Cushing’s Syndrome
Definition
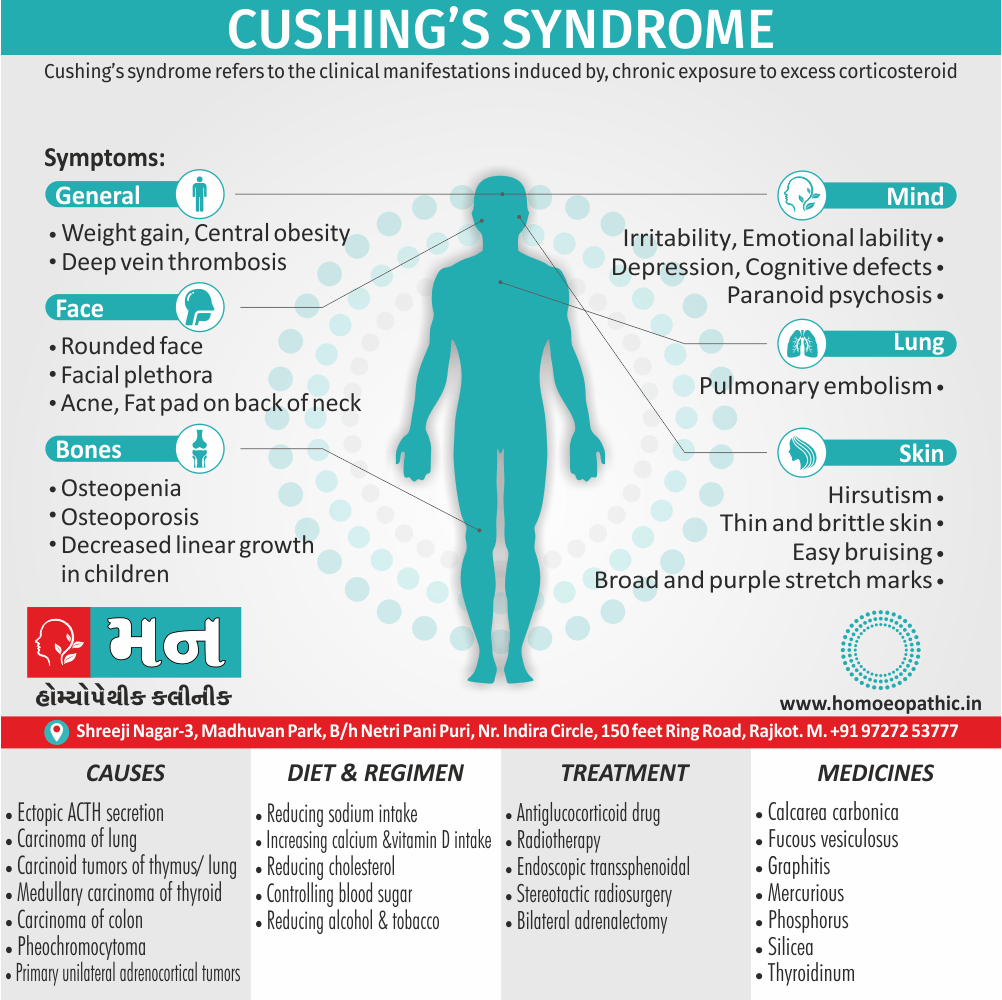
Cushing’s syndrome refers to the clinical manifestations induced by, chronic exposure to excess corticosteroid. [1]
There isn’t a true synonym for Cushing’s syndrome, but it is sometimes referred to by its medical term:
- Hypercortisolism – This term refers to the high levels of cortisol in the body that cause Cushing’s syndrome.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
Basically, Pituitary corticotrope adenomas account for 70% of patients with endogenous causes of Cushing’s syndrome.
However, it should be emphasized that iatrogenic hypercortisolism is the most common cause of cushingoid features.[1]
Epidemiology
Epidemiology
Cushing’s syndrome (CS) is a rare endocrine disorder caused by prolonged exposure to excess cortisol. While global epidemiological data on CS is available, India-specific data is limited.
