Conduct Disorder
Definition
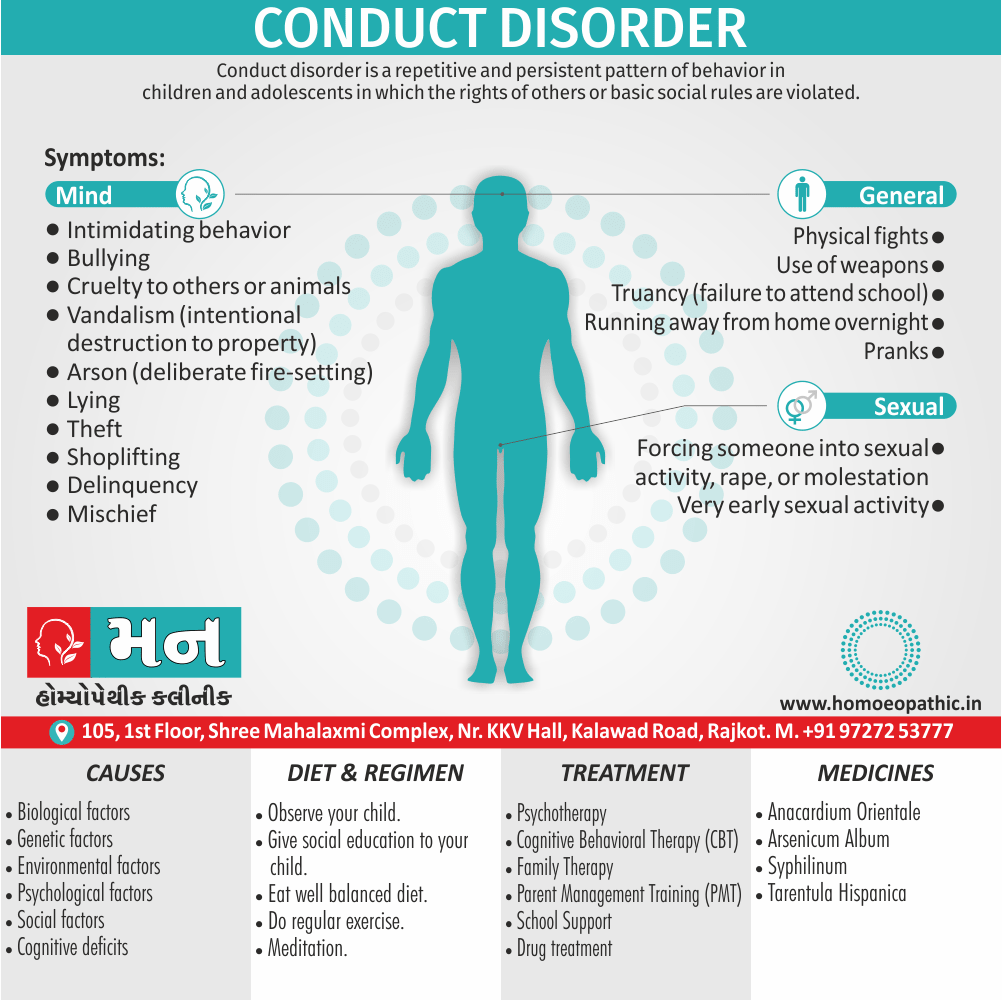
Conduct disorder is a repetitive and persistent pattern of behavior in children and adolescents in which the rights of others or basic social rules are violated. [1]
There aren’t direct synonyms for "conduct disorder" because it’s a specific clinical diagnosis. However, depending on the context, you can use phrases that capture some of its key characteristics:
- Focus on behavior: Antisocial behavior disorder, disruptive behavior disorder
- Legal aspects: Delinquency
These options emphasize different aspects of conduct disorder. Remember, they are not interchangeable with the formal diagnosis.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
It is estimated that 2-16% of children in the U.S. have conduct disorder.
It is more common in boys than in girls and most often occurs in late childhood or the early teen years.
This is not uncommon for children and teens to have behavior-related problems at some time during their development.
