Lichen planus
Definition
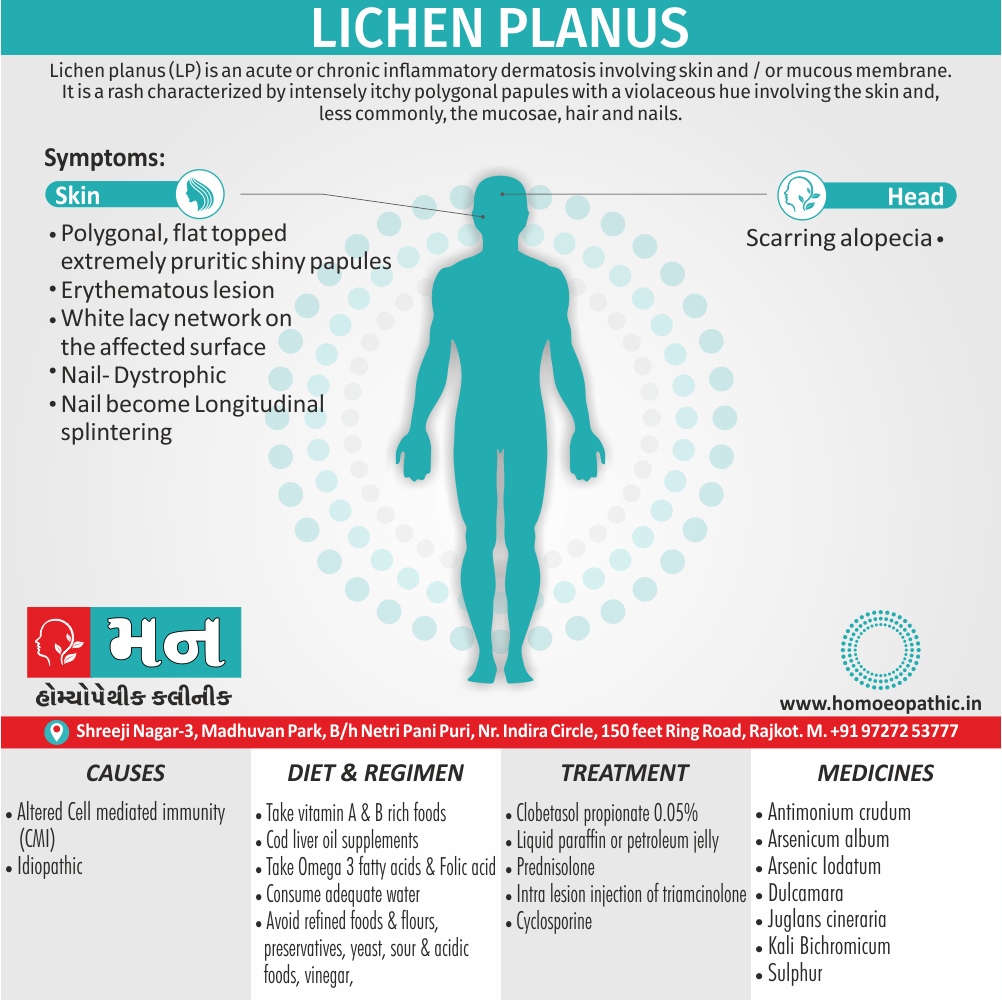
Lichen planus (LP) is an acute or chronic inflammatory dermatosis involving skin and / or mucous membrane. Additionally, It is a rash characterized by intensely itchy polygonal papules with a violaceous hue involving the skin and, less commonly, the mucosae, hair also nails.[1]
It doesn’t have true synonyms in the sense of another word that means exactly the same thing. However, there are a few terms related to lichen planus:
- Lichenoid eruptions: This is a general term for skin rashes that resemble lichen planus. They can be caused by medications, infections, or other underlying conditions.
- Variants of lichen planus: There are several different types of lichen planus, each with its own characteristics. Some examples include:
- Actinic lichen planus: This variant affects sun-exposed areas of the skin.
- Lichen planus pigmentosus: This variant causes dark patches on the skin.
- Erosive lichen planus: This variant causes sores to develop on the mucous membranes, such as the inside of the mouth or genitals.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Lichen planus
In general, It is a Autoimmune disorder. It is a recurrent, pruritic, inflammatory eruption characterized by small, discrete, polygonal, flat-topped, violaceous papules that may coalesce into rough scaly plaques, often accompanied by oral also genital lesions.
