Hiatal hernia
Definition
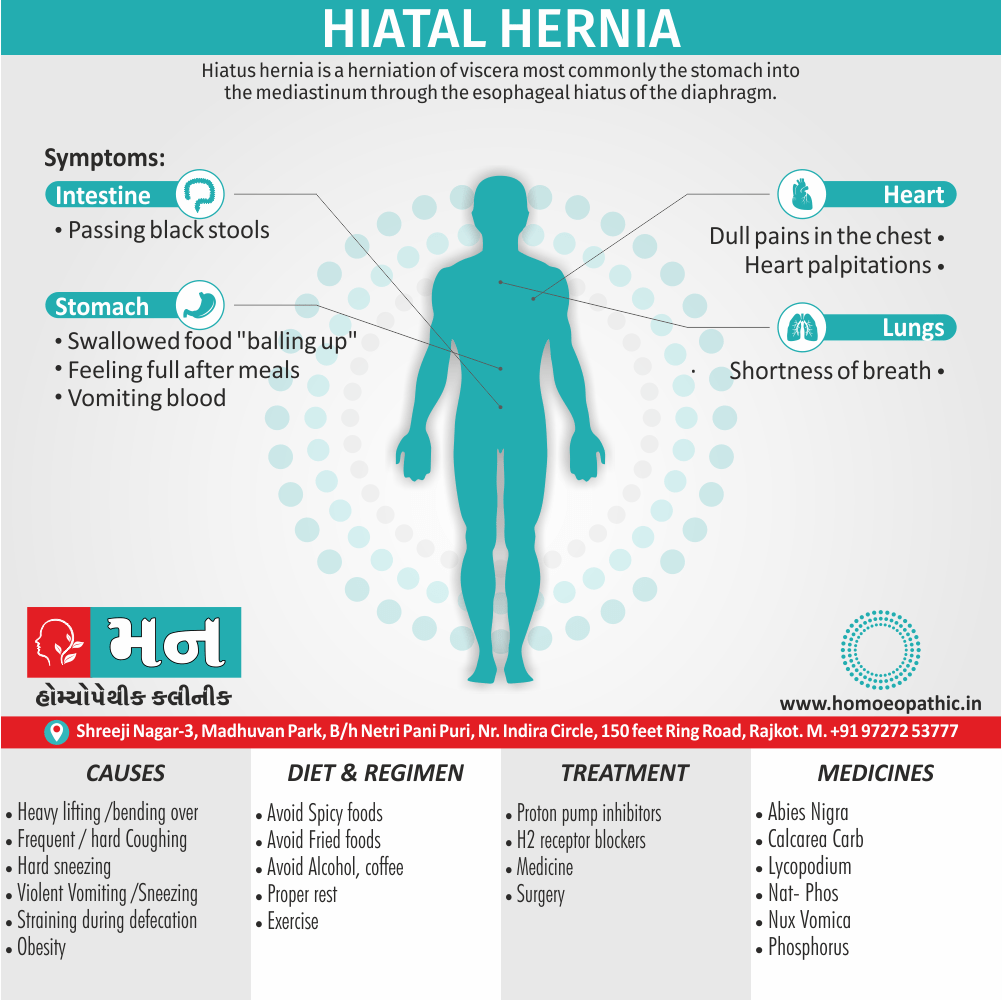
Hiatal hernia is a herniation of viscera, most commonly the stomach, into the mediastinum through the esophageal hiatus of the diaphragm.[1]
Here are some synonyms for hiatal hernia:
- Hiatus hernia: This is the most common way to refer to the condition, with "hiatus" referring to the opening in the diaphragm through which the esophagus passes.
- Esophageal hernia: A less common term, but still accurate, as the hernia involves the esophagus.
- Sliding hiatal hernia: This refers to the most common type of hiatal hernia, where the stomach and the gastroesophageal junction (the connection between the esophagus and stomach) slide up into the chest cavity.
- Paraesophageal hernia: This is a less common type of hiatal hernia where part of the stomach pushes through the diaphragm next to the esophagus, rather than above it.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Hiatal hernia
- This may result in gastroesophageal reflux disease (GERD) or laryngopharyngeal reflux (LPR) with symptoms such as a taste of acid in the back of the mouth or heartburn.
- Other symptoms may include trouble swallowing and chest pains.
- Complications may include iron deficiency anemia, volvulus, or bowel obstruction.[1]
Epidemiology
Epidemiology
The prevalence of hiatal hernia in the Indian population varies depending on the study and population examined. However, a study published in 2014 in the Journal of Indian Association of Pediatric Surgeons titled "Hiatal Hernia in Children" suggests that the prevalence of hiatal hernia in the Indian pediatric population is relatively low compared to Western countries.
