Meniere’s Disease
Definition
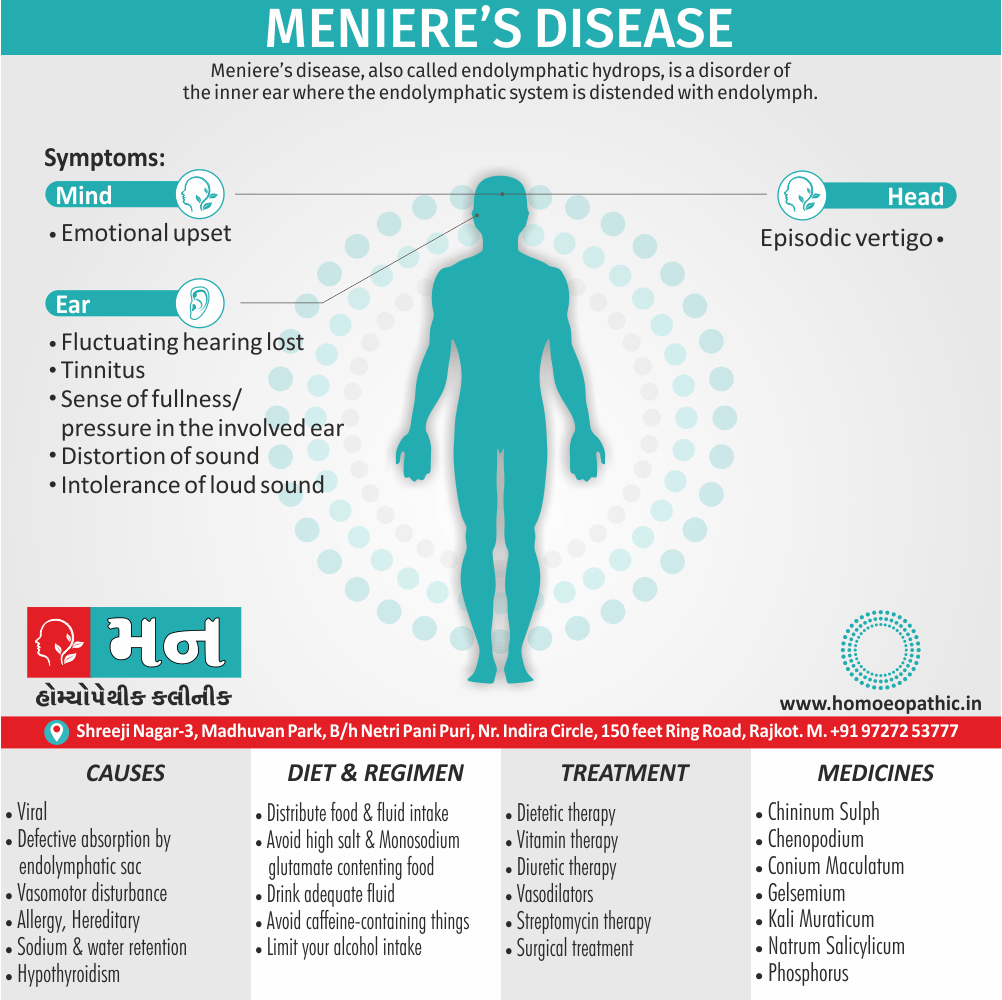
Meniere’s disease, also called endolymphatic hydrops, is a disorder of the inner ear where the endolymphatic system is distended with endolymph. It is characterized by
(i) Vertigo
(ii) Sensorineural hearing loss
(iii) Tinnitus and
(iv) Aural fullness. [1]
Meniere’s disease does have a few synonyms you might come across:
- Ménière disease: This is a slightly different spelling, using the accented "é".
- Meniere’s syndrome: This term emphasizes the collection of symptoms associated with the disease.
- Idiopathic endolymphatic hydrops: This is a more technical term that refers to the buildup of fluid in the inner ear, which is thought to be the underlying cause of Meniere’s disease.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Meniere’s Disease
- Varies from 7.5–157 per 100,000 persons. Affects primarily Caucasians with a slight female preponderance. About 10% of dizziness patients have Ménière’s.
- Age of onset is 4–90 years but peak incidence is in 40–60-year age group.
- Bilateral disease develops in 47% of cases followed up for 20 years. [2]
Epidemiology
Epidemiology
The incidence of Meniere’s disease in a tertiary care hospital in Mumbai was found to be 0.61% of all the patients tested for hearing impairment (Bhattacharya et al., 2021). [6]
Causes
Causes of Meniere’s Disease
Exact cause of the disease is not yet knew.
- Viral: The causative roles of viruses (HSV, cytomegalovirus or VZV) remain uncertain.
- Hereditary: Familial occurrence in 10–20% cases. There is an autosomal dominant mode of inheritance.
- Autoimmune: Certain genetically acquired major histocompatibility complexes specifically human leukocyte antigens (HLA) B8/DR3 and Cw7 have been associated with Meniere’s disease. [2]
- Defective absorption by endolymphatic sac: Normally, endolymph carry by the endolymphatic duct to the sac where it absorb. Defective absorption by the sac may be responsible for raised endolymph pressure.
