Joint Pain
Definition
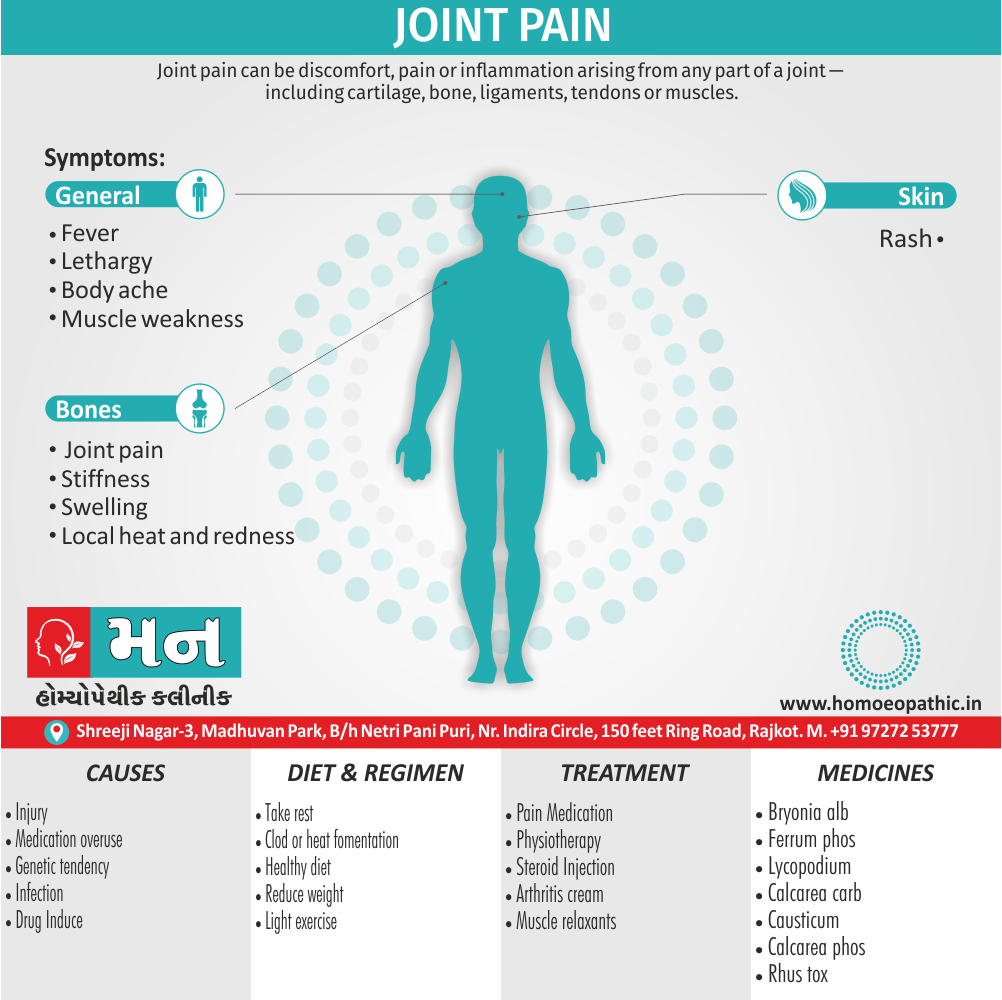
Joint pain can be discomfort, pain or inflammation arising from any part of a joint – including cartilage, bone, ligaments, tendons or muscles. Most commonly, however, joint pain refers to arthritis or arthralgia, which is inflammation or pain from within the joint itself.[1]
Certainly! Here’s an expanded breakdown of synonyms for joint pain, considering different aspects:
Formal synonyms:
- Arthralgia: This is the most precise medical term for joint pain, commonly used in clinical settings.
- Polyarthralgia: This refers to pain affecting multiple joints simultaneously.
Informal synonyms:
- General discomfort: Ache, discomfort, soreness, stiffness, tenderness – These terms convey a general unpleasant feeling in the joint.
- Intensity: Throbbing (pulsating pain), burning (intense heat sensation), stinging (sharp, quick pain), grinding (suggests friction).
- Movement-related: Stiffness (difficulty moving the joint), limitation of motion (reduced range of movement).
Additional options:
- Arthritic: While not a direct synonym for pain, "arthritic" implies joint pain associated with arthritis, a chronic inflammatory condition.
Choosing the best synonym depends on the context. For example, describing a general discomfort after exercise might use "soreness," while a doctor might use "arthralgia" in a diagnosis.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Joint pain
Joint pain can be mild, causing soreness only after certain activities, or it can be severe, making even limited movement, particularly bearing weight, extremely painful.
Disorders of the musculoskeletal system affect all ages and ethnic groups. In the UK, about 25% of new consultations in general practice are for musculoskeletal symptoms.
Musculoskeletal diseases may arise from processes affecting bones, joints, muscles, or connective tissues such as skin and tendon. The principal manifestations are pain and impairment of locomotor function.
Disorders more common in women also most increase in frequency with increasing age. Besides this, The two most common disorders are osteoarthritis and osteoporosis. Osteo arthritis is the most common type of arthritis also affects up to 80% of people over the age of 75.
All in all, Osteoporosis is the most common bone disease and affects 50% of women and 20% of men by their eighth decade. Diseases of the musculoskeletal system are the most common cause of physical disability in older people also account for one-third of physical disability at all ages. [1]
Evaluation of Patient
The Evaluation should proceed to ascertain if the complaint is;
[1] Firstly, Articular or non-articular in origin
[2] Secondly, Inflammatory or non-inflammatory in nature
[3] Thirdly, Acute or chronic in duration
[4] Lastly, Localized (mono-articular) or widespread (poly-articular) in distribution.
