Food Poisoning
Definition
Food poisoning, also known as gastroenteritis, is an illness caused by eating contaminated food or water that contains bacteria, parasites, viruses, or toxins. Symptoms can range from mild to serious and can last for a few hours or several days.
Symptoms of food poisoning include:
- Nausea,
- Vomiting,
- Diarrhea,
- Stomach cramps,
- Fever,
- Aching muscles,
- Chills,
- Blurred or double vision,
- Headache, and
- Loss of movement in limbs.
This symptoms usually begin within 1–2 days of eating contaminated food, but can start a few hours later or several weeks later. Most cases are caused by common bacteria such as staphylococcus or E coli.
Acute Diarrhea & Vomiting (Food Poisoning):
Acute Diarrhea & Vomiting are common symptoms that affect people of all ages, from babies also toddlers to adults. In addition, most of the time these two symptoms are the result of a stomach bug or food poisoning and resolve within a couple of days.
Here are some synonyms for food poisoning:
- Foodborne illness: This is a more general term that refers to any illness caused by consuming contaminated food or drink.
- Gastroenteritis: This term refers to inflammation of the stomach and intestines, which is a common symptom of food poisoning.
- Alimentary intoxication: This is a less common term that specifically refers to food poisoning caused by toxins produced by bacteria.
- Foodborne infection: This term refers to food poisoning caused by an infection from bacteria, viruses, or parasites.
- Belly ache: This is a more informal term for stomach pain, which is a common symptom of food poisoning.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
- First of all, Getting some rest and drinking plenty of fluids to avoid dehydration usually the only treatment need. [2]
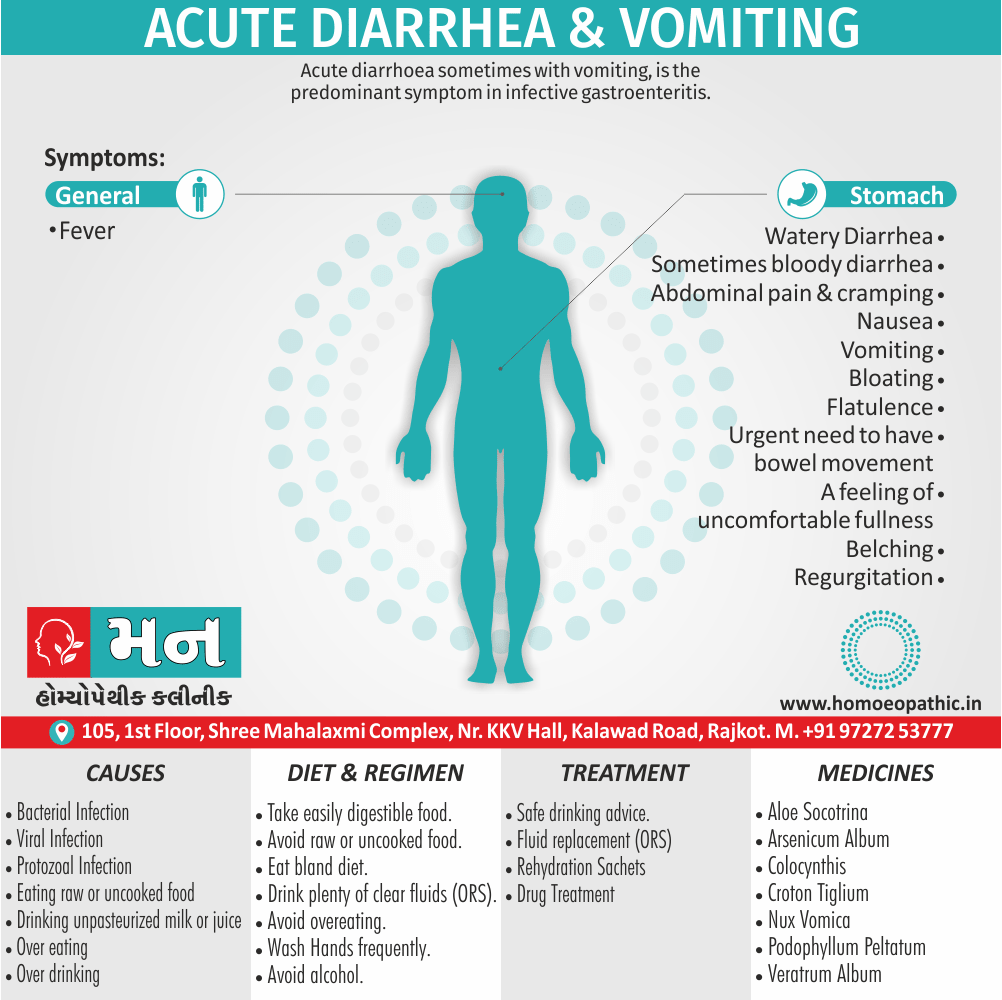
- Moreover, Acute diarrhea, sometimes with vomiting, is the predominant symptom in infective gastroenteritis.
- Acute diarrhea may also a symptom of other infectious and non-infectious diseases.
- Stress, whether psychological or physical, can also produce loose stools.
- The World Health Organization (WHO) estimates that there are more than 1000 million cases of acute diarrhea annually in developing countries, with 3–4 million deaths, half of these in infants and children.
- In developed countries, diarrhea remains an important problem also the people who are older in age are most vulnerable.
- The majority of episodes are due to infections spread by the faecal oral route and transmitted either on fomites, on contaminated hands, or in food or water.
- Measures such as the provision of clean drinking water, appropriate disposal of human and animal sewage, and the application of simple principles of food hygiene can all limit gastroenteritis. [1]
Epidemiology
Epidemiology
In India, the burden of foodborne diseases is not fully known due to underreporting, with most cases going unreported. Outbreaks are often only reported by the media, especially those with high morbidity rates or occurring in urban areas. ("Food-borne Diseases and Food Safety in India," National Centre for Disease Control, 2024).