- Experimental obstruction of endolymphatic sac and its duct also produces hydrops. Ischemia of sac has observe in cases of Meniere’s disease undergoing sac surgery, indicating poor vascularity and thus poor absorption by the sac.
- Distension of membranous labyrinth leads to rupture of Reissner’s membrane and thus mixing of perilymph with endolymph, which thought to bring about an attack of vertigo.
Vasomotor disturbance:
- There is sympathetic over activity resulting in spasm of internal auditory artery and/or its branches, thus interfering with the function of cochlear or vestibular sensory neuroepithelium.
- This is responsible for deafness and vertigo. Anoxia of capillaries of stria vascularis also causes increased permeability, with transudation of fluid and increased production of endolymph.
Allergy:
- The offending allergen may a foodstuff or an inhalant. Additionally, In these cases, inner ear acts as the “shock organ” producing excess of endolymph.
- Nearly 50% of patients with Ménière’s disease have concomitant inhalant and/or food allergy. Moreover, It is possible that Ménière’s disease is multifactorial, resulting in the common end point of endolymphatic hydrops with classical presentation.
- Lastly, Sodium also water retention: Excessive amounts of fluid retain leading to endolymphatic hydrops.
Hypothyroidism:
- In brief, Hypothyroidism: About 3% of cases of Ménière’s disease are due to hypothyroidism. Such cases benefit from thyroid replacement therapy.[1]
Types
Classification of Meniere’s Disease
Cochlear hydrops:
- Here, only the cochlear symptoms and signs of Ménière’s disease are present. Vertigo is absent.
- It is only after several years that vertigo will make its appearance.
- It is believed that in these cases, there is block at the level of ductus reunions, thereby confining the increased endolymph pressure to the cochlea only.
Vestibular hydrops
- Patient gets typical attacks of episodic vertigo while cochlear functions remain normal.
- It is only with time that a typical picture of Ménière’s disease will develop.
- Many of the cases of vestibular Ménière’s disease are labelled “recurrent vestibulopathy” as endolymphatic hydrops could not be demonstrated in the study of temporal bones in such cases.
Drop attacks (Tumarkin’s otolithic crisis):
- In this, there is a sudden drop attack without loss of consciousness.
- There is no vertigo or fluctuations in hearing loss. Patient gets a feeling of having been pushed to the ground or poleaxed.
- It is an uncommon manifestation of Ménière’s disease and occurs either in the early or late course of disease.
- Possible mechanism is deformation of the otolithic membrane of the utricle or saccule due to changes in the endolymphatic pressure.
Lermoyez syndrome:
- Here symptoms of Meniere’s disease are seen in reverse order.
- First there is progressive deterioration of hearing, followed by an attack of vertigo, at which time the hearing recovers.
Risk Factors
Risk Factors:
- Age: Meniere’s disease typically occurs in people between the ages of 40 and 60.
- Sex: Some studies suggest that women are slightly more likely to develop Meniere’s disease than men.
- Family history: If a family member has Meniere’s disease, you may be at a higher risk of developing it yourself. About 7% to 10% of people with Meniere’s disease have a family history of the disorder.
- Autoimmune diseases: People with autoimmune conditions, such as rheumatoid arthritis, lupus, or ankylosing spondylitis, may be more likely to develop Meniere’s disease.
- Head injury: A history of head injury may increase the risk of Meniere’s disease.
- Migraines: People who experience migraines may be more likely to develop Meniere’s disease.
It’s important to note that having one or more of these risk factors does not guarantee that you will develop Meniere’s disease. Conversely, some people without any risk factors may develop the condition.[7]
Pathogenesis
Pathogenesis
The pathogenesis of Meniere’s disease (MD) is not fully understood, but the leading theory is that it is caused by an excess of endolymph, the fluid that fills the inner ear. This excess endolymph can lead to a buildup of pressure in the inner ear, which can damage the delicate structures responsible for hearing and balance.
Possible causes of endolymphatic hydrops include:
- Blockage of the endolymphatic duct
- Abnormal immune response
- Viral infection
- Head trauma
- Genetic predisposition
The pathophysiologic sequence of events in Meniere’s disease includes:
- Endolymphatic hydrops
- Rupture of the membranous labyrinth
- Mixing of endolymph and perilymph
- Damage to hair cells and other inner ear structures
This damage to the inner ear can lead to the classic symptoms of Meniere’s disease, including:
- Episodic vertigo: A spinning sensation that can last for minutes to hours.
- Fluctuating sensorineural hearing loss: Hearing loss that comes and goes, and is usually worse in the lower frequencies.
- Tinnitus: A ringing, roaring, or buzzing sound in the ears.
- Aural fullness: A feeling of pressure or fullness in the ears.[8]
Pathophysiology
Pathophysiology of Meniere’s Disease
- Basically, Peri saccular ischemia and fibrosis lead to inadequate absorption of endolymph by the endolymphatic sac.
- Furthermore, Over accumulation of endolymph at the expense of peri lymphatic space results in the distortion of membranous labyrinth.
