Constipation
Definition
Constipation is a condition marked by infrequent bowel movements (typically less than 3 per week) and difficulty passing stool. The stool itself may be hard and dry, or soft and difficult to expel completely. Constipation is also defined as infrequent passage of hard stool. Even ineffectual urge or a sensation of incomplete stools can be termed as constipation.
Constipation also known as
Here are some synonyms for constipation, depending on the nuance you want to convey:
Informal:
- Costiveness (a more old-fashioned term)
- Backed up
- Bound up
- Stopped up
Medical:
- Dyschezia (difficulty passing stool)
- Fecal impaction (accumulation of hardened stool)
- Obstipation (severe constipation)
Focus on irregularity:
- Irregularity
- Bowel dysfunction
Figurative:
- Bottleneck (referring to a blockage)
- Block
- Impediment
Overview
Epidemiology
Types
Causes
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
Constipation may occur in many gastrointestinal and other medical disorders.
Demography
According to northern Indian community study, 555/4767 (11.6%) reported symptoms of constipation. Likewise in the former group, 1404 (53%) had self-perceived constipation. And in the latter, 846 (18%), 1030 (23%) reported straining at stools, and incomplete stool evacuation, respectively. Similarly in another community survey in rural northern India, the prevalence of constipation-predominant irritable bowel syndrome (IBS-C) was 2.4%.
Two smaller community surveys from Chandigarh and Bangalore reported the prevalence of constipation of 24.8% and 8.6%, respectively. Though the latter study was conducted exclusively among old age population, in an eastern Indian study, of 331 consecutive patients with Chronic Constipation. In which 65% were older than 60 years.
Epidemiology
Epidemiology
The epidemiology of constipation varies depending on the population studied and the definition of constipation used. However, it is generally considered a common condition affecting a significant portion of the global population.
- A systematic review and meta-analysis (Mugie et al., 2011) found that the prevalence of constipation ranges from 0.7% to 79%, with a pooled prevalence of 14%.[6]
- A community-based survey in India (Bharucha et al., 2013) reported a prevalence of self-reported constipation of 24.8% within the last year.[7]
- In Europe and Oceania, a systematic review (Suares and Ford, 2008) reported the mean prevalence of constipation as 17.1% (range 3.6%-39.6%).[8]
Several factors can influence the prevalence of constipation, including:
- Age: Constipation is more common in older adults.
- Gender: Women are more likely to experience constipation than men.
- Diet: Low-fiber diets and inadequate fluid intake can contribute to constipation.
- Physical activity: Sedentary lifestyles increase the risk of constipation.
- Medications: Certain medications, such as opioids and antidepressants, can cause constipation as a side effect.
It is important to note that these are just a few examples, and the epidemiology of constipation is a complex and evolving field of research.
Types
Types
three types, they are:
- Obstructive constipation: is the result of actual physical obstruction of the passage of feces. Causes include cystic fibrosis (in children), tumors, adhesions, scars formed in the abdomen (mostly after abdominal surgery), strictures firmed within the intestine (mostly caused by inflammation, like in Crohn’s disease), or damaged pelvic nerves (injuries, neurological diseases) that prevent relaxation of anal muscles.
- Atonic constipation: is the result of lack of intestinal muscle tone (tension) of the colon, abdominal wall or pelvic floor, also known as lazy colon. Person with this constipation simply does not feel the urge to defecate even when the colon is full of feces. It may occur in old age or bedridden patients or after prolonged dependence on laxatives. Most common among old people (weak muscle tone), woman (pelvic floor weakness), and diabetics (damage to intestinal nerves).
- Spastic constipation: is result from colonic spasms caused by irritation of the bowel or intestines. In this case, a diet that is low in fiber is usually suitable. It is also a symptom of irritable bowel syndrome.
Based on the duration of constipation, they are of two types
- Acute constipation (occasional problem) – constipation occurs suddenly and last for few days. Acute constipation with worrisome symptoms such as rectal bleeding, abdominal pain and cramps, nausea and vomiting, and involuntary loss of weight needs urgent diagnosis.