A variety of foods have been implicated in outbreaks in India, including dairy products, meat, poultry, fish, rice, street foods, and vegetables. ("Food-borne Diseases and Food Safety in India," National Centre for Disease Control, 2024). [5]
The Integrated Disease Surveillance Project (IDSP) has noted an increase in reported food poisoning outbreaks in India, although this may be due to improved reporting rather than an actual increase in incidence. ("Food-Borne Diseases," CD Alert). [6]
Causes
Causes
Toxin in food: < 6 hrs incubation |
|
Bacterial: 12–72 hrs incubation |
|
Viral: short incubation |
|
Protozoal: long incubation |
|
Foods associated with infectious illness, including gastroenteritis:
Raw seafood: |
|
Raw eggs: |
|
Undercooked meat or poultry like: |
|
Unpasteurised milk or juice such as: |
|
Unpasteurised soft cheeses for example: |
|
Homemade canned goods: |
|
Raw hot dogs, pâté: |
|
[1]
These infections can affect adults as well, but there are a number of other reasons why an adult may experience these symptoms simultaneously, such as drinking too much alcohol or being pregnant.
Viral gastroenteritis:
It is an infection in your intestines cause by a virus.
Viral gastroenteritis is often referred to as the stomach flu, but influenza viruses don’t cause these infections.
The viruses that most commonly cause gastroenteritis are like:
- Norovirus
- Rotavirus
- Astrovirus
- Adenovirus
While all of these viruses can affect people of any age, the latter three most often infect infants and toddlers according to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
These viruses are transmit from person to person by contact with infected stool also vomit.
This can happen when an infected person doesn’t wash their hands thoroughly after using the bathroom, after that touches surfaces used by other people or prepares food for others.
Viral gastroenteritis symptoms like:
Food poisoning:
Food poisoning is an infection in your gut caused by bacteria. It means, You get food poisoning by eating contaminated food.
This can happen either at home or in restaurants when food handle incorrectly or not cooked properly.
Several bacteria can cause food poisoning, such as:
- E. coli
- Campylobacter
- Salmonella
- Staphylococcus
- Shigella
- Listeria
Symptoms of food poisoning can start within hours of eating contaminated food and often resolve within a few hours to a few days. Hence, This usually happens without treatment.
Watery diarrhea and vomiting are the most common symptoms of food poisoning.
Other symptoms such as:
- Nausea
- Abdominal cramps and pain
- Bloody diarrhea
- Fever
Traveler’s diarrhea:
Traveler’s diarrhea is a digestive tract disorder that’s most often caused by either viruses, parasites, or bacteria consumed in water or food.
It’s most likely to occur when you’re visiting an area with a different climate or sanitation practices than what you’re accustomed to at home.
This disorder generally clears up within two or three days.
Common symptoms include:
- Watery diarrhea
- Abdominal cramps
- Nausea
- Vomiting
- Flatulence (in other words, gas)
- Bloating
- Fever
- Urgent need to have a bowel movement
Stress or anxiety:
Research shows that gastrointestinal function is influenced by stress and that stress also anxiety commonly cause a number of stomach-related symptoms, For instance:
- Diarrhea
- Nausea
- Vomiting
- Constipation
- Indigestion
- Heartburn
The stress hormones released by your body slow motility in your stomach and small intestines, additionally, it trigger an increase in movement in your large intestine.
Pregnancy:
- Your body goes through numerous changes during pregnancy.
- Morning sickness is the most common cause of vomiting in pregnancy.
- Despite its name, morning sickness can occur at any time of the day. It affects 7 out of 10 pregnant women, usually during the first 14 weeks of pregnancy.
- Some women develop hyperemesis gravidarum, which is a condition that causes severe nausea and vomiting.
- Diarrhea and vomiting in pregnancy can be caused by diet changes, hormonal changes, also new food sensitivities.
- Prenatal vitamins also cause diarrhea in some people.
- These symptoms can also be caused by gastroenteritis, which is common during pregnancy.
Overeating or over drinking:
Overindulging in food or drink can cause diarrhea and vomiting, along with some symptoms for instance:
- A feeling of uncomfortable fullness
- Indigestion
- Belching
- Heartburn
The type of food you eat also matters.
Eating large amounts of greasy or sugary foods can irritate your stomach and cause diarrhea and vomiting.
Overeating is even more likely to cause these symptoms if you already have a gastrointestinal condition, such as IBS, stomach ulcers, acid reflux, and GERD.
Alcohol causes diarrhea by speeding digestion, which stops your colon from absorbing water properly.
However, Even drinking a small amount of alcohol can have this effect.
Excessive alcohol use can cause a condition known as alcoholic gastritis, in other words, it is an irritation of the stomach lining.
Acute gastritis can occur either after binge drinking or become chronic in people who drink alcohol regularly.
Gastritis symptoms for example::
- Upper abdominal pain or burning
- Vomiting and nausea
- Bloating
- Regurgitation
- Symptoms that improve or worsen after eating, depending on the food [2]
Types
Types
The Types of Food Poisoning Covered:
- Bacterial: Salmonella, Campylobacter, Escherichia coli, Listeria monocytogenes, Staphylococcus aureus, Clostridium perfringens, Bacillus cereus, Shigella, Vibrio species, etc.
- Viral: Norovirus, Hepatitis A, Rotavirus
- Parasitic: Toxoplasma gondii, Trichinella spiralis, Cryptosporidium, Giardia
- Toxins: Mycotoxins, algal toxins, plant toxins, animal toxins [7]
Risk Factors
Risk factors of Food Poisoning
Unsafe food sources:
Contaminated raw materials, improper storage or transport, and cross-contamination during preparation can introduce pathogens into food.