- Alterations in the size of endolymphatic duct also sac along with reductions in tubular specializations of the lining of these structures have been observed.
- Endolymphatic hydrops mainly occurs in pars inferior (cochlea also saccule) and changes in pars superior (utricle also SCC) are usually less obvious.
- The basilar membrane gets distended into scala tympani.
Hennebert’s sign
- Saccular distension can distort not only utricle and SCCs but can also come in contact with stapes footplate. That can cause Hennebert’s sign.
- Hair cells and their neurons are usually spared.
- Membranous rupture, which can occur in any part of the inner ear, allows leakage of potassium-rich endolymph into perilymph. Besides this, The high concentration of K+ depolarizes the neurons and inactivates both vestibular and auditory neurons that result in vertigo (paralytic nystagmus) and deafness.
- Healing of membranes allows restitution of normal chemical also clinical status.
- Repeated membranous rupture and potassium exposure lead to chronic deterioration in the functions of inner ear. [2]
Clinical Features
Clinical Features
Meniere’s disease is a chronic disorder of the inner ear characterized by a triad of symptoms:
- Episodic Vertigo:
Spontaneous episodes of spinning sensation, often accompanied by nausea and vomiting. These episodes can last from 20 minutes to several hours.
Sensorineural Hearing Loss: Fluctuating hearing loss, typically affecting low frequencies initially but can progress to involve all frequencies.
Tinnitus: Ringing or buzzing sound in the affected ear.
Aural Fullness: A sensation of pressure or fullness in the affected ear.
These symptoms can occur in various combinations and severity, often leading to significant impairment in the patient’s quality of life.[9]
This comprehensive textbook provides in-depth information on the diagnosis and management of Meniere’s disease, including the latest research findings and clinical practices..
Sign & Symptoms
Sign & Symptoms of Meniere’s Disease
Age and sex: Disease is commonly seen in the age group of 35–60 years. Males are affected more than females. Usually, disease is unilateral but the other ear may be affected after a few years.
Cardinal symptoms of Ménière’s disease are
(1) Episodic vertigo
(2) Fluctuating hearing loss,
(3) Tinnitus
(4) Sense of fullness or pressure in the involved ear.
- It comes in attacks. The onset is sudden. Patient gets a feeling of rotation of himself or his environment. Sometimes, there is feeling of “to and fro” or “up and down” movement.
- Attacks come in clusters, with periods of spontaneous remission lasting for weeks, months or years. Usually, an attack is accompanied by nausea and vomiting with ataxia and nystagmus.
- Severe attacks may be accompanied by other symptoms of vagal disturbances such as abdominal cramps, diarrhoea, cold sweats, pallor and bradycardia.
- Usually, there is no warning symptom of an oncoming attack of vertigo but sometimes the patient may feel a sense of fullness in the ear, change in character of tinnitus or discomfort in the ear which herald an attack.
Hearing loss:
- It usually accompanies vertigo or may precede it. Hearing improves after the attack and may be normal during the periods of remission.
- This fluctuating nature of hearing loss is quite characteristic of the disease.
- With recurrent attacks, improvement in hearing during remission may not be complete; some hearing loss being added in every attack leading to slow and progressive deterioration of hearing which is permanent.
- Distortion of sound- Some patients complain of distorted hearing. A tone of a particular frequency may appear normal in one ear and of higher pitch in the other leading to diplacusis. Music appears discordant.
- Intolerance to loud sounds- Patients of Ménière’s disease cannot tolerate amplification of sound due to recruitment phenomenon. They are poor candidates for hearing aids.
- It is low-pitched roaring type and is aggravated during acute attacks. Sometimes, it has a hissing character.
- It may persist during periods of remission. Change in intensity and pitch of tinnitus may be the warning symptom of attack.
Sense of fullness or pressure:
- Like other symptoms, it also fluctuates.
- It may accompany or precede an attack of vertigo.
Other features:
- Patients of Ménière’s disease often show signs of emotional upset due to apprehension of the repetition of attacks.
- Earlier, the emotional stress was considered to be the cause of Meniere’s disease.[1]
Clinical Examination
Clinical Examination
Otoscopy:
- Look for a normal or retracted tympanic membrane.
- In cases of secondary endolymphatic hydrops, signs of middle ear pathology (e.g., otitis media with effusion) may be present.
Tuning Fork Tests:
- Weber Test: Lateralization of sound to the unaffected ear in unilateral cases.
- Rinne Test: Positive test (air conduction > bone conduction) in both ears.
Audiometry:
- Pure-tone audiometry will reveal sensorineural hearing loss in the affected ear(s).
- The hearing loss typically affects low and mid frequencies initially, but can progress to involve all frequencies.
- Fluctuating hearing loss is a characteristic feature of Meniere’s disease.
Vestibular Function Tests:
- Spontaneous Nystagmus: Nystagmus may be present during acute attacks and beats towards the unaffected ear.
- Gans SOP (Sensory Organization Performance) Test: To assess balance and postural control.
- Caloric Test: May reveal reduced or absent vestibular response in the affected ear.
