Hepatitis A
Definition
Acute viral hepatitis is a systemic infection affecting the liver predominantly caused by five well-characterized hepatotropic viruses, which are designated hepatitis A, B, C, D and E. [1]
Here are some synonyms for Hepatitis A:
Infectious hepatitis:
This term refers to the fact that the virus is contagious and can be spread from person to person.
Epidemic hepatitis:
This term highlights that Hepatitis A can sometimes cause outbreaks, particularly in areas with poor sanitation.
Type A hepatitis:
This term distinguishes Hepatitis A from other types of viral hepatitis, such as Hepatitis B and C.
Catarrhal jaundice:
This is an older term that refers to the yellowing of the skin and eyes (jaundice) that can be a symptom of Hepatitis A.
Overview
Epidemiology
Transmission
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Hepatitis A
Hepatitis A virus (HAV), hepatitis B virus (HBV), hepatitis C virus (HCV), the HBV-associated delta agent or hepatitis D virus (HDV), and hepatitis E virus (HEV). All these human hepatitis viruses are RNA viruses, except for hepatitis B, which is a DNA virus but replicates like a retrovirus.
Although these agents can be distinguished by their molecular and antigenic properties, all types of viral hepatitis produce clinically similar illnesses. These range from asymptomatic and inapparent to fulminant and fatal acute infections common to all types, on the one hand, and from subclinical persistent infections to rapidly progressive chronic liver disease with cirrhosis and even hepatocellular carcinoma, common to the bloodborne types (HBV, HCV, also HDV), on the other. [2]
Acute viral hepatitis
it’s may be asymptomatic, marked only by an increase in aminotransferase levels, or symptomatic with or without jaundice or sub fulminant or fulminant depending on the causative agent.
Though the natural history of acute hepatitis can vary according to the etiological agent, it can be divided as follows depending on clinical features and laboratory findings:
Prodromal period
- Bilirubinuria appears earlier than a rise in serum bilirubin.
- Serological viral markers help in arriving at a diagnosis.
- Urobilinogen and total bilirubin rise occur before clinical jaundice.
- Liver enzymes AST and ALT are > 500 units
- Leucopaenia may be observed with onset of fever.
Acute icteric stage
- Bilirubin rises, plateaus and then gradually decreases.
- Serum AST and ALT rise and fall rapidly and reach normal range in 2 to 5 weeks.
- ESR is raised initially and falls during convalescence
Defervescent stage
- Diuresis occurs at onset of convalescence.
- Bilirubinuria disappears, serum bilirubin is still increased.
- Urine urobilinogen increases.
- bilirubin becomes normal after 3 to 6 weeks [1]
Epidemiology
Epidemiology:
The epidemiology of Hepatitis A in India has shown a shift in recent years. While historically, most infections occurred in childhood and were often asymptomatic, there is now an increasing number of cases in adolescents and adults, resulting in more symptomatic disease. This is likely due to improved sanitation and hygiene, leading to less exposure and therefore less immunity in childhood.
Reference:
- Viral Hepatitis Surveillance — India, 2011–2013 (published in 2015 by the CDC) mentions that the "large numbers of hepatitis A cases might also reflect an epidemiologic shift in the affected population in India." It goes on to explain the potential reasons for this shift. (https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6428a3.htm)
Additional studies and surveillance data have further highlighted the increasing incidence of Hepatitis A in adolescents and adults in India, particularly during the monsoon season. [5]
Transmission
Transmission of Hepatitis A
The main route of transmission is faeco-oral, occasionally, HAV is transmitted by blood products or through illicit use of injectable drugs [1]
Causes
Causes of Hepatitis A
- Antibodies to HAV (anti-HAV) can be detected during acute illness when serum aminotransferase activity is elevated and fecal HAV shedding is still occurring.
- This early antibody response is predominantly of the IgM class and persists for several (~3) months, rarely for 6–12 months. During convalescence, however, anti-HAV of the IgG class becomes the predominant antibody.
- Therefore, the diagnosis of hepatitis A is made during acute illness by demonstrating anti HAV of the IgM class. After acute illness, anti-HAV of the IgG class remains detectable indefinitely, and patients with serum anti-HAV are immune to reinfection.
- Neutralizing antibody activity parallels the appearance of anti-HAV, and the IgG anti-HAV present in immune globulin accounts for the protection it affords against HAV infection.
Liver injury
it is immune mediated by natural killer cells, virus-specific CD8+ cytotoxic T lymphocytes and nonspecific cells recruited at the site of inflammation.[2]
Types
Classification of Hepatitis A
- Hepatitis A
- Hepatitis B
- Hepatitis C
- Hepatitis D
- Hepatitis E
Risk Factors
Risk factors:
According to Harrison’s Principles of Internal Medicine, the following are risk factors for acquiring hepatitis A:
Travel or residence in areas with high or intermediate endemicity:
- These are typically regions with poor sanitation and limited access to clean water.
Close personal contact with infected individuals:
- This includes household contacts and sexual partners.
Men who have sex with men (MSM):
- This group is at increased risk due to specific sexual practices.
Injection and non-injection drug use:
- Sharing needles or other drug paraphernalia can increase the risk of transmission.
Occupational exposure:
- Healthcare workers, daycare workers, and sewage workers may be at higher risk due to their occupational duties.
Consumption of contaminated food or water:
- Outbreaks have been associated with contaminated shellfish, fruits, and vegetables.