Inadequate cooking or reheating:
Insufficient cooking temperatures may not kill harmful bacteria, parasites, or viruses present in food.
Improper holding temperatures:
Holding cooked food at incorrect temperatures can allow bacteria to multiply rapidly.
Poor personal hygiene:
Food handlers who do not wash their hands properly or have infectious diseases can contaminate food.
Contaminated equipment and utensils:
Failure to clean and sanitize food contact surfaces can lead to cross-contamination.
Cross-contamination:
Transfer of pathogens from raw to cooked foods or between different types of food can occur through direct contact, dripping fluids, or contaminated hands or utensils. [8]
Additional Risk Factors
(Not Specifically Mentioned in the Book but Relevant):
- Consumption of raw or undercooked foods, especially meat, poultry, eggs, and seafood.
- Consumption of unpasteurized dairy products or juices.
- Eating food prepared by individuals who are ill or have poor hygiene.
- Eating food that has been left out at room temperature for extended periods.
- Consuming food from unsafe sources, such as street vendors or unlicensed establishments.
Pathogenesis
Pathogenesis
The pathogenesis can vary significantly depending on the type of agent involved:
Bacterial Infections:
- Ingestion: Consumption of contaminated food containing live bacteria.
- Adherence and Colonization: Bacteria adhere to the intestinal lining and multiply.
- Invasion: Some bacteria invade intestinal cells, causing damage and inflammation.
- Toxin Production: Many bacteria produce toxins that act on the intestines, causing symptoms like diarrhea, vomiting, and abdominal pain.
Bacterial Intoxications:
- Ingestion: Consumption of food containing pre-formed toxins produced by bacteria.
- Toxin Action: Toxins directly affect the body, often targeting the nervous system or the gastrointestinal tract. Symptoms can range from mild nausea to severe neurological damage or even death.
Viral Infections:
Parasitic Infections:
- Ingestion: Consumption of contaminated food containing parasites (eggs, cysts, or larvae).
- Maturation: Parasites mature and develop within the host.
- Tissue Invasion: Some parasites invade tissues, causing damage and inflammation.
- Nutrient Depletion: Parasites can compete with the host for nutrients, leading to malnutrition.
Toxins (Non-Infectious):
- Ingestion: Consumption of food containing naturally occurring toxins (mushrooms, plants, etc.) or chemical contaminants.
- Toxic Action: Toxins directly affect the body, targeting specific organs or systems, leading to various symptoms depending on the toxin. [7]
Pathophysiology
Pathophysiology
on the other hand, focuses on the functional changes that occur in the body due to the disease. It explains how the disease disrupts normal physiological processes and how this disruption leads to the signs and symptoms we see.
Imagine a car accident. Pathogenesis would be like understanding how the accident happened – what caused it, the sequence of events (e.g., one car ran a red light, then hit another car). Pathophysiology would be like understanding the damage caused by the accident – the bent fenders, deployed airbags, and any injuries to the passengers.
In simpler terms, pathogenesis is about the "why" of a disease, while pathophysiology is about the "how" of the disease’s effects.
Clinical Features
Clinical Features of Food Poisoning
The clinical features associated with food poisoning, which can vary depending on the causative agent, the amount of toxin ingested, and the individual’s health status. However, some common features include:
Gastrointestinal Symptoms:
- Nausea and Vomiting: Often the earliest symptoms, indicating irritation of the gastrointestinal tract.
- Diarrhea: Can range from mild to severe, watery or bloody, and may be accompanied by abdominal cramps.
- Abdominal Pain: Varies in intensity and location, often described as cramping or a dull ache.
Systemic Symptoms:
- Fever: May be present, indicating an inflammatory response to infection.
- Headache: Can accompany fever or occur independently.
- Muscle Aches and Weakness: May occur in some cases, particularly with infections.
- Dehydration: Can result from severe vomiting and diarrhea, leading to symptoms like dry mouth, thirst, dizziness, and decreased urine output.
Neurological Symptoms:
- Paresthesias: Tingling or numbness in the extremities.
- Visual Disturbances: Blurred vision or double vision.
- Difficulty Swallowing or Speaking: Can occur in severe cases of botulism.
Specific Symptoms Associated with Certain Pathogens:
Important Considerations:
- The incubation period (time from ingestion to onset of symptoms) can vary significantly depending on the causative agent.
- The severity of symptoms can range from mild discomfort to life-threatening illness.
- Some individuals, such as pregnant women, young children, the elders, and immunocompromised individuals, are at higher risk of complications from food poisoning. [9]
Sign & Symptoms
Sign and symptoms of Acute Diarrhea & Vomiting:
- The history should address foods ingested, duration and frequency of diarrhoea, presence of either blood or steatorrhoea, abdominal pain and tenesmus, additionally, other people have been affected.
- Fever and bloody diarrhoea suggest an invasive, colitis, also dysenteric process.
- An incubation period of less than 18 hours suggests toxin-mediated food poisoning, and longer than 5 days suggests diarrhoea caused by protozoa or helminths.
- Person-to-person spread suggests certain infections, such as shigellosis or cholera.
- Examination includes assessment of the degree of dehydration by skin turgor, pulse and blood pressure measurement.
- The urine output and ongoing stool losses should be monitored. [1]
Clinical Examination
Clinical Examination of Food Poisoning
The clinical examination of patients suspected of food poisoning:
History:
- Detailed dietary history: Recent food and water intake, including specific foods, preparation methods, dining locations, and travel history.
- Onset and duration of symptoms: Timing of symptom onset, duration, and progression.
- Nature of symptoms: Specific details about vomiting (frequency, volume, presence of blood), diarrhea (frequency, consistency, presence of blood or mucus), abdominal pain (location, character, severity), and any associated symptoms like fever, headache, muscle aches, or neurological changes.
