Organic Catatonic Disorder
Definition
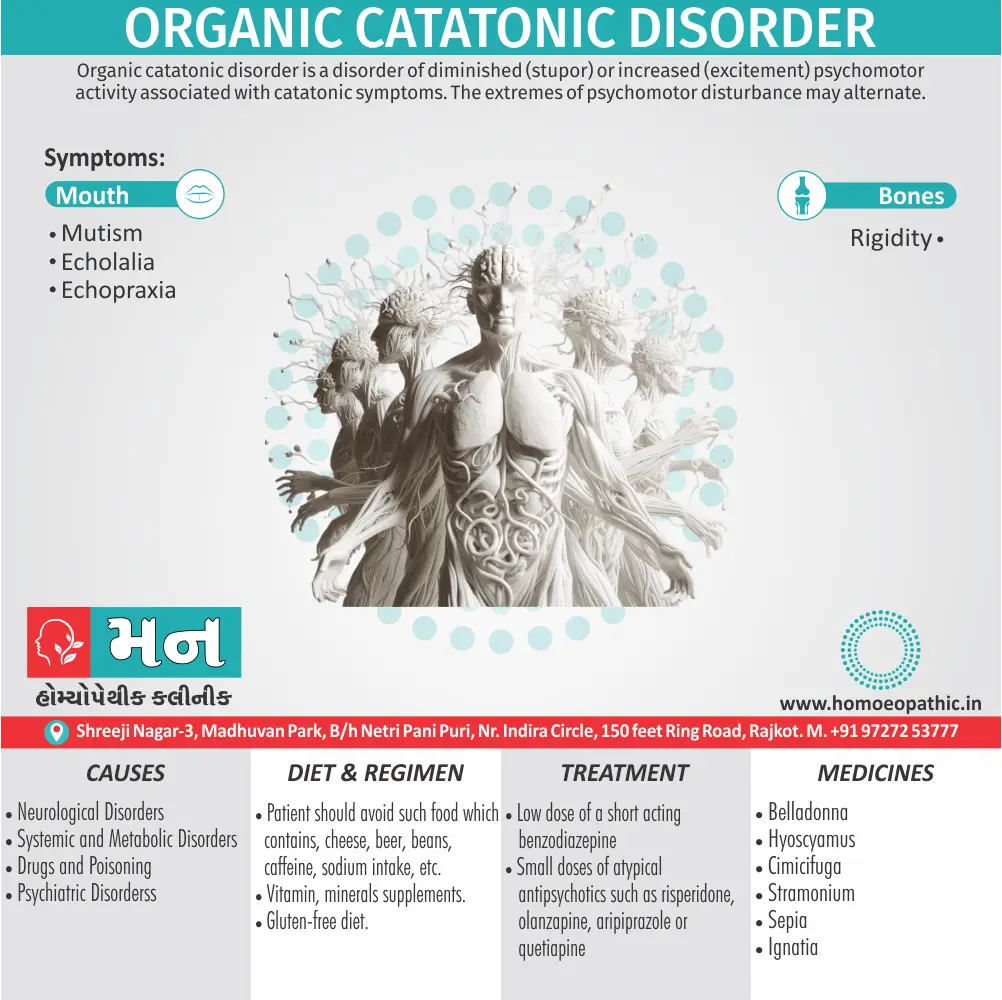
Organic catatonic disorder is a disorder of diminished (stupor) or increased (excitement) psychomotor activity associated with catatonic symptoms. Additionally; The extremes of psychomotor disturbance may alternate. [2]
There aren’t many direct synonyms for "organic catatonic disorder" because it’s a specific medical term. However, here are some options depending on the context:
- Medically induced catatonia: This emphasizes the cause being a medical condition.
- Organic mental disorder with catatonic features: This is broader and describes a decline in mental function with catatonic symptoms due to a physical cause.
- You can use terms related to specific symptoms: For example, stupor, mutism, waxy flexibility (depending on the prominent features).
Additionally, some historical terms might be encountered:
- Brain syndrome with catatonic features
- Psychoorganic syndrome with catatonia (These terms are less common now)
Important Note: These terms are for informational purposes only. If you’re looking for medical advice, consult a healthcare professional.
Overview
Epidemiology
Causes
Risk Factors
Pathogenesis
Pathophysiology
Types
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
According to the ICD-10 (F06.1) disorder of either diminished (stupor) or increased (excitement) psychomotor activity associated with catatonic symptoms.
Generally; The extremes of psychomotor disturbance may alternate. [2] In detail; The presence of other catatonic symptoms and signs increases the confidence in the diagnosis. [1]
Epidemiology
Epidemiology
Unfortunately, specific epidemiological data focusing solely on Organic Catatonic Disorder in India is limited. However, we can glean some insights from broader studies on catatonia and its association with organic causes.
One relevant study is "Phenomenology and treatment of Catatonia: A descriptive study from north India" published in 2011. It reported that 5.92% of catatonic cases were attributed to organic disorders like febrile encephalitis, Wilson’s disease, and other medical conditions. While this study doesn’t provide specific prevalence rates for Organic Catatonic Disorder, it highlights the presence of this condition within the broader context of catatonia in India.
It is important to note that:
- Organic Catatonic Disorder is diagnosed when catatonia is directly caused by an underlying medical condition, such as neurological disorders, metabolic disturbances, or infections.
