Hypertension
Definition
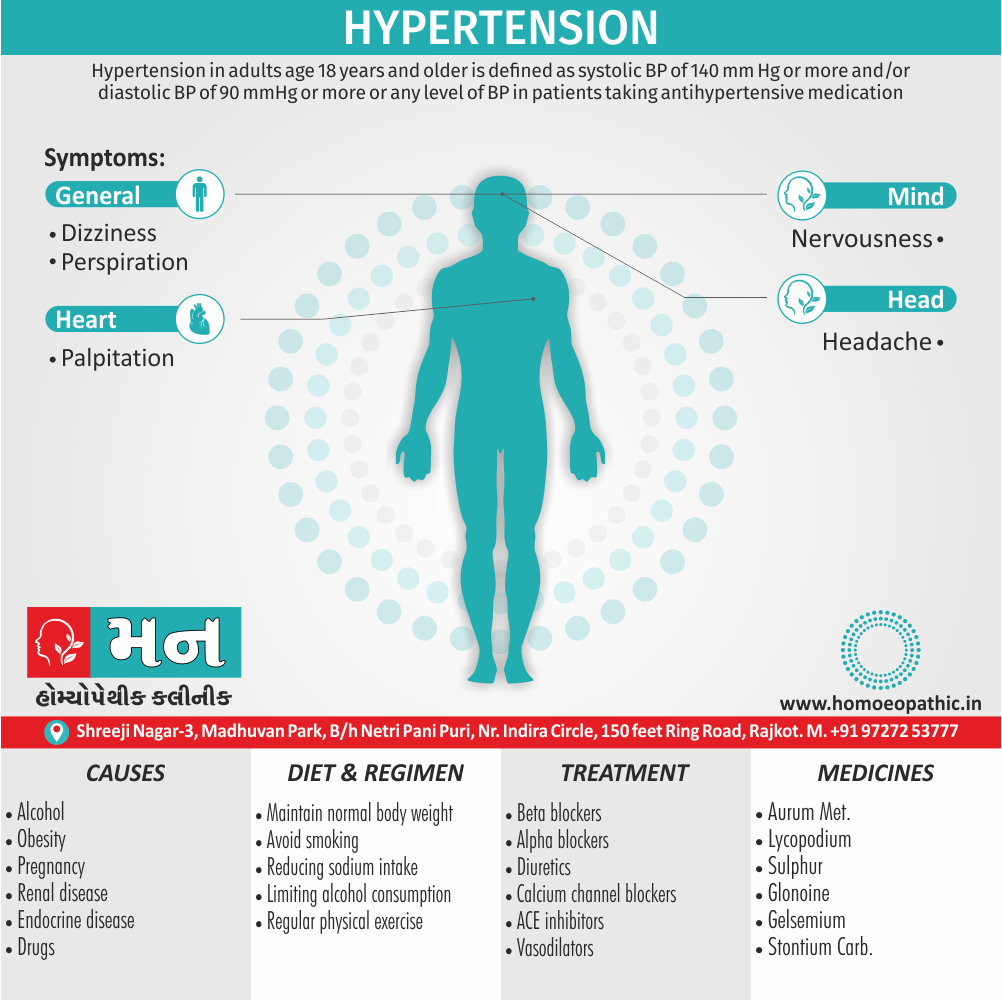
Hypertension in adults age 18 years and older, is defined as systolic BP of 140 mm Hg or more and/or diastolic BP of 90 mmHg or more or any level of BP in patients taking antihypertensive medication. [1]
Hypertension has a few well-understood synonyms you can use depending on the context:
- High blood pressure: This is the most common and straightforward synonym, easily understood by a general audience.
- Raised blood pressure: Similar to "high blood pressure," it emphasizes the elevated pressure in the arteries.
- Arterial hypertension: This term is more specific, indicating the location (arteries) where the high pressure is occurring.
Here’s when to use each option:
- General communication: Use "high blood pressure" for clear understanding.
- Medical contexts: "Hypertension" or "raised blood pressure" are both appropriate.
- Formal writing or highlighting the affected area: "Arterial hypertension" might be suitable.
Note: Avoid using less common synonyms like "hypertensive state" or "essential hypertension" unless you’re targeting a medical audience familiar with these terms.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Hypertension
- In general, Epidemiologic studies have revealed that with elevation in systolic also diastolic blood pressure above normal in adults, there is a continuous increased risk of cardiovascular disease, stroke and renal disease.
- Furthermore, Cardiovascular risk doubles with every 20 mmHg increase in systolic and 10 mmHg increase in diastolic blood pressure above normal levels.
- Recently, criteria for normal blood pressure, prehypertension and hypertension (stage 1 and stage 2) have been laid by the National Institutes of Health (NIH), US.