Moreover, Diagnosis is usually clinical and supported by skin biopsy. Besides this, Treatment generally requires topical or intralesional corticosteroids. Lastly, Severe cases may require phototherapy or systemic corticosteroids, retinoids, or immunosuppressants.[6]
Epidemiology
Epidemiology
It does not appear to be uncommon in the Indian subcontinent. Most of the large studies have been reported from India, the largest one by the authors in 2009 involving 100 children below 18 years of age seen over 6.5 years. Even in those studies where the actual number of lichen planus patients is not mentioned, the emphasis given in the discussion and the number of illustrations strongly suggest that It is seen not infrequently in the Indian subcontinent.
In a study carried out in Kashmir in the 1970s involving 333 patients of various skin conditions,It was seen in 18 patients. In the first half of the last century, a few cases of lichen from South India were described. the past few years, there has been an explosion of publications from the Indian subcontinent describing clinical and epidemiological characteristics of patients of lichen.[9]
Causes
Causes
- It is idiopathic in most cases.
- But it is evident that cell mediated immunity (in other words, CMI) plays a major role. Majority of the infiltrate contains CD 8+ and CD 45 RO+ memory cells.
- Drugs such as beta blockers, antimalarial, thiazides, gold also mercury salts and infection with hepatitis C virus result in altered cell mediated immunity. In detail, All these have been implicated as triggering factors for LP.[2]
Types
Types
- Hypertrophic lichen planus: – Presents as hyperkeratotic verrucous plaques especially on the lower parts of legs.
- Annular lesions: – It occur commonly on the glans penis.
- Linear violaceus papules of lichen planus: – It occur on the limbs also trunk .
- Follicular lesions: – It occur on the scalp.
- Graham Little syndrome: – It is the occurrence of follicular lesions also scarring alopecia of scalp with classical LP.
- Lichen planus actinicus: – the lesions are on the sites exposed to sunlight.
- Ulcerative lesions: – These are common on the soles also are resistant to therapy.[2]
Risk Factors
Risk Factors
Age: It Is most commonly affects middle-aged adults.
Sex: The oral form of lichen planus is more common in women.
Genetics: Having a family history of lichen planus increases your risk.
Underlying medical conditions: Certain conditions like hepatitis C, autoimmune diseases, and allergies may be associated with an increased risk of lichen planus.
Medications: Some medications, such as certain antibiotics, diuretics, and anti-inflammatory drugs, may trigger lichen planus.
Environmental factors: Exposure to certain chemicals or metals, such as those found in dental fillings, may be a risk factor.[10]
Pathogenesis
Pathogenesis
It is a chronic inflammatory mucocutaneous disease with a complex and incompletely understood pathogenesis. The current understanding suggests it is a T-cell-mediated autoimmune disease against basal keratinocytes, possibly triggered by an unknown antigen.
The proposed mechanisms include:
Antigen-specific immune response: An unknown antigen (possibly derived from stressed basal keratinocytes) is presented to CD4+ T cells by antigen-presenting cells, leading to their activation. These T cells release proinflammatory cytokines like interferon-gamma (IFN-γ) and tumor necrosis factor-alpha (TNF-α), which recruit and activate cytotoxic CD8+ T cells. These cytotoxic T cells then attack and destroy basal keratinocytes, resulting in the characteristic histological features of LP.
Non-specific immune response: In addition to the antigen-specific response, a non-specific inflammatory response also contributes to the pathogenesis of LP. This involves the activation of innate immune cells like natural killer (NK) cells and macrophages, which release additional proinflammatory cytokines and amplify the immune response.
Genetic factors: Genetic predisposition plays a role in the development of LP, as suggested by the association of certain human leukocyte antigen (HLA) alleles with the disease.
Environmental factors: Various environmental factors, including viral infections, certain medications, and contact allergens, have been implicated as potential triggers for LP, although their exact role remains unclear.[11]
Pathophysiology
Pathophysiology
It is a chronic inflammatory disorder characterized by a T-cell mediated autoimmune response against basal keratinocytes of the skin and mucous membranes. The exact trigger for this immune reaction remains unclear, but several factors are implicated:
Genetic Predisposition: Certain genetic variations increase susceptibility to LP, particularly within the human leukocyte antigen (HLA) system. These variations might influence antigen presentation and immune cell activation.