- Catatonia itself is a complex neuropsychiatric syndrome characterized by abnormalities in motor behavior, movement, and speech.
The limited availability of specific epidemiological data on Organic Catatonic Disorder in India underscores the need for further research in this area.[3]
Causes
Causes
1. Neurological Disorders i.e.:
- Post-encephalitic parkinsonism
- Limbic encephalitis
- Surgical procedures on basal ganglia
- Neoplasms in diencephalon, frontal lobe and limbic system
- Subacute sclerosing pan encephalitis (in other words; SSPE)
- General paresis of incomprehensible(GPI)
- Petit Mal status
- Post-ictal phase of epilepsy
- Subdural haematoma
- Cerebral malaria
- Cortical venous thrombosis
2. Systemic and Metabolic Disorders i.e.:
- Diabetic ketoacidosis
- Acute intermittent porphyria
- Hyperparathyroidism causing hypercalcaemia
- Pellagra
- Hepatic encephalopathy
- Systemic lupus erythematosus
- Homocystinuria
- Membranous glomerulonephritis
3. Drugs and Poisoning i.e.:
- Organic alkaloids
- Antipsychotics
- ACTH (therapeutic doses)
- Aspirin
- Illuminating gas
- Ethyl alcohol (especially large doses)
- Levodopa
- Disulfiram
- CO poisoning
- Lithium toxicity
- Methylphenidate
- Phencyclidine (specifically large doses)
- Mescaline
4. Psychiatric Disorders i.e.:
- Catatonic schizophrenia
- Depressive stupor wild stupor
- Periodic catatonia
- Conversion also dissociative disorder
- Reactive psychosis
- During hypnosis. [1]
Risk Factors
Risk Factors of Organic Catatonic Disorder
The development of Organic Catatonic Disorder is primarily associated with the presence of an underlying medical or neurological condition.
Neurological Disorders: Conditions such as epilepsy, brain tumors, strokes, encephalitis, and head injuries can disrupt brain function and increase the risk of catatonia.
Metabolic Disturbances: Electrolyte imbalances, hepatic encephalopathy, and endocrine disorders can impact neurotransmitter levels and brain metabolism, contributing to catatonia.
Infections: Systemic infections or those directly affecting the central nervous system, such as meningitis or encephalitis, can trigger an inflammatory response and lead to catatonia.
Autoimmune Diseases: Conditions like systemic lupus erythematosus and anti-NMDA receptor encephalitis can affect the brain and increase the risk of catatonia.
Medications: Certain medications, particularly those affecting dopamine and GABA neurotransmitter systems, can induce catatonia as a side effect.
Substance Abuse: Alcohol withdrawal and certain drug intoxications or withdrawals can precipitate catatonia.
This comprehensive guide provides valuable insights into the various risk factors, diagnostic criteria, and treatment options for catatonia, including the organic subtype.
It is important to emphasize that the presence of these risk factors does not guarantee the development of Organic Catatonic Disorder. However, they increase the likelihood of its occurrence, particularly in individuals with a predisposition to psychiatric or neurological conditions.[4]
Pathogenesis
Pathogenesis of Organic Catatonic Disorder
The pathogenesis of Organic Catatonic Disorder involves the disruption of neural circuits responsible for motor control, behavior, and cognition due to an underlying medical condition. These disruptions can affect various brain regions and neurotransmitter systems, leading to the characteristic symptoms of catatonia.
Key Mechanisms:
Neurotransmitter Imbalance:
- Dysregulation of dopamine, GABA, glutamate, and serotonin has been implicated in catatonia.
- Reduced GABAergic activity is a particularly prominent hypothesis, as GABA plays a crucial role in inhibiting motor and behavioral responses.
- Dopamine dysregulation, both hypo- and hyperactivity, has also been observed in catatonic states.
Brain Region Dysfunction:
- Functional neuroimaging studies have identified abnormalities in the frontal cortex, basal ganglia, thalamus, and cerebellum in patients with catatonia.
- These regions are crucial for motor control, executive functions, and emotional regulation, and their dysfunction can contribute to catatonic symptoms.
Underlying Medical Conditions:
- Organic catatonia can be triggered by a wide range of medical conditions, including:
- Neurological disorders (e.g., encephalitis, stroke, brain tumors)
- Metabolic disturbances (e.g., hepatic encephalopathy, electrolyte imbalances)
- Infections (e.g., sepsis, systemic lupus erythematosus)
- Autoimmune disorders
- Drug reactions or withdrawal
- Organic catatonia can be triggered by a wide range of medical conditions, including:
These conditions can disrupt brain function through various mechanisms, such as inflammation, neurotoxicity, or metabolic derangements. [5]
Pathophysiology
Pathophysiology of Organic Catatonic Disorder
Organic catatonic disorder, characterized by the presence of catatonic symptoms due to an underlying medical condition, reflects disruptions in complex neural circuits and neurotransmitter systems. The precise mechanisms remain incompletely understood, but several key factors contribute to its pathophysiology.
Neurotransmitter Imbalance:
- Dopamine: Dysregulation of dopamine pathways, particularly in the frontostriatal circuits, plays a crucial role. Both excessive and deficient dopaminergic activity have been implicated in catatonia.
- Glutamate: Abnormalities in glutamatergic transmission, particularly through NMDA receptor dysfunction, may also contribute to catatonic states.
