Irritable bowel syndrome (IBS)
Definition
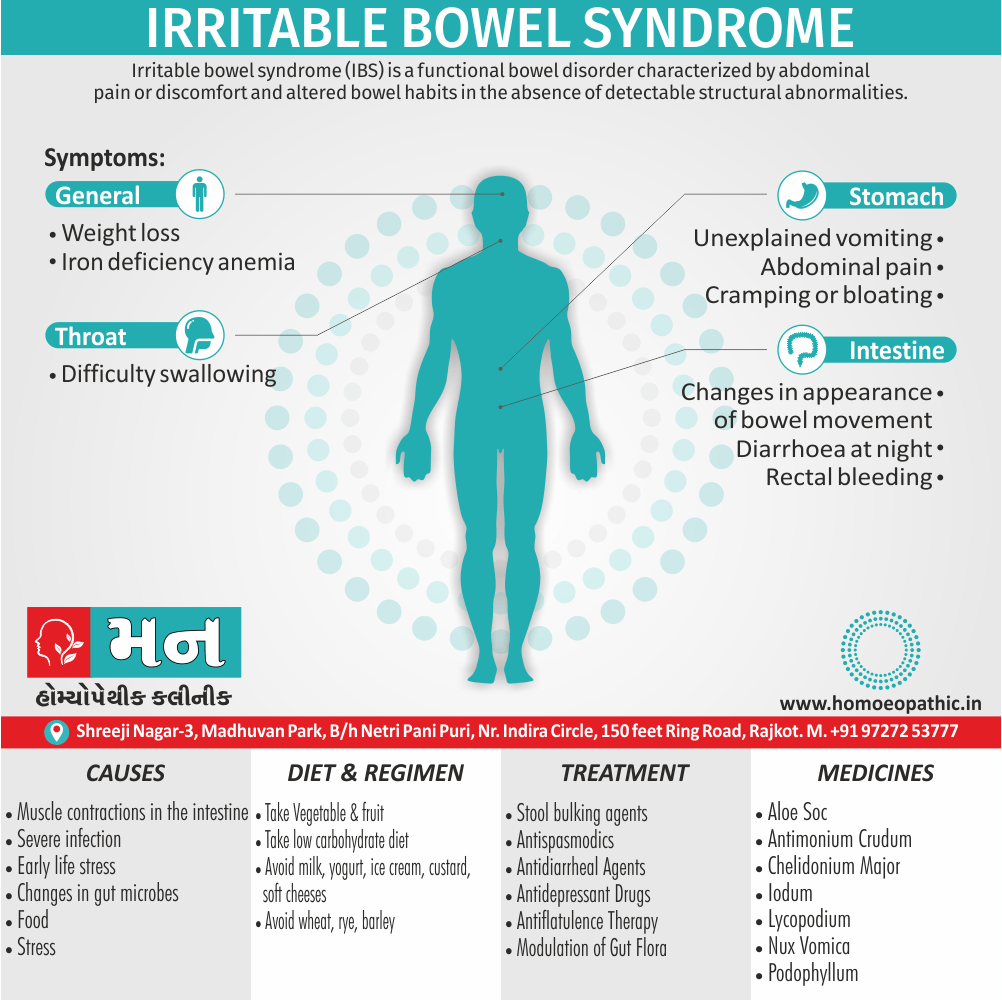
Irritable bowel syndrome (IBS) is a functional bowel disorder characterized by abdominal pain or discomfort and altered bowel habits in the absence of detectable structural abnormalities. [1]
Here are some synonyms for irritable bowel syndrome (IBS):
- Spastic colon
- Nervous colon
- Mucous colitis
- Functional bowel disease
It’s important to note that some of the older terms, like mucous colitis, are not used as commonly anymore. IBS is the most widely used and accepted term.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Irritable bowel syndrome (IBS)
No clear diagnostic markers exist for IBS, thus, the diagnosis of the disorder is based on clinical presentation. In 2006, the Rome II criteria for the diagnosis of IBS were revised.
Moreover, Throughout the world, about 10–20% of adults and adolescents have symptoms consistent with IBS, and most studies show a female predominance.
Severity of symptoms varies and can significantly impair quality of life, resulting in high health care costs. Advances in basic, mechanistic, and clinical investigations have improved our understanding of this disorder and its physiologic and psychosocial determinants. [1]
Epidemiology
Epidemiology
The epidemiology of Irritable Bowel Syndrome (IBS) in India is characterized by a few key points:
Prevalence: The prevalence of IBS in the Indian community varies widely, ranging from 0.4% to 7.9%, depending on the study population and diagnostic criteria used.
