Nephrotic syndrome
Definition
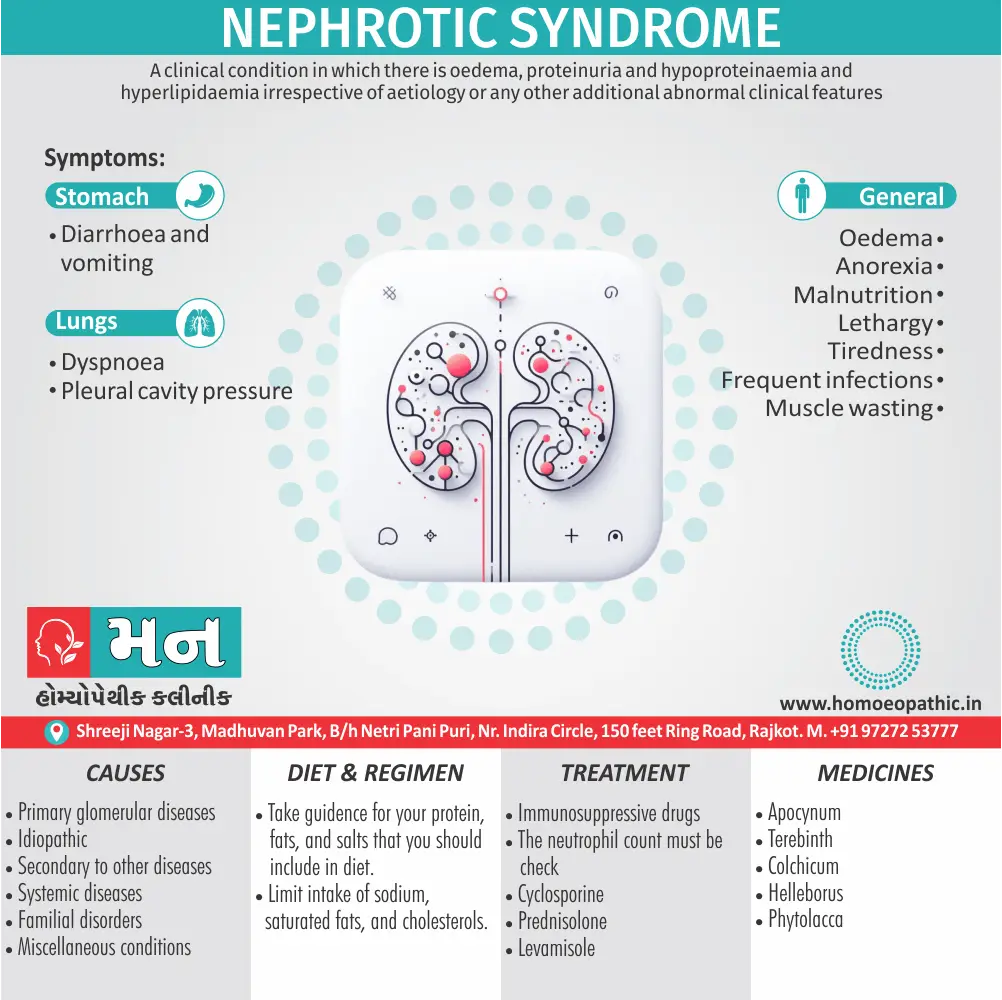
Nephrotic syndrome is a clinical condition in which there is oedema, proteinuria and hypoproteinaemia and hyperlipidaemia irrespective of aetiology. Or any other additional abnormal clinical features [1]
Nephrotic syndrome itself doesn’t have true synonyms because it’s a specific diagnosis. However, there are several ways to describe it depending on the context and desired level of detail.
For broader understanding:
You could use terms like "proteinuric kidney disease" or "glomerular disease with proteinuria." These terms highlight the key features of nephrotic syndrome: protein leakage in the urine (proteinuria) and damage to the glomeruli, the tiny filtering units within the kidneys.
Focusing on cause:
If you know the underlying cause of the nephrotic syndrome, you can use a more specific term. Here are some examples:
- Minimal change disease: This is the most common cause in children and is characterized by normal-looking glomeruli under a microscope despite causing significant proteinuria.
- Focal segmental glomerulosclerosis (FSGS): This is another cause affecting both children and adults, where scarring damages specific parts of the glomeruli.
- Membranous nephropathy: This is a cause more common in adults, where abnormal deposits form on the glomerular membrane, hindering its filtering function.
Hereditary forms:
For specific genetic types, you can use "hereditary nephrotic syndrome." This term indicates a familial predisposition to the condition.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Nephrotic syndrome
- If left undiagnosed or untreated, some of these syndromes will progressively damage enough glomeruli to cause a fall in GFR, producing renal failure.