A study published in 2015, titled "Psychosocial morbidity in Cushing disease: a study from India" investigated the psychological profile of patients with Cushing’s disease (CD) in India. Although the study focuses on the psychological aspect, it provides some insight into the demographics of the disease in India, noting a predominance of females (71.5%) with a mean age at onset of 20.38 years.[9]
Another study, "Pattern of Lipid Abnormalities Among South Asian Indians With Cushing’s Syndrome and the Short Term Impact of Surgical Correction of Hypercortisolism" (2019), while focusing on lipid abnormalities, also mentions that dyslipidemia was less common among Indian subjects with endogenous Cushing’s syndrome.[10]
A recent case report, "Cushing Syndrome Caused by Pituitary and Adrenal Hybrid Tumor: A Rare Case Report" (2023), highlights the challenges in diagnosing and managing CS in India due to its diverse presentation and the need for referral to specialized centers.[11]
While these studies provide some information, there is a lack of comprehensive epidemiological data on CS in India, including its prevalence, incidence, and regional variations. Large-scale studies are needed to understand the true burden of the disease and to develop appropriate diagnostic and treatment strategies for the Indian population.
Causes
Causes of Cushing’s Syndrome
1.Firstly, ACTH excess i.e.: –
- Cushing’s disease Ectopic ACTH secretion
- Carcinoma of lung (especially small cell)
- Carcinoid tumors of either thymus or lung
- Medullary carcinoma of thyroid
- Carcinoma of colon
- Pheochromocytoma
2.Secondly, Non-ACT dependent i.e.: –
- Primary unilateral adrenocortical tumors (either adenoma or carcinoma)
- McCune-Albright syndrome: Bilateral tumor (e.g. Gsα mutation)
- Primary pigmented nodular dysplasia
3. Thirdly, ACTH – independent i.e.: –
- Macronodular adrenal hyperplasia Spontaneous Cushing’s syndrome
Types
Types
There are two types of Cushing’s syndrome.
Exogenous Cushing’s syndrome
Exogenous Cushing’s syndrome is when the cause comes from something outside the body’s function.
It often results from long-term, high-dose usage of corticosteroid drugs, also known as glucocorticoids. These are similar to cortisol.
Examples include:
- prednisone
- dexamethasone
- methylprednisolone
People with rheumatoid arthritis, lupus, asthma, and recipients of an organ transplant may need high doses of these drugs.
Injectable corticosteroids, a treatment for joint pain, back pain and bursitis, can also lead to Cushing’s syndrome.
Steroid medications that do not appear to increase the risk of Cushing’s syndrome are:
The National Institute of Diabetes and Digestive and Kidney Diseases Trusted Source (NIDDK) note that over 10 million people in the United States use glucocorticoid medications each year, but it remains unclear how many develop the symptoms of Cushing’s syndrome.
Endogenous Cushing’s syndrome
Endogenous Cushing’s syndrome is when the cause comes from inside the body, for example, when the adrenal glands produce too much cortisol.
Cushing’s disease is an example of this.
Similar symptoms can also result from adrenal gland tumors or from a benign or malignant tumor in the pancreas, thyroid, thymus gland, or lung. (6)
Risk Factors
Risk factors of Cushing’s Syndrome
- Obesity, type 2 diabetes and poorly regulated blood glucose levels (blood sugar and hypertension)
- The taking of corticosteroid medications (long-term use)
- Pituitary gland tumours
- A primary adrenal gland disease or benign nodular enlargements of the adrenal glands
- An ectopic ACTH-secreting tumour. (4)
Pathogenesis
Pathogenesis
Cushing’s syndrome is a clinical state resulting from chronic exposure to excess glucocorticoids. The excess glucocorticoids may be exogenous (from administration of synthetic glucocorticoids) or endogenous (from overproduction of cortisol by the adrenal cortex).
Pathogenesis of Endogenous Cushing’s Syndrome
ACTH-Dependent Cushing’s Syndrome:
- Cushing’s Disease: In about 80% of endogenous cases, Cushing’s syndrome is caused by excessive secretion of ACTH by a pituitary adenoma. This is called Cushing’s disease. Excess ACTH stimulates the adrenal cortex to produce excessive cortisol.
- Ectopic ACTH Syndrome: In about 10% of endogenous cases, a non-pituitary tumor (e.g., small cell lung cancer) secretes ACTH, again leading to overproduction of cortisol.
ACTH-Independent Cushing’s Syndrome:
- Adrenal Adenomas or Carcinomas: These tumors secrete cortisol autonomously, without the need for ACTH stimulation.
