Migraine
Definition
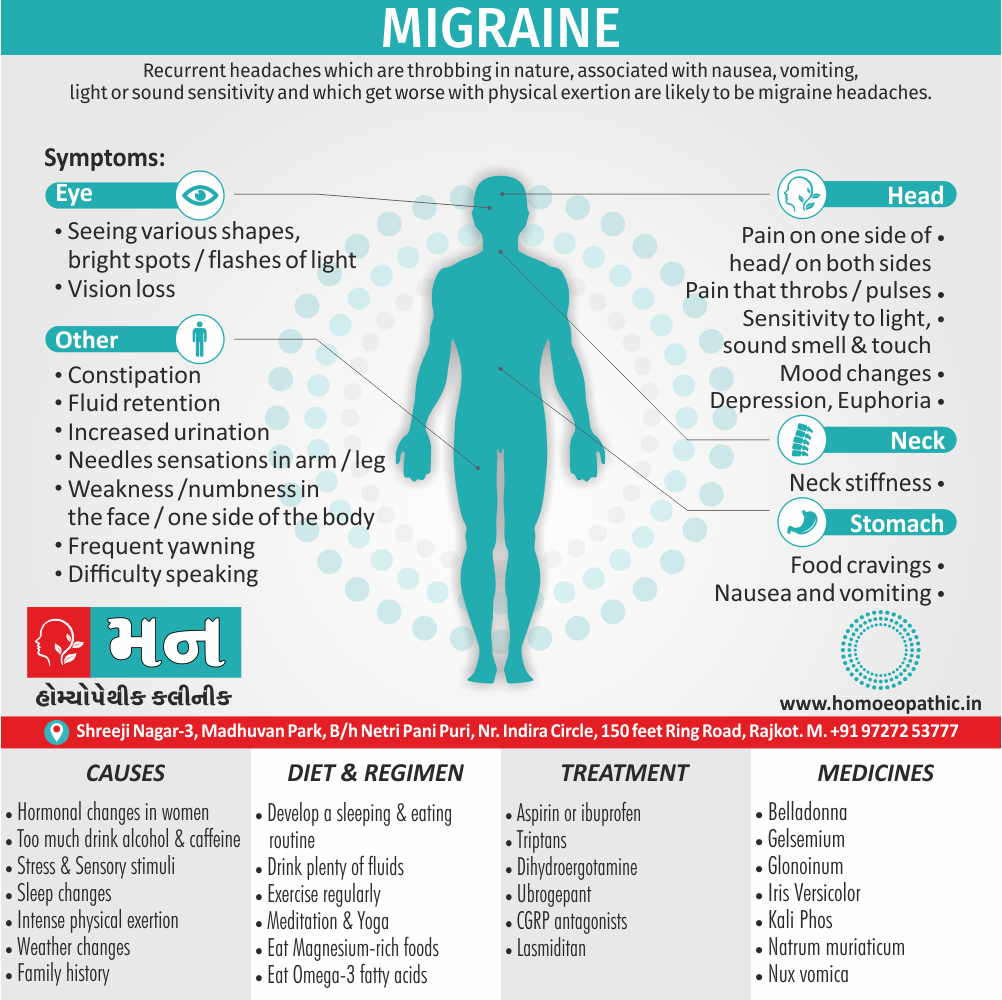
Recurrent headaches which are throbbing in nature, associated with nausea, vomiting, light or sound sensitivity and which get worse with physical exertion are likely to be migraine headaches. Focal neurological symptoms, particularly visual symptoms, are characteristic.[1]
There are a few synonyms for migraine, depending on the nuance you want to convey:
Formal:
- Cephalalgia (medical term for headache)
Informal:
- Megrim (especially in British English)
- Sick headache
General:
- Headache (broader term, doesn’t specify severity)
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview:
It is a headache that can cause severe throbbing pain or a pulsing sensation, usually on one side of the head. It’s often accompanied by nausea, vomiting, and extreme sensitivity to light and sound. Its attacks can last for hours to days, and the pain can be so severe that it interferes with your daily activities.
For some people, a warning symptom known as an aura occurs before or with the headache. An aura can include visual disturbances, such as flashes of light or blind spots, or other disturbances, such as tingling on one side of the face or in an arm or leg and difficulty speaking.
Medications can help prevent some migraines and make them less painful. The right medicines, combined with self-help remedies and lifestyle changes, might help. [3]
Epidemiology
Epidemiology
The epidemiology of migraine in India varies across regions and studies. Here are some key findings from recent publications:
- Prevalence, burden, and risk factors of migraine: A community-based study from Eastern India (2017): This study found a one-year prevalence of migraine of 14.12% in Eastern India, with education, environmental exposure, travel, and oral contraceptives identified as risk factors. The burden was highest among women aged 30-34 years. [3]
- The burden attributable to headache disorders in India: estimates from a community-based study in Karnataka State (2015): This study reported a one-year migraine prevalence of 25.2% in Karnataka, with a high symptom burden and significant loss of productive time due to migraine. [4]
- Neuroepidemiology study of headache in the region of Jammu of north Indian population: A cross-sectional study (2022): This study reviewed existing research on headache prevalence in different regions of India, noting a wide range in reported prevalence. It also highlighted a consistent finding of female preponderance in migraine prevalence across studies. [5]
These studies, along with others, indicate that migraine is a significant public health issue in India, with varying prevalence rates across regions. Further research is needed to better understand the factors contributing to these variations and to develop targeted interventions for prevention and treatment.