- Multiple studies have noted that the higher the 24-h urine protein excretion, the more rapid is the decline in GFR. [2]
- Over 80% of patients with nephrotic syndrome have idiopathic glomerular lesions.[1]
Epidemiology
Epidemiology
Several studies have examined the epidemiology of nephrotic syndrome in India. Here are a few, with their references and year of publication:
- (PDF) Nephrotic syndrome in Indian children (1975): This study found that the most common cause of nephrotic syndrome in Indian children was minimal change disease, followed by mild proliferative lesions and membranous glomerulonephritis. [8]
- Changing histologic spectrum of adult nephrotic syndrome over five decades in north India: A single center experience (2010): This study showed a significant increase in the incidence of focal segmental glomerulosclerosis (FSGS) over five decades, making it the most common cause of nephrotic syndrome in adults in North India at the time of publication. [9]
- Focal segmental glomerulosclerosis in India: An update (2016): This review article discusses the epidemiology, etiology, pathogenesis, clinical features, and treatment of FSGS in India, highlighting the increasing incidence of this condition and the need for further research. [10]
Causes
Causes of Nephrotic syndrome
1.Primary glomerular diseases
- Minimal change nephropathy.
- Mesangioproliferative glomerulonephritis.
- Membranous nephropathy.
2. Focal and segmental glomerulosclerosis.
- Crescentic glomerulonephritis.
3. Idiopathic
4. Secondary to other diseases
- Infections – Malaria, hepatitis B, herpes zoster, streptococcal and staphylococcal infections, syphilis, leprosy, schistosomiasis.
- Drugs – NSAlD’s.
- Malignancy – Hodgkin’s disease and other lymphomas.
- Systemic diseases – Diabetes mellitus, amyloidosis, SLE, Henoch-Schonlein purpura, cyroglobulinaemia, polyarteritis nodosa.
- Familial disorders – Congenital (neonatal) nephrotic syndrome, Airport’s syndrome, Fabry’s disease.
- Miscellaneous conditions – Reflux nephropathy, renal vein thrombosis, toxaemia of pregnancy, allergic reactions to insect bites, pollens and vaccines, renal artery stenosis. [1]
Types
Types
Nephrotic syndrome is a clinical entity characterized by heavy proteinuria, hypoalbuminemia, edema, and hyperlipidemia. It is caused by various underlying conditions that damage the glomerulus, the filtering unit of the kidney. The different types of nephrotic syndrome are classified based on the underlying cause and the histological pattern observed on kidney biopsy.
1. Primary Nephrotic Syndrome:
These result from diseases that directly affect the kidneys. The common types include:
- Minimal Change Disease (MCD): Most common cause in children, characterized by normal-appearing glomeruli on light microscopy but foot process effacement on electron microscopy.
- Focal Segmental Glomerulosclerosis (FSGS): Characterized by scarring in some (focal) areas of some (segmental) glomeruli.
- Membranous Nephropathy (MN): Immune-mediated disease characterized by thickening of the glomerular basement membrane. [12]
2. Secondary Nephrotic Syndrome:
These result from systemic diseases that affect the kidneys. The common causes include:
- Diabetic Nephropathy: Nephrotic syndrome due to long-standing diabetes mellitus.
- Systemic Lupus Erythematosus (SLE): Autoimmune disease that can cause various types of glomerulonephritis.
- Amyloidosis: Deposition of abnormal protein (amyloid) in organs, including the kidneys. [11]
Risk Factors
Risk Factors of Nephrotic Syndrome
Medical Conditions:
- Diabetes Mellitus: Diabetic nephropathy is a leading cause of nephrotic syndrome in adults.
- Systemic Lupus Erythematosus (SLE): This autoimmune disease can damage the kidneys and lead to nephrotic syndrome.
- Amyloidosis: The buildup of amyloid proteins in the body can affect the kidneys and cause nephrotic syndrome.
- Other Kidney Diseases: Conditions like focal segmental glomerulosclerosis (FSGS) and membranous nephropathy are also associated with nephrotic syndrome.
Medications:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These pain relievers can sometimes cause kidney damage and lead to nephrotic syndrome.
- Certain Antibiotics: Some antibiotics, particularly those used to treat infections, may increase the risk of nephrotic syndrome.
- Heroin: Intravenous drug use, especially heroin, has been linked to an increased risk of FSGS and nephrotic syndrome.
Infections:
- HIV: People with HIV have an increased risk of developing FSGS and nephrotic syndrome.
- Hepatitis B and C: These viral infections can damage the kidneys and lead to nephrotic syndrome.