- Additionally, According to these criteria, normal cut-off values for systolic also diastolic blood pressure are taken as < 120 and < 80 mmHg respectively.
Overview
- In detail, As per this criteria, arterial or systemic hypertension in adults is defined clinically as persistently elevated systolic blood pressure of 140-159 mmHg, or diastolic pressure of 90-99 mmHg as stage 1 hypertension, and corresponding values above 160 or above 100 mmHg as stage 2 hypertension.
- Besides this, Cases falling between upper normal values for systolic and diastolic blood pressure (i.e. above 120/80 mmHg) and those for stage 1 hypertension (120- 139/80-89 mmHg) are grouped under prehypertension requiring monitoring and follow-up.
- The diastolic pressure is often considered more significant.
- All in all, Since blood pressure varies with many factors such as age of the patient, exercise, emotional disturbances like fear and anxiety, it is important to measure blood pressure at least twice during two separate examinations under least stressful conditions.[3]
Epidemiology
Epidemiology
The epidemiology of hypertension in India is a significant public health concern, with varying prevalence rates reported in different studies.
- A 2019 study published in the BMJ Open revealed an age-adjusted prevalence of hypertension in India of 11.3%, with a higher prevalence in men (13.8%) compared to women (10.9%). The study also found a higher prevalence in urban areas (12.5%) compared to rural areas (10.6%). (Reference: "Prevalence and associated risk factors of hypertension among adults in India: results from the fifth National Family Health Survey" – BMJ Open, 2019)[7]
- Trends in hypertension epidemiology in India (2003) indicate a lower prevalence in rural populations, although there has been a steady increase over time. Recent studies using revised criteria (BP ≥ 140 and/or 90 mmHg) have shown a high prevalence among urban adults. (Reference: "Trends in hypertension epidemiology in India" – PubMed, 2003)[8]
- The World Health Organization (WHO) reports that uncontrolled blood pressure is a major risk factor for cardiovascular diseases (CVDs), which account for a significant proportion of deaths in India. (Reference: "Hypertension" – World Health Organization) [9]
- A 2022 study published in Frontiers in Cardiovascular Medicine focused on the prevalence of hypertension in young adults (20-39 years) in Kerala, South India. The study found a prevalence ranging from 11% to 22.7%, which is considerably higher than rates reported in developed countries. (Reference: "Prevalence, Awareness, Treatment, and Control of Hypertension in Young Adults (20–39 Years) in Kerala, South India" – Frontiers, 2022) [10]
These studies highlight the importance of continuous monitoring and targeted interventions to address the growing burden of hypertension in India.
Causes
Causes of Hypertension:
- Alcohol
- Obesity
- Pregnancy (in other words, pre-eclampsia)
- Renal disease
- Parenchymal renal disease, particularly glomerulonephritis
- Renal vascular disease
- Polycystic kidney disease
- Endocrine disease i.e.
- Pheochromocytoma
- Cushing’s syndrome
- Primary hyperaldosteronism (e.g. Conn’s syndrome)
- Glucocorticoid-suppressible hyperaldosteronism
- Hyperparathyroidism
- Acromegaly
- Primary hypothyroidism
- Thyrotoxicosis
- Congenital adrenal hyperplasia
- Drugs i.e.
- E.g. Oral contraceptives containing oestrogen, anabolic steroids, corticosteroids, NSAIDs, carbenoxolone, sympathomimetic agents
- Coarctation of the aorta.[2]
Types
Classification of Hypertension
Hypertension is generally classified into 2 types i.e.:
Firstly, Primary or essential hypertension:
- In which the cause of increase in blood pressure is unknown. Essential hypertension constitutes about 80-95% patients of hypertension.
- Genetic factors
- Racial and environmental factors
- Risk factors modifying the course
Secondly, Secondary hypertension:
- In which the increase in blood pressure is caused by diseases of the kidneys, endocrines or some other organs.
- Secondary hypertension comprises remaining 5-20% cases of hypertension.
a) Renal:
- Renovascular
- Renal parenchymal diseases
b) Endocrine:
- Adrenocortical hyperfunction
- Hyperparathyroidism
- Oral contraceptives
c) Coarctation of Aorta
d) Neurogenic [2]
Risk Factors
Risk factor of Hypertension
- Age: Younger the age at which hypertension is first noted but left untreated, lower the life expectancy.
- Sex: Females with hypertension appear to do better than males.
- Atherosclerosis: Accelerated atherosclerosis invariably accompanies essential hypertension. This could be due to contributory role of other independent factors like cigarette smoking, elevated serum cholesterol, glucose intolerance and obesity.