Neurological Examination:
- A comprehensive neurological examination should be performed to rule out other causes of vertigo and hearing loss.
Important Note:
- The clinical examination may vary depending on the stage of the disease and the individual patient.
- It is essential to correlate the clinical findings with the patient’s history and other investigations (e.g., MRI) to make an accurate diagnosis.
Additional Considerations:
- Meniere’s disease can have a significant impact on the patient’s quality of life.
- It is important to assess the patient’s functional status and emotional well-being.
- A multidisciplinary approach to management, involving otolaryngologists, audiologists, and vestibular therapists, is often necessary.[1]
Diagnosis
Diagnosis of Meniere’s Disease
Committee on Hearing and Equilibrium of the American Academy of Otolaryngology—Head and Neck Surgery (AAOHNS) classified the diagnosis of Ménière’s disease as follows:
Certain:
- Definite Ménière’s disease confirmed by histopathology.
Definite:
- Two or more definitive spontaneous episodes of vertigo lasting 20 min or longer.
- Audiometrically documented hearing loss on at least one occasion.
- Tinnitus or aural fullness in the affected ear.
- All other causes excluded.
Probable:
- One definitive episode of vertigo.
- Audiometrically documented hearing loss on at least one occasion.
- Tinnitus or aural fullness in the treated ear.
- Other causes excluded.
Possible:
- Episodic vertigo of Ménière’s type without documented hearing loss (vestibular variant) or
- Sensorineural hearing loss, fluctuating or fixed, with disequilibrium but without definitive episodes (cochlear variant).
- Other causes excluded. [1]
Other investigations are like;
- Pure tone audiometry: There is sensorineural hearing loss. In early stages, lower frequencies are affected and the curve is of rising type. When higher frequencies are involved curve becomes flat or a falling type.
- Speech audiometry: Discrimination score is usually 55–85% between the attacks but discrimination ability is much impaired during and immediately following an attack.
- Special audiometry tests: They indicate the cochlear nature of disease and thus help to differentiate from retrocochlear lesions, e.g. acoustic neuroma
(a) Recruitment test is positive.
(b) SISI (short increment sensitivity index) test. SISI score is better than 70% in two-thirds of the patients (normal 15%).
(c) Tone decay test. Normally, there is decay of less than 20 db.
- Electrocochleography: It shows changes diagnostic of Meniere’s disease. Normally, ratio of summating potential (SP) to action potential (AP) is 30%. In Meniere’s disease, SP/AP ratio is greater than 30%.
- Caloric test: It shows reduced response on the affected side in 75% of cases. Often, it reveals a canal paresis on the affected side (most common) but sometimes there is directional preponderance to healthy side or a combination of both canal paresis on the affected side and directional preponderance on the opposite side.
- Glycerol test: Glycerol is a dehydrating agent. When given orally, it reduces endolymph pressure and thus causes an improvement in hearing. [1]
Differential Diagnosis
Differential Diagnosis of Ménière’s Disease
Ménière’s disease is a disorder of the inner ear characterized by episodic vertigo, fluctuating sensorineural hearing loss, tinnitus, and aural fullness. It is crucial to differentiate Ménière’s disease from other conditions that can present with similar symptoms.
Differential Diagnoses:
- Benign Paroxysmal Positional Vertigo (BPPV): BPPV is the most common cause of vertigo. It is characterized by brief episodes of vertigo triggered by changes in head position. Unlike Ménière’s disease, BPPV does not cause hearing loss or tinnitus.
- Vestibular Migraine: Vestibular migraine is a type of migraine that causes vertigo, dizziness, and other vestibular symptoms. It can be difficult to differentiate from Ménière’s disease, but patients with vestibular migraine often have a history of migraines.
- Acoustic Neuroma (Vestibular Schwannoma): Acoustic neuroma is a benign tumor that grows on the vestibular nerve. It can cause hearing loss, tinnitus, and vertigo. Unlike Ménière’s disease, acoustic neuroma typically causes progressive hearing loss and may also cause facial numbness or weakness.
- Labyrinthitis and Vestibular Neuritis: Labyrinthitis and vestibular neuritis are inflammatory conditions of the inner ear that can cause vertigo, dizziness, and nausea. Unlike Ménière’s disease, labyrinthitis and vestibular neuritis usually have a sudden onset and may be associated with a viral infection.
- Autoimmune Inner Ear Disease (AIED): AIED is a rare condition in which the immune system attacks the inner ear, causing hearing loss, tinnitus, and vertigo. Unlike Ménière’s disease, AIED often causes bilateral hearing loss and may respond to immunosuppressive therapy.Autoimmune Inner Ear Disease (AIED)
- Central Vestibular Disorders: Central vestibular disorders are caused by problems in the brainstem or cerebellum. They can cause vertigo, dizziness, and imbalance, but unlike Ménière’s disease, they are not typically associated with hearing loss or tinnitus.
- Other Conditions: Other conditions that can mimic Ménière’s disease include multiple sclerosis, stroke, cardiovascular disorders, and certain medications.[10]
Note: A thorough evaluation by an otolaryngologist (ENT specialist) or a neurologist specializing in vestibular disorders is essential for accurate diagnosis and appropriate management.