Epidemiology
Epidemiology
The prevalence of joint pain in India varies depending on the specific cause. However, some studies have found that osteoarthritis is the most common cause of joint pain in India, affecting up to 15% of the population. Rheumatoid arthritis is also a significant problem, affecting an estimated 1% of the population. [7]
Causes
Causes of Joint Pain
- Many conditions and factors can cause a person to experience joint pain.
- Moreover, If a person has pain in multiple joints, it is known as polyarthralgia.
- Usually, joint pain is the result of injury, infection, illness, or inflammation.
- Below are some of the common causes of joint pain:
Injury
- Injury is a common cause of joint pain.
- Injuries can result from the excessive use or effort of the joints or from an impact that causes a fracture, sprain, or strain.
- For example, a common knee injury is damage to the anterior cruciate ligament (in other words; ACL)Trusted Source. People who play certain sports, such as soccer, basketball, or football, are more at risk of injuring their ACL.
Viral infection
- Some infections may result in joint pain.
- For example, the hepatitis C virus (in other words; HCV) can cause complications that result in joint pain.
- It is common for people with HCV to have related rheumatic diseases, which can cause problems, including pain in the joints.
Disease
- Generally, Some diseases can cause joint pain.
- Lupus Trusted Source is a chronic autoimmune disease, also common symptoms include muscle and joint pain.
- In fact, joint pain is the first symptom for more than half of those who develop lupus.
- People develop lupus because their body’s immune system becomes hyperactive also attacks normal, healthy tissue.
Arthritis
- Arthritis and arthralgia are very similar but have key differences.
- Both describe joint pain, but arthralgia occurs without the distinct inflammation in the joint that characterizes arthritis.
- Nearly half Trusted Source of adults with arthritis report persistent joint pain.
- There are more than 100 different kinds Trusted Source of arthritis, including: e.g. Osteoarthritis (OA), Rheumatoid arthritis (RA), Gout, Septic arthritis.
- The cause of arthritis varies Trusted Source among the different types.
- OA results from cartilage loss in the joints. In detail, Calcification of the cartilage around the joints eventually makes the cartilage thinner before damaging it. Older adults are more likely to develop OA.
- RA is an autoimmune response to a trigger. Moreover, The body tries to fight off what it thinks is an invader but instead degrades the cartilage and bones in the joints.
- Gout occurs due to the crystallization of uric acid in the body. Uric acid gets into the joint spaces, causing inflammation.
- In most cases, septic arthritis results from a bacterial infection. Bacteria get into the synovial fluid in the joints, which eventually degrades the cartilage, leading to arthritis.[6]
Types
Types of Joint Pain
Inflammatory Arthritis: This type of joint pain is caused by inflammation in the joints. It includes conditions like rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis.
Non-Inflammatory Arthritis: This type of joint pain is not caused by inflammation. It includes conditions like osteoarthritis, trauma-related joint pain, and fibromyalgia.
Crystal-Induced Arthritis: This type of joint pain is caused by the deposition of crystals in the joints. It includes conditions like gout and pseudogout.
Infectious Arthritis: This type of joint pain is caused by an infection in the joints. It can be caused by bacteria, viruses, or fungi.
Other Causes: Joint pain can also be caused by various other conditions, such as lupus, Lyme disease, and certain types of cancer. [8]
Risk Factors
Risk factors of Joint Pain
Age: The risk of developing joint pain, particularly osteoarthritis, increases with age. This is due to the wear and tear of joints over time.
Gender: Women are more likely to develop certain types of joint pain, such as rheumatoid arthritis and osteoarthritis, compared to men.
Genetics: A family history of certain types of arthritis, like rheumatoid arthritis or osteoarthritis, can increase the risk of developing joint pain.
Obesity: Excess weight puts additional stress on the joints, especially the knees and hips, leading to increased wear and tear and a higher risk of osteoarthritis.
Joint Injury: Previous injuries to joints can predispose individuals to developing joint pain later in life.
Occupation: Certain occupations that involve repetitive movements or heavy lifting can increase the risk of developing joint pain.
Infections: Some infections can trigger or worsen joint pain, especially in individuals with pre-existing conditions like rheumatoid arthritis.
Other Medical Conditions: Certain medical conditions, such as diabetes, lupus, and psoriasis, can increase the risk of developing joint pain. [8]
Pathogenesis
Pathogenesis of Joint Pain
Inflammation: In inflammatory arthritis, like rheumatoid arthritis, the immune system mistakenly attacks the synovium, the lining of the joints. This leads to inflammation, pain, swelling, and stiffness. The inflammatory process can also damage the cartilage and bone within the joint over time.
Cartilage Degeneration: In osteoarthritis, the cartilage, the smooth tissue that cushions the ends of bones, gradually breaks down. This leads to bone rubbing against bone, causing pain, stiffness, and loss of joint function.
Crystal Deposition: In crystal-induced arthritis, like gout, crystals of uric acid or calcium pyrophosphate dihydrate (CPPD) deposit in the joints. These crystals trigger an inflammatory response, leading to pain, swelling, and warmth.
Infection: Infectious arthritis is caused by the invasion of bacteria, viruses, or fungi into the joint space. The microorganisms trigger an inflammatory response, leading to pain, swelling, warmth, and redness.
Trauma: Joint pain can also result from injuries like sprains, strains, or fractures. These injuries can damage the ligaments, tendons, muscles, or bones around the joint, leading to pain and limited mobility.