- Chronic constipation (persistent problem) – is the constipation that lasts for longer durations. Your need medication and lifestyle change to normalize bowel movement.
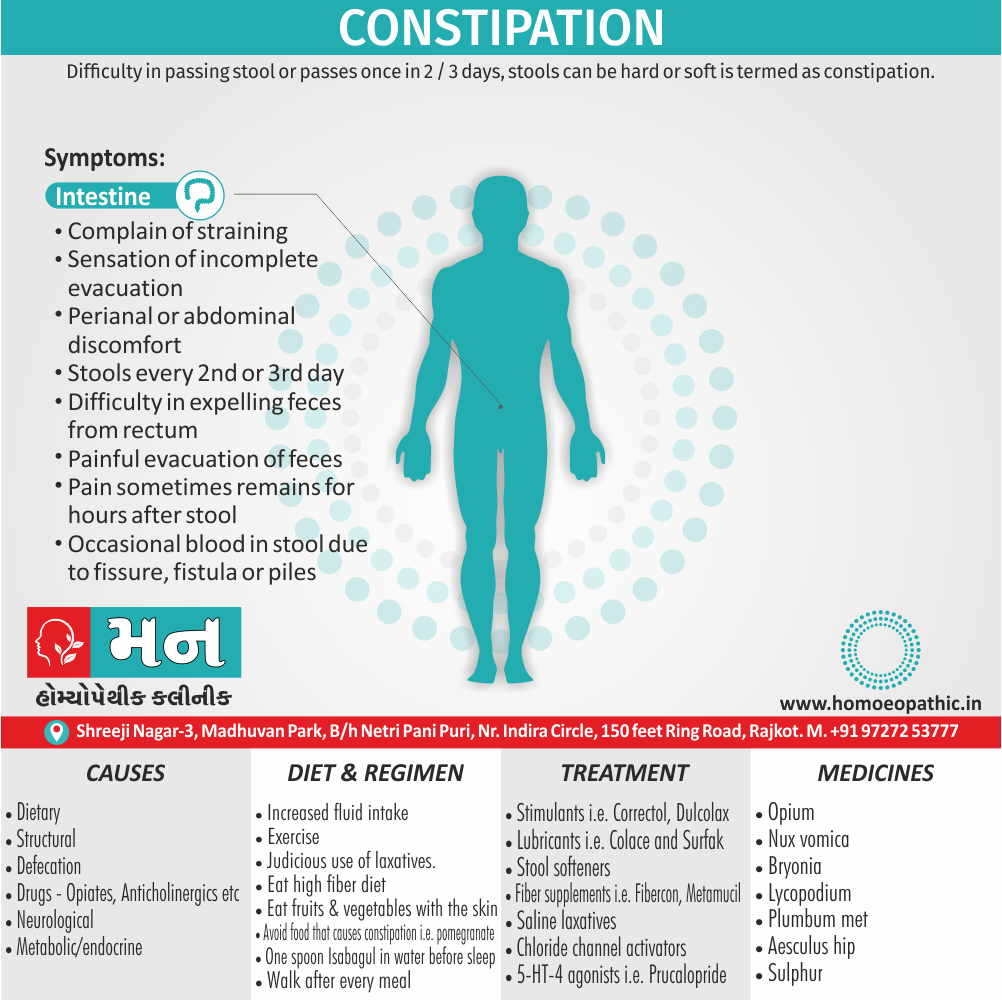
Causes
Cause
1.Gastrointestinal disorders
Dietary i.e.
- Lack of fibers also fluid intake Motility
- Slow-transit constipation
- Irritable bowel syndrome
- Drugs (see below)
- Chronic intestinal pseudo-obstruction
Structural i.e.
- Colonic carcinoma
- Diverticular disease
- Hirschsprung’s disease
Defecation i.e.
- Anorectal disease (e.g. Crohn’s, fissures, hemorrhoids)
- Obstructed defecation
2.Non-gastrointestinal
disorders
Drugs i.e.