However, the behavior is considered to be a conduct disorder when it is long-lasting and when it violates the rights of others, goes against accepted norms of behavior and disrupts the child’s or family’s everyday life. [2]
The child or adolescent usually exhibits these behavior patterns in a variety of settings at home, at school, also in social situations and they cause significant impairment in his or her social, academic, and family functioning. [1]
Epidemiology
Epidemiology
There is a limited number of studies on Conduct Disorder (CD) in the Indian context. A cross-sectional study conducted in 2015 found the prevalence of CD among primary school children in a rural area of India to be 5.48%, with a higher prevalence among males (66.67%) compared to females (33.33%). (Mishra et al., 2015)[9]
Causes
Causes of Conduct Disorder
The exact cause of this disorder not known, but it is believed that a combination of biological, genetic, environmental, psychological, also social factors play a role.
Biological:
- Some studies suggest that either defects or injuries to certain areas of the brain can lead to behavior disorders.
- Moreover, Damage to the frontal lobe of the brain has been linked to conduct disorder.
- The frontal lobe is the part of your brain that regulates important cognitive skills, such as problem-solving, memory, and emotional expression.
- Additionally, It’s also home to your personality.
- The frontal lobe in a person with conduct disorder may not work properly. [4]
- Its symptoms may occur if nerve cell circuits along these brain regions do not work properly.
- Further, many children and teens with conduct disorder also have other mental illnesses, such as attention-deficit/hyperactivity disorder (in other words, ADHD), learning disorders, depression, substance abuse, or an anxiety disorder, which may contribute to the symptoms of conduct disorder.
Genetics:
- In detail, Many children and teens with conduct disorder have close family members with mental illnesses, including mood disorders, anxiety disorders, substance use disorders also personality disorders.
- This suggests that a vulnerability to conduct disorder may be at least partially inherited.
Environmental:
- Factors such as a dysfunctional family life, childhood abuse, traumatic experiences, a family history of substance abuse, also inconsistent discipline by parents may contribute to the development of conduct disorder.
Psychological:
- In brief, Some experts believe that conduct disorders can reflect problems with moral awareness (notably, lack of guilt and remorse) and deficits in cognitive processing. [2]
Social:
- Low socioeconomic status and not being accepted by their peers, additionally, disorganized neighborhoods, poor schools, family breakdown, appear to be risk factors for the development of conduct disorder.
Cognitive deficits :
- Low IQ, poor verbal skills, and impairment in executive functioning may make children more vulnerable to conduct disorder. [2]
Types
Types of Conduct Disorder
There are three types of conduct disorder. They’re categorized according to the age at which symptoms of the disorder first occur:
- Childhood onset occurs when the signs of conduct disorder appear before age 10.
- Adolescent onset occurs when the signs of conduct disorder appear during the teen years.
- Unspecified onset means the age at which conduct disorder first occurs is unknown.
Risk Factors
Risk Factors
- Being male
- Living in an urban environment
- Living in poverty
- Having a family history of either conduct disorder or mental illness
- Other psychiatric disorders
- Has parents who abuse either drugs or alcohol
- A dysfunctional home environment
- History of experiencing traumatic events
- Being abused or neglected [4]
Pathogenesis
Pathogenesis
The pathogenesis of Conduct Disorder (CD) is complex and multifactorial, involving an interplay of genetic, environmental, and neurobiological factors.
The book Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry explains that genetic factors play a significant role in the development of CD, with heritability estimates ranging from 40% to 50%. Environmental factors, such as childhood maltreatment, neglect, and exposure to violence, also contribute to the development of CD. Neurobiological factors, such as abnormalities in brain structure and function, particularly in the prefrontal cortex and amygdala, have also been implicated in CD.
It is important to note that CD is a heterogeneous disorder, and the specific combination of factors that contribute to its development may vary from individual to individual.[10]
Pathophysiology
Pathophysiology
The pathophysiology of Conduct Disorder (CD) is complex and involves multiple interacting factors. While a specific book dedicated solely to the pathophysiology of CD might not exist, several resources discuss the topic within the broader context of child and adolescent psychiatry.