Please note that this is just one example, and there may be other studies with different findings on the epidemiology of hiatal hernia in India.[5]
Causes
Causes
The following are potential causes of a hiatal hernia.
Increased pressure within the abdomen caused by:
- Heavy lifting or bending over
- Frequent or hard coughing
- Hard sneezing
- Violent vomiting
- Straining during defecation (i.e., the Valsalva maneuver)
Obesity and age-related changes to the diaphragm are also general risk factors.
Types
Classification of Hiatal hernia
Four types of esophageal hiatal hernia are identified:
Type I:
A type I hernia, also known as a sliding hiatal hernia, occurs when part of the stomach slides up through the hiatal opening in the diaphragm. There is a widening of the muscular hiatal tunnel and circumferential laxity of the pharyngoesophageal ligament, allowing a portion of the gastric cardia to herniate upward into the posterior mediastinum. The clinical significance of type I hernias is in their association with reflux disease. Sliding hernias are the most common type and account for 95% of all hiatal hernias. [2]
Type II:
A type II hernia, also known as a paraoesophageal or rolling hernia, occurs when the fundus and greater curvature of the stomach roll up through the diaphragm, forming a pocket alongside the esophagus. It results from a localized defect in the phrenoesophageal ligament while the gastroesophageal junction remains fixed to the pre aortic fascia and the median arcuate ligament. The gastric fundus then serves as the leading point of herniation. Although type II hernias are associated with reflux disease, their primary clinical significance lies in the potential for mechanical complications.
Type III:
Type III hernias have elements of both types I and II hernias. With progressive enlargement of the hernia through the hiatus, the phrenoesophageal ligament stretches, displacing the gastroesophageal junction above the diaphragm, thereby adding a sliding element to the type II hernia.
Type IV:
Type IV hiatus hernia is associated with a large defect in the phrenoesophageal ligament, allowing other organs, such as colon, spleen, pancreas and small intestine to enter the hernia sac.
The end stage of type I and type II hernias occurs when the whole stomach migrates up into the chest by rotating 180° around its longitudinal axis, with the cardia and pylorus as fixed points. In this situation the abnormality is usually referred to as an intrathoracic stomach.[2]
Risk Factors
Risk factor of Hiatal hernia
- Old age
- Obesity
- Surgery
- Major trauma
- Scoliosis
Pathogenesis
Pathogenesis
Description:
The pathogenesis of hiatal hernia involves a combination of factors that weaken the phrenoesophageal membrane and widen the esophageal hiatus, allowing the stomach to herniate into the thorax. These factors include:
Anatomic Factors:
The esophageal hiatus is a natural opening in the diaphragm through which the esophagus passes to connect to the stomach. In some individuals, this opening may be congenitally larger or become weakened over time due to factors such as aging, obesity, or increased intra-abdominal pressure.
Increased Intra-abdominal Pressure:
Conditions that increase pressure within the abdomen, such as obesity, pregnancy, chronic coughing, constipation, or heavy lifting, can contribute to the development of a hiatal hernia.
Phrenoesophageal Membrane Weakness:
The phrenoesophageal membrane is a thin layer of tissue that helps anchor the esophagus to the diaphragm. Weakening of this membrane due to aging or other factors can make it easier for the stomach to herniate through the esophageal hiatus.
Esophageal Shortening:
In some cases, the esophagus may become shortened due to scarring from chronic acid reflux or other conditions. This can pull the stomach upwards through the esophageal hiatus.
Genetic Predisposition:
There may be a genetic component to the development of hiatal hernia, as it tends to run in families.
Please note that the pathogenesis of hiatal hernia is complex and multifactorial, and ongoing research is exploring additional factors that may contribute to its development.
Additional Information:
Types of Hiatal Hernia:
There are two main types of hiatal hernia: sliding hiatal hernia and paraesophageal hiatal hernia. Sliding hiatal hernia is more common and occurs when the gastroesophageal junction (GEJ) and a portion of the stomach slide upwards through the esophageal hiatus. Paraesophageal hiatal hernia occurs when a portion of the stomach herniates alongside the esophagus, without displacement of the GEJ.
Symptoms:
Many individuals with hiatal hernia are asymptomatic, but common symptoms include heartburn, regurgitation, chest pain, and difficulty swallowing.
Treatment:
Treatment options depend on the type and severity of the hernia and may include lifestyle modifications, medications to manage symptoms, or surgery in severe cases.[6]
Pathophysiology
Pathophysiology
Description:
The pathophysiology of hiatal hernia involves a disruption of the normal anatomical and physiological mechanisms that maintain the gastroesophageal junction (GEJ) and lower esophageal sphincter (LES) in their proper positions.
Key Points:
Anatomical Disruption:
Hiatal hernia occurs when a portion of the stomach protrudes through the esophageal hiatus, an opening in the diaphragm. This disrupts the normal anatomical relationship between the stomach, esophagus, and diaphragm.