- Primary Pigmented Nodular Adrenocortical Disease (PPNAD): This rare disorder is characterized by small, pigmented nodules in the adrenal cortex that secrete cortisol autonomously.
- Macronodular Adrenal Hyperplasia: This condition is characterized by enlarged adrenal glands with multiple nodules that secrete cortisol autonomously.[12]
Pathophysiology
Pathophysiology
The pathophysiology of Cushing’s syndrome is linked to hypercortisolism which can develop by excess ACTH secretion or excess cortisol secretion by adrenal glands. The underlying mechanisms are usually genetic mutations or overexpression of proteins.
- Excess ACTH secretion
- The excess ACTH secretion can be due to the pituitary adenoma or ectopic (non-pituitary) ACTH secretion. ACTH stimulates the adrenal cortex to release cortisol and is not regulated by the feedback mechanism.
- Pituitary adenoma: Various gene mutations are involved in the development of pituitary adenoma commonly USP8, MEN1, CDKIs, and CDKN1B/p27Kip1. Many proteins are also overexpressed like Brg1, HDAC2, TR4, PTTG, and EGFR. It is the most important cause of ACTH-dependent cushing’s syndrome and is also called cushing’s disease. It is considered that the corticotroph tumors are resistant to glucocorticoid negative feedback inhibition which results in the pathological adrenal cortisol secretion.
- Ectopic ACTH secretion: The molecular defects in the neuroendocrine tumors leading to ectopic ACTH secretion from gastroenteropancreatic tumors are largely unknown. Germline menin mutations or RET oncogene mutations in multiple endocrine neoplasias (MEN) may be responsible. Ectopic secretion of ACTH can be seen as a manifestation of the paraneoplastic syndrome in small cell lung carcinoma and carcinoid tumors(bronchial and thymus).
- The excess ACTH secretion can be due to the pituitary adenoma or ectopic (non-pituitary) ACTH secretion. ACTH stimulates the adrenal cortex to release cortisol and is not regulated by the feedback mechanism.
- Excess secretion of cortisol by adrenal gland
- Excess secretion of the cortisol by the adrenal gland is due to the adrenal causes independent of ACTH secretion.
- Benign Adrenocortical adenoma: Common defects leading to adrenocortical adenoma are mutations or activation of the cAMP-dependent or β-catenin signaling pathways and aberrant expression and function of various G-protein-coupled receptors (GPCR).
- Adrenal cortical carcinoma It is associated with germline TP53 mutations and MEN syndrome.
- Bilateral adrenal hyperplasia: It is associated with MEN1, familial adenomatous polyposis, and fumarate hydratase gene mutations. Several inactivating mutations of armadillo repeat containing 5 genes (ARMC5, chromosome 16p11.2) are also identified.(5)
- Excess secretion of the cortisol by the adrenal gland is due to the adrenal causes independent of ACTH secretion.
Clinical Features
Clinical Features
The clinical manifestations of Cushing’s syndrome are protean and result from the combined effects of chronic exposure to excessive levels of glucocorticoids and the underlying cause.
Common Clinical Features:
- Obesity: Typically central (truncal) with relatively thin extremities; moon facies (round face), and dorsocervical fat pad (buffalo hump).
- Skin Changes: Thinning of the skin with easy bruising, purple striae (stretch marks), impaired wound healing, and increased susceptibility to infections.
- Musculoskeletal: Proximal muscle weakness, osteoporosis, and increased risk of fractures.
- Cardiovascular: Hypertension, dyslipidemia (elevated cholesterol and triglycerides), and increased risk of cardiovascular disease.
- Metabolic: Glucose intolerance or diabetes mellitus, and increased appetite.
- Endocrine: Menstrual irregularities in women, decreased libido, and erectile dysfunction in men.
- Psychiatric: Depression, anxiety, irritability, and cognitive impairment.