- Other risk factors i.e.: Other factors which alter the prognosis in hypertension include: smoking, excess of alcohol intake, diabetes mellitus, persistently high diastolic pressure above normal and evidence of end-organ damage (i.e. heart, eyes, kidney and nervous system).[2]
Pathogenesis
Pathogenesis
The pathogenesis of hypertension, or high blood pressure, is a complex process involving various factors and mechanisms. A comprehensive resource for understanding this topic is:
The role of the sympathetic nervous system:
Increased sympathetic activity can lead to vasoconstriction and increased cardiac output, both of which contribute to elevated blood pressure.
The renin-angiotensin-aldosterone system (RAAS):
Activation of the RAAS leads to increased sodium and water retention, as well as vasoconstriction, further raising blood pressure.
Endothelial dysfunction:
Impaired endothelial function can disrupt the balance between vasodilators and vasoconstrictors, leading to increased vascular resistance and hypertension.
Genetic and environmental factors:
Various genetic predispositions and environmental factors, such as high sodium intake and obesity, can contribute to the development of hypertension.
By exploring these and other mechanisms, "Harrison’s Principles of Internal Medicine" offers a comprehensive understanding of the complex pathogenesis of hypertension.[11]
Pathophysiology
Pathophysiology of Hypertension
- The pathogenetic mechanism in essential hypertension is explained by many theories.
- These are as under i.e.:
- High plasma level of catecholamines.
- Increase in blood volume i.e. arterial overfilling (e.g. volume hypertension) and arteriolar constriction (e.g. vasoconstrictor hypertension).
- Increased cardiac output.
- Low-renin essential hypertension found in approximately 20% patients due to altered responsiveness to renin release.
- High rennin essential hypertension seen in about 15% cases due to decreased adrenal responsiveness to angiotensin II. [3]
Clinical Features
Clinical Features
Hypertension, often referred to as the "silent killer," is frequently asymptomatic in its early stages. However, as the condition progresses or in cases of severe hypertension, certain clinical features may manifest. A comprehensive resource for understanding these features is:
Asymptomatic Hypertension:
In most cases, particularly in the early stages, hypertension presents without any noticeable symptoms. This underscores the importance of regular blood pressure monitoring.
Symptoms of Severe Hypertension:
- Headaches: Often described as throbbing or pounding, headaches are a common symptom of severe hypertension.
- Dizziness or lightheadedness: These symptoms can occur due to impaired blood flow to the brain.
- Visual disturbances: Blurred vision or seeing spots can be a sign of damage to the blood vessels in the eyes.
- Nosebleeds: Spontaneous nosebleeds can occur due to increased pressure in the blood vessels.
- Shortness of breath: This may be a sign of heart or kidney damage resulting from prolonged hypertension.
- Chest pain: Chest pain can occur due to decreased blood flow to the heart muscle.
Signs of Target Organ Damage:
- Cardiovascular: Left ventricular hypertrophy, heart failure, coronary artery disease.
- Renal: Chronic kidney disease, proteinuria.
- Cerebrovascular: Stroke, transient ischemic attack.
- Ocular: Retinopathy.
"Braunwald’s Heart Disease" provides a thorough exploration of these clinical features, emphasizing the importance of early detection and management to prevent complications associated with hypertension.[12]
Sign & Symptoms
Sign & Symptoms of Hypertension
- There is variable elevation of the blood pressure with headache, dizziness, palpitation, perspiration also nervousness.
- Moreover, Eye ground changes may be found but papilledema is absent.
- Renal function tests and urine examination are normal in early stage.
- Besides this, In long-standing cases, there may be mild proteinuria with some hyaline or granular casts.
- occasionally, renal failure and uremia may occur.[3]
Clinical Examination
Clinical / Physical Examination For Hypertension
- Record 3 BP reading separated by 2 minutes, with patient either supine or sitting position and after standing for at least 2 minutes
- Examination of pulse and the extremities for delayed or absent femoral and peripheral arterial pulsations, bruits and pedal Oedema
- Examination of the neck for carotid murmurs, raised JVP or an enlarged thyroid gland.
- Cardiac examination for location of apex beat, abnormalities of rate and rhythm, fourth heart sound also murmur.
- Examination of lungs for rales and rhonchi.
- Abdominal examination for bruits, enlarged kidneys, masses and abnormal aortic pulsation.
- Neurological assessment and optic fundus examination. [2]
Diagnosis
Diagnosis of Hypertension
- Normal: SBP < 120mm Hg and DBP< 80mm Hg
- Prehypertension: SBP 120-139mm Hg or DBP 80-89mm Hg
- Stage 1 hypertension: SBP 140-159mm Hg or DBP 90-99mm Hg
- Stage 2 hypertension: SBP >160mm Hg or DBP >100mm Hg. [1]
Differential Diagnosis
Differential Diagnosis
It is crucial as it can either be primary (essential) with no identifiable cause, or secondary due to an underlying condition.