This textbook "Textbook of Child and Adolescent Mental Health" details the current understanding of CD pathophysiology, highlighting the interplay of genetic, neurobiological, and environmental factors. Key points include:
- Genetic Factors: Heritability plays a significant role, with studies suggesting a genetic predisposition to aggression and impulsivity.
- Neurobiological Factors: Abnormalities in brain structure and function, particularly in the frontal lobes, have been associated with impaired decision-making, impulse control, and emotional regulation.
- Environmental Factors: Childhood trauma, neglect, and exposure to violence can contribute to CD development by disrupting normal brain development and affecting stress response systems.
- Gene-Environment Interactions: The complex interplay between genetic predisposition and environmental stressors is crucial in understanding CD pathophysiology.
By exploring these factors, the textbook provides a comprehensive overview of the complex mechanisms underlying Conduct Disorder, aiding in the development of targeted interventions and treatments.[11]
Clinical Features
Clinical Features
Conduct Disorder (CD) is characterized by a persistent pattern of behavior that violates the basic rights of others or major age-appropriate societal norms or rules.
Clinical Features (as per DSM-5):
The DSM-5 outlines the following core clinical features of Conduct Disorder:
Aggression to People and Animals: This includes bullying, threatening, or intimidating others; initiating physical fights; using a weapon that can cause serious physical harm (e.g., a bat, brick, broken bottle, knife, gun); physical cruelty to people or animals; stealing while confronting a victim (e.g., mugging, purse snatching, extortion, armed robbery); and forcing someone into sexual activity.
Destruction of Property: This includes deliberately engaging in fire setting with the intention of causing serious damage; and deliberately destroying others’ property (other than by fire setting).
Deceitfulness or Theft: This includes breaking into someone else’s house, building, or car; often lying to obtain goods or favors or to avoid obligations (i.e., "cons" others); and stealing items of nontrivial value without confronting a victim (e.g., shoplifting but without breaking and entering; forgery).
Serious Violations of Rules: This includes staying out at night despite parental prohibitions, beginning before age 13 years; running away from home overnight at least twice while living in parental or parental surrogate home, or once without returning for a lengthy period; and often truant from school, beginning before age 13 years.
These behaviors cause clinically significant impairment in social, academic, or occupational functioning. The disturbance in behavior is not exclusively during the course of schizophrenia spectrum or bipolar disorder.[12]
Sign & Symptoms
Sign & Symptoms
Generally, Children who have conduct disorder are often hard to control and unwilling to follow rules.
Moreover, They act impulsively without considering the consequences of their actions.
Besides this, They also don’t take other people’s feelings into consideration.
Your child may have conduct disorder if they persistently display one or more of the following behaviors i.e. :
Aggressive Conduct:
Aggressive conduct causes or threatens physical harm to others and may include the following i.e.:
- Intimidating behavior
- Bullying
- Physical fights
- Cruelty to others or animals
- Use of a weapon(s)
- Forcing someone into sexual activity, either rape, or molestation
Destructive conduct:
Destructive conduct may include the following e.g.:
- Vandalism (in other words, intentional destruction to property)
- Arson (in other words, deliberate fire-setting)
Deceitfulness:
This may include breaking into homes or cars in order to steal & may include the following e.g.:
- Lying
- Theft
- Shoplifting
- Delinquency
Violation of rules:
Violation of ordinary rules of conduct or age-appropriate norms may include the following e.g.:
- Truancy (in other words, failure to attend school)
- Running away from home overnight
- Pranks
- Mischief
- Very early sexual activity
In conclusion, The symptoms of this disorder may resemble other medical conditions or behavioral problems. [3]
Clinical Examination
Clinical Examination
While a specific "clinical examination" for Conduct Disorder (CD) isn’t outlined in a standardized format within textbooks, the diagnostic process heavily relies on a comprehensive psychiatric evaluation.
This textbook Dulcan’s Textbook of Child and Adolescent Psychiatry emphasizes that the clinical assessment for CD typically involves:
Detailed Clinical Interview: This includes gathering information from the child or adolescent, parents, teachers, and other relevant individuals to assess the presence and severity of CD symptoms, as well as their impact on functioning.
