Paget’s Disease of Bone (PDB)
Definition:
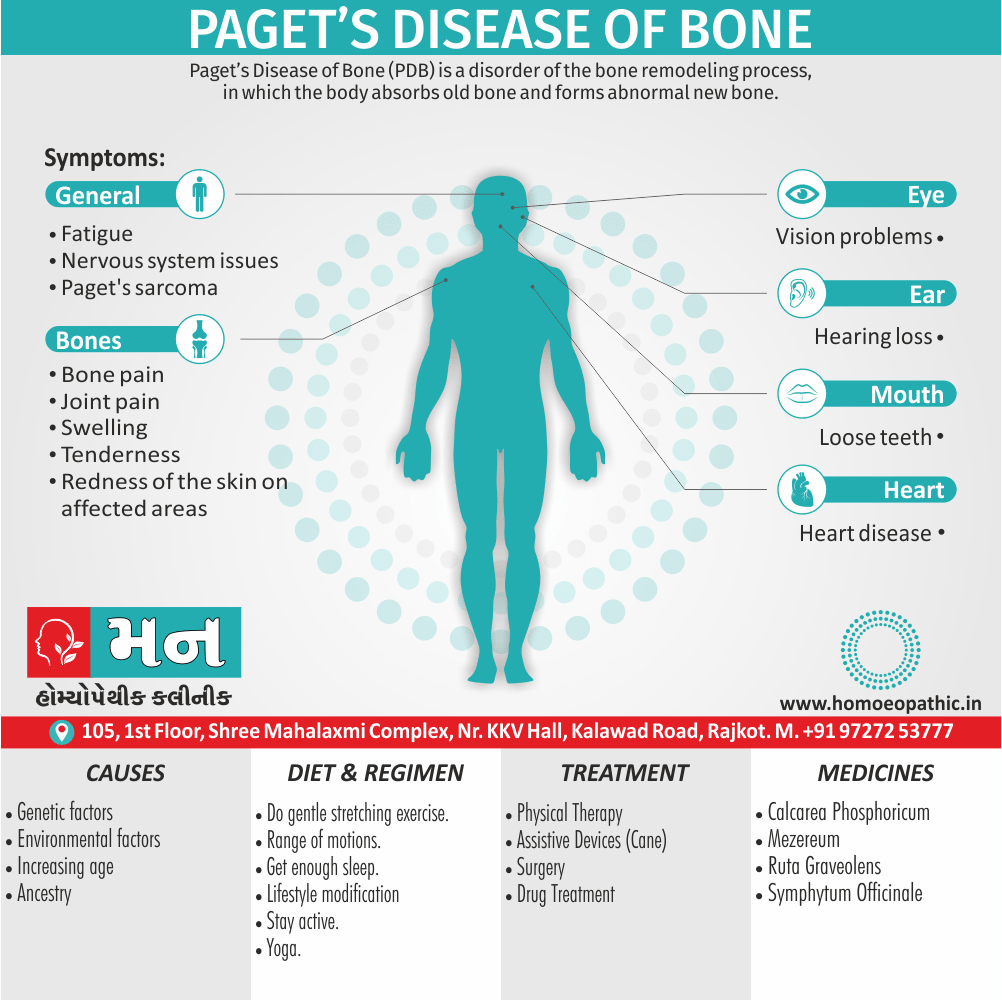
Paget’s Disease of Bone (PDB) is a chronic bone disorder characterized by abnormal bone remodeling.
Paget’s disease of bone also known by the following synonyms:
- Osteitis deformans This term literally translates to “deforming inflammation of bone” and reflects the historical understanding of the disease as an inflammatory process. However, we now know that inflammation is not a major feature of Paget’s disease.
While "Paget’s disease of bone" is the most common and preferred term, you might encounter "osteitis deformans" in older medical literature.
Frequently Asked Questions (FAQ)
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
Paget’s Disease of Bone (PDB) is the second most common bone disease after osteoporosis. In healthy bone, a process called remodeling continuously removes old bone and replaces it with new bone. In PDB, this process is disrupted, leading to the formation of new bone that is weak, enlarged, and prone to fractures.
Epidemiology
Epidemiology
Paget’s Disease of Bone (PDB) is relatively uncommon in India compared to Western countries. However, its prevalence appears to be increasing in recent years.
Prevalence:
While large-scale epidemiological studies on PDB in India are limited, several smaller studies and case reports suggest that the prevalence is significantly lower than in Western populations. Some estimates place the prevalence at around 0.1% to 0.5% of the population, compared to 1.5% to 8.3% in Western countries. However, it’s important to note that these numbers may underestimate the true prevalence due to underdiagnosis and reporting.