Lower Esophageal Sphincter Dysfunction:
The LES is a muscular ring at the lower end of the esophagus that prevents stomach acid and contents from refluxing back into the esophagus. Hiatal hernia can weaken the LES, leading to decreased LES pressure and impaired function. This allows stomach acid and contents to reflux into the esophagus, causing symptoms such as heartburn and regurgitation.
Acid Reflux and Esophagitis:
Chronic acid reflux due to hiatal hernia can lead to inflammation and damage to the esophageal lining, a condition known as esophagitis. This can cause symptoms such as chest pain, difficulty swallowing, and bleeding.
Impaired Esophageal Clearance:
Hiatal hernia can also impair the normal clearance mechanisms of the esophagus, leading to prolonged exposure of the esophagus to acid and other irritants. This further contributes to esophagitis and other complications.
Complications:
In some cases, hiatal hernia can lead to complications such as Barrett’s esophagus (a precancerous condition), esophageal stricture (narrowing of the esophagus), and aspiration pneumonia (lung infection due to aspiration of stomach contents).
Additional Information:
Types of Hiatal Hernia:
The two main types of hiatal hernia are sliding hiatal hernia (more common) and paraesophageal hiatal hernia.
Risk Factors:
Risk factors for hiatal hernia include obesity, older age, smoking, and conditions that increase intra-abdominal pressure.
Diagnosis:
Hiatal hernia is often diagnosed through imaging studies such as barium swallow or upper endoscopy.
Treatment:
Treatment options depend on the type and severity of the hernia and may include lifestyle modifications, medications to manage symptoms, or surgery in severe cases.[7]
Clinical Features
Clinical Features of Hiatal Hernia
Description:
The clinical features of hiatal hernia vary depending on the size and type of hernia, as well as the presence of associated complications. Many individuals with small hiatal hernias are asymptomatic, while others experience a range of symptoms, including:
Common Symptoms:
- Heartburn: A burning sensation in the chest, often worse after meals or when lying down.
- Regurgitation: The backflow of stomach acid or food into the mouth or esophagus.
- Dysphagia: Difficulty swallowing.
- Chest Pain: May mimic cardiac pain and can be severe.
- Belching: Excessive burping.
- Nausea and Vomiting: Less common but can occur.
- Early Satiety: Feeling full after eating a small amount of food.
Less Common Symptoms:
- Water Brash: Sudden filling of the mouth with saliva, often triggered by regurgitation of stomach acid.
- Globus Sensation: Feeling of a lump in the throat.
- Chronic Cough: Due to irritation of the esophagus or aspiration of stomach contents.
- Hoarseness: Due to acid reflux affecting the vocal cords.
- Asthma: In some cases, acid reflux can trigger or worsen asthma symptoms.
- Anemia: Chronic bleeding from esophagitis can lead to iron deficiency anemia.
Complications:
In severe cases or with long-standing hiatal hernia, complications can arise, including:
- Esophagitis: Inflammation of the esophagus due to chronic acid exposure.
- Esophageal Stricture: Narrowing of the esophagus due to scarring from esophagitis.
- Barrett’s Esophagus: Precancerous changes in the lining of the esophagus.
- Esophageal Ulcers: Open sores in the esophagus.
- Aspiration Pneumonia: Lung infection due to aspiration of stomach contents.
- Volvulus: Twisting of the stomach within the hernia sac, a rare but potentially life-threatening complication.[8]
Please note that the clinical features of hiatal hernia can overlap with other gastrointestinal conditions, so a thorough evaluation by a healthcare professional is essential for accurate diagnosis and appropriate management.
Sign & Symptoms
Sign & Symptoms
Hiatal hernia has often been called the "great mimic" because its symptoms can resemble many disorders.
Among them, a person with a hiatal hernia can experience
- Dull pains in the chest
- Shortness of breath (caused by the hernia’s effect on the diaphragm)
- Heart palpitations (due to irritation of the vagus nerve)
- Swallowed food "balling up" and causing discomfort in the lower esophagus until it passes on to the stomach
- Feeling especially full after meals
- Vomiting blood or passing black stools, which may indicate gastrointestinal bleeding.
In addition, hiatal hernias often result in heartburn but may also cause chest pain or pain with eating.
In most cases however, a hiatal hernia does not cause any symptoms. The pain and discomfort that a patient experience is due to the reflux of gastric acid, air, or bile. While there are several causes of acid reflux, it occurs more frequently in the presence of hiatal hernia.
In newborns, the presence of Bochdalek hernia can be recognized from symptoms such as difficulty breathing, fast respiration, increased heart rate.[2]
Clinical Examination
Clinical Examination of Hiatal Hernia
Description:
Physical examination alone is often not sufficient to diagnose a hiatal hernia, as many patients with small hernias are asymptomatic. However, a focused clinical examination can help identify associated signs and symptoms, and guide further investigations.