Review of Collateral Information: This includes reviewing school reports, legal records, and any previous mental health evaluations to gain a comprehensive understanding of the individual’s history and current presentation.
Mental Status Examination: This assesses the individual’s current mental state, including mood, affect, thought processes, and cognitive functioning.
Assessment of Comorbid Conditions: CD frequently co-occurs with other mental health disorders, such as attention-deficit/hyperactivity disorder (ADHD) and mood disorders. Therefore, a thorough assessment for comorbid conditions is essential.
Rating Scales and Questionnaires: Standardized rating scales and questionnaires, such as the Child Behavior Checklist (CBCL) and the Vanderbilt Assessment Scales, can aid in quantifying the severity of CD symptoms and monitoring treatment progress.
By combining these elements, clinicians can arrive at an accurate diagnosis of CD and develop a personalized treatment plan to address the individual’s specific needs.
Important Note: It’s crucial to remember that the diagnosis of CD is based on clinical judgment and a thorough assessment of the individual’s history and current presentation, rather than relying on a single test or examination.[13]
Diagnosis
Diagnosis
- A child psychiatrist or a qualified mental health professional usually diagnoses conduct disorders in children and adolescents.
- Moreover, A detailed history of the child’s behavior from parents and teachers, observations of the child’s behavior, also, sometimes, psychological testing contribute to the diagnosis.
- Parents who note symptoms of conduct disorder in their either child or teen can help by seeking an evaluation and treatment early.
- Besides this, Early treatment can often prevent future problems.
- Further, this disorder often coexists with other mental health disorders, including mood disorders, anxiety disorders, posttraumatic stress disorder, substance abuse, attention-deficit/hyperactivity disorder, and learning disorders, increasing the need for early diagnosis and treatment.
- Lastly, Consult your child’s doctor for more information. [3]
Differential Diagnosis
Differential diagnosis
- Oppositional defiant disorder
- Attention-deficit/hyperactivity disorder (ADHD)
- Mood disorder
- Intermittent explosive disorder.(6)
Complications
Complications
Conduct Disorder (CD) can lead to significant complications and long-term consequences if left untreated.
Book:Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry
Complications (as per the book):
Academic and Occupational Problems: Children with CD often experience difficulties in school, such as poor academic performance, truancy, and expulsion. These difficulties can persist into adulthood, leading to unemployment or underemployment.
Substance Abuse: Individuals with CD are at increased risk for developing substance use disorders. This is likely due to a combination of impulsivity, poor judgment, and association with deviant peer groups.
Legal Problems: CD is strongly associated with delinquent and criminal behavior. Individuals with CD are more likely to engage in theft, vandalism, assault, and other illegal activities, which can lead to arrest and incarceration.
Mental Health Disorders: CD is often comorbid with other mental health disorders, such as depression, anxiety disorders, and personality disorders. These co-occurring disorders can exacerbate the symptoms of CD and make treatment more challenging.
Social and Interpersonal Problems: Individuals with CD often have difficulty forming and maintaining healthy relationships. Their aggressive, impulsive, and deceitful behavior can alienate others and lead to social isolation.
Physical Health Problems: CD is associated with an increased risk of physical health problems, such as sexually transmitted infections (STIs), unintended pregnancies, and injuries from accidents or violence.
It is important to note that not everyone with CD will experience all of these complications. However, early identification and intervention are crucial to reducing the risk of long-term negative outcomes. [10]
Investigations
Investigation
While there isn’t a specific "investigation" in the medical sense for Conduct Disorder (CD), the diagnostic process involves a thorough assessment to determine the presence and severity of the disorder.
This textbook Textbook of Child and Adolescent Mental Health details the assessment process, which typically involves the following:
Clinical Interviews:
- Child/Adolescent: A comprehensive interview with the child or adolescent to gather information about their behaviors, thoughts, and feelings.
- Parents/Caregivers: Interviews with parents or caregivers to obtain information about the child’s behavior at home, school, and in other settings.
- Teachers/Other Adults: If relevant, interviews with teachers, school counselors, or other adults who have regular contact with the child can provide valuable information.