Homelessness:
- Individuals experiencing homelessness are at increased risk due to limited access to hygiene facilities and clean water.
Underlying chronic liver disease:
- Individuals with chronic liver disease may experience more severe outcomes if they contract hepatitis A.
Please note that this is not an exhaustive list, and other factors may contribute to the risk of hepatitis A infection. [6]
Disclaimer: This information is for educational purposes only and should not be considered a substitute for professional medical advice. Consult a healthcare provider for any health concerns.
Pathogenesis
Pathogenesis:
According to Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases, the pathogenesis of hepatitis A involves the following steps:
Entry and Primary Replication:
- The hepatitis A virus (HAV) enters the body through the fecal-oral route, usually by ingesting contaminated food or water. The virus then replicates in the oropharynx and intestinal epithelium.
Spread to the Liver:
- From the intestine, HAV enters the bloodstream and is transported to the liver, its primary target organ. The virus enters hepatocytes, the liver’s main functional cells, and replicates within them.
Immune Response:
- The host’s immune system recognizes HAV-infected hepatocytes and mounts a response, which includes both cellular and humoral components. Cytotoxic T lymphocytes (CTLs) play a crucial role in eliminating infected hepatocytes.
Liver Injury:
- While HAV itself is not directly cytopathic, the immune response against infected hepatocytes causes inflammation and liver cell damage. This leads to the characteristic symptoms of hepatitis A, including jaundice, fatigue, nausea, and abdominal pain.
Recovery and Viral Clearance:
- In most cases, the immune response successfully clears the virus, and the liver regenerates, leading to complete recovery. However, in rare instances, fulminant hepatitis may develop, resulting in severe liver failure. [7]
Disclaimer: This information is for educational purposes only and should not be considered a substitute for professional medical advice. Consult a healthcare provider for any health concerns.
Pathophysiology
Pathophysiology:
According to Robbins & Cotran Pathologic Basis of Disease, the pathophysiology of hepatitis A involves the following sequence of events:
Entry and Replication:
- The hepatitis A virus (HAV) is transmitted via the fecal-oral route, entering the body through ingestion of contaminated food or water. The virus initially replicates in the intestinal epithelium and is then transported to the liver via the portal circulation.
Hepatocellular Infection:
- In the liver, HAV enters hepatocytes (liver cells) by binding to specific cell surface receptors. Once inside, the virus replicates in the cytoplasm of the hepatocytes, leading to the accumulation of viral particles.
Immune-Mediated Injury:
- The presence of HAV antigens on the surface of infected hepatocytes triggers a host immune response. Cytotoxic T lymphocytes (CTLs) recognize and destroy infected hepatocytes, leading to hepatocellular injury and inflammation.
Clinical Manifestations:
The degree of liver injury determines the severity of the illness. Mild cases may be asymptomatic or present with flu-like symptoms, while more severe cases can manifest as jaundice, fatigue, abdominal pain, and other systemic symptoms.
Recovery and Resolution:
In most cases, the immune response effectively clears the virus within a few weeks, leading to complete recovery and lifelong immunity. However, in rare instances, fulminant hepatic failure can occur, which is a life-threatening condition.[8]
Disclaimer: This information is for educational purposes only and should not be considered a substitute for professional medical advice. Consult a healthcare provider for any health concerns.
Clinical Features
Clinical Features:
According to Goldman-Cecil Medicine, the clinical features of hepatitis A can be divided into three phases:
Prodromal Phase (Pre-icteric Phase):
- This phase occurs 1-2 weeks after exposure to the virus and lasts 3-7 days. Symptoms during this phase may include:
- Fever
- Fatigue
- Malaise
- Anorexia (loss of appetite)
- Nausea and vomiting
- Abdominal pain (typically in the right upper quadrant)
- Diarrhea
- Myalgias (muscle pain)
- Arthralgias (joint pain)
Icteric Phase:
- This phase is characterized by the onset of jaundice, which is a yellowing of the skin and eyes. Other symptoms during this phase may include:
- Dark urine
- Clay-colored stools
- Pruritus (itching)
- Hepatomegaly (enlarged liver)
Convalescent Phase:
This phase marks the recovery period, with the gradual resolution of symptoms. Jaundice fades, and liver function tests return to normal. This phase may last several weeks to months.
Additional Considerations:
- Children: Hepatitis A in children is often asymptomatic or presents with mild, nonspecific symptoms.
- Adults: Adults are more likely to experience symptomatic disease, with jaundice being a common feature.
- Fulminant Hepatitis: Rarely, hepatitis A can lead to fulminant hepatic failure, a life-threatening condition. [9]
Disclaimer: This information is for educational purposes only and should not be considered a substitute for professional medical advice. Consult a healthcare provider for any health concerns.
