Homeopathic Treatment
Homeopathic Treatment of Cluster Headache
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Cluster headache
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicine:
Cedron: Best Homeopathic medicine for Cluster Headache at precisely same hour
- Cedron is considered the top natural Homeopathic medicine that will provide immediate relief from Cluster Headaches.
- Cedron is of great help when the main symptom is severe pain around the eye at a particular hour.
- Periodicity in occurrence of periorbital pain is essentially marked. This pain may radiate into the ear.
- In other persons, the pain around the eye may radiate to the temples or back of head.
- Watering from eyes with burning may also present itself with eye pain.
- Night aggravation of pain is also noted. Although the pain may appear on any side, the pain over the left side of eye is felt more often for prescribing Homeopathic remedy Cedron.
Belladona: Homeopathic medicine for Cluster Headache with redness or swelling of eyes
- Belladona is the ideal natural Homeopathic medicine for Cluster Headache with redness or swelling of eyes and flushing of face.
- The characteristic feature for using this Homeopathic remedy is deep pain in the eyes, mostly throbbing or shooting in nature, with congestion and redness of eyes.
- The eyes also show protrusion.
- Photophobia i.e. intolerance to light or worsening of pain from light may also be noted.
- In most cases, lying down worsens the pain and tight bandage or pressure seems to provide relief.
- The sudden onset of a violent headache is also a marked feature.
- The attacks appear suddenly and with intensity and leave with the same suddenness.
Spigelia: Homeopathic medicine for left-side Cluster Headache
- Spigelia is a natural Homeopathic medicine which is very beneficial in treating the left-side Cluster Headache.
- Its use recommend when there is a severe violent pain around the eye and in the eye socket specifically on the left side. The eyeballs too appear large.
- The pain can be of varying nature like digging, boring, shooting, violent, throbbing or stitching pain, with a feeling of needles pricking in the eye on the left side.
- The main worsening factor given by a patient for using Homeopathic remedy Spigelia is pain in eye on moving or turning the eye.
- A few persons may also describe noise or touching the eye as the most aggravating factors.
- Rest in most cases seems to relieve the pain. Along with pain, redness of eyes with sensitivity to light and dropping of eyes also show their presence.
- Another marked feature for using Spigelia is occurrence of pain around the left eye in morning either on rising or while lying in bed.
- A characteristic relief from pain by washing with cold water is a peculiar symptom guiding the use of Homeopathic medicine Spigelia.
Sanguinaria Can: Right-side Cluster Headache
- For treating right-side Cluster Headache, natural Homeopathic medicine Sanguinaria Can is the ideal remedy.
- The use of Homeopathic medicine Sanguinaria Can consider in all those cases of Cluster Headache where the pain settles over or around the right eye.
- A bursting sensation with a feeling as if the eyes will be pressed out is very marked. Periodicity of pain note mostly with beginning of pain in morning and continuing till evening.
- The most aggravating factors in pain to kept in mind where Sanguinaria Can applicable are motion and light. And sleep and lying down still are the soothing factors.
- Characteristic relief from pain may also brought about by walking in open air for some patients needing Sanguinaria Can.
- Along with pain over right eye, there is a profuse watering of eyes. The eyes also very congested, and red with burning sensations.
- The face, especially cheeks, shows flushing. In a few persons, nasal congestion is a prominent feature.
Spigelia: Cluster Headache on left-side
- Spigelia is a top natural Homeopathic medicine for left-side cluster headache.
- In most cases, the person has a need to close the eye to get relief.
- Has marked elective affinity for the eye, heart, and nervous system.
- Neuralgia of the fifth nerve is very prominent in its effects. especially adapted to anaemic, debilitated, rheumatic, and scrofulous subjects. Stabbing pains. Heart affections and neuralgia.
- Very sensitive to touch, parts feel chilly, send shudder through frame.
- A remedy for stitches due to the presence of worms.
- Child refers to the navel as the most painful part.
- Semi-lateral, involving left eye; pain violent, throbbing; worse, making a false step. Pain as if a band around head.
Ignatia Amara – Effective for Cluster Headache With Stabbing Pain Deep In The Eyes
- Ignatia Amara a beneficial medicine use to treat a cluster headache when the person experiences stabbing pain deep in the eyes.
- A sensation of pressure in the eyes may also be felt. This attend with a sensation as if the eyes would fall out.
- Along with this, redness, flowing of tearing and burning in the eyes may also feel.
