Pregnancy induced hypertension
Definition
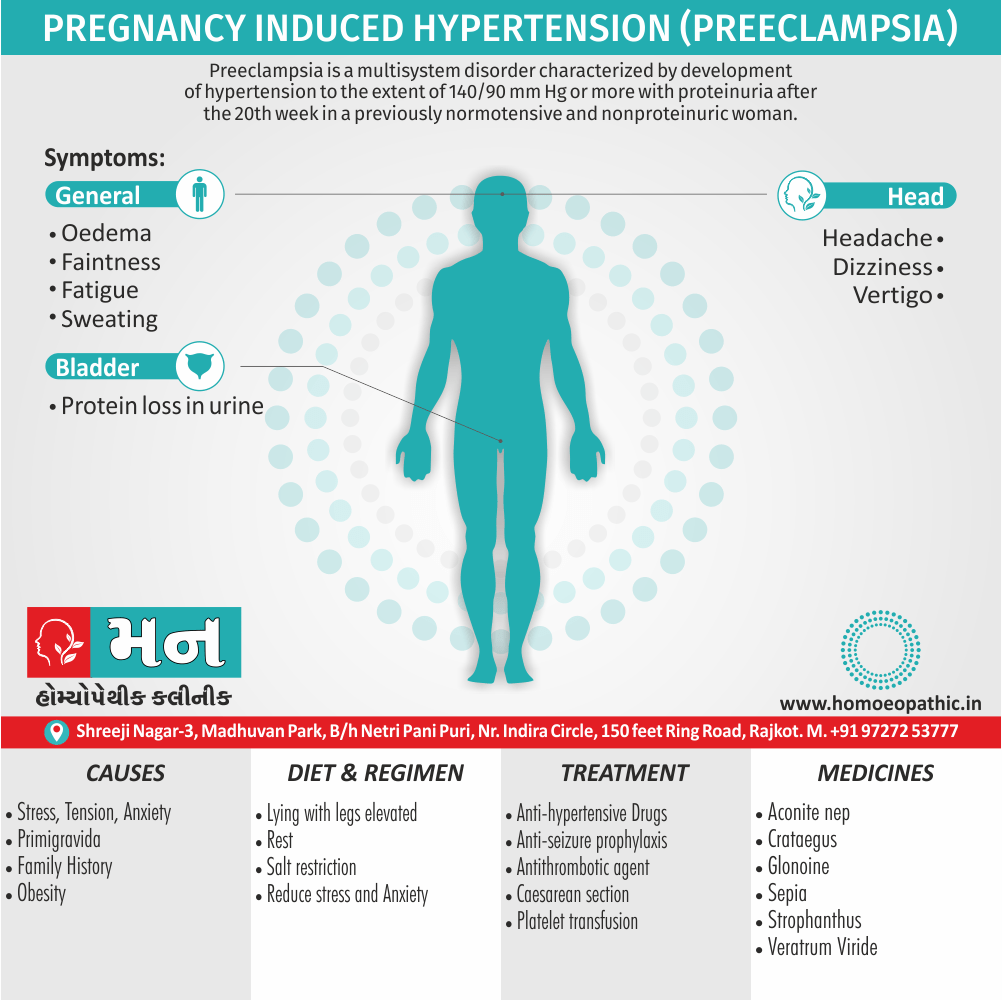
Pregnancy induced hypertension/ Pre-eclampsia is a multisystem disorder of unknown etiology characterized by development of hypertension to the extent of 140/90 mm Hg or more with proteinuria after the 20th week in a previously normotensive and nonproteinuric woman.[1]
Here are some synonyms for pregnancy-induced hypertension:
- Gestational hypertension
- Toxemia of pregnancy (older term, less commonly used now)
- Gestational hypertension without significant proteinuria
It’s important to note that gestational hypertension is not the same as preeclampsia. Preeclampsia is a more serious condition that includes high blood pressure along with protein in the urine (proteinuria) or other signs of organ damage.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Pregnancy induced hypertension
Hypertension is one of the common medical complications of pregnancy and contributes significantly to maternal and perinatal morbidity and mortality. Hypertension is a sign of an underlying pathology, which may be pre-existing or appears for the first-time during pregnancy.