Increasing Trend: The prevalence of IBS in India appears to be increasing, potentially due to factors such as changing dietary habits, increased stress levels, and greater awareness of the condition.
Regional Variation: There may be regional variations in the prevalence of IBS within India, with some studies suggesting a lower prevalence in rural areas compared to urban areas.
Gender Distribution: While some studies report a higher prevalence of IBS in women, others suggest a more balanced gender distribution, particularly in community-based studies.
Overlapping Conditions: IBS often overlaps with other functional gastrointestinal disorders, such as functional dyspepsia, adding complexity to its diagnosis and management.
References:
- Ghoshal UC, Abraham P, Bhatt C, et al. Epidemiological and clinical profile of irritable bowel syndrome in India: report of the Indian Society of Gastroenterology Task Force. Indian J Gastroenterol. 2008 Mar-Apr;27(2):22-9.
- Madisch A, Palsson OS, Andresen V, et al. Indian consensus statements on irritable bowel syndrome in adults: A guideline by the Indian Neurogastroenterology and Motility Association and jointly supported by the Indian Society of Gastroenterology. J Neurogastroenterol Motil. 2022 Aug 30;28(3):379-400.
- Aziz I, Palit S, Hossain S, et al. Epidemiological and clinical perspectives on irritable bowel syndrome in India, Bangladesh and Malaysia: A review. World J Gastroenterol. 2017 Oct 7;23(37):6788-6802.
Please note that the epidemiology of IBS is a dynamic field with ongoing research, and the figures mentioned here are based on available data.[6][7][8]
Causes
Causes of Irritable bowel syndrome (IBS)
The precise cause of IBS isn’t known. Factors that appear to play a role include:
Muscle contractions in the intestine i.e.:
The walls of the intestines are lined with layers of muscle that contract as they move food through your digestive tract. Contractions that are stronger and last longer than normal can cause gas, bloating and diarrhea. Weak intestinal contractions can slow food passage and lead to hard, dry stools.
Nervous system i.e.:
Abnormalities in the nerves in your digestive system may cause you to experience greater than normal discomfort when your abdomen stretches from gas or stool. constipation.
Severe infection i.e.:
IBS can develop after a severe bout of diarrhoea (gastroenteritis) caused by bacteria or a virus
Early life stress i.e.:
People exposed to stressful events, especially in childhood, tend to have more symptoms of IBS.
Changes in gut microbes i.e.:
Examples include changes in bacteria, fungi and viruses, which normally reside in the intestines also play a key role in health.
Triggered factors are:
Food i.e.:
The role of food allergy or intolerance in IBS isn’t fully understood. Additionally, A true food allergy rarely causes IBS.
Stress i.e.:
Most people with IBS experience worse or more-frequent signs and symptoms during periods of increased stress. But while stress may aggravate symptoms, it doesn’t cause them. [2]
Types
Types
Irritable Bowel Syndrome (IBS) is classified into four main types, based on the predominant bowel habit:
IBS with Constipation (IBS-C):
This type is characterized by infrequent bowel movements, hard or lumpy stools, and straining during defecation.
IBS with Diarrhea (IBS-D):
In this type, frequent loose or watery stools, urgency to defecate, and abdominal cramping are common.
IBS with Mixed Bowel Habits (IBS-M):
This type involves alternating episodes of constipation and diarrhea, with abdominal pain and bloating.
IBS Unclassified (IBS-U):
This type refers to cases where symptoms do not fit neatly into the other categories.
This comprehensive textbook Sleisenger and Fordtran’s Gastrointestinal and Liver Disease Review and Assessment provides in-depth information on the pathophysiology, diagnosis, and management of irritable bowel syndrome and its various subtypes. It is a valuable resource for healthcare professionals and researchers interested in this prevalent gastrointestinal disorder.[9]
Risk Factors
Risk factor of Irritable bowel syndrome (IBS)
Many people have occasional signs and symptoms of IBS. But you’re more likely to have the syndrome if you:
- Are young- IBS occurs more frequently in people under age 50.
- Are female- In the United States, IBS is more common among women. Additionally, Estrogen therapy before or after menopause also is a risk factor for IBS.
- Have a family history of IBS- Genes may play a role, as may shared factors in a family’s environment or a combination of genes also environment.
- Have anxiety, depression or other mental health issues- A history of sexual, either physical or emotional abuse also might be a risk factor. [2]
Pathogenesis
Pathogenesis
The pathogenesis of IBS is poorly understood, although roles of abnormal gut motor and sensory activity, central neural dysfunction, psychological disturbances, mucosal inflammation, stress, also luminal factors have been proposed. [1]
Pathophysiology
Pathophysiology
The pathophysiology of Irritable Bowel Syndrome (IBS) is complex and multifactorial, involving a combination of factors:
Altered Gut Motility:
Many individuals with IBS experience abnormal contractions of the intestines, leading to either slow transit (constipation) or rapid transit (diarrhea). This altered motility may be due to dysregulation of the enteric nervous system or hormonal imbalances.