- Opiates
- Anticholinergics
- Calcium antagonists
- Iron supplements
- Aluminum-containing antacids
Neurological i.e.
- Multiple sclerosis
- Spinal cord lesions
- Cerebrovascular accidents
- Parkinsonism
Metabolic/endocrine i.e.
- Diabetes mellitus
- Hypercalcemia
- Hypothyroidism
- Pregnancy
Others
- Any serious illness with immobility, especially in the older people
- Depression
Causes Constipation
Risk Factors
Risk factors of Constipation
- Either emotional or psychological problems
- Sedentary life
- Eating too much of meat also dairy products
- Chronic abuse of laxatives
- Bottle fed babies
- Pregnancy
- Drugs for instance; antacids, iron, calcium, blood pressure medications
- Certain digestive tract diseases
- Some School going children develop a habit to ignore the urge
- Cooking in aluminium, iron vessel
Pathogenesis
Pathogenesis
Constipation arises from a complex interplay of factors that disrupt normal bowel function. These factors can be broadly categorized into:
Slow Colonic Transit:
- Primary causes: Inherited or acquired disorders affecting the colonic nerves or muscles, leading to reduced peristalsis and prolonged stool transit time.
- Secondary causes: Medications (e.g., opioids, anticholinergics), metabolic disorders (e.g., hypothyroidism), neurological conditions (e.g., Parkinson’s disease), and lifestyle factors (e.g., low-fiber diet, sedentary lifestyle).
Pelvic Floor Dysfunction:
- Dyssynergic defecation: Impaired coordination of pelvic floor and abdominal muscles during defecation, leading to incomplete evacuation and straining.
- Anismus: Paradoxical contraction or failure to relax the anal sphincter during defecation.
Other Factors:
- Dietary factors: Low fiber intake, dehydration.
- Behavioral factors: Ignoring the urge to defecate, suppressing bowel movements.
- Psychological factors: Stress, anxiety, depression.[9]
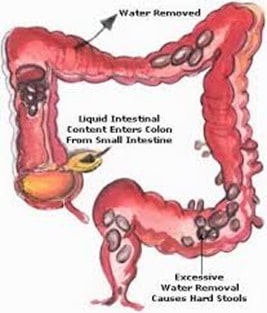
Pathophysiology
Pathophysiology
it results in various degrees of subjective symptoms and is associated with abnormalities (eg, colonic diverticular disease, hemorrhoidal disease, anal fissures) that occur secondary to an increase in colonic luminal pressure and intravascular pressure in the hemorrhoidal venous cushions.
Clinical Features
Clinical Features
The clinical features of constipation can vary widely depending on the underlying cause and individual patient characteristics. However, common features include:
Infrequent Bowel Movements:
- Fewer than three bowel movements per week is a hallmark of constipation.
- Some individuals may experience prolonged periods without bowel movements (obstipation).
Hard or Lumpy Stools:
- Stools are often dry, hard, and difficult to pass.
- They may be small, pebble-like, or fragmented.
Straining During Defecation:
- Excessive effort is required to pass stools.
- Straining may be accompanied by pain or discomfort.
Feeling of Incomplete Evacuation:
- A persistent sensation of not having fully emptied the bowels.
Other Symptoms:
- Abdominal pain, bloating, and distension.
- Nausea and vomiting (less common).
- Rectal bleeding or fissures (due to straining).
- Fecal impaction (severe constipation with hardened stool in the rectum).[9]
Sign & Symptoms
Sign & Symptoms of Constipation
- Complain of straining
- Moreover, Sensation of incomplete evacuation
- Either perianal or abdominal discomfort
- Stools every 2nd or 3rd day
- Additionally, Difficulty in expelling faeces from rectum
- Painful evacuation of faeces
- Besides this, Pain sometimes remains for hours after passing stool
- Lastly, Occasional blood in stool due to fissure, either fistula or piles

Clinical Examination
Clinical examination of Constipation
- Physical examination of patients with constipation is usually remarkable for anal fissure or palpable lumpy mass in abdomen (particularly in left quadrant).