Key Components of Clinical Examination:
General Observation: Assess the patient’s general appearance, body habitus (obesity is a risk factor), and any signs of discomfort.
Auscultation: Listen for bowel sounds in the chest, which may indicate the presence of a large hiatal hernia.
Palpation: Palpate the abdomen for tenderness, masses, or organomegaly.
Percussion: Percuss the chest and abdomen to assess for changes in resonance that may suggest the presence of a hernia.
Assessment of Associated Symptoms: Inquire about and assess for symptoms commonly associated with hiatal hernia, such as:
- Heartburn: A burning sensation in the chest, often worse after meals or when lying down.
- Regurgitation: Backflow of stomach acid or food into the mouth or esophagus.
- Dysphagia: Difficulty swallowing.
- Chest Pain: May mimic cardiac pain and can be severe.
Focused Examination for Complications: If complications are suspected, perform additional assessments, such as:
- Signs of Esophagitis: Look for signs of inflammation in the mouth or throat.
- Signs of Anemia: Look for pallor or other signs of anemia due to chronic blood loss.
Limitations of Clinical Examination:
- Physical examination findings are often non-specific and may not differentiate hiatal hernia from other conditions.
- Small hiatal hernias are usually not detectable on physical examination.
Importance of Further Investigations:
Due to the limitations of clinical examination, further investigations are crucial for the diagnosis of hiatal hernia. These may include:
- Barium Swallow: A radiographic study that assesses the anatomy of the esophagus and stomach.
- Upper Endoscopy: A procedure to visualize the esophagus and stomach lining directly.
- Esophageal Manometry: A test to measure the pressure and function of the esophagus and LES.
- pH Monitoring: A test to measure acid reflux in the esophagus.[9]
Diagnosis
Diagnosis of Hiatus hernia
The diagnosis of a hiatus hernia is typically made through an upper GI series, endoscopy or high-resolution manometry.[2]
Differential Diagnosis
Differential Diagnosis of Hiatus hernia
- Peptic ulcer disease
- Gastritis
- Acute coronary syndrome
- Coronary artery disease[2]
Complications
Complications of Hiatal Hernia
While many individuals with hiatal hernia remain asymptomatic or experience mild symptoms, several potential complications can arise, particularly in cases of large or long-standing hernias:
Gastrointestinal Complications:
- Gastroesophageal Reflux Disease (GERD): The most common complication, GERD occurs due to the weakening of the lower esophageal sphincter (LES), leading to acid reflux and associated symptoms like heartburn, regurgitation, and chest pain.
- Esophagitis: Chronic acid exposure from GERD can cause inflammation and damage to the esophageal lining, leading to pain, difficulty swallowing, and bleeding.
- Esophageal Stricture: Scarring from chronic esophagitis can lead to narrowing of the esophagus, causing difficulty swallowing and potentially requiring dilation.
- Barrett’s Esophagus: A precancerous condition where the normal squamous epithelium of the esophagus is replaced by columnar epithelium, increasing the risk of esophageal cancer.
- Esophageal Ulcers: Open sores in the esophagus caused by acid exposure.
- Cameron Ulcers: Ulcers that occur on the herniated portion of the stomach due to mechanical trauma.
- Bleeding: Esophageal ulcers or Cameron ulcers can lead to bleeding, which may manifest as hematemesis (vomiting blood) or melena (black, tarry stools).
- Iron Deficiency Anemia: Chronic blood loss from ulcers or esophagitis can lead to iron deficiency anemia.
Respiratory Complications:
- Aspiration Pneumonia: In severe cases, refluxed stomach contents can be aspirated into the lungs, causing pneumonia.
Rare Complications:
- Volvulus: Twisting of the stomach within the hernia sac, leading to obstruction and ischemia, requiring emergency surgery.
- Incarceration: The hernia becomes trapped and cannot be reduced, leading to complications like obstruction and ischemia.
- Strangulation: Incarcerated hernia with compromised blood supply, a surgical emergency.
Prevention and Management:
Early diagnosis and management of hiatal hernia are essential to prevent complications. Lifestyle modifications, medications, and surgery are the mainstays of treatment. Regular monitoring and follow-up are crucial to detect and manage complications promptly.[10]
Investigations
Investigation of Hiatal Hernia:
The diagnosis of hiatal hernia involves a combination of clinical assessment, imaging studies, and sometimes functional tests to evaluate the extent of the hernia and associated complications.
Key Investigations:
Barium Swallow: This is often the initial imaging study performed. The patient swallows a barium contrast agent, which allows for visualization of the esophagus, stomach, and gastroesophageal junction under X-ray. A hiatal hernia will appear as a portion of the stomach protruding above the diaphragm.