- The person needing Ignatia Amara suffers from a periodical headache that can occur every week, fortnight or every month.[3]
Diet & Regimen
Diet & Regimen of Cluster Headache
Regimen an diet for Cluster Headache
Diet:
- Identify and Avoid Triggers: This is crucial. Common triggers include alcohol, especially red wine, and smoked meats. Keeping a food diary can help pinpoint personal triggers.
- Anti-inflammatory Foods: A diet rich in fruits, vegetables, and whole grains may help reduce inflammation, which could play a role in cluster headaches.
- Magnesium-Rich Foods: Some studies suggest magnesium may be beneficial. Include foods like spinach, almonds, and avocados.
- Hydration: Staying well-hydrated is important for overall health and may help prevent headaches.
Regimen:
- Regular Sleep Schedule: Maintaining a consistent sleep pattern is vital, as even small changes can trigger attacks.
- Stress Management: Techniques like meditation, yoga, or deep breathing exercises can help manage stress, a potential trigger.
- Oxygen Therapy: Inhaling high-flow oxygen at the onset of an attack can be effective for some people.
- Medications:
- Acute Treatment: Triptans, ergotamine, and local anesthetics (like lidocaine) may help stop an attack in progress.
- Preventive Treatment: Verapamil, corticosteroids, lithium, and other medications may reduce the frequency and severity of attacks.
- Avoid High Altitudes: Lower oxygen levels at high altitudes can trigger attacks in some individuals.
Do’s and Don'ts
The Do’s and Don’ts of Cluster Headache:
The management of cluster headache (CH) involves both acute treatment to relieve attacks and preventive measures to reduce their frequency and severity. Certain lifestyle adjustments can also play a role in managing this condition.
Do’s:
Seek Medical Attention:
- If you experience symptoms suggestive of CH, consult a healthcare professional for accurate diagnosis and treatment planning.
Adhere to Treatment Plans:
- Follow your doctor’s recommendations for both acute and preventive therapies, as consistent treatment is essential for managing CH.
Identify and Avoid Triggers:
- Once diagnosed, try to identify potential triggers, such as alcohol, nicotine, or certain foods, and avoid them during cluster periods.
Maintain a Regular Sleep Schedule:
- Stick to a consistent sleep routine, as disruptions in sleep patterns can trigger attacks.
Consider Relaxation Techniques:
- Stress reduction methods like yoga, meditation, or deep breathing exercises may help manage stress and reduce attack frequency.
Don’ts:
Self-Medicate:
- Avoid self-medicating with over-the-counter pain relievers, as they are often ineffective for CH and can lead to medication overuse headache.
Ignore Warning Signs:
- If you experience premonitory symptoms, don’t delay treatment. Early intervention can sometimes abort or lessen the severity of an attack.
Consume Alcohol or Nitroglycerin:
- These are known triggers for CH attacks and should be strictly avoided during cluster periods.
Smoke:
- Smoking can exacerbate CH and should be avoided altogether.
Give Up:
- CH can be challenging to manage, but don’t lose hope. With proper treatment and lifestyle adjustments, many individuals experience significant improvement. [15]
Terminology
Terminology
Cluster Headache (CH):
- A neurological disorder characterized by recurrent, severe headaches on one side of the head, usually around the eye, accompanied by autonomic symptoms.
Neurological Disorder:
- A condition that affects the nervous system, including the brain, spinal cord, and nerves.
Paroxysmal Nocturnal Cephalgia:
- An older term for cluster headache, emphasizing its sudden onset, often at night.
Histamine Headache:
- An outdated term for cluster headache, suggesting a potential role of histamine in its mechanism.
Horton Headache (or Horton Syndrome):
- Eponymous terms for cluster headache, named after the physician who first described the condition.
Cranial Autonomic Syndrome 3 (CAS 3):
- A classification of cluster headache within a broader group of disorders characterized by cranial autonomic symptoms.
Trigeminal Autonomic Cephalgia (TAC):
- A family of headache disorders, including cluster headache, characterized by activation of the trigeminal nerve and associated autonomic symptoms.
Epidemiology:
- The study of the distribution and determinants of health-related states or events in specified populations.
Prevalence:
- The proportion of individuals in a population having a disease or characteristic at a specific time.
Incidence:
- The number of new cases of a disease or condition in a population over a specific period.
Pathogenesis:
- The biological mechanism(s) that lead to the development of a disease or condition.