- Malaria: This parasitic infection can also cause kidney damage and increase the risk of nephrotic syndrome. [11]
Pathogenesis
Pathogenesis
The core feature of nephrotic syndrome is increased glomerular permeability to proteins, particularly albumin. This leads to massive proteinuria (excess protein in the urine), hypoalbuminemia (low albumin levels in the blood), and edema (fluid accumulation in tissues). The mechanisms underlying this increased permeability can vary depending on the specific cause of nephrotic syndrome.
Primary Causes
Minimal Change Disease (MCD): The exact mechanism is unclear, but it is thought to involve immune dysregulation leading to the loss of negative charge in the glomerular basement membrane (GBM). This charge barrier is crucial for preventing protein leakage.
Focal Segmental Glomerulosclerosis (FSGS): Injury and loss of podocytes (specialized cells that maintain the integrity of the glomerular filtration barrier) are central to the pathogenesis of FSGS. This damage can be caused by various factors, including genetic mutations, circulating permeability factors, and infections.
Membranous Nephropathy (MN): Immune complexes (antibodies bound to antigens) deposit in the GBM, leading to complement activation, inflammation, and thickening of the GBM. This thickening disrupts the filtration barrier and allows proteins to escape.
Secondary Causes
Diabetic Nephropathy: High blood glucose levels damage the glomerulus through various mechanisms, including increased production of reactive oxygen species, activation of protein kinase C, and accumulation of advanced glycation end products.
Systemic Lupus Erythematosus (SLE): This autoimmune disease causes inflammation in the kidneys, leading to immune complex deposition and glomerular injury.
Amyloidosis: The deposition of amyloid fibrils in the glomerulus disrupts the filtration barrier and impairs kidney function. [11]
Pathophysiology
Pathophysiology of Nephrotic syndrome
Nephrotic syndrome is a kidney disorder characterized by heavy proteinuria (excess protein in the urine), hypoalbuminemia (low blood protein levels), hyperlipidemia (high blood cholesterol and triglycerides), and edema (swelling). This cluster of symptoms arises from damage to the glomeruli, the tiny filtering units in the kidneys.
Here’s a breakdown of the pathophysiology:
Glomerular Injury: The glomeruli are intricate networks of capillaries responsible for filtering blood and producing urine. In nephrotic syndrome, these glomeruli are injured, leading to structural and functional changes. This damage can stem from various causes, including:
- Primary Kidney Diseases: Minimal change disease, focal segmental glomerulosclerosis, membranous nephropathy.
- Systemic Diseases: Diabetes, lupus, amyloidosis.
Increased Glomerular Permeability: The injury disrupts the glomerular filtration barrier, making it excessively permeable to proteins, particularly albumin. This leads to significant protein leakage into the urine.
Hypoalbuminemia: As albumin, the main protein in blood, is lost in the urine, its concentration in the blood drops. Albumin plays a crucial role in maintaining oncotic pressure, which keeps fluid within blood vessels.
Edema: The decrease in oncotic pressure causes fluid to shift from the bloodstream into the interstitial spaces (spaces between cells), resulting in edema. This typically manifests as swelling in the legs, ankles, feet, and sometimes the face and hands.
Hyperlipidemia: The liver responds to the low albumin levels by increasing the production of proteins, including lipoproteins. This, coupled with impaired lipid metabolism, contributes to elevated cholesterol and triglyceride levels.
Other Complications: Loss of other important proteins in the urine can lead to various complications, including:
- Increased susceptibility to infections: Loss of immunoglobulins (antibodies).
- Blood clotting abnormalities: Loss of antithrombin III (a protein involved in preventing blood clots).
- Vitamin D deficiency: Loss of vitamin D binding protein.
Clinical Features
Clinical Features
The clinical features of nephrotic syndrome are primarily caused by the loss of protein in the urine and the resulting changes in fluid balance and blood composition.
Key Clinical Features:
- Edema: This is the most common and often the first presenting symptom. It is typically soft, pitting, and initially appears in dependent areas like the ankles and feet, but can progress to involve the face, hands, and abdomen.
- Massive Proteinuria: Defined as protein excretion exceeding 3.5 grams per day in adults. It is a hallmark of nephrotic syndrome and is usually detected on routine urinalysis.
- Hypoalbuminemia: Low levels of albumin in the blood due to its loss in the urine. This contributes to edema and can impair various bodily functions.
- Hyperlipidemia: Elevated levels of cholesterol and triglycerides in the blood, which can increase the risk of cardiovascular disease.
- Lipiduria: Presence of fats in the urine, often appearing as a frothy or milky urine.
- Thromboembolism: Increased risk of blood clots due to changes in clotting factors and loss of anticoagulant proteins in the urine.