References:
- A study published in ResearchGate in 2008 titled "Does Paget’s Disease Exist in India?: A series of 21 patients" reported a prevalence of 2.8 cases per 1 million persons in India.[1]
- Another study published in ResearchGate in 2009 titled "Paget’s disease in India" analyzed 48 cases and found that the disease often presents with polyostotic involvement (affecting multiple bones).[2]
Factors influencing prevalence:
Several factors might contribute to the lower prevalence of PDB in India, including:
- Genetic predisposition: Paget’s disease is more common in people of European descent and less common in Asian populations, including those in India.
- Environmental factors: While the exact cause of PDB is unknown, environmental factors may play a role, and these may differ between India and Western countries.
- Awareness and diagnosis: Lack of awareness among healthcare professionals and the general public, as well as limited access to diagnostic facilities, may contribute to underdiagnosis of PDB in India.
It’s important to note that research on Paget’s disease in India is ongoing, and a better understanding of the epidemiology and risk factors is crucial for effective prevention and management strategies.
Causes
Causes
This refers to the initiating factors that trigger a disease process.
- Examples of causes include:
- Pathogens: Viruses, bacteria, fungi, parasites (infectious diseases)
- Genetic mutations: Inherited or spontaneous changes in genes (genetic diseases)
- Environmental factors: Toxins, radiation, nutritional deficiencies
- Lifestyle choices: Smoking, unhealthy diet, lack of exercise (contributing factors)
Types
Types
Number of Bones Affected:
- Monostotic: Involves a single bone. This is less common, accounting for about 15% of cases.
- Polyostotic: Involves multiple bones. This is more common, accounting for about 85% of cases.
Stage of Disease:
- Active: Characterized by increased bone turnover (formation and breakdown), leading to bone pain, deformity, and increased risk of fractures.
- Inactive: Characterized by decreased bone turnover, with less pain and deformity.
Location of Affected Bones:
PDB can affect any bone, but it’s most commonly found in the:
- Pelvis
- Spine
- Skull
- Long bones of the legs (femur, tibia)
Book References:
Several books provide detailed information on Paget’s disease of bone, including its classification and clinical features:
- Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism (9th Edition): This comprehensive textbook offers a chapter dedicated to Paget’s disease, covering its epidemiology, etiology, pathophysiology, clinical manifestations, diagnosis, and treatment.[3]
- Endocrine and Metabolic Diseases: A Practical Approach: This book provides a practical guide to the diagnosis and management of endocrine and metabolic disorders, including Paget’s disease.[4]
- The Paget’s Foundation Introduction to Paget’s Disease of Bone: This book is a patient-friendly guide to Paget’s disease, providing information on symptoms, diagnosis, treatment options, and living with the condition.[5]
These references can help you understand the various ways Paget’s disease of bone can present and be classified. It’s important to consult with your doctor for accurate diagnosis and personalized treatment recommendations.
Risk Factors
Risk Factors
Several factors can increase your risk of developing Paget’s disease of bone:
- Age: The risk of Paget’s disease increases with age. People older than 50 are most likely to develop the condition.
- Sex: Men are slightly more likely to develop Paget’s disease than women.
- National origin: Paget’s disease is more common in people of Anglo-Saxon descent, particularly those from England, Scotland, central Europe, and Greece. It’s also more common in countries settled by European immigrants. It’s uncommon in Scandinavia and Asia.
- Family history: If you have a close relative with Paget’s disease, you’re more likely to develop the condition. This suggests a possible genetic link.[6]
Please Note: The information provided here is for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.
Pathogenesis
Pathogenesis
Paget’s disease of bone is characterized by abnormal bone remodeling, leading to structurally disorganized and weakened bone. The process involves three main phases:
- Osteolytic Phase: Excessive osteoclastic activity leads to increased bone resorption. Osteoclasts in Paget’s disease are often larger and contain more nuclei than normal.
- Mixed Phase: Both osteoclastic and osteoblastic activity occur. The osteoblasts attempt to compensate for the bone loss by rapidly laying down new bone, but this new bone is haphazard and structurally weak, often described as "woven bone."
- Osteosclerotic Phase: The osteoblastic activity dominates, leading to thickened, but still structurally abnormal, bone. This bone is more prone to fractures and deformities.
Key Factors in Pathogenesis:
- Genetic Predisposition: Multiple genes have been implicated in Paget’s disease, including SQSTM1 and VCP. Familial cases suggest an autosomal dominant inheritance pattern in some families.
- Environmental Triggers: Viral infections, particularly paramyxoviruses, have been suggested as possible triggers for the disease, but this remains controversial.
- Osteoclast Dysfunction: The primary driver of Paget’s disease is abnormal osteoclast function. These cells become hyperactive and over-responsive to signals that promote bone resorption.
Note: The specific page numbers regarding Paget’s disease may vary slightly between different editions of the book.