- Other pertinent information: Recent illnesses, medications, underlying medical conditions, and any other relevant information.
Physical Examination:
- General appearance: Assessment of the patient’s overall condition, including level of alertness, hydration status (dry mucous membranes, decreased skin turgor), and signs of distress.
- Vital signs: Measurement of temperature, blood pressure, heart rate, and respiratory rate to assess for fever, dehydration, or other systemic complications.
- Abdominal examination: Inspection for distension or tenderness, auscultation for bowel sounds, palpation for tenderness or masses, and percussion for tympany or dullness.
- Neurological examination: Assessment of mental status, cranial nerves, motor function, sensory function, and reflexes, especially in cases with suspected neurological complications.
- Other relevant examinations: May include a rectal exam to assess for blood in stool, a skin exam to look for rashes, or other examinations based on the suspected cause of food poisoning.
Important Considerations:
- The clinical examination may not be diagnostic in all cases of food poisoning, and further investigations like stool cultures, blood tests, or imaging studies may be required to confirm the diagnosis and identify the specific causative agent.
- The severity of the clinical presentation can vary widely depending on the type of food poisoning, the amount of toxin ingested, and the individual’s underlying health status.
- The clinical examination should guide the initial management, including supportive care for dehydration and other complications, as well as specific treatments if indicated. [10]
Diagnosis
Diagnosis
These include stool inspection for blood and microscopy for leukocytes, also an examination for ova, cysts and parasites if the history indicates former tropical residence or travel.
Stool culture should perform and C. difficile toxin sought.
FBC and serum electrolytes indicate the degree of inflammation also dehydration.
In a malarious area, a blood film for malaria parasites should be obtained.
Blood and urine cultures and a chest X-ray may identify alternative sites of infection, particularly if the clinical features suggest a syndrome other than gastroenteritis.
Differential Diagnosis
Differential Diagnosis:
Infectious causes such as: |
|
Non-infectious causes: |
Gastrointestinal causes for instance:
Metabolic:
Drugs and toxins such as:
|
| *(5-HT = it means, 5-hydroxytryptamine, serotonin; NSAID = non-steroidal anti-inflammatory drugs; VIP = vasoactive intestinal peptide) |
[1]
Complications
Complications of Food Poisoning
Food poisoning, while often a temporary inconvenience, can occasionally lead to severe complications, particularly in vulnerable populations. These complications can arise due to the body’s response to the toxins or pathogens ingested, or from the resulting dehydration and electrolyte imbalances.
Dehydration:
This is the most common complication. Vomiting and diarrhea, hallmarks of food poisoning, lead to significant fluid loss. If not replenished, dehydration can cause electrolyte imbalances, impairing vital bodily functions. Severe dehydration can be fatal, especially in children, the elders, and those with compromised immune systems.
Hemolytic Uremic Syndrome (HUS):
Certain strains of E. coli, a common culprit in food poisoning, can cause HUS. This life-threatening condition damages blood cells and kidneys, potentially leading to kidney failure. Young children are particularly susceptible.
Reactive Arthritis:
Some foodborne pathogens, like Salmonella and Campylobacter, can trigger reactive arthritis. This inflammatory condition affects joints, causing pain, swelling, and stiffness. While usually temporary, it can become chronic in some cases.
Guillain-Barré Syndrome (GBS):
Rarely, Campylobacter infection can lead to GBS. This serious autoimmune disorder attacks the peripheral nervous system, causing muscle weakness and paralysis. Most people recover, but some experience long-term effects.
Neurological Complications:
Listeria, a bacterium found in certain foods, can cause meningitis and encephalitis, inflammation of the membranes surrounding the brain and spinal cord. These conditions can lead to long-term neurological damage, particularly in newborns and the elders. [11]
Investigations
Investigations
These include stool inspection for blood and microscopy for leukocytes, also an examination for ova, cysts and parasites if the history indicates former tropical residence or travel.
Stool culture should perform and C. difficile toxin sought.
FBC and serum electrolytes indicate the degree of inflammation also dehydration.
In a malarious area, a blood film for malaria parasites should be obtained.
Blood and urine cultures and a chest X-ray may identify alternative sites of infection, particularly if the clinical features suggest a syndrome other than gastroenteritis.
Treatment
Treatment of Acute Diarrhea & Vomiting:
Firstly, All patients with acute, potentially infective diarrhoea should be appropriately isolated to minimise person to person spread of infection.
Secondly, If the history suggests a food-borne source, public health measures must be implemented to identify the source and to establish whether other linked cases exist.
Fluid replacement:
Replacement of fluid losses in diarrhoeal illness is crucial and may be life-saving.
Although normal daily fluid intake in an adult is only 1–2 L, there is considerable additional fluid movement in and out of the gut in secretions.
Altered gut resorption with diarrhoea can result in substantial fluid loss, e.g. 10–20 L of fluid may be lost in 24 hours in cholera.
The fluid lost in diarrhoea is isotonic, so both water and electrolytes need to be replaced. However, Absorption of electrolytes from the gut is an active process requiring energy.
Infected mucosa is capable of very rapid fluid and electrolyte transport particularly, if carbohydrate is available as an energy source.
Oral rehydration solutions (ORS) therefore contain sugars, as well as water and electrolytes. In addition, ORS can be just as effective as intravenous replacement fluid, even in the management of cholera.
In mild to moderate gastroenteritis, adults should be encouraged to drink fluids also, if possible, continue normal dietary food intake.
If this is impossible, e.g. due to vomiting, intravenous fluid administration will be required.
In very sick patients, or those with cardiac or renal disease, monitoring of urine output also central venous pressure may be necessary.
The volume of fluid replacement required should be estimated based on the following considerations. for instance,
Established deficit Replacement:
- After 48 hours of moderate diarrhoea (6–10 stools per 24 hours), however, the average adult will be 2-4 L depleted from diarrhoea alone.