Environmental Triggers: Various environmental factors can potentially trigger LP in genetically predisposed individuals. These include:
- Viral infections (e.g., hepatitis C virus)
- Medications (e.g., certain antihypertensives, antimalarials, and hypoglycemic agents)
- Contact allergens (e.g., dental amalgam)
- Trauma
- Stress
Immunological Dysregulation: Once triggered, the immune system mounts a response against basal keratinocytes, leading to their destruction. This involves the activation of CD4+ and CD8+ T cells, release of pro-inflammatory cytokines (e.g., interferon-gamma, tumor necrosis factor-alpha), and recruitment of other immune cells (e.g., macrophages). The resulting inflammation causes the characteristic clinical and histological features of LP.[10]
Clinical Features
Clinical Features
It is a chronic inflammatory disease that affects the skin, mucous membranes (oral, genital, and other mucosal sites), hair, and nails. The clinical presentation varies depending on the affected site.
Skin
- Papules: The most common manifestation is small, flat-topped, polygonal, violaceous papules. These papules can coalesce to form plaques.
- Pruritus: Intense itching is a characteristic feature.
- Wickham’s striae: Fine, white, lacy lines on the surface of papules.
- Koebner phenomenon: Development of new lesions at sites of trauma.
- Distribution: Commonly affects the flexor surfaces of the wrists, forearms, ankles, and legs. It can also involve the trunk, genitalia, and nails.
Oral Mucosa
- Reticular lesions: Most common form, characterized by white, lacy lines or patches.
- Erosive lesions: Painful ulcers or erosions with erythematous borders.
- Atrophic lesions: Areas of thinning and redness of the mucosa.
- Bullous lesions: Rare, fluid-filled blisters.
Other Mucosal Sites
- Genital: White patches or erosions on the vulva, vagina, glans penis, or foreskin.
- Esophageal: White patches or strictures.
- Ocular: Conjunctivitis or scarring.
Hair
- Lichen planopilaris: Inflammation of the hair follicles leading to scarring alopecia.
Nails
- Thinning: Longitudinal ridging, splitting, or complete loss of the nail plate..[10]
Sign & Symptoms
Sign & Symptoms
- Basically, The onset is usually insidious with the classical violaceous, polygonal, flat topped extremely pruritic shiny papules distributed symmetrically over the flexor aspect of forearms, wrists, lower parts of legs also genitalia.
- Furthermore, The initial lesions may be erythematous.
- Some lesions show a white lacy network (Wickham’s striae) on the surface.
- Koebner phenomenon (spread of lesions along the lines of trauma) is seen.
- In two thirds of cases, the buccal mucosa is involved.
- Sometimes scalp involvement leads to scarring alopecia.
- Nails become dystrophic with longitudinal splintering.[2]
Clinical Examination
Clinical Examination
It is a chronic inflammatory condition affecting the skin and mucous membranes. The clinical presentation can vary depending on the site of involvement and the type of lesions.
Cutaneous Lichen Planus
Inspection:
- Primary lesions: Pruritic, polygonal, planar, purple papules
- Wickham striae: Fine white lines or lacy pattern on the surface of papules (best seen with a hand lens or dermoscope)
- Koebner phenomenon: Development of new lesions at sites of trauma or scratching
- Distribution: Most common on flexor surfaces of wrists, forearms, ankles, lower legs, genitalia, and oral mucosa
Palpation:
- Papules are firm and flat-topped
Oral Lichen Planus
Inspection:
- White reticular or plaque-like lesions on buccal mucosa, gingiva, tongue, palate, or lips
- Erosive or ulcerative lesions (less common)
Palpation:
- Lesions may be tender or asymptomatic
Nail Lichen Planus
Inspection:
- Thinning, ridging, splitting, or loss of nails
- Pterygium formation: Scar tissue extending from the proximal nail fold onto the nail plate
Scalp Lichen Planus (Lichen Planopilaris)
Inspection:
- Redness, scaling, and follicular hyperkeratosis
- Hair loss (scarring alopecia)[12]
Diagnosis
Diagnosis
A diagnosis based on your symptoms, your medical history, a physical examination and, if necessary, the results of lab tests. These tests may include i.e.:
- Biopsy: – Your doctor removes a small piece of affected tissue for examination under a microscope. Additionally, The tissue is analyzed to determine whether it has the cell patterns characteristic of lichen planus.