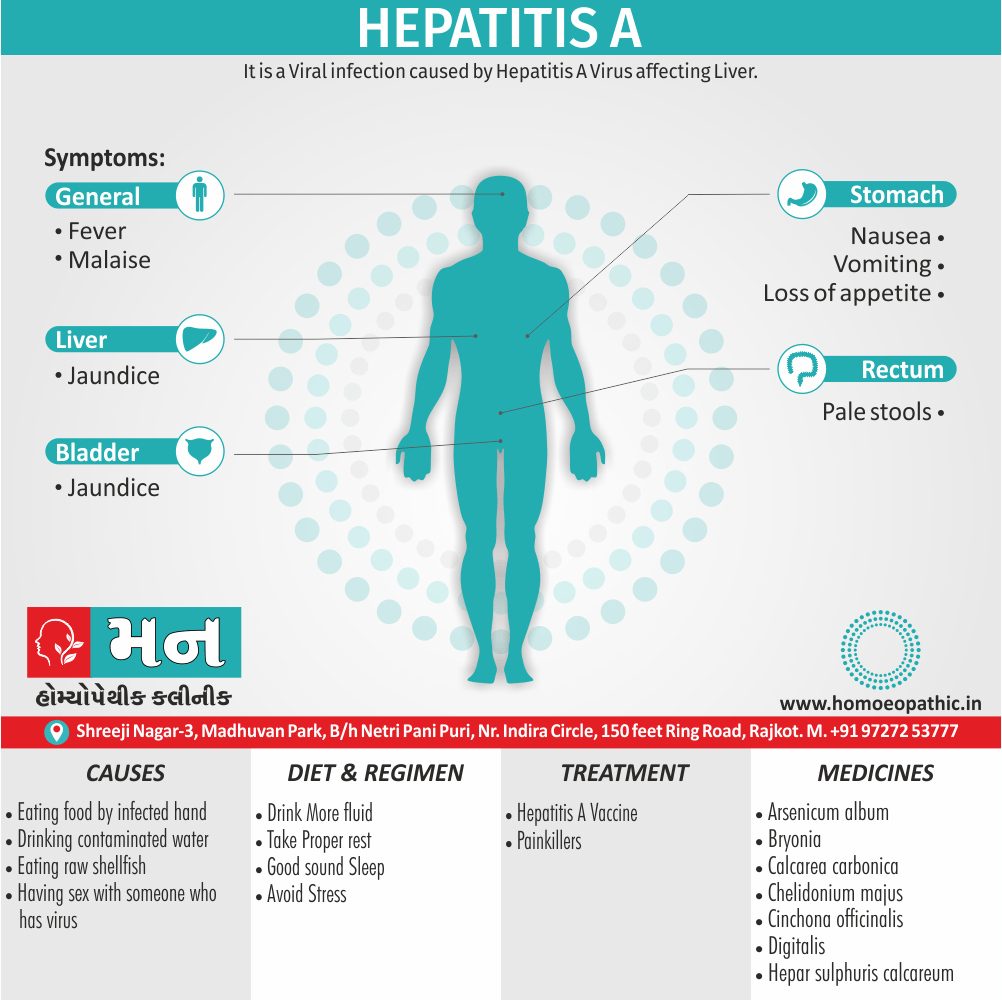
Sign & Symptoms
Sign & Symptoms of Hepatitis A
Acute viral hepatitis occurs after an incubation period that varies according to the responsible agent Incubation period 2–6 weeks, related to the infecting dose.
Prodromal symptoms consist of i.e.
- Malaise
- Loss of appetite
- Nausea, Vomiting
- Fever also Headache
- Dark urine
- Pale stool
- Fatigue, Malaise
- Arthralgias
- Photophobia
- Pharyngitis, cold, cough
- Anorexia
Age is the most important determinant of the severity of hepatitis A as also presence of chronic liver disease [1]
- Generally, incubation periods for hepatitis A range from 15–45 days (mean, 4 weeks), for hepatitis B and D from 30–180 days (mean, 8–12 weeks), for hepatitis C from 15–160 days (mean, 7 weeks), and for hepatitis E from 14–60 days (mean, 5–6 weeks).
- Additionally, The prodromal symptoms of acute viral hepatitis are systemic and quite variable.
- Constitutional symptoms of anorexia, nausea also vomiting, fatigue, malaise, arthralgias, myalgias, headache, photophobia, pharyngitis, cough, and coryza may precede the onset of jaundice by 1–2 weeks. The nausea, vomiting, and anorexia are frequently associated with alterations in olfaction and taste.
- Besides this, A low-grade fever between 38° and 39°C (100°–102°F) is more often present in hepatitis A and E than in hepatitis B or C, except when hepatitis B is heralded by a serum sickness–like syndrome; rarely, a fever of 39.5°–40°C (103°–104°F) may accompany the constitutional symptoms.
- All in all, Dark urine and clay-colored stools may be noticed by the patient from 1–5 days before the onset of clinical jaundice.[2]
Clinical Examination
Clinical Examination:
During the physical examination of a patient with suspected hepatitis A, the healthcare provider will typically focus on the following:
General Appearance:
- Assess for signs of jaundice, including yellowing of the skin and sclera (whites of the eyes).
- Observe for any signs of dehydration, such as dry mucous membranes, decreased skin turgor, or orthostatic hypotension.
Vital Signs:
- Measure the patient’s temperature, as fever is a common symptom of hepatitis A.
- Assess for tachycardia (rapid heart rate) and tachypnea (rapid breathing), which may be present in more severe cases.
Abdominal Examination:
- Palpate the abdomen for hepatomegaly (enlarged liver), which is often tender to touch.
- Assess for splenomegaly (enlarged spleen), which is less common but may be present in some cases.
- Check for abdominal tenderness, especially in the right upper quadrant.
Skin Examination:
- Look for any rashes or skin lesions, which may be associated with hepatitis A in some cases.
Neurological Examination:
- Assess the patient’s mental status, as hepatic encephalopathy (a neurological complication of liver disease) can occur in severe cases.