The identification of this clinical entity and effective management plays a significant role in the outcome of pregnancy, both for the mother and the baby. Some amount of edema is common in a normal pregnancy. Edema has been excluded from the diagnostic criteria unless it is pathological.
The preeclamptic features may appear even before the 20th week as in cases of hydatidiform mole and acute polyhydramnios. The term, “Pregnancy-induced hypertension (PIH)” is defined as the hypertension that develops as a direct result of the gravid state.
Pregnancy induced hypertension includes
(i) Gestational hypertension,
(ii) Preeclampsia and
(iii) Eclampsia.[1]
Epidemiology
Epidemiology of Pregnancy induced hypertension
Pregnancy-induced hypertension (PIH), encompassing gestational hypertension, pre-eclampsia, and eclampsia, poses a significant health risk in India. While global estimates suggest PIH affects 5-8% of pregnancies, with pre-eclampsia occurring in roughly 10%, Indian studies reveal varying prevalence rates.
- This study observed a lower PIH prevalence of 4.4%, with pre-eclampsia at 1.3% and eclampsia at 0.5%.
- The authors attribute these variations to factors like racial differences, socioeconomic status, parity, and age.
- They also highlight that other Indian studies report pre-eclampsia incidence between 8-10% and eclampsia at 0.71%.[5]
- This study found a PIH prevalence of 6.5% among Kashmiri women.
- They identified older maternal age and higher pre-pregnancy BMI as risk factors.[6]
Other Studies
These studies, along with others, underscore the variability in PIH prevalence across different regions and populations within India. Factors such as socioeconomic conditions, access to healthcare, and genetic predisposition likely contribute to these differences. It’s crucial to recognize that even with varying prevalence rates, PIH remains a major contributor to maternal and fetal morbidity and mortality in India, necessitating continued research and targeted interventions to improve pregnancy outcomes.
Causes
Causes of Pregnancy induced hypertension
Generally, the exact cause of preeclampsia likely involves several factors. In detail, Experts believe it begins in the placenta — the organ that nourishes the fetus throughout pregnancy. Besides this, Early in a pregnancy, new blood vessels develop and evolve to supply oxygen and nutrients to the placenta.
In women with preeclampsia, these blood vessels don’t seem to develop or work properly. All in all, Problems with how well blood circulates in the placenta may lead to the irregular regulation of blood pressure in the mother.
Other high blood pressure disorders during pregnancy
Preeclampsia is one high blood pressure (in other words; hypertension) disorder that can occur during pregnancy. Other disorders can happen, too:
Gestational hypertension
It is high blood pressure that begins after 20 weeks without problems in the kidneys or other organs. Some women with gestational hypertension may develop preeclampsia.
Chronic hypertension
It is high blood pressure that was present before pregnancy or that occurs before 20 weeks of pregnancy. High blood pressure that continues more than three months after a pregnancy also is called chronic hypertension.
Chronic hypertension with superimposed preeclampsia
It occurs in women diagnosed with chronic high blood pressure before pregnancy, who then develop worsening high blood pressure and protein in the urine or other health complications during pregnancy.[4]
Types
Types of Preeclampsia of Pregnancy induced hypertension
Mild Preeclampsia:
- Characterized by elevated blood pressure (≥140/90 mmHg) and proteinuria (≥300mg in a 24-hour urine collection) after 20 weeks of gestation.
- May present with mild symptoms or be asymptomatic.
Severe Preeclampsia:
- Involves higher blood pressure readings (≥160/110 mmHg) and significant proteinuria (≥5g in a 24-hour urine collection).
- Associated with organ dysfunction, affecting the liver, kidneys, brain, or blood clotting.
- Symptoms may include severe headaches, visual disturbances, upper abdominal pain, nausea, vomiting, and decreased urine output.
Early-Onset Preeclampsia:
- Occurs before 34 weeks of gestation.
- Often associated with severe features and increased risk of maternal and fetal complications.
- May necessitate preterm delivery.
Late-Onset Preeclampsia:
- Develops after 34 weeks of gestation.
- While potentially less severe, it still requires close monitoring and management.
Superimposed Preeclampsia:
- Occurs in women with pre-existing chronic hypertension.
