Inflammatory Bowel Disease
Definition:
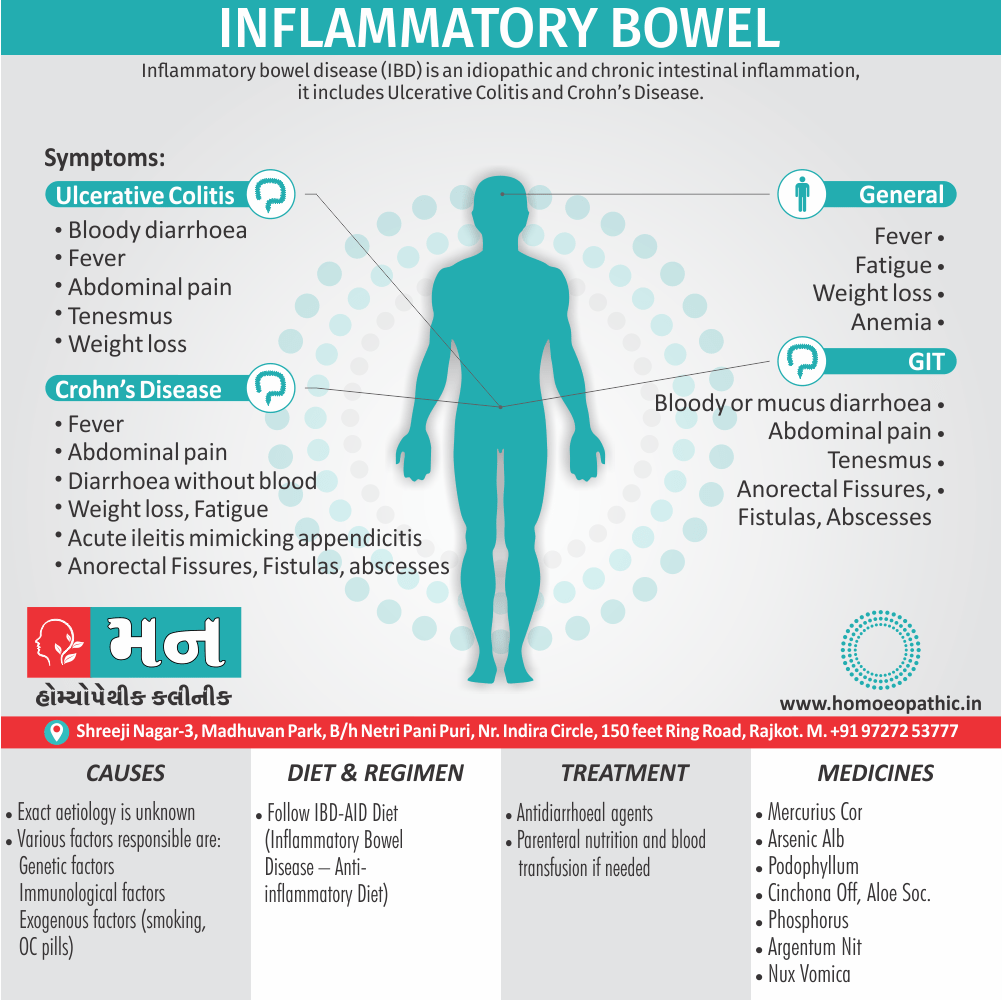
Inflammatory bowel disease (IBD) is an idiopathic and chronic intestinal inflammation.[1]
Inflammatory bowel disease (IBD) itself doesn’t have a direct synonym, but it encompasses two main conditions:
- Crohn’s disease: This can affect any part of the digestive tract, from the mouth to the anus.
- Ulcerative colitis: This primarily affects the inner lining of the large intestine (colon) and rectum.
There’s also a category called indeterminate colitis, which presents features of both Crohn’s and ulcerative colitis.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Inflammatory Bowel Disease (IBD)
Inflammatory bowel disease (IBD) is a chronic, relapsing inflammatory condition of the gastrointestinal tract. The two main types of IBD are Crohn’s disease and ulcerative colitis. Both diseases are characterized by abnormal immune responses, causing inflammation, ulcers, and damage to the lining of the digestive tract.
Crohn’s Disease:
- This can affect any part of the digestive tract, from the mouth to the anus. It often involves the small intestine and the beginning of the large intestine. The inflammation can extend through the entire thickness of the bowel wall.
Ulcerative Colitis:
- This affects only the colon (large intestine). The inflammation usually begins in the rectum and extends upwards continuously. Unlike Crohn’s, it affects only the innermost lining of the colon.