- The presence of thrombosed external hemorrhoids, skin tags, rectal prolapse, anal fissure, anal warts, excoriation or evidence of pruritus ani due to fecal soiling on physical examination are suggestive of constipation.[1]
Appearance of the Patient
- Patients with chronic constipation usually appear to be discomfort while sitting due to anal pain
Skin
- Dry skin may be seen in systemic sclerosis
HEENT
- Extra-ocular movements may be abnormal
Neck
- Thyromegaly/thyroid nodules may be seen in hypothyroidism
Abdomen
- Abdominal distention
- Abdominal tenderness in the left lower abdominal quadrant
- A palpable abdominal mass in the left lower abdominal quadrant
Neuromuscular
- Altered mental status
- Clonus may be present
- Hyperreflexia
- Positive (abnormal) Babinski
- Muscle rigidity
- Abnormal gait (Parkinsonian gait)
- Unilateral/bilateral tremor (pill-rolling) (5)
Diagnosis
Diagnosis
Detailed History:
- Onset, duration, and frequency of symptoms (e.g., infrequent bowel movements, straining, hard stools).
- Dietary habits (e.g., fiber and fluid intake).
- Medical history (e.g., medications, underlying conditions).
- Psychosocial factors (e.g., stress, anxiety).
Physical Examination:
- Abdominal examination (e.g., tenderness, distension, masses).
- Digital rectal examination (e.g., anal tone, stool consistency, rectal masses).
Additional Tests (If Indicated):
- Blood tests: To rule out metabolic or endocrine disorders (e.g., thyroid function tests).
- Colonic transit studies: To assess the speed of stool movement through the colon (e.g., radiopaque markers, wireless motility capsule).
- Anorectal manometry: To evaluate the function of the anal sphincter and rectum during defecation.
- Balloon expulsion test: To assess the ability to expel stool from the rectum.
- Defecography: To visualize the process of defecation and identify any structural abnormalities.
- Colonoscopy: To rule out structural abnormalities or other conditions (e.g., colorectal cancer).[9]
Additional Information:
The Rome IV criteria are commonly used to diagnose functional constipation, which is the most common type of constipation. These criteria include:
- Must include two or more of the following:
- Straining during at least 25% of defecations.
- Lumpy or hard stools in at least 25% of defecations.
- Sensation of incomplete evacuation for at least 25% of defecations.
- Sensation of anorectal obstruction/blockage for at least 25% of defecations.
- Manual maneuvers to facilitate at least 25% of defecations (e.g., digital evacuation, support of the pelvic floor).
- Fewer than three spontaneous bowel movements per week.
- Loose stools are rarely present without the use of laxatives.
- Insufficient criteria for irritable bowel syndrome.
The diagnosis of constipation is often a process of elimination, ruling out other potential causes before attributing symptoms to functional constipation.
Differential Diagnosis
Differential diagnosis of Constipation
- Malignancy
- Diabetic autonomic neuropathy
- Irritable bowel syndrome
- Rectocele
- Fissure
- Anismus
- Systemic sclerosis
- Hypothyroidism
- Parkinson’s disease
- Multiple sclerosis
- Hypomagnesemia,
- Hypocalcemia,
- Depression. (5)
Complications
Complications
- Haemorrhoids
- Anal fissure
- Faecal impaction
- Rectal bleeding after continually straining to pass stools
Investigations
Investigations
Careful examination contributes more to the diagnosis than extensive investigation
First visit
Digital rectal examination
Proctoscopy and sigmoidoscopy (especially for detect anorectal disease)
Routine biochemistry including serum calcium and thyroid function tests
Full blood count should be carried out
If these are normal, a 1-month trial of dietary fibre and/or laxatives is justified
Next visit
If symptoms persist, then examination of the colon by barium enema or CT colonography is indicated to look for structural disease.
Further investigation
Generally, If no cause is found and disabling symptoms are present, then specialist referral for investigation of possible dysmotility may be necessary
Treatment
Treatment of Constipation
In the majority of cases, constipation resolves itself without any treatment or risk to health.