Less Common Clinical Features:
- Hirsutism (excess hair growth)
- Acne
- Hyperpigmentation (darkening of the skin)
- Virilization (masculinization) in women
- Growth retardation in children[13]
Sign & Symptoms
Sign & Symptoms of Cushing’s Syndrome
| Body compartment/system | Signs and symptoms |
| Body fat – | Weight gain, central obesity, rounded face, fat pad on back of neck (in other words, “buffalo hump”) |
| Skin – | Facial plethora, thin also brittle skin, easy bruising, broad also purple stretch marks, acne, hirsutism |
| Bone – | Osteopenia, osteoporosis (especially, vertebral fractures), decreased linear growth in children |
| Muscle – | Weakness, proximal myopathy(prominent atrophy of gluteal also upper leg muscles) either with difficulty climbing stairs or getting up from a chair |
| Cardiovascular system – | Hypertension, hypokalemia, edema, additionally atherosclerosis |
| Metabolism – | Glucose intolerance/diabetes, dyslipidemia |
| Reproductive system – | Decreased libido, in women amenorrhea (due to cortisol-mediated inhibition of gonadotropin release) |
| Central nervous system – | Irritability, emotional lability, depression, sometimes cognitive defects; occasionally, in severe cases, overly suspicious psychosis |
| Blood and immune system – | Increased susceptibility to infections, increased white blood cell count, eosinopenia, hypercoagulation with increased risk of deep vein thrombosis also pulmonary embolism. |
[1]
Clinical Examination
Clinical examination
Physical examination of patients with Cushing’s syndrome is as follows:
Appearance of the patient
- Patients with Cushing’s syndrome are usually higher weighter.
Vital signs
- Hypertension, due to cortisol’s enhancement of epinephrine’s vasoconstrictive effect.
Head
- Moon-face is a medical sign where the face swells up into a rounded shape. It is often associated with Cushing’s syndrome, which has led to it being known as Cushingoid facies ("Cushings-like face"), or steroid treatment, which has led to the name steroid facies.
Skin
- Hyperpigmentation – this is due to melanocyte stimulating hormone (MSH) production, as a byproduct of ACTH synthesis from Proopiomelanocortin (POMC)
- Telangiectasia (dilation of capillaries)
- Thinning of the skin (which causes easy bruising)
- Purple or red striae (the weight gain in Cushing’s stretches the skin, which is thin and weakened, causing it to hemorrhage) on the trunk, buttocks, arms, legs or breasts, proximal muscle weakness (hips, shoulders)
- Hirsutism (facial male-pattern hair growth)
Eye
- Bitemporal hemianopsia – pituitary lesion may cause compression of the optic chiasm.
Neck
- Growth of fat pads along the collar bone and on the back of the neck (known as lipodystrophy). (5)
Diagnosis
Diagnosis of Cushing’s Syndrome
- In general, These tests may include increased 24-h urinary free cortisol excretion in three separate collections, failure to appropriately suppress morning cortisol after overnight exposure to dexamethasone, also evidence of loss of diurnal cortisol secretion with high levels at midnight, the time of the physiologically lowest secretion.
- Tests indicating cortisol overproduction i.e.-
- 24-hour urinary cortisol excretion
- Overnight dexamethasone suppression test
- Low-dose dexamethasone suppression test
- High-dose dexamethasone suppression test
- Corticotrophin-releasing hormone test [1]
Differential Diagnosis
Differential Diagnosis
The differential diagnosis of Cushing’s syndrome is broad and includes both endocrine and non-endocrine disorders. The following is a list of the most common conditions that may mimic Cushing’s syndrome:
Endocrine Disorders:
- Pseudo-Cushing’s syndrome: This condition presents with clinical features resembling Cushing’s syndrome but without cortisol excess. It is most commonly associated with obesity, depression, alcoholism, and chronic illness.
- Polycystic ovary syndrome (PCOS): Women with PCOS may have some overlapping features with Cushing’s syndrome, such as obesity, hirsutism, and menstrual irregularities.
- Primary aldosteronism: This condition is caused by excess aldosterone production and can present with hypertension and hypokalemia, which can also be seen in Cushing’s syndrome.
- Pheochromocytoma: This rare tumor of the adrenal gland can cause paroxysmal hypertension and other symptoms that may be mistaken for Cushing’s syndrome.
Non-Endocrine Disorders:
- Obesity: This is a common cause of central obesity and other features that can mimic Cushing’s syndrome.
- Depression: Chronic stress and depression can lead to elevated cortisol levels and some of the clinical manifestations of Cushing’s syndrome.
- Alcoholism: Chronic alcohol abuse can cause pseudo-Cushing’s syndrome.
- Chronic medication use: Certain medications, such as glucocorticoids, can cause iatrogenic Cushing’s syndrome.[14]
Complications
Complications
Untreated or inadequately treated Cushing’s syndrome can lead to a multitude of complications, affecting various organ systems and significantly impacting the patient’s quality of life. These complications are primarily due to the prolonged exposure to excess cortisol.
