
Musculoskeletal Pain
Definition
Musculoskeletal pain is the pain that affects the muscles, ligaments also tendons, bones and nerves.
There are a few ways to describe musculoskeletal pain depending on the context:
- General terms: These are broad descriptions of the discomfort:
- Myalgia: Pain in the muscles
- Arthralgia: Pain in the joints
- Aches and pains
- Discomfort
- Stiffness
- Cause-specific terms: These terms imply the cause of the pain:
- Repetitive motion injury (RMI): Pain caused by repeated movements
- Overuse injury: Similar to RMI, but emphasizes overuse
- Work-related musculoskeletal disorder (WMSD): Pain linked to work activities
- Other terms: These describe specific sensations:
- Tenderness: A localized area of pain to touch
- Soreness: A dull, aching pain
The best term depends on how much detail you want to convey. For a general conversation, "aches and pains" might suffice. For a more specific discussion, "myalgia" or "RMI" could be better.
Overview
Types
Generalised Musculoskeletal Pain
Neck Pain
Elbow Pain
Hand and Wrist Pain
Ankle and Foot Pain
Sign & Symptoms
Homeopathic Treatment
Exercise Guidance
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
In general, It can be acute (having a rapid onset with severe symptoms) or chronic (especially long-lasting).
Musculoskeletal pain can be localized either in one area, or widespread.
Lower back pain is the most common type of musculoskeletal pain.
Other common types include tendonitis, myalgia (in other words, muscle pain), and stress fractures. [2]
Types
Types of Musculoskeletal Pain
There are two types of musculoskeletal pain i.e.;
- Generalized Musculoskeletal Pain
- Regional Musculoskeletal Pain
The Regional musculoskeletal pain is a common presenting complaint, usually occurring as the result of age related degenerative disease of tendons and ligaments, OA also repetitive strain injuries due to overuse.
Regional Musculoskeletal Pain include:
- Back pain
- Cervical (Neck) pain
- Shoulder pain
- Elbow pain
- Hand & Wrist pain
- Hip pain
- Knee pain
- Ankle & Foot pain [1]
Generalised Musculoskeletal Pain
Generalised Musculoskeletal Pain
Basically, Relentlessly progressive pain occurring in association with weight loss suggests malignant disease with bone metastases.
Furthermore, Generalised bone pain may also occur in Paget’s disease if the disease is widespread, but Pagetic pain is usually more focal and localised to the site of involvement.
In detail, Widespread pain can occur in OA but this also tends to be localised to sites of involvement, such as the lumbar spine, hips, knees and hands.
Signs of OA may be apparent on clinical examination.
Osteomalacia can cause generalised bone pain that is associated with bone tenderness also limb girdle weakness.
Besides this, Fibromyalgia can present with generalised pain particularly affecting the trunk, back also neck.
Accompanying features include fatigue, poor concentration also focal areas of hyperalgesia.
All in all, Another potential cause is joint hypermobility, the features of which should be apparent on clinical examination.
Causes of generalised pain i.e.:
- Metastatic bone disease
- Fibromyalgia
- Joint hypermobility
- Osteomalacia
- Osteoarthritis
- Paget’s disease
- Polymyalgia rheumatica
- Myositis
Diagnosis:
- Radionuclide bone scanning is of value in patients suspected of having bone metastases and Paget’s disease, along with further imaging as appropriate.
- Myeloma should be excluded by plasma also urinary protein electrophoresis.
- If these results are positive, a radiological skeletal survey should be performed, since the isotope bone scan may be normal in myeloma.
- Routine biochemistry, vitamin D levels and PTH measurement should be performed if osteomalacia is suspected.
- In Paget’s disease, ALP may be elevated but can be normal in localised disease.
- Lastly, Laboratory investigations are normal in patients with fibromyalgia and benign hypermobility.
Management:
- Management should be directed towards the underlying cause.
- Chronic pain of unknown cause also that associated with fibromyalgia responds poorly to analgesics and NSAID, but may respond partially to antineuropathic agents such as amitriptyline, duloxetine, gabapentin and pregabalin. [1]
Neck Pain
Neck Pain
It is a common symptom that can occur following injury (for example, whiplash), after falling asleep in an awkward position, as a result of stress, or in association with OA of the spine.
Most cases resolve spontaneously or with a short course of NSAID or analgesics, and a soft collar.
Patients with persistent pain that follows a nerve root distribution and those with neurological signs and symptoms should be investigated by MRI scan, and if necessary referred for a neurosurgical opinion.
Causes of neck pain:
Mechanical i.e.:
- Postural
- Whiplash injury
- Disc prolapse
- Cervical spondylosis
Inflammatory i.e.:
- Infections
- Spondylitis
- Juvenile idiopathic arthritis
- RA
- Polymyalgia rheumatica
Metabolic i.e.
- Osteoporosis
- Osteomalacia
- Paget’s disease
Neoplasia i.e.:
- Metastases
- Myeloma
- Lymphoma
- Intrathecal tumours
Other:
- Fibromyalgia
- Torticollis
Referred pain i.e.:
- Pharynx
- Cervical lymph nodes
- Teeth
- Angina pectoris
- Aortic aneurysm
- Pancoast tumour
- Diaphragm [1]
Back Pain
It is a common symptom that affects 60–80% of people at some time in their lives.
