Organic Mood Disorder
Definition
Organic mood disorder are characterized by those that involve the moods or emotions of a person that are changed due to a physiological problem with the brain or nervous system. [3]
Disorders characterized by a change in mood or affect, usually accompanied by a change in the overall level of activity, depressive, hypomanic, wild or bi-polar, but arising as a consequence of an organic disorder. [2]
Organic Mood Disorder is an outdated term that was used to describe mood disturbances (like depression or mania) caused by an underlying medical condition. While not used in current diagnostic manuals, here are some related or synonymous terms you might encounter:
Here are some synonyms for organic mood disorder, depending on the specific nuance you want to convey:
General terms:
- Mood disorder due to a general medical condition (MD-GMC): This is the most accurate and widely recognized term in a clinical setting.
- Medical mood disorder: This is a simpler option but might be less informative.
Terms emphasizing specific aspects:
- Secondary mood disorder: This highlights that the mood disorder is a consequence of another medical condition.
- Organic affective disorder: "Affective" refers to emotions or moods, so this term emphasizes the emotional disturbance caused by a physical issue. (This term is less common than others).
Important Note:
- These terms are for informational purposes only. If you’re looking for medical advice, consult a healthcare professional.
- Please note that the specific terminology used can vary depending on the context and the exact medical condition involved.
- If you have further questions or need clarification on any of these terms, feel free to ask!
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
Organic mood disorder are characterized by those that involve the moods or emotions of a person that are changed due to a physiological problem with the brain or nervous system. [3]
Disorders characterized by a change in mood or affect, usually accompanied by a change in the overall level of activity, depressive, hypomanic, wild or bi-polar, but arising as a consequence of an organic disorder. [2]
Epidemiology
Epidemiology
Unfortunately, specific epidemiological data focusing solely on Organic Mood Disorder (OMD) in India is limited. However, we can gather insights from broader studies on mood disorders and mental health in India.
A meta-analysis of 13 psychiatric epidemiological studies (Ganguli, 1982) indicated a prevalence rate of 0.4 per 1000 population for organic psychosis, a category under which OMD may fall.
Another study (Reddy & Chandrashekar, 1998) reported that the prevalence of mood disorders among the old age person in India was estimated to be between 22 and 33 per 1000 population. This group is particularly susceptible to OMDs due to age-related changes and medical conditions.
More recent research highlights the increasing burden of mental health issues in India, including mood disorders, but specific data on OMD remains scarce.
Key points to note:
- The prevalence of OMD is likely underestimated due to underreporting and misdiagnosis.
- The old age population is at a higher risk for OMD.
- There is a need for more targeted research on OMD in India to better understand its epidemiology and develop appropriate interventions.[3][4]
Disclaimer:
Please note that due to the limited availability of specific epidemiological data on Organic Mood Disorder in India, the information provided here is based on broader studies and may not fully represent the true prevalence of this condition. Further research is needed to gain a more accurate understanding of the epidemiology of OMD in India.
Causes
Causes
1. Drugs:
- Mania: for example; INH, Levodopa, Bromide, LSD, Corticosteroids (hypomania), Hallucinogens, Tricyclic antidepressants, Cocaine, Baclofen, Amphetamines, Bromocriptine, Cimetidine, Procyclidine
- Depression: Reserpine, Ethanol, Clonidine, Methyldopa, Propranolol, Corticosteroids, Antipsychotics (particularly typical antipsychotics), Cimetidine, Anticancer chemo therapy, Oral contraceptives. Additionally; Any drug a depressed person is taking should be considered a potential factor in the causation of depressive episode.
2. Endocrine disorders:
Mania: Hyperthyroidism
Depression: for example; Hypothyroidism, Cushing’s syndrome, Addison’s disease, hyper also hypoparathyroidism.
3. CNS disorders:
Parkinsonism, Huntington’s chorea, PSP (progressive supranuclear palsy; depression more likely), CVAs (in other words; cerebrovascular accidents; left-sided anterior lesions and right sided posterior lesions cause depression in stroke), cerebral tumours, epilepsy (complex partial seizures), neurosyphilis (GPI), head injury (mania more likely), multiple sclerosis.
4. Post-viral illnesses:
Influenza, infectious mononucleosis, viral pneumonia, also infectious hepatitis.
5. Deficiencies:
Pellagra, deficiency of thiamine, folate, niacin, folate, also B12.
