Mastitis
Definition
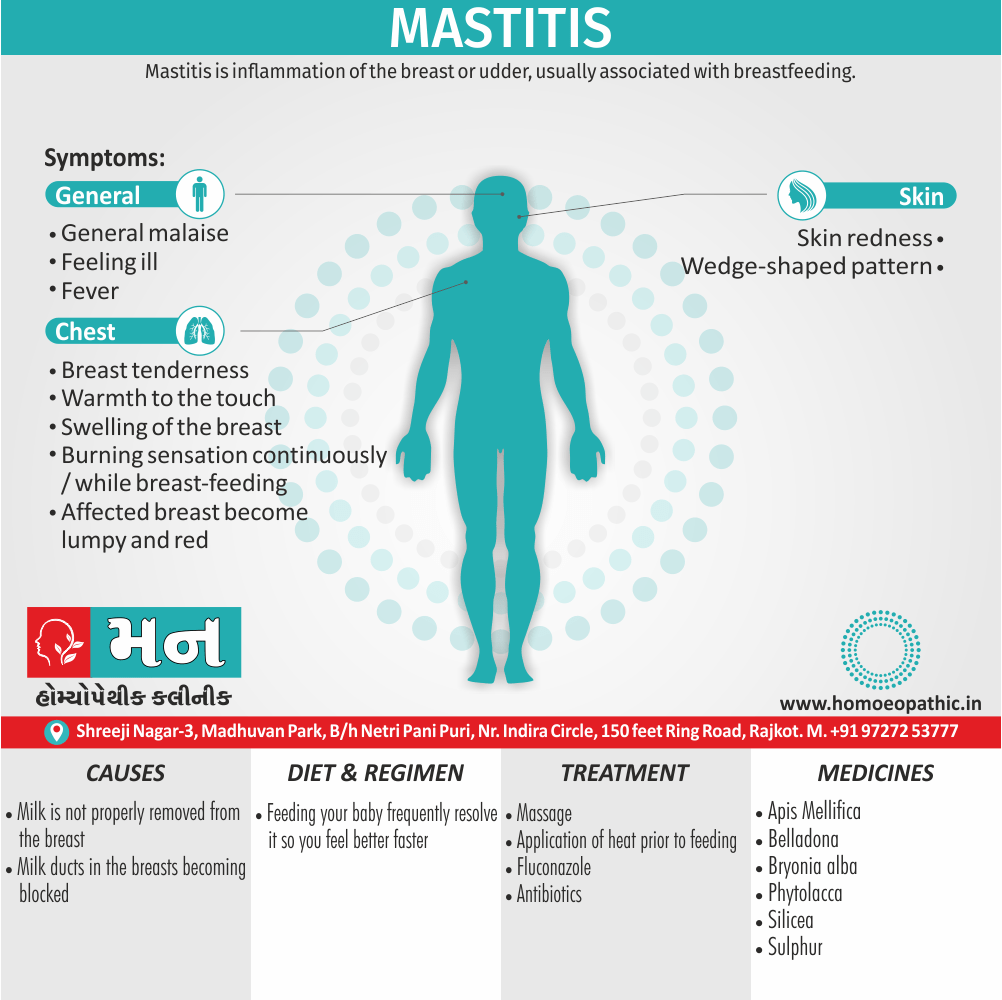
Mastitis is inflammation of the breast or udder, usually associated with breastfeeding.[1]
Here are some synonyms for mastitis:
- Mammitis: This is a less common synonym derived from the Latin "mamma" meaning breast.
- Garget: This is an informal term, primarily used in veterinary medicine, for mastitis in cows and other animals. It’s important to note that while "mammitis" is technically a synonym, "mastitis" is the more widely used term in modern medicine.