According to underlying cause
Stimulants:
These make the muscles in the intestines contract rhythmically. Additionally, These include Correctol, Dulcolax, and Senokot.
Lubricants:
These help the stool move down the colon more easily. Furthermore, These include mineral oil and Fleet
Stool softeners:
These moisten the stool. Stool softeners include Colace also Surfak.
Fiber supplements:
In detail, These are perhaps the safest laxatives. Additionally, They are also called bulk laxatives. They include Fiber Con, Metamucil, Konsyl, Serutan, also Citrucel and should be taken with plenty of water. Lastly, If you want to buy bulk laxatives, then there is an excellent selection online with thousands of customer reviews
Osmotics:
These facilitate the movement of fluids through the colon. These include Cephulac, Sorbitol, also Miralax
Saline laxatives:
In brief, These draw water into the colon and include milk of magnesia
Chloride channel activators:
These require a prescription and include lubiprostone (specifically, Amitiza)
5-HT-4 agonists:
They increase the secretion of fluid in the intestines and speed up the rate at which food passes through the colon. Additionally, They include Prucalopride
Prevention
Prevention of Constipation
- Constipation is usually easier to prevent than to treat. The relief of constipation with osmotic agents, i.e., lactulose, polyethylene glycol (PEG), or magnesium salts, should also be immediately followed by prevention using increased fiber (fruits, vegetables, and grains) and a nightly decreasing dose of osmotic laxative.
- Effective measures for the primary prevention of constipation include fiber supplementation, appropriate fluid intake, toilet habits, and exercise.
Fiber supplementation
- Including enough fibers in the daily diet is the most important primary prevention measure.
Fluid intake
- Fluid intake is the key factor to maintain the body hydration status and firm consistency of stools.
- Caffeine, alcohol, and fizzy drinks should be limited, preferably avoided completely.
Toilet habits
- Ignorance to toilet urge can lead to constipation.
- Never delay the defecation in case of urgency
Physical exercise
- It is postulated that 150 minutes of physical exercises can prevent constipation. (5)
- The sufficient fiber intake for general gastrointestinal health is 30 g per day, while more is better.
Homeopathic Treatment
Homeopathic treatment for Constipation
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Constipation:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
Opium
An inclination to evacuate but feeling as if the orifice were closed; no regular pressure; sensation as if a load on abdomen; heavy drowsy feeling; dry mouth, thirst, want of appetite. Stool hard round black balls like marbles.
Nux vomica
In sedentary persons and those accustomed to drink spirits. Bad taste in the mouth, want of appetite, especially in the morning, slimy tongue, irritability, headache; frequent urging, little or nothing passes
Pulsatilla
After taking rich or fat food; with moroseness also taciturnity.
Bryonia
With indigestion, weight at stomach after food also pain between shoulders; patient irritable, feels chilly, subject to rheumatism. Furthermore, Stool hard, large, light-coloured, and dry.
Lycopodium
Constipation with sadness, complete loss of appetite. Moreover, When there is much flatulence and gravelly urine.
Plumbum met.
Constipation of hard round balls; colic; abdomen drawn in; also constipation of children with large bellies in mesenteric disease
Aesculus hip.
In brief, Constipation of hard round balls, backache aggravated by walking.
Nat. mur
Constipation in chilly subjects; earthy complexion; feeling of contraction at the anus; and as if something were lodged in the rectum (in other words, lower bowel).
Sulphur
Frequent disposition to go to stool with ineffectual efforts. Sinking sensation at stomach, hot flushes, and faintly spells.
Diet & Regimen
Diet & Regimen of Constipation
Regimen and diet for Constipation
Diet
- Fiber is King: Increase both soluble (oats, beans, apples) and insoluble (whole grains, vegetables) fiber gradually to add bulk to stool and promote regularity.
- Hydrate Right: Drink plenty of water and fluids like prune juice to soften stool.
- Focus on Fruits and Veggies: Load up on high-fiber options like berries, pears, broccoli, and leafy greens.