6. Others:
Carcinoma pancreas (i.e. depression), SLE, pernicious anaemia, temporal arteritis (i.e. depression), carcinoid syndrome (i.e. mania). [1]
Types
Types of Organic Mood Disorder
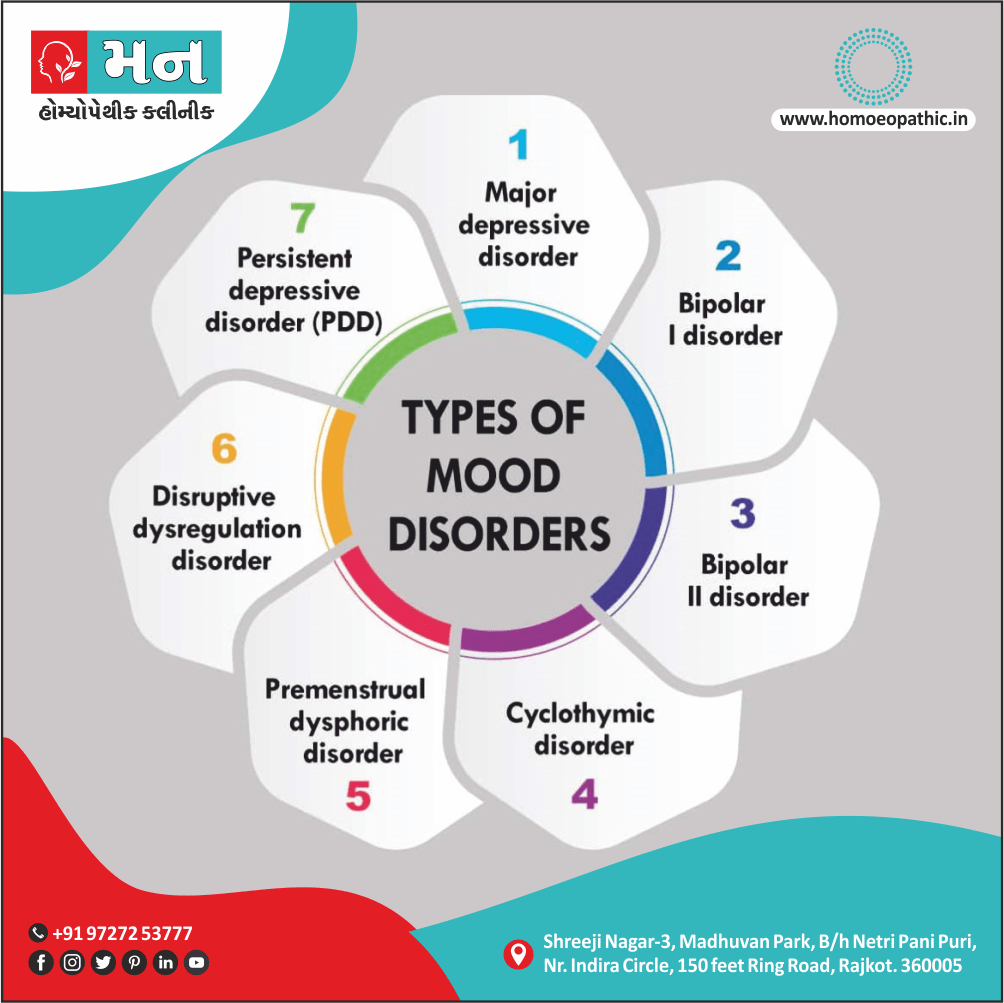
These are the two major types of mood disorders.
- Firstly; Depressive disorders concern feelings of hopelessness and other negative emotions associated with depression. There are varying degrees of problems with depression, ranging from Major Depressive disorder (with several sub-varieties) to chronic cases of depression labeled dysthymia, where a person has a continual low mood for more than 24 months at a time.
- Secondly; Bi-polar disorders include depression – including any of the different varieties of depression but people affected also exhibit manic episodes on the other end of the emotional spectrum. Besides this; Some go back and forth between extremes multiple times very rapidly depending on the degree of the disorder. [3]
Risk Factors
Risk Factors:
- Advanced Age: The old age population is at a higher risk due to age-related physiological changes and increased prevalence of medical conditions.
- Underlying Medical Conditions: Neurological disorders (stroke, Parkinson’s disease, epilepsy, brain tumors, multiple sclerosis), endocrine disorders (hypothyroidism, hyperthyroidism, Cushing’s disease), infections (HIV, syphilis), autoimmune disorders (systemic lupus erythematosus), and nutritional deficiencies (vitamin B12 deficiency) can predispose individuals to OMD.
- Medication Use: Certain medications, such as corticosteroids, antihypertensives, and chemotherapeutic agents, can induce mood disturbances.
- Substance Abuse: Chronic alcohol or drug abuse can damage the brain and increase the risk of OMD.
- Genetic Predisposition: Family history of mood disorders or other psychiatric conditions may increase vulnerability to OMD.
- Environmental Toxins: Exposure to heavy metals or other toxins can affect brain function and contribute to the development of OMD.[5]
Please Note:
- It is crucial to consult with a qualified healthcare professional for any concerns related to OMD or mental health.
- This information is for educational purposes only and should not be considered a substitute for professional medical advice.
Pathogenesis
Pathogenesis
Organic mood disorders arise from disruptions in brain function caused by identifiable medical conditions or substances. The exact mechanisms are complex and vary based on the underlying etiology, but generally involve:
Neurotransmitter Imbalance:
- Many medical conditions and substances can alter the levels or functioning of key neurotransmitters (like serotonin, dopamine, norepinephrine) crucial for mood regulation.