Hypothalamus:
- A region of the brain that controls many bodily functions, including the sleep-wake cycle and hormone release.
Trigeminal Nerve:
- The fifth cranial nerve, responsible for sensation in the face and motor functions like biting and chewing.
Autonomic Nervous System:
- The part of the nervous system that controls involuntary bodily functions like heart rate, digestion, and pupil dilation.
Circadian Rhythm:
- A natural, internal process that regulates the sleep-wake cycle and repeats roughly every 24 hours.
Pathophysiology:
- The disordered physiological processes associated with disease or injury.
Miosis:
- Constriction of the pupil of the eye.
Ptosis:
- Drooping of the upper eyelid.
Horner Syndrome:
- A combination of symptoms caused by disruption of a nerve pathway from the brain to the face and eye on one side of the body.
Photophobia:
- Sensitivity to light.
Phonophobia:
- Sensitivity to sound.
Magnetic Resonance Imaging (MRI):
- A medical imaging technique that uses a magnetic field and computer-generated radio waves to create detailed images of the organs and tissues in your body.
Homeopathy:
- A system of alternative medicine based on the principle of "like cures like," using highly diluted substances to trigger the body’s natural healing processes.
Miasmatic Tendency:
- In homeopathy, a predisposition to certain types of diseases based on inherited or acquired weaknesses.
Cluster headaches are debilitating attacks of severe pain around one eye, often accompanied by autonomic symptoms. Homeopathic treatment aims to address the root cause of these headaches and provide relief through individualized remedies tailored to the patient’s unique symptoms and constitution. Learn more about the potential benefits of homeopathy for cluster headache, including commonly used remedies and their indications.
- Cluster headache, homeopathy, homeopathic remedies, natural treatment, headache relief, Spigelia Anthelmia, Belladonna, Iris Versicolor, Gelsemium.
References
References use for Article Cluster Headache
- Harrison-s_Principles_of_Internal_Medicine-_19th_Edition-_2_Volume_Set
- https://en.wikipedia.org/wiki/Cluster_headache
- https://www.drhomeo.com/headache/top-homeopathic-remedies-for-cluster-headaches/
- https://www.sapnamed.com/blog/what-foods-and-drinks-help-headaches/
- https://www.aafp.org/pubs/afp/issues/2013/0715/p122.html
- https://www.healthline.com/health/cluster-headache#types
- https://www.wikidoc.org/index.php/Cluster_headache_physical_examination
- https://www.google.com/search?q=investigation++of+cluster+headache
- https://www.google.com/search?q=prevention+++of+cluster+headach
- Neuroepidemiology study of headache in the region of Jammu of north Indian population: A cross-sectional study (2022)
- Prevalence of Primary Headache Disorders in a Population of Semi-Urbanized Area of South India: A Cross-Sectional Study (Year not explicitly mentioned in the reference)
- Cluster Headache – Incidence and Its Association with Age, Gender and Triggers (2021)
- The burden attributable to headache disorders in India: estimates from a community-based study in Karnataka State (2015)
- (PDF) EHMTI-0333. The prevalence and burden of migraine in India: results of a population-based study in Karnataka state (Year not explicitly mentioned in the reference)
- Book: Headache Disorders, 4th Edition, Editors: James Olesen, Peter J. Goadsby, Paul R. Martin, Year: 2022, Publisher: Oxford University Press
Also Search As
Also Search As
Online Search Engines:
- Google Scholar: This is a great resource for finding scholarly articles and research studies on cluster headache. Use keywords like "cluster headache," "pathogenesis," "treatment," or "epidemiology" to refine your search.
- PubMed: This is another excellent database for finding medical literature on cluster headache. You can use similar keywords as above to find relevant articles.
- Google: A simple Google search using keywords like "cluster headache" or "cluster headache articles" will also yield a variety of results, including news articles, blog posts, and patient resources.
Medical Websites and Organizations:
- Mayo Clinic: This website provides comprehensive information on cluster headache, including symptoms, causes, diagnosis, and treatment options.
- Cleveland Clinic: This website also offers detailed information on cluster headache, with a focus on patient education and resources.
- American Migraine Foundation: While primarily focused on migraines, this website also has information on other headache disorders, including cluster headache.
Other Resources:
- Medical Libraries: If you have access to a medical library, you can ask a librarian for help finding articles on cluster headache.
- Support Groups: Online or in-person support groups for people with cluster headache can be a valuable resource for finding information and connecting with others who understand the condition.