- Increased Susceptibility to Infections: Loss of immunoglobulins in the urine can compromise the immune system and make individuals more prone to infections.
- Fatigue and Malaise: Often experienced due to the underlying disease process and the physiological effects of nephrotic syndrome.
Other Possible Features:
- Loss of Appetite
- Abdominal Pain
- Foamy Urine
- Weight Gain (due to fluid retention)
- Difficulty Breathing (if fluid accumulates in the lungs) [12]
Sign & Symptoms
Sign & Symptoms of Nephrotic syndrome
1. Age and sex :
- Two to three times more common in childhood with peak incidence at 2–3 years.
- In this age group, there is a male: female ratio of 2.5: 1, in adults, sex incidence is equal.
2. Oedema :
- In children, oedema may be more obvious in the face and abdomen.
- Usually massive generalized anasarca, the patient almost weighing double his true weight.
- Intense oedema of the scrotum or vulva may occur.
- There may be bilateral hydrothorax.
- Oedema may persist for many weeks or months.
- Spontaneous subsidence with diuresis (nephrotic crisis) may occur, to befollowed again by increase of oedema.
3. GI symptoms :
4. General symptoms :
- Prolonged protein loss causes anorexia, lethargy, tiredness, frequent infections and muscle wasting.
- Dyspnoea may occur if there is fluid in the pleural cavity pressure.
- There may be periods of hypertension; ultimately with development of chronic nephritis permanent hypertension may develop. [1]
Clinical Examination
Clinical Examination
The clinical examination of a patient suspected of having nephrotic syndrome involves a comprehensive assessment to identify signs and symptoms related to the condition.
General Appearance:
- Assess the patient’s overall appearance, noting any signs of fatigue, malaise, or distress.
- Observe for edema, especially in dependent areas such as the ankles, feet, and face.
- Note any signs of pallor, which may indicate anemia.
Vital Signs:
- Measure blood pressure, as hypertension is a common finding in nephrotic syndrome.
- Assess heart rate and respiratory rate for any abnormalities.
Cardiovascular Examination:
- Listen for a pericardial friction rub, which may be present due to pericarditis associated with nephrotic syndrome.
- Assess for signs of heart failure, such as jugular venous distension, peripheral edema, and pulmonary congestion.
Abdominal Examination:
- Palpate the abdomen for ascites (fluid accumulation in the abdominal cavity), which can occur in severe cases of nephrotic syndrome.
- Check for hepatomegaly (enlarged liver) and splenomegaly (enlarged spleen), as these can be associated with underlying causes of nephrotic syndrome.
Skin Examination:
- Examine the skin for signs of edema, pallor, and dryness.
- Look for any rashes or skin lesions that may be associated with underlying systemic diseases.
Neurological Examination:
- Assess for any neurological deficits, which may be present if there are complications related to nephrotic syndrome, such as hypertensive encephalopathy or thromboembolic events. [13]
Diagnosis
Dignosis of Nephrotic syndrome
1. Age and sex :
- Two to three times more common in childhood with peak incidence at 2–3 years.
- In this age group, there is a male: female ratio of 2.5: 1, in adults, sex incidence is equal.
2. Oedema :
- In children, oedema may be more obvious in the face and abdomen.
- Usually massive generalized anasarca, the patient almost weighing double his true weight.
- Intense oedema of the scrotum or vulva may occur.
- There may be bilateral hydrothorax.
- Oedema may persist for many weeks or months.
- Spontaneous subsidence with diuresis (nephrotic crisis) may occur, to befollowed again by increase of oedema.
3. GI symptoms :
4. General symptoms :
- Prolonged protein loss causes anorexia, lethargy, tiredness, frequent infections and muscle wasting.
- Dyspnoea may occur if there is fluid in the pleural cavity pressure.
- There may be periods of hypertension; ultimately with development of chronic nephritis permanent hypertension may develop. [1]
Differential Diagnosis
Differential Diagnosis of Nephrotic syndrome
1.From acute nephritic syndrome
- Table 9 lists the differences between acute nephritic syndrome and nephrotic syndrome
2. Of conditions causing nephrotic syndrome
- Cases due to diabetes, anaphylactoid purpura, drug therapy or irradiation of the kidneys can be diagnosed from the history or other typical findings.
- Amyloid disease history of chronic suppuration; positive liver or gum biopsy or renal biopsy. In thrombosis of renal vein, there is evidence of inferior vena caval thrombosis or presence of only one kidney. Polyarteritis can be diagnosed from other characteristic features like fever, peripheral neuritis etc., or positive muscle biopsy. Disseminated lupus – Anti-dsDNA and anti-SM antibodies.