- For example, stroke or Parkinson’s disease may damage brain areas involved in dopamine production, leading to depressive symptoms.
Structural and Functional Brain Changes:
- Brain lesions, tumors, infections, or neurodegenerative diseases can directly damage or disrupt neural circuits crucial for mood control.
- Chronic inflammation associated with some medical conditions can also impact brain function and mood.
Hormonal Dysregulation:
- Conditions like thyroid dysfunction or Cushing’s disease can cause significant hormonal imbalances affecting mood.
- Corticosteroids, often used for treating various medical conditions, can also induce mood changes due to their impact on the hypothalamic-pituitary-adrenal (HPA) axis.
Neurotoxicity and Metabolic Disturbances:
- Exposure to toxins, heavy metals, or certain medications can damage brain cells and lead to mood disturbances.
- Metabolic disorders, like vitamin deficiencies or electrolyte imbalances, can also impair brain function and contribute to mood symptoms.[5]
Pathophysiology
Pathophysiology
The pathophysiology of Organic Mood Disorder (OMD) is complex and multifactorial, involving disruptions in various brain systems and neurochemical pathways. While the precise mechanisms underlying OMD can vary depending on the specific etiology, several key factors contribute to its development:
Direct Brain Insult: OMD often arises due to a direct insult to the brain, such as a stroke, traumatic brain injury, tumor, or neurodegenerative disease. These conditions can disrupt critical brain regions involved in mood regulation, including the prefrontal cortex, limbic system (amygdala, hippocampus), and basal ganglia.
Neurotransmitter Imbalance: Neurotransmitter systems, particularly those involving serotonin, dopamine, norepinephrine, and GABA, play a crucial role in mood regulation. Disruptions in these systems due to underlying medical conditions or their treatments can lead to OMD. For example, Parkinson’s disease, characterized by dopamine depletion, can manifest with depressive symptoms.
Hormonal Dysregulation: Hormonal imbalances, particularly those affecting the hypothalamic-pituitary-adrenal (HPA) axis, can contribute to OMD. Chronic stress, certain medications, and endocrine disorders can disrupt the HPA axis, leading to elevated cortisol levels, which have been linked to depressive symptoms.
Inflammatory Processes: Mounting evidence suggests a role for inflammation in the pathophysiology of mood disorders, including OMD. Chronic inflammation, often associated with medical conditions like autoimmune diseases or infections, can impact brain function and contribute to mood dysregulation.
Genetic Predisposition: While OMD is primarily associated with underlying medical conditions, genetic factors can influence an individual’s susceptibility to developing mood disturbances in the context of brain insult or systemic illness.[5]
Clinical Features
Clinical Features of Organic Mood Disorder
OMD presents with a diverse range of clinical features, reflecting the underlying medical condition and its impact on brain function. The presentation can vary widely, but common clinical features include:
Depressed Mood: The most prominent feature is a persistent feeling of sadness, emptiness, or hopelessness. Individuals may experience a loss of interest or pleasure in previously enjoyed activities (anhedonia), fatigue, and decreased energy levels.
Irritability and Anxiety: OMD can also manifest with increased irritability, restlessness, and anxiety. These symptoms may be particularly prominent in certain medical conditions, such as hyperthyroidism or Cushing’s syndrome.
Cognitive Impairment: Cognitive dysfunction, including difficulties with concentration, memory, and decision-making, is a frequent accompaniment to OMD. The severity of cognitive impairment can range from mild deficits to significant dementia, depending on the underlying cause.
Sleep Disturbances: Sleep problems, such as insomnia or hypersomnia, are common in OMD. These disturbances can further exacerbate mood symptoms and contribute to fatigue and cognitive dysfunction.
Appetite Changes: Changes in appetite, either increased or decreased, can occur in OMD. Weight loss or gain may be observed, particularly in conditions affecting metabolism or hormonal balance.
Psychomotor Changes: Psychomotor agitation or retardation may be present, characterized by restlessness and fidgeting or slowed movements and speech, respectively.
Psychotic Symptoms: In some cases, OMD can be accompanied by psychotic symptoms, such as delusions or hallucinations. These symptoms are more likely to occur in severe cases or in the context of specific medical conditions, such as delirium or dementia.
Fluctuating Course: The course of OMD often fluctuates, with symptoms waxing and waning depending on the underlying medical condition and its treatment. This fluctuation can distinguish OMD from primary mood disorders, which typically follow a more persistent course.[5]
Sign & Symptoms
Sign & Symptoms of Organic Mood Disorders
- Extreme changes in personality
- Prolonged depression
- Easy irritability also agitation
- Extreme aggression
- Extreme anxiety [3]
Clinical Examination
Clinical Examination
The Clinical examinations for Organic Mood Disorder (OMD) involve a comprehensive assessment to identify the underlying medical condition causing the mood disturbance and evaluate its impact on the individual’s cognitive and emotional functioning. The following components are crucial in the clinical examination of OMD:
Thorough Medical History:
- Detailed inquiry into the patient’s current and past medical conditions, including any recent illnesses, surgeries, or hospitalizations.