- Hepatitis C test: – You may have your blood drawn to test for hepatitis C, which is a possible trigger for lichen planus.
- Allergy tests: – Your doctor may refer you to an allergy specialist (in other words, allergist) or dermatologist to find out if you’re allergic to something that can trigger lichen planus.[3]
Differential Diagnosis
Differential Diagnosis
- Lichen Nitidus
- Lichen Simplex Chronicus
- Pediatric Syphilis
- Pityriasis Rosea
- Plaque Psoriasis
- Tinea Corporis [9]
Complications
Complications
Oral Lichen Planus (OLP):
- Increased risk of oral cancer, especially in erosive or atrophic forms.
- Painful oral lesions leading to difficulty eating, speaking, and swallowing.
- Secondary infections due to open sores.
Cutaneous Lichen Planus:
- Hyperpigmentation (darkening of the skin) after lesions heal, especially in darker skin tones.
- Scarring, particularly in hypertrophic or ulcerative forms.
- Nail changes, including thinning, ridging, splitting, and even permanent nail loss.
- Hair loss (alopecia) in rare cases involving the scalp.
Genital Lichen Planus:
- Painful sexual intercourse (dyspareunia).
- Phimosis (tightening of the foreskin) in men.
- Vaginal stenosis (narrowing of the vagina) in women.
Other Complications:
- Esophageal involvement leading to difficulty swallowing.
- Ocular involvement causing dry eyes, irritation, and blurred vision.
- Psychological distress due to chronic itching, pain, and cosmetic concerns.[12]
Investigations
Investigations
Lichen is primarily a clinical diagnosis, but certain investigations can be helpful to confirm the diagnosis, rule out other conditions, and assess the extent of involvement.
Skin biopsy: A skin biopsy is the gold standard for diagnosing lichen planus. It involves taking a small sample of affected skin for microscopic examination. The biopsy typically shows characteristic features of lichen planus, such as band-like lymphocytic infiltration at the dermoepidermal junction, basal cell degeneration, and hyperkeratosis.
Direct immunofluorescence (DIF): DIF can be performed on a skin biopsy to detect the presence of specific antibodies or immune complexes. In lichen planus, DIF may show deposition of fibrinogen along the basement membrane zone.
Blood tests: Blood tests may be done to rule out other conditions that can mimic lichen planus, such as autoimmune diseases or infections.
Patch testing: Patch testing can be used to identify potential allergens that may trigger or worsen lichen planus in some individuals.
Other tests: Depending on the clinical presentation, other tests like oral biopsy (for oral lichen planus), scalp biopsy (for lichen planopilaris), or nail biopsy (for nail lichen planus) may be necessary.[13]
Treatment
Treatment
- Classic LP can be treated with potent topical steroids such as Clobetasol propionate 0.05% twice daily for 2-3 weeks.
- Either Liquid paraffin or petroleum jelly should be applied 4-5 times daily.
- In acute generalized LP, oral corticosteroids such as Prednisolone 30-40 mg/day tapered over 1-3 months halt the rapid progression.
- Intra lesion injection of 0.1 ml of triamcinolone (10 mg/ml) is effective in hypertrophic LP.
- Cyclosporine in a dose of 3-5 mg/ kg orally for chronic LP induces long lasting remission.[2]
Prevention
Prevention of Lichen Planus
There is no known way to prevent lichen planus as the exact cause is unknown. However, identifying and avoiding potential triggers may help reduce the risk of developing the condition or experiencing flare-ups. These triggers can include certain medications, contact with allergens, and underlying infections.
It’s important to maintain good oral hygiene and avoid any potential irritants if you have oral lichen planus. If you suspect a medication or other trigger is causing a flare-up, it’s crucial to consult with your doctor to discuss alternative options.[10]
Homeopathic Treatment
Homeopathic Treatment of Lichen planus
It the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Lichen planus:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Medicine:
Antimonium crudum:
- Scaly, pustular eruption with burning and itching, worse especially at night.
- It is pre-eminently a scrofulous medicine, corresponding to gross constitutions with tendency to rough scaling skin with horny patches. Additionally, With these horny patches is great tenderness.