Visceral Hypersensitivity:
People with IBS often have heightened sensitivity to sensations in their gut, causing them to experience pain or discomfort from normal amounts of gas or stretching. This hypersensitivity may be due to changes in nerve signaling or processing in the brain.
Brain-Gut Interaction:
The brain and gut communicate bidirectionally, and disruptions in this communication can contribute to IBS symptoms. Stress, anxiety, and depression can worsen gut symptoms, while gut problems can also affect mood and mental well-being.
Gut Microbiota:
The community of bacteria in the gut, known as the microbiota, plays a role in gut health and may be altered in IBS. Changes in the gut microbiota can affect motility, inflammation, and sensitivity, potentially contributing to symptoms.
Inflammation:
Low-grade inflammation in the gut lining has been observed in some individuals with IBS. This inflammation may be triggered by infections, stress, or dietary factors, and it could contribute to pain and altered bowel habits.
This comprehensive textbook Sleisenger and Fordtran’s Gastrointestinal and Liver Disease Review and Assessment provides a detailed discussion on the pathophysiology of IBS, exploring the various mechanisms involved in its development and manifestation. It offers insights into the latest research findings and clinical implications, making it a valuable resource for healthcare professionals and researchers seeking to understand this complex disorder.[9]
Clinical Features
Clinical Features
The clinical features of Irritable Bowel Syndrome (IBS) are diverse and can vary significantly among individuals. However, some common characteristics include:
Abdominal Pain and Discomfort:
This is a hallmark symptom of IBS and can manifest as cramping, bloating, or a feeling of fullness. The pain is often relieved by passing stool or gas.
Altered Bowel Habits:
Changes in bowel habits are common in IBS and can involve constipation, diarrhea, or a combination of both. The frequency and consistency of stools may fluctuate.
Bloating and Gas:
Many people with IBS experience bloating and excessive gas, which can contribute to abdominal discomfort and distension.
Mucus in Stool:
While not always present, the passage of mucus with stool is a possible symptom of IBS.
Other Symptoms:
Additional symptoms may include nausea, fatigue, backache, and urinary urgency or frequency.
This comprehensive textbook Sleisenger and Fordtran’s Gastrointestinal and Liver Disease Review and Assessment provides a thorough overview of the clinical features of IBS, highlighting the variability and overlap with other functional gastrointestinal disorders. It discusses the diagnostic criteria and the importance of a careful evaluation to rule out other potential causes of symptoms.[9]
Sign & Symptoms
Sign & Symptoms of Irritable bowel syndrome (IBS)
The signs and symptoms of IBS vary but are usually present for a long time. The most common include:
- Abdominal pain, either cramping or bloating that is related to passing a bowel movement
- Changes in appearance of bowel movement
- Changes in how often you are having a bowel movement
- Other symptoms that are often related include bloating, increased either gas or mucus in the stool.
More-serious signs and symptoms include:
Clinical Examination
Clinical Examination
The clinical examination for Irritable Bowel Syndrome (IBS) is generally unremarkable, as there are no specific physical findings unique to the condition. However, it plays a crucial role in:
Assessing Abdominal Tenderness:
The physician may palpate the abdomen to identify areas of tenderness, which can be diffuse or localized, and may vary in intensity depending on the individual.
Detecting Abdominal Distention:
The examiner may observe abdominal distention or bloating, which can be a sign of gas accumulation or altered bowel function.
Evaluating Bowel Sounds:
Listening to bowel sounds with a stethoscope can help assess intestinal activity and identify any abnormal patterns, such as increased or decreased bowel sounds.
Rectal Examination:
A digital rectal examination may be performed to assess for any abnormalities in the rectum or anal canal, and to check for stool consistency.
This comprehensive textbook Sleisenger and Fordtran’s Gastrointestinal and Liver Disease Review and Assessment emphasizes the importance of a thorough clinical examination in the evaluation of IBS. It outlines the steps involved in the physical examination and highlights the potential findings that may be relevant in the diagnostic process. The book also discusses the role of the clinical examination in differentiating IBS from other gastrointestinal disorders with similar symptoms.[9]
Diagnosis
Diagnosis of Irritable bowel syndrome (IBS)
There’s no test to definitively diagnose IBS. Your doctor is likely to start with a complete medical history, physical exam and tests to rule out other conditions, such as celiac disease.