Although the prevalence has not increased, reported disability from back pain has risen significantly in the last 30 years.
In Western countries, back pain is the most common cause of sickness related work absence.
Clinical assessment:
The main purpose of clinical assessment is to differentiate the self limiting disorder of acute mechanical back pain from serious spinal pathology.
Mechanical Back Pain i.e.:
- Mechanical back pain is the most common cause of acute back pain in people aged 20–55.
- This accounts for more than 90% of episodes, and is usually acute and associated with lifting or bending.
- It is exacerbated by activity and is generally relieved by rest.
- It is usually confined to the lumbar–sacral region, buttock or thigh, is asymmetrical, and does not radiate beyond the knee (which would imply nerve root irritation).
- On examination, there may be asymmetric local paraspinal muscle spasm, tenderness, and painful restriction of some but not all movements.
Low Back Pain i.e.:
- Low back pain is more common in manual workers, particularly those in occupations that involve heavy lifting and twisting.
- The prognosis is generally good.
- After 2 days, 30% are better and 90% have recovered by 6 weeks.
- Recurrences of pain may occur and about 10–15% of patients go on to develop chronic back pain that may be difficult to treat.
- Psychological elements, such as job dissatisfaction, depression and anxiety, are important risk factors for the transition to chronic pain and disability.
- Degenerative disc disease is a common cause of chronic low back pain.
- Prolapse of an intervertebral disc presents with nerve root pain, which can be accompanied by a sensory deficit, motor weakness, and asymmetrical reflexes.
Examination i.e.
- Examination may reveal a either positive sciatic or femoral stretch test.
- In detail, About 70% of patients improve by 4 weeks.
- Arachnoiditis is a rare cause of chronic severe low back pain.
- It is due to chronic inflammation of the nerve root sheaths in the spinal canal and can complicate meningitis, spinal surgery, or myelography with oil based contrast agents.
Back pain secondary to serious spinal pathology i.e.:
- Generally, Back pain secondary to serious spinal pathology has different characteristics.
- Moreover, If there is clinical evidence of spinal cord or nerve root compression, or a cauda equina lesion, urgent investigation is needed.
- In detail, Spinal stenosis presents with leg discomfort on walking that is relieved by rest (pseudoclaudication).
- Either Bending forwards or walking uphill may also relieve the pain.
- Besides this, Common causes include Paget’s disease, in which enlargement of the vertebrae may encroach on the spinal canal, and osteoarthritis of the spine, in which osteophytes can have the same effect.
- All in all, Patients may adopt a characteristic simian posture, with a forward stoop and slight flexion at hips and knees.
Inflammatory Back Pain i.e.:
- Inflammatory back pain due to seronegative spondyloarthritis has a gradual onset and almost always occurs before the age of 40.
- It is associated with morning stiffness also improves with movement.
- Besides this, Spondylolisthesis may cause back pain that is typically aggravated by standing and walking.
- Occasionally, diffuse idiopathic skeletal hyperostosis can cause back pain but it is usually asymptomatic.
Causes of low back pain i.e.:
- Mechanical back pain
- Prolapsed intervertebral disc
- Osteoarthritis
- Vertebral fracture
- Spinal stenosis
- Paget’s disease
- Spondylolysis
- Bone metastases
- Spondylolisthesis
- Arachnoiditis
- Scheuermann’s disease
Features of mechanical low back pain i.e.:
- Pain varies with physical activity (improved with rest)
- Sudden onset, precipitated either by lifting or bending
- Recurrent episodes
- Pain limited to either back or upper leg
- No clear-cut nerve root distribution
- No systemic features
- Prognosis good (90% recovery at 6 wks)
Red flags for possible spinal pathology:
History i.e.:
- Age: presentation < 20 yrs or > 55 yrs
- Character: constant, progressive pain unrelieved by rest
- Location: thoracic pain
- Past medical history: for example; carcinoma, tuberculosis, HIV, systemic corticosteroid use, osteoporosis
- Constitutional: for example; systemic upset, sweats, weight loss
- Major trauma
Examination i.e.:
- Painful spinal deformity
- Severe/symmetrical spinal deformity
- Saddle anaesthesia
- Progressive neurological signs/muscle-wasting
- Multiple levels of root signs
Clinical features of radicular pain:
Nerve root pain i.e.:
- Unilateral leg pain worse than low back pain
- Pain radiates beyond knee
- Paraesthesia in same distribution
- Nerve irritation signs (reduced straight leg raising that reproduces leg pain)
- Motor, sensory or reflex signs (limited to one nerve root)
- Prognosis reasonable (50% recovery at 6 wks)
Cauda equina syndrome i.e.:
- Difficulty with micturition
- Loss of anal sphincter tone or faecal incontinence
- Saddle anaesthesia
- Gait disturbance
- Pain, numbness or weakness affecting one or both legs
Diagnosis:
- Basically, Investigations are not required in patients with acute mechanical back pain.
- Those with persistent pain (especially > 6 weeks) should undergo further investigation.
- MRI is the investigation of choice since it can demonstrate spinal stenosis, either cord compression or nerve root compression, as well as inflammatory changes in spondyloarthropathy, additionally infectious causes such as spinal abscess.