Causes
Causes and Triggers:
Though migraine causes aren’t fully understanding, genetics and environmental factors appear to play a role.
Changes in the brainstem and its interactions with the trigeminal nerve, a major pain pathway, might involve.
So, might imbalances in brain chemicals — including serotonin, which helps regulate pain in your nervous system.
Researchers are studying the role of serotonin in migraines. Other neurotransmitters play a role in the pain of migraine, including calcitonin gene-related peptide (CGRP).
Migraine triggers: – There are a number of migraine triggers, including:
- Hormonal changes in women- Fluctuations in oestrogens, such as before or during menstrual periods, pregnancy and menopause, seem to trigger headaches in many women.
- Drinks–These include alcohol, especially wine, and too much caffeine, such as coffee.
- Stress-Stress at work or home can cause migraines.
- Sensory stimuli–Bright or flashing lights can induce migraines, as can loud sounds. Strong smells — such as perfume, paint thinner, second-hand smoke trigger migraines in some people.
- Sleep changes- Missing sleep or getting too much sleep can trigger migraines in some people.
- Physical factors-Intense physical exertion, including sexual activity, might provoke migraines.
- Weather changes– A change of weather or barometric pressure can prompt a migraine.
- Medications- Oral contraceptives and vasodilators, such as nitro-glycerine, can aggravate migraines.
- Foods- Aged cheeses and salty and processed foods might trigger migraines. [3]
Types
TYPES:
With aura or classic migraine i.e.:
- Here the episode begins with prominent neurologic symptoms (auras) such as visual disturbances like dazzling zig-zag lines, homonymous hemianopia, field defects or rarely total blindness, sensory disturbances affecting one-half of the body, disturbances of speech or hemiparesis.
- These neurologic symptoms last for 15-30 minutes and generalized throbbing headache with nausea and vomiting, all of which may last even for 1 to 2 days. [4]
Migraine without aura or common migraine i.e.:
- There is onset of headache, nausea and vomiting following the same sequence.
- Migraine has differentiated from other organic disorders such as raised intracranial tension, subarachnoid haemorrhage and arteriovenous malformations.[4]
Without head pain i.e.:
- “Silent migraine” or “acephalgic migraine,” as this type also known as, includes the aura symptom but not the headache that typically follows.
Hemiplegic migraine i.e.:
- You’ll have temporary paralysis (hemiplegia) or sensory changes on one side of your body.
- The onset of the headache may associate with temporary numbness, extreme weakness on one side of your body, a tingling sensation, a loss of sensation and dizziness or vision changes.
Retinal migraine (occular migraine) i.e.:
- You may notice temporary, partial or complete loss of vision in one of your eyes, along with a dull ache behind the eye that may spread to the rest of your head.
- That vision loss may last a minute, or as long as months.
Chronic migraine i.e.:
Migraine with brainstem aura i.e.:
- With this migraine, you’ll have vertigo, slurred speech, double vision or loss of balance, which occur before the headache.
- The head pain may affect the back of your head.
- These symptoms usually occur suddenly and can be associated with the inability to speak properly, ringing in ears and vomiting.
Status migraneous:
- This is a rare and severe type of migraine that can last longer than 72 hours.
- The headache and nausea can be extremely bad. [5]
Risk Factors
Risk Factors :
- Family history- If you have a family member with migraines, then you have a chance of developing them too.
- Age-Migraines c
- an begin at any age, though the first often occurs during adolescence. Migraines tend to peak during your 30s, and gradually become less severe and less frequent in the following decades.
- Sex-Women are three times more likely than men to have migraines.[3]
Pathogenesis
Pathogenesis of Migraine
The pathogenesis of migraine is a complex and evolving field, with several contributing factors.
Pathogenesis Overview (Key Points):
- Cortical Spreading Depression (CSD): CSD is considered a key trigger for migraine aura and potentially the headache phase in some patients. It involves a wave of neuronal and glial depolarization that spreads across the cortex, leading to changes in blood flow and neurotransmitter release.
- Trigeminovascular Activation: The trigeminal nerve, which innervates the meninges and blood vessels, plays a crucial role in migraine pain. Activation of this system leads to the release of inflammatory mediators, including calcitonin gene-related peptide (CGRP), which contribute to pain and vasodilation.