Nerve Damage: In some cases, joint pain can be caused by nerve damage. This can occur due to compression of nerves, inflammation of nerves, or other conditions affecting the nervous system. [8]
Pathophysiology
Pathophysiology
Joint pain, also known as arthralgia, arises from various pathophysiological mechanisms, often reflecting the complex interplay of inflammation, cartilage degeneration, crystal deposition, infection, and trauma. The initial evaluation aims to pinpoint the source of the pain and identify the underlying pathophysiologic process.
Several key pathophysiologic types of joint disease contribute to joint pain:
Synovitis:
nflammation of the synovial membrane, characterized by synovial hypertrophy, increased blood flow, and inflammatory cell infiltration. This process leads to the release of inflammatory mediators, such as prostaglandins and cytokines, which sensitize and activate nociceptors, resulting in pain, swelling, and stiffness.
Enthesopathy:
Inflammation at the site of tendon or ligament attachment to bone. This can involve the enthesis itself, adjacent bone, or surrounding soft tissues. Enthesopathy often causes localized pain and tenderness, particularly during movement or stress on the affected area.
Crystal Deposition:
Formation and deposition of crystals within the joint, such as monosodium urate crystals in gout or calcium pyrophosphate dihydrate crystals in pseudogout. These crystals trigger an intense inflammatory response, leading to acute pain, swelling, and redness.
Infection:
Invasion of the joint by microorganisms, causing septic arthritis. The infection triggers a robust inflammatory response, leading to severe pain, swelling, warmth, and limited range of motion.
Structural or Mechanical Derangements:
Abnormalities in joint structure or mechanics, such as osteoarthritis, ligament tears, or meniscus injuries. These conditions can cause pain due to cartilage degeneration, bone-on-bone contact, joint instability, or impingement of soft tissues.
These pathophysiologic processes are not mutually exclusive and can coexist, contributing to the complexity of joint pain. For example, crystal deposition can occur in osteoarthritis, synovitis can be present in enthesopathies, and cartilage destruction can result from chronic synovitis.
Understanding the underlying pathophysiology of joint pain is crucial for accurate diagnosis, appropriate treatment, and effective management of this common and often debilitating condition.[11]
Clinical Features
Clinical Features
Pain:
The hallmark feature of joint pain is pain, which can range from mild to severe and can be constant or intermittent. The pain may worsen with movement or activity and improve with rest.
Stiffness:
Joint stiffness is often associated with pain and is more pronounced in the morning or after periods of inactivity. It typically improves with movement and activity.
Swelling:
Joint swelling is a common feature of inflammatory arthritis, indicating inflammation within the joint. It can also be present in other types of joint pain, like osteoarthritis, due to fluid accumulation or bony enlargement.
Warmth and Redness:
Warmth and redness over the affected joint are characteristic of inflammatory arthritis and infectious arthritis, indicating active inflammation.
Limited Range of Motion:
Joint pain can restrict the normal range of motion of the affected joint, making it difficult to move the joint freely.
Deformity:
In chronic or severe cases of joint pain, deformity of the affected joint can occur. This can be due to damage to the joint structures, such as cartilage or bone, or due to muscle weakness or imbalance.
Constitutional Symptoms:
In some cases of joint pain, particularly inflammatory arthritis, individuals may experience constitutional symptoms like fatigue, fever, weight loss, and malaise.
Other Symptoms:
Depending on the underlying cause, individuals with joint pain may also experience other symptoms like skin rashes, nodules, eye inflammation, or gastrointestinal problems. [8]
Sign & Symptoms
Sign & Symptoms of Joint Pain
Other symptoms that commonly accompany joint pain i.e.:
- Joint tenderness
- Joint stiffness
- Joint swelling
- Limited joint movement
- Weakness in the joint, or the joint becoming unstable
- Fatigue [6]
Clinical Examination
Clinical Examination of Joint
The examination typically involves the following steps:
History: A detailed history of the patient’s symptoms is crucial to understand the nature and onset of joint pain. This includes asking about the location, duration, intensity, and character of the pain, as well as any aggravating or relieving factors.
Inspection: The affected joint is visually inspected for any signs of swelling, redness, deformity, or muscle wasting. The patient’s gait and posture are also observed.
Palpation: The joint is palpated to assess for tenderness, warmth, swelling, and crepitus (a grating or crackling sensation). The surrounding muscles and tendons are also palpated for tenderness or tightness.
Range of Motion: The active and passive range of motion of the joint is assessed to determine any limitations or pain with movement.
Special Tests: Specific tests are performed to assess the integrity of the ligaments, tendons, and other structures around the joint. These tests may include stress tests, stability tests, and provocative maneuvers.
Neurovascular Examination: The neurovascular status of the limb is assessed to ensure that there is no compromise of the blood supply or nerve function.
Diagnosis
Diagnosis of Joint Pain
The initial diagnosis of joint pain will likely involve an evaluation by a doctor. They will usually look at the person’s medical history and carry out a physical examination.
The doctor may ask questions, such as whether the pain appeared after an injury or whether there is a family history of joint disease.