- Medication review, including prescription drugs, over-the-counter medications, and herbal supplements, to identify potential mood-altering effects.
- Substance use history, including alcohol, tobacco, and illicit drugs.
- Family history of medical and psychiatric conditions.
Mental Status Examination:
- Assessment of the patient’s appearance, behavior, mood, affect, speech, thought process, thought content, perception, cognition, and insight.
- Screening for cognitive impairment using standardized tools like the Mini-Mental State Examination (MMSE) or Montreal Cognitive Assessment (MoCA).
- Evaluation of the severity and duration of mood symptoms, including depressive features.
Physical Examination:
- Complete physical examination to identify any signs of underlying medical conditions, particularly those affecting the nervous system or endocrine system.
- Neurological examination to assess motor function, sensory function, reflexes, and cranial nerves.
Laboratory and Imaging Studies:
- Blood tests to evaluate complete blood count, electrolytes, liver function, kidney function, thyroid function, vitamin B12 and folate levels, and inflammatory markers.
- Other specialized tests depending on the suspected underlying medical condition (e.g., neuroimaging, EEG, lumbar puncture).
Collateral Information:
- Gathering information from family members or caregivers about the patient’s behavior, mood changes, and functional impairment.[5]
Diagnosis
Diagnosis
The diagnosis of Organic Mood Disorder (OMD) involves a comprehensive evaluation to identify the underlying medical condition causing the mood disturbance and to rule out other psychiatric disorders. Here’s the general approach:
Detailed Medical History: A thorough medical history is crucial to identify any current or past medical conditions, medications, or substance use that could contribute to mood symptoms. This includes neurological disorders, endocrine disorders, autoimmune diseases, infections, and any recent surgeries or hospitalizations.
Mental Status Examination: A mental status examination assesses the patient’s current mood, affect, thought processes, cognitive function, and behavior. This helps identify the specific mood disturbance (e.g., depression, mania) and its severity.
Physical Examination: A physical examination may reveal signs of underlying medical conditions that could contribute to OMD. Neurological examination is particularly important to assess any focal deficits or signs of neurodegenerative disease.
Laboratory and Imaging Studies: Blood tests, imaging studies (e.g., MRI, CT scan), and other diagnostic tests may be necessary to identify the underlying medical condition causing the mood disturbance.
Diagnostic Criteria: The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) provides specific criteria for diagnosing OMD. The key features include:
- A prominent and persistent disturbance in mood (e.g., depression, mania, or mixed features).
- Evidence from the history, physical examination, or laboratory findings that the disturbance is the direct pathophysiological consequence of another medical condition.
- The disturbance is not better explained by another mental disorder.
- The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.[6]
Differential Diagnosis
Differential Diagnoses
OMD presents with mood disturbances (depression, mania, or mixed states) that are directly attributable to an underlying medical condition or its treatment. It is essential to differentiate OMD from other psychiatric disorders with similar presentations to ensure appropriate management. The following are key differential diagnoses to consider:
Primary Mood Disorders: Major Depressive Disorder (MDD) and Bipolar Disorder can also manifest with significant mood disturbances. However, in these disorders, the mood symptoms are not directly caused by a medical condition or its treatment. Distinguishing between OMD and primary mood disorders can be challenging, requiring careful evaluation of the patient’s medical history, temporal relationship between mood symptoms and medical conditions, and response to treatment.
Substance-Induced Mood Disorder: Substance use or withdrawal can induce mood disturbances that mimic OMD. A thorough substance use history and toxicological screening are essential to rule out this possibility.
Adjustment Disorder with Depressed Mood: Significant stressors can trigger adjustment disorder, characterized by emotional or behavioral symptoms in response to an identifiable stressor. While adjustment disorder can present with depressed mood, it is typically less severe and persistent than OMD.
Anxiety Disorders: Anxiety disorders, such as generalized anxiety disorder or panic disorder, can sometimes co-occur with mood disturbances, making it challenging to differentiate from OMD. A comprehensive assessment of the patient’s symptoms and their temporal relationship to medical conditions is crucial for accurate diagnosis.
Personality Disorders: Certain personality disorders, such as borderline personality disorder, can present with mood instability and impulsivity, which may overlap with OMD. A thorough evaluation of the patient’s long-term patterns of behavior and functioning is necessary to distinguish between these conditions.[6]
Complications
Complications of Organic Mood Disorder
Organic Mood Disorder (OMD) can lead to various complications that impact an individual’s overall health and well-being. These complications can arise directly from the underlying medical condition, the mood disturbance itself, or the interaction between the two.
Potential Complications of OMD:
- Impaired Cognitive Function: OMD can affect attention, memory, concentration, and decision-making, leading to difficulties in daily functioning and potentially impacting work or academic performance.
- Increased Disability: The combination of physical limitations from the underlying medical condition and the emotional burden of OMD can increase an individual’s overall level of disability, affecting their independence and quality of life.
- Social Isolation and Withdrawal: The emotional distress and potential cognitive impairment associated with OMD can lead to social withdrawal and isolation, further exacerbating mood symptoms and impacting interpersonal relationships.