Common Complications:
- Cardiovascular: Hypertension, atherosclerosis, myocardial infarction, stroke, and congestive heart failure.
- Metabolic: Diabetes mellitus, dyslipidemia (elevated cholesterol and triglycerides), and obesity.
- Musculoskeletal: Osteoporosis, fractures, and muscle weakness (myopathy).
- Infectious: Increased susceptibility to infections due to impaired immune function.
- Neuropsychiatric: Depression, anxiety, cognitive impairment, and psychosis.
- Reproductive: Menstrual irregularities, infertility, and decreased libido.
- Ophthalmologic: Cataracts and glaucoma.
Less Common Complications:
- Nephrolithiasis (kidney stones)
- Pancreatitis
- Peptic ulcer disease
- Avascular necrosis (bone death)[15]
Investigations
Investigations
- Full blood count
- Urea and electrolytes – Hypokalaemia occurs with severe cortisol excess.
- Liver function test
- Bone profile
- Fasting glucose, lipids and glycosylated haemoglobin – Cardiovascular risk is greatly increased in Cushing’s syndrome. Annual risk assessment is therefore mandatory.
- Thyroid stimulating hormone
- Urinary free cortisol
- Low dose dexamethasone suppression test
- Hydroxyprogesterone
- Testosterone, androstenedione, dehydroepiandrosterone, sex hormone binding globulin
- Luteinising hormone, follicle stimulating hormone
- High dose dexamethasone suppression test (7)
Treatment
Treatment of Cushing’s Syndrome
- Basically, Antiglucocorticoid drug.
- Moreover, In ACTH-independent disease, treatment consists of surgical removal of the adrenal tumor.
- The treatment of choice is selective removal of the pituitary corticotrope tumor, usually via an endoscopic transsphenoidal approach.
- Besides this, If pituitary disease recurs, there are several options, including second surgery, radiotherapy, stereotactic radiosurgery, also bilateral adrenalectomy.
- Lastly, In some patients with very severe, overt Cushing’s (e.g., difficult to control hypokalemic either hypertension or acute psychosis), it may be necessary to introduce medical therapy to rapidly control the cortisol excess during the period leading up to surgery. [1]
Prevention
Prevention of Cushing’s Syndrome
- There are no specific methods for prevention of Cushing’s disease.
- Awareness of the symptoms associated with this disease is found to be the most crucial element in order to identify and treat the problem in early stages.
- The treatment depends on the cause of the problem.
- Corticosteroid medications which have caused this syndrome are usually decreased under some medical supervision, while pituitary or adrenal tumor requires surgery.
- To enhance your recovery from this disease, doctors advise sensible eating, using nutritious and wholesome food, with plenty of calcium and vitamin D.
- Take care of your body and soothe aches and pains you might have, but increase your activities slowly.
- Monitor your mental health and if you happen to notice any signs of depression, don’t hesitate to consult your doctor.
- Your brain may also need some exercise, so engage in math problems or crosswords to recover and improve its function.(8)
Homeopathic Treatment
Homeopathic Treatment of Cushing’s Syndrome
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Cushing’s Syndrome
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicine for Cushing’s Syndrome:
Calcarea carbonica:
- Fair, fat, flabby and perspiring also cold, damp and sour. Additionally, Apprehensive.
- Craving for indigestible things – chalk, coal, peanuts.; also, for eggs, salt also sweets. Milk disagrees.
- Ravenous hunger. Besides this, Repugnance to hot food. Wants cold drinks.
- All in all, Loss of appetite when overworked. Palpitation. Weakness. Worse – especially; at night, after eating.
Fucous vesiculosus:
- Especially indicated medicine "For obesity and non – toxic goiter."
- Furthermore, Digestion is furthered and flatulence is diminished, Obstinate constipation.
- Forehead feels as if compressed by iron ring.
- Lastly, Thyroid enlargement in higher weighter subjects.
Graphites:
- Generally, Stout, fair complexion with tendency to skin affections also constipation, fat, chilly and costive.
- Moreover, Tendency to obesity. Aversion to meat. Besides this, Sweets nauseate.
- Hot drinks disagree. Additionally, Burning in stomach causing hunger.
- Worse – warmth, night, during also after menstruation. On the other hand, Better – dark, from wrapping up.