As part of the physical exam, they will inspect the joints and check their range of motion.[6]
Differential Diagnosis
Differential Diagnosis
Inflammatory Causes:
- Rheumatoid Arthritis (RA)
- Systemic Lupus Erythematosus (SLE)
- Psoriatic Arthritis
- Ankylosing Spondylitis
- Reactive Arthritis
- Gout
- Pseudogout
- Infectious Arthritis (bacterial, viral, fungal)
Non-Inflammatory Causes:
- Osteoarthritis (OA)
- Trauma (fractures, sprains, strains)
- Fibromyalgia
- Polymyalgia Rheumatica
- Bursitis
- Tendinitis
- Myofascial Pain Syndrome
- Osteonecrosis
Other Causes:
- Lyme Disease
- Sarcoidosis
- Endocrine Disorders (hypothyroidism, hyperparathyroidism)
- Hematologic Disorders (leukemia, sickle cell disease)
- Neoplastic Disorders (bone tumors, metastatic cancer)
Approach to Differential Diagnosis:
Harrison’s Principles of Internal Medicine outlines a systematic approach to differentiate between these various causes of joint pain. This approach involves a careful history taking, physical examination, and laboratory and imaging studies.
History:
- Onset, duration, and pattern of pain (acute vs. chronic, inflammatory vs. mechanical)
- Number and distribution of affected joints (monoarticular vs. polyarticular, symmetrical vs. asymmetrical)
- Associated symptoms (fever, rash, stiffness, fatigue)
- Risk factors (age, gender, family history, previous injuries)
Physical Examination:
- Inspection (swelling, redness, deformity)
- Palpation (tenderness, warmth, crepitus)
- Range of motion (active and passive)
- Special tests (to assess specific joints and structures)
Laboratory and Imaging Studies:
- Complete blood count (CBC)
- Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP)
- Antinuclear antibodies (ANA)
- Rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) antibodies
- Uric acid
- Joint aspiration and synovial fluid analysis
- X-rays
- MRI
- Ultrasound
Complications
Complications of Joint Pain
Some of the common complications include:
Joint Damage and Deformity: Chronic joint pain, especially in inflammatory arthritis, can lead to progressive joint damage, erosion of cartilage, and bone deformities. This can result in significant functional impairment and disability.
Decreased Mobility and Function: Joint pain can restrict the range of motion and limit the ability to perform daily activities, leading to decreased mobility and impaired function.
Muscle Weakness and Atrophy: Due to pain and limited use, the muscles surrounding the affected joint can weaken and atrophy, further contributing to functional impairment.
Chronic Pain and Disability: Persistent joint pain can lead to chronic pain syndromes, affecting the individual’s quality of life, mental health, and overall well-being.
Systemic Complications: Some types of joint pain, like rheumatoid arthritis, can have systemic manifestations, affecting other organs and systems in the body. These complications can include cardiovascular disease, lung disease, eye inflammation, and nerve damage.
Osteoporosis: Chronic inflammation in certain types of joint pain can contribute to the development of osteoporosis, a condition characterized by weakened bones and increased risk of fractures.
Infections: Individuals with joint pain, especially those on immunosuppressive medications, may be at increased risk of developing infections in the affected joint or other parts of the body.
Psychological Impact: Chronic pain and disability associated with joint pain can lead to psychological distress, including depression, anxiety, and social isolation.
Economic Burden: Joint pain can impose a significant economic burden on individuals and society due to healthcare costs, lost productivity, and disability. [8]
Investigations
Investigation of Joint Pain
- X-Ray
- Ultrasonography
- CBC
- Blood Sugar
- ESR
- CRP
- Rh Factor [6]
Treatment
Treatment of Joint Pain
- Treatment for joint pain will vary depending on the underlying cause.
- Typically, a doctor may prescribe pain medication to relieve pain. For example, for arthritis, they may suggest nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, or disease-modifying antirheumatic drugs (DMARDs).
- If the joint pain is due to an infection, a doctor will prescribe antibiotics or antivirals to reduce and manage the symptoms.
- For people who don’t find joint pain relief from oral or topical medications, the doctor may try injections- Steroids, Platelet-rich plasma therapy, Prolotherapy.
- If the pain is due to an injury or arthritis, a doctor may refer people to a physical therapist for rehabilitation. In more severe cases, or if the pain persists, a doctor may recommend undergoing surgery.
Home remedies
- The results of using home remedies will likely vary depending on the underlying cause of joint pain. People may be able to manage joint pain at home by taking over-the-counter NSAIDs, such as ibuprofen, or using topical capsaicin.
- Using the RICE method may also be beneficial for alleviating pain. This method involves resting the injured area, applying ice packs, wrapping the injured area with an elastic bandage, and elevating the area to reduce swelling. Using crutches or a wheelchair may also help a person avoid putting unnecessary pressure on painful joints.
You can relieve short-term joint pain with a few simple techniques at home. One method is known by the acronym PRICE:
- Protect the joint with a brace or wrap.
- Rest the joint, avoiding any activities that cause you pain.
- Ice the joint for about 15 minutes, several times each day.
- Compress the joint using an elastic wrap.
- Elevate the joint above the level of your heart.[5]
Physical Therapy
You can work with a physical therapist to strengthen the muscles around the joint, stabilize the joint, and improve your range of motion.
The therapist will use techniques such as ultrasound, heat or cold therapy, electrical nerve stimulation, and manipulation.
If you are higher-weight person, losing weight can relieve some of the pressure on your painful joints.
Exercise is one effective way to lose weight (along with diet), but be careful to stick with low-impact exercises that won’t further irritate the joint.
Swimming and bicycling are among the best exercises because both allow you to exercise your joints without putting impact on them. Because water is buoyant, swimming also relieves some of the pressure on your joints.[5]
Prevention
Prevention
Maintain a Healthy Weight: Excess weight puts additional stress on joints, particularly the knees and hips, increasing the risk of osteoarthritis. Maintaining a healthy weight through a balanced diet and regular exercise can help reduce this risk.