- A notable characteristic is the thickly coated tongue. Generally, it is thick and white; milky-white; or like whitewash evenly laid. In detail, The edges may be red and sore
- Sensitive to cold bathing.
- Thick, hard, honey-coloured scabs
- All in all, Itching when warm in bed.
Arsenicum album:
- Itching, burning, swellings; edema, eruption, papular, dry, rough, scaly; worse cold also scratching.
- Ulcers with raised and hard edges, surrounded by a red and shining crown; with the bottoms like lard, or of a blackish-blue colour, with burning pains or shooting, when the parts affected become cold.
- Lastly, A very deep acting remedy, affecting every organ and tissue.
Arsenic Iodatum:
- Dry, scaly, itching.
- Marked exfoliation of skin in large scales, leaving a raw exuding surface beneath.
Dulcamara:
- Basically; Pruritus, always worse in cold, wet weather Humid eruptions on face, genitals, hands Warts, large, smooth, on face also palmar surface of hands.
- Thick, brown-yellow crusts, bleeding when scratched.
Juglans cineraria:
- Eruption resembling eczema simplex on upper chest, with itching pricking when heated by over-exertion.
- Furthermore, Pustules on thighs, hips, and nates, with itching and burning, a few pustules on body, face, and arms.
- Itching in spots, now here, now there, on head, neck, also shoulders, with pricking, burning and redness.
- Itching on arms > scratching.
Kali Bichromicum:
- Papular eruption.
- Hands become covered with deep, stinging cicatrice.
- Ulcer with punched-out edges, with tendency to penetrate and tenacious exudation.
Ledum palustre:
- Eruption of small pimple like red millet seed over the body.
- Excessive itching on the back of both feet worse especially after scratching and by warmth of bed > scratching.
Sulphur:
- Dirty, filthy people, prone to skin affections. Aversion to being washed.
- Very red lips also face.
- Dry, scaly, unhealthy; every little injury suppurates. Itching, burning; worse scratching also washing.
- Skin affections after local medication. Pruritus, especially from warmth, is evening, often recurs in spring-time, in damp weather.[5]
Diet & Regimen
Diet & Regimen
- Vitamin B rich foods like Eat green vegetables, sesame seeds, pulses, whole grain.
- Vitamin A rich foods like yellow orange fruits, vegetables, cereals, fortified foods can help.
- Cod liver oil supplements containing Vitamin A and D are also very helpful.
- Include Omega 3 fatty acids which are good for your skin such as flaxseed, olive oil, walnuts, corn.
- Green teas a great antioxidant, which can help in Lichen Planus.
- Folic acid rich foods like green vegetables prevent dry skin.
- Consume adequate water to maintain good hydration.
- Avoid excess of salt, sugar, refined foods, artificial foods, preservatives.
- Avoid yeast, sour and acidic foods, vinegar, tamarind, refined flours.
- Avoid foods which can cause allergy in you.
- Avoid very tight clothes.[4]
Do’s and Don'ts
Do’s and Don’ts
It is a chronic inflammatory skin condition that can cause discomfort and affect your quality of life. While there’s no cure, managing the condition effectively can help alleviate symptoms and prevent complications. Here’s a list of do’s and don’ts to help you navigate life with lichen planus:
Do’s:
Consult a dermatologist: Get a proper diagnosis and discuss treatment options.
Follow your treatment plan: Adhere to your doctor’s recommendations for medications and therapies.
Maintain good oral hygiene: Brush and floss regularly, use a soft-bristled toothbrush, and rinse with a non-alcoholic mouthwash if you have oral lichen planus.
Keep your skin moisturized: Use a gentle, fragrance-free moisturizer to soothe dry, itchy skin.
Identify and avoid triggers: Keep track of potential triggers like stress, certain medications, or allergens, and try to minimize exposure.
Manage stress: Practice relaxation techniques like yoga, meditation, or deep breathing to reduce stress, which can worsen symptoms.
Protect your skin from the sun: Wear protective clothing and use a broad-spectrum sunscreen with SPF 30 or higher.
Eat a healthy diet: Focus on a balanced diet rich in fruits, vegetables, and whole grains to support your immune system and overall health.
Don’ts:
- Scratch or pick at the lesions: This can damage your skin, increase the risk of infection, and worsen scarring.