- Choose Whole Grains: Opt for whole-grain bread, pasta, and brown rice over refined grains.
- Limit Problem Foods: Reduce intake of processed foods, red meat, and dairy, which can contribute to constipation.
Regimen for Constipation:
- Establish a Routine: Set a regular time each day to try to have a bowel movement, even if you don’t feel the urge.
- Don’t Delay: When you feel the urge, go to the bathroom promptly.
- Get Moving: Regular physical activity, even a short walk, can stimulate bowel movements.
- Consider Probiotics: Some probiotics may help improve gut health and regularity. Talk to your doctor about the right strains.
- Manage Stress: Stress can affect digestion. Practice relaxation techniques like yoga or meditation.
Do’s and Don'ts
Do’s & Don’ts
Constipation Do’s & Don’ts
Do’s:
- Eat a high-fiber diet. Include plenty of fruits, vegetables, and whole grains in your diet. Aim for 25 to 30 grams of fiber per day.
- Drink plenty of fluids. Fluids help soften stool and make it easier to pass. Aim for eight glasses of water per day.
- Exercise regularly. Exercise helps stimulate bowel movements.
- Go to the bathroom when you have the urge. Don’t delay having a bowel movement when you feel the urge.
- Consider using a fiber supplement. If you can’t get enough fiber from your diet, talk to your doctor about using a fiber supplement.
- Try an over-the-counter laxative. If lifestyle changes don’t help, talk to your doctor about using an over-the-counter laxative.
Don’t:
- Ignore the urge to have a bowel movement. Delaying a bowel movement can make constipation worse.
- Eat a low-fiberdiet. A low-fiber diet can make constipation worse.
- Drink too much caffeine or alcohol. Caffeine and alcohol can dehydrate you, which can make constipation worse.
- Take laxatives too often. Laxatives can be habit-forming. Use them only as directed by your doctor.
- Assume constipation is normal. If you have constipation that lasts for more than a few weeks, or if it’s accompanied by other symptoms, such as blood in your stool or abdominal pain, see your doctor.[10]
Terminology
Terminology
- Atonic Constipation: A type of constipation resulting from weak intestinal muscle tone, often seen in older adults, women with pelvic floor weakness, and diabetics.
- Chronic Constipation: Persistent constipation lasting for extended periods, requiring medication and lifestyle changes.
- Dyschezia: Difficulty passing stool, often associated with pain or discomfort.
- Epidemiology: The study of the distribution and determinants of health-related states or events in specified populations, in this context referring to the prevalence and patterns of constipation.
- Fecal Impaction: A severe form of constipation where a hard mass of stool becomes lodged in the rectum.
- Obstructed Defecation: Difficulty emptying the bowels due to a blockage or narrowing in the rectum or anus.
- Obstipation: Severe constipation characterized by the complete inability to pass stool or gas.
- Obstructive Constipation: Constipation caused by a physical blockage in the intestines, such as tumors, adhesions, or strictures.
- Pathogenesis: The development of a disease or morbid condition, referring here to the mechanisms leading to constipation.
- Pathophysiology: The disordered physiological processes associated with disease or injury, in this case, the abnormal bowel functions causing constipation.
- Peristalsis: The involuntary constriction and relaxation of the muscles of the intestine, creating wave-like movements that push the contents of the canal forward.
- Spastic Constipation: Constipation resulting from intestinal spasms caused by irritation, often associated with irritable bowel syndrome.
- Strictures: Abnormal narrowing of a body passage, in this context referring to narrowing in the intestines.
References
Reference
- https://link.springer.com/journal/12664
- https://www.medicalnewstoday.com/articles/150322.php
- Davidson’s Principles and Practice of Medicine (22nd edition)
- Hompath Zomeo Ultimate lane software/Diet and nutrition
- Constipation physical examination – wikidoc
- Mugie, S. M., Benninga, M. A., & Di Lorenzo, C. (2011). Epidemiology of constipation in children andadults: a systematic review. Best Practice & Research Clinical Gastroenterology, 25(1), 3–18.