Remember: Paget’s disease is a complex disorder with multiple contributing factors. The exact interplay of these factors is still under investigation. [7]
Pathophysiology
Pathophysiology
Paget’s disease of bone (PDB) is characterized by excessive and abnormal bone remodeling. The process involves three phases:
Initial Osteolytic Phase: This phase is marked by increased osteoclastic activity. The osteoclasts are abnormally large and have numerous nuclei. They cause excessive bone resorption, leading to lytic lesions and focal areas of bone weakness.
Mixed Osteolytic-Osteoblastic Phase: In this phase, there’s a compensatory increase in osteoblastic activity in an attempt to repair the damage. However, the new bone formation is haphazard and disorganized, leading to the characteristic "mosaic" pattern of woven and lamellar bone. The bone marrow is replaced by highly vascular fibrous tissue.
Final Osteosclerotic Phase: In this phase, osteoblastic activity continues, leading to excessive bone deposition and thickening of the affected bone. The new bone is structurally weak and prone to fractures.
Key Points:
- Etiology: The exact cause of PDB is unknown. However, both genetic and environmental factors are thought to play a role.
- Genetic: Familial clustering is seen in about 15-30% of cases. Mutations in the SQSTM1 gene have been identified in some families.
- Environmental: Viral infections (particularly paramyxoviruses) have been implicated, but the evidence is not conclusive.
- Clinical Features: The clinical manifestations depend on the extent and location of the affected bone.
- Bone Pain: The most common symptom is bone pain, which is often described as deep and aching.
- Bone Deformity: Enlargement and bowing of the affected bones can occur.
- Fractures: The abnormal bone is prone to fractures.
- Neurological Complications: Nerve compression can occur if the skull or spine is involved.
- High-Output Cardiac Failure: In severe cases, the increased vascularity of the affected bone can lead to high-output cardiac failure.
- Osteosarcoma: A rare but serious complication is malignant transformation to osteosarcoma.[7].
Clinical Features
Clinical Features
Paget’s disease of bone (PDB) is a chronic disorder characterized by focal areas of increased and disorganized bone turnover. This results in bone that is structurally abnormal, enlarged, and weakened, making it susceptible to fractures and deformities. The clinical presentation of PDB varies depending on the extent and location of the skeletal involvement.
Common Clinical Features
Bone pain: This is the most frequent presenting symptom, and it can range from mild to severe. The pain is often described as deep, aching, and worse at night or with weight-bearing activities. The affected bones may also be tender to palpation.
Bone deformities: Enlargement and bowing of the long bones, especially the femur and tibia, are common. The skull may also enlarge, leading to a characteristic "leontiasis ossea" appearance. Other deformities may include kyphosis, coxa vara, and genu varum.
Fractures: The weakened bone in PDB is prone to fractures, which can occur with minimal trauma or even spontaneously.
Neurologic complications: Nerve compression can occur due to bone enlargement or deformities, leading to symptoms such as hearing loss, facial palsy, and spinal cord compression.
Secondary osteoarthritis: Joint pain and stiffness can develop due to abnormal joint mechanics caused by the bone deformities.
High-output cardiac failure: In rare cases, extensive PDB can lead to increased blood flow to the affected bones, causing the heart to work harder and potentially leading to heart failure.
Osteosarcoma: A rare but serious complication of PDB is the development of osteosarcoma, a primary bone cancer.
Other potential features:
- Warmth over affected bone: Due to increased vascularity.
- Headache and hearing loss: If the skull is involved.
- Skin changes: Overlying skin may be warm and flushed.
- Increased alkaline phosphatase: A blood test marker of bone turnover.[8]
Sign & Symptoms
Signs and Symptoms
Key Symptoms
- Bone pain: This is the most common symptom and can vary in intensity and location. It’s often described as a deep, aching pain.
- Deformities: Affected bones may become enlarged, bowed, or misshapen, particularly in the skull, spine, pelvis, and legs.
- Fractures: Weakened bones are more susceptible to fractures, even with minor injuries.
- Joint pain and stiffness: Paget’s disease can lead to osteoarthritis in nearby joints.
- Neurological symptoms: Nerve compression can occur if the skull or spine is affected, leading to headaches, hearing loss, or numbness and tingling in the extremities.
Additional Symptoms
- Increased warmth over affected bones: Due to increased blood flow in areas of active bone remodeling.
- Fatigue: May occur due to the body’s increased effort to remodel bone.
- High blood calcium levels (hypercalcemia): Rarely, if the disease is widespread and active.[6]
Note: The signs and symptoms of Paget’s disease of bone can vary depending on the location and extent of the affected bones. Some individuals may have no symptoms at all, while others may experience significant pain and disability.