Overview
Epidemiology
Causes
Risk Factors
Pathogenesis
Pathophysiology
Types
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
Mastitis is an inflammatory condition that affects the mammary glands, primarily in breastfeeding women. It’s often characterized by breast pain, swelling, redness, and warmth. Mastitis can lead to complications if left untreated, such as abscess formation. [7]
Risk factors include poor latch, cracked nipples, use of a breast pump, and weaning. [1]
Mastitis: Causes, Symptoms, Treatment, and Prevention – Your Comprehensive Guide
This in-depth article covers every aspect of Mastitis, a condition that can cause significant discomfort and worry for breastfeeding mothers. Article delve into the various causes of Mastitis, including blocked milk ducts and bacterial infections. We outline the key symptoms to watch for, such as breast pain, swelling, and redness.
We explore a range of treatment options, from homoeopathic remedies and over-the-counter medications to prescription antibiotics. Article also provide practical tips for preventing Mastitis, empowering mothers to take proactive steps to protect their breast health.
Epidemiology
Causes
Causes
- Mastitis typically develops when the milk is not properly removed from the breast.
- Milk stasis can lead to the milk ducts in the breasts becoming blocked, as the breast milk is not being properly and regularly expressed.
- Mastitis may occur when the baby is not appropriately attached to the breast while feeding, when the baby has infrequent feeds or has problems suckling the milk out of the breast.
- The presence of cracks or sores on the nipples increases the likelihood of infection.
- Tight clothing or ill-fitting bras may also cause problems as they compress the breasts.
- There is a possibility that infants carrying infectious pathogens in their noses can infect their mothers the clinical significance of this finding is still unknown.
- Mastitis and breast abscesses can also be caused by direct trauma to the breast. Such injury can occur for example during sports activities or due to seat belt injury.
Risk Factors
Risk factors
Milk Stasis:
Incomplete or infrequent milk removal due to factors like engorgement, plugged ducts, tight clothing, or poor latch.
Nipple Trauma:
Cracked or damaged nipples provide an entry point for bacteria.
Bacterial Infection:
Often caused by Staphylococcus aureus or Streptococcus species.
Maternal Factors:
Stress, fatigue, illness, and poor nutrition can compromise the immune system.
Breastfeeding Practices:
Inconsistent feeding patterns, abrupt weaning, and improper hygiene can increase risk.
Previous Mastitis:
A history of mastitis increases the likelihood of recurrence.
Please note that this is just a summary of risk factors covered in the book. For a more comprehensive understanding, it is recommended to consult the reference text directly.[4]
Pathogenesis
Pathogenesis
Milk Stasis:
Incomplete milk removal leads to milk stasis, creating a favorable environment for bacterial growth.
Bacterial Invasion:
Bacteria, most commonly Staphylococcus aureus, enter the breast through cracks or fissures in the nipple.
Inflammatory Response:
The body reacts to the bacterial invasion, causing inflammation and swelling.
Ductal Blockage:
Inflammation and swelling can block milk ducts, further exacerbating milk stasis.
Tissue Damage:
In severe cases, the infection can lead to abscess formation and tissue damage.
Key Points:
- Mastitis is primarily caused by a bacterial infection.
- Milk stasis is a major contributing factor to mastitis.
- The inflammatory response plays a crucial role in the pathogenesis of mastitis.
Please note that this is a simplified explanation of the pathogenesis of mastitis. The actual process can be more complex and involve various factors. For a more comprehensive understanding, it is recommended to consult the reference text directly.[5]
Pathophysiology
Pathophysiology
- In lactational mastitis, it is likely that bacteria (often originating from the mouth of the infant) gain entry via cracks or fissures in the nipple surface.
- Once the primary defences are breached, organisms have an ideal culture environment in nutrient rich maternal milk leading to rapid replication.[1]
Types
Classification
Puerperal mastitis
- When it occurs in breastfeeding mothers, it is known as puerperal mastitis lactation mastitis, or lactational mastitis.
Non-puerperal mastitis
- When it occurs in non-breastfeeding women it is known as non-puerperal or nonlocational.