Additional Considerations:
- The healthcare provider may also perform a lymph node examination to check for lymphadenopathy (enlarged lymph nodes), which is a nonspecific finding but may be present in some cases of hepatitis A. [10]
Disclaimer: This information is for educational purposes only and should not be considered a substitute for professional medical advice. Consult a healthcare provider for any health concerns.
Diagnosis
Diagnosis of Hepatitis A
- Raised serum bilirubin
- Serum AST also ALT levels remain high
- Alkaline phosphatase level is only mildly elevated, though if it remains persistently high, it suggests hepatitis-associated cholestasis
- Hepatitis A specific IgM antibody can be detected at the onset of symptoms and at the first rise in serum ALT.
- IgG anti HAV becomes positive at onset of illness and is detectable for many years.
- Nucleic acid-based tests like PCR performed on stool. [1]
Differential Diagnosis
Differential Diagnosis:
According to Tintinalli’s Emergency Medicine, the differential diagnosis for hepatitis A includes the following conditions:
Other Viral Hepatitis:
- Hepatitis B, C, D, and E can present with similar symptoms to hepatitis A, including jaundice, fatigue, and abdominal pain. Serological testing is crucial to differentiate between these viral causes.
Alcoholic Hepatitis:
- Excessive alcohol consumption can lead to liver inflammation and damage, mimicking the clinical presentation of hepatitis A. A thorough history and laboratory tests can help distinguish alcoholic hepatitis.
Drug-Induced Liver Injury (DILI):
- Certain medications and toxins can cause liver injury, resulting in symptoms similar to hepatitis A. A detailed medication history and liver function tests can aid in the diagnosis of DILI.
Autoimmune Hepatitis:
- This is a chronic inflammatory liver disease of unknown etiology, characterized by elevated liver enzymes and autoantibodies. Liver biopsy and specific antibody tests are often required for diagnosis.
Metabolic Liver Diseases:
- Certain metabolic disorders, such as Wilson’s disease and hemochromatosis, can present with liver dysfunction and mimic hepatitis A. Specialized tests are needed to diagnose these conditions.
Biliary Tract Diseases:
- Conditions like cholecystitis and cholangitis can cause jaundice and abdominal pain, overlapping with the symptoms of hepatitis A. Imaging studies and laboratory tests can help differentiate these conditions.
Additional Considerations:
Less common causes of acute hepatitis, such as Epstein-Barr virus (EBV) infection, cytomegalovirus (CMV) infection, and herpes simplex virus (HSV) infection, should also be considered in the differential diagnosis.
In patients with a history of travel to endemic areas, other infectious causes of hepatitis, such as malaria and leptospirosis, should be ruled out. [11]
Disclaimer: This information is for educational purposes only and should not be considered a substitute for professional medical advice. Consult a healthcare provider for any health concerns.
Complications
Complications:
According to Current Medical Diagnosis and Treatment, complications of hepatitis A are relatively uncommon, but they can include:
Cholestatic Hepatitis:
- This is a rare complication where bile flow from the liver is obstructed, leading to prolonged jaundice, itching, and pale stools. It usually resolves on its own within a few weeks to months.
Relapsing Hepatitis:
- Some individuals may experience a relapse of symptoms weeks to months after the initial infection. These relapses are usually mild and self-limiting.
Fulminant Hepatitis (Acute Liver Failure):
- This is a rare but life-threatening complication where the liver rapidly loses its function. It is more common in older adults and individuals with underlying liver disease. Symptoms may include jaundice, encephalopathy (confusion), bleeding, and ascites (fluid accumulation in the abdomen).
Triggering of Autoimmune Hepatitis:
- In rare cases, hepatitis A infection may trigger the development of autoimmune hepatitis, a chronic liver disease characterized by the body’s immune system attacking the liver.
Additional Considerations:
- Hepatitis A does not cause chronic liver disease or increase the risk of liver cancer.
- The majority of individuals recover from hepatitis A without any long-term complications. [12]
Disclaimer: This information is for educational purposes only and should not be considered a substitute for professional medical advice. Consult a healthcare provider for any health concerns.
Investigations
Investigations:
According to Henry’s Clinical Diagnosis and Management by Laboratory Methods, the following investigations are helpful in diagnosing and managing hepatitis A:
Liver Function Tests (LFTs):
- Aminotransferases (ALT and AST): These enzymes are released from damaged liver cells and are typically elevated in hepatitis A. ALT is often more specific for liver injury than AST.
- Alkaline Phosphatase (ALP) and Bilirubin: These may be elevated, indicating cholestasis (impaired bile flow) or jaundice.
- Albumin and Prothrombin Time (PT): These tests assess liver synthetic function, which can be impaired in severe hepatitis A.
Serological Tests:
- Anti-HAV IgM: The presence of IgM antibodies indicates an acute or recent hepatitis A infection.
- Anti-HAV IgG: The presence of IgG antibodies indicates a past infection and lifelong immunity.
Other Tests:
- Complete Blood Count (CBC): May show leukocytosis (increased white blood cells) in acute hepatitis.
- Viral PCR: May be used to detect HAV RNA in the blood or stool, especially in early infection or when serological tests are inconclusive.
- Liver Imaging: Ultrasound or CT scan may be performed to assess liver size and rule out other causes of liver disease.
- Liver Biopsy: Rarely needed for diagnosis but may be considered in atypical cases or to assess the severity of liver damage.