Primary (Essential) Hypertension:
The most common form, accounting for 90-95% of cases, with no identifiable cause.
Secondary Hypertension:
Caused by underlying conditions, this form requires identifying and managing the root cause. Some key differentials include:
- Renal: Renovascular hypertension (renal artery stenosis), chronic kidney disease, polycystic kidney disease.
- Endocrine: Primary aldosteronism, Cushing’s syndrome, pheochromocytoma, thyroid disorders, hyperparathyroidism.
- Cardiovascular: Coarctation of the aorta, sleep apnea.
- Other: Medications (e.g., oral contraceptives, NSAIDs), illicit drug use (e.g., cocaine, amphetamines), alcohol abuse.
The book Hypertension: A Companion to Braunwald’s Heart Disease provides detailed information on the clinical presentation, diagnostic workup, and management of each differential diagnosis, emphasizing the importance of a systematic approach to identify the underlying cause of secondary hypertension.[13]
Complications
Complications
Hypertension, if left untreated or poorly controlled, can lead to a multitude of complications affecting various organ systems. A comprehensive resource for understanding these complications is:
Cardiovascular Complications:
- Coronary Artery Disease (CAD): Hypertension accelerates atherosclerosis, leading to narrowing of coronary arteries and increasing the risk of angina and myocardial infarction (heart attack).
- Left Ventricular Hypertrophy (LVH): Increased workload on the heart due to high blood pressure causes thickening of the left ventricle wall, leading to heart failure and arrhythmias.
- Heart Failure: Prolonged hypertension weakens the heart muscle, impairing its ability to pump blood effectively.
- Aortic Dissection: High blood pressure can weaken the aortic wall, increasing the risk of a tear (dissection), a life-threatening condition.
Cerebrovascular Complications:
- Stroke: Hypertension is a major risk factor for both ischemic (blockage of blood flow) and hemorrhagic (bleeding) strokes.
- Transient Ischemic Attack (TIA): Often called a "mini-stroke," TIA is a temporary disruption of blood flow to the brain, often a warning sign of an impending stroke.
Renal Complications:
- Chronic Kidney Disease (CKD): Hypertension damages blood vessels in the kidneys, leading to impaired function and eventually kidney failure.
- Nephrosclerosis: Hardening of the small arteries in the kidneys due to high blood pressure, contributing to CKD.
Other Complications:
- Hypertensive Retinopathy: Damage to blood vessels in the eyes, leading to vision loss.
- Peripheral Artery Disease (PAD): Narrowing of arteries in the legs, causing pain and cramping during exercise.
- Sexual Dysfunction: Erectile dysfunction in men and decreased libido in both sex
"Kumar & Clark’s Clinical Medicine" emphasizes the importance of early detection and effective management of hypertension to prevent these serious complications.[14]
Investigations
Investigation of Hypertension
Routine i.e.:
- Urine examination for protein and glucose also microscopic for RBCs and other sediments.
- HB, fasting blood sugar, serum creatinine, total cholesterol also potassium
Additional investigations in special circumstances i.e.
- Fasting lipid profile also uric acid
- Radiograph of chest
- Echocardiogram
- USG for renal sizes
- Renal Doppler study to rule out renovascular disease
- Examination of Fundus
- Thyroid hormone profile and urinary metanephrine study in young patients. [1]
Treatment
Treatment of Hypertension
Secondary hypertension is cured by treating the disease causing hypertension.
Primary hypertension can be controlled but cannot be cured.
Following are the antihypertensive drugs to control primary hypertension:
- Beta adrenoceptor blockers: Beta adrenoceptor blockers or beta antagonists (adrenergic beta blockers or beta blockers) block the effect of sympathetic nerves on heart also blood vessels by binding with beta adrenoceptors, so that there is reduction in cardiac output and inhibition of vasoconstriction, leading to fall in blood pressure.
- Alpha adrenoceptor blockers: Alpha adrenoceptor blockers or alpha antagonists (either adrenergic alpha blockers or alpha blockers) block the effect of sympathetic nerves on blood vessels by binding with alpha adrenoceptors, leading to vasodilatation and fall in blood pressure.
- Calcium channel blockers: Calcium channel blockers are drugs, which block the calcium channels in myocardium and thereby, reduce the contractility of myocardium. It causes decrease in cardiac output and fall in blood pressure.
- Vasodilators: Vasodilator agents reduce blood pressure by vasodilatation.
- Diuretics: Diuretics cause diuresis and reduce the ECF volume and blood volume. So, blood pressure is decreased.