Upper Endoscopy: This procedure involves inserting a flexible tube with a camera (endoscope) through the mouth to directly visualize the esophagus, stomach, and duodenum. It allows for assessment of the mucosa, identification of complications like esophagitis or Barrett’s esophagus, and biopsy if needed.
Esophageal Manometry: This test measures the pressure and coordination of muscle contractions in the esophagus. It can help assess the function of the lower esophageal sphincter (LES) and identify motility disorders that may contribute to symptoms.
24-Hour pH Monitoring: This test measures the acidity levels in the esophagus over a 24-hour period. It helps determine the frequency and severity of acid reflux episodes, especially in patients with atypical symptoms or those not responding to initial treatment.
High-Resolution Manometry (HRM): A more advanced form of esophageal manometry that provides detailed pressure topography of the esophagus, aiding in the diagnosis of subtle motility disorders.
Additional Investigations:
- Chest X-ray: May show a large hiatal hernia as an air-fluid level in the chest.
- CT Scan or MRI: Can be helpful in visualizing large or complex hiatal hernias and assessing for complications.
Choosing the Appropriate Test:
The choice of investigation depends on the patient’s clinical presentation, suspected type of hernia, and the need to evaluate for complications. Your doctor will determine the most appropriate tests based on your individual case.[7]
Treatment
Treatment of Hiatus hernia
In the great majority of cases, people experience no significant discomfort, and no treatment is required. People with symptoms should elevate the head of their beds and avoid lying down directly after meals. If the condition has been brought on by stress, stress reduction techniques may be prescribed, or if higher weighter, weight loss may be indicated.
Medications
Anti secretory drugs like proton pump inhibitors and H2 receptor blockers can be used to reduce acid secretion. Medications that reduce the lower esophageal sphincter (LES) pressure should be avoided.
Procedures
There is tentative evidence from non-controlled trials that oral neuromuscular training may improve symptoms.
Surgery
However, in some unusual instances, as when the hiatal hernia is unusually large, or is of the paraoesophageal type, it may cause esophageal stricture or severe discomfort. About 5% of hiatus hernias are paraoesophageal.
If symptoms from such a hernia are severe for example if chronic acid reflux threatens to severely injure the esophagus or is causing Barrett’s esophagus, surgery is sometimes recommended.[2]
Prevention
Prevention of Hiatal Hernia
While hiatal hernia cannot always be prevented, certain lifestyle modifications and measures can help reduce the risk of its development or minimize symptoms in individuals with existing hernias:
Maintain a Healthy Weight:
- Obesity is a significant risk factor for hiatal hernia due to increased intra-abdominal pressure. Losing weight and maintaining a healthy weight can reduce pressure on the diaphragm and lower the risk of hernia formation.
Eat Smaller, More Frequent Meals:
- Large meals increase pressure in the stomach and can contribute to hernia formation. Eating smaller portions more frequently throughout the day can help manage this pressure.
Avoid Trigger Foods and Drinks:
- Certain foods and drinks can trigger or worsen symptoms of GERD, which is often associated with hiatal hernia. These include fatty or fried foods, spicy foods, acidic foods (citrus fruits, tomatoes), chocolate, caffeine, alcohol, and carbonated beverages. Limiting or avoiding these triggers can help manage symptoms and reduce the risk of complications.
Quit Smoking:
- Smoking weakens the lower esophageal sphincter (LES), making it more susceptible to reflux and potentially contributing to hernia development. Quitting smoking can improve LES function and reduce the risk of complications.
Elevate the Head of Your Bed:
- Elevating the head of your bed by 6-8 inches can help reduce nighttime reflux and associated symptoms by using gravity to keep stomach acid from flowing back into the esophagus.
Manage Chronic Conditions:
- Conditions like chronic constipation or chronic cough can increase intra-abdominal pressure and contribute to hiatal hernia. Managing these conditions effectively can help reduce pressure and lower the risk of hernia development.
Avoid Straining and Heavy Lifting:
- Activities that involve straining or heavy lifting can increase intra-abdominal pressure and should be avoided or minimized.
Additional Measures:
- Wear loose-fitting clothing to avoid constricting the abdomen.
- Manage stress, as stress can exacerbate GERD symptoms.[11]
Please note that these are general preventive measures, and individual recommendations may vary depending on your specific situation and risk factors. Consult with your doctor for personalized advice on preventing hiatal hernia and managing associated symptoms.
Homeopathic Treatment
Homeopathic Treatment of Hiatus hernia
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Hiatus hernia:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Homoeopathic approach
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines are selected after a full individualizing examination and case-analysis, which includes the medical history of the patient, physical and mental constitution, family history, presenting symptoms, underlying pathology, possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) is also often taken into account for the treatment of chronic conditions. A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’.