Pregnancy related
- Generally, Puerperal mastitis is the inflammation of the breast in connection with pregnancy, breastfeeding or weaning.
- It appears that proper breastfeeding technique, frequent breastfeeding and avoidance of stress are the most important factors that can be influenced.
- All in all, Light cases of mastitis are often called breast engorgement; the distinction is overlapping and possibly arbitrary or subject to regional variations.
Non pregnancy related
- The term nonpuerperal mastitis describes inflammatory lesions of the breast occurring unrelated to pregnancy and breastfeeding.
- Names for non-puerperal mastitis are not used very consistently and include mastitis, subareolar abscess, duct ectasia, periductal inflammation, Zuska’s disease also others.
- it is predicted that smoking may be related. Additionally, this condition is mainly seen in young women but can also be seen in men. [1]
Clinical Features
Clinical Features
Localized Breast Pain:
Pain is often described as throbbing, aching, or burning and is usually focused in one area of the breast.
Breast Swelling and Redness:
The affected area may appear swollen, warm to the touch, and red or pink.
Flu-like Symptoms:
Fever, chills, body aches, and fatigue are common systemic symptoms.
Nipple Changes:
The nipple may appear cracked, blistered, or sore.
Changes in Milk:
Milk may appear watery, lumpy, or even contain streaks of blood or pus.
Additional Clinical Features (Not specifically mentioned in the book):
Hardened Area in the Breast:
A firm lump or area of engorgement may be palpable.
Tender Axillary Lymph Nodes:
Lymph nodes under the arm on the affected side may be swollen and tender.
Please note: This is just a summary of clinical features. The severity and presentation of mastitis can vary, and not all symptoms may be present in every case. It’s important to consult a healthcare professional for proper diagnosis and treatment.[5]
Sign & Symptoms
Sign & Symptoms of Mastitis
Lactation mastitis usually affects only one breast and the symptoms can develop quickly.
The signs and symptoms usually appear suddenly and they include i.e.:
- Breast either tenderness or warmth to the touch
- Either General malaise or feeling ill
- Swelling of the breast
- Pain or a burning sensation continuously or while breast-feeding
- Skin redness, often in a wedge-shaped pattern
- Fever of 101 F (38.3 C) or greater
- The affected breast can then start to appear lumpy and red.
Some women may also experience flu-like symptoms such as:
- Aches
- Shivering and chills
- Feeling anxious or stressed
- Fatigue
- Contact should be made with a health care provider with special breastfeeding competence as soon as the patient recognizes the combination of signs and symptoms.
- Most of the women first experience the flu-like symptoms and just after they may notice a sore red area on the breast.
- Also, women should seek medical care if they notice any abnormal discharge from the nipples, if breast pain is making it difficult to function each day, or they have prolonged, unexplained breast pain.
Clinical Examination
Clinical Examination
Inspection:
- Observe the breasts for asymmetry, redness, swelling, or areas of warmth.
- Look for skin changes like dimpling, peau d’orange (orange peel appearance), or nipple changes (cracks, blisters, discharge).
Palpation:
- Gently palpate the breasts for areas of tenderness, firmness, or masses.
- Check for enlarged or tender axillary lymph nodes.
- If a fluctuant mass is felt, it may indicate an abscess.
Expression of Milk:
- Express milk from the affected breast to assess for changes in color, consistency (watery, thick, lumpy), or presence of blood or pus.
Vital Signs:
Additional Assessment:
- Inquire about the patient’s medical history, breastfeeding practices, and current medications.
- Ask about the onset and duration of symptoms, pain severity, and any associated symptoms like chills or fatigue.
Important Considerations:
- Early diagnosis and treatment of mastitis are crucial to prevent complications.
- Clinical examination should be done with a gentle touch to avoid further pain or discomfort.
- If mastitis is suspected, it is important to differentiate it from other breast conditions like abscess, plugged duct, or inflammatory breast cancer.