Clinical Examination
Clinical Examination of Paget’s Disease of Bone
Patients with Paget’s disease may be asymptomatic or present with a variety of symptoms depending on the affected bones. Common presenting complaints include:
- Bone Pain: This is the most common symptom and can be localized to the affected bone or referred. The pain may be constant or intermittent, dull or aching, and may worsen with activity or at night.
- Bone Deformity: Enlargement and bowing of long bones, especially the tibia and femur, can occur. Skull involvement can lead to an enlarged head (leontiasis ossea) and hearing loss.
- Fractures: The abnormal bone in Paget’s disease is more susceptible to fractures.
- Neurological Complications: Nerve compression can occur due to bone enlargement, leading to symptoms such as hearing loss, facial palsy, or spinal cord compression.
- Secondary Osteoarthritis: Joint degeneration can occur in joints adjacent to affected bones.
Physical Examination Findings:
Affected Bone:
- Warmth: Increased vascularity in the affected bone can lead to warmth and increased skin temperature over the area.
- Tenderness: The bone may be tender to palpation.
- Enlargement: Enlarged bones may be visible or palpable, especially in the skull, tibia, or femur.
- Deformity: Bowing of long bones or other deformities may be apparent.
Neurological Examination:
- Cranial Nerves: Assess for hearing loss, facial palsy, or other cranial nerve deficits if the skull is involved.
- Sensory & Motor Function: Evaluate for sensory changes, muscle weakness, or other neurological deficits if spinal cord or nerve compression is suspected.
Joint Examination:
- Range of Motion: Assess for decreased range of motion and crepitus in joints adjacent to affected bones.
Additional Considerations:
- Cardiovascular: High-output heart failure can occur in severe cases due to increased vascularity in affected bones.
- Laboratory Findings:
- Elevated Alkaline Phosphatase: This is a hallmark of Paget’s disease and reflects increased bone turnover.
- Normal Calcium and Phosphate: Serum calcium and phosphate levels are usually normal.
- Elevated Urine Hydroxyproline: This reflects increased bone resorption.
Remember:
- The clinical examination is just one part of the diagnostic process for Paget’s disease.
- Imaging studies (X-rays, bone scans) are crucial for confirming the diagnosis and assessing the extent of bone involvement.
- It is essential to rule out other conditions that can mimic Paget’s disease, such as metastatic bone disease or primary bone tumors.[3]
Diagnosis
Diagnosis of Paget’s Disease of Bone
The diagnosis of Paget’s Disease of Bone (PDB) involves a combination of clinical presentation, laboratory tests, and imaging studies:
Clinical Presentation:
- Bone pain (most common symptom)
- Skeletal deformities (e.g., enlarged skull, bowing of legs)
- Pathological fractures
- Hearing loss (if skull involved)
- Neurological symptoms (if spine or skull involved)
Laboratory Tests:
- Elevated serum alkaline phosphatase (ALP) – a marker of increased bone turnover
- Normal calcium and phosphate levels (usually)
- Elevated urine markers of bone resorption (e.g., N-telopeptide, C-telopeptide)
Imaging Studies:
- X-rays: Characteristic findings include osteolytic (bone destruction) and osteosclerotic (bone thickening) areas, bone enlargement, and deformities.
- Bone scan: Shows increased uptake in affected areas, helpful for identifying extent of disease.[6]
Important Considerations:
- Asymptomatic patients: PDB is often discovered incidentally on X-rays or blood tests done for other reasons.
- Differential Diagnoses: Other conditions that can mimic PDB include bone metastases, osteomyelitis, and primary bone tumors.
- Early Diagnosis and Management: Early diagnosis and appropriate management are crucial to prevent complications such as fractures, deformities, and neurological problems.
Differential Diagnosis
Differential Diagnoses for Paget’s Disease of Bone
Osteoarthritis:
- While PDB can cause joint pain, osteoarthritis is a more common cause, particularly in older individuals.
- In osteoarthritis, joint space narrowing and osteophyte formation are typical imaging findings, whereas in PDB, the bone itself is enlarged and has a disorganized appearance.
Metastatic Bone Disease:
- Bone pain and elevated alkaline phosphatase levels are seen in both PDB and metastatic bone disease.
- Imaging findings can sometimes overlap, but metastatic disease often presents with multiple lytic or sclerotic lesions, while PDB typically involves a single bone or a few contiguous bones with a characteristic mixed lytic and sclerotic pattern.
Primary Bone Tumors:
- Certain primary bone tumors, such as osteosarcoma or giant cell tumor, can cause bone pain and localized bone enlargement, mimicking PDB.
- Biopsy and histopathological examination are essential to differentiate these conditions.
Fibrous Dysplasia:
- This benign bone disorder can cause bone pain, deformity, and fractures, especially in young individuals.