Complications
Complications of Meniere’s Disease
Meniere’s disease, while not life-threatening, can significantly impact quality of life due to the following complications:
- Permanent hearing loss: The fluctuating hearing loss associated with Meniere’s disease can become permanent over time, especially if left untreated.
- Falls and injuries: Vertigo attacks can lead to falls, resulting in injuries ranging from minor cuts and bruises to more serious fractures.
- Psychological distress: The unpredictable nature of Meniere’s disease, combined with the debilitating symptoms, can lead to anxiety, depression, and social isolation.
- Impact on daily activities: The combination of hearing loss, vertigo, and tinnitus can make it difficult to work, drive, or participate in social activities.
This comprehensive medical textbook provides in-depth information on the diagnosis, management, and complications of Meniere’s disease.[11]
Additional Resources:
- Meniere’s disease – Symptoms and causes – Mayo Clinic: https://www.mayoclinic.org/diseases-conditions/menieres-disease/symptoms-causes/syc-20374910
- Meniere’s Disease | National Institute on Deafness and Other Communication Disorders (NIDCD): https://www.nidcd.nih.gov/health/menieres-disease
Investigations
Investigations
Typically include a combination of clinical assessment, audiological tests, and imaging studies.
Audiological Tests:
- Pure Tone Audiometry: Assesses the degree and type of hearing loss.
- Speech Audiometry: Evaluates the ability to understand speech at different volumes.
- Tympanometry: Measures middle ear function.
- Electrocochleography (ECochG): Detects changes in the inner ear’s electrical responses, which can suggest endolymphatic hydrops (increased fluid pressure), a hallmark of Meniere’s disease.
- Vestibular Evoked Myogenic Potentials (VEMPs): Assesses the function of the saccule and inferior vestibular nerve.
Imaging Studies:
- Magnetic Resonance Imaging (MRI): Rules out other causes of vertigo or hearing loss, such as brain tumors or acoustic neuromas.
- Computed Tomography (CT): May be used if MRI is contraindicated.
Other Tests:
- Blood tests: Rule out other conditions that can mimic Meniere’s disease, such as thyroid problems, autoimmune disorders, or infections.
- Glycerol test: This dehydration test can sometimes temporarily improve symptoms in people with Meniere’s disease, supporting the diagnosis.
This book offers detailed insights into the diagnosis and management of Meniere’s disease, including the specific investigations mentioned above.
Please note that this information is not a substitute for professional medical advice. Always consult with a qualified healthcare provider for diagnosis and treatment.[12]
Treatment
Treatment of Meniere’s Disease
There is no definite treatment of this condition. Various methods (medical and surgical) have adopted to alleviate the patient’s symptoms. The general management of the patient is of prime importance. An understanding and sympathetic approach to the problem is essential. Strong reassurance and stressing the nonfatal nature of the disorder is necessary.
- Treatment of the acute attack – The patient is put to bed rest. Any of the vestibular suppressants give to control the vestibular symptoms. The following drugs commonly use— prochlorperazine (Stemetil) 15 to 75 mg daily, orally or by injections; promethazine (Avomine, Phenergan); chlorpromazine (Largactil 25 mg thrice daily); or dimenhydrinate (Dramamine). The dosage adjust according to the patient’s needs. Sometimes the stellate ganglion block during an acute attack helps to relieve the symptoms. The long-term medical treatment has base on various theories.
Dietetic therapy i.e.:
It suggest that low salt and limited water intake reduces the hydrops.
Vitamin therapy i.e.:
All the vitamins, coenzymes and trace elements have use. Favorable effects have resulted from the administration of nicotinic acid and vitamin A and D.
Diuretic therapy i.e.:
Diuretics like acetazolamide have use on the assumption that these drugs will reduce the hydrops.
Vasodilators i.e.:
Such drugs have used with an idea that they relieve the angiospastic vascular changes in the endarterial distribution of the labyrinthine artery. Recently betahistadine hydrochloride (Vertin, Serc) has shown good results.
Streptomycin therapy i.e.:
Previously large doses of streptomycin use particularly in bilateral cases to induce labyrinthine damage (Chemical Labyrinthectomy).
Surgical treatment of Meniere’s disease Surgery consider for those cases of Meniere’s disease, which do not respond to medical therapy and where the disabling symptoms continue to occur.
The following procedures have used i.e.:
- Cervical sympathectomy
- Myringotomy with grommet insertion
- Operations on the endolymphatic sac
- Vestibular neurectomy
- Labyrinth destruction
- Selective destruction of vestibular labyrinth by cryosurgery or ultrasound: These physical methods have recently used for the treatment of Ménière’s disease. Additionally, This accomplish by selective destruction of the vestibular end organs in the labyrinth without damaging the cochlea or facial nerve.
- Cryosurgical methods[3]
Prevention
Prevention
There is no definitive way to prevent Meniere’s disease, as the exact cause is unknown. However, some lifestyle modifications and treatments may help reduce the frequency and severity of symptoms.