The disease diagnosis is important but in homeopathy, the cause of disease is not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness are also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology is not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can be greatly improved with homeopathic medicines.
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications are also taken into account for selecting a remedy.
Medicines:
Abies nigra:
- In general, Abies nigra is effective for Hiatus hernia with a sensation as if a hardboiled egg had lodged in the cardiac end of the stomach.
- Moreover, A distressing also constriction just above the pit of the stomach, as if everything were knotted up.
- Pain in stomach immediately after eating. Lastly, Waterbrash with choked feeling in the throat.[3]
Calcarea carbonicum:
- Calcarea carb is an excellent remedy for Hiatus hernia, also it helps for strengthening the relaxed weak muscles.
- Calcarea carb is suitable for fat, flabby persons who perspire profusely.
- Heartburn also loud belching.
- Frequent sour belching, sour vomiting especially of curdled milk. Additionally, Cramps in stomach, worse pressure, cold water.
- Besides this, Swelling over pit of stomach like a saucer turned bottom up.
- Pain in epigastric region to touch.
- Aggravation while eating.
- There is a special craving for indigestible things e.g. chalk, coal, pencils etc.
Carbo veg:
- Carbo vegetabilis is excellent for Hiatus hernia with difficulty in breathing.
- A contractive pain extending to chest with distension of abdomen.
- Waterbrash, asthmatic breathing specifically from flatulence.
- Belching after eating and drinking, temporary relief from belching. Additionally, Eating the simplest kind of food causes sour belching.
- Belching, heaviness, fullness also sleepiness, tense from flatulence with pain, worse lying down.
- Epigastric region is very sensitive.
Lycopodium Clavatum:
- Lycopodium is indicated for Hiatus hernia with great weakness of digestion with much bloating, Heartburn and indigestion after takin flatulent food, cabbage, beans, oysters also onions.
- Furthermore, Belching’s rise only to pharynx.
- Patient prefers hot food also hot drinks. Craving for sweets.
Natrum phos:
- Natrum Phos is prescribed where heartburn and sour belching are present.
- Belching’s after eating.
- Spit’s mouthfuls of food. Vomiting of sour cheesy masses, especially in the morning.
- Heaviness and pressure in the epigastrium.[3]
Nux vomica:
- Nux vomica is best for Hiatus hernia with great sensitivity in the area of stomach.
- Complaints after taking highly spicy food, coffee and alcoholic drinks.
- Waterbrash, sour and bitter risings, nausea and vomiting. Indigestion with Hiatus hernia.
- The patient is highly irritable and sensitive to noise and light.
Phosphorus:
- Phosphorus is another remedy for Hiatus hernia with sour taste and sour eructation’s after every meal.
- Belching large quantities of wind after eating.
- Throws up foods by the mouthfuls.
- Water is thrown up as soon as it gets warm in the stomach.
- Pain in stomach, relieved by cold foods, ices etc.
Pulsatilla:
- Pulsatilla is effective for Hiatus hernia Where the complaints arise after taking fatty, rich foods.
- Stomach disordered and feels heavy.
- Waterbrash with foul taste in the morning.
- Heartburn and tight feeling in stomach.
Robinia:
- Robinia is one of the effective medicines for Hiatus hernia with heartburn and acidity of stomach.
- Sour stomach. Great acidity of stomach at night on lying down.
- Nausea with sour belching.
- Profuse vomiting of an intensely sour fluid. Heavy, aching, dullness in stomach.
- Very severe, sharp pains in stomach all day and night.
- Great distension of stomach and bowels.[3]
Diet & Regimen
Diet & Regimen of Hiatus hernia
The foods and beverages you should avoid-
These foods include:
- Onions and garlic
- Certain citrus fruits such as limes and oranges
- Tomatoes and tomato-based foods, such as salsa and spaghetti sauce
- Spicy foods
- Fried foods
- Foods high in sodium
- Cocoa and chocolate
- Peppermint and mint
Beverages to avoid include:
- Alcohol, such as wine, beer, and spirits
- Coffee
- Caffeinated teas
- Carbonated drinks, such as seltzer water and soda
- Whole milk [4]
Foods and beverages to eat
There are still plenty of good foods that won’t produce as much acid in your stomach. Many whole foods, for example, are good options because they aren’t processed. This means they contain more fiber, which can help with acid reflux.
Try eating:
- Non-citrus fruits, such as apples, pears, melons, and berries
- Vegetables, such as artichokes, carrots, sweet potatoes, asparagus, squash, green beans, leafy greens, and peas
- Whole grains
- Nuts and seeds, like almonds also chia seeds
- Lean protein
- Yogurt
- Plant-based milks, like either soy or almond milk
- Certain juices, like aloe Vera, carrot, or cabbage juice [4]
Do’s and Don'ts
Do’s & Don’ts
Hiatal hernia do’s & Don’ts
Do’s:
- Eat smaller, more frequent meals: This can help reduce pressure on the stomach and lower esophageal sphincter (LES), minimizing reflux.