Symptoms:
Both Crohn’s disease and ulcerative colitis share common symptoms, including:
- Abdominal pain and cramping
- Rectal bleeding
- Weight loss
- Fatigue
- Fever
Causes:
- The exact cause of IBD is unknown. However, it is believed to involve a complex interaction between genetic predisposition, environmental factors, and an abnormal immune response to the gut’s normal bacteria.
Treatment: Treatment aims to control inflammation, relieve symptoms, and prevent complications. It often involves a combination of medications (anti-inflammatory drugs, immunosuppressants, biologics), dietary modifications, and, in some cases, surgery. [6]
Epidemiology
Epidemiology
The epidemiology of inflammatory bowel disease (IBD) in India is rapidly evolving, with a significant increase in incidence and prevalence observed in recent years. While population-based studies on the exact prevalence of Crohn’s disease (CD) are lacking, a prospective study across 13 Asia Pacific countries estimated the mean annual incidence in (South) Indians to be 3.91 (95% CI 3.31–4.57/100000 population) for CD and 5.40 (95% CI 4.70–6.18/100000 population) for ulcerative colitis (UC).
The Global Burden of Disease (GBD) study estimated the number of IBD patients in India to be 2.7 lakhs (0.27 million) in 2019, a substantial increase from 1.3 lakhs in 1990. However, some experts believe these figures might underestimate the actual burden of IBD in India, as clinical practice suggests a higher number of new cases.
Reference:
Rapidly changing epidemiology of inflammatory bowel disease: Time to gear up for the challenge before it is too late
Indian Journal of Gastroenterology
Year of Publication: 2023
This article provides a comprehensive overview of the current epidemiological trends of IBD in India, highlighting the need for further research and improved healthcare infrastructure to address this growing public health concern. [7]
Causes
Causes
This refers to the initiating factors that trigger a disease process.
- Examples of causes include:
- Pathogens: Viruses, bacteria, fungi, parasites (infectious diseases)
- Genetic mutations: Inherited or spontaneous changes in genes (genetic diseases)
- Environmental factors: Toxins, radiation, nutritional deficiencies
- Lifestyle choices: Smoking, unhealthy diet, lack of exercise (contributing factors)
Types
Types
- Types of InflammatoryThe term ‘inflammatory bowel disease (IBD)’is commonly used to include 2 idiopathic bowel disease having many similarities but the conditions usually have distinctive morphological appearance.
- These 2 conditions are Crohn’s disease (regional enteritis) and ulcerative colitis [2]
Risk Factors
Risk Factors
The exact aetiology of IBD remains unknown. However, multiple factors are implicated which can be considered under the following 3 groups:
1. Genetic factors:
- There is about 3 to 20 times higher incidence of occurrence of IBD in first-degree relatives.
- There is approximately 50% chance of development of IBD in monozygotic twins.
- Although no specific and consistent gene association with IBD has been seen, genome wide search has revealed that disease-predisposing loci are present in chromosomes 16q, 12p, 6p, 14q and 5q.
2. Immunologic factors:
- Defective immunologic regulation in IBD has been shown to play significant role in the pathogenesis of IBD:
- Defective regulation of immune suppression
- Transgenic mouse experimental model studies
- Type of inflammatory cells.
- In both types of IBD, activated CD4+ T cells are present in the lamina propria and in the peripheral blood.
- These cells either activate other inflammatory cells (e.g. macrophages and B cells), or recruit more inflammatory cells by stimulation of homing receptor on leucocytes and vascular endothelium.
There are two main types of CD4+ T cells in IBD:
TH1 cells secrete proinflammatory cytokines IFN-γ and TNF which induce transmural granulomatous inflammation seen in Crohn’s disease. IL-12 initiates TH1 cytokine pathway.
TH2 cells secrete IL-4, IL-5 and IL-13 which induce superficial mucosal inflammation characteristically seen in ulcerative colitis.
3. Exogenous factors:
Microbial factors
Psychosocial factors
Smoking
Oral contraceptives [2]
Pathogenesis
Pathogenesis of Inflammatory Bowel Disease (IBD)
The exact cause of IBD remains unknown, but it is believed to arise from a complex interplay of genetic predisposition, environmental triggers, and a dysregulated immune response to the gut microbiome.
Key Factors in IBD Pathogenesis:
Genetic Predisposition:
- Numerous genetic variants have been associated with an increased risk of IBD. These genes are involved in immune regulation, epithelial barrier function, and microbial sensing.
Environmental Factors:
- Diet, smoking, infections, and antibiotic use have been implicated as potential environmental triggers for IBD. These factors can alter the gut microbiome and immune responses, potentially contributing to disease development.
Dysregulated Immune Response:
- In IBD, the immune system mistakenly attacks the harmless bacteria in the gut, leading to chronic inflammation. This immune dysregulation involves both the innate and adaptive immune systems.