- Radiographically, fibrous dysplasia typically shows a "ground-glass" appearance, distinct from the mixed lytic-sclerotic pattern seen in PDB.
Osteoporosis:
- Although both PDB and osteoporosis can lead to fractures, osteoporosis typically causes diffuse bone loss with decreased bone density on imaging, whereas PDB shows localized areas of increased bone turnover and abnormal bone remodeling.
Hyperparathyroidism:
- Elevated serum calcium and parathyroid hormone levels are seen in hyperparathyroidism, which can cause bone pain, fractures, and osteolytic lesions.
- Unlike PDB, hyperparathyroidism usually affects multiple bones and shows a more generalized pattern of bone resorption on imaging.[6]
Important Note:
- It’s essential to perform a thorough clinical evaluation, including a detailed history, physical examination, and appropriate imaging studies, to arrive at the correct diagnosis.
- In some cases, a bone biopsy may be necessary to confirm the diagnosis of Paget’s disease or rule out other conditions.
Complications
Complications of Paget’s Disease of Bone
Bone Fractures and Deformities: Paget’s disease weakens bones, making them more prone to fractures. The excessive bone growth can also lead to deformities, such as bowing of the legs or enlargement of the skull.
Osteoarthritis: The abnormal bone remodeling in Paget’s disease can place stress on nearby joints, leading to the development of osteoarthritis, a painful degenerative joint disease.
Neurological Problems: When Paget’s disease affects the skull or spine, it can compress nerves, causing pain, numbness, tingling, or even paralysis. Hearing loss can also occur if the bones of the inner ear are involved.
Heart Failure: In rare cases, the increased blood flow to the affected bones can put a strain on the heart, potentially leading to heart failure.
Bone Cancer (Osteosarcoma): While rare, Paget’s disease can increase the risk of developing a type of bone cancer called osteosarcoma.[6]
Investigations
Investigations for Paget’s Disease of Bone
Blood Tests:
- Serum Alkaline Phosphatase (ALP):
- This is the most sensitive marker for Paget’s disease.
- Elevated levels indicate increased bone turnover.
- The degree of elevation often correlates with the extent and activity of the disease.
- Serum Calcium:
- Usually normal, unless the patient is immobilized or has concurrent hyperparathyroidism.
- Urinary N-telopeptide (NTx) and C-telopeptide (CTx):
- These are markers of bone resorption and may be elevated in active Paget’s disease.
- Serum Alkaline Phosphatase (ALP):
Imaging Studies:
- X-rays:
- Often the first imaging test performed.
- Can show characteristic findings like bone enlargement, cortical thickening, lytic lesions, and osteosclerosis.
- May also reveal complications like fractures, osteoarthritis, and bone deformities.
- Bone Scan:
- Highly sensitive for detecting areas of increased bone turnover.
- Useful for assessing the extent and activity of the disease, especially in patients with normal ALP levels.
- Can also help identify complications like fractures and bone tumors.
- X-rays:
Other Investigations:
- Bone Biopsy:
- Rarely needed for diagnosis but may be considered in atypical presentations or to rule out other bone diseases.
- Histologic examination shows characteristic mosaic pattern of lamellar bone.
- Computed Tomography (CT) or Magnetic Resonance Imaging (MRI):
- May be helpful for evaluating specific complications, such as spinal stenosis, nerve compression, or bone tumors.
- Bone Biopsy:
Interpretation of Findings
- Elevated ALP with normal calcium suggests Paget’s disease.
- Characteristic X-ray findings confirm the diagnosis.
- Bone scan shows increased uptake in affected areas.
- Bone biopsy, if performed, shows mosaic pattern of bone.
Important Considerations
- Asymptomatic patients with incidentally detected elevated ALP should be investigated further to confirm or rule out Paget’s disease.
- The extent of investigations may vary depending on the patient’s symptoms and clinical presentation.
- A multidisciplinary approach involving rheumatologists, endocrinologists, and orthopedic surgeons may be needed for optimal management of Paget’s disease and its complications.[8]
Treatment
Treatment of Paget’s Disease of Bone
Primary Treatment Modality: Bisphosphonates
- Mechanism: These drugs inhibit osteoclast activity, thereby reducing bone resorption and turnover, leading to a decrease in pain and normalization of bone markers (alkaline phosphatase).
- Administration:
- Oral: Alendronate, risedronate
- Intravenous: Zoledronic acid, pamidronate
Choice of Bisphosphonate and Regimen
- Asymptomatic patients: Often no treatment is necessary, but if alkaline phosphatase is significantly elevated, or there’s a risk of complications, oral bisphosphonates may be considered.
- Symptomatic patients: Intravenous zoledronic acid is often the preferred initial therapy due to its efficacy and ease of administration.