Mercurious:
- Good medicine for Cushing’s Syndrome.
- Bruised pain in small of back, especially when sitting. Tearing pain in coccyx, better pressing on abdomen.
- Extremities – Weakness of limbs, bone-pain alsonin limbs, worse night.
- Patient very sensitive to cold. Additionally, Oily perspiration.
- Trembling extremities, especially hands, paralysis agitans. Specifically, Lacerating pains in joints.
- Cold, clammy sweat on legs at night. Lastly, Dropsical swelling of feet also legs.
Phosphorus:
- Back- Burning in back; especially, pain as if broken, heat between the shoulder blades, Weak spine.
- Extremities- Weakness and trembling from every exertion.
- Can scarcely hold anything with hands. Tibia inflamed also becomes necrosed.
- Arms, hands become numb. All in all, Can lie only right side, joints suddenly give way.
Thyroidinum:
- Specifically indicated medicine for Cushing’s Syndrome.
- Most importantly, Thyroid exercises a general regulating influence over the mechanism of the organs of nutrition, growth and development.
- Another key point is that, Thyroid weakness causes decided craving for large amounts of sweets.
- At last, Excessive obesity. Best with pale patients. Weak; tachycardia; Palpitation from least exertion.
Silicea:
- Back Weak spine, very susceptible to draughts on back. Additionally, Pain in coccyx, diseases of bones of spine.
Capsicum:
- Lax fiber, weak; diminished vital heat. Generally, Fat, indolent, opposed to physical exertion.
- General uncleanliness of body. Especially in Homesickness.
- Worse – while eating, from heat. Whereas; Better – open air, uncovering, draughts.[2]
Diet & Regimen
Diet & Regimen of Cushing’s Syndrome
Regimen and Diet for Cushing Syndrome:
Diet for Cushing Syndrome:
- Control Blood Sugar: Cushing syndrome can lead to high blood sugar. Focus on:
- Low Glycemic Index (GI) Foods: Choose complex carbohydrates like whole grains, legumes, and non-starchy vegetables.
- Limit Sugar and Processed Foods: Reduce intake of sugary drinks, sweets, and processed foods.
- Low Glycemic Index (GI) Foods: Choose complex carbohydrates like whole grains, legumes, and non-starchy vegetables.
- Low Sodium Intake: Limit sodium intake by avoiding processed foods and added salt.
- Potassium-Rich Foods: Include potassium-rich foods like bananas, sweet potatoes, and leafy greens.Manage Blood Pressure: High blood pressure is common in Cushing syndrome.
- Low Sodium Intake: Limit sodium intake by avoiding processed foods and added salt.
- Support Bone Health: Cushing syndrome can weaken bones.
- Calcium and Vitamin D: Ensure adequate intake of calcium (dairy, leafy greens) and vitamin D (fatty fish, fortified foods).
- Calcium and Vitamin D: Ensure adequate intake of calcium (dairy, leafy greens) and vitamin D (fatty fish, fortified foods).
- Protein Power: Maintain muscle mass with adequate protein intake from lean sources like poultry, fish, and beans.
Regimen for Cushing Syndrome:
- Medication Management: Work closely with your doctor to manage medications that may be contributing to Cushing syndrome or to treat its underlying cause.
- Surgery: In some cases, surgery may be necessary to remove a tumor causing Cushing syndrome.
- Radiation Therapy: Radiation therapy may be used to treat tumors that cannot be surgically removed.
- Monitor and Manage Symptoms: Regular checkups and monitoring are essential to manage symptoms and complications of Cushing syndrome.
- Lifestyle Modifications:
- Stress Management: Practice stress-reducing techniques like yoga and meditation.
- Regular Exercise: Engage in regular physical activity as appropriate for your health condition.
- Weight Management: Maintain a healthy weight to reduce strain on your body.
Do’s and Don'ts
The Do’s & Don’ts
Do’s:
- Seek medical attention: If you experience symptoms suggestive of Cushing’s syndrome, consult a healthcare provider promptly for evaluation and diagnosis.
- Follow treatment plan: Adhere to the prescribed treatment plan, which may include medication, surgery, or radiation therapy.
- Monitor blood pressure and glucose: Regularly check blood pressure and blood glucose levels as directed by your doctor.
- Maintain a healthy lifestyle: Eat a balanced diet rich in fruits, vegetables, and whole grains. Engage in regular physical activity as tolerated.