After other conditions have been ruled out, your doctor is likely to use one of these sets of diagnostic criteria for IBS:
Rome criteria:
These criteria include abdominal pain and discomfort lasting on average at least one day a week in the last three months, associated with at least two of these factors: Pain and discomfort are related to defecation, the frequency of defecation is altered, or stool consistency is altered.
Type of IBS:
For the purpose of treatment, IBS can be divided into three types, based on your symptoms: constipation-predominant, diarrhoea-predominant or mixed.
Your doctor will also likely assess whether you have other signs or symptoms that might suggest another, more serious, condition.
These signs and symptoms include:
- Onset of signs and symptoms after age 50
- Weight loss
- Rectal bleeding
- Fever
- Nausea or recurrent vomiting
- Abdominal pain, especially if it’s not related to a bowel movement, or occurs at night
- Diarrhoea that is persistent or awakens you from sleep
- Anemia related to low iron
If you have these signs or symptoms, or if an initial treatment for IBS doesn’t work, you’ll likely need additional tests. [2]
Differential Diagnosis
Differential Diagnosis of Irritable bowel syndrome (IBS)
- Inflammatory bowel disease as in Crohn’s disease (ulcerative colitis)
- Intestinal pseudo-obstruction
- Abuse of medications such as laxatives or bowel binders
- Lactose intolerance
- Psychiatric disorders (such as depression, anxiety or somatization disorder)
- Infections of the digestive tract
- Malabsorption syndromes (such as celiac disease or pancreatic insufficiency)
- Endocrine disorders (such as hypothyroidism, hyperthyroidism, diabetes or Addison’s disease)
- Certain rare endocrine tumors (such as gastrinoma or carcinoid tumors)
- Carcinomas of the intestine [5]
Complications
Complications
Irritable Bowel Syndrome (IBS) itself is not a life-threatening condition and does not typically lead to serious complications like inflammatory bowel disease or colon cancer.
However, chronic and severe IBS can be associated with the following:
Impaired Quality of Life:
The recurrent abdominal pain, altered bowel habits, and other symptoms can significantly impact a person’s daily life, work, and social activities, leading to emotional distress and decreased quality of life.
Mood Disorders:
People with IBS are more likely to experience anxiety and depression, which can further worsen IBS symptoms and create a vicious cycle.
Hemorrhoids:
Chronic constipation or diarrhea associated with IBS can increase the risk of developing hemorrhoids (swollen blood vessels in the anus and rectum).
While this textbook Sleisenger and Fordtran’s Gastrointestinal and Liver Disease Review and Assessment does not specifically list complications in a dedicated section, it discusses the impact of IBS on quality of life and the association with psychological comorbidities. It also addresses the management of constipation and diarrhea, which can help prevent associated complications like hemorrhoids.[9]
Investigations
Investigation
The investigation of Irritable Bowel Syndrome (IBS) primarily focuses on ruling out other potential causes of symptoms and confirming the diagnosis based on established criteria. The following investigations may be considered:
Complete Blood Count (CBC):
To assess for anemia, which could indicate bleeding or inflammation in the gut.
C-Reactive Protein (CRP) and Erythrocyte Sedimentation Rate (ESR):
To evaluate for inflammation, which may suggest other conditions like inflammatory bowel disease.
Celiac Disease Serology:
To rule out celiac disease, an autoimmune disorder triggered by gluten.
Stool Tests:
To check for infections (e.g., parasites, bacteria), occult blood (hidden blood in stool), and inflammation.
Hydrogen Breath Test:
To detect lactose intolerance or small intestinal bacterial overgrowth (SIBO), which can contribute to IBS symptoms.
Colonoscopy or Flexible Sigmoidoscopy:
To visualize the colon and rectum and rule out structural abnormalities or inflammation.
Imaging Studies (e.g., CT scan, MRI):
Rarely used in IBS diagnosis, but may be considered if there are atypical symptoms or concerns about other conditions.
This comprehensive textbook Sleisenger and Fordtran’s Gastrointestinal and Liver Disease Review and Assessment provides a detailed overview of the investigations used in the diagnosis of IBS. It discusses the rationale behind each test, their sensitivity and specificity, and the potential findings that may be relevant in the diagnostic process. The book also emphasizes the importance of tailoring the investigation based on the individual’s clinical presentation and risk factors.[9]
Treatment
Treatment of Irritable bowel syndrome (IBS)
Stool-Bulking Agents
- High-fiber diets and bulking agents, such as bran or hydrophilic colloid, are frequently used in treating IBS.
- The water-holding action of fibers may contribute to increased stool bulk because of the ability of fiber to increase fecal output of bacteria. Fiber also speeds up colonic transit in most persons.
Antispasmodics
- Clinicians have observed that anticholinergic drugs may provide temporary relief for symptoms such as painful cramps related to intestinal spasm.