- Genetics: Migraine has a strong genetic component, with multiple genes identified that contribute to susceptibility. These genes are involved in various pathways, including ion channel function, neurotransmitter signaling, and vascular regulation.
- Other Factors: Several other factors can contribute to migraine pathogenesis, including hormonal fluctuations, stress, sleep disturbances, dietary triggers, and environmental factors. [6]
Pathophysiology
Pathophysiology of Migraine :
- Though the exact mechanism is unknown, it is the consensus that an attack of migraine consists of a neurovascular disorder of the intracranial as well as the extracranial vessels.
- Sequential studies of cerebral blood flow show an initial reduction which may localize or generalize followed by increase in blood flow (35-50%) later. The basic cause of this circulatory disturbance is not knew.
- It found that the blood levels of histamine, serotonin, and norepinephrine increase during the attacks. There is also increase in platelet aggregability.
- This may account for strokes which sometimes complicate migraine. The headache has attributed to excessive pulsation of extracranial arteries, and possibly intracranial ones also.[4]
Clinical Features
Clinical Features of Migraine
Headache:
- Typically unilateral (one-sided), but can be bilateral.
- Pulsating or throbbing quality.
- Moderate to severe intensity.
- Aggravated by routine physical activity.
- Lasts 4-72 hours (untreated or unsuccessfully treated).
Associated Symptoms:
- Nausea and/or vomiting.
- Photophobia (sensitivity to light) and phonophobia (sensitivity to sound).
- Osmophobia (sensitivity to smell) may also occur.
Aura:
- Present in about 25% of migraine patients.
- Most commonly visual disturbances (e.g., flashing lights, blind spots, zigzag lines).
- Can also include sensory symptoms (e.g., tingling, numbness) or language difficulties.
Prodrome and Postdrome:
- Prodrome: Warning symptoms that occur hours or days before the headache (e.g., mood changes, fatigue, yawning).
- Postdrome: "Migraine hangover" characterized by fatigue, difficulty concentrating, and mood changes after the headache subsides. [7]
Sign & Symptoms
Sign & Symptoms:
- It can progress through four stages: prodrome, aura, attack and post-drome.
- Not everyone who has migraines goes through all stages.
Prodrome: –
One or two days before a migraine, you might notice subtle changes that warn of an upcoming migraine, including:
- Constipation
- Mood changes, from depression to euphoria
- Food cravings
- Neck stiffness
- Increased urination
- Fluid retention
- Frequent yawning
Aura: –
For some people, an aura might occur before or during migraines. Auras are reversible symptoms of the nervous system.
Its auras include:
- Visual phenomena, such as seeing various shapes, bright spots or flashes of light
- Vision loss
- Pins and needles sensations in an arm or leg
- Weakness or numbness in the face or one side of the body
- Difficulty speaking
Attack: –
During a migraine, you might have:
- Pain usually on one side of your head, but often on both sides
- Pain that throbs or pulses
- Sensitivity to light, sound, and sometimes smell and touch
- Nausea and vomiting
Post-drome: –
After a its attack, you might feel drained, confused. Some people report feeling elated. Sudden head movement might bring on the pain again briefly.[7]
Clinical Examination
Clinical Examination of Migraine
There is no specific clinical examination for migraine as it is primarily a diagnosis of exclusion based on the patient’s history and ruling out other causes of headache. However, a thorough neurological examination is essential to exclude any underlying neurological conditions.
Key Components of a Neurological Examination for Migraine:
- History: A detailed history is the most crucial aspect of the assessment. The examiner should inquire about:
- Headache characteristics: onset, duration, frequency, location, quality, severity, and associated symptoms.
- Triggers: factors that worsen or precipitate the headache.
- Family history of migraine or other headache disorders.
- Previous treatments and their effectiveness.
- Comorbid conditions, medications, and allergies.
- General Examination: Assess for signs of systemic illness or infection, which could be contributing to the headache.
- Mental Status Examination: Evaluate for cognitive impairment, which could suggest an underlying neurological condition.
- Cranial Nerve Examination: Assess for cranial nerve deficits, particularly those related to vision (II, III, IV, VI) and facial sensation (V), as these could indicate a neurological cause of the headache.
- Motor and Sensory Examination: Assess for motor weakness, sensory loss, or coordination abnormalities, which could suggest a neurological lesion.
- Reflexes: Check deep tendon reflexes and plantar responses for any abnormalities. [8]
Diagnosis
Diagnosis:
If you have migraines or a family history of migraines, a doctor trained in treating headaches (neurologist) will likely diagnose it based on your medical history, symptoms, and a physical and neurological examination.
If your condition is unusual, complex or suddenly becomes severe, tests to rule out other causes for your pain might include:
- Magnetic resonance imaging (MRI)
- Computerized tomography (CT) [3]
Differential Diagnosis
Differential Diagnosis of Migraine
Primary Headache Disorders:
- Tension-type headache (TTH): The most common type of headache, usually bilateral, pressing or tightening quality, mild to moderate intensity.