3. Of generalized anasarca [1]
Complications
Complications
Major Complications:
Thromboembolism: This is a significant risk in nephrotic syndrome due to the loss of anticoagulant proteins in the urine, increased platelet aggregation, and elevated levels of clotting factors. Patients may develop deep vein thrombosis (DVT), pulmonary embolism (PE), or even renal vein thrombosis.
Infections: The loss of immunoglobulins and complement proteins in the urine impairs the immune system, making individuals more susceptible to infections, particularly those caused by encapsulated bacteria like Streptococcus pneumoniae.
Acute Kidney Injury (AKI): This can occur due to a variety of factors, including hypovolemia (decreased blood volume) from fluid shifts, renal vein thrombosis, or the use of nephrotoxic medications.
Anemia: Chronic inflammation and iron deficiency from urinary protein loss can contribute to the development of anemia in nephrotic syndrome.
Hyperlipidemia and Atherosclerosis: Elevated levels of cholesterol and triglycerides can accelerate atherosclerosis, increasing the risk of cardiovascular events like heart attack and stroke.
Protein Malnutrition: Excessive loss of protein in the urine can lead to malnutrition, muscle wasting, and impaired wound healing. [12]
Investigations
Investigation of Nephrotic syndrome
Urine
- Oliguria while oedema is forming, diuresis or normal amount of urine during period of subsidence of oedema.
- Proteinuria Massive, usually more than 5 g/day though variable from time to time; urine becomes almost solid on boiling.
- Daily loss of protein may be 20–50 g.
- Red blood cells absent or Few.
- Casts Fatty casts, tubular cells, oval fat bodies, doubly refractile bodies.
Blood
- Anaemia – Slight, normochromic.
- Hypoalbuminaemia – Serum albumin usually less than 3 g/100 mL.
- Total serum globulin concentration frequently lowered with often elevation of a2 and β globulins.
- Hyperlipoproteinemia (LDL level in particular) and hyperfibrinogenaemia (contributing to raised ESR).
- Renal biopsy is normal on light microscopy but electron microscopy shows typical abnormalities (effacement of epithelial cell foot processes). [3]
Treatment
Treatment of Nephrotic syndrome
1. Immunosuppressive drugs
In steroid-resistant patients, or in those in whom remission can only be maintained by heavy doses of steroids, cyclophosphamide 1.5–2 mg/kg/day for 8-12 weeks with concomitant prednisolone 1. 7.5–15 mg/day.
2. The neutrophil count must be check
Every 2 weeks and cyclophosphamide stopped if it falls below 2 × 103/mm3.
- Cyclosporine 3–5 mg/kg/day is effective in some corticosteroid resistant or dependent patients.
- Prednisolone 7.5–15 mg/day is also given.
- Levamisole – In corticosteroid dependent children 2.5 mg/kg to maximum 150 mg on alternate days is useful in maintenance of remission. [3]
Prevention
Prevention of Nephrotic syndrome
Causes of nephrotic syndrome cannot be prevented, but you can surely follow measures that can help prevent the damage caused to the glomeruli. Here is how you can prevent it:
- If you have diabetes or high blood pressure, make sure that you follow all means to gain control over your sugar and BP level.
- Also, ensure that u are vaccinated for all sorts of common infections, especially if you live or work in a surrounding where people are infected with hepatitis or other common diseases.
- If antibiotics are prescribed, do take them per the doctor’s direction and complete the medication course as per the prescription, even if you feel better. [4]
Homeopathic Treatment
Homeopathic Treatment of Nephrotic syndrome:
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Nephrotic syndrome:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Nephrotic syndrome:
1. Apocynum
- Seems to act somewhat on the kidneys and give rise to various dropsical conditions.
- It produces a scanty urine, which is light in color , or, as it is given, sherry-colored .
- Its first effect is to produce a copious diuresis; this is followed by the scantiness of urine which results in dropsy.
- It also produces an incontinence and may be useful in enuresis.
- A sinking bruised feeling at the stomach is an indication for its use.
- it differs from Arsenic and Apis in the fact that it has unquenchable thirst. Arsenic wants little and often, Apis is thirstles [6]
2. TEREBINTH [TER]
- The urine of Terebinth is one of its most characteristic features.
- It is smoky, turbid, depositing a sediment like coffee grounds, which indicates the presence of disintegrated blood cells.
- Haematuria from venous congestion of the kidneys calls often for Terebinth.
- It has burning during micturition and most painful strangury; the urine, too, may contain albumen and has the odor of violets.
- Peculiar odors to urine may be found under the Viola tricolor, where it smells like that of the cat, and Benzoic acid, where it smells strong and ammoniacal, like that of a horse.