Antidiarrheal Agents
- Peripherally acting opiate-based agents are the initial therapy of choice for IBS-D.
Antidepressant Drugs
- In addition to their mood-elevating effects, antidepressant medications have several physiologic effects that suggest they may be beneficial in IBS.
Antiflatulence Therapy
- The management of excessive gas is seldom satisfactory, except when there is obvious aerophagia or disaccharides deficiency.
Modulation of Gut Flora
- Antibiotic treatment benefits a subset of IBS patients.
Prevention
Prevention
While there is no definitive way to prevent Irritable Bowel Syndrome (IBS), certain lifestyle modifications and dietary changes may help reduce the risk of developing the condition or alleviate symptoms in those already diagnosed:
Dietary Changes:
- Increase Fiber Intake: Gradually increase the consumption of soluble fiber (found in oats, fruits, vegetables, and legumes) to promote regular bowel movements and reduce constipation.
- Limit Trigger Foods: Identify and avoid foods that trigger symptoms, such as fatty or greasy foods, caffeine, alcohol, carbonated beverages, and artificial sweeteners.
- FODMAP Diet: For some individuals, a low-FODMAP diet (restricting fermentable carbohydrates) may help manage symptoms.
Stress Management:
- Practice Relaxation Techniques: Engage in stress-reducing activities like yoga, meditation, deep breathing exercises, or progressive muscle relaxation.
- Seek Counseling: Consider therapy or counseling to learn coping mechanisms for managing stress and anxiety.
Regular Exercise:
- Engage in Moderate Physical Activity: Aim for at least 30 minutes of moderate-intensity exercise most days of the week to promote gut motility and reduce stress.
Probiotics:
- Consider Probiotic Supplements: Some studies suggest that probiotics (beneficial bacteria) may help alleviate IBS symptoms, but more research is needed.
While the book Sleisenger and Fordtran’s Gastrointestinal and Liver Disease Review and Assessment does not have a dedicated section on IBS prevention, it discusses the role of diet, stress management, and probiotics in the management of IBS symptoms, which can indirectly contribute to prevention in individuals at risk.[9]
Homeopathic Treatment
Homeopathic Treatment of Irritable bowel syndrome (IBS)
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Irritable bowel syndrome (IBS):
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Medicines:
Nux Vomica:
- In general, Flatulent distension with spasmodic colic.
- Bruised soreness of abdominal walls.
- Furthermore, Colic with upward pressure, causing short breath also desire to stool.
- Constipated with frequent ineffectual urging.
- Besides this, Irregular peristaltic action.
- Dysentery, stools relieve pain for a time.
- Worse – morning, after eating, spices, stimulants, cold. On the other hand, Better – rest, damp, wet weather.
Aloe:
- Abdomen feels full, heavy, hot, bloated.
- Pulsating pain around navel. Additionally, Great accumulation of flatus pressing downwards, causing distress in lower bowels.
- Sensation of plug between symphysis pubis and coccyges, with urging to stool. Basically, Colic before and during stool. Burning copious flatus.
- Sense of insecurity in rectum, when passing flatus. In detail, Lumpy watery stool.
- Especially, Jelly-like stools, with soreness in rectum after stool.
- Burning in anus also rectum.
- Constipation with heavy pressure in lower part of abdomen. Diarrhoea from beer. Worse – heat. whereas Better – cold.
Asterias Rubens:
- Ineffectual desire.
- Stool like olives – diarrhoea, watery brown, gushing out in jet.
Podophyllum:
- Generally, in Long standing diarrhoea.
- Constipation, clay coloured, hard, dry, difficult.
- Constipation alternating with diarrhoea.
- Green watery fetid, profuse, also gushing.
- Prolapse of rectum before or with stool.
- Worse – specifically hot weather.
Antimonium Crudum:
- Excessive irritability also fretfulness. Loss of appetite. In detail, Constant belching.
- Bloated after eating. Diarrhoea alternating with constipation, especially in old people.
- Diarrhoea after acids, sour wine, overeating. Additionally, Slimy flatulent stools. Mucus. Piles. Continued oozing of mucus, hard lumps mixed with watery discharge.
- Catarrhal proctitis. Besides this, Stools composed entirely of mucus.
- Worse – heat, acids, wine, water. On the other hand, Better – rest, moist warmth.
Lycopodium:
- Basically, Abdomen is bloated, full.
- Pain shooting across lower abdomen from right to left.
- Furthermore, Diarrhoea, inactive intestinal canal. Ineffectual urging, stool hard, difficult, small, incomplete.
- Worse – especially right side from right to left, from above downward, 4-8.00 p.m., heat. On the other hand, Better – motion, warm food and drinks.