Gut Microbiome Dysbiosis:
- The gut microbiome plays a crucial role in maintaining intestinal health. In IBD, there is an imbalance in the gut microbiome, known as dysbiosis, characterized by a decrease in beneficial bacteria and an increase in potentially harmful bacteria. This dysbiosis can further exacerbate inflammation and contribute to disease progression.
Impaired Epithelial Barrier Function:
- The intestinal epithelium acts as a barrier between the gut lumen and the underlying immune cells. In IBD, this barrier function is compromised, allowing bacteria and other antigens to penetrate the epithelium, triggering an immune response and perpetuating inflammation. [8]
Pathophysiology
Pathophysiology
- Activation of immune cells by unknown inciting agent (microorganism, dietary component, bacterial or self-antigen)
- Leading to release of cytokines and inflammatory mediator [3]
Clinical Features
Clinical Features
ULCERATIVE COLITIS:
A. Macroscopic features
- UC usually involves the rectum and extends proximally to involve all or part of the colon.
- Proximal spread occurs in continuity without areas of uninvolved mucosa. When the whole colon is involved, the inflammation extends 1 to 2 cm into the terminal ileum. This is called backwash ileitis and is of little clinical significance.
- With mild inflammation, the mucosa is erythematous and has a fine granular surface that looks like sandpaper. In more severe disease, the mucosa is haemorrhagic, oedematous, and ulcerated.
- In long-standing disease, inflammatory polyps may be present because of epithelial regeneration.
- In patients with many years of disease it appears atrophic and featureless, and the entire colon becomes narrowed and shortened.
- Patients with fulminant disease can develop a toxic colitis or megacolon where the bowel wall thins, and the mucosa is severely ulcerated; this may lead to perforation.
B. Microscopic Features:
- The process is limited to the mucosa and superficial submucosa, with deeper layers unaffected except in fulminant disease. In UC, two major histologic features are indicative of chronicity and help distinguish it from infectious or acute self-limited colitis.
- First, the crypt architecture of the colon is distorted; crypts may be bifid and reduced in number, often with a gap between the crypt bases and the muscularis mucosae.
- Second, some patients have basal plasma cells and multiple basal lymphoid aggregates.
- Mucosal vascular congestion with oedema and focal haemorrhage, and an inflammatory cell infiltrate of neutrophils, lymphocytes, plasma cells, and macrophages may be present.
- The neutrophils invade the epithelium, usually in the crypts, and give rise to cryptitis and, ultimately, to crypt abscesses.
CROHN’S DISEASE:
A. Microscopic features:
- CD can affect any part of the gastrointestinal tract from the mouth to the anus.
- Unlike UC, which almost always involves the rectum, the rectum is often spared in CD.
- CD is segmental, with skip areas amidst a diseased intestine.
- Perirectal fistulas, fissures, abscesses, and anal stenosis are present in one-third of patients with CD.
- Endoscopically, aphthous or small superficial ulcerations characterize mild disease; in more active disease, stellate ulcerations fuse longitudinally and transversely to demarcate islands of mucosa that frequently are histologically Normal.
- This “cobblestone” appearance is characteristic of CD, both endoscopically and by barium radiography.
- Active CD is characterized by focal inflammation and formation of fistula tracts, which resolve by fibrosis and stricturing of the bowel which can cause obstructions.
- Projections of thickened mesentery encase the bowel (“creeping fat”), and serosa and mesenteric inflammation promote adhesions and fistula formation.
B. Macroscopic features:
- The earliest lesions are aphthoid ulcerations and focal crypt abscesses with loose aggregations of macrophages, which form noncaseating granulomas in all layers of the bowel wall from mucosa to serosa.
- Granulomas can be seen in lymph nodes, mesentery, peritoneum, liver, and pancreas.
- Although granulomas are a pathognomonic feature of CD, they are rarely found on mucosal biopsies. Surgical resection reveals granulomas in about half of cases.
- Other histologic features of CD include submucosal or subserosal lymphoid aggregates, particularly away from areas of ulceration, gross and microscopic skip areas, and transmural inflammation that is accompanied by fissures that penetrate deeply into the bowel wall and sometimes form fistulous tracts or local abscesses.[1]
Sign & Symptoms
Sign & Symptoms
Ulcerative Colitis:
- The major symptoms of UC are diarrhoea, rectal bleeding, tenesmus, passage of mucus, and crampy abdominal pain.
- Patients with proctitis usually pass fresh blood or blood-stained mucus, either mixed with stool or streaked onto the surface of a normal or hard stool.