- Besides this, Plain radiographs can be of value in patients suspected of having vertebral compression fractures, OA also degenerative disc disease.
- If metastatic disease is suspected, additionally radionuclide bone scan or SPECT should be considered.
- Additional investigations that may be required include routine biochemistry and haematology with measurement of ESR and CRP (specifically, to screen for sepsis and inflammatory disease), protein also urinary electrophoresis (for myeloma) and prostate specific antigen (especially for prostate carcinoma).
Management:
- Education is important in patients with mechanical back pain.
- It should emphasise the self limiting nature of the condition and the fact that exercise is helpful rather than damaging.
- Regular analgesia and/or NSAIDs may be required to improve mobility and facilitate exercise.
- Return to work and normal activity should take place as soon as possible.
- Bed rest is not helpful and may increase the risk of chronic disability.
- Referral for physiotherapy or manipulation should be considered if a return to normal activities has not been achieved by 6 weeks.
- Low Dose tricyclic antidepressant drugs may help pain, sleep and mood.
Other treatment i.e.
- Other treatment modalities that are occasionally used include epidural and facet joint injection, traction and lumbar supports, though there is little evidence to support their use.
- Malignant disease, osteoporosis, Paget’s disease and spondylo arthropathies require specific treatment of the underlying condition.
- Surgery is required in less than 1% of patients with low back pain but may be needed in spinal stenosis, in spinal cord compression and in some patients with nerve root compression.
Management of low back pain i.e.:
- Reassure patients (favourable prognosis)
- Advise patients to stay active
- Prescribe medication if necessary (preferably at fixed time intervals)
- Paracetamol
- NSAID
- Consider opioids, muscle relaxants
- Discourage bed rest
- Consider spinal manipulation for pain relief
- Do not advise lumbar supports, back-specific exercises, traction, acupuncture, either epidural or facet injections. [1]
Shoulder pain
It is a common complaint in all genders over the age of 40, and is most often due to degenerative disease of tendons in the rotator cuff.
Clinical findings in shoulder pain:
Rotator cuff lesion i.e.:
Pain reproduced by resisted active movement:
- Abduction: supraspinatus
- External rotation: infraspinatus, teres minor
- Internal rotation: subscapularis
Subacromial bursitis i.e.:
- Pain on full abduction but no pain on resisted active abduction
Bicipital (long head) tendinitis i.e.:
- Tender over bicipital groove
- Pain reproduced by resisted active wrist supination or elbow flexion
Management:
- Management is symptomatic, with analgesics, NSAID, local corticosteroid injections also physiotherapy aimed at restoring normal movement and function.
- Surgery may be required in patients who have debilitating symptoms in association with rotator cuff tears.
- Adhesive capsulitis (in other words; frozen shoulder) presents with upper arm pain that can progress over 4-10 weeks before subsiding over a similar time course.
- Restriction of glenohumeral movement is characteristic.
- In the early phase, there is marked anterior joint/ capsular tenderness and stress pain in a capsular pattern; later there is painless restriction, often of all movements.
- Frozen shoulder is more common in diabetes mellitus, but may also be triggered by a rotator cuff tear, local trauma, myocardial infarction or hemiplegia.
- Treatment in the early stage is with analgesia, intra and extracapsular steroid injection, additionally regular ‘pendulum’ exercises of the arm to prevent the capsule from overtightening.
- In brief, Mobilising and strengthening exercises are the sole treatment in the painless ‘frozen’ stage.
- The natural history is for slow but complete recovery, sometimes taking up to 2 years.
Elbow Pain
Elbow Pain
Olecranon bursitis can also follow local repetitive trauma but other causes include infections, gout and RA.
The most common causes are repetitive strain injury affecting the lateral epicondyle (tennis elbow) and medial epicondyle (golfer’s elbow).
Local causes of elbow pain:
Lesion | Pain | Examination findings |
Tennis elbow | Lateral epicondyle Radiation to extensor forearm | Tender over epicondyle, Pain reproduced by resisted active wrist extension |
Golfer’s elbow | Medial epicondyle Radiation to flexor forearm | Tender over epicondyle, Pain reproduced by resisted active wrist flexion |
Olecranon bursitis | Olecranon | Fluctuant tender swelling over olecranon |
Management:
- Management is by rest, analgesics and topical or systemic NSAID.
- Symptoms may also respond to local application of glyceryl trinitrate patches.
- Local corticosteroid injections may be required in resistant cases. [1]
Hand and Wrist Pain
Hand and Wrist Pain
Pain from hand or wrist joints is well localised to the affected joint, except for pain from the first metacarpal joint, commonly targeted by OA; although maximal at the thumb base, the pain often radiates down the thumb and to the radial aspect of the wrist.
Nonarticular causes of hand pain include:
- Tenosynovitis: either flexor or extensor (pain and swelling, with or without fine crepitus on volar or extensor aspect). Additionally, De Quervain’s tenosynovitis involves the tendon sheaths of abductor pollicis longus and extensor pollicis brevis, and produces pain maximal over the radial aspect of the distal forearm and wrist. In detail, It usually occurs as the result of a repetitive strain injury. There is tenderness (with or without warmth, linear swelling and fine crepitus) over the distal radius and marked pain on forced ulnar deviation of the wrist with the thumb held across the patient’s palm (in other words; Finkelstein’s sign).