- Further diagnostic tests (e.g., milk culture, ultrasound) may be warranted in some cases.[6]
Diagnosis
Diagnosis
- The diagnosis of mastitis and breast abscess can usually made based on a physical examination. The doctor will also take into account the signs and symptoms of the condition.
- However, if the doctor is not sure whether the mass is an abscess or a tumor, a breast ultrasound may perform.
- In cases of infectious mastitis, cultures may need in order to determine what type of organism is causing the infection. Cultures are helpful in deciding the specific type of antibiotics that will use in curing the disease.
- These cultures may take either from the breast milk or of the material aspirated from an abscess.
- Mammograms or breast biopsies are normally performing on women.
Differential Diagnosis
Differential Diagnosis
- Galactocele
- Breast engorgement
- Mastodynia
- Fibrocystic breast disease
- Breast cancer
- Fibroadenoma
- Mondor’s disease
- Breast abscess
Complications
Complications
Abscess Formation:
If left untreated, mastitis can progress to form an abscess, a localized collection of pus within the breast tissue. This requires surgical drainage or needle aspiration.
Recurrent Mastitis:
Women who experience mastitis are at increased risk of recurrence, especially if underlying risk factors are not addressed.
Chronic Mastitis:
In rare cases, mastitis can become chronic, persisting for weeks or months despite treatment. This may require further investigation and specialized care.
Impaired Milk Production:
Severe or prolonged mastitis can lead to decreased milk supply in the affected breast.
Psychological Impact:
Mastitis can cause significant pain and discomfort, leading to emotional distress and negatively impacting breastfeeding experience.
Additional Complications (Not specifically mentioned in the book):
Sepsis:
In rare cases, untreated mastitis can lead to sepsis, a life-threatening systemic infection.
Infant Infection:
Although uncommon, bacteria causing mastitis can be transmitted to the infant through breast milk.
It is important to note that timely diagnosis and treatment of mastitis can significantly reduce the risk of complications. If you suspect you have mastitis, consult a healthcare professional promptly.[5]
Investigations
Investigations
Physical Examination:
- A thorough breast examination is the first step in diagnosing mastitis. The healthcare provider will look for signs of inflammation, such as redness, swelling, warmth, and tenderness. They may also check for enlarged lymph nodes under the arm.
Milk Expression and Observation:
- Expressing a small amount of milk from the affected breast can help determine if the milk is discolored, thickened, or contains blood or pus. This can be an indication of infection.
Milk Culture (Optional):
- A milk culture is not routinely recommended for uncomplicated mastitis. However, if symptoms are severe, persistent, or recurrent, or if there are concerns about antibiotic resistance, a milk culture may be performed to identify the specific bacteria causing the infection.
Other Tests (Rarely Needed):
- In rare cases, additional tests like ultrasound or biopsy may be needed to rule out other conditions that can mimic mastitis, such as breast abscess or inflammatory breast cancer.
Important Considerations:
- The decision to perform additional investigations depends on the severity of symptoms, the individual’s medical history, and the clinical judgment of the healthcare provider.
- It is important to note that not all cases of mastitis require investigation beyond a physical examination and milk expression.
- If you suspect you have mastitis, consult with a healthcare professional for proper diagnosis and treatment.
Treatment
Treatment
- In lactation mastitis, frequent emptying of both breasts by breastfeeding is essential. Also essential is adequate fluid supply for the mother and baby.
- For breastfeeding women with light mastitis, massage and application of heat prior to feeding can help as this may aid unblocking the ducts.
- No puerperal mastitis is treated by medication and possibly aspiration or drainage (see in particular treatment of subareolar abscess and treatment of granulomatous mastitis).
- In idiopathic granulomatous mastitis, successful treatment includes invasive surgical procedures or less invasive treatment with steroid medications. [1]
Prevention
Prevention
Effective Milk Removal:
- Frequent and complete emptying of the breasts is crucial to prevent milk stasis, a major risk factor for mastitis.