- Cluster headache: Severe, unilateral headache with associated autonomic symptoms (e.g., tearing, nasal congestion, ptosis).
- Other trigeminal autonomic cephalalgias (TACs): Similar to cluster headache but with different patterns of attacks.
- Hemicrania continua: Continuous unilateral headache with fluctuations in intensity.
Secondary Headache Disorders:
- Medication overuse headache (MOH): Headache caused by frequent use of acute headache medications.
- Headache attributed to head and/or neck trauma: Headache following head or neck injury.
- Headache attributed to cranial or cervical vascular disorder: Headache caused by problems with blood vessels in the head or neck (e.g., stroke, dissection).
- The Headache attributed to non-vascular intracranial disorder: Headache caused by conditions affecting the brain (e.g., tumor, infection, hydrocephalus).
- Headache attributed to substance use or withdrawal: Headache triggered by substance use or withdrawal (e.g., caffeine, alcohol).
- Headache attributed to infection: Headache caused by infections (e.g., meningitis, sinusitis).
- The Headache attributed to homeostasis disturbance: Headache caused by conditions affecting the body’s internal balance (e.g., hypoglycemia, hypertension).
- Headache or facial pain attributed to disorder of cranium, neck, eyes, ears, nose, sinuses, teeth, mouth, or other facial or cranial structures: Headache caused by problems in these areas (e.g., sinusitis, temporomandibular joint disorder).
- Headache attributed to psychiatric disorder: Headache associated with psychiatric conditions (e.g., depression, anxiety). [7]
Complications
Complications
Chronic Migraine (CM):
- Defined as headache occurring on 15 or more days per month for more than 3 months, with features of migraine on at least 8 days per month.
- Associated with increased disability, reduced quality of life, and higher healthcare utilization.
Medication Overuse Headache (MOH):
- Caused by the frequent use of acute headache medications, leading to a rebound headache cycle.
- Requires withdrawal of the overused medication and preventive treatment.
Migrainous Infarction:
- Rare but serious complication where migraine aura is associated with ischemic stroke.
- Risk factors include prolonged aura, age over 45 years, smoking, and use of oral contraceptives.
Persistent Aura Without Infarction:
- Prolonged aura symptoms lasting more than 7 days without evidence of infarction on imaging.
Status Migrainosus:
- A severe and prolonged migraine attack lasting more than 72 hours.
- Often requires hospitalization and aggressive treatment.
Migraine-Triggered Seizures:
- Rarely, migraine attacks can trigger seizures, especially in individuals with a history of epilepsy.
Psychiatric Comorbidity:
- Migraine is associated with increased risk of depression, anxiety, and other psychiatric disorders.
Cognitive Dysfunction:
- Some studies suggest that migraine may be associated with subtle cognitive changes, but more research is needed. [7]
Investigations
Investigations of Migraine
Neuroimaging:
- MRI: The preferred modality for evaluating brain structure and identifying potential causes of secondary headaches (e.g., tumors, vascular malformations).
- CT: May be used if MRI is contraindicated or unavailable, but less sensitive for detecting subtle abnormalities.
Laboratory Tests:
- Blood Tests:
- Complete blood count (CBC): To rule out infection or anemia.
- Erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP): To assess for inflammation.
- Thyroid function tests: To rule out thyroid disorders.
- Lumbar Puncture: May be considered if there is suspicion of meningitis or other inflammatory conditions.
Other Investigations:
- Electroencephalogram (EEG): To rule out epilepsy in patients with aura or other paroxysmal symptoms.
- Visual Evoked Potentials (VEP): To assess visual pathway function in patients with visual aura.
- Neuropsychological Testing: To evaluate for cognitive impairment in patients with chronic migraine or suspected complications. [7]
Treatment
Treatment :
Medications used to relieve pain work best when taken at the first sign of an oncoming migraine — as soon as signs and symptoms of a migraine begin. Medications that can be used to treat it include:
Pain relievers:
- Pain relievers include aspirin or ibuprofen (Advil, Motrin IB, others).
Triptans:
- Prescription drugs such as sumatriptan (Imitrex, Tosymra) and rizatriptan (Maxalt, Maxalt-MLT) are used to treat migraine because they block pain pathways in the brain.
Dihydroergotamine (D.H.E. 45, Migranal):
- Available as a nasal spray or injection, this drug is most effective when taken shortly after the start of migraine symptoms for migraines that tend to last longer than 24 hours.
- People with coronary artery disease, high blood pressure, or kidney or liver disease should avoid dihydroergotamine.
Lasmiditan:
- This newer oral tablet is approved for the treatment of migraine with or without aura.
- Lasmiditan can have a sedative effect and cause dizziness, so people taking it are advised not to drive or operate machinery for at least eight hours.