Tips for Effective Searching:
- Use specific keywords: Instead of just searching for "cluster headache," try adding more specific terms like "cluster headache treatment guidelines" or "cluster headache prevalence in India" to narrow down your results.
- Use quotation marks: Enclosing your search terms in quotation marks (e.g., "cluster headache") will ensure that the exact phrase is searched, rather than individual words.
- Use Boolean operators: Words like "AND," "OR," and "NOT" can help you combine search terms to find more relevant results.
By using these strategies, you can find a wealth of information on cluster headache to learn more about this complex condition.
Online Resources:
- Search Engines: Use general search engines like Google, Bing, or DuckDuckGo, with search terms like "cluster headache," "cluster headache research," or "cluster headache treatment." To focus on scholarly articles, use Google Scholar or Semantic Scholar.
- Medical Databases: PubMed, MEDLINE, and Embase are valuable databases for finding medical research articles. You can use keywords like "cluster headache" and filters for publication dates or specific journals to narrow your search.
- Specialized Websites: Websites like the Mayo Clinic, Cleveland Clinic, American Migraine Foundation, and the National Headache Foundation offer information and resources on cluster headache.
Other Methods:
- Libraries: University or medical libraries often have access to academic journals and databases not available to the general public.
- Citation Indexes: If you find a relevant article, check its reference list for other potentially useful sources.
- Social Media: Following researchers and organizations focused on headache disorders on Twitter or LinkedIn can lead you to new publications.
Tips for Effective Searching:
- Use specific keywords: Instead of just searching for "cluster headache," try "cluster headache treatment guidelines" or "cluster headache prevalence."
- Combine keywords with Boolean operators: Use "AND," "OR," and "NOT" to refine your search (e.g., "cluster headache" AND "oxygen therapy").
- Use filters: Most databases and search engines allow filtering by date, article type, and other criteria.
- Check the reference list: Once you find a relevant article, look at its references for other potential sources.
By using these methods and strategies, you can find a wealth of information on cluster headache, ranging from the latest research findings to patient resources and support groups.
Frequently Asked Questions (FAQ)
What is a cluster headache?
Definition:
Cluster headache is a rare but extremely painful type of headache that occurs in cyclical patterns or clusters. It is characterized by severe pain on one side of the head, usually around the eye, and often accompanied by other symptoms like tearing, nasal congestion, and restlessness.
How long do cluster headache attacks last?
Individual cluster headache attacks typically last 15 minutes to 3 hours. However, the frequency and duration of clusters can vary from person to person. Some people may have multiple attacks per day for weeks or months, followed by periods of remission.
What causes cluster headaches?
The exact cause of cluster headaches is unknown, but it is believed to be related to the hypothalamus, a part of the brain that controls our biological clock. Activation of the trigeminal nerve and changes in brain chemicals like serotonin may also play a role.
What are the triggers for cluster headaches?
Common triggers for cluster headaches include alcohol, nicotine, strong smells, and changes in sleep patterns.
How are cluster headaches treated?
Cluster headache treatment aims to reduce the severity and frequency of attacks. This can include oxygen therapy, triptans, corticosteroids, and preventive medications like verapamil or lithium. In some cases, nerve blocks or neuromodulation may be recommended.
How can homeopathy help with cluster headaches?
Homeopathy aims to address the root cause of cluster headaches and provide relief by stimulating the body’s natural healing abilities. It considers the individual’s unique symptoms, triggers, and overall constitution to select the most appropriate remedies.
What homeopathic remedies are commonly used for cluster headaches?
Some commonly used homeopathic remedies for cluster headaches include:
Spigelia Anthelmia, Belladonna, Iris Versicolor, and Gelsemium. However, the selection of the most suitable remedy depends on the specific symptoms and individual case.
Is homeopathic treatment safe for cluster headaches?
Homeopathic remedies are generally considered safe when prescribed by a qualified practitioner. They are often derived from natural substances and are typically highly diluted, minimizing the risk of side effects.
Can homeopathy cure cluster headaches?
While there is no cure for cluster headaches, homeopathic treatment aims to reduce the frequency, duration, and intensity of attacks. It can also help manage associated symptoms and improve overall quality of life.
Should I consult a homeopath for cluster headaches?
Yes
If you are considering homeopathic treatment for cluster headaches, it is essential to consult a qualified homeopathic practitioner. They will conduct a thorough evaluation of your symptoms and medical history to determine the most appropriate treatment plan for you.