- Maintain a healthy weight: Obesity increases intra-abdominal pressure and worsens symptoms. Losing weight can significantly improve hiatal hernia-related issues.
- Elevate the head of your bed: Raising the head of your bed by 6-8 inches can help prevent nighttime reflux by using gravity to keep stomach acid down.
- Choose foods that are easy to digest: Opt for lean proteins, vegetables, fruits, and whole grains. Avoid fatty, fried, spicy, acidic, or processed foods.
- Stay hydrated: Drink plenty of water throughout the day to aid digestion and prevent constipation, which can exacerbate symptoms.
- Manage stress: Stress can worsen GERD symptoms. Practice relaxation techniques like yoga, meditation, or deep breathing exercises.
- Follow your doctor’s recommendations: Take any prescribed medications as directed and attend follow-up appointments.
Don’ts:
- Don’t eat large meals, especially before bed: This can increase pressure on the stomach and trigger reflux.
- Don’t lie down or bend over after eating: Wait at least 2-3 hours after meals before lying down or bending over.
- Don’t smoke: Smoking weakens the LES and worsens reflux symptoms.
- Don’t wear tight-fitting clothes: Tight clothing can constrict the abdomen and increase pressure, worsening symptoms.
- Don’t consume trigger foods and drinks: Avoid or limit caffeine, alcohol, chocolate, fatty foods, spicy foods, acidic foods (citrus fruits, tomatoes), and carbonated beverages.
- Don’t lift heavy objects or engage in strenuous activity: These can increase intra-abdominal pressure and exacerbate symptoms.
Additional Tips:
- Keep a food diary: Track your meals and symptoms to identify any potential triggers.
- Eat slowly and chew thoroughly: This aids digestion and reduces the amount of air swallowed, which can worsen reflux.
- Stop eating 3 hours before bed: This gives your stomach time to empty before lying down.
- If higherweight, talk to your doctor about weight loss strategies: They can provide personalized guidance and support.
Terminology
Terminologies
Hiatal Hernia:
A condition where a portion of the stomach protrudes through the esophageal hiatus, an opening in the diaphragm.
Esophageal Hiatus:
The opening in the diaphragm through which the esophagus passes to connect to the stomach.
Gastroesophageal Junction (GEJ):
The junction between the esophagus and the stomach.
Lower Esophageal Sphincter (LES):
A ring of muscle at the end of the esophagus that acts as a valve to prevent stomach acid and contents from flowing back into the esophagus.
Gastroesophageal Reflux Disease (GERD):
A chronic condition where stomach acid and contents flow back into the esophagus, causing symptoms like heartburn and regurgitation.
Esophagitis:
Inflammation of the esophagus, often caused by acid reflux.
Barrett’s Esophagus:
A precancerous condition where the normal lining of the esophagus changes, increasing the risk of esophageal cancer.
Esophageal Stricture:
Narrowing of the esophagus, often caused by scarring from chronic inflammation.
Volvulus:
Twisting of the stomach within the hernia sac, potentially leading to obstruction and ischemia.
Incarceration:
A condition where the herniated portion of the stomach becomes trapped and cannot be reduced.
Strangulation:
A serious complication where the blood supply to the incarcerated hernia is cut off, requiring emergency surgery.
Reflux:
The backward flow of stomach acid or contents into the esophagus.
Regurgitation:
The effortless return of stomach contents to the mouth.
Heartburn:
A burning sensation in the chest caused by acid reflux.
Dysphagia:
Difficulty swallowing.
Barium Swallow:
An X-ray test using barium contrast to visualize the esophagus and stomach.
Endoscopy:
A procedure using a flexible tube with a camera to visualize the esophagus and stomach.
Manometry:
A test to measure the pressure and coordination of muscle contractions in the esophagus.
pH Monitoring:
A test to measure the acidity levels in the esophagus over time.
References
References use for Article Hiatus hernia
- Medicine Golwala
- https://en.wikipedia.org/wiki/Hiatul_hernia
- https://www.linkedin.com/pulse/homoeopathy-hiatal-hernia-hiatus-dr-ks-gopi
- https://www.healthline.com/health/hiatus-hernia-diet#cooking-tips
- The Journal of Indian Association of Pediatric Surgeons titled "Hiatal Hernia in Children" 2014.
- Schwartz’s Principles of Surgery,11th Edition, F. Charles Brunicardi, Dana K. Andersen, Timothy R. Billiar, David L. Dunn, John G. Hunter, Jeffrey B. Matthews, Raphael E. Pollock,2019,McGraw Hill Professional
- Sleisenger and Fordtran’s Gastrointestinal and Liver Disease,11th Edition, Mark Feldman, Lawrence S. Friedman, Lawrence J. Brandt,2021,Elsevier.