- Inhibitors of angiotensin-converting enzyme (in other words, ACE inhibitors): ACE inhibitors reduce the blood pressure by blocking the formation of angiotensin.
- Depressors of vasomotor center: Depressor drugs act on vasomotor center and reduce the vasomotor tone. So, vasoconstriction is prevented.
- Angiotensin II receptor blockers: Angiotensin II receptor blockers or antagonists are the antihypertensive drugs that decrease the blood pressure by blocking the effect of angiotensin II (vasoconstriction and secretion of aldosterone). [4]
Prevention
Prevention of Hypertension
- Relief of stress
- Dietary management
- Regular aerobic exercise
- Weight reduction (if needed)
- Control of other risk factors contributing to the development of arteriosclerosis. [5]
Homeopathic Treatment
Homeopathic Treatment of Hypertension
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Hypertension
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Homoeopathic Approach:
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines are selected after a full individualizing examination and case-analysis, which includes the medical history of the patient, physical and mental constitution, family history, presenting symptoms, underlying pathology, possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) is also often taken into account for the treatment of chronic conditions. A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’. The disease diagnosis is important but in homeopathy, the cause of disease is not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness are also looked for.
Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition. The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology is not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can be greatly improved with homeopathic medicines.
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications are also taken into account for selecting a remedy.
Medicines:
Aurum Met:
- High blood-pressure with despondency also suicidal tendency.
- Sensation as if the heart stopped beating. Palpitation, which compels him to remain still.
- Irregular beatings, Pulse irregular, rapid and feeble. [6]
- Sensation as if the stopped beating, immediately followed by hard rebound.
- Oppressions at the heart.
- Violent palpitation, at puberty.
- Cardiac hypertrophy.
- Pulse, rapid, feeble, also irregular. [7]
Lycopodium:
- Blood-pressure of the dyspeptics.
- Weak memory.
- Dreads Company wants to be alone.
- Irritable, thinks his end is coming. Additionally, Vertigo.
- Palpitation sensation as if the circulation stopped.
- Pulse accelerated.
- Great emaciation also of the heart.
- Sleepy during day, wakeful at night.[6]
Sulphur:
- Weak memory, dullness, vertigo.
- Palpitation of heart, worse when going up-stairs, pulse full, hard, accelerated, intermittent. [6]
- Palpitation, aggravation especially by lying, at night, in bed, going up an ascent.
- Comparatively Pulse more rapid in morning, than in the evening.
- Pericarditis with effusion.
- Sharp pains go through chest in between shoulders. [7]
Gelsemium:
- Generally; Dullness, drowsiness, dizziness, or trembling is the keynotes of this remedy.
- Desire to be left alone and to remain quite.
- Vertigo also giddiness.
- Fear of death.
- Besides this, Excessive action of the heart, palpitation.
- Sensation as if heart’s action would cease.
- Pulse slow and full, frequent soft and weak, almost imperceptible, intermittent. [6]
Strontium Carb:
- Affects the circulation causing congestive feeling of tension.
- Heart, kidneys, marrow, ankles also right side are also affected.
- Pains are fleeting; can hardly tell where they are, seemingly felt in marrow of bones; increase and decrease gradually or make the patient faint and sick all over.
- Burning, gnawing.
- Violent involuntary starts of the body.
- Immobility; of one side. – Sense of paralytic weakness.[7]
Lycopus virginicus:
- A heart remedy, lowers the blood pressure, reduces the rate of heart and increases the length of systole.
- Heart with many side symptoms, or associated with rapid tumultuous heart beats.
- Haemorrhages due to valvular heart diseases, or passive, from nose, piles, lungs etc.
- Shifting pains, from heart to eyes, head to heart, from heart to wrist etc.
- Ill effects of suppressed Haemorrhoidal flow. [7]
Glonoine:
- Wawes of terrible, bursting, pounding, headache, with feeling as if standing on the head.
- With expanding and contracting sensation or as if blood were surging back and forth in the head, from carotids to heart.
- Amelioration vomiting.
- Alternating between temples
- Aggravation by sunshine, damp days.
- Cracking, snapping, shocks, explosions or soreness deep in brain.
- Head heavy but cannot lay it on a pillow.
- Headache before, during, after or in place of menses.
- Headache ameliorates from long sleep. [7]
Diet & Regimen
Diet & Regimen
For Hypertension
Diet:
- Emphasize fruits, vegetables, and whole grains. These provide essential nutrients and fiber, which can help lower blood pressure.
- Choose lean protein sources. Opt for fish, poultry, beans, and nuts. Limit red meat and processed meats.
- Include low-fat dairy products. Milk, yogurt, and cheese can be part of a healthy diet.