- Raynaud’s phenomenon
- C8/T1 radiculopathy
- Reflex sympathetic dystrophy [1]
Hip Pain
Pain from the hip joint is usually maximal deep in the anterior groin, with variable radiation to the buttock, anterolateral thigh, knee or shin.
Trochanteric bursitis is a common cause, typically affecting heavier person women, and occurring in isolation or secondary to an abnormal gait, such as in hip or knee OA.
Pain in the hip region may also be referred from the back.
Root entrapment can cause pain in the lateral thigh (T12–L1) or the inguinal region and lateral thigh (L2–4), but is worsened by coughing and straining more than by movement and is often accompanied by sensory disturbance.
Other less common causes include psoas abscess, retroperitoneal haemorrhage or pelvic inflammation, which can cause inguinal and lateral thigh pain that is aggravated by resisted hip flexion.
Local causes of hip pain:
Lesion | Pain | Examination findings |
Trochanteric bursitis | Upper lateral thigh, worse on lying on that side at night | Tender over greater trochanter |
Gluteal enthesopathy | Upper lateral thigh, worse on lying on that side at night | Tender over greater trochanter, Pain reproduced by resisted active hip abduction |
Adductor tendinitis | Upper inner thigh Usually clearly sports-related | Tender over adductor origin/tendon/muscle, Pain reproduced by resisted active hip adduction |
Ischiogluteal bursitis | Buttock, worse on sitting | Tender over ischial prominence |
iliopectineal bursitis | Anterior groin | Tender (± fluctuant swelling) lateral to femoral pulse, not worsened by internal rotation of hip (cf. hip pain) |
[1]
Knee Pain
The most common cause of knee pain is OA, the features.
Pain that is associated with locking of the knee (sudden painful inability to extend fully) is usually due to a meniscal tear or osteochondritis dissecans.
Referred pain from the hip may present at the knee and is reproduced by hip not knee movement.
Pain from periarticular lesions is well localised to the involved structure.
Anterior knee pain may be due to bursitis occurring as the result of repetitive occupational kneeling, as well as infection and gout.
Anterior knee pain, aggravated by sports, may occur in adolescent girls but is usually self limiting.
Rarely, anterior knee pain may be the result of chondromalacia patellae, in which degenerative changes of the articular cartilage occur.
Local causes of knee pain:
Lesion | Pain | Examination findings |
Pre-patellar bursitis | Anterior patella | Tender fluctuant swelling in front of patella |
Superficial and deep infrapatellar bursitis | Anterior knee, inferior to patella | Tender fluctuant swelling in front of (superficial) or behind (deep) patella tendon |
Anserine bursitis | Upper medial tibia | Tenderness (± warmth, swelling) over upper medial tibia |
Inferior medial collateral ligament enthesopathy | Upper medial tibia | Localized tenderness of upper medial tibia, Pain reproduced by valgus stress on partly flexed knee |
Popliteal cyst (in other words; Baker’s cyst) | Popliteal fossa | Tender swelling of popliteal fossa, usually reducible by massage with knee in mid-flexion |
Patella tendon enthesopathy | Anterior upper tibia | Tenderness also firm swelling of tibial tubercle |
Osteochondritis (Osgood– Schlatter disease) | Anterior upper tibia | Affects adolescents, And Pain on resisted active knee extension |
[1]
Ankle and Foot Pain
Ankle and Foot Pain
- Pain from the mortise joint of the ankle (the tibiofibular– talar joint) is felt between the malleoli and is worse on weight bearing.
- Pain from the subtalar joint is also worse on weight bearing on uneven surfaces.
- The mortise joint is commonly affected by OA, whereas RA tends to affect the subtalar joint.
- Pain under the heel can arise from plantar fasciitis or subcalcaneal bursitis.
- Pain affecting the back of the heel may be due to Achilles tendinitis or bursitis.
spondyloarthritis
- Generally, Patients with seronegative spondyloarthritis may develop enthesopathy affecting this region, resulting in plantar fasciitis, which presents with pain also tenderness under the heel, or as Achilles enthesitis, which presents with pain at the tendon insertion into the calcaneus.
- Moreover, The MTP joints of the feet are commonly involved in RA.
- Besides this, The presentation is with pain on walking below the metatarsal heads, often described as ‘walking on marbles’.
- Patients with active inflammation of the MTP joints have pain when the forefoot is squeezed.
- Involvement of the first MTP joint is common in OA and is associated with a valgus deformity (hallux valgus).
- This joint is also a classical target in acute gout.
Claw foot
- Claw foot (pes cavus) can be associated with anterior foot pain and is characterised by a high arch and clawing of the toes.
- It may be an isolated phenomenon or secondary to neurological disorders such as Friedreich’s ataxia or spina bifida.
Bursitis
- Bursitis and enthesitis resistant to standard measures may respond to local steroid injections.
- Morton’s neuroma is the name given to an entrapment neuropathy of the interdigital nerves of the feet, which presents with shooting pain that is usually located between the third and fourth metatarsal heads.