- Ensure proper latch and positioning during breastfeeding to facilitate optimal milk transfer.
- If the baby is unable to nurse effectively, express milk manually or with a pump to maintain milk flow.
Nipple Care:
- Prevent nipple trauma by ensuring a proper latch and avoiding forceful removal of the baby from the breast.
- Use soothing nipple creams or ointments to keep nipples hydrated and prevent cracking.
- Seek help from a lactation consultant if experiencing nipple pain or latch difficulties.
Hygiene:
- Wash hands thoroughly before and after breastfeeding or handling breast pumps.
- Clean breast pump parts regularly according to manufacturer’s instructions.
- Change nursing pads frequently to prevent moisture buildup and bacterial growth.
Supportive Practices:
- Get adequate rest and sleep to maintain a healthy immune system.
- Eat a balanced diet rich in nutrients to support overall well-being.
- Manage stress through relaxation techniques or seeking support from others.
- Avoid tight clothing or bras that can restrict milk flow.
Early Recognition and Treatment:
- Be aware of the early signs and symptoms of mastitis, such as breast pain, redness, swelling, and fever.
- Seek prompt medical attention if you suspect mastitis to prevent complications and ensure timely treatment.
Please note that this is just a summary of prevention strategies covered in the book. For a more comprehensive understanding, it is recommended to consult the reference text directly.[4]
Homeopathic Treatment
Homeopathic Treatment Of Mastitis
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Medicines:
Apis Mellifica
- Erysipelatous mastitis
- High fever, but no sweat
- Swelling, hardness of and burning, stinging in mammae
- Threatening in less degree to pass into suppuration and ulceration, great sensitiveness to touch or to slightest pressure. [2]
- Aggravation especially By cold applications.[2]
Belladona:
- Breasts feel heavy, red streaks running like radii from a central point.
- Accompanied by pulsating pains, heavy headache, constipation also scanty urine.
- Erysipelatous inflammation, stitches appear also disappear quickly.
- Aggravation specifically from jar or jolt.[2]
Bryonia:
- Stony heaviness of breast, hot, hard, painful, but not very red
- Severe stitching pains in breast
- Aggravation when lifting arm or motion, feels sick on first sitting up in bed or in a chair, and worse on standing up
- First stage of mammary abscess.[2]
Phytolaca:
- Hardness apparent from the start, caked breast, gathered breast, with large fistulous gaping also angry ulcers
- Discharging a watery foetid pus, nipples and mammae sensitive, even after suppuration has taken place
- Right mammae; when child nurse pain goes from the nipple all over the body.
- Aggravation evening. on the other hand; Amelioration after midnight.[2]
Phosphorus:
- Phlegmonous inflammation
- Breasts swollen, red in spots or streaks
- Hard knots in different places, with fistulous openings, burning stinging pains
- Watery, offensive discharge, hectic fever and night-sweats.[2]
Pulsatilla:
- Mastitis from mechanical pressure on gland, particularly in young girls.
- Nodosities in mammae, tensive pressure and swelling as from accumulation of milk during nursing.[2]
Silicea:
- Fistulous ulcers with callous edges,
- Discharge thin and watery or thick and offensive, substance of the breast seems to discharge into one common ulcer, often with pain, or there may be several orifices, one for each lobe.[2]
Sulphur:
- Inflammation running in radii from nipple, threatening suppuration.
- When the lumps first appear, easing the pain and modifying the destruction of tissue.
- Profuse suppuration with chilliness in the forenoon and heat in the afternoon, old ulcerations.
- Breasts feel hot, night-sweats, flushes of heat, weak and faint spells, irresistible hunger towards noon.[2]
Diet & Regimen
Diet & Regimen
Diet:
- Hydration is key: Drink plenty of fluids, especially water, to help flush out toxins and support milk production if breastfeeding.
- Nutrient-rich foods: Focus on whole, unprocessed foods like fruits, vegetables, whole grains, and lean protein to support your immune system and overall health.