- On getting cold, from being uncovered.
Chelidonium Major:
- Fermentation and sluggish bowels. Distension.
- Constipation stools hard round balls like sheep’s dung.
- Bright yellow pasty clay coloured.
- Alteration of diarrhoea and constipation.
- Burning and itching of anus.
- Worse – motion, touch, change of weather, but Better by- after dinner, from pressure.
Gambodia–
- Garcinia Morella: Pain and distension of abdomen, from flatulence, after stool.
- Rumbling and rolling. Dysentery with retained scybala, with pain in sacral region.
- Diarrhoea with sudden and forcible ejection of bilious stools.
- Tenesmus after, with burning of anus.
- Ileo-sacral region sensitive to pressure.
- Profuse watery diarrhoea in hot weather, particularly in old people.
- Worse – towards evening, especially night.
Iodum:
- Anxiety and depression. Acute catarrh of all mucus membranes.
- Acute exacerbation of chronic inflammation.
- Cutting pain in abdomen. Constipation alternating with diarrhoea.
- Constipation with ineffectual urging.
- Diarrhoea whitish, frothy, fatty.
- Hemorrhage at every stool.
- Worse – quiet, warm room. whereas Better – open air, walking about.
Diet & Regimen
Diet & Regimen of Irritable bowel syndrome (IBS)
To ease chronic IBS-associated constipation
IBS-C: Compliant Foods i.e.
- Whole-grain bread and cereals, Oat bran
- Fruits (especially apples, pears, kiwifruit, figs, and kiwifruit)
- Vegetables (especially green leafy vegetables, sweet potato, and Brussels sprouts)
- Beans, peas, and lentils, Clear soups
- Dried fruit, Prune juice
- Non-fat milk
- Yogurt and Kefir
- Skinless chicken, Fish
- Seeds (especially chia seed and ground flaxseed)
IBS-C: Non-Compliant Foods i.e.
- White bread, pasta, also crackers
- Unripe bananas
- Fast or fried foods, Baked goods (e.g. cookies, muffins, cakes)
- White rice
- Full-fat cream and dairy (including ice cream)
- Alcohol (especially beer), Red meat[4]
- Potato chips, Chocolate, Creamy soups
If IBS symptoms involve diarrhea,
IBS-D: Compliant Foods i.e.
- White bread, pasta, and crackers, Whole grains
- White rice, Oatmeal
- Skinless chicken, Lean meat
- Lean fish ,Eggs
- Boiled or baked potato
- Beans, peas, and legumes
- Rice milk, almond milk, or coconut milk
- Low-fat lactose-free milk
- Low-fat probiotic yogurt
- Unsweetened clear fruit juice
IBS-D: Non-Compliant Foods i.e.
- Fast or fried foods, Foods high in sugar (e.g., baked goods)
- Fatty meats ,Processed meats
- Sardines and oil-packed canned fish
- Cruciferous vegetables ,Salad greens also raw vegetables
- Bean, peas, and legumes
- Citrus fruits, Dried fruits
- Caffeine, Alcohol
- Milk and dairy products
- Sweetened juices and fruit nectars [4]
Do’s and Don'ts
Do’s and Don’ts
IBS do’s and don’ts
Do’s
Dietary Changes:
- Increase soluble fiber intake gradually (found in oats, fruits, vegetables, legumes) to regulate bowel movements.
- Drink plenty of water throughout the day to help soften stools and prevent constipation.
- Keep a food diary to identify trigger foods and avoid them.
- Do consider a low-FODMAP diet if certain carbohydrates worsen symptoms.
- Eat regular meals and avoid skipping meals to maintain a consistent digestive pattern.
Lifestyle Modifications:
- Manage stress through relaxation techniques (yoga, meditation, deep breathing) or counseling.
- Do exercise regularly for at least 30 minutes most days of the week.
- Get enough sleep to help regulate bowel function and reduce stress.
- Do seek support from friends, family, or support groups.
Medical Management:
- Do consult a doctor for diagnosis and personalized treatment plan.
- Take medications prescribed by your doctor as directed.
- Keep track of your symptoms and discuss any changes with your doctor.
Don’ts:
Dietary Habits:
- Not eat large meals; opt for smaller, more frequent meals instead.
- Don’t consume excessive caffeine, alcohol, or carbonated drinks, as they can worsen symptoms.
- Not eat too quickly; chew your food thoroughly to aid digestion.
- Don’t overindulge in fatty or greasy foods, as they can trigger diarrhea.
- Don’t use artificial sweeteners, as they may worsen bloating and gas.
Lifestyle Factors:
- Don’t ignore stress or emotional triggers; address them actively.
- Don’t smoke, as it can aggravate IBS symptoms.