- Substance Abuse: Individuals with OMD may be at an increased risk for developing substance use disorders as a maladaptive coping mechanism to manage their emotional distress.
- Suicidal Ideation and Behavior: In severe cases, OMD can lead to suicidal thoughts or attempts, particularly when accompanied by feelings of hopelessness and worthlessness.
- Poor Treatment Adherence: The mood disturbance and cognitive difficulties associated with OMD can impact an individual’s ability to adhere to treatment plans for their underlying medical condition, potentially worsening their physical health.
- Increased Mortality Risk: Studies have shown that individuals with OMD, particularly those with comorbid medical conditions, may experience an increased risk of mortality.[5]
Investigations
Investigations of Organic Mood Disorder
The Investigations for Organic Mood Disorder (OMD) aim to identify the underlying medical condition or substance use contributing to the mood disturbance. A comprehensive approach involves a combination of clinical assessment, laboratory tests, and neuroimaging studies.
Clinical Assessment:
- Detailed History: A thorough history focusing on the onset, duration, and severity of mood symptoms, as well as any past or current medical conditions, medications, and substance use is crucial. Particular attention should be given to neurological symptoms, cognitive changes, and any recent head injuries or illnesses.
- Mental Status Examination: This assesses the patient’s current mental state, including mood, affect, thought processes, cognitive function, and insight.
- Physical Examination: A comprehensive physical examination is performed to identify any signs of systemic illness or neurological abnormalities that may be contributing to the mood disorder.
Laboratory Investigations:
- Complete Blood Count (CBC): To assess for anemia, infections, or other blood disorders that can impact mood.
- Electrolyte Panel: To check for electrolyte imbalances, such as hyponatremia or hypercalcemia, which can cause mood disturbances.
- Liver Function Tests (LFTs): To assess liver function as liver disease can affect mood.
- Thyroid Function Tests (TFTs): To evaluate thyroid function as both hypothyroidism and hyperthyroidism can present with mood symptoms.
- Vitamin B12 and Folate Levels: To rule out deficiencies that can contribute to mood disorders.
- Toxicology Screen: To detect any substance use that may be contributing to mood symptoms.
- Other Tests: Additional tests may be ordered based on the patient’s clinical presentation, such as HIV testing, syphilis testing, or autoimmune markers.
Neuroimaging Studies:
- Magnetic Resonance Imaging (MRI): The preferred imaging modality to assess for structural brain abnormalities, such as tumors, strokes, or neurodegenerative changes.
- Computed Tomography (CT) Scan: May be used in emergency situations or when MRI is contraindicated to evaluate for structural brain lesions.
- Electroencephalogram (EEG): To assess brain electrical activity and identify any seizure activity or other abnormalities that may be contributing to mood symptoms.[5]
This concise yet comprehensive textbook provides a practical approach to the diagnosis and management of psychiatric disorders, including OMD. It offers detailed guidance on the clinical assessment and investigations necessary to identify the underlying medical cause of mood disturbance.
Remember, the specific investigations required may vary depending on the patient’s clinical presentation and suspected etiology. A thorough evaluation by a healthcare professional is essential to develop an appropriate diagnostic and treatment plan.
Treatment
Treatment of Organic Mood Disorder
1. Firstly; Management of the underlying organic cause, if treatable.
2. Secondly; Symptomatic management, if the episodes are severe.
For example, for a manic episode, low dose antipsychotic medication (such as risperidone, haloperidol, olanzapine) and/or a mood stabiliser (such as valproate); also for a depressive episode, low dose antidepressants (such as sertraline or mirtazapine).
Antipsychotics are not recommend in patients who have suffered from stroke and/or dementia as the risk of mortality is higher.
Pathological laughter and crying (associated with multiple sclerosis or stroke) can similarly respond to small dose SSRIs or small dose amitriptyline. [1]
Prevention
Prevention of Organic Mood Disorder (OMD)
Given the diverse etiologies of OMD, prevention strategies focus primarily on reducing the risk factors for the underlying medical conditions that can trigger mood disturbances. While some causes are unavoidable, adopting healthy lifestyle choices and proactive healthcare practices can significantly lower the risk of OMD.
Key preventive measures include:
Managing Chronic Medical Conditions: Effectively managing chronic diseases like diabetes, hypertension, heart disease, and autoimmune disorders through medication adherence, regular checkups, and lifestyle modifications can help mitigate their impact on brain health and mood regulation.
Minimizing Head Injury Risk: Wearing protective gear during activities that carry a risk of head injury, such as sports or cycling, can prevent traumatic brain injuries, a potential cause of OMD.
Healthy Lifestyle Choices: Engaging in regular exercise, maintaining a balanced diet, getting adequate sleep, and managing stress effectively can promote overall brain health and resilience, reducing the vulnerability to mood disturbances.
Avoiding Substance Abuse: Excessive alcohol consumption and drug use can damage the brain and increase the risk of OMD. Moderating alcohol intake and avoiding illicit substances is crucial for brain health preservation.