- Associated vomiting will compound this.
- Adults with this symptomatology should therefore be given rapid replacement of 1–1.5 L, either orally (ORS) or by intravenous infusion (normal saline), within the first 2–4 hours of presentation.
- Longer symptomatology or more persistent/severe diarrhoea rapidly produces fluid losses comparable to diabetic ketoacidosis and is a metabolic emergency requiring active intervention.
Replacement of ongoing losses:
- The average adult’s diarrhoeal stool accounts for a loss of 200 ml of isotonic fluid.
- Stool losses should be carefully charted also an estimate of ongoing replacement fluid calculated.
- Commercially available rehydration sachets are conveniently produced to provide 200 ml of ORS; In addition, one sachet per diarrhoea stool is an appropriate estimate of supplementary replacement requirements.
Replacement of normal daily requirement:
- The average adult has a daily requirement of 1–1.5 L of fluid in addition to the calculations above.
- This will be increased substantially in fever or a hot environment.
Antimicrobial agents:
- In non-specific gastroenteritis, antibiotics have been shown to shorten symptoms by only 1 day in an illness usually lasting 1–3 days.
- This benefit, when related to the potential for the development of antimicrobial resistance or side-effects, does not justify treatment, except if there is systemic involvement, a host with immunocompromised or significant comorbidity.
- Evidence suggests that, in EHEC infections, the use of antibiotics may make the complication of haemolytic uraemic syndrome (HUS) more likely due to increased toxin release.
- Antibiotics should therefore not be used in this condition.
- Conversely, antibiotics are indicated in Sh. dysenteriae infection and in invasive salmonellosis in particular, typhoid fever.
- Antibiotics may also be advantageous in cholera epidemics, reducing infectivity and controlling the spread of infection.
Antidiarrhoeal, antimotility and antisecretory agents:
- These agents are not usually recommended in acute infective diarrhoea.
- Loperamide, diphenoxylate and opiates are potentially dangerous in dysentery in childhood, as a result, intussusception.
- Antisecretory agents, such as bismuth and chlorpromazine, may be effective but can cause significant sedation.
- They do not reduce stool fluid losses, although the stools may appear more bulky.
- Adsorbents, such as kaolin or charcoal, have little effect. [1]
Prevention
Prevention of Food Poisoning
Safe Food Handling:
- Clean: Wash hands thoroughly with soap and water before and after handling food. Clean surfaces, utensils, and cutting boards with hot soapy water after each use, especially after contact with raw meat, poultry, or seafood.
- Separate: Prevent cross-contamination by using separate cutting boards and utensils for raw and cooked foods. Store raw meat, poultry, and seafood on the bottom shelf of the refrigerator to prevent juices from dripping onto other foods.
- Cook: Cook food to the proper internal temperature to kill harmful bacteria. Use a food thermometer to ensure thorough cooking.
- Chill: Refrigerate perishable foods promptly and thaw frozen foods in the refrigerator or microwave. Don’t leave perishable foods at room temperature for extended periods.
Additional Tips:
- Wash produce: Wash fruits and vegetables thoroughly under running water, even if you plan to peel them.
- Avoid raw or undercooked foods: Be cautious of raw or undercooked meat, poultry, seafood, and eggs, as they are more likely to harbor harmful bacteria.
- Pasteurized products: Choose pasteurized milk, cheese, and other dairy products to minimize the risk of bacterial contamination.
- Safe water: Drink safe water from a reliable source or treat it if unsure of its safety.
- Travel precautions: When traveling to areas with different hygiene standards, be cautious of food and water sources. Stick to cooked foods, bottled water, and avoid raw fruits and vegetables that cannot be peeled.
By following these guidelines and practicing safe food handling habits, you can significantly reduce your risk of food poisoning and enjoy meals safely.
Homeopathic Treatment
Homoeopathic Treatment
Acute diarrhea & vomiting is natural, safe and without any side-effects. In addition, one can enjoy immense relief from these frustrating symptoms.
It is a patient-oriented science additionally, medicines are prescribed on the characteristics of the individual instead of just the symptoms of the disease.
These medicines help in boosting the self-healing mechanism of the body also fight the infection.
They help control the symptoms of food poisoning particularly, speeding up the recovery process.
Homeopathic medicine such as, Arsenic Album the first aid medicine use in food poisoning cases.
It can be taken in 30C potency three to four times a day, but depending upon the severity of symptoms.
It helps control symptoms including diarrhea, nausea, also vomiting.
Arsenic Album
- Arsenic Album is a highly recommended homeopathic medicine for food poisoning, also known as the ‘homeopathic first aid’ for food poisoning.
- Food poisoning with diarrhea, nausea, additionally, vomiting is indicative of using this medicine.
- Vomiting may contain either clear water or thick glairy mucus.
- If the person eats anything, as a result, vomited out quickly.
- The stool is loose, foul smelling, also is attended with weakness.
- Burning pain in the abdomen may be present.
- In conclusion, Frequent thirst for water at short intervals is usually present.
Veratrum Album
- Firstly, Veratrum Album is a homeopathic medicine prepared from a plant named ‘white hellebore.’
- Secondly, It belongs to the family Liliaceae.
- Moreover, Veratrum Album is a beneficial homeopathic medicine for food poisoning where there is copious vomiting.
- In addition, Even the smallest amount of water gets vomited, and excessive weakness follows the vomiting.
- Along with this, nausea and copious loose stool may be present.
- At last, The body may feel cold, apart from the above symptoms.
Aloe Socotrina
- Aloe is a natural homeopathic medicine prepared from plant Aloe Socotrina. Moreover, The natural order of this plant is Liliaceae.
- Particularly, It is indicated in cases of food poisoning with marked diarrhea.