Please note: These are general recommendations, and individual needs may vary. It is crucial to consult with your doctor for personalized advice and treatment for your specific IBS condition.
Terminology
Terminology
Core Terminologies:
- Irritable Bowel Syndrome (IBS): A chronic functional gastrointestinal disorder characterized by abdominal pain, discomfort, bloating, and changes in bowel habits (diarrhea, constipation, or both).
- Functional Gastrointestinal Disorder (FGID): A group of disorders affecting the digestive system where symptoms occur without any identifiable structural or biochemical abnormalities.
- Visceral Hypersensitivity: Increased sensitivity to sensations in the gut, leading to heightened pain perception.
- Gut-Brain Axis: The bidirectional communication between the brain and the gut, influencing both gastrointestinal function and emotional well-being.
IBS Subtypes:
- IBS with Constipation (IBS-C): IBS predominantly characterized by constipation.
- IBS with Diarrhea (IBS-D): IBS predominantly characterized by diarrhea.
- IBS with Mixed Bowel Habits (IBS-M): IBS with alternating constipation and diarrhea.
Other Relevant Terms:
- Rome IV Criteria: The most recent set of diagnostic criteria for IBS, based on symptom patterns.
- FODMAPs: Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols – a group of carbohydrates that can trigger IBS symptoms in some individuals.
- Probiotics: Live bacteria and yeasts that are beneficial for gut health and may help alleviate IBS symptoms.
- Antispasmodics: Medications that help relax the muscles of the gastrointestinal tract to relieve abdominal cramps and pain.
- Low-FODMAP Diet: A diet that restricts FODMAPs to manage IBS symptoms.
- Cognitive Behavioral Therapy (CBT): A type of psychotherapy that helps manage IBS symptoms by addressing the emotional and psychological aspects of the condition.
Example Usage in an Article:
"Irritable Bowel Syndrome (IBS) is a common functional gastrointestinal disorder affecting millions of people worldwide. The exact cause of IBS remains unknown, but it is believed to involve a complex interplay of factors, including altered gut motility, visceral hypersensitivity, and dysregulation of the gut-brain axis. Recent research has highlighted the potential role of the gut microbiota in IBS pathophysiology. Management of IBS typically involves dietary modifications, such as a low-FODMAP diet, along with lifestyle changes, stress management techniques, and medications like antispasmodics. In some cases, cognitive behavioral therapy (CBT) may also be helpful in managing IBS symptoms."
I hope this helps! Let me know if you have any other questions.
References
References
- Harrison-s_Principles_of_Internal_Medicine-_19th_Edition-_2_Volume_Set
- https://www.mayoclinic.org/diseases-conditions/irritable-bowel-syndrome/diagnosis-treatment/drc-20360064
- Homoeopathic Body-System Prescribing – A Practical Workbook of Sector Remedies
- https://www.verywellhealth.com/ibs-nutrition-4013556
- https://www.news-medical.net/health/Irritable-Bowel-Syndrome-(IBS)-Differential-Diagnosis.aspx
- Ghoshal UC, Abraham P, Bhatt C, et al. Epidemiological and clinical profile of irritable bowel syndrome in India: report of the Indian Society of Gastroenterology Task Force. Indian J Gastroenterol. 2008 Mar-Apr;27(2):22-9. .
- Madisch A, Palsson OS, Andresen V, et al. Indian consensus statements on irritable bowel syndrome in adults: A guideline by the Indian Neurogastroenterology and Motility Association and jointly supported by the Indian Society of Gastroenterology. J Neurogastroenterol Motil. 2022 Aug 30;28(3):379-400.
- Aziz I, Palit S, Hossain S, et al. Epidemiological and clinical perspectives on irritable bowel syndrome in India, Bangladesh and Malaysia: A review. World J Gastroenterol. 2017 Oct 7;23(37):6788-6802.
- Sleisenger and Fordtran’s Gastrointestinal and Liver Disease Review and Assessment (11th Edition) by Anthony J. DiMarino Jr. and Michael Camilleri (2021). Saunders, an imprint of Elsevier.
Also Search As
Also Search As
There are several ways people can search for homeopathic articles on Irritable Bowel Syndrome (IBS):
Online Search Engines:
- Use specific keywords: Search using terms like "homeopathy IBS," "homeopathic treatment IBS," or "homeopathic remedies IBS."
- Include reputable sources: Add phrases like "homeopathic journal," "homeopathic research," or names of known homeopathic organizations to your search.
Homeopathic Journals and Publications:
- Browse through online or physical copies of homeopathic journals like "The American Journal of Homeopathic Medicine," "Homeopathy," or "The European Journal of Integrative Medicine."