Early Detection and Treatment of Mental Health Issues: Seeking prompt evaluation and treatment for mental health concerns, such as depression or anxiety, even if seemingly unrelated to physical illness, can help prevent the development of OMD.
Regular Health Checkups: Regular medical examinations and screenings can help identify and address underlying medical conditions early on, potentially mitigating their impact on mood and brain function.[7]
Homeopathic Treatment
Homeopathic Treatment of Organic Mood Disorder
Homeopathy offers several remedies for managing the symptoms of Organic Mood Disorder (OMD), aiming to address the individual’s unique presentation and underlying cause. While conventional medicine primarily focuses on treating the underlying medical condition, homeopathic treatment aims to restore balance and stimulate the body’s innate healing capabilities.
Commonly used homeopathic remedies for OMD include:
- Ignatia: Often indicated for mood swings, grief, and emotional turmoil.
- Natrum Muriaticum: Helpful for individuals experiencing depression, sadness, and withdrawal.
- Aurum Metallicum: Can be beneficial for deep despair, hopelessness, and suicidal thoughts.
- Pulsatilla: Suitable for individuals with changeable moods, weepiness, and a need for consolation.
- Sepia: May be helpful for indifference, irritability, and aversion to loved ones.
- Staphysagria: Indicated for suppressed anger, resentment, and feelings of humiliation.
- Nux Vomica: Beneficial for individuals experiencing irritability, impatience, and oversensitivity.
Important Considerations:
- Individualized Treatment: Homeopathic treatment is highly individualized, based on the patient’s specific symptoms, temperament, and underlying condition.
- Professional Consultation: It is crucial to consult a qualified homeopathic practitioner for proper diagnosis and selection of the most appropriate remedy.
- Complementary Approach: Homeopathy can be used as a complementary therapy alongside conventional medical treatment for OMD.
Disclaimer:
- Limited Scientific Evidence: The effectiveness of homeopathy for OMD is not fully supported by scientific evidence.
- Not a Substitute for Conventional Treatment: Homeopathy should not be considered a replacement for conventional medical treatment for the underlying cause of OMD.
- Professional Guidance: Always consult a qualified healthcare professional for proper diagnosis and treatment of OMD.
Diet & Regimen
Diet & Regimen for Organic Mood Disorder
While a specific diet cannot cure Organic Mood Disorder (OMD), adopting healthy eating habits and maintaining a balanced lifestyle can contribute significantly to improving overall well-being and potentially alleviating some symptoms.
Dietary recommendations:
- Nutrient-rich foods: Focus on whole, unprocessed foods, including plenty of fruits, vegetables, whole grains, lean proteins, and healthy fats. These provide essential nutrients for brain health and function.
- Omega-3 fatty acids: These healthy fats found in fatty fish (salmon, tuna), flaxseeds, chia seeds, and walnuts have been linked to improved mood and cognitive function.
- Vitamin D: Sunlight exposure and dietary sources like fatty fish and fortified foods can help ensure adequate vitamin D levels, which play a role in mood regulation.
- B vitamins: Found in whole grains, leafy greens, and legumes, B vitamins are crucial for neurotransmitter production and mood stability.
- Limit processed foods: Highly processed foods, sugary drinks, and excessive caffeine can negatively impact mood and overall health.
- Hydration: Drink plenty of water throughout the day to maintain optimal brain function and overall well-being.
Lifestyle recommendations:
- Regular exercise: Engaging in regular physical activity, even moderate amounts, can help improve mood, reduce stress, and promote better sleep.
- Stress management: Techniques like meditation, deep breathing exercises, and yoga can help manage stress and anxiety, which can exacerbate OMD symptoms.
- Adequate sleep: Aim for 7-8 hours of quality sleep each night, as sleep deprivation can negatively impact mood and cognitive function.
- Social connection: Maintain strong relationships with friends and family, as social support can be crucial for emotional well-being.
- Avoidance of harmful substances: Limit or avoid alcohol and recreational drugs, as these can worsen OMD symptoms and interact negatively with medications.[8]
This comprehensive textbook explores the integration of conventional and complementary therapies for various health conditions, including mood disorders. It provides valuable insights into the role of diet, lifestyle, and mind-body practices in promoting overall well-being and managing symptoms associated with OMD.
Important Note:
Always consult with a qualified healthcare professional before making any significant changes to your diet or lifestyle, especially if you have an existing medical condition or are taking medications. Individual needs and tolerances may vary, and a personalized approach is essential for optimal results.
Remember that these recommendations are general guidelines, and working with a healthcare professional or registered dietitian can help tailor a plan that suits your specific needs and preferences.
Do’s and Don'ts
Do’s:
- Seek Professional Help: The most crucial step is to consult a healthcare professional, preferably a psychiatrist or neurologist specializing in mood disorders. They can conduct a thorough evaluation, diagnose the underlying cause, and create a personalized treatment plan.