- Healthy fats: Include foods rich in omega-3 fatty acids, like salmon, avocados, and nuts, to help reduce inflammation.
- Probiotic-rich foods: Consider adding yogurt, kefir, sauerkraut, and other fermented foods to support gut health, which can indirectly boost immunity.
- Limit sugar and processed foods: These can contribute to inflammation and may hinder healing.
Regimen:
- Rest: Get plenty of rest to allow your body to recover.
- Frequent breastfeeding or pumping: If breastfeeding, continue to nurse frequently or pump to ensure adequate milk drainage.
- Warm compresses: Apply warm compresses to the affected breast before and after feeding or pumping to help relieve pain and encourage milk flow.
- Proper breastfeeding technique: Ensure a good latch and proper positioning to help prevent milk stasis, which can contribute to mastitis.
- Pain relief: Use over-the-counter pain medications like ibuprofen or acetaminophen as needed.
- Antibiotics: If your doctor diagnoses an infection, it’s crucial to complete the full course of prescribed antibiotics.
- Supportive bra: Wear a comfortable, supportive bra that doesn’t restrict milk flow.
- Hydration is key: Drink plenty of fluids, especially water, to help flush out toxins and support milk production if breastfeeding.
Do’s and Don'ts
Do’s & Don’ts
Mastitis Do’s
- Continue breastfeeding or pumping: Frequent milk removal is crucial for healing. Start nursing on the affected side first to help with emptying.
- Rest: Get plenty of rest to help your body fight the infection.
- Hydrate: Drink plenty of fluids to stay hydrated and support milk production.
- Pain relief: Take over-the-counter pain relievers like ibuprofen or acetaminophen (if not contraindicated).
- Warm compresses: Apply warm compresses to the affected breast before and during feeding to help with milk flow and pain relief.
- Cold compresses: Use cold compresses between feedings to reduce inflammation and pain.
- Gentle massage: Gently massage the affected area while breastfeeding or pumping to help with milk flow.
- Consult a healthcare professional: Seek prompt medical attention for diagnosis and treatment. Antibiotics may be necessary.
- Practice good hygiene: Wash hands frequently and keep nipples clean and dry.
- Wear a supportive bra: A supportive bra can help reduce discomfort and provide support.
Mastitis Don’ts:
- Don’t stop breastfeeding: Unless advised by a healthcare professional, continue breastfeeding as it helps clear the infection.
- Don’t ignore symptoms: Early treatment is important to prevent complications. Seek medical attention if symptoms worsen or do not improve within 24-48 hours.
- Don’t apply heat before feeding: Heat can increase inflammation and worsen pain.
- Don’t massage vigorously: Gentle massage is okay, but avoid deep or forceful massage as it can damage breast tissue.
- Don’t wear tight clothing or bras: Tight clothing can restrict milk flow and exacerbate symptoms.
- Don’t delay seeking help: If you’re unsure about your symptoms or treatment, consult a healthcare professional or lactation consultant.
Please note that this is general advice, and individual recommendations may vary. It is always best to consult with a healthcare professional for personalized guidance.
Terminology
Terminology
Mastitis:
Inflammation of the breast tissue, usually caused by a bacterial infection.
Lactational Mastitis:
Mastitis occurring in breastfeeding women.
Non-Lactational Mastitis:
Mastitis occurring in women who are not breastfeeding.
Acute Mastitis:
Sudden onset of mastitis symptoms, usually accompanied by fever and localized breast pain.
Chronic Mastitis:
Persistent or recurrent mastitis that lasts for weeks or months.
Subclinical Mastitis:
Mastitis that does not cause obvious symptoms but can be detected through milk analysis.
Clinical Mastitis:
Mastitis with visible signs and symptoms, such as breast pain, redness, swelling, and fever.
Milk Stasis:
Incomplete or infrequent milk removal from the breast, leading to engorgement and increased risk of mastitis.