- Use harsh soaps or detergents: These can irritate your skin and exacerbate symptoms.
- Smoke or use tobacco products: These can worsen oral lichen planus and increase the risk of oral cancer.
- Drink excessive alcohol: Alcohol can irritate your mouth and make oral lichen planus symptoms worse.
- Self-medicate: Don’t try to treat lichen planus with over-the-counter remedies without consulting your doctor.
- Ignore your symptoms: If you notice any changes in your skin or mouth, seek medical advice promptly.
By following these do’s and don’ts, you can effectively manage lichen planus and improve your quality of life. Remember, consistency is key, and working closely with your healthcare provider is crucial for optimal results.
Terminology
Terminology
Here are some terminologies and their meanings commonly used in articles about Lichen Planus:
- Lichen Planus: A chronic inflammatory skin condition characterized by itchy, flat-topped, purplish bumps.
- Lesions: Areas of damaged or abnormal tissue caused by the disease.
- Plaques: Raised, flat-topped lesions larger than 1 cm in diameter.
- Papules: Small, raised lesions less than 1 cm in diameter.
- Pruritus: Itching, a common symptom of lichen planus.
- Hypertrophic Lichen Planus: A variant of lichen planus with thick, warty plaques.
- Atrophic Lichen Planus: A variant of lichen planus with thin, white, wrinkled lesions.
- Bullous Lichen Planus: A variant of lichen planus with fluid-filled blisters.
- Oral Lichen Planus: Lichen planus affecting the mucous membranes of the mouth.
- Erosive Lichen Planus: A type of oral lichen planus with painful sores and ulcers.
- Reticular Lichen Planus: The most common type of oral lichen planus, with a lacy white pattern.
- Wickham’s Striae: Fine, white lines seen in the lesions of lichen planus.
- Koebner Phenomenon: The appearance of new lesions at sites of injury.
- Immunosuppressants: Medications that suppress the immune system, used to treat severe cases of lichen planus.
- Corticosteroids: Anti-inflammatory medications used to reduce inflammation and itching in lichen planus.
- Retinoids: Vitamin A derivatives used to treat skin conditions, sometimes used for lichen planus.
These are just a few of the terminologies used in articles about lichen planus. Understanding these terms can help you better understand the condition and its treatment options.
Terminology Related To Homoeopathy
- Miasm: A predisposition to chronic disease, believed to be inherited. In homeopathy, Lichen Planus is often associated with the Psora and Sycosis miasms.
- Constitutional Remedy: A homeopathic medicine chosen based on the individual’s overall physical, mental, and emotional characteristics, rather than just the specific symptoms of Lichen Planus.
- Repertorization: The process of selecting a homeopathic remedy by matching the patient’s symptoms with those listed in a repertory (a reference book of symptoms and their corresponding remedies).
- Keynote Symptoms: Characteristic symptoms that are particularly indicative of a specific homeopathic remedy.
- Aggravation: A temporary worsening of symptoms after taking a homeopathic remedy, often seen as a positive sign of healing.
- Amelioration: An improvement of symptoms after taking a homeopathic remedy.
- Potency: The strength or dilution of a homeopathic remedy.
- Proving: A systematic study in which healthy volunteers take a homeopathic remedy to record its effects, helping to understand the remedy’s potential uses.
References
References use for Article Lichen planus
- Davidsons Medicine 21th
- Textbook of Medicine, 5th Edition
- https://www.mayoclinic.org/diseases-conditions/lichen-planus/diagnosis-treatment/drc-20351383
- https://www.welcomecure.com/diseases/lichen-planus/diet-and-nutrition
- https://www.msdmanuals.com/en-in/professional/dermatologic-disorders/psoriasis-and-scaling-diseases/lichen-planus
- https://www.lybrate.com/topic/lichen-planus-everything-you-need-to-know/a248493cdb4740ba62436e4fbcde8ebc
- https://www.researchgate.net/figure/Etiopathogenesis-of-oral-lichen-planus_fig1_346385208
- https://emedicine.medscape.com/article/1123213-differential.
- Sharma, A., Gupta, S., Ramam, M., & Sharma, R. K. (2010). Indian epidemiology of lichen planus. Indian Journal of Dermatology, Venereology and Leprology, 76(1), 12-17, 2010.