- GABA: Alterations in GABAergic inhibitory systems may disrupt the balance between excitation and inhibition in the brain, predisposing to catatonia.
Structural and Functional Brain Abnormalities:
- Frontal Lobe Dysfunction: The frontal lobes, responsible for executive functions, motor planning, and behavioral control, are frequently implicated. Disruptions in frontal lobe activity can lead to the motor and behavioral abnormalities seen in catatonia.
- Basal Ganglia Involvement: The basal ganglia, crucial for motor control and procedural learning, also play a role. Dysfunction in these structures can contribute to the motor disturbances and stereotypies observed in catatonia.
- Limbic System Dysregulation: The limbic system, involved in emotional processing and motivation, may be implicated. Emotional dysregulation can lead to the affective changes and withdrawal seen in some cases of catatonia.
Underlying Medical Conditions:
- Neurological Disorders: Conditions like encephalitis, epilepsy, tumors, and neurodegenerative diseases can disrupt brain function and lead to catatonic symptoms.
- Metabolic Disturbances: Electrolyte imbalances, hepatic encephalopathy, and endocrine disorders can impact neuronal function and precipitate catatonia.
- Infections: Systemic infections or those directly affecting the central nervous system can trigger catatonic states.
- Autoimmune Disorders: Some autoimmune diseases, like systemic lupus erythematosus and anti-NMDA receptor encephalitis, can affect the brain and lead to catatonia.[5]
This renowned textbook provides in-depth insights into the pathophysiology of various psychiatric disorders, including catatonia and its organic causes.
Please note that the pathophysiology of organic catatonic disorder is complex and multifactorial. Further research is needed to fully elucidate the underlying mechanisms and develop targeted interventions.
Types
Types
While the DSM-5 no longer explicitly categorizes Organic Catatonic Disorder into specific subtypes, the underlying medical conditions causing it can be broadly classified, offering insight into different presentations:
- Neurological Disorders: Conditions like encephalitis, epilepsy, stroke, brain tumors, and neurodegenerative diseases can disrupt brain function and lead to catatonic symptoms.
- Metabolic Disturbances: Electrolyte imbalances, vitamin deficiencies (particularly B12), and endocrine disorders (like thyroid dysfunction) can impact neurotransmitter systems and contribute to catatonic states.
- Infections: Systemic infections or those directly affecting the central nervous system (like meningitis or encephalitis) can trigger an inflammatory response and cause catatonia.
- Autoimmune Disorders: Conditions like Systemic Lupus Erythematosus (SLE) or anti-NMDA receptor encephalitis can affect the brain and lead to catatonic manifestations.
- Drug-Induced Catatonia: Certain medications or substance abuse (like amphetamines or cocaine) can disrupt neurotransmitter balance and induce catatonic symptoms.
This comprehensive textbook provides in-depth information on catatonia, including its association with various medical conditions and its management.
It’s important to emphasize that the presentation of Organic Catatonic Disorder can vary depending on the specific underlying medical condition and individual factors. Therefore, accurate diagnosis and treatment require a thorough medical evaluation and collaboration between psychiatrists and other medical specialists.[5]
Clinical Features
Clinical Features of Organic Catatonic Disorder
Organic Catatonic Disorder, characterized by catatonic symptoms directly caused by an underlying medical condition, presents with a range of clinical features. These features may include:
- Motor Immobility: This may manifest as stupor (unresponsiveness to the environment), catalepsy (maintaining rigid postures), or waxy flexibility (limbs remaining in positions placed by others).
- Motor Excitement: Excessive and purposeless motor activity, agitation, or stereotyped movements may occur.
- Mutism: Absence or near-absence of speech.
- Negativism: Resistance to instructions or attempts to be moved.
- Posturing: Assuming and maintaining bizarre or uncomfortable postures.
- Echolalia or Echopraxia: Involuntary repetition of others’ words or actions.
- Automatic Obedience: Exaggerated compliance with commands.
- Other Catatonic Signs: Grimacing, mannerisms, or verbigeration (repetition of phrases or words).
These clinical features can vary depending on the underlying medical condition causing the catatonia. It’s crucial to identify and address the underlying medical cause to effectively treat Organic Catatonic Disorder.
This comprehensive textbook provides a detailed overview of Organic Catatonic Disorder, including its clinical features, diagnostic criteria, and treatment approaches. It is a valuable resource for clinicians and researchers in the field of psychiatry.
Please note:
- The specific clinical presentation can vary depending on the individual and the underlying medical condition.
- A thorough medical evaluation is essential to diagnose Organic Catatonic Disorder and identify its underlying cause.
- Early identification and treatment of the underlying medical condition are crucial for improving outcomes.
It’s recommended to consult the latest edition of Kaplan & Sadock’s Synopsis of Psychiatry or other reliable psychiatric resources for the most up-to-date information on Organic Catatonic Disorder.[5]
Sign & Symptoms
Sign & Symptoms of Organic Catatonic Disorder
1. Mutism i.e.:
In brief; Complete absence of speech.
2. Rigidity i.e.:
Maintenance of a rigid posture against efforts to be moved.
3. Negativism i.e.:
An apparently motiveless resistance to all commands and attempts either to be moved, or doing just the opposite.
4. Posturing i.e.:
Voluntary assumption of an inappropriate also often bizarre posture for long periods of time.