Exercise Regularly: Regular exercise strengthens the muscles around joints, providing support and stability. It also helps maintain joint flexibility and range of motion. Low-impact exercises like swimming, cycling, and walking are particularly beneficial for joint health.
Avoid Joint Injuries: Take precautions to avoid joint injuries during physical activities or sports. This may involve using proper equipment, warming up before exercise, and avoiding overexertion.
Maintain Good Posture: Poor posture can put unnecessary stress on joints, leading to pain and stiffness. Maintaining good posture while sitting, standing, and lifting can help protect your joints.
Use Proper Body Mechanics: When lifting heavy objects, use proper body mechanics to avoid straining your joints. Bend your knees and lift with your legs, not your back.
Wear Supportive Shoes: Wearing comfortable, supportive shoes can help reduce stress on your feet, ankles, knees, and hips.
Manage Chronic Conditions: If you have a chronic condition like diabetes or lupus, managing it effectively can help reduce the risk of developing joint pain.
Eat a Healthy Diet: A diet rich in fruits, vegetables, and whole grains can provide essential nutrients for joint health, such as vitamin D and calcium.
Limit Alcohol and Tobacco Use: Excessive alcohol and tobacco use can negatively impact bone and joint health.
Get Regular Checkups: Regular checkups with your doctor can help identify and address any potential risk factors for joint pain early on. [10]
Homeopathic Treatment
Homeopathic Treatment of Joint Pain
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Joint Pain:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Ferrum Phos
- At the commencement this remedy should be given in repeated doses when there are febrile symptoms present, and later on in the disease it may be given as an intercurrent.
- The joints are painful on moving, motion sets up also increases the pain.
- Tenalgia crepitans (Inflammation of a tendon sheath that on motion results in a cracking sound).[2]
Kali Mur
- In acute arthritis, for the swelling or when the tongue is coated white.
- It may be alternated with Ferrum Phos.
- Movement aggravates the pains.
- It is useful especially after Ferrum Phos.
- Tenalgia crepitans.
Natrum Mur
- Chronic arthritis, joints crack.
- Synovitis, gout, sore hamstrings.
- Acute gout, Chronic gout, profuse, sour-smelling sweat.
- Rheumatic arthritis, especially of finger joints. Additionally, Urine dark red.
- Pains go suddenly to heart; sore hamstrings. Lastly, It seems to have also a marked effect in hot painful swellings of the knee joint. [2]
Rhus tox:
- This remedy is an irritating agent to the Skin especially of face, scalp, genitals; affects the fibrous tissue, ligaments and joints causing rheumatic symptoms.
- Moreover, Parts feel sore, bruised also Stiff.
- Pains as if the flesh was torn loose from the bones.
- Dislocating sensation, Muscles twitch, Crawling.
- Besides this, Numbness of parts paralyzed.
- Trembling, turning, swelling, and lividity.
- Mucous discharges are acrid.
- Inflammation and swelling of the long bones, scraping, gnawing, tearing loose in periosteum.
- Rheumatism in cold season. Additionally, Soreness of prominent projection of bones.[3]
- Worse – exposure to wet, cold, air, draught, chilled, when hot or sweaty, uncovering, parts, beginning of motion, rest, before storms, sprains, after exertion, after midnight, blows, jar, riding, ice cold drinks, side lain on.
- Better – Continued motion, heat, hot bath, if heated, warm wrapping, rubbing, nosebleed, holding affected part, abdomen, head etc., stretching limbs, change of position, warm dry, weather.
Lycopodium:
- Pain in bones and joints at night.
- Curvature and caries of bones.
- Furthermore, Inflammation of bones, mostly at ends (joints); softening also caries of bones.
- Numbness, also drawing and tearing in limbs, especially while at rest or at night.
- Heaviness of arms. In detail, Tearing in shoulder and elbow joints. In detail, One foot hot, the other cold.
- Worse – Pressure of clothes, warmth, awakening, wind, eating, even a little, or to satiety, especially from 4 to 8 p.m., wet weather, stormy weather, pressure, before, or from suppressed menses.
- Better – Warm drinks and food, cold applications, motion, eructation, urinating, specifically after midnight.
Calcarea carbonica:
- Sharp sticking, as if parts were either wrenched or sprained.
- Cold, damp feet; feel as if damp stockings were worn.
- Cold knees, cramps in calves.
- Sour foot-sweat.
- Weakness of extremities.
- Swelling of joints, especially knee. Additionally, weakness and trembling of limbs.
- Arthritic; nodosities; deformans.
- Worse – Cold, raw air, bathing, cooling off, change of weather to cold, exertion – physical, mental, ascending eye strain, dentition, puberty, pressure of clothes, milk, anxiety, awakening, full moon, standing, looking up, climaxis, turning head.
- Better – Dry climate and weather, lying, on painful side, on back, sneezing (headache), rubbing, scratching, wiping or soothing with hands, after breakfast, dark.[3]
Causticum:
- Manifests its action mainly in chronic rheumatic, arthritic also paralytic affections.
- Indicated by the tearing, drawing pains in the muscular and fibrous tissues, with deformities about the joints.
- Progressive loss of muscular strength, tendinous contractures, seems to choose preferable dark complexioned and rigid-fibered persons.
- Restlessness at night, with tearing pains in joints also bones, and sinking of strength, progresses until we have gradually appeared paralysis.
- Burning, rawness also soreness is characteristic.