Plugged Duct:
Blockage of a milk duct, causing localized pain and swelling.
Abscess:
A collection of pus within the breast tissue, often a complication of untreated mastitis.
Inflammatory Breast Cancer:
A rare but aggressive form of breast cancer that can mimic the symptoms of mastitis.
Galactocele:
A milk-filled cyst that can develop in the breast during lactation or weaning.
Mammary Duct Ectasia:
A benign condition characterized by widening and inflammation of the milk ducts.
Periductal Mastitis:
Inflammation of the tissue around the milk ducts, often associated with smoking.
Lactation Consultant:
A healthcare professional specializing in breastfeeding support and management.
Antibiotics:
Medications used to treat bacterial infections, often prescribed for mastitis.
I hope this list is helpful! If you have any other questions, feel free to ask.
In homeopathic literature on mastitis, you might find these terms and their meanings:
Mastitis:
Inflammation of the breast tissue, often accompanied by pain, swelling, redness, and sometimes fever.
Mammary Abscess:
A collection of pus within the breast tissue, a potential complication of untreated mastitis.
Galactorrhea:
Excessive or spontaneous flow of milk from the breast, not associated with childbirth or breastfeeding.
Engorgement:
Overfilling of the breasts with milk, causing discomfort and potential complications like mastitis.
Suppression of Lactation:
The intentional stopping of milk production, sometimes done due to mastitis or other medical reasons.
Phytolacca Decandra:
A homeopathic remedy often used for mastitis with shooting pains and lumpy breasts.
Belladonna:
A homeopathic remedy for mastitis with sudden onset, redness, throbbing pain, and high fever.
Bryonia Alba:
A remedy for mastitis with stitching pains worsened by movement and a desire to lie still.
Pulsatilla:
A remedy for mastitis with shifting pains, emotional sensitivity, and a thick, creamy discharge.
Hepar Sulphuris Calcareum:
A remedy for mastitis with abscess formation, splinter-like pains, and sensitivity to cold.
Please note that homeopathic treatment should always be done under the guidance of a qualified homeopathic practitioner. This information is not a substitute for professional medical advice.
References
References
- https://en.wikipedia.org/wiki/Mastitis
- Homoeopathic Therapeutics By Lilienthal
- The New Indian Journal of OBGYN, 5(1), 30-34. (2018).
- Breastfeeding and Human Lactation (6th Edition),Authors: Karen Wambach, Jan Riordan,(2021),Publisher: Jones & Bartlett Learning.
- Core Curriculum for Lactation Consultant Practice (4th Edition)
Editor: Nancy Mohrbacher
(2017)’Publisher: Jones & Bartlett Learning. - Breastfeeding A Guide for the Medical Profession (9th Edition)
Authors: Ruth A. Lawrence, Robert M. Lawrence,(2020),Publisher: Elsevier - Title: Veterinary Reproduction
Edition: 11th Edition
Author(s): Senger, P.L.
Year of Publication: 2012
Publisher: Wiley-Blackwell
Also Search As
Also Search As
There are several ways people can search for homeopathic articles on mastitis:
Online Databases:
PubMed: While primarily for conventional medicine, it sometimes includes homeopathic studies. Use keywords like "homeopathy mastitis" or "homeopathic treatment mastitis."
The National Center for Homeopathy (NCH): This organization’s website may have articles or links to research on homeopathic approaches to mastitis.
Homeopathic Journals:
- The Indian Journal of Research in Homeopathy
- The American Journal of Homeopathic Medicine
Homeopathic Libraries:
Many homeopathic colleges and organizations have libraries with collections of books and journals on homeopathy. You can search their catalogs for articles on mastitis.
Homeopathic Practitioners:
Experienced homeopathic practitioners may have access to resources or can recommend relevant articles based on their knowledge and experience.
Online Search Engines:
Use search terms like "homeopathy mastitis research" or "homeopathic remedies for mastitis" to find articles, case studies, or discussions on homeopathic forums and websites.