- Bharucha, A. E., Dorn, S. D., Lembo, A., & Pressman, A. (2013). Functional Bowel Disorders. Gastroenterology, 140(6), 1510–1525.e3.
- Suares, N. C., & Ford, A. C. (2011). Prevalence of, and risk factors for, chronic idiopathic constipation in the community: systematic review and meta-analysis. American Journal of Gastroenterology, 106(9), 1582–1591.
- Sleisenger and Fordtran’s Gastrointestinal and Liver Disease (11th edition, 2021), edited by Mark Feldman, Lawrence S. Friedman, and Lawrence J. Brandt, published by Elsevier.
- The Mayo Clinic Guide to Digestive Health, 1st Edition, by Sahil Khanna, M.D., 2019.
Also Search As
Also Search As
1. Using the Title:
- Search directly for "Constipation" in the search bar of the website or platform where it is published.
- Include additional keywords like "homeopathic treatment" or "do’s and don’ts" for more specific results.
2. Using Synonyms:
- Try searching for related terms like "costiveness," "irregularity," "bowel dysfunction," or "difficulty passing stool."
3. Using Specific Sections:
- If you remember a specific section, search for terms like "constipation causes," "homeopathic remedies for constipation," or "constipation diet."
4. Using Author or Publication:
- If you know the author’s name or the publication where it was featured, include those in your search.
5. Using Search Engines:
- Search on Google or other search engines using relevant keywords and phrases.
- Use quotes around the phrase "constipation homeopathic treatment" to get more precise results.
Additional Tips:
- Try different combinations of keywords and synonyms.
- Check the "Related Articles" or "Suggested Searches" sections for similar content.
- Consider using advanced search options to filter by date, language, or region.
Frequently Asked Questions (FAQ)
What is Constipation?
Definition
Difficulty in passing stool or passes once in 2 / 3 days, stools can be hard or soft is termed as constipation. Constipation is also defined as infrequent passage of hard stool.
How is constipation diagnosed?
Diagnosis
Doctors usually diagnose constipation based on a patient’s medical history, physical examination, and sometimes additional tests like blood tests or colonoscopy to rule out underlying conditions.
What are the causes of Constipation?
Causes
- Lack of fibers and fluid intake
- Slow-transit constipation
- Irritable bowel syndrome
- Chronic intestinal pseudo-obstruction
- Anorectal disease
- Obstructed defecation
- Opiates, Calcium antagonists, Iron supplements
- Diabetes mellitus, Hypothyroidism
- Pregnancy
- Any serious illness with immobility
What are the symptoms of Constipation?
Symptoms
- Complain of straining
- Sensation of incomplete evacuation
- Either perianal or abdominal discomfort
- Stools every 2nd or 3rd day
- Difficulty in expelling faeces from rectum
- Painful evacuation of faeces
- Pain- remains for hours after passing stool
- Occasional blood
Can homeopathy cure chronic constipation?
Homeopathy has shown promising results in treating chronic constipation by addressing underlying imbalances and promoting overall well-being. However, individual responses may vary, and it’s essential to consult a qualified homeopath for personalized treatment.
Is homeopathic treatment for constipation safe?
Homeopathic remedies are generally considered safe when prescribed by a qualified practitioner. They are highly diluted and unlikely to cause side effects.
What is constipation from a homeopathic perspective?
constipation isn’t just about infrequent bowel movements. It also considers the individual’s overall health, including emotional and mental states, to find a remedy that addresses the root cause.
Are there any complications associated with constipation?
Yes,
chronic constipation can lead to complications like hemorrhoids, anal fissures, fecal impaction, and rectal bleeding.
What are the lifestyle changes that can help relieve constipation?
Lifestyle changes
That can help relieve constipation include increasing fiber intake (through fruits, vegetables, and whole grains), drinking plenty of fluids, exercising regularly, and not ignoring the urge to defecate.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Constipation?
Homoeopathic Medicines For Constipation
- Opium
- Nux vomica
- Pulsatilla
- Bryonia
- Lycopodium
- Plumbum met
- Aesculus