Ubrogepant:
- This oral calcitonin gene-related peptide receptor antagonist is approved for the treatment of acute migraine with or without aura in adults
CGRP antagonists:
- Ubrogepant and Rimegepant are oral CGRP antagonists recently approved for the treatment of acute migraine with or without aura in adults.
- Drugs from this class were more effective than placebo in relieving pain and other related symptoms such as nausea and sensitivity to light and sound two hours after taking it.
Anti-nausea drugs:
Prevention
Prevention of Migraine
Lifestyle Modifications:
- Identify and avoid triggers: Keep a headache diary to track potential triggers (e.g., stress, certain foods, alcohol, sleep disturbances) and take steps to avoid them.
- Maintain regular sleep patterns: Aim for consistent sleep and wake times, even on weekends.
- Eat a healthy diet: Avoid processed foods, caffeine, and alcohol, and eat regular meals.
- Exercise regularly: Engage in moderate-intensity aerobic exercise most days of the week.
- Manage stress: Practice relaxation techniques (e.g., yoga, meditation, deep breathing exercises).
Pharmacological Interventions:
- Preventive Medications: These medications are taken daily to reduce the frequency and severity of migraine attacks. Commonly used options include:
- Beta-blockers (e.g., propranolol, metoprolol)
- Antiepileptic drugs (e.g., topiramate, divalproex sodium)
- Antidepressants (e.g., amitriptyline, venlafaxine)
- CGRP monoclonal antibodies (e.g., erenumab, fremanezumab)
- Choice of medication depends on individual patient factors, such as comorbidities, side effects, and response to previous treatments.
Non-pharmacological Therapies:
- Behavioral therapies:
- Cognitive-behavioral therapy (CBT): Helps identify and modify negative thought patterns and behaviors that contribute to migraine.
- Relaxation training: Techniques like progressive muscle relaxation and biofeedback can help reduce stress and muscle tension.
- Physical therapies:
- Massage therapy: May help reduce muscle tension and improve circulation.
- Acupuncture: May help reduce pain and improve quality of life in some patients. [6]
Homeopathic Treatment
Homeopathic Treatment :
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines select after a full individualizing examination and case-analysis.
which includes;
- the medical history of the patient,
- physical and mental constitution,
- family history, presenting symptoms,
- underlying pathology, possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often take into account for the treatment of chronic conditions.
What Homeopathic Doctors Do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus usually on what cause the disease condition? Why ‘this patient’ is sick ‘this way’?. The disease diagnosis is important but in homeopathy, the cause of disease is not just probing to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness are also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic.
Homeopathic Medicines
The correct homeopathy remedy tries to correct this disease predisposition. The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology is not very advance, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not directly relate to this disease because in homeopathy general symptoms and constitutional indications are also taking into account for selecting a remedy.
Homoeopathic medicine:
1. Belladonna –
- Belladonna is a helpful for migraine headaches with intense throbbing, pulsating headaches.
- It is also indicated when there is an extreme fullness in the head. Light seems to worsen the headache.
- Noise is unbearable. Some cases have, exposure to cold air can trigger a its episode.
- In others, a head bath with cold water can bring on migraine headaches.
- Belladonna has sensation of fullness with a throbbing headache.
- It is also used for headaches resulting from high blood pressure.
2. Glonoinum –
- Glonoinum is helpful in treating migraine with excessive congestion in the head.
- The head feels very large, as if it would burst. In such a migraine attack, patients in pain are seen holding their head in hands.
- The eyeballs seem protruded.
- Extreme heaviness in the head is felt. Also, heat around the head is unbearable. Uncovering the head relieves the headache.
- The migraine gets better with sleep while walking worsens the migraine headache.
- Glonoinum most suitable medicine for migraine headache triggered by sun exposure.
3. Iris Versicolor –
- Iris Versicolor is a medicine for migraine when attending with intense nausea, vomiting or acidity.
- Burning may note in any part of the alimentary canal.
- Vomiting of acidic, sour, bitter nature is observed.
- Bitter, acrid, belching with intense burning behind the sternum and in the throat is well marked.
- Acidic stomach reflux leads to headaches.
- Headache with diarrhoea.
- It is also useful where migraine begins with a blur before the eyes.
4. Epiphegus –
- Epiphegus is a medicine for migraine where exhaustion – mental or physical.
- It is used where the slightest deviation from routine work brings on a migraine attack.
- Although it works for both sided migraine, yet comparatively better results are seen in left-sided headaches with Epiphegus.
- A peculiar attending symptom increase saliva with constant inclination to spit.
5. Kali Phos –
- In case of a migraine attack triggered by stress, Kali Phos proves extremely useful.
- The unique indication for use of Kali Phos is that stress, tensions and worry lead to migraine headaches.
- Migraine headaches are common among students who suffer school or college related stress.
- Exhaustion and weakness usually accompany the migraine.
6. Natrum Muriaticum –
- Natrum Muriaticum is the best prescription for migraine attacks that worsen around the menstrual cycle.