- Adhere to Treatment: Once a treatment plan is established, it’s essential to follow it diligently. This may include medications, therapy, or a combination of both. Consistency is key to managing symptoms and preventing relapses.
- Prioritize Healthy Lifestyle: Adopting a healthy lifestyle can significantly improve overall well-being and mood stability. Focus on regular exercise, balanced nutrition, adequate sleep, stress management techniques, and avoidance of harmful substances like alcohol and drugs.
- Build a Support System: Connect with loved ones, support groups, or mental health professionals for emotional support and encouragement. Sharing experiences and feelings can be incredibly helpful in managing OMD.
- Practice Self-Care: Make time for activities that bring you joy and relaxation, such as hobbies, spending time in nature, or listening to music. Taking care of your physical and emotional needs is vital for managing OMD.
- Educate Yourself: Learn about OMD, its causes, symptoms, and treatment options. Understanding the condition can empower you to make informed decisions and actively participate in your recovery.
Don’ts:
- Self-Diagnose or Self-Treat: OMD requires professional evaluation and diagnosis. Avoid self-diagnosing or self-treating, as it can lead to delays in proper treatment and potentially worsen the condition.
- Ignore Symptoms: Don’t dismiss or downplay changes in mood, even if they seem subtle. Early detection and intervention are crucial for managing OMD effectively.
- Isolate Yourself: While it’s normal to experience periods of withdrawal, avoid isolating yourself completely. Social interaction and support are vital for emotional well-being and recovery.
- Compare Yourself to Others: Everyone’s experience with OMD is unique. Avoid comparing your journey to others, as this can lead to feelings of inadequacy or discouragement. Focus on your progress and individual needs.
- Give Up: Managing OMD can be challenging, but it’s important to persevere. With proper treatment, support, and self-care, individuals with OMD can experience significant improvement and regain control over their lives.
Terminology
Terminology of Organic Mood Disorder
Here are some key terminologies and their meanings commonly used in articles about Organic Mood Disorder (OMD):
Organic Mood Disorder (OMD): This is the overarching term referring to mood disturbances (like depression or mania) that are directly caused by an underlying medical condition or its treatment.
Mood Disturbance: A significant change in a person’s emotional state, typically involving either a depressed mood or an elevated/irritable mood.
Medical Condition: Any physical illness or disease process, ranging from neurological disorders (like stroke or Parkinson’s) to systemic illnesses (like infections or hormonal imbalances).
Neurotransmitter: Chemical messengers in the brain that facilitate communication between neurons; imbalances in neurotransmitters like serotonin, dopamine, and norepinephrine are often implicated in OMD.
Inflammation: The body’s immune response to injury or infection; chronic inflammation has been linked to mood disorders, including OMD.
Comorbidity: The presence of two or more medical conditions or disorders in the same individual; OMD often coexists with other psychiatric conditions like anxiety disorders.
Psychopharmacology: The study of how medications affect mood, behavior, and cognition; relevant to OMD as medications are often used to manage both the underlying medical condition and the mood disturbance itself.
Psychotherapy: A form of treatment for mental health conditions involving talking with a trained mental health professional; can be beneficial in OMD to address emotional distress and develop coping mechanisms.
Prognosis: The likely course or outcome of a disease or condition; in OMD, the prognosis often depends on the severity and treatability of the underlying medical cause.
Remission: A period of time when the symptoms of a disease or condition are reduced or absent; the goal of treatment in OMD is often to achieve and maintain remission of mood symptoms.
Homoeopathic Terminology & Its Meaning
Vital Force: The fundamental energy or life force that animates the body and maintains health, according to homeopathic principles. Imbalance or disruption of the vital force is believed to lead to disease, including OMD.
Miasm: Inherited or acquired predisposition to certain disease patterns, including mental and emotional disturbances. Homeopaths believe that understanding a patient’s miasm is crucial in selecting the most effective remedy for OMD.
Totality of Symptoms: The complete picture of a patient’s physical, mental, and emotional symptoms, including their unique characteristics and modalities (factors that make symptoms better or worse). This information is vital for homeopathic remedy selection.
Materia Medica: Detailed descriptions of homeopathic remedies, their properties, and the symptoms they are known to produce. Homeopaths consult materia medica to confirm remedy selection and understand its potential effects.
Potentization: The process of diluting and succussing (vigorously shaking) a homeopathic remedy to increase its therapeutic power while reducing its potential toxicity.
Constitutional Remedy: A remedy that matches a patient’s overall physical and mental constitution, addressing their underlying susceptibility to disease and promoting long-term healing.
Understanding these terminologies can facilitate your comprehension of homeopathic approaches to OMD and help you engage in informed discussions with homeopathic practitioners.
References
References
- A Short Textbook of Psychiatry by Niraj Ahuja / Ch 3.
- http://apps.who.int/classifications/icd10/browse/2016/en#/F00-F09.
- Ganguli, H. C. (1982). Mental disorders in India: An analysis of epidemiological studies. Indian Journal of Social Work, 43(3), 403-414.