Additional Considerations:
- Hepatitis A is usually a self-limited illness, and most patients recover completely without specific treatment.
- Supportive care, including rest, hydration, and management of symptoms, is the mainstay of treatment.
- Vaccination is the most effective way to prevent hepatitis A infection. [13]
Disclaimer: This information is for educational purposes only and should not be considered a substitute for professional medical advice. Consult a healthcare provider for any health concerns.
Treatment
Treatment of Hepatitis A
- Unlike other types of viral hepatitis, hepatitis A rarely causes long-term liver damage and doesn’t become a long-term (chronic) illness.
- There isn’t a specific treatment for hepatitis A, and most people will recover fully within one to two months.
- Usually, symptoms are managed at home
- Plenty of rest
- Painkillers and medication to help with itchiness, nausea or vomiting.
Occasionally hepatitis A can last longer and, in rare cases, it can be life-threatening if it causes the liver to stop working properly (liver failure).[2]
Prevention
Prophylaxis of Hepatitis A
Hepatitis A Vaccine: –
Dose primary course of 2 doses (1 mL each) one month apart. Booster Dose—One dose of 6–12 months after first dose for active immunization which provides long-lasting immunity.
Apart from individuals at high risk, hepatitis A vaccination is recommended in patients with chronic hepatitis C. Post-exposure Prophylaxis For intimate contacts (household, sexual, institutional) of persons with hepatitis A.
Dose: Immunoglobulin 0.02 mL/kg is recommended as early after exposure as possible; it may be effective even when administered as late as 2 weeks after exposure [1]
Homeopathic Treatment
Homeopathic Treatment of Hepatitis A
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Hepatitis A:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Medicines:
Arsenicum album
- In general, Great exhaustion after the slightest exertion; septic infections and low vitality;
- Headaches, Relieved especially by cold
- Intense photophobia; hay-fever also coryza; face yellow.
- Cannot bear the sight also smell of food; nausea, retching, vomiting.
- Liver and spleen enlarged and painful; additionally abdomen swollen and painful; high temperature.
- Worse – after, midnight, from cold, cold drinks or food, right side. On the other hand, Better – with heat, warm drinks, head elevated.
Bryonia
- Liver region swollen, sore, tensive. In detail, Stitching pain, tenderness of abdominal walls.
- Furthermore; Aching muscles, irritable, oppressive headache.
- Dry lips, mouth, excessive thirst, bitter taste, stools large, dry hard, red brown urine, dry cough.
- Weakness, apathy,
- Coryza, dark coated tongue, abnormal hunger, loss of taste.
- Vomiting of bile and water immediately after eating, constipation.
- Worse – pressure, coughing, breathing, warmth, warm drinks, motion, morning, eating, exertion, touch, stooping, opening eyes, sitting up. whereas Better – lying on painful side, rest, cold things.
Calcarea carbonica
- Headache from over-‘lifting, mental exertion, with nausea; eyes sensitive to light; coryza.
- Abdomen sensitive to slightest pressure; additionally liver region painful when stooping; dark brown urine.
- Tickling cough, troublesome at night; pain between shoulder blades.
- Worse – exertion, ascending, cold, standing. whereas Better – dry weather, lying on painful side.
Cinchona officinalis
- Basically, Yellowish sclera; photophobia; coryza, sneezing, watery discharge.
- Pain in right upper abdomen; liver and spleen swollen also enlarged; jaundice; intermittent fever.
- Worse – slightest touch, draughts, night, after eating, bending over. on the other hand Better – bending double, pressure, open air, warmth.
Chelidonium manjus
- Heavy, lethargic; drowsiness very marked; right-sided headache down behind ears also shoulder blade; face yellow.
- In detail, Nausea, vomiting; jaundice due to hepatic obstruction; liver enlarged; dark turbid urine; clay-colored stools, float in water.
- Short exhausting cough; spasmodic cough; pain in right side of chest also shoulder.
- Besides this, Fixed pain under inner and lower angle of right shoulder blade; yellow skin.
- Worse – especially right side, motion, touch, change of weather, early morning. whereas Better – after dinner, pressure.
Hepar sulphuris calcareum
- Stitching in region of liver when walking, coughing, either breathing, or touching it.
- Must turn in bed constantly; irritable, dejected, sad;
- Furthermore, Craving acids, wine, strong tasting food.
- Aversion to fats; belching without taste or smell.
- Burning in stomach; additionally heaviness and pressure in stomach after slight meal.
- Abdomen distended, tense; soft fetid clay colored stool, difficult to expel; croupy cough, asthma.
- Worse – dry cold winds, cool air, slight draught, touch, lying especially on painful side, evening and night. whereas Better – damp weather, wrapping head up, warmth, after eating, loosening clothing.
Mercuris
- Catarrhal headaches; In detail Coryza with sneezing.
- Liver enlarged and, hard, sore to touch; jaundice; whitish-grey stools; urine dark.
- Cannot lie specifically on right side; generally either gastric or bilious fever.
- Worse – night, wet weather, lying on right side, perspiring, warm room, also warm bed.
Digitalis
- Dull lethargy with slow pulse; excessive nausea not relieved by vomiting; enlarged sore painful liver.
- Moreover, Cough with raw sore feeling in chest.
- Continuous sleepiness; jaundice; additionally sudden flushes of heat followed by great nervous weakness.
- Worse – sitting erect, after meals and music but Better – empty stomach, open air.
Lachesis
- Sun headaches; coryza, preceded by headache; face jaundiced.