5. Stupor i.e.:
Akinesis (no movement) with mutism but with evidence of relative preservation of conscious awareness.
6. Echolalia i.e.:
Repetition, echo or mimic king of either phrases or words heard.
7. Echopraxia i.e.:
Repetition, echo or mimic king of actions observed.
8. Waxy flexibility i.e.:
In detail; Parts of body can be placed in positions that will be maintained for long periods of time, even if very uncomfortable; flexible like wax.
9. Ambitendency i.e.:
Due to ambivalence, conflicting impulses and tentative actions are made, but no goal directed action occurs, e.g. on asking to take out tongue, tongue is slightly protruded but taken back again
10. Other signs i.e.:
Such as mannerisms, stereotypies (verbal also behavioural), automatic obedience (commands are followed automatically, irrespective of their nature) and verbigeration (incomprehensible speech). [1]
Clinical Examination
Clinical Examination
Mental Status Examination
- Appearance and Behavior: Note any abnormalities in posture, movement, or facial expressions. Observe for signs of immobility, rigidity, posturing, or excessive motor activity.
- Mood and Affect: Assess the patient’s emotional state and responsiveness. Note any signs of flat affect, withdrawal, or agitation.
- Speech: Evaluate the patient’s speech patterns. Observe for mutism, echolalia, or other speech abnormalities.
- Thought Content: Assess the patient’s thoughts and beliefs. Note any signs of confusion, delusions, or hallucinations.
- Cognition: Evaluate the patient’s cognitive abilities, including attention, memory, orientation, and judgment.
Physical Examination
- Neurological Examination: Perform a thorough neurological examination to identify any focal neurological deficits or signs of underlying neurological disorders.
- General Medical Examination: Conduct a complete physical examination to identify any signs of systemic illness or medical conditions that might contribute to catatonia.
Diagnostic Investigations
- Laboratory Tests: Perform blood tests, urine tests, and other relevant investigations to rule out metabolic disturbances, infections, or other medical conditions.
- Neuroimaging: Consider brain imaging studies (CT scan or MRI) to evaluate for structural abnormalities or evidence of neurological disorders.
- Electroencephalography (EEG): An EEG may be helpful in identifying seizure activity or other electrophysiological abnormalities.
This comprehensive textbook provides in-depth information on various psychiatric disorders, including catatonia and its organic causes.
Important considerations:
- Early identification and treatment of the underlying medical cause are crucial for the successful management of Organic Catatonic Disorder.
- A multidisciplinary approach involving psychiatrists, neurologists, and other medical specialists is often necessary for accurate diagnosis and comprehensive treatment.
Remember that this is a general outline of a clinical examination for Organic Catatonic Disorder. The specific assessment may vary depending on the individual patient’s presentation and the suspected underlying medical cause.[5]
Diagnosis
Diagnosis of Organic Catatonic Disorder
According to the ICD-10(F06.1), the following features are required for the diagnosis of organic catatonic disorder, additionally to the general guidelines for the diagnosis of other organic mental disorders, described earlier:
1. Stupor (diminution or complete absence of spontaneous movement with partial or complete mutism, negativism, also rigid posturing).
2. Excitement (gross hyper-motility either with or without a tendency to assaultiveness).
3. Mixed (shifting rapidly also unpredictably from hypo- to hyperactivity). [1]
Differential Diagnosis
Differential Diagnosis of Organic Catatonic Disorder
The diagnosis of Organic Catatonic Disorder involves a thorough evaluation to rule out other conditions that can present with similar clinical features. Some key differentials include:
Primary Psychiatric Disorders:
- Schizophrenia: Catatonic features can occur in schizophrenia, often accompanied by hallucinations, delusions, and disorganized thinking.
- Mood Disorders: Severe depression or mania with catatonic features can mimic Organic Catatonic Disorder.
- Neurodevelopmental Disorders: Autism Spectrum Disorder, especially in individuals with intellectual disability, can present with catatonic-like behaviors.
Neurological Disorders:
- Epilepsy: Non-convulsive status epilepticus and certain types of seizures can cause catatonic symptoms.
- Encephalitis: Inflammation of the brain, often due to infection, can lead to catatonia.
- Stroke: Particularly those involving the frontal lobes or basal ganglia can result in catatonic states.
- Neurodegenerative Disorders: Parkinson’s disease, Huntington’s disease, and other neurodegenerative conditions can present with catatonia, especially in later stages.
Other Medical Conditions:
- Metabolic Disorders: Electrolyte imbalances, hepatic encephalopathy, and other metabolic disturbances can cause catatonic symptoms.
- Infections: Systemic infections or those directly affecting the central nervous system can trigger catatonia.
- Autoimmune Disorders: Conditions like Systemic Lupus Erythematosus (SLE) and anti-NMDA receptor encephalitis can manifest with catatonic features.
- Drug-Induced: Certain medications, particularly those affecting dopamine levels, can cause catatonia as a side effect.
Important Considerations:
- Thorough History and Physical Examination: Careful assessment of the patient’s medical history, including recent illnesses, medications, and substance use, is crucial.
- Laboratory and Imaging Studies: Blood tests, EEG, brain imaging (CT or MRI), and other investigations help identify underlying medical conditions causing catatonia.