Review of Records:
- School Records: Academic performance, disciplinary reports, and any notes from teachers or counselors.
- Medical Records: History of any medical or neurological conditions that could contribute to behavioral problems.
- Legal Records: Any history of involvement with the juvenile justice system.
Psychological Testing:
- Behavior Rating Scales: Standardized questionnaires completed by parents, teachers, or the child themselves to assess the frequency and severity of CD symptoms.
- Cognitive Assessments: Tests to assess intellectual functioning and identify any cognitive deficits that could be contributing to the behavior problems.
- Personality Assessments: To assess for personality traits or disorders that may be associated with CD.
Observation of Behavior:
- In the Clinic: Observing the child’s behavior during the assessment can provide valuable information about their social skills, emotional regulation, and impulsivity.
- In Other Settings: If possible, observing the child in their natural environment (e.g., at school or home) can provide additional insights into their behavior.
By combining information from these different sources, clinicians can make an accurate diagnosis of CD and develop a comprehensive treatment plan.[11]
Treatment
Treatment of Conduct Disorder
It is based on many factors, including the child’s age, the severity of symptoms, as well as the child’s ability to participate in and tolerate specific therapies.
Treatment usually consists of a combination of the following:
Psychotherapy:
- Psychotherapy (in other words, a type of counseling) aimed at helping the child learn to express and control anger in more appropriate ways.
- A type of therapy called cognitive-behavioral therapy aims to reshape the child’s thinking (in other words, cognition) to improve problem solving skills, anger management, moral reasoning skills, and impulse control.
- Family therapy may use to help improve family interactions and communication among family members.
- A specialized therapy technique called parent management training (in other words, PMT) teaches parents ways to positively alter their child’s behavior in the home.
School support:
- It is another important part of treatment for conduct disorder.
- For children and teens in school, a team of people will assemble to help your child with conduct disorder.
- This team typically involves school counselors, school psychologists, social workers, administrators, and others.
- If your child diagnose with conduct disorder, they may qualify for an Individualized Educational Plan (in other words, IEP) or a 504 plan, which can provide them with the needed accommodations to ensure their academic also social success at school.
Medication:
Although there is no medication formally approved to treat it, various drugs may be used to treat some of its distressing symptoms (impulsivity, aggression), as well as any other mental illnesses that may be present, such as ADHD or major depression. [2]
Prevention
Prevention of Conduct Disorder
- Things such as a traumatic experience, social problems, and biological factors may be involved.
- To reduce the risk for conduct disorder, parents can learn positive parenting strategies.
- This can help to create a closer parent-child relationship.
- It can also create a safe and stable home life for the child.(7)
Homeopathic Treatment
Homeopathic Treatment of Conduct Disorder
We treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Conduct Disorder:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity for conduct disorder but this is not a complete and definite guide to the homeopathy treatment of conduct disorder. The symptoms listed against each homeopathic remedy may not be directly related to conduct disorder because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicines for conduct disorder only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines for conduct disorder:
Anacardium:
- The child exhibits wickedness and malice with no remorse for its actions.
- This is often accompanied by gastric complaints.
Syphilinum:
- The child exhibits tendency to destroy things also harm people.
- This is often accompanied by recurrent ulcers in the mouth that bleed, teeth that are carried gums that are swollen. [5]
Belladonna
- It is very useful medicine for Conduct Disorder
- Sudden, violent effects. Dryness. bright redness. Burning heat, great pain.
- Congestion to head with throbbing of carotids. Sensitive to drafts of cold air.
- Pains – throbbing, sharp cutting, shooting. Jerks, spasms.
- Dilated pupils. Photophobia. Dry, hot mouth and throat.
- Bright red, glossy skin. Jerks during sleep.
- Wildly delirious, restless, biting mania.
4. Hyoscyamus
- Flamboyant stage of exhibitionism or mania. Loquacious. Jealous. Suspicious.
- Sexual minded. Masturbation. Absence of morals. Shamelessness.
- Restlessness. Dancing.
- Depression or mania after breaking of romantic relationships.
- Convulsions.