- Women are most commonly affected.
- Local sensory loss and a palpable tender swelling between the metatarsal heads may be detected.
- Footwear adjustment, with or without a local corticosteroid injection, often helps but surgical decompression may be required if symptoms persist. [1]
Sign & Symptoms
Sign & Symptoms of Musculoskeletal pain
Musculoskeletal pain symptoms can vary from person to person, but generally include i.e.:
- Pain
- Stiffness
- Fatigue
- Burning sensation in muscles
- Sleep disturbance
- Muscle twitching [1]
Homeopathic Treatment
Homeopathic Treatment of Musculoskeletal Pain
Here, the Homeopathic treatment for musculoskeletal pain is natural, safe and without any side-effects, and one can enjoy immense relief from these frustrating symptoms.
It is a patient-oriented science and medicines are prescribed on the characteristics of the individual rather than just the symptoms of the disease.
Homeopathic medicines for deltoid muscle pain:
Sanguinaria Canadensis i.e.:
- Sanguinaria Canadensis is an excellent medicine for homeopathic treatment of deltoid muscle pain when the right side deltoid is affected.
- This homeopathic remedy is of great help for patients who complain of excessively sharp pain in the right shoulder, especially at night.
- Another marked feature of sanguinaria canadensis is when the patient of deltoid pain has excessive muscle soreness and stiffness in the right shoulder.
- The stitching pains make it difficult to even raise the arm.
Rhus Toxicodendron i.e.:
- Rhus Toxicodendron is also a very beneficial remedy for treating deltoid muscle pain and can be given to all those patients of deltoid pain where the pain is the result of over lifting, overstretching or overstraining of the affected upper limb.
- The patient also complains of pain in the shoulder and upper arm with excessive muscle stiffness.
- This muscle stiffness gets worse by taking rest and improves with the movement of upper limb of the affected side.
Ferrum Metallicum i.e.:
- The deltoid pain of left side which is of drawing, tearing nature and gets worse when lying on the bed and by raising the arm can be treated with Ferrum Metallicum.
Nux Moschata i.e.:
- Nux Moschata is used for deltoid muscle pain, additionally the symptoms are pain in left deltoid muscle which gets worse in cold air and is always better in warm surroundings.
Homeopathic medicines for pain in neck muscles:
Actaea Racemosa:
- Actaea Racemosa is of great help for patients who complain of excessive pain, muscular soreness also stiffness in the neck region, especially after using arms for typewriting, using the keyboard or playing the piano.
Ranunculus Bulbosus:
- Patients who complain of a stitching kind of pain along with a burning sensation in the neck after excessive either typewriting or piano playing can benefit by the use of Ranunculus Bulbosus.
Gelsemium Sempervirens:
- It is another helpful homeopathic medicine for neck muscle pain also can be given to those patients who complain of pain in neck muscles and excessive muscle soreness along with headache.
- These patients want to lie down perfectly still to get relief.
Lachnanthes Tinctoria:
- This gives good results in patients of neck muscle pain who complain of worsening of pain at the slightest movement also whose neck is excessively stiff and drawn to one side.
Homeopathic remedies for pain in muscles of lower back:
Rhus Toxicodendron & Bryonia Alba:
- The two homeopathic medicines that are of great help in curing muscle pain of lower back are Rhus Toxicodendron and Bryonia Alba.
- Both these can help in treating excessive pain and stiffness of lower back muscles, but one key difference between the two homeopathic remedies should be kept in mind.
- While Rhus Toxicodendron is best suited as a homeopathic cure for patients whose back muscle pain gets worse while resting and gets better by being in motion or walking, Bryonia Alba is ideal for patients whose back muscle pain gets better through resting and worsens when there is even the slightest motion.
- Rhus Toxicodendron is also without doubt the best medicine for treating muscle pain of back that has arisen after straining or stretching of back muscles by lifting heavy weights or injury to back muscles after a fall.
Arnica Montana:
- Arnica Montana is a very effective medicine for patients whose back muscles started to hurt after an injury caused by blunt instruments.
- It is also of great help for patients complaining of excessive muscle soreness of back and bruised pain in back.
- The pain gets worse by touching and being in motion.
Kali Carbonicum:
- This is another useful Homeopathic medicine that can be given to patients who complain of pain in muscles of lower back in which the prominent symptoms are stitching type of pains in back muscles with excessive weakness of back.
- It gets worse when resting and upon touching.
- The pain in the lower back muscles, which extends in an upward or downward direction of the back or downwards to the thighs, can be treated with this homeopathic medicine.
Homeopathic medicines for pain in calf muscles of leg:
Causticum:
- It is a very useful homeopathic medicine for treating pain in calf muscles, especially of the right side, and when the pain is of a tearing nature with muscle spasms and the calf muscle feels contracted with restlessness of legs at night.
- Causticum is helpful for homeopathic treatment of patients who complain of pain in calf muscles which gets better by the heat of the bed.
Calcarea Carbonica:
- This is another beneficial medicine for homeopathic treatment of pain in calf muscles.
- The symptoms for the use of this homeopathic remedy are tearing, cramping pains in calf muscles with coldness of feet.