- The stool is watery, also there is an urgent need to pass it.
- Rumbling and gurgling in the rectum is present, additionally, a constant bearing down is felt in the rectum.
Colocynthis
- Colocynthis is a homeopathic medicine prepared from a plant called ‘bitter cucumber.’ In addition, It belongs to the plant family Cucurbitaceae.
- Colocynthis is considered for food poisoning when marked abdominal cramps are present.
- Apart from cramping, the medicine is also indicated when cutting, colicky pains in the abdomen are present.
- Either Bending double or pressing the stomach helps relieve the pain.
- The pain tends to worsen from slight eating or drinking.
- Along with this loose stool, vomiting and nausea are also present.
China Officinalis
- Homeopathic medicine China Officinalis is prepared either from the Peruvian bark or the Cinchona tree that belongs to the natural order Rubiaceae.
- It is a well-indicated homeopathic medicine for food poisoning with diarrhea also extreme weakness.
- The stool is watery, foul, and painless with marked exhaustion also debility.
- Excessive flatulence may be present, and the abdomen may be bloated.
- China is also a well-indicated medicine for food poisoning that occurs from the consumption of bad meat, unripe fruit, and bad water.
- It is also indicated for traveler’s diarrhea.
Nux Vomica
- Nux Vomica is a prominent homeopathic medicine for food poisoning with excessive retching in other words, efforts to vomit.
- The person in such a case wants to vomit but cannot.
- A frequent ineffectual urge to pass the stool is present.
- The person may attempt to pass stool frequently but is only able to expel small quantities.
- Loud, rumbling, gurgling sounds in the abdomen may be present along with the above symptoms.
Ipecac
- Homeopathic medicine Ipecac is prepared from the ipecac root, which belongs to the natural order Rubiaceae.
- In addition, Ipecac is used to treat food poisoning accompanied by intense nausea and vomiting.
- The nausea is present all the time.
- Vomiting appears, but it does not relieve nausea.
- Particularly, Vomiting of watery fluids, green mucus, or blackish matter may be present.
- A frothy stool and pain around navel are often noted with the above symptoms.
Croton Tiglium
- Croton Tig is a significant homeopathic medicine for food poisoning.
- Hence, its chief indicating features are copious, watery, and gushing stool.
- The urge to pass stool is constant, additionally, stool pass suddenly with great force in one gush.
- Colic before passing stool is also present.
Podophyllum Peltatum
- Firstly, Homeopathic medicine Podophyllum Peltatum a plant-base medicine prepared from Mayapple (Podophyllum).
- Secondly, The plant belongs to family Berberidaceae.
- Furthermore, The characteristic features to use this medicine are a profuse, offensive, yellowish or greenish stool.
- At last, Fetid flatus, mucus in the stool, also vomiting of hot, frothy mucus may also be present.
Elaterium Officinarum
- Elaterium Officinarum a natural medicine prepare from a plant commonly named as the Squirting Cucumber. In addition, It belongs to the natural order Cucurbitaceae.
- Elaterium Officinarum is a valuable homeopathic medicine for food poisoning with violent vomiting also diarrhea.
- The stool is copious, watery, forceful, greenish, also frothy.
- At last, Cutting pain in the abdomen may be present.
Zingiber Officinale
- Zingiber Officinale prepare from the dried root of ginger, which belongs to the natural order Zingiberaceae.
- It is a particularly, indicated homeopathic medicine for food poisoning contracted by drinking impure water.
- Diarrhea with excessive flatulence and colic, heaviness and rumbling in the stomach, and belching are the primary symptoms so, that indicate the need for this medicine.
- It is also suited for diarrhea that results from eating melons. [4]
Diet & Regimen
Diet & Regimen
When recovering from food poisoning, the diet and regimen play a crucial role in easing symptoms, replenishing lost fluids, and promoting a speedy recovery. Here’s what you should focus on:
Hydration:
The cornerstone of food poisoning recovery is rehydration. Vomiting and diarrhea can lead to significant fluid loss, so replenishing them is vital. Start with small sips of:
- Clear liquids: Water, clear broth, herbal tea, diluted fruit juice (without pulp), and oral rehydration solutions (ORS) like Pedialyte or homemade solutions with salt, sugar, and water.
As your symptoms improve, gradually increase fluid intake.
Bland Diet (BRAT):
Once vomiting subsides, you can introduce the BRAT diet, which consists of:
- Bananas: Easy to digest and provide potassium.
- Rice: Plain, white rice is gentle on the stomach and provides energy.
- Applesauce: Provides pectin, which may help firm stools.
- Toast: Plain, dry toast is easy to digest and can help settle the stomach.
These foods are bland, low in fiber, and less likely to irritate the digestive system.
Probiotics:
Probiotics, found in yogurt or supplements, may help restore the balance of good bacteria in the gut and aid digestion.
Foods to Avoid:
During recovery, avoid the following:
- Dairy products: Milk, cheese, and ice cream can worsen diarrhea.
- Fatty or fried foods: Difficult to digest and can irritate the stomach.
- Spicy foods: Can worsen nausea and diarrhea.
- Caffeine and alcohol: Dehydrating and can irritate the stomach.
- High-fiber foods: Whole grains, raw fruits, and vegetables can be hard to digest.
Rest:
Adequate rest is essential for recovery. Your body needs energy to fight off the infection and heal.
Gradual Reintroduction of Normal Diet:
As you feel better, gradually reintroduce other foods into your diet, starting with easily digestible options like cooked vegetables, lean protein, and plain crackers.
Do’s and Don'ts
Do’s and Don’ts
Food Poisoning do’s and don’ts
Do’s:
- Firstly, Try sucking ice cubes or icy poles if you are having trouble keeping fluids down.
- Secondly, Regularly drink small amounts of water to prevent dehydration once the vomiting has stopped.