- Limit saturated and unhealthy fats. Avoid fried foods, fatty meats, and processed snacks.
- Reduce sodium intake. Aim for no more than 2,300 mg of sodium per day, ideally 1,500 mg.
- Increase potassium intake. Potassium helps balance sodium levels. Good sources include bananas, sweet potatoes, and leafy greens.
- Limit alcohol consumption. Excessive alcohol can raise blood pressure.
Regimen:
- Regular exercise: Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Maintain a healthy weight: Losing even a small amount of weight can make a difference.
- Manage stress: Practice relaxation techniques like deep breathing or meditation.
- Monitor blood pressure: Regularly check your blood pressure at home or with your doctor.
- Quit smoking: Smoking significantly increases your risk of heart disease and stroke.
- Medication: If lifestyle changes aren’t enough, your doctor may prescribe medication to help manage your blood pressure.
Do’s and Don'ts
The Do’s & Don’ts
Do’s
Monitor blood pressure regularly:
Regular monitoring at home or with a healthcare provider is crucial for tracking progress and adjusting treatment as needed.
Maintain a healthy weight:
Losing even a small amount of weight can significantly lower blood pressure.
Adopt a balanced diet:
The DASH (Dietary Approaches to Stop Hypertension) diet, rich in fruits, vegetables, whole grains, and low-fat dairy products, has been proven to lower blood pressure.
Reduce sodium intake:
Aim for less than 2,300 milligrams of sodium per day, ideally 1,500 milligrams. Read food labels carefully and avoid processed foods, which are often high in sodium.
Increase potassium intake:
Foods rich in potassium, such as bananas, spinach, and sweet potatoes, can help lower blood pressure. Consult a healthcare provider before taking potassium supplements.
Limit alcohol consumption:
If you drink alcohol, do so in moderation. For men, that means up to two drinks a day; for women, up to one drink a day.
Engage in regular physical activity:
Aim for at least 150 minutes of moderate-intensity exercise or 75 minutes of vigorous-intensity exercise per week.
1. bondibeauty.com.aubondibeauty.com.auManage stress:
Practice relaxation techniques such as deep breathing, meditation, or yoga.
Take medications as prescribed:
If prescribed medication for hypertension, take it consistently and as directed by your healthcare provider.
Attend regular checkups:
Regular visits to your healthcare provider are essential for monitoring your blood pressure, adjusting treatment plans, and detecting any potential complications.
Don’ts
Don’t ignore symptoms:
While hypertension is often asymptomatic, be aware of potential signs like headaches, dizziness, or vision changes and seek medical attention if needed.
Don’t smoke:
Smoking damages blood vessels and significantly increases the risk of heart disease and stroke.
Don’t consume excessive caffeine:
While moderate caffeine intake is generally safe, excessive amounts can raise blood pressure temporarily.
Don’t rely solely on over-the-counter medications:
Consult your healthcare provider before taking any over-the-counter medications for pain or cold relief, as some can raise blood pressure.
Don’t skip doses of medication:
Missing doses can lead to fluctuations in blood pressure and increase the risk of complications.
Don’t self-treat:
Consult your healthcare provider for proper diagnosis and treatment of hypertension. Self-treatment can be dangerous and may delay necessary medical intervention.
By following these do’s and don’ts, individuals with hypertension can effectively manage their condition, reduce the risk of complications, and improve their overall health and well-being.
Terminology
Terminology
It is Used in Articles on Hypertension and Their Meanings:
Blood Pressure (BP):
The force exerted by circulating blood against the walls of blood vessels. It is measured in millimeters of mercury (mmHg) and expressed as two numbers: systolic pressure (the higher number) over diastolic pressure (the lower number).
Hypertension:
A chronic medical condition characterized by persistently elevated blood pressure. It is defined as a systolic blood pressure of 140 mmHg or higher and/or a diastolic blood pressure of 90 mmHg or higher.
Systolic Blood Pressure (SBP):
The pressure in your arteries when your heart beats.
Diastolic Blood Pressure (DBP):
The pressure in your arteries when your heart rests between beats.
Essential (Primary) Hypertension:
The most common type of hypertension, with no identifiable underlying cause. It is thought to be caused by a combination of genetic and environmental factors.
Secondary Hypertension:
Hypertension caused by an underlying medical condition, such as kidney disease, adrenal gland disorders, or sleep apnea.
White Coat Hypertension:
A phenomenon where blood pressure readings are higher in a medical setting than at home, likely due to anxiety.
Masked Hypertension:
The opposite of white coat hypertension, where blood pressure readings are normal in a medical setting but elevated at home.
Hypertensive Crisis:
A severe elevation in blood pressure that requires immediate medical attention, as it can lead to organ damage.