- The headache may be triggered before, during or at the close of the menstrual cycle.
- Migraine headache that starts with sunrise, continues through the day and vanishes after sunset. This is popularly known as the “sunrise to sunset headache”.
- Migraine headache feels like little hammers knocking on the brain, Natrum Muriaticum will help.
- It is also the most suitable prescription for migraine headaches in school girls or in girls who are anaemic.
- Natrum mur is also a very effective medicine for headache caused by eye strain.
7. Nux Vomica –
- Nux Vomica is a very effective remedy for migraine with gastric troubles.
- Migraine due to indigestion, flatulence, constipation also piles.
- Nux Vomica also helps where migraine headaches get worse after taking coffee, spicy food also alcoholic drinks.
- The headache may be located in any part of the head.
- The person specifically feels the need to press the head against something hard for relief.
8. Gelsemium –
- It works well when dim sight occurs with a headache. In some cases, temporary blindness precedes onset of headache.
- Moreover, In most cases the pain is felt in the back of the head.
- With this a sensation of band around the head may be present.
- Besides this, Heaviness of eyelids can also there. is also made when
- Headache worsens especially, from mental exertion. Pressure may give relief in pain when it need.
9. Spigelia –
- Generally, Spigelia is a most effective medicine for left-sided migraine.
- It indicate when the headache is locating over the left temporal region, forehead and eyes.
- In most cases, the pain begins in the occipital region of the head, extends upward and settles over the left eye.
- The pain is violent, throbbing and pulsating in nature. In detail, There is a sensation of a tight band around the head.
- Stooping seems to worsen the headache. All in all, Severe pain in the eyeballs may attend. Eye movement worsens this pain.
10. Sanguinaria Canadensis –
- Sanguinaria Canadensis is a good medicine for right-sided migraine.
- The pain starts from the back of the head i.e. occiput, ascends and settles over the right eye. Lying down quietly in a dark room brings relief.
- In some cases, sleep may relieve pain.
- Fasting often triggers a migraine headache in persons prescribed Sanguinaria Canadensis.
- It is also the medicine to prescribe when the headache starts in the morning, increases during the day and lasts until sunset.
- Sanguinaria Canadensis is a significant for migraine in women during menopause.
Diet & Regimen
Diet & regimen :
- Develop a sleeping and eating routine: – Don’t sleep too much or too little. Set and follow a consistent sleep and wake schedule daily. Try to eat meals at the same time every day.
- Drink plenty of fluids: – Staying hydrated, particularly with water, might help.
- Exercise regularly: – Regular aerobic exercise such as walking, swimming and cycling, Warm up slowly reduce tension and can help to prevent it.
- Meditation and yoga: – Meditation may relieve stress, which is a known trigger of migraines. Done on a regular basis, yoga may reduce the frequency and duration of migraines.[3]
- Magnesium-rich foods: – Foods rich in magnesium include dark leafy greens, avocado, and tuna.
- Omega-3 fatty acids: – Research indicates that increasing omega-3 fatty acid may help people with migraine. Food rich in omega-3 fatty acid include fish such as mackerel and salmon, and seeds and legumes. [7]
Do’s and Don'ts
Do’s:
- Maintain a headache diary: Track headache frequency, duration, intensity, and associated symptoms. Note potential triggers (foods, stress, sleep changes, hormonal fluctuations) to identify patterns and avoid them.
- Follow a consistent sleep schedule: Go to bed and wake up at the same time each day, even on weekends.
- Eat regular meals: Don’t skip meals, as fluctuating blood sugar levels can trigger migraines.
- Stay hydrated: Drink plenty of water throughout the day, as dehydration can be a trigger.
- Manage stress: Practice relaxation techniques like yoga, meditation, or deep breathing exercises.
- Exercise regularly: Moderate-intensity aerobic exercise can help reduce migraine frequency.
- Identify and avoid triggers: Common triggers include certain foods (aged cheese, processed meats, red wine), caffeine, alcohol, bright lights, loud noises, and strong smells.
- Seek medical help: If you experience frequent or severe migraines, consult a doctor to discuss treatment options.
- Take medications as prescribed: If you are prescribed preventive or acute medications, take them as directed by your doctor.
- Rest in a dark, quiet room: When a migraine strikes, rest in a dark, quiet room with a cool compress on your forehead or neck.
Don’ts:
- Overuse pain medication: Overusing pain relievers can lead to rebound headaches. Limit the use of over-the-counter pain medications to no more than 2-3 days per week.
- Skip meals or go long periods without eating: This can lead to low blood sugar levels, which can trigger migraines.
- Consume excessive caffeine or alcohol: These can dehydrate you and trigger migraines.
- Ignore your body’s signals: Pay attention to warning signs of an impending migraine and take steps to manage it before it becomes severe.
- Self-treat chronic or severe migraines: If you experience frequent or severe migraines, seek professional help for proper diagnosis and treatment.