- After that, Drink oral re hydration drinks such as Gastrolyte (available from pharmacies).
- Then, If you feel like eating, eat bland foods such as crackers, rice or dry toast.
- Rest while you feel unwell.
- Complete any medications prescribed by your doctor.
- Wash hands diligently after using the toilet and prior to eating. In Addition, Thoroughly clean and disinfect contaminated surfaces immediately after an episode of illness by using a bleach-based household cleaner.
- Immediately remove and wash any either clothes or bedding contaminated with vomit or diarrhea using soap and hot water.
- When travelling overseas, drink and brush your teeth with bottled water. In addition, Try to avoid raw foods and only eat well cooked meats.
- At last, Drink lots of clear fluids like water, broth, clear sodas, also sports drinks.
Don’ts:
- Do not take anti-diarrhea medications without advice from doctor.
- After that, Avoid drink alcohol, carbonated drinks or eat spicy foods.
- Avoid smoke cigarettes also take recreational drugs.
- Don’t go to work or school for at least 24 hours after symptoms have stopped
- Do not Handle or prepare food for others for at least 24 hours after symptoms have stopped. [3]
Terminology
Terminology
Food poisoning (Foodborne Illness):
A general term referring to illness caused by consuming contaminated food or drink. It can be caused by bacteria, viruses, parasites, or toxins.
Contamination:
The presence of harmful substances, such as bacteria, viruses, parasites, or toxins, in food or drink.
Pathogen:
A microorganism (bacteria, virus, or parasite) that can cause disease.
Toxin:
A poisonous substance produced by certain living organisms, such as bacteria, fungi, or plants.
Incubation period:
The time between consuming contaminated food and the onset of symptoms.
Gastroenteritis:
Inflammation of the stomach and intestines, often a symptom of food poisoning.
Dehydration:
A dangerous condition resulting from excessive loss of body fluids, often due to vomiting and diarrhea.
Electrolytes:
Minerals in the body that carry an electric charge and are essential for various bodily functions. Imbalances can occur due to dehydration.
Hemolytic Uremic Syndrome (HUS):
A serious complication of E. coli infection that can lead to kidney failure.
Reactive Arthritis:
A type of arthritis that can be triggered by certain foodborne infections.
Guillain-Barré Syndrome (GBS):
A rare neurological disorder that can be triggered by Campylobacter infection.
Cross-contamination:
The transfer of harmful microorganisms from one food to another, typically from raw to cooked food.
Pasteurization:
A process of heating food (e.g., milk) to a specific temperature to kill harmful bacteria.
Safe food handling:
Practices that reduce the risk of food contamination and food poisoning.
Symptoms & Conditions:
- Nausea/Vomiting: Common early signs of food poisoning.
- Diarrhea: Can range from mild to severe, watery, or bloody.
- Abdominal pain/Cramps: Often present with varying intensity.
- Fever: May indicate a more serious infection.
- Headache, Weakness, Fatigue: Can occur as the body fights the infection.
- Neurological symptoms: In some cases, food poisoning can cause tingling, numbness, or paralysis (e.g., from botulism or ciguatera poisoning).
Medical Interventions:
- Rehydration therapy: Essential to replace lost fluids and electrolytes.
- Antiemetics: Medications to reduce nausea and vomiting.
- Antidiarrheals: Medications to control diarrhea (use with caution, as they can sometimes prolong the illness).
- Antibiotics: In specific cases of bacterial infection.
- Antiparasitic drugs: If the cause is a parasite.
Other Relevant Terms:
- Fecal-oral transmission: The most common route of foodborne illness transmission.
- Outbreak: When two or more people get the same illness from the same contaminated food or drink.
- Food recall: Action taken to remove contaminated food from the market.
- HACCP (Hazard Analysis and Critical Control Points): A preventive system to ensure food safety.
In homeopathic articles about food poisoning, you might encounter some specific terminologies related to homeopathic principles and practice. Here are some key terms and their meanings:
- Vital force: The fundamental energy or life force that animates living beings and maintains health. Homeopathy aims to stimulate the vital force to promote healing.
- Law of Similars: The central principle of homeopathy, stating that a substance that can cause symptoms in a healthy person can cure similar symptoms in a sick person.
- Remedy: A homeopathic medicine, usually highly diluted and potentized substances, chosen based on the law of similars to address specific symptoms.
- Potency: The degree of dilution and succussion (vigorous shaking) a homeopathic remedy undergoes. Higher potencies are considered to have a deeper and longer-lasting effect.
- Proving: A systematic process of testing a substance on healthy individuals to determine the symptoms it can produce, which then guides its use as a remedy.
- Aggravation: A temporary worsening of symptoms after taking a remedy, often considered a positive sign of the body’s response to treatment.
- Constitutional type: The individual’s unique physical and mental characteristics, which guide the selection of homeopathic remedies for overall health and well-being.
- Miasm: Inherited predispositions or tendencies towards certain diseases, considered an important factor in homeopathic treatment.
- Nosode: A homeopathic remedy prepared from diseased tissue or products (e.g., bacteria, viruses) and used to treat similar conditions.