- They also have tenesmus, or urgency with a feeling of incomplete evacuation.
- When the disease extends beyond the rectum, blood is usually mixed with stool or grossly bloody diarrhea occurs.
- When the disease is severe, patients pass a liquid stool containing blood, pus, and faecal matter.
- Diarrhoea is often nocturnal and/or postprandial.
- Severe cramping and abdominal pain can occur in association with severe attacks of the disease.
- Other symptoms in moderate to severe disease include anorexia, nausea, vomiting, fever, and weight loss.
- Patients with a toxic colitis have severe pain and bleeding, and those with megacolon have hepatic tympany.[1]
Crohn’s Disease:
- CD involves following 2 patterns:
- a fibro stenotic-obstructing pattern
- a penetrating-fistulous pattern
Ileocolitis:
- The most common site of inflammation is the terminal ileum, the usual presentation of ileocolitis is a chronic history of recurrent episodes of right lower quadrant pain and diarrhoea.
- Weight loss is common.
- In the early stages of disease, bowel wall Edema and spasm produce intermittent obstructions and symptoms of postprandial pain.
Jejunoileitis:
- Extensive inflammatory disease is associated with a loss of digestive and absorptive surface, resulting in malabsorption and steatorrhea.
Colitis and Perianal Disease:
- Colitis
- low-grade fevers, malaise, diarrhoea, crampy abdominal pain, and sometimes haematochezia.
- Pain is caused by passage of faecal material through narrowed and inflamed segments of large bowel.
- Strictures can occur in the colon and produce symptoms of bowel obstruction.
Gastroduodenal Disease:
Clinical Examination
Clinical Examination of Inflammatory Bowel Disease (IBD)
The clinical examination of patients with suspected IBD is crucial for assessing disease activity, identifying complications, and guiding further investigations.
Key Components of the Clinical Examination:
History:
- Detailed history taking is essential, including:
- Onset, duration, and pattern of symptoms (e.g., abdominal pain, diarrhea, rectal bleeding)
- Presence of extraintestinal manifestations (e.g., joint pain, skin rashes, eye inflammation)
- Family history of IBD
- Past medical history and medication use
Physical Examination:
- General appearance: Assess for signs of malnutrition, weight loss, or pallor
- Abdominal examination: Palpate for tenderness, masses, or distension
- Rectal examination: Look for anal fissures, fistulas, or perianal disease
- Extraintestinal manifestations: Assess for joint swelling, skin rashes, or eye inflammation
Laboratory Tests:
- Complete blood count (CBC): Check for anemia or signs of inflammation
- Inflammatory markers (C-reactive protein, erythrocyte sedimentation rate): Assess for inflammation
- Stool tests: Check for occult blood, infection, or inflammation
Imaging Studies:
- Abdominal X-ray: Rule out bowel obstruction or perforation
- Ultrasound, CT scan, or MRI: Assess bowel wall thickness, inflammation, or complications
- Capsule endoscopy or balloon-assisted enteroscopy: Visualize the small bowel
Endoscopy:
- Colonoscopy or sigmoidoscopy: Direct visualization of the colon and rectum with biopsy
- Upper endoscopy: Visualize the esophagus, stomach, and duodenum [9]
Diagnosis
Diagnosis
Ulcerative Colitis:
- Sigmoidoscopy/colonoscopy: mucosal erythema, granularity, friability, exudate, haemorrhage, ulcers, inflammatory polyps (pseudo polyps).
- Barium enema: loss of haustrations, mucosal irregularity, ulcerations.
Crohn’s Disease:
- Sigmoidoscopy/colonoscopy, barium enema, upper GI and small-bowel series shows:
- Nodularity, rigidity, ulcers that may be deep or longitudinal, cobble stoning, skip areas, strictures, fistulas.
- CT scan:
- Shows thickened, matted bowel loops or an abscess.[3]
Differential Diagnosis
Differential Diagnosis
- Ischemic bowel disease
- Appendicitis
- Diverticulitis
- Radiation enterocolitis
- Bile salt-induced diarrhoea (ileal resection)
- Drug-induced colitis (e.g., NSAIDs)
- Bleeding colonic lesion (e.g., neoplasm)
- Irritable bowel syndrome (no bleeding)
- Microscopic (lymphocytic) or collagenous colitis (chronic watery diarrhoea)-normal colonoscopy but biopsies show superficial colonic epithelial inflammation
- In collagenous colitis, a thick subepithelial layer of collagen; response to amino salicylates and glucocorticoids variable.[3]
Complications
Complications of Inflammatory Bowel Disease (IBD)
Inflammatory bowel disease (IBD) can lead to various complications, both within the gastrointestinal (GI) tract and in other organ systems. These complications can significantly impact a patient’s quality of life and may require additional medical or surgical interventions.