This book chapter explores various non-surgical treatment options for Meniere’s disease, including lifestyle modifications, medications, and therapies that could potentially contribute to prevention efforts. It may provide valuable insights and strategies for managing and potentially reducing the risk of future episodes.
Additional Tips:
- Manage Stress: Stress is a known trigger for Meniere’s disease symptoms. Practicing relaxation techniques like yoga, meditation, or deep breathing exercises may help manage stress and reduce symptom frequency.
- Limit Salt Intake: A low-sodium diet can help regulate fluid balance in the inner ear, potentially reducing the severity of Meniere’s attacks.
- Avoid Caffeine and Alcohol: Both caffeine and alcohol can worsen Meniere’s symptoms and should be avoided or limited.
- Get Adequate Sleep: Maintaining a regular sleep schedule and getting enough rest can help manage overall health and potentially reduce the frequency of Meniere’s episodes.
Please note that this information is not intended as a substitute for professional medical advice. If you are concerned about Meniere’s disease or experiencing symptoms, consult with a healthcare provider for proper diagnosis and treatment.[13]
Homeopathic Treatment
Homeopathic Treatment of Meniere’s Disease
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Meniere’s Disease:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Medicines:
Chininum Sulph
- Chinimum sulph is one of the top-indicated remedies for tinnitus present along with Meniere’s .
- The leading symptom to use this medicine in most of the cases is the presence of tinnitus. There is an unusual sensation of ringing or roaring in the ears, and it is invariably associated with vertigo.
- People in whom Chinimum sulph may generally be indicated have complaints of postural dizziness and heaviness in the ears.
- Vertigo could be very sudden in onset and in severe cases the person may fall due to loss of balance.
- Generally, they may feel uncomfortable in a standing posture. Chininum sulph gives desired results when there is a considerable degree of hearing loss (especially that affects the left ear).
Conium Maculatum
- Conium is usually suitable for people who experience severe Vertigo in Meniere’s disease.
- Sideways motion of the head tends to worsen the condition.
- A feeling of moving around in a circle may be present, and vertigo may also get worse from any movement in bed.
Gelsemium
- Use of this medicine is considered when there is marked dizziness Meniere’s Disease.
- Difficulty in walking with a loss of balance may arise from dizziness.
- Dim vision and heaviness of eyelids may attend above features may also be present.
4.Chenopodium Anthelminticum
- It is suitable for Meniere’s disease when the person hears a buzzing noise in the ear.
- Sudden vertigo episodes, better for high pitched sounds than low pitched sounds.
- Tinnitus that is synchronous with heartbeats are the symptoms indicative of using Chenopodium.
Salicylicum Acid
- Salicylicum Acid works well in those cases of Meniere’s disease where tinnitus and vertigo are present with troublesome nausea.
- The noises in the ear can be roaring, ringing, or buzzing (similar to flies or a swarm of bees) in nature.
- In some cases, a person hears musical noises. There is vertigo, diminished hearing, and with intense nausea.
Theridion
- Theridion is prescribed to people who are generally sensitive to noises and may feel a sudden discomfort when they hear loud and unpleasant sounds.
- The guiding symptom for Theridion to be prescribed is that vertigo appears when the person closes the eyes.
- Theridion may be indicated in people who detest traveling because it triggers attacks of vertigo.
- There may be an uneasy sensation in the ears with fullness or heaviness in one or both ears.
Kali Muraticum
- Kali Muraticum is a remedy that works especially in cases where there is deafness due to swelling of internal ear and eustachian tube.
- It causes a diminution (reduction) of the fluid secretion and gradually reduces the swelling. It is also useful for noises in the ears.
- There is a crackling noise in the ears on swallowing. Additionally, Vertigo is present, along with head congestion.
- A sensation of having a plug inside ears may be present along with the above symptoms.
- Lastly, There may be a history of chronic catarrhal conditions of the middle ear.
Natrum Salicylicum
- Natrum Salicylicum is a well-indicated for tinnitus of low tone.
- Along with noises, there is giddiness and deafness.
- Vertigo that gets worse from raising the head, on the other hand gets better upon lying down is present.
Silicea
- Silicea is a significant medicine for Meniere’s disease with prominent hissing noises in the ear.
- In some cases, the sounds may be loud and pistol-like. In detail, There is a feeling of blockage in the ears.
- Itching in the ears also vertigo spells upon closing the eyes are also present.
- Lastly, The person needing Silicea may have a history of ear discharges of offensive, fetid nature.
Cocculus Indicus
- Cocculus Indicus is an excellent medicine for Meniere’s disease when vertigo and dizziness with nausea and vomiting are present.
- There are noises in the ear that resemble the sound of rushing water.
- This is attended with loss of balance, hardness of hearing, a feeling of blockage in the ear, and dread of sudden noise.
Phosphorus
- Phosphorous is specifically used in cases where the person experiences noises in the ear along with severe vertigo also fainting spells.
- The sounds may be roaring or ringing in nature.
- Along with this, there is vertigo that is worse from looking up or down.