- Collaboration with Other Specialists: Consultation with neurologists, internists, and other relevant specialists may be necessary for proper diagnosis and management.
Remember: Early recognition and treatment of the underlying medical condition are essential for improving outcomes in Organic Catatonic Disorder.[5]
Complications
Complications of Organic Catatonic Disorder
Organic Catatonic Disorder, a condition where catatonia is caused by an underlying medical illness, can lead to a variety of complications, both physical and psychological.
Physical Complications:
- Malnutrition and Dehydration: Due to the potential for immobility, refusal to eat or drink, or difficulty swallowing, individuals with Organic Catatonic Disorder are at risk of malnutrition and dehydration. These can lead to further health problems, including electrolyte imbalances and organ dysfunction.
- Deep Vein Thrombosis and Pulmonary Embolism: Immobility also increases the risk of blood clots forming in the deep veins of the legs (deep vein thrombosis). These clots can break loose and travel to the lungs, causing a potentially fatal pulmonary embolism.
- Pressure Sores: Prolonged immobility can lead to the development of pressure sores (bedsores), which are painful ulcers that can become infected.
- Muscle Contractures: When muscles are not used for extended periods, they can shorten and tighten, leading to contractures that limit movement and cause pain.
- Pneumonia: Difficulty swallowing and immobility can increase the risk of aspiration pneumonia, which occurs when food or liquid enters the lungs and causes an infection.
- Rhabdomyolysis: In severe cases of catatonia with muscle rigidity, muscle breakdown (rhabdomyolysis) can occur, releasing harmful substances into the bloodstream and potentially causing kidney damage.
Psychological Complications:
- Cognitive Impairment: The underlying medical condition causing Organic Catatonic Disorder can also affect cognitive function, leading to difficulties with memory, attention, and problem-solving.
- Emotional Distress: The experience of catatonia can be distressing for individuals, leading to anxiety, depression, and confusion.
- Social Isolation: The symptoms of catatonia can make it difficult to interact with others, leading to social withdrawal and isolation.[5]
It is important to note that early recognition and treatment of Organic Catatonic Disorder can help to prevent or minimize these complications. If you or someone you know is experiencing symptoms of catatonia, it is crucial to seek medical attention immediately.
Please remember that this information is intended for general knowledge and educational purposes only, and does not constitute medical advice. It is essential to consult a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.
Investigations
Investigations for Organic Catatonic Disorder
Organic Catatonic Disorder requires a comprehensive assessment to identify the underlying medical cause. Investigations generally include:
- Complete Blood Count (CBC): To assess for infections, anemia, or other blood disorders.
- Electrolyte Panel: To check for electrolyte imbalances, which can sometimes cause catatonia.
- Liver Function Tests (LFTs): To assess liver function, as liver disease can contribute to catatonia.
- Renal Function Tests (RFTs): To assess kidney function, as kidney disease can also cause catatonia.
- Thyroid Function Tests (TFTs): To assess thyroid function, as both hypothyroidism and hyperthyroidism can cause catatonia.
- Toxicology Screen: To rule out drug or alcohol intoxication or withdrawal as a cause of catatonia.
- Brain Imaging: Such as CT scan or MRI, to identify any structural abnormalities in the brain that could be causing catatonia.
- Electroencephalogram (EEG): To assess brain electrical activity and identify any seizures or other abnormalities that could be causing catatonia.
- Lumbar Puncture (Spinal Tap): To obtain cerebrospinal fluid (CSF) for analysis, which can help identify infections or other conditions that could be causing catatonia.[5]
Additional tests may be ordered depending on the patient’s clinical presentation and suspected underlying cause.
Please note that this is a general overview and the specific investigations required may vary depending on the individual case. Always consult a qualified healthcare professional for personalized medical advice.
Treatment
Treatment of Organic Catatonic Disorder
1. Treatment of the underlying cause, if amenable to treatment.
2. Symptomatic treatment with low dose of a short acting benzodiazepine (e.g. Lorazepam), or electroconvulsive therapy (if needed).
Anti-psychotics should usually be avoided as they can make catatonic features worse; however small doses of atypical anti-psychotics such as Risperidone, Olanzapine, Aripiprazole or Quetiapine can be used with care. [1]
Prevention
Prevention of Organic Catatonic Disorder
Since Organic Catatonic Disorder is directly caused by an underlying medical condition, the most effective preventive measure is to focus on:
Early detection and treatment of underlying medical conditions: Prompt identification and management of neurological disorders, infections, metabolic disturbances, or any other health issues can significantly reduce the risk of developing catatonia.
Careful medication monitoring: Certain medications can trigger catatonia in susceptible individuals. Regular medication reviews and dose adjustments, especially with psychotropic medications, can help minimize the risk.
Healthy lifestyle choices: Maintaining a healthy lifestyle with regular exercise, balanced nutrition, adequate sleep, and stress management can contribute to overall physical and mental well-being, reducing the likelihood of developing medical conditions that could lead to catatonia.
Specific preventive measures may be relevant for individuals with a known predisposition to certain medical conditions. For example:
- People with a family history of neurological disorders may benefit from regular neurological checkups.
- Individuals with a history of substance abuse should seek appropriate treatment and support to prevent relapses and potential complications.
It is important to note that:
- Complete prevention of Organic Catatonic Disorder may not always be possible, as some underlying medical conditions are unpredictable.