- Worse – dry, cold winds, in clear fine weather, cold air, from motion of carriage. On the other hand, Better – in damp, wet weather; warmth, heat of bed.
Calcarea phos:
- A special affinity where bones form either sutures or symphysis.
- Pain, burning along sutures, Shifting pains.
- Arthritis, Rheumatism.
- Aggravation from Exposure to weather changes, Draughts, Cold melting snow, Dentition, Mental exertion, Loss of fluids, Puberty, Fruits, cider, Motion – Thinking of symptoms, lifting, ascending.
- Better – In summer, warm dry weather, lying down.
Bryonia:
- Stitching, tearing pain aggravation especially by motion, better by rest.
- Joints red, swollen hot, with stitches and tearing, every spot is painful on pressure.
- Pins also needles in soles, preventing walking. In detail, Knees stiff and painful, Hot swelling of feet.
- Moreover, Swelling of elbow, Knees totter and bend under him when walking.
- Worse – Least motion, raising up, stooping, coughing, exertion, deep breathing, Dry cold or heat, becoming hot in room, hot weather, drinking, while hot, eating Vegetables, Acids, vexation, touch, suppressions, taking cold, early a.m.
- Better – Pressure, lying on painful part, bandaging, Cool open air, cloudy, damp days, drawing knees up, heat to inflamed part, descending, sitting up, cold food, drink.[3]
Colchicum:
- Affects markedly muscles, fibrous tissue, serous membranes, joints esp. small.
- It causes extreme relaxation of muscles.
- Patient is weak, cold but sensitive and restless.
- Pains are, tearing, digging, drawing.
- Many joints are affected at the same time.
- Small, rapidly shifting areas of severe pain, but little swelling, Tingling, crawling.
- Cardio-arthritic affections, Dropsy, Hydropericardium, hydrothorax; ascites, hydrometra, Tendency to collapse.
- Worse – motion, touch, night, stubbing toes, vibrations, cold, damp weather, in damp room, changing weather, autumn, slight exertion, stretching, checked sweat, sunset to sunrise, loss of sleep, smell of food.
- Better – warmth, rest, doubling up, sitting, after stools, stooping.
Ferrum phos:
- Rheumatism attacking one joint after another aggravation from slightest motion.
- Sore bruised pain in shoulders extending to chest and wrist.
- Wrists ache with loss of power to grasp.
- Palms hot; in children, Jerking in limbs, Omodynia.
- Sprains of the elbows, Hands swollen and painful.
- Worse – night, 4-6 a.m., motion, noise, jar, cold air, touch, checked sweat, cold drinks and sour food, meat, herring, coffee, cake.
- Better – cold application, bleeding, lying down.
Iodum:
- Arthritic deformans with swollen joints; after acute attack of rheumatism.
- Secretions are hot, acrid or watery, persistent or salty.
- Acute catarrhal of the mucus membranes.
- Vasoconstriction, causing Oedema, ecchymoses, hemorrhages, Vascular degeneration.
- Atrophy or induration of testes, ovaries, uterus.
- Stiff and enlarged joints, Synovitis, Stiff and enlarged joints.
- Cold hands and feet, Acrid sweat on back of feet. Oedema of the feet.
- Back of hands; brown, as if swollen painful when turning hand, not when closing fingers.
- Worse – Heat of room, air, wraps, exertion, ascending, talking, fasting, night, rest, touch, pressure.
- Better – Cold air, bathing, walking about in open air, eating, sitting up. [3]
Diet & Regimen
Diet and Regiment of Joint Pain
Omega-3 Fatty Acids / Fish Oils
- Cold-water fish are a terrific source of Omega-3s fatty acids, which are essential nutrients for human health.
- These important nutrients are also sometimes referred to as polyunsaturated fatty acids.
- Not only are they proven to reduce inflammatory proteins in the body, but they also improve brain function and lower risk of heart disease, diabetes and other illnesses.
- Omega-3 can be found in cold-water fish such as tuna, salmon, trout, halibut and sardines. Taking a daily fish oil supplement is another way to absorb Omega-3s. [1]
Nuts and Seeds
- There’s good news for the vegans and vegetarians among us. Omega-3 can also be found in a variety of nuts and seeds.
- A small daily portion of walnuts, almonds, flax seeds, chia seeds or pine nuts can help reduce inflammation in the joints and connective tissue.
Brassica Vegetables
- Leafy greens like mustard greens, arugula, kale and purple cabbage are in the brassica family. Several other popular vegetables make the list, including broccoli, cauliflower and Brussel sprouts.
Colorful Fruits
- Fruits sometimes get a bad rap because of their high sugar content, but many are excellent antioxidants. Just like with vegetables, certain fruits are more effective than others in reducing inflammation in the body.
Olive Oil
- Toss out your vegetable oil, sunflower oil and peanut oil – all of which can increase inflammation.
Lentils and Beans
- Beans and lentils are known for their health benefits. They’re an excellent source of protein, fiber and essential minerals. They also have antioxidant and anti-inflammatory properties.
- Black beans, lentils, chickpeas, pinto beans and soybeans are all great sources of anthocyanins – that magical flavonoid that reduces inflammation.
Garlic and Root Vegetables
- Garlic, onions, ginger and turmeric have anti-inflammatory properties.
Whole Grains
- Research suggests that proteins found in refined grains (such as white bread, white rice and regular pasta) may trigger an inflammatory response in the body. However, high-fiber whole grains help produce fatty acids that are thought to counteract inflammation. Therefore, stick with the whole grains.
Dark Chocolate
- Chocolate has anti-inflammatory properties.