Tips for Effective Searching:
- Use specific keywords: Include terms like "homeopathy," "mastitis," "treatment," "remedies," and "research."
- Use filters: If searching a database, use filters to narrow down results by date, publication type, or language.
- Be critical: Evaluate the quality of the information you find. Look for articles published in reputable journals and consider the evidence presented.
- Consult a homeopathic practitioner: If you are considering homeopathic treatment for mastitis, it’s important to consult with a qualified practitioner for personalized advice.
There are several ways to search for information on mastitis:
Online Resources:
- Search Engines: Use search engines like Google, Bing, or DuckDuckGo with keywords like "mastitis," "breast infection," or "breastfeeding complications."
- Reputable Websites: Consult reliable websites like the Mayo Clinic, Cleveland Clinic, WebMD, or the National Institutes of Health (NIH) for comprehensive information on mastitis.
- Medical Databases: If you’re looking for scientific publications or research articles on mastitis, search databases like PubMed, Google Scholar, or ScienceDirect.
Offline Resources:
- Medical Textbooks: Refer to medical textbooks like "Breastfeeding A Guide for the Medical Profession" by Ruth A. Lawrence and Robert M. Lawrence, or "Core Curriculum for Lactation Consultant Practice" edited by Nancy Mohrbacher, for in-depth information on mastitis.
- Medical Libraries: If you have access to a medical library, you can search for books, journals, and articles on mastitis.
- Healthcare Professionals: Consult with a doctor, nurse, lactation consultant, or other healthcare provider for personalized advice and guidance on mastitis.
Specific Search Tips:
- Use specific keywords: Instead of just searching for "mastitis," use more specific terms like "mastitis symptoms," "mastitis treatment," or "mastitis prevention."
- Combine keywords: You can combine multiple keywords to narrow down your search, such as "mastitis antibiotics" or "mastitis breastfeeding."
- Use filters: Many search engines and databases allow you to filter your results by date, publication type, or language.
- Check the source: Always evaluate the source of information to ensure it’s credible and reliable. Look for articles published in reputable journals or websites written by healthcare professionals.
By using a combination of online and offline resources, you can find a wealth of information on mastitis. Remember to consult with a healthcare professional for any medical concerns or questions.
Frequently Asked Questions (FAQ)
What is Mastitis?
Mastitis is inflammation of the breast or udder, usually associated with breastfeeding.
What causes Mastitis?
- Milk is not properly removed from the breast
- When the baby is not appropriately attached to the breast while feeding
- When the baby has infrequent feeds
- Problems suckling the milk out of the breast
- Cracks or sores on the nipples increases infection
- Tight clothing
- Direct trauma to the breast
How is mastitis treated?
Treatment for mastitis typically includes:
- Antibiotics to fight the infection
- Pain relievers to reduce discomfort
- Frequent breastfeeding or pumping to help drain the breast
- Rest and fluids
Give the types of Mastitis?
What are the symptoms of Mastitis?
- Breast tenderness or warmth to the touch
- General malaise or feeling ill
- Swelling of the breast
- Pain or a burning sensation continuously or while breast-feeding
- Skin redness, often in a wedge-shaped pattern
- Fever of 101 F (38.3 C) or greater
- Lumpy and red
Can homeopathy help with mastitis?
Yes, homeopathy offers a gentle and supportive approach to managing mastitis symptoms and promoting healing.
Are there any side effects of homeopathic remedies?
Homeopathic remedies are generally safe and have minimal side effects when used correctly. However, it’s always best to consult a homeopath before starting any new treatment.
How long does it take to see results with homeopathy?
The response time to homeopathic treatment can vary depending on the individual and the severity of the condition. Some people may experience relief quickly, while others may need more time.
Can I use homeopathy alongside conventional treatment?
Yes, homeopathy can be used as a complementary therapy alongside conventional treatment for mastitis.