5. Cantharis
- Irritation, disposition to fly into a rage. Fits of rage with crying, barking, striking, renewed by the sight of bright, dazzling objects and of water, and by touching the larynx.
- Acute mania, generally of a sexual type, amorous frenzy, fiery sexual desire. Sudden loss of consciousness with red face.
- Moaning and violent cries, interspersed with barking.
- Convulsion and howling like a dog, ending in a stupor.
- Constantly attempts to do something but accomplishes nothing.
6. HeparSulph
- Peevish, highly impulsive. Impulse to stab or kill.
- Anguish in evening and night, with thoughts of suicide.
- Irritable and dissatisfied with oneself and others.
- Starting on falling asleep.
- Agoraphobia.
- Fear and dreams of fire. Wants to set things or house on fire. Throws things into fire.
7. Tarentula Hispanica
- Moral depravity. Lacks control.
- Suddenly changing moods, fancies, or strength.
- Crafty, cunning, dishonest, selfish, destructive, destroys whatever she can lay hand on, tears her clothes, etc.
- Hateful, throws things away. Malingering.
- Hysteria.
- When attention is directed to her, she begins to twitch, feigns, fainting. Sensibility, but looks sideways to observe the effect on those around her.
- Desires to strike herself or others.
- Aversion to being touched.
- Kleptomania, laughs, mocks run, dances, gesticulates, jokes, cries, sings till hoarse or exhausted.
8. Stramonium
- VIOLENCE AND FEAR OF VIOLENCE. A subconscious, dark element. Intense emotions leading to violence; out of control, sudden anger.
- Can be destructive with striking, biting, tearing, smashing, strangling. Rage and violence, has the capacity to commit murder.
9. Chamomilla
- Piteous moaning because child cannot have what he wants.
- Child can be quieted only when carried about or petted constantly.
- Ugly in behavior, cross, uncivil, quarrelsome.
- Snappish, cannot return a civil answer.
- Vexed at every trifle.
- Anger from pain.
- Impatient; intolerant of being spoken to or interrupted when spoken to.
- Aversion to being touched or even looked at.
- Sensitive to music, noise.
10. Veratrum Album
Diet & Regimen
Diet & Regimen of Conduct Disorder
- Observe your child.
- Give social education to your child.
- Eat well balanced diet.
- Do regular exercise.
- Meditation.
Do’s and Don'ts
The Do’s & Don’ts:
Managing Conduct Disorder (CD) involves a multifaceted approach that includes both therapeutic interventions and behavioral strategies. While a specific "Do’s and Don’ts" list might not exist in a single book, several resources provide valuable guidance.
Although not exclusively about CD, this book "Parenting the Strong-Willed Child" offers insights applicable to managing children with challenging behaviors. Based on the principles outlined in this book and other relevant sources, here’s a synthesized list of Do’s and Don’ts for managing CD:
Do’s:
- Seek professional help: Early intervention is crucial. Consult with a mental health professional to assess the child’s needs and develop a personalized treatment plan.
- Establish clear and consistent rules: Clearly define expectations and consequences for misbehavior. Consistency is key to helping the child understand and follow the rules.
- Use positive reinforcement: Focus on rewarding positive behaviors, rather than just punishing negative ones. Praise, attention, and privileges can be powerful motivators.
- Stay calm and consistent: Avoid yelling, lecturing, or reacting emotionally to misbehavior. Remain calm and firm, enforcing consequences consistently.
- Teach problem-solving skills: Help the child develop alternative ways to manage anger, frustration, and conflict.
- Collaborate with school and other professionals: Work with teachers, school counselors, and therapists to create a supportive and consistent environment for the child.
- Take care of yourself: Parenting a child with CD can be challenging. Make sure to prioritize your own well-being, seeking support from friends, family, or professionals if needed.
Don’ts:
- Don’t give up: Managing CD takes time and patience. Don’t get discouraged if you don’t see immediate results.
- Don’t engage in power struggles: Arguing or negotiating with the child about rules and consequences will only escalate the situation.
- Don’t resort to physical punishment: Physical discipline is ineffective and can worsen the child’s behavior.