Gastrointestinal Complications:
- Bowel Strictures: Narrowing of the bowel due to chronic inflammation, leading to obstruction and abdominal pain.
- Fistulas: Abnormal connections between different parts of the bowel or between the bowel and other organs (e.g., bladder, skin), causing infections and drainage.
- Abscesses: Collections of pus that can form in the bowel wall or surrounding tissues, causing pain, fever, and sepsis.
- Perforation: A hole in the bowel wall, leading to leakage of intestinal contents into the abdomen, a life-threatening emergency.
- Toxic Megacolon: Severe dilation and inflammation of the colon, potentially leading to perforation and sepsis.
- Increased Risk of Colorectal Cancer: Especially in patients with long-standing ulcerative colitis.
Extraintestinal Complications:
- Joint Problems: Arthritis, arthralgia (joint pain)
- Skin Manifestations: Erythema nodosum (red, tender nodules), pyoderma gangrenosum (ulcers)
- Eye Inflammation: Uveitis, episcleritis
- Liver Disease: Primary sclerosing cholangitis (PSC), fatty liver
- Bone Loss: Osteoporosis
- Blood Clots: Deep vein thrombosis (DVT), pulmonary embolism (PE) [9]
Investigations
Investigations
Ulcerative Colitis:
- Complete Blood Count (low Hb, rise in platelet count, leucocytosis)
- Rise in Erythrocyte sedimentation rate (ESR)
- C-Reactive Protein (increased)
- Stool Examination
- Histology of rectal or colonic biopsy specimens.
- Sigmoidoscopy
- Contrast Barium Enema
Crohn’s Disease:
- Complete Blood Count (low Hb, rise in platelet count, leucocytosis)
- Rise in Erythrocyte sedimentation rate (ESR)
- C-Reactive Protein (increased)
- Serum Albumin (low)
- Endoscopy
- Colonoscopy
- CT scan
- MRI [1]
Treatment
Treatment
- Antidiarrheal agents (diphenoxylate and atropine, loperamide) in mild disease.
- IV hydration and blood transfusions in severe disease; Parenteral nutrition or defined enteral formulas effective as primary therapy in Crohn’s Disease.
- Emotional support [3]
Prevention
Prevention of Inflammatory Bowel Disease (IBD)
While there is no definitive way to prevent inflammatory bowel disease (IBD) due to its complex and multifactorial nature, emerging research suggests that certain lifestyle modifications and interventions may help reduce the risk of developing the disease or lessen its severity.
Potential Preventive Measures:
Dietary Modifications:
- Increase Fiber Intake: A diet rich in fruits, vegetables, and whole grains can promote a healthy gut microbiome and reduce inflammation.
- Limit Processed Foods: Processed foods, high in sugar, fat, and additives, have been linked to an increased risk of IBD.
- Consider Probiotics: Probiotics, found in yogurt, kefir, and supplements, contain beneficial bacteria that may help maintain gut health.
Lifestyle Changes:
- Quit Smoking: Smoking is a major risk factor for Crohn’s disease and can worsen IBD symptoms.
- Moderate Alcohol Consumption: Excessive alcohol intake can irritate the gut lining and exacerbate inflammation.
- Manage Stress: Stress can trigger or worsen IBD flare-ups. Techniques like yoga, meditation, or mindfulness may help manage stress.
Early Intervention:
- Prompt Diagnosis and Treatment: Early diagnosis and appropriate treatment can help control inflammation and prevent complications.
- Regular Follow-up: Regular check-ups with a gastroenterologist can help monitor disease activity and adjust treatment plans as needed. [10]
Homeopathic Treatment
Homeopathic Treatment of IBD
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic medicines for Inflammatory Bowel Disease
Mercurius Corrosivus:
- For Blood and Mucus in Stool in Ulcerative Colitis.
- This medicine is suited to those patients in whom blood and shreds of mucus membranes are passed along with the stool.
- There is constant urge to pass stool that is scanty, hot and have offensive odour.
- There is recurrent urge of stool with no satisfaction.
- There are cutting pains in the rectum accompany the passage of stool.
Colchicum Autumnale:
- For Ulcerative Colitis with Jelly-like Mucus in Stool.
- Nausea and faintness from the odour of cooking food, mainly eggs and meat.
Arsenicum Album:
- For Ulcerative Colitis with Stool of offensive Odour and Blood.
- Patient complains of offensive and dark coloured blood stool which is aggravated at night and the patient feels lethargic.
- There is constant burning pain in abdomen and rectum which is relieved by warm drinks.