Arsenicum Album:
- It is effective in treating pain in calf muscles which is spasmodic, burning and cramping, and when the patient gets relief from warm applications on the calf muscle.
Homeopathic remedies for muscle pain when thigh muscles are involved:
Colocynthis:
- This is a very good Homeopathic medicine for treatment of pain in thigh muscles.
- Colocynthis is the ideal homeopathic cure for patients who complain of pain in thigh muscles, especially of the right side, with a contracted feeling in thigh and worsening of pain by motion.
Ruta Graveolens:
- It is suitable when the thigh muscle pain gets worse with stretching and muscles of back of thigh feels shortened.
Pulsatilla Nigricans:
- This is another good homeopathic remedy for pain of thigh muscles when the pain is of a drawing nature and constantly shifts from one part to the other.
- Pulsatilla Nigricans is also recommended as an effective homeopathic treatment when the pain in thighs is accompanied by restlessness, making the patient sleepless. [3]
Exercise Guidance
Exercise Guidance
Below are examples of basic stretches for back, neck, hands and finger exercises.
As always, consult a registered physiotherapist and/or medical doctor before beginning any exercise or strengthening program to ensure that these particular exercises are suitable for your condition.
Tips for General Stretches:
- Wear comfortable clothes.
- Stretching should be pain free. Additionally, Never force the body into difficult positions.
- Slowly move into the stretch also avoid bouncing, which may actually tear muscles.
- Lastly, Stretch on a clean, flat surface that is large enough to move freely.
Exercise for Lower back pain:
Avoid: Toe Touches i.e.

Toe Touch Exercise
- Any mild discomfort felt at the start of these exercises should disappear as muscles become stronger.
- But if pain is more than mild and lasts more than 15 minutes during exercise, patients should stop exercising and contact a doctor.
- Some exercises may aggravate pain.
- Standing toe touches, for example, put greater stress on the discs and ligaments in your spine.
- They can also overstretch lower back muscles and hamstrings.
Avoid: Sit-ups
Sit Ups Exercise
- Although you might think sit-ups can strengthen your core or abdominal muscles, most people tend to use muscles in the hips when doing sit-ups.
- Sit-ups may also put a lot of pressure on the discs in your spine.
Avoid: Leg Lifts
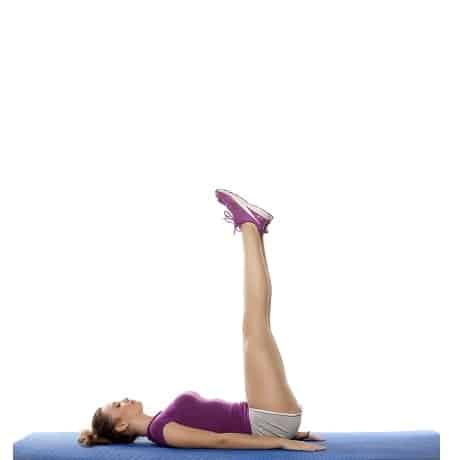
Leg Lifts Exercise
- Leg lifts are sometimes suggested as an exercise to "strengthen your core" or abdominal muscles.
- Exercising to restore strength to your lower back can be very helpful in relieving pain yet lifting both legs together while lying on your back is very demanding on your core.
- If weak, this exercise can make back pain worse.
- Instead, try lying on your back with one leg straight and the other leg bent at the knee.
- Next, keep your lower back flat on floor and slowly lift the straight leg up about 6 inches and hold briefly and then lower the leg slowly.
Try: Bridging

Bridge Exercise
- Lie on your back with knees bent and just your heels on the floor.
- Push your heels into the floor, squeeze your buttocks, and lift your hips off the floor until shoulders, hips, and knees are in a straight line.
- Hold about 6 seconds and then slowly lower hips to the floor and rest for 10 seconds.
- Then, Repeat 8 to 12 times.
- After that, Avoid arching your lower back as your hips move upward.
- Avoid overarching by tightening your abdominal muscles prior also throughout the lift.
Try: Hamstring Stretches

Hamstring Stretches
- Lie on your back and bend one knee.
- Loop a towel under the ball of your foot.
- Straighten your knee and slowly pull back on the towel.
- You should feel a gentle stretch down the back of your leg.
- Hold for at least 15 to 30 seconds.
- Do 2 to 4 times for each leg.
Try: Press-up Back Extensions

Press Up Back Extensions
- Lie on your stomach with your hands under your shoulders.
- Push with your hands so your shoulders begin to lift off the floor.
- If it’s comfortable for you, put your elbows on the floor directly under your shoulders and hold this position for several seconds.