- Cocoa, the main ingredient in chocolate, contains antioxidants that can counteract genetic predisposition to insulin resistance and inflammation.
- The higher the percentage of cocoa in the chocolate, the higher its anti-inflammatory effect.[4]
Do’s and Don'ts
Do’s & Don’ts
Joint pain Do’s & Don’ts
Do’s:
Do stay active: Engaging in low-impact exercises like swimming, cycling, or walking can help strengthen the muscles around your joints, improve flexibility, and reduce pain.
Do maintain a healthy weight: Excess weight puts extra pressure on your joints, especially the knees and hips. Losing even a small amount of weight can significantly reduce joint pain.
Do apply heat or cold: Heat therapy, such as warm baths or heating pads, can help relax muscles and ease joint stiffness. Cold therapy, such as ice packs, can help reduce inflammation and numb pain.
Do use assistive devices: If you have difficulty moving around, consider using assistive devices like canes, walkers, or crutches to reduce stress on your joints.
Do practice good posture: Maintaining proper posture while sitting, standing, and lifting can help reduce stress on your joints and prevent pain.
Do eat a healthy diet: A balanced diet rich in fruits, vegetables, and whole grains can provide essential nutrients for joint health, such as vitamin D and omega-3 fatty acids.
Do get enough sleep: Adequate sleep is essential for overall health and can help reduce inflammation and pain.
Do manage stress: Stress can worsen pain perception. Practice relaxation techniques like yoga, meditation, or deep breathing to manage stress and alleviate pain.
Don’ts:
Don’t ignore persistent pain: If joint pain persists or worsens, seek professional medical advice for diagnosis and treatment.
Don’t overdo it: Avoid activities that exacerbate your joint pain. Listen to your body and rest when needed.
Don’t smoke: Smoking can worsen inflammation and increase the risk of joint damage.
Don’t rely on self-treatment: While some home remedies may provide temporary relief, it’s important to consult a doctor for proper diagnosis and treatment.
Don’t neglect your mental health: Chronic pain can take a toll on your mental well-being. Seek support from friends, family, or a therapist if you’re feeling overwhelmed.
Terminology
Terminology
General Terms:
- Arthralgia: Pain originating from within a joint.
- Arthritis: Inflammation of one or more joints.
- Myalgia: Muscle pain.
- Arthropathy: Any disease or condition affecting a joint.
Types of Arthritis:
- Osteoarthritis (OA): The most common type of arthritis, caused by wear and tear on the joints over time.
- Rheumatoid arthritis (RA): A chronic inflammatory autoimmune disease that affects the lining of the joints.
- Psoriatic arthritis: A form of arthritis associated with psoriasis, a skin condition.
- Gout: A type of arthritis caused by the accumulation of uric acid crystals in the joints.
- Juvenile idiopathic arthritis (JIA): A type of arthritis that affects children under 16.
Symptoms:
- Stiffness: Difficulty moving a joint or feeling of tightness.
- Swelling: Enlargement of a joint due to inflammation or fluid buildup.
- Warmth: Increased temperature around the affected joint.
- Redness: Discoloration of the skin over the joint.
- Crepitus: A grating or crackling sound or sensation produced by friction between bone and cartilage or the fractured parts of a bone.
- Effusion: The escape of fluid into a joint cavity.
Diagnosis and Treatment:
- Synovial fluid analysis: Examination of the fluid within a joint to diagnose the cause of arthritis.
- Imaging studies: X-rays, MRI, or ultrasound to visualize joint damage or inflammation.
- Anti-inflammatory drugs (NSAIDs): Medications to reduce pain and inflammation.
- Disease-modifying antirheumatic drugs (DMARDs): Medications that slow or stop the progression of rheumatoid arthritis.
- Corticosteroids: Powerful anti-inflammatory drugs used to treat severe joint pain and inflammation.
- Physical therapy: Exercises and other techniques to improve joint function and reduce pain.
- Occupational therapy: Techniques to help people with arthritis perform daily activities.
- Surgery: Joint replacement or other surgical procedures to repair or replace damaged joints.
Remedies:
- Rhus Tox: A common remedy for joint pain that is worse with initial movement but improves with continued motion. It’s often used for pain that feels stiff, achy, and worse in cold, damp weather.
- Bryonia: Used for joint pain that is worse with any movement and better with rest. The affected joints may feel hot and swollen.
- Arnica: Typically used for joint pain resulting from injuries or overexertion. It’s known for its anti-inflammatory and pain-relieving properties.
- Ledum: Often used for joint pain that starts in the lower extremities and moves upwards. It’s also indicated for pain that feels cold to the touch but is relieved by cold applications.
- Colchicum: A remedy commonly used for gouty arthritis, characterized by intense pain, swelling, and redness in the affected joint.
Other Terminologies:
- Aggravation: A temporary worsening of symptoms after taking a homeopathic remedy, often considered a positive sign of healing.
- Amelioration: An improvement of symptoms after taking a homeopathic remedy.
- Potency: The strength or dilution of a homeopathic remedy.
- Repertorization: The process of selecting the most appropriate homeopathic remedy based on the patient’s symptoms.
- Constitutional Remedy: A remedy that matches the patient’s overall physical and mental characteristics, used for long-term treatment.
References
Reference of Article about Joint pain
- [1] Harrison-s_Principles_of_Internal_Medicine-_19th_Edition-_2_Volume_Set
- [2] Twelve Tissue Remedies Comprising of Theory, Therapeutics, Applications, Materia Medica and Complete Repertory of Tissue Remedies [Therap Part] By Boericke & Dewey.