- Expose yourself to known triggers: If you know certain factors trigger your migraines, avoid them as much as possible.
Terminology
Terminology
Migraine:
- A neurological condition characterized by recurrent episodes of moderate to severe headache, often accompanied by nausea, vomiting, and sensitivity to light and sound.
Aura:
- A sensory disturbance that precedes or accompanies a migraine attack, often involving visual, sensory, or speech disturbances.
Prodrome:
- Early symptoms that occur hours or days before a migraine attack, such as fatigue, mood changes, or food cravings.
Postdrome:
- Symptoms that persist after a migraine attack, such as fatigue, difficulty concentrating, or mood changes.
Trigeminovascular system:
- A network of nerves and blood vessels in the head and neck that plays a key role in migraine pain.
Cortical spreading depression (CSD):
- A wave of neuronal and glial depolarization that spreads across the cerebral cortex and is thought to be involved in migraine aura.
Calcitonin gene-related peptide (CGRP):
- A neuropeptide involved in pain transmission and vasodilation, and a key target for migraine therapy.
Triptans:
- A class of medications that act on serotonin receptors and are used to treat acute migraine attacks.
Preventive medications:
- Medications taken regularly to reduce the frequency and severity of migraine attacks.
Trigger:
- A factor that can provoke a migraine attack, such as stress, certain foods, or hormonal changes.
Terminologies related to Homoeopathy:
Constitutional Remedy:
- A remedy chosen based on the individual’s overall physical and mental characteristics, aimed at addressing the underlying cause of the disease.
Acute Remedy:
- A remedy used for immediate relief of migraine symptoms during an attack.
Prophylaxis:
- The use of homeopathic remedies to prevent future migraine attacks.
Aggravation:
- A temporary worsening of symptoms after taking a remedy, often seen as a positive sign of healing.
Amelioration:
- Improvement of symptoms after taking a remedy.
Potency:
- The strength or dilution of a homeopathic remedy.
Common Homeopathic Remedies for Migraine:
Belladonna:
- For throbbing, pulsating headaches with heat and redness of the face, sensitivity to light and noise, and dilated pupils.
Bryonia:
- For migraines worsened by movement and relieved by pressure, with a bursting or splitting sensation in the head.
Gelsemium:
- For migraines with dizziness, weakness, blurred vision, and a heavy feeling in the head, often triggered by stress or anticipation.
Glonoinum:
- For congestive headaches with a feeling of fullness and throbbing, often triggered by heat or sun exposure.
Ignatia:
- For migraines associated with emotional stress, grief, or disappointment, often with a feeling of a lump in the throat.
Iris versicolor:
- For migraines with nausea, vomiting, and blurred vision, often accompanied by digestive disturbances.
Natrum muriaticum:
- For migraines triggered by emotional stress or suppressed emotions, with a preference for solitude and aversion to consolation.
Nux vomica:
- For migraines caused by overindulgence in food or alcohol, with irritability, nausea, and vomiting.
Sanguinaria canadensis:
- For right-sided migraines that start at the back of the head and move towards the right eye, often worse in the morning and from light.
Spigelia:
- For left-sided migraines with sharp, stabbing pain around the eye and temple, often worse from movement and noise.
References
References
- Davidson’s foundations of clinical practice (2009)
- Harrison’s Manual of Medicine: Nineteenth Edition
Prevalence, burden, and risk factors of migraine: A community-based study from Eastern India (2017): Ray BK, Das SK, Pal S, Banerjee M. Prevalence, burden, and risk factors of migraine: A community-based study from Eastern India. J Family Med Prim Care. 2017 Jan-Mar;6(1):95-99. doi: 10.4103/2249-4863.224910. PMID: 29560012; PMCID: PMC5810835.
The burden attributable to headache disorders in India: estimates from a community-based study in Karnataka State (2015): Kulkarni GB, Rao GN, Gururaj G, Taly AB, Shamanna BR, Ashtekar MD. The burden attributable to headache disorders in India: estimates from a community-based study in Karnataka State. J Headache Pain. 2015 Oct 16;16:87. doi: 10.1186/s10194-015-0574-9. PMID: 26472095; PMCID: PMC4608454.
- Neuroepidemiology study of headache in the region of Jammu of north Indian population: A cross-sectional study (2022): Bhat RA, Sofi FA, Wani ZA, Wani MA, Mir SA, Bashir H. Neuroepidemiology study of headache in the region of Jammu of north Indian population: A cross-sectional study. Front Neurol. 2022 Oct 13;13:1030940. doi: 10.3389/fneur.2022.1030940. PMID: 36321392; PMCID: PMC9599415.