- Tickling and itching in ears may be there. Difficulty in hearing human voices may also be present. [4]
Diet & Regimen
Diet & Regimen of Meniere’s Disease
The goal of treatment is to provide stable body fluid/blood levels so that secondary fluctuations in the inner ear fluid can be avoided.
- Distribute your food and fluid intake evenly throughout the day and from day to day-
Eat approximately the same amount of food at each meal and do not skip meals. If you eat snacks, have them at regular times.
- Avoid eating foods or fluids which have a high salt content.
- Drink adequate amounts of fluid daily
- Avoid caffeine-containing fluids and foods (such as coffee, tea and chocolate). Caffeine has stimulant properties that may make your symptoms worse. Caffeine also may make tinnitus louder. Large amounts of caffeine may trigger migraine (migraine can be difficult diagnostically to separate from Meniere’s disease). Chocolate is also a migraine trigger.
- Limit your alcohol intake to one glass of beer or wine each day. Alcohol may trigger migraine associated vertigo.
- Avoid foods containing MSG (monosodium glutamate). This is often present in pre-packaged food products and in Chinese food. It may increase symptoms in some patients, possibly because of the link to migraine associated vertigo, and also because it contains sodium.[5]
Do’s and Don'ts
Do’s & Don’ts
Meniere’s disease is a chronic condition that affects the inner ear, causing episodes of vertigo, hearing loss, tinnitus (ringing in the ears), and a feeling of fullness in the ear. While there’s no cure, managing the condition involves lifestyle modifications and medical treatments to reduce the frequency and severity of symptoms.
Do’s:
- Follow a low-sodium diet: Reducing salt intake helps regulate fluid balance in the inner ear and can lessen the severity of Meniere’s attacks.
- Do manage stress: Stress is a known trigger for Meniere’s symptoms. Practice relaxation techniques like yoga, meditation, or deep breathing exercises.
- Get regular exercise:Staying physically active can improve overall health and may help reduce the frequency of episodes.
- Do stay hydrated:Drink plenty of water throughout the day to maintain proper fluid balance.
- Do get enough sleep:Aim for 7-8 hours of sleep per night to help manage overall health and potentially reduce symptom frequency.
Follow your doctor’s treatment plan: This may include medications, therapies, or other interventions to manage symptoms.
Don’ts:
- Don’t consume excessive salt: Avoid processed foods, fast food, and salty snacks.
- Avoid smoking: Smoking can worsen Meniere’s symptoms and should be avoided.
- Don’t consume excessive caffeine or alcohol: These substances can dehydrate the body and worsen symptoms.
- Avoid skip meals: Eating regular meals helps maintain stable blood sugar levels and can prevent triggering episodes.
- Don’t ignore your symptoms: If you experience a sudden worsening of symptoms, seek medical attention promptly.
Important Note:
This information is not intended as a substitute for professional medical advice. Always consult with a healthcare provider for proper diagnosis and treatment of Meniere’s disease.
Terminology
Terminology
Meniere’s disease is a complex condition with a unique set of terminology. Understanding these terms is crucial to comprehending the disease and its management. Here are some key terms and their meanings:
Vertigo: A spinning sensation or a feeling that you or your surroundings are moving. This is a hallmark symptom of Meniere’s disease and can be quite debilitating.
Tinnitus: Ringing, buzzing, hissing, roaring, or other sounds in the ears or head. This is another common symptom of Meniere’s and can vary in intensity and frequency.
Sensorineural hearing loss: Hearing loss caused by damage to the inner ear (cochlea) or the nerve pathways from the inner ear to the brain. Meniere’s disease often leads to fluctuating sensorineural hearing loss.
Aural fullness: A feeling of pressure or fullness in the ear, often described as if the ear is plugged. This is a common symptom during Meniere’s attacks.
Endolymphatic hydrops: An abnormal increase in the volume of endolymph fluid within the inner ear. This is believed to be a key factor in the development of Meniere’s disease.
Vestibular system: The part of the inner ear responsible for balance and spatial orientation. Meniere’s disease affects the vestibular system, leading to vertigo and balance problems.
Cochlea: The spiral-shaped cavity in the inner ear that houses the organ of hearing. Damage to the cochlea contributes to hearing loss in Meniere’s disease.
Meniere’s attack: An episode of vertigo, tinnitus, hearing loss, and aural fullness that can last from minutes to hours. Attacks can occur sporadically and vary in frequency and severity.
Diuretics: Medications that increase urine production, helping to reduce fluid retention in the body. Diuretics are sometimes used to manage Meniere’s symptoms.
Vestibular rehabilitation therapy (VRT): A type of physical therapy that helps improve balance and reduce dizziness. VRT is often recommended for people with Meniere’s disease.
Ablative therapy: Procedures that destroy the vestibular nerve or inner ear structures to eliminate vertigo. These are considered for severe cases when other treatments have failed.