- Terebinth is a useful remedy in cystitis, with much tenesmus of the bladder and the scanty, bloody urine; there is also pressure in the bladder, which extends to the kidneys.
- In acute and chronic nephritis it is often indicated.
- The urine, oedema and the bronchial catarrh may all point to the remedy. [6]
3. COLCHICUM [COLCH]
- Nephritis with bloody, ink-like, albuminous urine, pain in renal region; urine turbid; leaves an orange-colored ring on vessel; after scarlatina or from gouty troubles [5]
4. HELLEBORUS [HELL]
- Nephritis causing dropsical symptoms; congestion of kidneys with extensive effusion of serum in abdominal cavity and tissues of lower extremities urging to urinate, with scanty discharge.
- Urine scanty, dark, with floating dark specks, like coffee- grounds; albuminous or smoky from admixture of decomposed blood; post-scarlatinal nephritis; tubercular meningitis. [5]
5. PHYTOLACCA [PHYT]
- Weakness, dull pain and soreness in the region of the kidneys, most on right side, and connected with heat, uneasiness down the ureters; chalklike sediment in the urine, albuminous urine [5]
Diet & Regimen
Diet & Regimen of Nephrotic syndrome
Nephrotic syndrome requires careful management, and diet is a key player. Here’s what you need to know:
Diet:
- Protein: Moderate is key. Too much can strain your kidneys, but you still need it. Lean meats, poultry, fish, eggs, and low-fat dairy are good sources. Your doctor or a dietitian can help you find the right balance.
- Sodium: Keep it low to fight swelling. Avoid processed foods, canned soups, salty snacks, and added salt.
- Fluids: You might need to limit fluids if swelling is a problem. Your doctor will advise you.
- Fat: Choose healthy fats (olive oil, avocados, nuts, seeds) and limit saturated and trans fats to help manage cholesterol.
- Potassium: Some medications for nephrotic syndrome can affect potassium levels, so talk to your doctor about what’s right for you.
Regimen:
- Medication: Your doctor may prescribe corticosteroids, diuretics, and blood pressure meds to control symptoms and prevent complications.
- Monitoring: Regular checkups are important to track blood pressure, urine protein, and cholesterol levels.
- Weight: Aim for a healthy weight to ease the burden on your kidneys.
- Exercise: Stay active as your condition allows.
- Smoking: If you smoke, quitting is crucial for your kidney health.
Do’s and Don'ts
The Do’s & Don’ts
Do’s:
Follow your doctor’s instructions: It is crucial to adhere to the treatment plan prescribed by your nephrologist or healthcare provider. This includes taking prescribed medications as directed and attending regular checkups.
Maintain a healthy diet:
Monitor your weight daily: Keep track of your weight and report any significant changes to your doctor, as this can indicate fluid retention.
Get vaccinated: Due to the increased risk of infections, it is important to stay up-to-date with vaccinations, including those for influenza and pneumococcal disease.
Practice good hygiene: Wash your hands frequently and avoid close contact with people who are sick to minimize the risk of infections.
Exercise regularly: Engage in moderate physical activity as recommended by your doctor to maintain muscle strength and overall health.
Monitor your blood pressure and cholesterol: Regular monitoring of these parameters is essential to manage potential complications associated with nephrotic syndrome.
Educate yourself: Learn as much as you can about nephrotic syndrome, its causes, treatments, and potential complications. This will help you make informed decisions about your health and actively participate in your care.
Don’ts:
Never Consume excessive salt: Limit your intake of salty foods, processed foods, and fast food, as these can worsen edema and blood pressure.
Do not Smoke or use tobacco products: Smoking can further damage your kidneys and increase the risk of cardiovascular complications.
No self-medication: Avoid taking over-the-counter medications or herbal supplements without consulting your doctor, as some may interact with your prescribed medications or worsen your condition.
Don’t ignore symptoms: If you experience any new or worsening symptoms, such as increased swelling, fatigue, or difficulty breathing, contact your doctor immediately.
Never Skip medications or appointments: Consistency with your treatment plan is crucial for managing nephrotic syndrome and preventing complications.
Terminology
Terminology
Albumin:
A protein made by the liver that helps keep fluid in the bloodstream so it doesn’t leak into other tissues. Low levels (hypoalbuminemia) are a hallmark of nephrotic syndrome.
Anasarca:
Severe generalized edema (swelling) throughout the body, often seen in advanced cases of nephrotic syndrome.
Ascites:
Accumulation of fluid in the abdominal cavity, a potential complication of nephrotic syndrome.
Azotemia:
Elevated levels of nitrogenous waste products (urea and creatinine) in the blood, which can occur if nephrotic syndrome progresses to kidney failure.