- Early recognition of catatonic symptoms and prompt medical intervention are crucial for effective treatment and improved outcomes.[5]
This resource provides a comprehensive overview of psychiatric disorders, including catatonia, and discusses the importance of addressing underlying medical conditions for both prevention and treatment.
Homeopathic Treatment
Homoeopathic treatment for Organic Catatonic Disorder
It is crucial to understand that homeopathic treatment for serious conditions like Organic Catatonic Disorder should never replace or delay conventional medical treatment. Consulting a qualified healthcare professional is paramount for proper diagnosis and management.
Having said that, certain homeopathic remedies are sometimes considered as supportive or complementary therapy, alongside conventional treatment, for symptoms associated with catatonia. However, their effectiveness is not scientifically proven and varies based on individual cases.
Some homeopathic remedies that might be considered, depending on the specific symptoms and underlying cause of the Organic Catatonic Disorder, include:
- Hyoscyamus niger: Often considered when there is delirium, agitation, and incoherent speech.
- Stramonium: Might be suggested if the patient exhibits fear, mania, and hallucinations.
- Veratrum album: Sometimes used when there’s a combination of physical and mental exhaustion along with delusions.
- Cuprum metallicum: May be considered if there are muscle cramps, spasms, or convulsions.
- Helleborus niger: Could be suggested in cases of mental dullness, slowness, and lack of response.
The choice of remedy, dosage, and duration of treatment depend on the individual’s unique presentation and should be determined by a qualified homeopathic practitioner.
Key Points to Remember:
- Consult a doctor first: Never self-treat Organic Catatonic Disorder with homeopathy. Conventional medical intervention is critical for managing the underlying cause and preventing complications.
- Homeopathy as supportive therapy: Homeopathic remedies, when used alongside conventional treatment, might aid in managing some symptoms, but their efficacy is not scientifically established.
- Individualized treatment: Homeopathic treatment is tailored to the individual’s specific symptoms and constitution, necessitating consultation with a qualified homeopathic practitioner.
- No guarantees: Homeopathy does not offer a guaranteed cure for Organic Catatonic Disorder. Its role is mainly supportive and complementary to conventional medical management.
Diet & Regimen
Diet & Regimen for Organic Catatonic Disorder
It recommendations for Organic Catatonic Disorder should always be secondary to addressing the underlying medical cause through appropriate medical intervention.
Once the underlying cause is being addressed, the following dietary and lifestyle modifications may be beneficial in supporting overall health and potentially aiding recovery:
Diet
- Nutrient-rich diet: Focus on whole foods, including plenty of fruits, vegetables, whole grains, and lean protein sources. These provide essential nutrients for brain function and overall health.
- Hydration: Ensure adequate fluid intake to prevent dehydration, which can worsen confusion and other symptoms.
- Limit processed foods: Minimize processed foods, sugary drinks, and unhealthy fats, which can negatively impact overall health and potentially exacerbate symptoms.
- Consider specific dietary needs: Depending on the underlying medical cause, specific dietary adjustments might be necessary. For instance, individuals with diabetes might need a carbohydrate-controlled diet.
Regimen
- Regular sleep schedule: Maintain a consistent sleep-wake cycle to promote optimal brain function and overall well-being.
- Gentle exercise: Engage in regular physical activity as tolerated, such as walking or gentle stretching. Exercise can improve mood, reduce stress, and enhance cognitive function.
- Stress management: Practice relaxation techniques, such as deep breathing exercises or meditation, to manage stress and promote emotional well-being.
- Social engagement: Encourage social interaction and participation in enjoyable activities to stimulate cognitive function and combat social withdrawal.
- Medication adherence: Ensure consistent medication adherence as prescribed by the healthcare professional to manage the underlying medical condition and prevent complications.[5]
This comprehensive resource provides insights into the management of various psychiatric disorders, including those with organic causes, and emphasizes the importance of a holistic approach that includes dietary and lifestyle modifications alongside conventional medical treatment.
Disclaimer:
- The information provided here is not a substitute for personalized medical advice. Always consult a qualified healthcare professional for specific recommendations tailored to your individual needs and underlying medical condition.
- The effectiveness of dietary and lifestyle modifications may vary from person to person. It’s essential to work closely with your healthcare team to develop a plan that supports your overall health and recovery.
Do’s and Don'ts
Do’s:
- Seek immediate medical attention: If you suspect you or someone you know is experiencing catatonic symptoms, especially if accompanied by signs of an underlying medical condition, seek immediate medical attention. Early diagnosis and treatment are crucial for managing the underlying cause and improving outcomes.
- Follow the prescribed treatment plan: Adhere to the treatment plan recommended by your healthcare professional, which may include medications, therapies, or other interventions. Consistency is key to managing the underlying medical condition and improving catatonic symptoms.
- Maintain a healthy lifestyle: Focus on a balanced diet, regular exercise, adequate sleep, and stress management techniques to support overall physical and mental well-being.
- Create a supportive environment: Surround yourself with supportive and understanding individuals who can provide emotional support and encouragement throughout the recovery process.
- Communicate openly with your healthcare team: Discuss any concerns or questions you may have about your condition, treatment, or recovery process. Open communication fosters trust and collaboration, leading to more effective treatment and improved outcomes.