References
References
- Davidson’s Principles and Practice of Medicine (22nd edition) Ch. 13
- https://www.healthline.com/health/diarrhea-and-vomiting#causes
- https://healthywa.wa.gov.au/Articles/A_E/Diarrhoea-and-vomiting
- https://www.drhomeo.com/homeopathic-treatment/homeopathic-medicine-for-food-poisoning/
- "Food-borne Diseases and Food Safety in India," National Centre for Disease Control, 2024
- "Food-Borne Diseases," CD Alert (no publication year provided)
- Foodborne Infections and Intoxications(4th edition), by Hans Riemann and Dean O. Cliver (2006), Published by Elsevier
- Control of Communicable Diseases Manual (20th edition) , by David L. Heymann, 2014, Published by American Public Health Association
- Harrison’s Principles of Internal Medicine (19th edition), by Dennis L. Kasper, Anthony S. Fauci, Stephen L. Hauser, Dan L. Longo, J. Larry Jameson, Joseph Loscalzo (2015), Published by McGraw-Hill Education
- Tintinalli’s Emergency Medicine: A Comprehensive Study Guide (9th edition) (2020) by Judith E. Tintinalli, J. Stephan Stapczynski, O. John Ma, Donald M. Yealy, Garth D. Meckler, David M. Cline
- Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases (9th Edition) by John E. Bennett, Raphael Dolin, Martin J. Blaser (2020)
Also Search As
Also Search As
There are several ways people can search for homeopathic articles on food poisoning:
Online Search Engines:
- Use specific keywords: Search for phrases like "homeopathy for food poisoning," "homeopathic remedies for food poisoning," or "homeopathic treatment for foodborne illness."
- Include reputable sources: Add terms like "National Center for Homeopathy," "Homeopathic Educational Services," or names of well-known homeopathic practitioners or organizations to your search.
Homeopathic Websites and Blogs:
- Visit the websites of homeopathic organizations: Look for articles, blogs, or resource sections on their websites.
- Follow homeopathic blogs: Many homeopathic practitioners and enthusiasts maintain blogs where they share information and experiences.
Homeopathic Libraries and Resource Centers:
- Visit local homeopathic libraries: Many homeopathic schools or clinics have libraries with resources on various topics, including food poisoning.
- Contact homeopathic organizations: They may have online or physical resource centers where you can access articles and information.
Consult a Homeopathic Practitioner:
- Seek professional guidance: A qualified homeopathic practitioner can provide personalized advice and recommend relevant articles or resources based on your specific situation.
There are several ways to search for information on food poisoning, depending on your needs and the type of information you’re seeking:
Search Engines:
- Use search engines like Google, Bing, or DuckDuckGo and enter keywords like "food poisoning," "foodborne illness," "food poisoning symptoms," "food poisoning treatment," or specific food-related illnesses (e.g., "salmonella poisoning"). This will provide a wide range of results, including articles, news, websites, and medical resources.
Homeopathic Journals and Publications:
Search online databases: Platforms like PubMed or Google Scholar may have indexed homeopathic journals where you can find relevant articles.
Subscribe to homeopathic journals: Consider subscribing to publications like "The Homeopathic Journal" or "Homeopathy" for access to research and case studies.
Health and Medical Websites:
- Reputable health websites like the Centers for Disease Control and Prevention (CDC), Mayo Clinic, World Health Organization (WHO), or government health departments often have dedicated sections on food poisoning, providing comprehensive information on symptoms, causes, treatment, and prevention.
Medical Encyclopedias:
- Online medical encyclopedias like MedlinePlus, WebMD, or the Merck Manual can offer in-depth information on food poisoning, its various forms, and related medical conditions.
Academic Databases:
- If you’re a researcher or student, you can use academic databases like PubMed or Google Scholar to search for scientific articles, research papers, and clinical studies on food poisoning.
Government Resources:
- Many government agencies, such as the Food and Drug Administration (FDA) or the U.S. Department of Agriculture (USDA), have resources on food safety and foodborne illnesses, including recalls, alerts, and prevention tips.
Social Media:
- Social media platforms like Twitter or Facebook can be used to follow health organizations, experts, or news outlets that share information on food poisoning outbreaks, recalls, or prevention campaigns.
Consult a Healthcare Professional:
- If you’re experiencing symptoms of food poisoning or have concerns about a specific food item, it’s always best to consult a doctor or healthcare provider for personalized advice and treatment.
Frequently Asked Questions (FAQ)
What is Food Poisoning?
Acute Diarrhea & Vomiting are common symptoms that affect people of all ages, from babies also toddlers to adults. In addition, most of the time these two symptoms are the result of a stomach bug or food poisoning and resolve within a couple of days.
How can I treat food poisoning at home?
Rest, stay hydrated, and consider over-the-counter medications for symptom relief. If symptoms are severe, seek medical attention.
Best things to eat after Food Poisoning?
- Eat bland foods (crackers, rice or dry toast.)
- Try to avoid raw foods
- Only eat well cooked meats.
- Drink lots of clear fluids
- Avoid drink alcohol, eating spicy foods.
What are the symptoms of Food Poisoning?
- Acute Diarrhea & Vomiting
- Abdominal pain and tenesmus
- Fever and bloody diarrhoea
- Steatorrhoea
- Dehydration by skin turgor
When should I see a doctor for food poisoning?
Consult a doctor if you have bloody stools, high fever, dehydration, or symptoms that don’t improve.
Are homeopathic remedies safe for food poisoning?
When used correctly under professional guidance, homeopathic remedies are generally safe and have no known side effects.
What is the homeopathic approach to food poisoning?
Homeopathy focuses on treating the individual and their unique symptoms rather than just suppressing the illness.
Which homeopathic remedies are commonly used for food poisoning?
Remedies like Arsenicum album (for burning pains and anxiety), Nux vomica (for nausea and irritability), Pulsatilla (for changeable moods and aversion to fatty foods), and Carbo vegetabilis (for bloating and gas) are often recommended.
Can I use homeopathic remedies alongside conventional treatments for food poisoning?
It’s best to discuss this with both your homeopathic practitioner and your conventional doctor to ensure a safe and effective treatment plan.
Homeopathic Medicines use by Homeopathic Doctors in treatment of Food Poisoning?
Homeopathic Medicines for Food Poisoning
- Arsenicum Alb
- Veratrum Alb
- Aloe Socotrina
- Colocynth
- China
- Nux Vomica
- Croton Tig
- Podophyllum