- Don’t blame yourself: CD is a complex disorder with multiple contributing factors. It’s not your fault as a parent.
- Don’t isolate yourself: Reach out to others for support and information. You’re not alone in this.
Remember, managing Conduct Disorder is a journey that requires patience, understanding, and professional guidance. By following these do’s and don’ts and working collaboratively with your child’s treatment team, you can help your child develop healthier coping skills and behaviors.[5]
Terminology
Terminology
Here’s a breakdown of the terminologies used in the article, along with their meanings:
Conduct Disorder (CD):
A mental health disorder characterized by persistent behavior that violates the rights of others or societal norms. This includes aggression, destruction, deceit, theft, and rule-breaking.
Antisocial Behavior Disorder:
A broader term sometimes used interchangeably with CD, emphasizing behaviors that go against social norms and cause harm to others.
Disruptive Behavior Disorder:
Another umbrella term encompassing a range of behavioral problems in children, including CD and Oppositional Defiant Disorder (ODD).
Delinquency:
Refers to illegal acts committed by minors, often associated with CD.
Frontal Lobe:
A brain region responsible for executive functions like decision-making, impulse control, and social behavior. Abnormalities in this area are linked to CD.
Cognitive Processing:
Mental processes involved in thinking, understanding, and problem-solving. Deficits in cognitive processing may contribute to CD.
Comorbid:
The presence of two or more disorders or conditions in an individual simultaneously (e.g., CD and ADHD).
Psychotherapy:
A type of therapy that aims to address mental health issues through talk therapy and various behavioral techniques.
Cognitive-Behavioral Therapy (CBT):
A specific type of psychotherapy that helps individuals identify and change negative thought patterns and behaviors.
Family Therapy:
Therapy involving the entire family to improve communication, relationships, and problem-solving skills.
Parent Management Training (PMT):
A program teaching parents strategies to manage their child’s behavior effectively.
Individualized Education Plan (IEP):
A tailored educational plan for children with functional needs to provide support and accommodations.
504 Plan:
A plan that outlines accommodations and support for students with disabilities to ensure equal access to education.
Homeopathy:
A system of alternative medicine based on the principle of "like cures like," using highly diluted substances to stimulate the body’s healing response.
Miasm:
A homeopathic concept referring to a predisposition to certain types of diseases or illnesses.
Case Taking:
The process in homeopathy where a practitioner gathers detailed information about a patient’s symptoms, medical history, and personality to determine the appropriate remedy.
References
References for Conduct Disorder
- https://www.mentalhealthamerica.net/conditions/conduct-disorder
- https://www.webmd.com/mental-health/mental-health-conduct-disorder#1
- https://www.stanfordchildrens.org/en/topic/default?id=conduct-disorder-90-P02560
- https://www.healthline.com/health/conduct-disorder#risk-factors
- Parenting the Strong-Willed Child
Author: Rex Forehand, Edition: Revised Edition, (2005), Publication: Guilford Press. - differntial diagnosis of conduct disorder – Search (bing.com)
- Conduct Disorder | Johns Hopkins Medicine
- Conduct Disorder Management with Homeopathy using Zomeo Software (hompath.com)
- Mishra, K.N., Prabhakar, B.S., & Singh, A.R. (2015). Prevalence of Conduct Disorder in Primary School Children of Rural Area. ResearchGate. https://www.researchgate.net/publication/276179943_PREVALENCE_OF_CONDUCT_DISORDER_IN_PRIMARY_SCHOOL_CHILDREN_OF_RURAL_AREA
- Title: Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry, Edition: 11th Edition, Authors: Benjamin J. Sadock, Virginia A. Sadock, Pedro Ruiz, (2014), Publication: Wolters Kluwer.
- Title: Textbook of Child and Adolescent Mental Health
Editors: Mina K. Dulcan, Sarah M. Horwitz, Mark A. Riddle
Edition: 5th Edition (2023)
Publication: American Psychiatric Association Publishing. - Title: Diagnostic and Statistical Manual of Mental Disorders
Edition: 5th Edition (DSM-5)
Author: American Psychiatric Association
Year of Publication: 2013
Publication: American Psychiatric Publishing. - Title: Dulcan’s Textbook of Child and Adolescent Psychiatry
Editors: Mina K. Dulcan, Sarah M. Horwitz, Mark A. Riddle, Edition: 7th Edition, (2019), Publication: American Psychiatric Association Publishing.