Don’ts:
- Ignore or dismiss symptoms: Catatonia is a serious condition that requires prompt medical attention. Ignoring or dismissing symptoms can lead to delayed diagnosis and treatment, potentially worsening the underlying medical condition and increasing the risk of complications.
- Self-medicate or self-treat: Avoid self-medicating or attempting to treat catatonia without professional guidance. This can be dangerous and may worsen the condition.
- Isolate yourself: Social withdrawal can be a symptom of catatonia and can hinder recovery. Make an effort to connect with others and engage in social activities as tolerated.
- Give up on treatment: Recovery from Organic Catatonic Disorder may take time and require ongoing treatment and support. Don’t give up on the process; with patience and perseverance, improvement is possible.
- Stigmatize or judge individuals with catatonia: Catatonia is a medical condition, not a character flaw. Avoid stigmatizing or judging those with catatonia. Offer understanding and support instead.
Remember:
- These are general guidelines. Always consult a qualified healthcare professional for personalized advice and treatment recommendations tailored to your specific situation.
- With timely and appropriate medical intervention, along with supportive care and lifestyle modifications, individuals with Organic Catatonic Disorder can experience significant improvement and achieve a better quality of life.
Terminology
Terminology
Organic Catatonic Disorder: A specific type of catatonia where the symptoms are directly caused by an underlying medical condition.
Catatonia: A neuropsychiatric syndrome characterized by abnormalities in motor behavior, movement, and speech. These abnormalities can include:
- Stupor: A state of decreased responsiveness and awareness.
- Catalepsy: Maintaining rigid postures for extended periods.
- Waxy flexibility: Resistance to movement but allowing limbs to be moved into positions that are then maintained.
- Mutism: Absence or near absence of speech.
- Negativism: Resistance to instructions or attempts to be moved.
- Echolalia: Repeating words or phrases spoken by others.
- Echopraxia: Imitating the movements of others.
Organic: Refers to a medical condition caused by a physical or physiological change in the body, such as an infection, injury, or metabolic disturbance.
Underlying Medical Condition: The specific physical or physiological issue that is directly causing the catatonic symptoms. This can include a wide range of conditions, such as:
- Neurological disorders (e.g., encephalitis, brain tumors, stroke)
- Metabolic disturbances (e.g., electrolyte imbalances, vitamin deficiencies)
- Infections (e.g., sepsis, meningitis)
- Autoimmune diseases (e.g., systemic lupus erythematosus)
- Endocrine disorders (e.g., hyperthyroidism, hypothyroidism)
- Drug or medication toxicity or withdrawal
Differential Diagnosis: The process of distinguishing Organic Catatonic Disorder from other conditions that may present with similar symptoms, such as:
- Psychiatric disorders (e.g., schizophrenia, major depressive disorder)
- Neuroleptic malignant syndrome (a rare but serious reaction to antipsychotic medications)
- Other medical conditions (e.g., Parkinson’s disease, akinetic mutism)
Understanding these key terms is essential for comprehending the complex nature of Organic Catatonic Disorder and its relationship to underlying medical conditions.
Homoeopathic Terminology
Here are some terminologies and their meanings that might be used in a homeopathic article discussing Organic Catatonic Disorder, keeping in mind that homeopathy has its own specific vocabulary:
- Organic Catatonic Disorder: While this term is primarily used in conventional medicine, a homeopathic article might also use it to acknowledge the underlying medical cause of the catatonic symptoms.
- Catatonia: Homeopaths would likely recognize the characteristic symptoms of catatonia, such as stupor, catalepsy, waxy flexibility, mutism, negativism, etc.
- Underlying Cause/Aetiology: Homeopaths may refer to the underlying medical condition causing the catatonia as the ‘aetiology’ or ‘causative factor.’
- Totality of Symptoms: This is a core principle in homeopathy. It emphasizes considering not just the catatonic symptoms but also the patient’s overall physical, mental, and emotional state, as well as their medical history and individual characteristics, when choosing a remedy.
- Constitutional Remedy: This refers to a homeopathic remedy that matches the patient’s overall constitution or inherent tendencies, and is believed to address their susceptibility to illness.
- Repertory: A reference book used by homeopaths to find remedies based on specific symptoms.
- Materia Medica: A collection of detailed descriptions of the properties and effects of homeopathic remedies.
- Potency: The strength or dilution of a homeopathic remedy.
- Aggravation: A temporary worsening of symptoms that sometimes occurs after taking a homeopathic remedy, which is often seen as a positive sign of the body’s response to the treatment.
- Proving: A process in which healthy individuals take a homeopathic remedy to record its effects, helping to understand its potential uses.
Additional terms that might appear in a homeopathic context
- Vital Force: The concept of a life energy or self-healing mechanism within the body.
- Law of Similars: The principle that "like cures like," meaning a substance that causes symptoms in a healthy person can cure similar symptoms in a sick person.
- Miasm: A theoretical concept in homeopathy referring to inherited predispositions to certain diseases.
Important Note: Homeopathic approaches to serious conditions like Organic Catatonic Disorder should always be used as a complementary therapy alongside conventional medical treatment. It is crucial to consult with qualified healthcare professionals for proper diagnosis and management.
Please let me know if you have any other questions or would like further explanation of any of these terms.
References
References
- A Short Textbook of Psychiatry by Niraj Ahuja / Ch 3/ Ch 5/ Ch 19.