Basement membrane:
A thin, supportive layer of tissue that underlies the cells lining various organs, including the glomerulus in the kidneys. Damage to this membrane is often involved in nephrotic syndrome.
Edema:
Swelling caused by fluid buildup in the body’s tissues, a key symptom of nephrotic syndrome.
Glomerular filtration rate (GFR):
A measure of how well the kidneys are filtering waste products from the blood. This can be decreased in nephrotic syndrome, especially if there is underlying kidney damage.
Glomerulonephritis:
Inflammation of the glomeruli, the tiny filtering units in the kidneys. This can be a primary cause of nephrotic syndrome or a secondary complication.
Glomerulosclerosis:
Scarring of the glomeruli, which can lead to impaired kidney function and nephrotic syndrome.
Hematuria:
Blood in the urine, which is not typically seen in nephrotic syndrome but may indicate other kidney problems.
Hyperlipidemia:
Elevated levels of lipids (fats) in the blood, a common feature of nephrotic syndrome.
Hypoalbuminemia:
Low levels of albumin in the blood, a hallmark of nephrotic syndrome.
Nephrotic range proteinuria:
Loss of 3.5 grams or more of protein in the urine per day, a defining characteristic of nephrotic syndrome.
Podocyte:
Specialized cells in the glomerulus that play a key role in maintaining the filtration barrier. Damage to podocytes is a common feature in certain types of nephrotic syndrome.
Proteinuria:
Presence of excess protein in the urine, the cardinal feature of nephrotic syndrome.
Thrombosis:
Formation of blood clots, a potential complication of nephrotic syndrome due to changes in blood clotting factors.
Key Principles:
Individualization:
Homeopathic treatment is tailored to the individual patient, considering their unique physical, mental, and emotional symptoms, as well as the underlying cause of their nephrotic syndrome.
Holistic Approach:
Homeopathy aims to treat the whole person, not just the disease, focusing on restoring balance and promoting overall health and well-being.
Law of Similars:
The central principle of homeopathy, where a substance that can cause symptoms in a healthy person is used in a highly diluted form to treat similar symptoms in a sick person.
Commonly Used Homeopathic Remedies:
Apis Mellifica:
For edema, particularly with stinging and burning sensations.
Apocynum Cannabinum:
For edema with thirst, difficulty breathing, and heart palpitations.
Arsenicum Album:
For anxiety, restlessness, and thirst for small sips of water.
Helleborus Niger:
For edema with drowsiness and slow mental processes.
Natrum Sulphuricum:
For edema worsened by dampness and humidity.
References
References
- Golwala’s Medicine for student 25th edition 2017
- Harrison-s_Principles_of_Internal_Medicine-_19th_Edition-_2_Volume_Set
- Hutchison’s clinical methods_22nd edition [ pg –298]
- https://www.medanta.org/patient-education-blog/nephrotic-syndrome-diet-causes-prevention-medanta
- Homoeopathic Therpeutics By Lilienthal
- Practical Homoeopathic Therapeutics By Dewey W.A
- PATHOPHYSIOLOGY OF NEPHROTIC SYNDROME – Histopathology.Mentor
- Srivastava RN, Moudgil A, Mandal RN, et al. Nephrotic syndrome in Indian children. Indian J Med Res. 1975;63(9):1317-1324.
- Jha V, Guleria S, Sakhuja V, Joshi K, Kohli HS. Changing histologic spectrum of adult nephrotic syndrome over five decades in north India: A single center experience. Indian J Nephrol. 2010 Jul;20(3):130-5. doi: 10.4103/0971-4065.68401. PMID: 20823887; PMCID: PMC2931186.
- Dinda AK, Agrawal V, Kohli HS, et al. Focal segmental glomerulosclerosis in India: An update. World J Nephrol. 2016 Apr 6;5(2):169-80. doi: 10.5527/wjn.v5.i2.169. PMID: 27114861; PMCID: PMC4827203.
- Brenner & Rector’s The Kidney, 11th Edition (2020) by Karl Skorecki, Glenn M. Chertow, Philip A. Marsden, Maarten W. Taal, Alan S. L. Yu, and Jürgen Floege. Published by Elsevier.
- Harrison’s Principles of Internal Medicine, 21st Edition (2022) by Dennis L. Kasper, Anthony S. Fauci, Stephen L. Hauser, Dan L. Longo, J. Larry Jameson, and Joseph Loscalzo. Published by McGraw Hill Education.
- Davidson’s Principles and Practice of Medicine, 24th Edition (2023) by Stuart Ralston, Ian Penman, Mark WJ Strachan, and Richard Hobson. Published by Elsevier.