Also Search As
Also Search As
People can search for the article on Conduct Disorder and Homeopathy using the following search terms and phrases:
Specific terms:
- Conduct disorder
- Homeopathy for conduct disorder
- Homeopathic remedies for behavior problems
- Alternative treatment for conduct disorder
- Natural remedies for conduct disorder in children
Question phrases:
- Can homeopathy help with conduct disorder?
- What are homeopathic remedies for conduct disorder?
- Is homeopathy safe for children with conduct disorder?
- Can homeopathy replace conventional treatment for conduct disorder?
There are several ways to search for the article on Conduct Disorder and Homeopathy:
Search Engines:
Use search engines like Google, Bing, or DuckDuckGo. Enter relevant keywords or phrases mentioned earlier, such as "homeopathy for conduct disorder" or "homeopathic remedies for behavior problems." You can also try using question phrases like "Can homeopathy help with conduct disorder?"
Academic Databases:
If you have access to academic databases like PubMed, Google Scholar, or ScienceDirect, you can search for scholarly articles on the topic. Use keywords like "conduct disorder," "homeopathy," and "children" to narrow down your search.
Homeopathic Websites and Forums:
Many websites and online forums are dedicated to homeopathy. Search these platforms for articles, discussions, or case studies related to Conduct Disorder and homeopathy.
Social Media:
Search for relevant hashtags on social media platforms like Twitter or Facebook. Look for groups or pages dedicated to homeopathy or child mental health, where you might find discussions or links to articles.
Ask a Homeopathic Practitioner:
If you know a homeopathic practitioner, they may be able to direct you to relevant resources or research on the topic.
By utilizing these different methods, you can increase your chances of finding the information you need on Conduct Disorder and Homeopathy.
Frequently Asked Questions (FAQ)
What is Conduct Disorder?
Conduct disorder is a repetitive and persistent pattern of behavior in children and adolescents in which the rights of others or basic social rules are violated.
What are the treatment options for CD?
Treatment often involves a combination of psychotherapy, parent training, and medication if necessary. Early intervention is crucial for improving outcomes.
What are the causes of conduct disorder?
Causes for Conduct Disorder
- Defects or injuries to certain areas of the brain
- Genetics
- Childhood abuse
- Traumatic experiences
- Low socioeconomic status
- Family breakdown
- Low IQ
- Poor verbal skills
What are the symptoms of conduct disorder?
Symptoms of Conduct Disorder
- Hard to control
- Act impulsively
- Intimidating behavior
- Bullying
- Physical fights
- Cruelty to others or animals
- Use of a weapon
- Vandalism
- Lying
- Theft
- Shoplifting
- Delinquency
How does a homeopath choose the right remedy for Conduct Disorder?
A homeopathic practitioner will conduct a detailed case taking, considering the child’s physical, emotional, and mental symptoms, as well as their overall temperament and personality, to select the most appropriate remedy.
How long does it take for homeopathic treatment to show improvement in Conduct Disorder?
The response to homeopathic treatment can vary depending on the individual and the severity of the condition. In some cases, improvement may be seen within a few weeks or months, while in others, it may take longer.
Is homeopathic treatment safe for Conduct Disorder?
Homeopathic remedies are generally considered safe when used appropriately under the guidance of a qualified homeopathic practitioner. However, it’s crucial to inform your healthcare provider about any homeopathic remedies you are taking, especially if you are pregnant, breastfeeding, or have any existing medical conditions.
Can homeopathy be used alongside conventional treatment for Conduct Disorder?
Homeopathy can be used as a complementary therapy alongside conventional treatment for Conduct Disorder. However, it’s essential to consult with a qualified homeopathic practitioner and inform your conventional healthcare provider about any homeopathic remedies you are taking.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Conduct Disorder?
Homoeopathic Medicines for Conduct Disorder
- Anacardium
- Syphilinum