- Liver region sensitive, cannot bear anything around waist; hot flushes also hot perspiration; abdomen sensitive, painful.
- Stools clay colored, light yellow urine, eyes yellow, cough also vomiting together.
- Worse – after sleep, left side, warm bath, pressure, hot drinks, especially closing eyes. On the other hand Better – appearance of discharges, warm applications.
Natrum sulphuricum
- Specifically A liver remedy.
- Duodenal catarrh, hepatitis, jaundice and vomiting of bile; additionally liver sore to touch, with sharp stitching pains; cannot bear tight clothing around waist.
- Coryza, yellow conjunctiva, photophobia, cough, yellow diarrhoea.
- Worse – lying especially on left side, music, damp weather. whereas Better-dry weather, pressure, changing position. [4]
Diet & Regimen
Diet & Regimen of Hepatitis A
Diet:
- Focus on whole, unprocessed foods: Choose plenty of fruits, vegetables, whole grains, and lean protein sources.
- Limit saturated and trans fats: These can contribute to liver inflammation. Opt for healthy fats like those found in avocados, nuts, and olive oil.
- Avoid alcohol: Alcohol can further damage the liver, especially during Hepatitis A infection.
- Stay hydrated: Drink plenty of water to help flush out toxins and support liver function.
- Consider smaller, more frequent meals: This can be easier on the digestive system, especially if you experience nausea or fatigue.
Regimen:
- Rest: Get adequate rest to allow your body to recover.
- Hygiene: Practice good hygiene, including frequent handwashing, to prevent the spread of the virus.
- Medications: Over-the-counter pain relievers can help manage symptoms like fever and aches. Consult your doctor before taking any medications, especially if you have underlying liver conditions.
- Vaccinations: If you have not been vaccinated against Hepatitis A, talk to your doctor about getting vaccinated. Vaccination can prevent future infections.
Do’s and Don'ts
The Do’s & Don’ts
Do’s:
- Get vaccinated: The hepatitis A vaccine is safe and effective in preventing infection.
- Practice good hygiene: Wash your hands thoroughly with soap and water after using the toilet, changing diapers, and before preparing or eating food.
- Drink safe water: Avoid drinking untreated water or ice from unknown sources, especially when traveling to areas with poor sanitation.
- Cook food thoroughly: Ensure that food is cooked to a safe temperature to kill any potential viruses.
- Be cautious with shellfish: Avoid raw or undercooked shellfish, as they can be contaminated with HAV.
- Get tested: If you experience symptoms of hepatitis A or have been exposed to someone with the virus, get tested promptly.
- Seek medical advice: Consult a healthcare provider for diagnosis, treatment, and advice on managing the infection.
- Rest: Get plenty of rest to allow your body to recover.
- Eat a healthy diet: Eat a balanced diet with plenty of fruits, vegetables, and whole grains.
- Stay hydrated: Drink plenty of fluids to prevent dehydration.
Don’ts:
- Don’t share personal items: Avoid sharing towels, toothbrushes, eating utensils, or other personal items with an infected person.
- Don’t have unprotected sex: Use condoms to reduce the risk of transmission during sexual activity.
- Not donate blood or organs: If you have hepatitis A, avoid donating blood or organs until you have fully recovered.
- Don’t drink alcohol: Alcohol can further damage the liver, so avoid it during and for a few months after recovery.
- Don’t take unnecessary medications: Some medications can be harmful to the liver, so consult your doctor before taking any over-the-counter or prescription drugs.
- Not prepare food for others: If you have hepatitis A, avoid preparing food for others until you are no longer contagious.
Terminology
Terminology:
Here are some common terminologies used in articles about Hepatitis A, along with their meanings:
Hepatitis:
- Inflammation of the liver, often caused by viral infections, alcohol abuse, or certain medications.
Hepatitis A virus (HAV):
- The specific virus that causes Hepatitis A.
Acute Hepatitis:
- A short-term inflammation of the liver, usually resolving within a few weeks.
Chronic Hepatitis:
- Long-term inflammation of the liver, lasting for more than six months. Hepatitis A does NOT cause chronic hepatitis.
Fecal-oral transmission:
- The mode of transmission of HAV, where the virus is shed in the feces of infected individuals and then ingested by others through contaminated food or water.
Incubation period:
- The time between exposure to the virus and the onset of symptoms, typically ranging from 2 to 6 weeks for Hepatitis A.
Prodromal phase:
- The initial phase of the illness, often characterized by non-specific symptoms like fatigue, nausea, and low-grade fever.
Icteric phase:
- The phase where jaundice (yellowing of the skin and eyes) develops due to elevated bilirubin levels in the blood.
Convalescent phase:
- The recovery phase, where symptoms gradually subside and liver function returns to normal.
Fulminant hepatitis:
- A rare but severe complication of hepatitis, characterized by rapid liver failure and high mortality rates.
Anicteric hepatitis:
- A form of hepatitis where jaundice does not occur.
Asymptomatic infection:
- An infection where the individual does not experience any noticeable symptoms.
Hepatocellular injury:
- Damage to the liver cells caused by the virus or the body’s immune response.
Liver enzymes (ALT, AST):
- Enzymes found in liver cells that are released into the bloodstream when the liver is damaged, used as markers of liver function.
Serology:
- Blood tests that detect antibodies against the hepatitis A virus, used for diagnosis.