- http://apps.who.int/classifications/icd10/browse/2016/en#/F00-F09
- Grover, S., Chakrabarti, S., & Avasthi, A. (2011). Phenomenology and treatment of Catatonia: A descriptive study from north India. Indian Journal of Psychiatry, 53(1), 26.
- Catatonia: A Clinician’s Guide to Diagnosis and Treatment,1st Edition, Max Fink, Michael Alan Taylor, 2003, Cambridge University Press.
- Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry (12th Edition), Benjamin J. Sadock, Virginia A. Sadock, Pedro Ruiz, 2022, Wolters Kluwer.
Also Search As
Also Search As
People can search for homeopathic articles on Organic Catatonic Disorder using a variety of approaches:
Online search engines:
- Use specific keywords:
- Organic catatonic disorder homeopathy
- Homeopathic remedies for catatonia
- Catatonia treatment in homeopathy
- Homeopathic approach to organic catatonia
- Refine search results:
- Use advanced search options to specify the type of information you’re looking for (e.g., articles, case studies, research papers).
- Add additional keywords related to specific symptoms or underlying causes (e.g., "encephalitis and homeopathy").
Homeopathic websites and databases:
Explore websites of homeopathic organizations and institutions: Many organizations have resources and articles on various health conditions, including catatonia.
Search specialized homeopathic databases: These may contain case studies, provings, and materia medica information related to catatonia and potential remedies.
Consult online homeopathic forums and communities: These platforms may offer insights and discussions on homeopathic approaches to catatonia, although it’s essential to be discerning and verify information from reliable sources.
Homeopathic practitioners and libraries:
Consult a qualified homeopath: They can provide personalized guidance and recommend relevant resources.
Visit homeopathic libraries: These libraries often have a vast collection of books and journals on homeopathy, including information on various health conditions.
Important Considerations:
- Critical evaluation: While searching for information, it’s important to critically evaluate the sources and assess the quality of the evidence presented.
- Prioritize conventional medicine: Remember that homeopathy should not replace or delay conventional medical treatment for Organic Catatonic Disorder.
- Consult a qualified healthcare professional: Always seek the advice of a qualified healthcare professional for proper diagnosis and treatment of any health condition.
By utilizing these search strategies and being mindful of the considerations mentioned above, people can access information on homeopathic approaches to Organic Catatonic Disorder, while ensuring that they prioritize their safety and well-being.
You can search for information on Organic Catatonic Disorder using a variety of approaches:
Medical websites and databases:
- Explore reputable medical websites: Many organizations and institutions like the Mayo Clinic, National Institutes of Health (NIH), and World Health Organization (WHO) provide reliable information on various medical conditions, including Organic Catatonic Disorder.
- Search medical databases: PubMed, MedlinePlus, and other medical databases contain scholarly articles and research papers on Organic Catatonic Disorder.
- Consult online medical forums and communities: While these can provide valuable insights, it’s important to exercise caution and verify information from reliable sources.
Medical professionals and libraries:
Consult a qualified healthcare professional: They can provide personalized guidance and recommend relevant resources.
Visit medical libraries: These libraries often have a vast collection of books and journals on various medical topics, including Organic Catatonic Disorder.
Additional resources:
Patient advocacy groups: Organizations focused on mental health or specific medical conditions associated with catatonia may offer resources and support.
Support groups: Connecting with others who have experienced catatonia or similar conditions can provide emotional support and valuable information.
By utilizing these search strategies and being mindful of the considerations mentioned above, you can access reliable and relevant information about Organic Catatonic Disorder.
Frequently Asked Questions (FAQ)
What is Organic Catatonic Disorder?
It is a disorder of diminished (stupor) or increased (excitement) psychomotor activity associated with catatonic symptoms.
What causes Organic Catatonic Disorder?
- Neurological Disorders
- Systemic and Metabolic Disorders
- Drugs and Poisoning
- Psychiatric Disorders
Can Organic Catatonic Disorder be prevented?
Prompt diagnosis and management of underlying medical conditions can help prevent the development of Organic Catatonic Disorder.
What are the symptoms of Organic Catatonic Disorder?
- Mutism
- Rigidity
- Negativism
- Posturing
- Stupor
- Echolalia
- Echopraxia
- Waxy flexibility
How is Organic Catatonic Disorder diagnosed?
Diagnosis involves a thorough medical evaluation to identify the underlying cause, including physical exams, lab tests, and imaging studies.
Can homeopathy help with Organic Catatonic Disorder?
Homeopathy might offer supportive care by addressing some symptoms associated with catatonia, but it should never replace conventional medical treatment for the underlying cause.
How does homeopathic treatment work in conjunction with conventional medical care?
Homeopathy may be used alongside conventional treatment to potentially support overall well-being and manage specific symptoms. However, it should never replace necessary medical interventions.
Are there any risks or side effects associated with homeopathic treatment for Organic Catatonic Disorder?
When used correctly, homeopathic remedies are generally considered safe. However, consulting a qualified practitioner is vital to ensure appropriate use and avoid any potential interactions with other medications.
What homeopathic remedies are used for catatonic symptoms?
Homoeopathic Medicines For Organic Catatonic Disorder
Remedies like Hyoscyamus niger, Stramonium, and Veratrum album might be considered based on the individual’s specific symptoms, but their use should be guided by a qualified homeopath.