- Manage stress: Practice stress reduction techniques such as yoga, meditation, or deep breathing exercises.
- Communicate with your doctor: Discuss any concerns or side effects of treatment with your healthcare provider.
- Attend regular checkups: Schedule regular follow-up appointments with your endocrinologist to monitor your condition and adjust treatment as needed.
Don’ts:
- Ignore symptoms: Don’t dismiss symptoms as minor or unrelated. Seek medical attention if you experience any changes in your health.
- Self-medicate: Don’t take any medications or supplements without consulting your doctor.
- Stop treatment abruptly: Don’t stop taking prescribed medications or skip appointments without discussing it with your healthcare provider.
- Overexert yourself: Avoid strenuous exercise or activities that may cause injury or strain.
- Consume excessive salt: Limit your intake of salty foods to help manage blood pressure.
- Smoke or drink alcohol: These habits can worsen the complications of Cushing’s syndrome.[16]
Terminology
Terminology
1. Cushing’s Syndrome: A disorder caused by chronic exposure to excess corticosteroids, leading to various clinical manifestations.
2. Hypercortisolism: Another term for Cushing’s syndrome, referring specifically to the high levels of cortisol in the body.
3. Epidemiology: The study of the distribution and determinants of health-related states or events in specific populations, and the application of this study to control health problems.
4. Pathogenesis: The origin and development of a disease.
5. Pathophysiology: The study of the disordered physiological processes associated with disease or injury.
6. Clinical Features: The signs and symptoms observed in patients with a particular condition.
7. Diagnosis: The process of identifying a disease or condition from its signs and symptoms.
8. Differential Diagnosis: The distinguishing of a particular disease or condition from others that present similar clinical features.
9. Complications: Secondary conditions or diseases that develop in the course of a primary disease.
10. Investigations: The diagnostic tests and procedures used to identify the nature and cause of a medical condition.
11. Treatment: The medical care given to a patient for an illness or injury.
12. Prevention: Measures taken to prevent disease or injury.
13. Homeopathic Treatment: A system of alternative medicine that uses small, highly diluted doses of natural substances that in larger amounts would produce symptoms of the ailment in healthy people.
14. Diet & Regimen: The recommended diet and lifestyle modifications for managing a health condition.
15. Do’s and Don’ts: Recommendations and precautions for managing a health condition.
16. Terminology: Specific terms and definitions used in the context of the article.
References
Reference
- Medicine Golwala
- ABC Manual Of Materia Medica And Therapeutics (Therap Part) By Clarke G. H.
- https://www.healthline.com/health/cushings-syndrome#:~:text=Cushing%20syndrome%20can%20lead%20to,high%20blood%20pressure%20(hypertension).
- What risk factors are associated with Cushing’s syndrome? (mymed.com)
- Cushing’s syndrome pathophysiology – wikidoc
- Cushing’s syndrome: Causes, symptoms, types, and diagnosis (medicalnewstoday.com)
- Cushing’s syndrome diagnosis – investigation (endobible.com)
- Prevention of cushing’s disease | Healthy Living articles | Well Being center | SteadyHealth.com
- Psychosocial morbidity in Cushing disease: a study from India 2015.
- Pattern of Lipid Abnormalities Among South Asian Indians With Cushing’s Syndrome and the Short Term Impact of Surgical Correction of hypercortisolism 2019.
- Cushing Syndrome Caused by Pituitary and Adrenal Hybrid Tumor: A Rare Case Report (2023).
- Williams Textbook of Endocrinology.
- Harrison’s Principles of Internal Medicine.
- Greenspan’s Basic & Clinical Endocrinology 11th Edition.
- Endocrinology: Adult and Pediatric 7th Edition.
- The Complete Guide to Cushing’s Syndrome 1st Edition.
Also Search As
Cushing’s Syndrome Also Search As
- Cushing’s syndrome: This is the most obvious and direct search term.
- Hypercortisolism: This is the medical term for Cushing’s syndrome.
- Symptoms of Cushing’s syndrome: This will bring up articles that list the symptoms of the condition.
- Causes of Cushing’s syndrome: This will bring up articles that discuss the causes of the condition.
- Treatment of Cushing’s syndrome: This will bring up articles that discuss the treatment options for the condition.
- Homeopathic treatment of Cushing’s syndrome: This will bring up articles that discuss homeopathic treatment options for the condition.