- [3] Homoeopathic Body-System Prescribing – A Practical Workbook of Sector Remedies
- [4] https://www.caryortho.com/10-foods-that-help-reduce-joint-pain/
- [5] https://www.webmd.com/pain-management/guide/joint-pain
- [6] https://www.medicalnewstoday.com/articles/joint-pain#diagnosis
- [7] Osteoarthritis in India: An Epidemiologic Aspect (Azad et al., 2017)
- [8] Kelley’s Textbook of Rheumatology (11th Edition) Gary S. Firestein, Ralph C. Budd, Sherine E. Gabriel, Iain B. McInnes, and James R. O’Dell and was published in 2021 by Elsevier.
- [9] DeLee & Drez’s Orthopaedic Sports Medicine (5th Edition) by Mark D. Miller, Stephen R. Thompson, Published in 2023 by Elsevier
- [10] Rheumatology (6th Edition) by Marc C. Hochberg, Alan J. Silman, Josef S. Smolen, Michael E. Weinblatt, Michael H. Weisman in 2015
Kelley’s Textbook of Rheumatology, 11th Edition By: S. Louis Bridges Jr., MD, PhD, FRCP (Edin) (2023) Publisher: Elsevier.
Also Search As
Also Search As
There are several ways people can search for homeopathic articles on joint pain:
Online Search Engines:
Use search terms like "homeopathy joint pain," "homeopathic remedies for arthritis," or "homeopathic treatment for joint pain" on search engines like Google, DuckDuckGo, or Ecosia. This will yield a variety of articles, blog posts, and research studies on the topic.
Homeopathic Websites and Journals: Many reputable homeopathic organizations and journals have websites and online resources that feature articles on joint pain. Some examples include:
- The National Center for Homeopathy (NCH): Offers articles and resources on homeopathic treatment for various conditions, including joint pain.
- The North American Society of Homeopaths (NASH):Provides information on homeopathic education, research, and practice, including articles on joint pain.
- The Homeopathic Educational Services (HES): Offers online courses and resources on homeopathy, including articles on various health conditions.
- Homeopathy journal: A peer-reviewed journal that publishes original research and clinical studies on homeopathy.
Online Libraries and Databases:
Several online libraries and databases offer access to homeopathic journals and articles. Some examples include:
- Pubmed: A free search engine accessing primarily the MEDLINE database of references and abstracts on life sciences and biomedical topics.
- ScienceDirect: A leading full-text scientific database offering journal articles and book chapters from a wide range of scientific fields.
Homeopathic Clinics and Practitioners: Many homeopathic clinics and practitioners have websites or blogs where they share information and articles on homeopathic treatment for various conditions, including joint pain. You can also contact a homeopathic practitioner directly for personalized advice and resources.
Social Media:
Social media platforms like Facebook, Twitter, and Instagram can be a good source of information and articles on homeopathy. Look for groups, pages, or hashtags related to homeopathy and joint pain.
Specific Journals:
Look for articles in journals that specialize in rheumatology, orthopedics, or related fields. Some examples include:
- Osteoarthritis and Cartilage
- Journal of Orthopaedic Research
- Arthritis & Rheumatology
- Arthritis Care & Research
- The Journal of Rheumatology
ResearchGate and Academia.edu:
These platforms are social networking sites for scientists and researchers.
They allow you to follow researchers, access their publications, and ask questions directly.
ClinicalTrials.gov:
This is a database of privately and publicly funded clinical studies conducted around the world.
It can be a valuable resource for finding the latest research on osteoarthritis treatments.
Frequently Asked Questions (FAQ)
What is Joint Pain?
Joint pain can be discomfort, pain or inflammation arising from any part of a joint — including cartilage, bone, ligaments, tendons or muscles.
What causes Joint Pain?
- Injury
- Viral infection
- Disease
- Arthritis
How is joint pain diagnosed?
Diagnosis involves a thorough medical history, physical examination, and potentially lab tests or imaging studies like X-rays or MRI.
Is homeopathy safe for joint pain?
Homeopathic remedies are generally considered safe when prescribed by a qualified practitioner.
However, it’s crucial to consult with a professional before starting any new treatment, especially if you are pregnant, breastfeeding, or have any underlying medical conditions.
What are the symptoms of Joint Pain?
- Joint tenderness
- Joint stiffness
- Joint swelling
- Limited joint movement
- Weakness in the joint, or the joint becoming unstable
- Fatigue
Can homeopathy help with joint pain?
Yes, homeopathy offers a holistic approach to managing joint pain.
It aims to address the underlying cause of the pain, not just the symptoms, by stimulating the body’s natural healing processes.
What are the treatment options for joint pain?
Treatment depends on the cause and severity of pain. It may include medications (pain relievers, anti-inflammatories), physical therapy, lifestyle changes (weight management, exercise), or in severe cases, surgery.
What are the most common homeopathic remedies for joint pain?
Some frequently used remedies for joint pain include Rhus Tox (for pain worse with initial movement), Bryonia (for pain worse with any movement), Arnica (for pain from injuries), Ledum (for pain starting in lower extremities), and Colchicum (for gout).
How long does it take to see results from homeopathic treatment for joint pain?
The response time to homeopathic treatment varies depending on the individual, the cause of pain, and the chosen remedy. Some people may experience relief within days or weeks, while others may require longer-term treatment.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Joint Pain?
Homoeopathic Medicines for Joint Pain
- Ferrum Phos
- Kali Mur
- Natrum Mur
- Rhus tox
- Lycopodium
- Calcarea carb