- Headache and Face Pain: A Multidisciplinary Approach (Second Edition) by Werner J. Becker, Peter J. Goadsby, and Stephen D. Silberstein (2021) Cambridge University Press
- The Headaches (4th Edition) by Jes Olesen, Peter J. Goadsby, Hans-Christoph Diener, Paul R. Martin, Michael A. Moskowitz (2018, Oxford University Press)
- Neurological Examination Made Easy (5th Edition) Geraint Fuller (2017, Churchill Livingstone)
Also Search As
Also Search As
People can search for homeopathic articles on migraines using various online resources and platforms:
1. Online Databases and Libraries:
- Homeopathic Educational Services (HES): HES is a renowned resource for homeopathic literature, offering access to books, journals, and articles on various topics, including migraines.
- National Center for Homeopathy (NCH): The NCH website features a library section with articles, research papers, and publications related to homeopathy, including migraine research.
- Pubmed: While not exclusively for homeopathy, Pubmed is a vast database of medical literature that may include some homeopathic studies and articles on migraines.
2. Homeopathic Websites and Organizations:
- The American Institute of Homeopathy (AIH): The AIH website provides resources, including articles and research updates, on homeopathy, which may include information on migraine treatment.
- Council for Homeopathic Certification (CHC): The CHC website offers resources and educational materials on homeopathy, which may include articles on migraine.
- Homeopathic websites and blogs: Many websites and blogs are dedicated to homeopathy, offering articles, case studies, and information on using homeopathic remedies for migraines.
3. Search Engines:
- Google Scholar: This search engine specializes in academic literature and may provide access to research papers and articles on homeopathic treatment for migraines.
- Google: Using specific keywords like "homeopathic treatment for migraine," "homeopathic remedies for migraine," or "homeopathic research on migraine" can lead to relevant articles and resources.
4. Social Media Groups and Forums:
- Facebook groups: There are numerous Facebook groups dedicated to homeopathy, where members share information, articles, and experiences with homeopathic treatment for migraines.
- Online forums: Various online forums discuss homeopathy, where users can ask questions and find information on homeopathic remedies for migraines.
There are several ways to search for information about migraines, depending on your needs and preferences:
Online Search Engines:
- General search engines: Use search engines like Google, Bing, or DuckDuckGo to search for broad terms like "migraine," "migraine symptoms," or "migraine treatment." You’ll find a wide range of results, including articles, websites, and personal blogs.
- Medical websites: Reputable websites like Mayo Clinic, WebMD, and the American Migraine Foundation offer comprehensive information on migraines, including causes, symptoms, diagnosis, and treatment options.
- Academic search engines: Google Scholar can be used to find scientific articles and research papers on migraines.
Online Forums and Support Groups:
- Online communities dedicated to migraines can provide valuable insights and support from people who are also dealing with the condition.
- You can ask questions, share experiences, and learn from others who have similar struggles.
Libraries and Bookstores:
- Libraries often have a selection of books and resources on migraines.
- Bookstores may carry books on migraine prevention, management, and coping strategies.
Health Professionals:
- Your doctor or a neurologist specializing in migraines is the best source of personalized information and advice.
- They can provide accurate diagnosis, recommend treatment options, and answer any questions you may have.
Mobile Apps:
- There are several mobile apps designed to help track migraine triggers, symptoms, and medications.
Frequently Asked Questions (FAQ)
What is Migraine?
What causes Migraine?
Causes:
- Hormonal changes in women
- Drinks
- Stress
- Sensory stimuli
- Sleep changes
- Physical factors
- Weather changes
- Medications- Oral contraceptives
- Foods
Give the types of Migraine?
What triggers a migraine?
Migraine triggers differ for each person, but common ones include stress, hormonal changes, certain foods (e.g., aged cheese, chocolate), alcohol, lack of sleep, and weather changes.
What are the symptoms of Migraine?
Symptoms
- Visual phenomena
- Vision loss
- Pins and needles sensations in an arm or leg
- Weakness or numbness
- Difficulty speaking
- Pain usually on one side of your head
- Pain that throbs or pulses
- Sensitivity to light, sound, smell and touch
- Nausea and vomiting
Can homeopathy help with migraines?
Yes,
Many people find relief from migraines using homeopathic remedies. Homeopathy aims to stimulate the body’s natural healing abilities to address the underlying causes of migraines.
Are there natural remedies for migraines?
Some people find relief from migraines using natural remedies like applying cold compresses, resting in a dark room, practicing relaxation techniques, and using herbal supplements (e.g., butterbur, feverfew).
Can homeopathy prevent migraines from occurring?
Yes,
Homeopathic treatment aims to address the underlying causes of migraines, which can lead to a reduction in the frequency and intensity of attacks over time.
How long does it take to see results from homeopathic migraine treatment?
The response time varies depending on the individual and the severity of the condition. Some people may experience relief quickly, while others may require longer-term treatment.
How does homeopathic treatment for migraines differ from conventional approaches?
Homeopathy takes a holistic approach, considering your overall health and individual characteristics to select a personalized remedy. Conventional treatments often focus on symptom suppression.