Phosphorus:
- For Ulcerative Colitis with Stool Containing Blood and Greenish Mucus and there is extreme offensiveness.
- The complaint gets aggravated in the morning. There is excessive craving for cold drinks, ice cream and juicy things.
Aloe Socotrina:
- For Crohn’s Disease with Loose Stool which worse immediately after eating or drinking anything.
- There is sudden urge to pass stool and patient has to rush to the toilet to pass the stool.
- There are cutting pains in lower abdomen which get worse before and during passing stool and relieved after passing the stool.
- Faintness usually follows stool. This medicine can also prescribed to control the diarrhoea that gets worse due to the intake of beer.
Podophyllum:
Cinchona Officinalis:
Argentum Nitricum:
- For Crohn’s Disease with Watery Green Stool and Flatulence.
- The diarrhoea mainly gets worse by over- eating sweets or after any emotional excitement.
Sulphur:
- Remedy for IBD with diarrhoea that get worse in the morning.
- Patient must rush out of bed early morning to pass out stool.
- The soles of feet, palms and head are hot.
Nux Vomica:
- It is indicated for Inflammatory Bowel Disease with tenesmus.
- The patient suffered from ineffectual but constant urge to pass stool.
- The stool is scanty with no satisfaction. There is recurrent urge to pass stool at very short intervals.
- There is pain in the abdomen which is relieved for a little while after passing of stool, but reappears very soon.
Mercurius Solubilis:
- It is another remedy which is indicated for tenesmus in Inflammatory Bowel Disease.
- The stool is slimy, blood-stained accompanied with excessive chilliness.[5]
Diet & Regimen
Diet & Regimen
Irritable Bowel Disease Diet and regimen
Dietary Strategies:
Potential Limits (depending on triggers):
- High-fiber foods (raw fruits, vegetables, whole grains)
- Spicy, fatty foods
- Dairy products
- Alcohol, caffeine
- Processed foods
Foods to Emphasize:
- Low-fiber foods during flares (cooked/canned fruits/veggies)
- Lean protein
- Hydration (plenty of water)
- Small, frequent meals
- Probiotic-rich foods (yogurt)
Lifestyle Strategies:
- Manage stress (exercise, meditation)
- Regular gentle exercise
- Quit smoking
- Adequate sleep
- Medication adherence (if prescribed)
- Regular checkups with your doctor
Do’s and Don'ts
Do’s & Don’ts
Inflammatory bowel Disease Do’s & Don’ts
Do’s:
- Maintain a Food Diary: Track your meals and symptoms to identify trigger foods that worsen your symptoms.
- Eat Small, Frequent Meals: This can help reduce the strain on your digestive system.
- Stay Hydrated: Drink plenty of fluids, especially water, to prevent dehydration, especially during flare-ups.
- Choose Low-Fiber Foods During Flare-ups: Opt for easily digestible foods like cooked vegetables, white rice, and lean proteins.
- Consider Probiotics: Probiotics may help restore a healthy gut microbiome and reduce inflammation.
- Manage Stress: Stress can trigger flare-ups, so practice relaxation techniques like yoga, meditation, or deep breathing exercises.
- Exercise Regularly: Moderate exercise can help reduce stress, improve bowel function, and boost your overall well-being.
- Get Adequate Sleep: Sleep is essential for immune function and overall health.
- Take Medications as Prescribed: Follow your doctor’s instructions regarding medications and dosage.
- Attend Regular Check-ups: Regular appointments with your gastroenterologist are crucial for monitoring disease activity and adjusting treatment as needed.
Don’ts:
- Smoke: Smoking can worsen IBD symptoms and increase the risk of complications.
- Consume Excessive Alcohol: Alcohol can irritate the gut lining and trigger flare-ups.
- Skip Meals: Skipping meals can lead to low blood sugar and worsen fatigue.
- Eat High-Fiber Foods During Flare-ups: High-fiber foods can be difficult to digest and may worsen symptoms during flare-ups.
- Consume Trigger Foods: Identify and avoid foods that trigger your symptoms.
- Ignore Symptoms: If you experience new or worsening symptoms, contact your doctor.
- Self-Medicate: Always consult your doctor before starting any new supplements or over-the-counter medications.[11]
Terminology
Terminology:
Inflammatory Bowel Disease (IBD):
- A group of chronic inflammatory disorders of the gastrointestinal (GI) tract, primarily Crohn’s disease and ulcerative colitis.
Crohn’s Disease:
A type of IBD that can affect any part of the GI tract, from the mouth to the anus, causing inflammation, ulcers, and complications.
Ulcerative Colitis (UC):
- A type of IBD that affects only the colon (large intestine), causing inflammation and ulcers in the innermost lining.