- Brenner & Rector’s The Kidney by Alan S.L. Yu, Glenn T. Nagami, and Thomas M. Coffman
Also Search As
Also Search As
People can search for homeopathic articles on nephrotic syndrome using several methods:
Online Search Engines:
- Use specific keywords: Search terms like "homeopathic treatment for nephrotic syndrome," "homeopathy for nephrotic syndrome," or "homeopathic remedies for nephrotic syndrome" can yield relevant results.
- Combine terms: Combine broader terms like "homeopathy" and "nephrotic syndrome" to cast a wider net.
Homeopathic Journals and Websites:
- Reputable sources: Search for articles in established homeopathic journals like "The American Homeopath," "Homeopathy," or "The International Journal of High Dilution Research."
- Homeopathic organizations: Websites of national or international homeopathic organizations often have resources and articles on various conditions, including nephrotic syndrome.
Homeopathic Practitioner Websites:
- Individual practitioners: Many homeopathic practitioners have websites or blogs where they share information and case studies related to their practice, including nephrotic syndrome.
Online Forums and Communities:
- Discussion boards: Look for forums or discussion boards dedicated to homeopathy, where you can find discussions and potentially articles about nephrotic syndrome.
Social Media:
- Homeopathic groups: Many homeopathic groups and pages on platforms like Facebook and Twitter share relevant articles and information.
There are several ways to search for information on nephrotic syndrome:
Online Search Engines:
- Use search terms like "nephrotic syndrome," "symptoms of nephrotic syndrome," "causes of nephrotic syndrome," or "treatment of nephrotic syndrome."
- You can also search for specific types of nephrotic syndrome like "minimal change disease" or "focal segmental glomerulosclerosis."
Reputable Medical Websites:
- Look for information on websites of well-known medical institutions like the Mayo Clinic, Cleveland Clinic, National Institutes of Health (NIH), or the National Kidney Foundation.
Medical Databases:
- Access databases like PubMed or Google Scholar to search for scientific articles and research papers on nephrotic syndrome.
Books and Medical Journals:
- Consult textbooks on nephrology or internal medicine for comprehensive information on nephrotic syndrome.
- Search for articles in peer-reviewed medical journals for the latest research and findings on nephrotic syndrome.
Consult a Healthcare Professional:
- If you have specific questions or concerns about nephrotic syndrome, it’s always best to consult with a doctor, nephrologist, or other healthcare professional for personalized advice and guidance.
Frequently Asked Questions (FAQ)
What is nephrotic syndrome?
Definition
Nephrotic syndrome is a kidney disorder characterized by large amounts of protein leaking into the urine, low blood protein levels, swelling (edema), and high cholesterol.
What causes nephrotic syndrome?
Several conditions can cause nephrotic syndrome, including diseases directly affecting the kidneys (like minimal change disease or focal segmental glomerulosclerosis) and systemic diseases like diabetes or lupus.
How is nephrotic syndrome treated?
Treatment depends on the underlying cause. It often includes medications to control blood pressure, reduce protein loss, and manage cholesterol levels.
Dietary changes like reducing salt intake are also important.
How is nephrotic syndrome diagnosed?
Diagnosis
Diagnosis involves a combination of urine tests to measure protein levels, blood tests to check kidney function and protein levels, and sometimes a kidney biopsy to examine the kidney tissue.
What are the symptoms of nephrotic syndrome?
Common symptoms include swelling in the legs, feet, ankles, or face, foamy or bubbly urine, weight gain from fluid retention, fatigue, and loss of appetite.
Can homeopathy treat nephrotic syndrome?
Homeopathy offers a complementary approach to manage nephrotic syndrome alongside conventional treatment. It aims to address the root cause and individual symptoms to improve overall health and well-being.
How does homeopathy work for nephrotic syndrome?
Homeopathic practitioners prescribe remedies based on the individual’s unique symptom profile and constitution.
The goal is to stimulate the body’s self-healing mechanisms to reduce inflammation, control proteinuria, and improve kidney function.
Are homeopathic remedies safe for nephrotic syndrome?
Homeopathic remedies are highly diluted and considered safe, with minimal side effects.
However, it’s crucial to consult a qualified homeopathic practitioner for proper assessment and prescription.
Can homeopathy replace conventional treatment for nephrotic syndrome?
Homeopathy is not a replacement for conventional treatment. It is best used as a complementary therapy alongside conventional medical care for optimal management of nephrotic syndrome.
Which homeopathic remedies are commonly used for nephrotic syndrome?
Homoeopathic Medicines for Nephrotic Syndrome
Several remedies are used based on individual symptoms, such as Apis mellifica for edema with burning sensation, Apocynum cannabinum for edema with thirst, and Arsenicum album for anxiety and restlessness.