- Presents with new-onset proteinuria or worsening hypertension after 20 weeks of gestation.[7]
Key Takeaway
Understanding the different types of preeclampsia is crucial for healthcare providers to assess the severity of the condition, predict potential complications, and tailor management strategies to optimize maternal and fetal outcomes.
Remember: If you suspect you have any signs or symptoms of preeclampsia, seek immediate medical attention. Early diagnosis and management are key to preventing serious complications.
Risk Factors
Risk factor of Pregnancy induced hypertension
Conditions that are linked to a higher risk of preeclampsia include:
- Preeclampsia in a previous pregnancy
- Being pregnant with more than one baby
- Chronic high blood pressure (hypertension)
- Type 1 or type 2 diabetes before pregnancy
- Kidney disease
- Autoimmune disorders
- Use of in vitro fertilization
- First pregnancy with current partner
- Obesity
- Family history of preeclampsia
- Maternal age of 35 or older
- Complications in a previous pregnancy
- More than 10 years since previous pregnancy [4]
Pathogenesis
Pathogenesis of Preeclampsia
Abnormal Placentation:
- Inadequate trophoblast invasion and remodeling of the spiral arteries lead to reduced placental perfusion.
- This results in placental ischemia and hypoxia, triggering the release of various factors that contribute to the maternal systemic response.
Maternal Systemic Inflammatory Response:
- Placental ischemia releases inflammatory mediators, oxidative stress molecules, and anti-angiogenic factors into the maternal circulation.
- This triggers a systemic inflammatory response and oxidative stress, leading to endothelial dysfunction.
Endothelial Dysfunction:
- Damage to the endothelium, the lining of blood vessels, results in vasoconstriction, increased vascular permeability, and platelet activation.
- This contributes to hypertension, proteinuria, and other clinical manifestations of preeclampsia.[7]
Key Takeaway
While the exact cause of preeclampsia remains elusive, understanding the key steps in its pathogenesis is crucial for developing effective preventive and therapeutic strategies. Ongoing research aims to unravel the precise mechanisms involved and identify potential targets for intervention.
Remember: Preeclampsia is a serious condition that can have significant consequences for both mother and baby. If you’re pregnant, it’s important to attend regular prenatal checkups and report any concerning symptoms to your healthcare provider.
Pathophysiology
Pathophysiology
- While the question as to why the syndrome occurs still remains unsolved, the pathological changes are well documented, especially in severe preeclampsia or in eclampsia.
- Central to today’s explanations are impaired placental development, with defective trophoblast invasion into the spiral arteries and gradual reduction in placental perfusion.
- This leads to the release of substances in the maternal circulation which cause a generalized dysfunction of endothelial cells.
- This produced generalized vasospasm with increased vascular permeability and can be associated with an intravascular activation of the coagulation cascade.
Uteroplacental bed:
- There are increased evidences of premature aging of the placenta. Areas of occasional acute red infarcts and white infarcts are visible on the maternal surface of the placenta.
- Villi: Syncytial degeneration, increased syncytial knots, marked proliferation of cytotrophoblast, thickening of the basement layer, and proliferative endarteritis are evident in varying degrees. In preeclampsia, the normal endovascular invasion of cytotrophoblast into the spiral arteries fails to occur beyond decidua-myometrial junction.
- As a result, the musculoelastic media in the myometrial segment remains responsive to vasoconstrictor stimuli resulting in decreased blood flow. There is acute atherosis of spiral arteries with obliteration of lumen.
- Intervillous circulation: The blood flow is impaired to the extent of about one-third, secondary to the changes in the maternal blood vessels.
- This results in placental changes, anatomical and functional, which are responsible for fetal jeopardy.[1]
Kidney:
- The changes are conspicuous in the glomerulus which becomes enlarged. Endothelial cells swell up and fibrin-like deposits occur in the basement membrane.
- The lumen may be occluded. Interstitial cells in between the capillaries proliferate. There is associated spasm of the afferent glomerular arterioles.
- Patchy areas of damage of the tubular epithelium due to anoxia are evident. The net effects are reduced renal blood flow and glomerular filtration rate (25%), and impaired tubular reabsorption or secretory function.
- Recovery is likely to be complete following delivery. In severe cases, intense anoxia may produce extensive arterial thrombosis leading to bilateral renal cortical necrosis.