- Monitoring: Alkaline phosphatase levels and bone-specific markers are checked periodically to assess treatment response.
Other Treatment Options:
- Calcitonin: A less commonly used option for patients who cannot tolerate bisphosphonates. It is given by injection or nasal spray.
- Surgery: May be necessary in cases of severe bone deformity, fractures, or nerve compression.
- Pain Management: Analgesics and nonsteroidal anti-inflammatory drugs (NSAIDs) may be used for pain relief.
Important Considerations:
- Calcium and Vitamin D Supplementation: Adequate intake is crucial for optimal bone health.
- Dental Care: Patients should maintain good oral hygiene and have any necessary dental work done before starting bisphosphonate therapy due to the rare risk of osteonecrosis of the jaw.
- Monitoring for Complications: Regular follow-up with a physician is essential to monitor for complications such as hearing loss, fractures, and neurological symptoms.
Key Points:
- Bisphosphonates are the mainstay of treatment for Paget’s disease of bone.
- Treatment decisions are individualized based on the patient’s symptoms, disease severity, and potential complications.
- Regular monitoring and follow-up are crucial for optimizing treatment outcomes and managing potential complications.[8]
Prevention
Prevention of Paget’s Disease of Bone
Unfortunately, the exact cause of Paget’s disease of bone remains unknown, which makes primary prevention challenging. There are no specific lifestyle changes or preventative measures that are guaranteed to prevent the onset of this condition. However, some recommendations can promote overall bone health and potentially reduce the risk of complications associated with Paget’s disease if it does develop.
Maintain a Healthy Lifestyle:
- A balanced diet rich in calcium and vitamin D is essential for bone health.
- Regular weight-bearing exercise can also help maintain bone density and strength.
- Avoiding smoking and excessive alcohol consumption is crucial for overall health, including bone health.
Early Detection and Management:
- While there is no way to prevent Paget’s disease itself, early diagnosis and management can significantly improve outcomes. If you have a family history of Paget’s disease or experience any symptoms such as bone pain, fractures, or deformities, consult your doctor for evaluation.[3]
Homeopathic Treatment
Homeopathic Treatment for Paget’s Disease of Bone
Homeopathy offers a holistic approach to managing Paget’s disease of bone by focusing on the individual’s unique symptoms and constitutional tendencies. While conventional medicine primarily aims to control pain and slow the progression of the disease, homeopathy aims to stimulate the body’s inherent healing capabilities and address the underlying imbalances that contribute to the condition.
Key Considerations:
Individualization: Homeopathic treatment is highly individualized. A detailed case analysis considers the patient’s physical, mental, and emotional symptoms, as well as their medical history and family background.
Constitutional Remedy: The goal is to find the patient’s "constitutional remedy," a single medicine that matches their overall symptom picture and underlying predisposition.
Symptom Management: Homeopathic remedies can also be used to target specific symptoms such as bone pain, deformities, or neurological complications.
Potential Homeopathic Remedies:
Calcarea carbonica:
This remedy is often considered for patients with Paget’s disease who experience bone pain, deformities, and a tendency towards obesity.
Calcarea fluorica:
This remedy is indicated for patients with bone hardening, exostoses (bony growths), and joint stiffness.
Phosphorus:
This remedy may be helpful for patients with bone pain, weakness, and a tendency towards anxiety and restlessness.
Silicea:
This remedy is often considered for patients with brittle bones, deformities, and a tendency towards coldness and sensitivity.
Symphytum:
This remedy is known for its bone-healing properties and may be used to support fracture healing in Paget’s disease.
Important Considerations:
- Consultation with a Homeopath: It is essential to consult a qualified homeopath for a proper diagnosis and individualized treatment plan.
- Conventional Treatment: Homeopathy can be used as a complementary therapy alongside conventional treatment for Paget’s disease.
- Ongoing Management: Homeopathic treatment is often an ongoing process that requires regular follow-ups and adjustments as the patient’s condition evolves.
Disclaimer: Homeopathy is a complementary therapy and should not be considered a substitute for conventional medical treatment for Paget’s disease. It is crucial to consult with your doctor before starting any new treatment, including homeopathy.
Remember:
- Homeopathy offers a personalized approach to managing Paget’s disease.
- Consult a qualified homeopath for a comprehensive assessment and individualized treatment plan.
- Use homeopathy as a complementary therapy alongside conventional medical care.
Diet & Regimen
Diet and Regimen for Paget’s Disease of Bone
A balanced diet and healthy lifestyle are essential components in managing Paget’s Disease of Bone, alongside medical treatment. While there’s no specific diet to cure the disease, certain recommendations help maintain bone health and manage symptoms.