Target Organ Damage (TOD):
Damage to organs such as the heart, kidneys, brain, or eyes caused by prolonged or uncontrolled hypertension.
Antihypertensive Medications:
Drugs used to lower blood pressure. There are various classes of antihypertensive medications, each working through different mechanisms.
Lifestyle Modifications:
Changes to diet, exercise habits, and other lifestyle factors that can help lower blood pressure and reduce the risk of complications.
Hypertensive Encephalopathy:
A severe complication of hypertension characterized by brain swelling and dysfunction.
Hypertensive Retinopathy:
Damage to the blood vessels in the retina of the eye caused by high blood pressure.
Hypertensive Nephropathy:
Damage to the kidneys caused by high blood pressure, which can lead to chronic kidney disease and kidney failure.
Terminologies used in Homeopathic articles on Hypertension and their meanings:
Similimum:
The homeopathic remedy that most closely matches the totality of symptoms experienced by the individual, both physical and mental/emotional.
Repertory:
A reference book used by homeopaths to find remedies based on specific symptoms.
Materia Medica:
A comprehensive reference book detailing the symptoms and therapeutic uses of homeopathic remedies.
Potentization:
The process of diluting and succussing (vigorously shaking) a substance to increase its therapeutic potency.
Constitutional Type:
The individual’s unique physical, mental, and emotional characteristics, which are considered when selecting a homeopathic remedy.
Aggravation:
A temporary worsening of symptoms after taking a homeopathic remedy, often seen as a positive sign that the remedy is working.
Proving:
A systematic process of testing a substance on healthy individuals to determine its potential therapeutic effects.
Miasm:
A predisposition to certain types of diseases, believed to be inherited or acquired. Homeopathic treatment often considers miasmatic tendencies.
Vital Force:
The energy that animates and maintains life, believed to be disturbed in illness and restored by homeopathic remedies.
Law of Similars:
The fundamental principle of homeopathy, stating that a substance that can cause symptoms in a healthy person can cure similar symptoms in a sick person.
Specific remedies mentioned in homeopathic articles on hypertension and their key indications:
- Aconitum Napellus: For sudden onset hypertension with anxiety and palpitations.
- Belladonna: For hypertension with a flushed face, throbbing headache, and dilated pupils.
- Glonoinum: For hypertension with a pulsating headache and a feeling of fullness in the head.
- Natrum Muriaticum: For hypertension associated with grief, suppressed emotions, and fluid retention.
- Nux Vomica: For hypertension in irritable, ambitious individuals with digestive problems.
- Rauwolfia Serpentina: For hypertension with anxiety, insomnia, and nervous tension.
It is important to note that homeopathic treatment should always be individualized and supervised by a qualified homeopathic practitioner.
References
References use for Article Hypertension:
- Golwala’s medicine for students 25th edition 2017
- Davidson’s principles and practice of medicine 22nd
- Textbook of pathology by Harsh Mohan 6th
- Essentials of medical physiology by K. Sembuligam 6th
- Harrison’s Principle of external medicine 16th
- The homoeopathic family practice by M.Bhattacharya
- "Prevalence and associated risk factors of hypertension among adults in India: results from the fifth National Family Health Survey" – BMJ Open, 2019.
- "Trends in hypertension epidemiology in India" – PubMed, 2003.
- "Hypertension" – World Health Organization.
- "Prevalence, Awareness, Treatment, and Control of Hypertension in Young Adults (20–39 Years) in Kerala, South India" – Frontiers, 2022.
Harrison’s Principles of Internal Medicine (21st edition),Authors: Dennis L. Kasper, Anthony S. Fauci, Stephen L. Hauser, Dan L. Longo, J. Larry Jameson, Joseph Loscalzo,(2022),Publisher: McGraw Hill.
Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine (12th edition),Editors: Douglas P. Zipes, William J. Stevenson, Joseph Loscalzo
(2022),Publisher: Elsevier.Hypertension: A Companion to Braunwald’s Heart Disease (4th Edition),Editors: Henry R. Black, William J. Elliott,(2020),Publisher: Elsevier.
Kumar & Clark’s Clinical Medicine (10th Edition),Editors: Parveen Kumar, Michael L. Clark,(2021),Publisher: Elsevier
Also Search As
Also Search As
People can search for homeopathic articles on hypertension in several ways:
Online Resources:
Search engines: Using keywords like "homeopathy hypertension," "homeopathic remedies for high blood pressure," or "homeopathic treatment for hypertension" on search engines like Google, DuckDuckGo, or Ecosia can yield numerous articles, blog posts, and research papers.