Other Ways To Search
Within the Document Itself:
- Browser Search (Ctrl+F or Cmd+F): The fastest way if you have the text open. Type in keywords like "Cushing’s," "symptoms," "homeopathy," etc., to jump to relevant sections.
- Table of Contents (If present): Some articles have a clickable TOC at the start, allowing you to navigate by section headings.
- Terminology Section (If present): The article mentions such a section, which may have key terms listed that you could then search for.
If the Article IS Published Online:
- Website Search Bar: Most websites have a search function, use it with the same keywords mentioned above.
- Site-Specific Search Operators: If the site is large, try adding
site:websitename.combefore your keywords in a general search engine (e.g.,site:medicalnewstoday.com Cushing's syndrome homeopathy)
General Web Search:
- Keywords: Use the ones mentioned previously, like "Cushing’s syndrome," its synonyms, or specific aspects you’re interested in (symptoms, causes, etc.).
- Adding Detail: If the initial search is too broad, refine it with things like "homeopathic treatment of Cushing’s syndrome" or "Cushing’s syndrome diet."
- Search Engine Filters: Use tools like date range (to find recent articles) or site type (to focus on medical/health sites) if available on your search engine.
Additional Notes:
- Medical Databases: If you’re in academia or healthcare, search platforms like PubMed or ScienceDirect may have the full article if it’s been formally published.
- Social Media: Some organizations share their articles on platforms like Twitter or Facebook, so you could try searching there using hashtags (#CushingsSyndrome, etc.).
- Ask the Author: If you know who wrote the excerpt, reaching out to them directly might be the most reliable way to get the full article.
Frequently Asked Questions (FAQ)
What is Cushing’s Syndrome?
Definition
Cushing’s syndrome refers to the clinical manifestations induced by, chronic exposure to excess corticosteroid.
What are the symptoms of Cushing’s Syndrome?
- Weight gain
- Central obesity
- Rounded face, fat pad on back of neck (in other words, “buffalo hump”)
- Facial plethora
- Thin also brittle skin
- Osteopenia, Osteoporosis
- Weakness
- Proximal myopathy
- Hypertension
- Hypokalemia
- Edema
- Atherosclerosis
- Irritability, Motional lability, also Depression
What are the causes of Cushing’s Syndrome?
Causes
- Ectopic ACTH secretion
- Carcinoma of lung
- Carcinoid tumors of either thymus or lung
- Medullary carcinoma of thyroid
- Carcinoma of colon
- Pheochromocytoma
- adenoma
- McCune-Albright syndrome
- Primary pigmented nodular dysplasia
- Macronodular adrenal hyperplasia
How is Cushing's Syndrome Diagnosed?
Diagnosis
Diagnosing Cushing’s syndrome involves a series of tests to measure cortisol levels in urine, saliva, and blood. These tests may include a 24-hour urine collection, a dexamethasone suppression test, and blood tests. Imaging scans like MRI or CT scans may also be used to check for tumors.
What are the Treatment Options for Cushing's Syndrome?
Treatment
Treatment depends on the underlying cause of the condition. It may involve reducing or discontinuing corticosteroid medication, surgery to remove tumors, radiation therapy, or medications to control cortisol production.
What are the Long-Term Complications of Cushing's Syndrome?
Complications
If left untreated, Cushing’s syndrome can lead to serious health problems, including heart disease, high blood pressure, type 2 diabetes, infections, and bone loss. Early diagnosis and treatment are essential to prevent complications.
Can Homeopathy Help with Cushing's Syndrome?
Homoeopathic For Cushing’s Syndrome
Homeopathy offers a holistic approach to managing Cushing’s syndrome by focusing on the individual’s unique symptoms and constitution. While homeopathic remedies are not a replacement for conventional medical treatment, they may be used as a complementary therapy to support overall well-being and potentially alleviate some symptoms.
Is Homeopathic Treatment Safe for Cushing's Syndrome?
Homeopathic remedies are generally considered safe when prescribed by a qualified practitioner. However, it’s crucial to inform your homeopath about any other medications or treatments you’re receiving to ensure there are no interactions.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Cushing’s Syndrome?
Homoeopathic Medicines for Cushing’s Syndrome
- Calcarea carbonica
- Fucous vesiculosus
- Graphites
- Mercurious
- Phosphorus
- Thyroidinum
- Silicea
- Capsicum