Dietary Recommendations
- Calcium & Vitamin D: Adequate intake is crucial for bone health. Include dairy products, leafy greens, fortified foods, and consider supplements if dietary intake is insufficient.
- Protein: Supports muscle and bone health. Choose lean sources like poultry, fish, beans, and lentils.
- Fruits & Vegetables: Provide essential vitamins, minerals, and antioxidants. Aim for a variety of colorful options.
- Limit Sodium: High sodium intake can lead to calcium loss. Avoid processed foods and excessive salt.
- Hydration: Adequate water intake is essential for overall health, including bone health.
Lifestyle Recommendations
- Weight-bearing Exercise: Helps maintain bone density and strength. Consult your doctor for suitable activities like walking, dancing, or tai chi.
- Avoid Smoking & Excessive Alcohol: These habits negatively impact bone health and overall well-being.
- Manage Pain: Use heat therapy, gentle stretching, or relaxation techniques to alleviate pain. Consult your doctor for appropriate pain medication if needed.
- Assistive Devices: Use canes, walkers, or braces as recommended by your doctor to improve mobility and prevent falls.
- Regular Checkups: Monitor the progression of the disease and adjust treatment as needed. [3]
Do’s and Don'ts
Do’s and Don’ts of Paget’s Disease of Bone
Managing Paget’s disease involves a combination of medical treatment and lifestyle modifications. Here are some key do’s and don’ts to help you navigate the condition effectively:
Do’s
- Consult Your Doctor Regularly: Regular check-ups are vital to monitor disease progression, adjust medication as needed, and address any emerging complications.
- Follow Medical Advice: Adhere to your doctor’s prescribed treatment plan, including medication and any recommended physical therapy or assistive devices.
- Maintain a Healthy Diet: Prioritize a balanced diet rich in calcium and vitamin D, crucial for bone health.
- Exercise Regularly: Engage in weight-bearing exercises as recommended by your doctor or physical therapist to maintain bone strength and improve mobility.
- Manage Pain: Use heat therapy, gentle stretching, or relaxation techniques. If needed, discuss appropriate pain medication with your doctor.
- Use Assistive Devices: Utilize canes, walkers, or braces as recommended to improve mobility and prevent falls.
- Prevent Falls: Take precautions to avoid falls, such as removing tripping hazards at home and using grab bars in bathrooms.
- Stay Informed: Educate yourself about the disease, its potential complications, and treatment options.
- Communicate: Discuss any concerns or questions you have with your healthcare team.
Don’ts
- Ignore Symptoms: Don’t dismiss persistent bone pain, deformities, or other symptoms. Seek medical attention for prompt diagnosis and treatment.
- Self-Treat: Avoid self-medicating or relying solely on alternative therapies without consulting your doctor.
- Overexert: Avoid high-impact activities or exercises that could put undue stress on affected bones.
- Smoke or Drink Excessively: These habits can worsen bone health and negatively impact overall well-being.
- Neglect Mental Health: Paget’s disease can affect emotional well-being. Don’t hesitate to seek support or counseling if you’re feeling anxious or depressed.
Additional Considerations
- Protect Your Joints: If Paget’s disease affects your joints, be mindful of protecting them from excessive strain.
- Listen to Your Body: Pay attention to your body’s signals and adjust your activity levels as needed.
- Be Patient: Managing Paget’s disease is a long-term process. Be patient with yourself and your body’s healing journey.
Terminology
Terminology
- Paget’s Disease of Bone: A chronic bone disorder characterized by abnormal bone remodeling, leading to enlarged, weakened, and deformed bones.
- Osteoclasts: Cells responsible for breaking down old bone tissue.
- Osteoblasts: Cells responsible for building new bone tissue.
- Bone Remodeling: The continuous process of bone breakdown and rebuilding.
- Osteolytic Phase: The initial phase of Paget’s disease where osteoclasts become overactive, leading to excessive bone breakdown.
- Mixed Phase: The phase where both osteoclasts and osteoblasts are overactive, resulting in rapid, chaotic bone turnover and the formation of disorganized bone.
- Osteosclerotic Phase: The final phase where osteoblasts dominate, leading to the formation of dense, but weak and brittle, bone.
- Bisphosphonates: A class of drugs that inhibit osteoclast activity and slow down bone breakdown.
- Calcitonin: A hormone that can also help reduce bone breakdown.
- Pain Management: Strategies to reduce pain associated with Paget’s disease, including medication, physical therapy, and assistive devices.
- Bone Deformities: Changes in bone shape, such as bowing of the legs or enlargement of the skull.
- Osteoarthritis: Joint pain and inflammation that can occur when Paget’s disease affects bones near joints.
- Neurological Complications: Nerve compression or damage that can occur when Paget’s disease affects the skull or spine.
- Osteosarcoma: A rare but serious complication of Paget’s disease, where bone cancer develops in affected areas.