Homeopathic journals and websites: Many reputable homeopathic organizations and journals publish articles on hypertension. Examples include:
- The National Center for Homeopathy (NCH): https://www.homeopathycenter.org/
- The American Institute of Homeopathy (AIH): https://homeopathyusa.org/
- The International Journal of High Dilution Research: [invalid URL removed]
Online databases: Databases like PubMed or Google Scholar may include research articles on homeopathic interventions for hypertension.
Offline Resources:
Homeopathic libraries: Many cities have homeopathic libraries or clinics with collections of books and journals on homeopathy, including articles on hypertension.
Homeopathic practitioners: Consulting a qualified homeopathic practitioner can provide access to relevant articles and resources.
Additional Tips:
Specify your search: Use specific keywords like the names of homeopathic remedies (e.g., "Aconitum Napellus for hypertension") or specific symptoms (e.g., "homeopathy for hypertension with anxiety").
Look for peer-reviewed articles: For reliable information, prioritize articles published in peer-reviewed journals or reputable homeopathic organizations.
Consult a homeopathic practitioner: If you have questions or are considering homeopathic treatment for hypertension, consult a qualified practitioner for personalized advice and guidance.
By utilizing these resources and strategies, individuals can access a wealth of information on homeopathic approaches to hypertension, enabling them to make informed decisions about their healthcare.
There are numerous ways to search for information on hypertension, each catering to different needs and preferences:
Online Search Engines:
Use search terms like "hypertension," "high blood pressure," "symptoms of hypertension," "causes of hypertension," or "treatment of hypertension."
Popular search engines include Google, Bing, DuckDuckGo, or Ecosia.
Be specific with your search terms to get more relevant results.
Reputable Health Websites:
Websites of organizations like the World Health Organization (WHO), Mayo Clinic, American Heart Association (AHA), and National Institutes of Health (NIH) offer comprehensive information on hypertension.
Look for websites ending in .gov, .edu, or .org for reliable information.
Medical Journals and Databases:
PubMed and Google Scholar are good resources for finding scientific articles and research papers on hypertension.
Search for specific topics or keywords to narrow down your search.
Books and Libraries:
Medical textbooks and reference books on cardiovascular health or internal medicine often have dedicated sections on hypertension.
Visit your local library or bookstore for a wide selection of books on the topic.
Healthcare Professionals:
Your doctor or other healthcare providers can be a valuable resource for information on hypertension.
Ask questions about your specific concerns or risk factors.
Support Groups and Online Communities:
Joining online forums or support groups for people with hypertension can provide a platform for sharing experiences and getting advice.
Social Media:
Following reputable health organizations on social media can provide updates on the latest research and guidelines on hypertension.
Mobile Apps:
Many apps are available for tracking blood pressure, providing information on hypertension, and offering tips for managing the condition.
Educational Videos:
YouTube and other video platforms host educational videos on hypertension created by healthcare professionals and organizations.
Choose the method that best suits your needs and preferences. Always verify the information you find with a healthcare professional before making any decisions about your health.
Frequently Asked Questions (FAQ)
What is Hypertension?
Definition
Hypertension in adults age 18 years and older, is defined as systolic BP of 140 mm Hg or more and/or diastolic BP of 90 mmHg or more or any level of BP in patients taking antihypertensive medication.
What causes Hypertension?
- Alcohol
- Obesity
- Pregnancy (pre-eclampsia)
- Renal disease
- Endocrine disease
Give the types of Hypertension?
- Primary or essential hypertension
- Secondary hypertension
What are the symptoms of Hypertension?
Symptoms
- Variable elevation of the blood pressure
- Headache
- Dizziness
- Palpitation
- Perspiration
- Nervousness.
- Eye ground changes may be found but papilledema is absent
How does homeopathic treatment for hypertension work?
A homeopath will conduct a detailed consultation to understand your physical and emotional symptoms, medical history, and lifestyle. Based on this, they will select a remedy tailored to your specific needs.
Can homeopathy help with hypertension?
Homeopathy aims to address the underlying causes of hypertension, considering individual symptoms and constitution. While some studies suggest potential benefits, more research is needed to confirm its effectiveness.
How long does homeopathic treatment for hypertension take?
The response time varies. Some may experience improvement within weeks, while others may take longer. Chronic cases may require ongoing treatment.
Are there any side effects of homeopathic remedies?
Homeopathic remedies are generally considered safe when taken as directed. In rare cases, a temporary worsening of symptoms (aggravation) may occur.
Can I take homeopathic remedies alongside conventional medications for hypertension?
It’s generally safe to combine homeopathic remedies with conventional medications. However, inform your doctor and homeopath about all medications you are taking.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Hypertension?
Homeopathic Medicines for Hypertension
- Aurum Met
- Lycopodium
- Sulphur
- Gelsemium
- Strontium Carb
- Lycopus virginicus
- Glonoine