Remission:
- A period of time when IBD symptoms are minimal or absent, and inflammation is controlled.
Flare-up:
- A period of increased disease activity, with worsening of symptoms and inflammation.
Extraintestinal Manifestations:
- Symptoms or complications of IBD that occur outside of the GI tract, such as joint pain, skin rashes, or eye inflammation.
Immunosuppressants:
- Medications that suppress the immune system’s activity, used to control inflammation in IBD.
Biologics:
- Targeted therapies that block specific proteins involved in the inflammatory process, used for moderate to severe IBD.
Colectomy:
- Surgical removal of the colon, performed in severe cases of ulcerative colitis.
Bowel Resection:
- Surgical removal of a diseased portion of the bowel, performed in Crohn’s disease.
Fistulizing Disease:
- The development of fistulas (abnormal connections) between the bowel and other organs or the skin, a complication of Crohn’s disease.
Stricture:
- A narrowing of the bowel lumen due to chronic inflammation, a complication of Crohn’s disease.
Dysbiosis:
- An imbalance in the gut microbiome, with a decrease in beneficial bacteria and an increase in harmful bacteria, often associated with IBD.
Terminologies and Meanings in Homeopathic Articles:
Totality of Symptoms:
- This refers to the complete picture of the patient’s physical, mental, and emotional symptoms, which is essential for selecting the appropriate homeopathic remedy.
Repertory:
- A book that lists symptoms and the homeopathic remedies associated with them, used by homeopaths to find the most suitable remedy for a patient.
Materia Medica:
- A comprehensive reference book that describes the properties and symptoms of homeopathic remedies.
Constitutional Remedy:
- A remedy that matches the patient’s overall constitution, including their physical, mental, and emotional characteristics, and is used to address the underlying cause of their disease.
Acute Remedy:
- A remedy used to treat the immediate, acute symptoms of a flare-up, such as pain, diarrhea, or bleeding.
Aggravation:
- A temporary worsening of symptoms after taking a homeopathic remedy, often seen as a sign that the remedy is working.
Potency:
- The strength or dilution of a homeopathic remedy. Higher potencies are believed to have a deeper and longer-lasting effect.
Miasm:
- A predisposition to certain types of diseases, according to homeopathic theory. The three main miasms are psora (related to skin conditions and functional disorders), sycosis (related to overgrowth and chronic inflammation), and syphilis (related to destructive processes).
Proving:
- A process in which healthy volunteers take a homeopathic remedy and record their symptoms, helping to understand the remedy’s potential effects.
Individualization:
- The process of tailoring homeopathic treatment to the unique needs of each patient, based on their individual symptoms and constitution.
References
References
- Harrison’s Principles of Internal Medicine 16th Edition
- Harsh Mohan’s Textbook of Pathology
- Harrison’s Manual of Medicine 19th Edition
- The Inflammatory Bowel Disease Anti-Inflammatory Diet (verywellhealth.com)
- A homoeopathic approach to inflammatory bowel disease (IBD) (homoeopathicjournal.com)
Book Inflammatory Bowel Disease: Pathogenesis, Diagnosis, and Management, Editors: Ramona Rajapakse, Publisher: Springer
Year of Publication: 2021, Edition: 1st- Rapidly changing epidemiology of inflammatory bowel disease:Indian Journal of Gastroenterology, Year of Publication: 2023
Book Inflammatory Bowel Disease: A Comprehensive Review, Author: Ashwin N. Ananthakrishnan, Publisher: Springer, Year of Publication: 2015, Edition: 1st
Book Sleisenger and Fordtran’s Gastrointestinal and Liver Disease, Review and Assessment, Authors: Anthony J. DiMarino Jr., Chung Owyang, Publisher: Elsevier, Year of Publication: 2021, Edition: 11th
Book Inflammatory Bowel Disease: Diagnosis and Therapeutics
Editors: William J. Sandborn, Stephan R. Targan, Publisher: Elsevier, Year of Publication: 2016
Edition: 4thBook The Crohn’s and Colitis Diet Guide, Author: Liz Lipski, PhD, CCN, Publisher: Keats Publishing
Year of Publication: 2005, Edition: 3rd
Also Search As
Also Search As
Online Resources:
- Homeopathic Journals and Databases: Reputable online journals like The Homoeopathic Journal and Indian Journal of Research in Homoeopathy often publish case reports and research articles related to homeopathy and IBD.
- ResearchGate: This platform allows researchers to share their work, including homeopathic studies on IBD.
- Google Scholar: A broader search engine, Google Scholar can help you find scholarly articles and research papers on the topic.