References
References
- A study published in ResearchGate in 2008 titled "Does Paget’s Disease Exist in India?: A series of 21 patients" reported a prevalence of 2.8 cases per 1 million persons in India.
- ResearchGate in 2009 titled "Paget’s disease in India" analyzed 48 cases and found that the disease often presents with polyostotic involvement (affecting multiple bones)
- Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism (9th Edition)
- Endocrine and Metabolic Diseases: A Practical Approach.
- The Paget’s Foundation Introduction to Paget’s Disease of Bone.
- Kelley’s Textbook of Rheumatology, 11th Edition, Gary S. Firestein, Ralph Budd, Sherine Gabriel, Iain McInnes, James O’Dell, 2021, Elsevier.
- Robbins & Cotran Pathologic Basis of Disease, 10th Edition, Vinay Kumar, Abul K. Abbas, Jon C. Aster, 2021, Elsevier.
- Harrison’s Principles of Internal Medicine, 21st Edition, by Dennis L. Kasper, Anthony S. Fauci, Stephen L. Hauser, Dan L. Longo, J. Larry Jameson, and Joseph Loscalzo. Published in 2022 by McGraw Hill.
Also Search As
Paget’s Disease Of Bone Also Search As
Online Search Engines:
Use specific keywords:
- "Homeopathy Paget’s Disease of Bone"
- "Homeopathic treatment for Paget’s Disease"
- "Homeopathic remedies for Paget’s"
Include additional terms to narrow down your search:
- "Case studies"
- "Research articles"
- "Clinical trials"
Homeopathic Websites and Databases:
National Center for Homeopathy (NCH): The NCH website features a searchable database of articles and resources related to homeopathy.
Homeopathy Plus: This website offers a collection of articles and research papers on various health conditions, including Paget’s Disease.
The American Institute of Homeopathy: Their website provides information about homeopathy and may have links to relevant articles.
Homeopathic Journals and Publications:
The Journal of the American Institute of Homeopathy
Homeopathy: The Journal of the Faculty of Homeopathy
Simillimum: The Journal of the Homeopathic Academy of Naturopathic Physicians
Social Media and Online Forums:
Homeopathic groups and pages: Join online communities focused on homeopathy to ask questions and find articles shared by other members.
Homeopathic forums: Participate in discussions and ask for recommendations for articles on Paget’s Disease of Bone.
Additional Tips:
Consult a Homeopath: Ask your homeopathic practitioner for recommendations for articles or research on Paget’s Disease and homeopathy.
Visit a Homeopathic Library: Some libraries may have specialized collections on homeopathy with books and journals related to Paget’s Disease.
Use Advanced Search Options: Refine your search results by using advanced search operators such as quotation marks for exact phrases or using the minus sign to exclude certain terms.
By utilizing these resources and search strategies, you can find valuable homeopathic articles and information regarding the treatment and management of Paget’s Disease of Bone.
What is Paget's disease of bone?
Paget’s disease of bone is a chronic disorder that disrupts the normal cycle of bone renewal and repair. In affected areas, bone breaks down too quickly and is replaced with new bone that is abnormally large, weak, and brittle.
What are the symptoms of Paget's disease?
Many people with Paget’s disease have no symptoms. When symptoms occur, the most common complaint is bone pain. Other symptoms can include bone deformities, fractures, hearing loss, and neurological problems.
Homoeopathic Medicines For Paget's Disease Of Bone?
Homoeopathic Medicines For Paget’s Disease Of Bone
- Calc Flour
- Symphytum
- Calc Phos
- Hecla Lava
- Ruta.
What causes Paget's disease?
The exact cause of Paget’s disease is unknown. It is believed to be a combination of genetic and environmental factors, possibly including a viral infection.
What are the treatment options for Paget's disease?
Treatment aims to relieve pain and prevent complications. Medications, such as bisphosphonates and calcitonin, can help slow down bone breakdown. Surgery may be necessary to correct deformities, repair fractures, or replace joints.
How does homeopathy work in the context of Paget's disease?
Homeopathy is based on the principle of "like cures like," using highly diluted substances to trigger the body’s healing response. Remedies are selected based on the individual’s specific symptoms and the overall picture of their health.
How long does it take to see results with homeopathic treatment for Paget's disease?
The response to homeopathic treatment can vary depending on the individual and the severity of the condition. It is important to be patient and consistent with treatment. Some individuals may experience improvement in symptoms within weeks or months, while others may take longer.
What lifestyle changes can support homeopathic treatment for Paget's disease?
Maintaining a healthy weight, engaging in regular exercise (as tolerated), getting adequate calcium and vitamin D, and avoiding smoking and excessive alcohol consumption can all support bone health and complement homeopathic treatment.