- Andrews’ Diseases of the Skin: Clinical Dermatology,13th Edition, William D. James, Timothy G. Berger, Dirk M. Elston, 2020, Elsevier.
- Bolognia, J. L., Jorizzo, J. L., & Schaffer, J. V. (2018). Dermatology (4th ed.). Elsevier, Jean L. Bolognia, Joseph L. Jorizzo, Julie V. Schaffer, 2018, Elsevier.
- Rook’s Textbook of Termatology, 9th Edition, Christopher Griffiths, Jonathan Barker, Tanya Bleiker, Richard Chalmers, Daniel Creamer, et al. 2016, Wiley Blackwell.
- Bolognia JL, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
Also Search As
Also Search As
People can search for homeopathic articles on Lichen Planus using various methods:
Online Search Engines:
- Use search terms like "homeopathy Lichen Planus," "homeopathic treatment for Lichen Planus," or "Lichen Planus homeopathic remedies" on search engines like Google, DuckDuckGo, or Bing. This will lead to websites, blogs, and articles on the topic.
- Look for reputable sources like the National Center for Homeopathy, homeopathic journals, or websites of recognized homeopathic practitioners and organizations.
Homeopathic Databases:
- Search in specialized homeopathic databases like HOMER, RadarOpus, or Synthesis. These databases often contain case studies, provings, and materia medica information relevant to Lichen Planus.
Homeopathic Practitioners:
- Consult with a qualified homeopathic practitioner. They can provide you with relevant articles, research papers, and case studies on Lichen Planus from their own resources or direct you to reliable sources.
Social Media Groups:
- Join online forums and social media groups dedicated to homeopathy. These platforms often have discussions and shared resources on homeopathic treatment of Lichen Planus.
Homeopathic Libraries:
- Visit a local homeopathic library or the library of a homeopathic college. They usually have a collection of books, journals, and other resources on homeopathic treatment of various conditions, including Lichen Planus.
Remember to critically evaluate the information you find and consult with a qualified homeopathic practitioner for personalized advice and treatment.
Frequently Asked Questions (FAQ)
What is Lichen planus ?
Lichen planus (LP) is an acute or chronic inflammatory dermatosis involving skin and / or mucous membrane. It is a rash characterized by intensely itchy polygonal papules with a violaceous hue involving the skin and, less commonly, the mucosae, hair and nails.
How is Lichen Planus diagnosed?
It is usually made based on the appearance of the skin lesions and sometimes a biopsy may be needed to confirm the diagnosis.
What are the types of Lichen Planus ?
- Hypertrophic lichen planus
- Annular lesions
- Linear violaceus papules of lichen planus.
- Follicular lesions
- Graham Little syndrome
- Lichen planus actinicus
- Ulcerative lesions
What are the symptoms of Lichen Planus?
Symptoms
Common symptoms include itchy, purple or reddish-purple bumps, lacy white patches in the mouth, and sometimes, pain or burning in the affected areas.
Can homeopathy treat Lichen Planus effectively?
Homeopathy offers a holistic approach to Lichen Planus treatment, aiming to address the root cause and individual symptoms. While results vary, many people find relief and improvement in their condition through homeopathic remedies.
Is homeopathic treatment safe for Lichen Planus?
Homeopathic remedies are generally considered safe when prescribed by a qualified practitioner. They are prepared in highly diluted forms and are unlikely to cause side effects.
What are the treatment options for Lichen Planus?
Treatment aims to relieve symptoms and may include topical corticosteroids, oral medications, light therapy, or other options depending on the severity and location of the condition.
How long does it take for homeopathic treatment to show results in Lichen Planus?
The response to homeopathic treatment varies from person to person. Some individuals may experience improvement in symptoms within a few weeks, while others may take longer.
Is it important to consult a doctor for Lichen Planus even if considering homeopathic treatment?
Yes, it’s crucial to consult a doctor or dermatologist for a proper diagnosis and to rule out any other underlying conditions. Homeopathic treatment can be used as a complementary therapy alongside conventional medical advice.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Lichen Planus?
Homoeopathic Medicines For lichen Planus
- Antimonium crudum
- Arsenicum album
- Arsenic Iodatum
- Dulcamara
- Juglans cineraria
- Kali Bichromicum
- Ledum palustre
- Sulphur