Specific Search Terms:
- "homeopathic treatment inflammatory bowel disease"
- "homeopathy for Crohn’s disease"
- "homeopathy for ulcerative colitis"
- "case reports homeopathy IBD"
Other Tips:
- Consult a Homeopathic Practitioner: They can provide personalized recommendations and resources based on your specific case.
- Look for Reputable Sources: Prioritize articles from peer-reviewed journals and well-established homeopathic organizations.
By combining these approaches, you can find a wealth of information on the homeopathic approach to managing IBD.
Important Note: It’s crucial to remember that homeopathy is a complementary therapy and should not replace conventional medical treatment for IBD.
Always consult with a qualified healthcare professional for proper diagnosis and treatment.
There are several ways to search for information on Inflammatory Bowel Disease (IBD):
Online Search Engines:
- Use search engines like Google, Bing, or DuckDuckGo with keywords like "inflammatory bowel disease," "IBD," "Crohn’s disease," or "ulcerative colitis." This will lead you to websites, articles, and resources on IBD.
- Reputable Medical Websites:
- Mayo Clinic: Provides comprehensive information on IBD symptoms, causes, diagnosis, and treatment.
- Cleveland Clinic: Offers an overview of IBD, including risk factors, complications, and lifestyle changes. (https://my.clevelandclinic.org/health/diseases/15587-inflammatory-bowel-disease-overview)
Medical Libraries and Databases:
- PubMed: A free resource for searching biomedical literature, including research articles and clinical studies on IBD.
- MedlinePlus: A service of the National Library of Medicine, providing consumer-friendly health information on IBD.
Books and Publications:
- Sleisenger and Fordtran’s Gastrointestinal and Liver Disease: A comprehensive textbook covering all aspects of IBD.
- Inflammatory Bowel Disease: A Comprehensive Review: Provides an in-depth overview of IBD pathogenesis, diagnosis, and management.
Social Media Groups and Forums:
- Online communities can connect you with other individuals living with IBD, offering support, advice, and shared experiences. Look for groups on platforms like Facebook or Reddit.
Healthcare Professionals:
- Consult with a gastroenterologist or other healthcare provider specializing in IBD for personalized information and guidance.
By utilizing these resources, you can gain a comprehensive understanding of IBD, its symptoms, causes, treatment options, and available support networks.
Frequently Asked Questions (FAQ)
What causes IBD?
Causes
The exact cause is unknown, but it is believed to involve a complex interaction of genetic predisposition, environmental triggers, and an abnormal immune response to the gut microbiome.
How is IBD diagnosed?
Diagnosis typically involves a combination of medical history, physical examination, laboratory tests (blood tests, stool tests), imaging studies (X-ray, CT scan, MRI), and endoscopy (colonoscopy or sigmoidoscopy).
What are the symptoms of IBD?
Symptoms
Common symptoms include abdominal pain, diarrhea, rectal bleeding, weight loss, fatigue, and fever.
However, the specific symptoms can vary depending on the type and severity of IBD.
Is homeopathic treatment safe for IBD?
Homeopathic remedies are generally considered safe when prescribed and monitored by a qualified homeopathic practitioner.
However, it is crucial to inform your conventional doctor about any homeopathic treatment you are receiving.
What are the treatment options for IBD?
Treatment aims to control inflammation, relieve symptoms, and prevent complications.
It may involve medications (anti-inflammatory drugs, immunosuppressants, biologics), dietary modifications, and in some cases, surgery.
What is inflammatory bowel disease (IBD)?
Definition:
IBD is a group of chronic inflammatory disorders of the gastrointestinal (GI) tract, primarily Crohn’s disease and ulcerative colitis.
What are the homeopathic remedies for IBD?
Homeopathic medicines for IBD
There is no single remedy for IBD in homeopathy. The choice of remedy depends on the individual’s unique symptoms, overall constitution, and the specific type of IBD (Crohn’s disease or ulcerative colitis). Some commonly used remedies include Arsenicum album, Nux vomica, Mercurius corrosivus, and Sulphur.
How does homeopathic treatment for IBD work?
Homeopathic practitioners assess the individual’s symptoms and constitution to select a remedy that matches their specific needs.
The remedy, given in highly diluted form, aims to stimulate the body’s healing response and reduce inflammation.
How long does homeopathic treatment for IBD take?
The duration of treatment varies depending on the individual’s response and the severity of the condition. Some people may experience improvement in symptoms within weeks or months, while others may require longer-term treatment.
Can homeopathy cure inflammatory bowel disease (IBD)?
Homeopathy aims to stimulate the body’s natural healing abilities and manage symptoms.
While some individuals report positive experiences, homeopathy is not a proven cure for IBD and should not replace conventional medical treatment.