Anti-HAV IgM:
- Antibodies that appear early in the course of infection, indicating an acute infection.
Anti-HAV IgG:
- Antibodies that appear later and persist for life, indicating past infection and immunity.
Vaccine:
- A preparation of weakened or inactivated virus that stimulates the immune system to produce antibodies, providing protection against future infection.
Here are some common terminologies used in homeopathic articles about Hepatitis A, along with their meanings:
Vital Force:
- The fundamental energy or life force that animates living beings and maintains health. In homeopathy, disease is seen as a disturbance of the vital force.
Miasm:
- A predisposition to certain types of diseases, often inherited or acquired. Homeopaths consider miasms when choosing remedies for chronic conditions.
Similia Similibus Curentur:
- The fundamental principle of homeopathy, meaning "like cures like." This principle states that a substance that can cause symptoms in a healthy person can cure similar symptoms in a sick person.
Proving:
- A systematic process of testing a substance on healthy volunteers to determine its potential effects and symptom picture.
Repertory:
- A reference book that lists symptoms and the homeopathic remedies associated with them.
Materia Medica:
- A comprehensive collection of information about homeopathic remedies, including their sources, preparation, and symptom pictures.
Potency:
- The degree of dilution and succussion (shaking) of a homeopathic remedy. Higher potencies are believed to be more powerful.
Constitutional Remedy:
- A homeopathic remedy that matches the individual’s overall physical, mental, and emotional characteristics.
Acute Prescribing:
- The use of homeopathic remedies to treat acute illnesses or specific symptoms.
Chronic Prescribing:
- The use of homeopathic remedies to address underlying predispositions and chronic conditions.
Aggravation:
- A temporary worsening of symptoms after taking a homeopathic remedy, often considered a positive sign of healing.
Amelioration:
- An improvement of symptoms after taking a homeopathic remedy.
Specific Remedies for Hepatitis A (These may vary based on individual symptoms and practitioner):
- Phosphorus: For individuals with jaundice, weakness, and a thirst for cold drinks.
- Chelidonium: For individuals with right-sided abdominal pain, nausea, and clay-colored stools.
- Nux Vomica: For individuals with irritability, nausea, and constipation.
- Lycopodium: For individuals with right-sided abdominal pain, bloating, and irritability.
Important Note: Homeopathy is a complementary and alternative medicine (CAM) system. The effectiveness of homeopathy for treating Hepatitis A has not been scientifically proven. If you are considering homeopathic treatment for Hepatitis A, consult a qualified homeopathic practitioner for personalized advice and treatment.
References
References use for Article Hepatitis A
- Medicine Golwala
- Harrison-s_Principles_of_Internal_Medicine-_19th_Edition-_2_Volume_Set
- Encyclopedia of Diets – A Guide to Health and Nutrition (PDF Drive )
- Homoeopathic Body-System Prescribing – A Practical Workbook of Sector Remedies
- Viral Hepatitis Surveillance — India, 2011–2013
Book Title:Harrison’s Principles of Internal Medicine, Edition: 21st Edition, Writer: Dennis L. Kasper, Anthony S. Fauci, Stephen L. Hauser, Dan L. Longo, J. Larry Jameson, Joseph Loscalzo
Year of Publication: 2022
Publisher: McGraw HillBook Title: Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases, Edition: 9th Edition, Writer: John E. Bennett, Raphael Dolin, Martin J. Blaser, Year of Publication: 2020
Publisher: ElsevierBook Title: Robbins & Cotran Pathologic Basis of Disease, Edition: 10th Edition, Writer: Vinay Kumar, Abul K. Abbas, Jon C., Aster , Year of Publication: 2021
Publisher: Elsevier SaundersBook Title: Goldman-Cecil Medicine
Edition: 26th Edition, Writer: Lee Goldman, Andrew I. Schafer, Year of Publication: 2020, Publisher: ElsevierBook Title: Bates’ Guide to Physical Examination and History Taking
Edition: 13th Edition, Writer: Lynn S. Bickley, Peter G. Szilagyi
Year of Publication: 2022, Publisher: Lippincott Williams & WilkinsBook Title: Tintinalli’s Emergency Medicine: A Comprehensive Study Guide Edition: 9th Edition
Writer: Judith E. Tintinalli, J. Stephan Stapczynski, O. John Ma, Donald M. Yealy, Garth D. Meckler, David M. Cline Year of Publication: 2020 Publisher: McGraw HillBook Title: Current Medical Diagnosis and Treatment, Edition: 2024, Writer: Maxine A. Papadakis, Stephen J. McPhee, Michael W. Rabow, Year of Publication: 2023
Publisher: McGraw HillBook Title: Henry’s Clinical Diagnosis and Management by Laboratory Methods, Edition: 24th Edition, Writer: Richard A. McPherson, Matthew R. Pincus
Year of Publication: 2022, Publisher: ElsevierBook Title: The Merck Manual of Diagnosis and Therapy, Edition: 21st Edition, Writer: Robert S. Porter, Justin L. Kaplan
Year of Publication: 2022, Publisher: Merck Sharp & Dohme Corp.
Also Search As
Also Search As
There are several ways people can search for homeopathic articles on Hepatitis A:
Online Databases:
- ResearchGate: This platform hosts a variety of research publications, including case reports and studies on homeopathic treatment of Hepatitis A.
- The National Center for Biotechnology Information (NCBI): This database includes PubMed, which indexes a vast number of medical articles, some of which may discuss homeopathic approaches to Hepatitis A.