- Harrison’s Principles of Internal Medicine,21st Edition,Dennis L. Kasper, Anthony S. Fauci, Stephen L. Hauser, Dan L. Longo, J. Larry Jameson, Joseph Loscalzo ,2022,McGraw Hill Professional.
- Current Diagnosis & Treatment: Surgery,15th Edition,Gerard M. Doherty, 2023, McGraw Hill Professional.
- Sabiston Textbook of Surgery, 21st Edition,Courtney M. Townsend Jr., R. Daniel Beauchamp, Kenneth L. Mattox, B. Mark Evers,2022 Elsevier
- The Cleveland Clinic Guide to GERD,1st Edition, Daniel J. DeAngelo, M.D.,2011,Kaplan Publishing.
Also Search As
Also Search As
People can search for homeopathic articles on hiatal hernia in the following ways:
Online Resources:
Search Engines:
Use search engines like Google, DuckDuckGo, or Ecosia with keywords like "homeopathic treatment hiatal hernia," "homeopathy for hiatal hernia," or "homeopathic remedies GERD."
Homeopathic Websites and Forums:
Explore websites of homeopathic organizations, clinics, and practitioners, as well as online forums and communities dedicated to homeopathy. Many of these platforms offer articles, case studies, and discussions on homeopathic approaches to various conditions, including hiatal hernia.
Online Libraries and Databases:
Access online libraries and databases that specialize in alternative medicine or homeopathy. These resources may contain research articles, journal publications, and other scholarly materials on the topic.
Offline Resources:
Homeopathic Books and Journals:
Look for books and journals on homeopathy at local libraries, bookstores, or specialized homeopathic booksellers. Classic homeopathic texts like Materia Medica and repertories can also be helpful in understanding the remedies used for hiatal hernia.
Consult a Homeopathic Practitioner:
Seek guidance from a qualified homeopathic practitioner who can provide personalized advice and treatment options based on your individual symptoms and constitution.
Additional Tips:
Combine Keywords:
Use a combination of keywords related to homeopathy and hiatal hernia for a more targeted search.
Specify the Type of Information:
Indicate the type of information you’re looking for (e.g., articles, research studies, case reports) to refine your search results.
Evaluate Sources:
Always assess the credibility and reliability of the sources you find. Look for articles published in reputable journals or written by qualified homeopathic practitioners.
By utilizing these resources and search strategies, you can access a wealth of information on homeopathic approaches to hiatal hernia and make informed decisions about your healthcare.
Frequently Asked Questions (FAQ)
What is Hiatal hernia?
Definition
Hiatal hernia is a herniation of viscera, most commonly the stomach, into the mediastinum through the esophageal hiatus of the diaphragm
How is a hiatal hernia diagnosed?
Diagnosis typically involves a barium swallow X-ray, upper endoscopy, or esophageal manometry.
Can homeopathy cure hiatal hernia?
Homoeopathy For Hiatal Hernia
Homeopathy aims to address the underlying causes and symptoms of hiatal hernia, potentially leading to significant improvement and relief for some individuals.However, it is essential to consult a qualified homeopathic practitioner for individualised treatment.
What is the main cause of Hiatal hernia?
Causes
- Heavy lifting or bending over
- Frequent or hard coughing
- Hard sneezing
- Violent vomiting
- Straining during defecation
What are the symptoms of a hiatal hernia?
Symptoms
Many people with hiatal hernias have no symptoms.
Common symptoms include heartburn, acid reflux, regurgitation, difficulty swallowing, chest pain, and belching.
What are the warning signs of Hiatal hernia?
Sign
- Dull pains in the chest
- Shortness of breath
- Heart palpitations
- Swallowed food "balling up"
- Discomfort in the lower esophagus until it passes on to the stomach
- Feeling especially full after meals
- Vomiting blood or passing black stools
What are the treatment options for a hiatal hernia?
Treatment depends on the severity of symptoms and can include lifestyle modifications (weight loss, dietary changes), medications (antacids, proton pump inhibitors), or surgery for severe cases.
Are there any side effects of homeopathic remedies for hiatal hernia?
Homeopathic remedies are generally safe and well-tolerated, with minimal side effects. However, it is essential to consult a qualified practitioner to ensure proper selection and dosage of remedies.
How long does it take to see results from homeopathic treatment for hiatal hernia?
The response to homeopathic treatment varies depending on individual factors. Some individuals may experience relief within a few days, while others may take weeks or months to see significant improvement.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Hiatal hernia?
Homeopathic Medicines of Hiatal hernia
- Abies nigra
- Calcarea carb
- Carbo veg
- Lycopodium
- Natrum phos
- Nux vomica
- Phosphorus
- Pulsatilla
- Robinia