Other Exercises:
Neck Stretch i.e.:
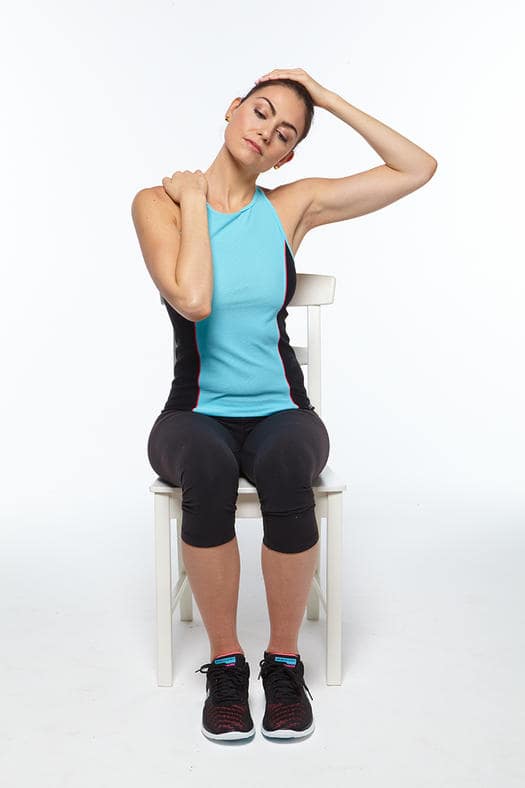
Neck Stretch
- Basically, This stretch works best if you keep your shoulder down as you lean away from it.
- Furthermore, To help you remember to do this, start by relaxing your shoulders also lightly holding on to your thighs or your chair.
- Tilt your head toward your shoulder after that, hold for 15 to 30 seconds.
- If you would like a little added stretch, in detail use your hand to gently and steadily pull your head toward your shoulder.
- For example, keeping your right shoulder down, lean your head to the left.
- Besides this, Let the weight of your head stretch your muscles, or use your left hand to pull gently down on your head.
- Lastly, Repeat 2 to 4 times toward each shoulder.
Pinch Strengthener i.e.:

Pinch Strengthener
- This exercise helps strengthen the muscles of your fingers also thumb.
- It can help you turn keys, open food packages, also use the gas pump more easily.
- Firstly, Pinch a soft foam ball or some putty between the tips of your fingers and your thumb.
- After that, Hold for 30 to 60 seconds.
- Then, Repeat 10 to 15 times on both hands.
- Do this exercise two to three times a week, but rest your hands for 48 hours in between sessions.
- All in all, Don’t do this exercise if your thumb joint is damaged. [3]
Do’s and Don'ts
The Do’s & Don’ts
Do’s:
- Rest: Avoid activities that worsen the pain.
- Apply heat or cold: Heat can help relax muscles and increase blood flow, while cold can reduce inflammation.
- Take over-the-counter pain relievers: Ibuprofen or acetaminophen can help manage pain and reduce inflammation.
- Stretch and exercise: Gentle stretching and exercise can help improve flexibility and reduce pain.
- Maintain a healthy weight: Excess weight can put extra stress on joints.
- See a doctor: If the pain is severe, persistent, or accompanied by other symptoms, consult a doctor to determine the cause and appropriate treatment.
Don’ts:
- Ignore the pain: Ignoring pain can lead to further injury or chronic pain.
- Overdo it: Avoid activities that cause pain or make it worse.
- Push through the pain: Rest when needed and avoid activities that aggravate the pain.
- Self-medicate: Consult a doctor before taking any medication, especially if you have underlying medical conditions.
- Neglect your overall health: Maintain a healthy lifestyle with regular exercise, a balanced diet, and adequate sleep.
Terminology
Terminology
- Musculoskeletal (MSK) system: The complex system that includes your bones, muscles, cartilage, tendons, ligaments, joints, and other connective tissues.
- Acute pain: Pain that comes on suddenly and lasts for a short period, usually less than 6 weeks.
- Chronic pain: Pain that persists for a longer duration, typically more than 3 to 6 months.
- Nociceptive pain: Pain caused by damage to body tissues.
- Neuropathic pain: Pain caused by damage or disease affecting the nervous system.
- Inflammatory pain: Pain associated with inflammation in the body.
- Referred pain: Pain felt in a part of the body other than its actual source.
- Myalgia: Muscle pain.
- Arthralgia: Joint pain.
- Sprain: An injury to a ligament.
- Strain: An injury to a muscle or tendon.
More Relevant Terms:
- Tendonitis: Inflammation of a tendon.
- Bursitis: Inflammation of a bursa (a fluid-filled sac that cushions joints).
- Arthritis: A general term for conditions that cause joint inflammation.
- Osteoarthritis: A degenerative joint disease caused by wear and tear.
- Rheumatoid arthritis: An autoimmune disease that causes joint inflammation.
- Fibromyalgia: A chronic pain syndrome characterized by widespread pain and tenderness.
- Physical therapy (PT): A healthcare profession focused on restoring movement and function in individuals affected by injury, illness, or disability.
- Occupational therapy (OT): A healthcare profession that helps people participate in the activities of daily living through the therapeutic use of everyday activities.
- Analgesics: Pain-relieving medications.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): A class of drugs that reduce pain and inflammation (e.g., ibuprofen, naproxen).
- Opioids: Strong pain-relieving medications (e.g., morphine, codeine).
- Corticosteroids: Medications used to reduce inflammation.
Homeopathic Terminology:
- Similia Similibus Curentur: The fundamental principle of homeopathy, meaning "like cures like." This principle suggests that a substance that can cause symptoms in a healthy person can cure similar symptoms in a sick person.
- Remedy: A homeopathic medicine prepared from natural substances (plants, minerals, or animals) through a process of dilution and succussion (vigorous shaking).
- Potency: The strength or dilution level of a homeopathic remedy.