Homeopathic Journals:
- The Homoeopathic Journal: This peer-reviewed journal often publishes articles on the homeopathic treatment of various diseases, including Hepatitis A.
- Other Homeopathic Journals: Many other homeopathic journals exist, and some may contain relevant articles. You can search for these journals online or through a library.
Homeopathic Websites and Blogs:
- Websites of Homeopathic Organizations: Many homeopathic organizations have websites that provide information on homeopathic treatments, including articles on specific conditions like Hepatitis A.
- Blogs of Homeopathic Practitioners: Some homeopathic practitioners maintain blogs where they share their experiences and knowledge, including case studies of patients treated with homeopathy for Hepatitis A.
Books:
- Homeopathic Materia Medica: These books contain detailed information on homeopathic remedies and their indications, which may include Hepatitis A.
- Homeopathic Repertories: These books help practitioners find the most appropriate homeopathic remedy based on a patient’s symptoms.
Keywords to Use:
When searching for homeopathic articles on Hepatitis A, use keywords like:
- "Homeopathic treatment of Hepatitis A"
- "Homeopathy for Hepatitis A"
- "Homeopathic remedies for Hepatitis A"
- "Case studies of Hepatitis A treated with homeopathy"
Please note: While homeopathy is a popular alternative medicine system, its effectiveness for treating Hepatitis Ahas not been scientifically proven. If you are considering homeopathic treatment for Hepatitis A, it is important to consult a qualified homeopathic practitioner and discuss the risks and benefits.
There are numerous ways to search for information on Hepatitis A, depending on the kind of information you’re looking for and the depth of research you need:
General Search Engines:
- Use search engines like Google, Bing, or DuckDuckGo to find basic information on Hepatitis A. Use specific keywords like "Hepatitis A", "Hepatitis A symptoms", "Hepatitis A transmission", or "Hepatitis A treatment" to narrow down your search.
Official Health Organizations:
- World Health Organization (WHO): Provides comprehensive information on Hepatitis A, including global statistics, prevention strategies, and treatment guidelines.
- Centers for Disease Control and Prevention (CDC): Offers detailed information on Hepatitis A for both the public and healthcare professionals, including fact sheets, FAQs, and clinical guidance.
- National Health Portal of India: Provides information on Hepatitis A specific to the Indian context, including prevention, vaccination, and treatment options.
Medical Websites and Databases:
- Mayo Clinic: Offers detailed information on Hepatitis A, including symptoms, causes, risk factors, diagnosis, and treatment.
- MedlinePlus: Provides easy-to-understand information on Hepatitis A from the National Library of Medicine.
- PubMed: A searchable database of medical literature that allows you to find research articles on Hepatitis A.
Books and Journals:
- Medical textbooks: Standard medical textbooks like Harrison’s Principles of Internal Medicine and Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases provide in-depth information on Hepatitis A.
- Medical journals: Peer-reviewed medical journals like The Lancet, The New England Journal of Medicine, and Clinical Infectious Diseases publish research articles on various aspects of Hepatitis A.
Other Resources:
- Patient support groups: Online or in-person support groups can provide valuable information and emotional support for people living with or affected by Hepatitis A.
- Healthcare providers: Your doctor or other healthcare providers can answer your questions about Hepatitis A and provide personalized advice.
By using a combination of these resources, you can gather reliable and comprehensive information on Hepatitis A to suit your specific needs.
Frequently Asked Questions (FAQ)
What is Hepatitis A?
Definition:
Hepatitis A is a viral infection that affects the liver, caused by the Hepatitis A virus (HAV). It spreads primarily through contaminated food and water.
What are the symptoms of Hepatitis A?
Symptoms of Hepatitis A include jaundice, fatigue, abdominal pain, loss of appetite, nausea, and fever. In some cases, symptoms may be mild or asymptomatic.
How is Hepatitis A transmitted?
Hepatitis A is transmitted through ingestion of contaminated food or water, often due to poor sanitation or hygiene. It can also spread through close contact with an infected person.
When should I seek medical attention for Hepatitis A?
Medical attention should be sought if symptoms are severe, persist for a prolonged period, or if there is significant discomfort or worsening of symptoms. Consulting a healthcare provider is crucial for proper diagnosis and management.
How can I prevent Hepatitis A?
Preventive measures include vaccination, practicing good hygiene, and avoiding consumption of contaminated food and water. Ensuring proper sanitation can significantly reduce the risk of infection.
Can hepatitis A be treated with homeopathy?
Yes,
Homeopathy offers potential supportive treatments for hepatitis A, focusing on symptom relief and liver function.
What are some homeopathic remedies for hepatitis A?
Some homeopathic remedies that may be considered for hepatitis A include Phosphorus, Nux vomica, Chelidonium, and Lycopodium.
Are there any side effects of homeopathic remedies for hepatitis A?
Homeopathic remedies are generally safe and have minimal side effects when used as directed. However, it’s important to consult a qualified practitioner to ensure proper selection and dosage.
Can homeopathy prevent hepatitis A infection?
Homeopathy is not a substitute for vaccination.
The most effective way to prevent hepatitis A infection is through vaccination and good hygiene practices.
Are there any specific dietary recommendations during homeopathic treatment for hepatitis A?
A healthy diet is important for liver health and recovery from hepatitis A. Your homeopathic practitioner may recommend specific dietary modifications based on your individual needs.