- Reddy, M. V., & Chandrashekar, C. R. (1998). Prevalence of mental and behavioural disorders in India: A meta-analysis. Indian Journal of Psychiatry, 40(2), 119-126.
- Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry, 11th Edition, Benjamin J. Sadock, Virginia A. Sadock, Pedro Ruiz, 2015, Wolters Kluwer.
- Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, American Psychiatric Association, 2013.
- The American Psychiatric Association Publishing Textbook of Psychosomatic Medicine and Consultation-Liaison Psychiatry, 3rd Edition, James L. Levenson, M.D., and Jon Streltzer, M.D., 2016, American Psychiatric Association Publishing.
- Integrative Medicine, 4th Edition, David Rakel, 2018, Elsevier.
Also Search As
Organic Mood Disorder Also Search As
Online Search Engines:
- Use specific keywords: Combine keywords like "homeopathy," "organic mood disorder," "treatment," and "remedies."
- Try different search terms: Also search using synonyms, like "homeopathic treatment for mood disorders caused by medical conditions" or "homeopathic approach to depression with underlying medical cause."
- Use advanced search operators: Employ quotation marks for exact phrases, the minus sign to exclude irrelevant results, and the tilde for synonyms.
Homeopathic Websites and Journals:
- Visit reputable homeopathic websites: Explore websites of recognized homeopathic organizations, colleges, or journals.
- Search their article archives: Look for relevant articles within their databases using the search bar or browsing by category.
- Subscribe to newsletters or updates: Stay informed about the latest homeopathic research and articles by subscribing to their newsletters or updates.
Homeopathic Libraries and Bookstores:
- Visit local homeopathic libraries or bookstores: Access specialized collections of books and journals on homeopathy.
- Seek assistance from librarians or staff: They can guide you to relevant resources and articles specific to OMD.
- Browse through homeopathic materia medica: Explore the sections on mental and emotional symptoms to identify potential remedies for OMD.
Homeopathic Practitioner Consultations:
- Consult a qualified homeopathic practitioner: Discuss your interest in homeopathic approaches to OMD.
- Ask for recommendations: Inquire about any relevant articles or research they may be aware of.
- Request access to their library or resources: Some practitioners may have collections of homeopathic articles they can share.
Social Media and Online Forums:
- Join homeopathic groups and forums: Participate in online communities discussing homeopathy, seeking recommendations and insights from experienced practitioners or patients.
- Follow homeopathic organizations on social media: Stay updated on recent articles and research shared through their social media channels.
Important Considerations:
- Critical Evaluation: Approach all information with a critical mindset, assessing the credibility of sources and authors.
- Consult a Professional: Always consult a qualified healthcare professional for diagnosis and treatment of OMD, including exploring homeopathic options alongside conventional treatment if desired.
- Research Limitations: Recognize that research on homeopathy for OMD might be limited compared to conventional medicine, but valuable insights can still be found through dedicated exploration.
By employing these strategies and maintaining a discerning approach, individuals can uncover valuable homeopathic articles on OMD to enhance their understanding and explore potential complementary treatment options.
Frequently Asked Questions (FAQ)
How is OMD diagnosed?
Diagnosis involves a comprehensive medical and psychiatric evaluation, including a review of medical history, physical examination, and potentially laboratory tests or imaging studies to identify the underlying medical condition.
What is Organic Mood Disorder?
They are characterized by those that involve the moods or emotions of a person that are changed due to a physiological problem with the brain or nervous system.
What causes Organic Mood Disorder?
- Drugs
- Endocrine disorders
- CNS disorders
- Post-viral illnesses
- Deficiencies
Give the 5 signs of Organic Mood Disorder?
- Extreme changes in personality
- Prolonged depression
- Easy irritability and agitation
- Extreme aggression
- Extreme anxiety
What are the types of Organic Mood Disorder?
- Depressive disorders
- Bi-polar disorders
Is homeopathic treatment safe for OMD?
When administered by a qualified homeopathic practitioner, homeopathic remedies are generally considered safe and have minimal side effects.However, it’s crucial to inform your practitioner about any existing medical conditions or medications you’re taking.
Can homeopathy help with Organic Mood Disorder (OMD)?
Homeopathy offers a holistic approach to managing OMD symptoms by addressing the individual’s unique constitution and emotional state. While research on its effectiveness is limited, many individuals report benefits from homeopathic treatment alongside conventional medical care.
Can homeopathy replace conventional treatment for Organic Mood Disorder?
Homeopathy should not replace conventional medical treatment. It can be used as a complementary approach alongside conventional care.
Are there any risks or side effects associated with homeopathic treatment for Organic Mood Disorder?
Homeopathic remedies are generally considered safe when used correctly. However, it’s essential to work with a qualified practitioner.
Which homeopathic remedies are commonly used for OMD?
Homoeopathic Medicines for Organic Mood Disorder
Remedies like Ignatia, Natrum Muriaticum, Aurum Metallicum, Pulsatilla, Sepia, Staphysagria, and Nux Vomica are frequently prescribed, but the specific choice depends on the individual’s symptoms and underlying medical condition.