- Look for articles with titles related to IBS or gastrointestinal disorders.
Homeopathic Websites and Databases:
- Visit websites of reputable homeopathic organizations like the National Center for Homeopathy (NCH) or the British Homeopathic Association (BHA).
- Search their databases or resource sections for articles or publications on IBS.
Libraries:
- Explore the medical or alternative medicine sections of libraries for books or journals on homeopathy and IBS.
Homeopathic Practitioners:
Consult with a qualified homeopathic practitioner. They can often provide access to relevant articles, research papers, or case studies.
Tips:
- Be specific in your search terms to get relevant results.
- Look for articles published in peer-reviewed journals for credibility.
- Cross-reference information from different sources for a comprehensive understanding.
- Consult with a homeopathic practitioner to discuss the suitability of homeopathic treatment for your specific IBS condition.
There are several ways to search for information on Irritable Bowel Syndrome (IBS):
Online Search Engines:
- Use search engines like Google, Bing, or DuckDuckGo with keywords like "IBS," "Irritable Bowel Syndrome," "IBS symptoms," "IBS treatment," or specific questions you have about the condition.
Medical Websites:
- Reputable websites like Mayo Clinic, Cleveland Clinic, National Institutes of Health (NIH), and WebMD provide reliable information on IBS, its symptoms, causes, diagnosis, and treatment options.
- Look for articles, blogs, and patient resources specifically dedicated to IBS on these websites.
Medical Databases:
- If you need scholarly articles or research papers on IBS, databases like PubMed, Google Scholar, or ScienceDirect are good resources.
- These databases contain a vast collection of scientific publications related to IBS.
Books and eBooks:
- Look for books specifically about IBS or gastrointestinal disorders at your local library or online bookstores.
- These books often provide a comprehensive overview of the condition and its management.
Social Media Groups and Forums:
- There are many online support groups and forums dedicated to IBS where you can connect with other people experiencing similar symptoms, share experiences, and learn from each other.
- However, be cautious about the information shared in such groups and always consult with your doctor for medical advice.
- There are many online support groups and forums dedicated to IBS where you can connect with other people experiencing similar symptoms, share experiences, and learn from each other.
Health Professionals:
- Consult with your doctor or a gastroenterologist (specialist in digestive disorders) for personalized information and treatment options tailored to your specific needs.
Tips for Effective Searching:
- Use specific keywords: Instead of just searching for "IBS," try using more specific terms like "IBS with constipation," "IBS diet," or "IBS triggers" to get more relevant results.
- Check the source: Always ensure that the information you find comes from reputable sources like medical institutions, government organizations, or well-known health websites.
- Consult with a professional: For personalized advice and treatment recommendations, always consult with your doctor or a qualified healthcare provider.
Frequently Asked Questions (FAQ)
What is Irritable bowel syndrome?
Irritable bowel syndrome (IBS) is a functional bowel disorder characterized by abdominal pain or discomfort and altered bowel habits in the absence of detectable structural abnormalities.
What are 3 causes of Irritable bowel syndrome?
- Muscle contractions in the intestine
- Abnormalities in the nerves in your digestive system
- Severe infection
- Early life stress
- Changes in gut microbes
What are the symptoms of Irritable bowel syndrome?
- Abdominal pain, cramping or bloating
- Changes in appearance of bowel movement
- Changes in how often you are having a bowel movement
- Increased gas or mucus in the stool.
- Weight loss
- Diarrhea at night
- Rectal bleeding
- Unexplained vomiting
- Difficulty swallowing
Homeopathic Medicines used by Homeopathic Doctors in treatment of Irritable bowel syndrome?
Homeopathic Medicines for Irritable bowel syndrome
- Nux Vomica
- Aloe
- Asterias Rubens
- Podophyllum
- Antimonium Crudum
- Lycopodium
- Chelidonium Major
- Gambodia
- Iodum
Are there any side effects of homeopathic remedies?
Homeopathic remedies are generally considered safe when taken as directed. In rare cases, a temporary worsening of symptoms (aggravation) may occur.
What lifestyle changes can help with IBS?
Stress management techniques, dietary adjustments (avoiding trigger foods, FODMAPs), regular exercise, and adequate sleep can complement homeopathic treatment.
Can I take homeopathic remedies alongside conventional medications?
It is generally safe to combine homeopathic remedies with conventional medications. Inform your doctor and homeopath about all medications you are taking.
How long does homeopathic treatment for IBS take?
Response to treatment varies. Some experience relief within weeks, while others may need months. Chronic cases may require longer-term treatment.
How does homeopathic treatment for IBS work?
Homeopathic practitioners consider your unique symptoms, medical history, and personality to select a remedy. The remedy stimulates your body’s healing response