- Proving: A systematic process of testing a remedy on healthy individuals to determine its symptom picture.
- Repertory: A reference book that lists symptoms and the remedies associated with those symptoms.
- Materia Medica: A comprehensive reference book that describes the properties and therapeutic applications of homeopathic remedies.
- Constitutional Remedy: A remedy that matches the overall physical, mental, and emotional characteristics of an individual.
- Acute Prescribing: The use of remedies for short-term, self-limiting conditions.
- Chronic Prescribing: The use of remedies for long-term, complex, or recurring conditions.
- Aggravation: A temporary worsening of symptoms after taking a remedy, often considered a positive sign of healing.
- Amelioration: An improvement of symptoms after taking a remedy.
Other Relevant Terms:
- Vital force: The energy or life force that animates the body and maintains health.
- Holistic: An approach that considers the whole person – physical, mental, emotional, and spiritual – in health and disease.
- Individualized treatment: The tailoring of treatment to the unique characteristics and needs of each person.
References
References
- Davidson’s Principles and Practice of Medicine (22nd edition) Ch. 25
- https://www.drhomeo.com/pain/natural-homeopathic-remedies-for-muscle-pain-and-aches/
- http://www.palmaholistichealth.com/wp-content/uploads/2017/01/Homeopathy-Benefits-in-Treatments-with-Musculoskeletal-Disorders-via-Holistic-Conventional-Methods-By-Palma-Cicco.pdf
Also Search As
Also Search As
There are several ways to search for information about musculoskeletal (MSK) pain:
Online Resources:
- Search engines: Use general search engines like Google, Bing, or DuckDuckGo with keywords such as "musculoskeletal pain," "types of MSK pain," "causes of MSK pain," or "treatment for MSK pain."
- Reputable health websites: Look for information on websites of trusted organizations like the World Health Organization (WHO), Mayo Clinic, Cleveland Clinic, WebMD, or the National Institutes of Health (NIH).
- Medical journals and databases: Access resources like PubMed, Google Scholar, or Cochrane Library for scientific articles and research studies on MSK pain.
Healthcare Professionals:
- Doctor: Consult your primary care physician or a specialist (such as an orthopedist, rheumatologist, or physiatrist) for diagnosis and treatment recommendations.
- Physical therapist: A physical therapist can assess your condition, provide exercises, and teach you techniques to manage pain and improve function.
- Other specialists: Depending on the cause of your pain, you may need to consult other specialists, such as a neurologist, pain specialist, or occupational therapist.
Libraries and Bookstores:
- Medical textbooks and reference books: Look for books on anatomy, physiology, pain management, or specific musculoskeletal conditions.
- Consumer health books: Find books written for the general public about MSK pain, its causes, and treatment options.
Support Groups:
- Online forums and communities: Connect with others experiencing MSK pain to share experiences, tips, and support.
- In-person support groups: Find local support groups to meet with others face-to-face and learn from each other’s experiences.
Other Resources:
- Health apps and trackers: Some apps can help you track your pain, activity levels, and medication use.
- Podcasts and videos: Listen to podcasts or watch videos by healthcare professionals or individuals with MSK pain.
Frequently Asked Questions (FAQ)
What is Musculoskeletal Pain?
Definition
Musculoskeletal pain is the pain that affects the muscles, ligaments and tendons, bones also nerves.
What are the symptoms of Musculoskeletal Pain?
- Pain
- Stiffness
- Fatigue
- Burning sensation in muscles
- Sleep disturbance
- Muscle twitching
Give the types of Musculoskeletal Pain?
- Generalized Musculoskeletal Pain
- Regional Musculoskeletal Pain
What are the most common causes of MSK pain?
Cause
MSK pain can stem from various factors, including strains, sprains, osteoarthritis, rheumatoid arthritis, fibromyalgia, and poor posture. Age, occupation, and lifestyle also play a role.
What is the most common Musculoskeletal Pain?
- Back pain
- Neck pain
- Shoulder pain
- Elbow pain
- Hand and Wrist pain
- Hip pain
- Knee pain
- Ankle and Foot pain
Can homeopathy help with musculoskeletal pain?
Yes, homeopathy offers a holistic approach to managing musculoskeletal (MSK) pain by addressing the root cause and stimulating the body’s natural healing abilities.
Is homeopathic treatment safe for MSK pain?
Homeopathic remedies are generally safe and have minimal side effects when prescribed by a qualified homeopath.
How does homeopathy compare to conventional treatments for MSK pain?
Homeopathy offers a complementary approach to conventional treatments, focusing on individualized treatment plans and minimizing potential side effects from medications.
How long does it take to see results with homeopathy for MSK pain?
The response time varies depending on individual cases, the severity of the condition, and the chosen remedies. Some individuals may experience relief quickly, while others may require more time.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Musculoskeletal Pain?
Homoeopathic Medicines for Musculoskeletal Pain
- Sanguinaria Canadensis
- Rhus Toxicodendron
- Ferrum Metallicum
- Nux Moschata
- Actaea Racemosa
- Ranunculus Bulbosus
- Gelsemium Sempervirens
- Rhus Toxicodendron & Bryonia Alba
- Arnica Montana
- Kali Carbonicum
- Causticum