References
References use for Article Meniere’s Disease
- Disease of Ear, Nose and Throat & Head and Neck surgery 6th edition
- Mohan Bansal – Diseases of Ear, Nose & Throat
- Maqbool – textbook of Ear, Nose & Throat disease; 11th edition
- https://www.drhomeo.com/menieres/menieres-disease-wonderful-homeopathic-remedies-for-its-treatment/
- https://dizziness-and balance.com/disorders/menieres/hydrops.html
- Bhattacharya, S., Gharat, S., & Merchant, S. N. (2021). Incidence of Meniere disease in a tertiary healthcare center in Mumbai. Indian Journal of Otolaryngology and Head & Neck Surgery, 73(3), 326-330.
- Meniere’s Disease : What you need to know, 1st Edition, P. J. Haybach, Jerry Underwood, August 27, 1998, Vestibular Disorders Assn.
- Disease of Ear, Nose and Throat by PL Dhingra, 26th edition, published by Elsevier in 2015.
- Cummings Otolaryngology – Head and Neck Surgery, 7th Edition, Paul W. Flint, Bruce H. Haughey, Valerie J. Lund, John K. Niparko, Mark A. Richardson, K. Thomas Robbins, J. Regan Thomas, 2021, Elsevier.
- Dizziness: A Practical Approach to Diagnosis and Management, by Michael Strupp, Marianne Dieterich, Thomas Brandt (5th Edition, 2021, Springer)
- Meniere Disease, 2nd Edition, Lloyd B. Minor, C. Gary Jackson, John P. Carey, 2021, Thieme.
- Meniere’s Disease,Various contributors, Brian J. McKinnon, Richard A. Chole’ 2nd Edition, 2016, Plural Publishing 978-1597565804
Meniere’s Disease: Nonsurgical Treatment (Chapter in the book "Meniere’s Disease"), Yetkin Zeki Yilmaz, Begum Bahar Yilmaz, and Aysegul Batioglu-Karaaltin, 2nd edition (published 2023).
Also Search As
Meniere’s Disease Also Search As
Online Search Engines:
- Use specific keywords: Search using terms like "homeopathy Meniere’s disease," "homeopathic treatment Meniere’s," or "homeopathic remedies Meniere’s."
- Specify article type: Include terms like "article," "research," or "case study" to filter results.
- Use academic databases: Explore resources like Google Scholar or PubMed for scholarly articles.
Homeopathic Websites and Journals:
- Visit websites of reputable homeopathic organizations: Many organizations publish articles and research on homeopathy.
- Browse online homeopathic journals: Look for journals specializing in homeopathy or complementary and alternative medicine.
Homeopathic Libraries and Resource Centers:
- Check local or university libraries: They may have collections of homeopathic books and journals.
- Visit homeopathic resource centers: Some cities have centers dedicated to homeopathic information and resources.
Consult a Homeopathic Practitioner:
- Ask for recommendations: Homeopathic practitioners often have access to resources and can suggest relevant articles.
Specific Resources:
- Dr. Care Homeopathy: Offers information on homeopathic treatment for Meniere’s disease: https://drcarehomeopathy.com/treatments/menieres-disease/
- International Journal of AYUSH Case Reports: Published a case series on homeopathic treatment for Meniere’s disease: https://ijacare.in/index.php/ijacare/article/view/148
Frequently Asked Questions (FAQ)
What is Meniere’s Disease?
Definition
Meniere’s disease, also called endolymphatic hydrops, is a disorder of the inner ear where the endolymphatic system is distended with endolymph.
What causes Meniere’s Disease?
- Viral
- Hereditary
- Autoimmune
- Defective absorption by endolymphatic sac
- Vasomotor disturbance
- Anoxia of capillaries of stria vascularis
- Allergy
How is Meniere's disease diagnosed?
Diagnosis involves:
- A detailed medical history
- Physical examination
- Hearing tests
- Balance tests
- Sometimes, imaging tests like MRI
Can Meniere's disease be prevented?
The exact cause of Meniere’s disease is unknown, so prevention is not always possible.However, managing stress, maintaining a healthy lifestyle, and avoiding triggers like caffeine and alcohol may help reduce the frequency and severity of episodes.
What are the symptoms of Meniere’s Disease?
Can homeopathy cure Meniere's disease?
While homeopathy aims to address the root cause and promote healing, it’s important to maintain realistic expectations and acknowledge that the potential for a complete cure can vary from person to person.
Can homeopathy help with Meniere's disease?
Homeopathy is a complementary and alternative medicine (CAM) system that some people find helpful in managing Meniere’s disease symptoms. It focuses on treating the individual as a whole, considering physical, mental, and emotional factors.
Is homeopathic treatment for Meniere's disease safe?
Homeopathic remedies are generally considered safe when prescribed and administered by a qualified practitioner. However, it’s important to consult with your doctor to ensure it complements your existing treatment plan.
What are the treatment options for Meniere's disease?
- Lifestyle changes (low-sodium diet, stress management)
- Medications (diuretics, anti-nausea drugs)
- Physical therapy (vestibular rehabilitation)
- Injections (steroids, gentamicin)
- Surgery (for severe cases)
Homeopathic Medicines used by Homeopathic Doctors in treatment of Meniere’s Disease?
Homoeopathic Medicines for Menier’s Disease
- Chininum Sulph
- Conium Maculatum
- Gelsemium
- Chenopodium
- Salicylicum Acid
- Theridion