Blood vessels:
- There is intense vasospasm. Circulation in the vasa vasorum is impaired leading to damage of the vascular walls, including the endothelial integrity.
Liver:
- Periportal hemorrhagic necrosis of the liver occurs due to thrombosis of the arterioles.
- The necrosis starts at the periphery of the lobule. There may be subcapsular hematoma.
- Hepatic insufficiency seldom occurs because of the reserve capacity and regenerative ability of liver cells.
- Liver function tests are especially abnormal in women with HELLP syndrome.
HELLP Syndrome:
- This is an acronym for Hemolysis (H), Elevated Liver enzymes (EL) and Low Platelet count (LP) (70 IU/L, LDH >600 IU/L) and bilirubin (>1.2 mg/dL).
- There may be subcapsular hematoma formation (which is diagnosed by CT scan) and abnormal peripheral blood smear.
- Eventually liver may rupture to cause sudden hypotension, due to hemoperitoneum.[1]
Clinical Features
Clinical Features of Preeclampsia:
Hypertension:
- New-onset or worsening hypertension after 20 weeks of gestation.
- Blood pressure readings typically ≥140/90 mmHg.
Proteinuria:
- Presence of protein in the urine.
- Usually ≥300mg in a 24-hour urine collection or a protein/creatinine ratio ≥0.3.
Additional Symptoms:
- Severe headaches
- Visual disturbances (blurred vision, flashing lights, temporary vision loss)
- Upper abdominal pain (often right-sided)
- Nausea or vomiting
- Decreased urine output
- Sudden weight gain or swelling (edema), particularly in the face, hands, or feet
- Shortness of breath
Severe hypertension:
- Blood pressure readings ≥160/110 mmHg.
Significant proteinuria:
- ≥5g in a 24-hour urine collection.
End-organ dysfunction:
- Elevated liver enzymes
- Decreased kidney function
- Low platelet count (thrombocytopenia)
- Pulmonary edema
- Neurological symptoms (seizures, altered mental status)[7]
Sign & Symptoms
Sign & Symptoms
The defining feature of preeclampsia is high blood pressure, proteinuria, or other signs of damage to the kidneys or other organs. You may have no noticeable symptoms. The first signs of preeclampsia are often detected during routine prenatal visits with a health care provider.
Along with high blood pressure, preeclampsia signs and symptoms may include:
- Excess protein in urine (proteinuria) or other signs of kidney problems
- Decreased levels of platelets in blood (thrombocytopenia)
- Increased liver enzymes that indicate liver problems
- Severe headaches
- Changes in vision, including temporary loss of vision, blurred vision or light sensitivity
- Shortness of breath, caused by fluid in the lungs
- Pain in the upper belly, usually under the ribs on the right side
- Nausea or vomiting
- Weight gain and swelling (edema) are typical during healthy pregnancies.
- However, sudden weight gain or a sudden appearance of edema — particularly in your face and hands — may be a sign of preeclampsia. [4]
Clinical Examination
Clinical Examination:
Vital Signs:
- Blood Pressure: Accurate measurement using a properly sized cuff is crucial. Multiple readings may be necessary to establish a baseline and assess for variability.
- Pulse: Assess for tachycardia, which may be present in severe preeclampsia or associated with complications.
- Respiratory Rate: Evaluate for tachypnea, which could indicate pulmonary edema or other respiratory issues.
- Temperature: Check for fever, which might suggest an underlying infection.
General Appearance:
- Edema: Assess for the presence and extent of edema, particularly in the face, hands, feet, and ankles.
- Mental Status: Evaluate for any signs of altered mental status, such as confusion, agitation, or lethargy, which may indicate cerebral involvement.
Abdominal Examination:
- Fundal Height: Measure to assess fetal growth and estimate gestational age.
- Fetal Heart Rate: Auscultate or use electronic fetal monitoring to evaluate fetal well-being.
- Uterine Tone: Assess for any uterine tenderness or contractions, which could suggest placental abruption or preterm labor.
- Liver Size and Tenderness: Palpate the liver to assess for enlargement or tenderness, which may indicate hepatic involvement.
Neurological Examination:
- Deep Tendon Reflexes: Evaluate for hyperreflexia or clonus, which may indicate increased central nervous system irritability.
- Visual Fields: Assess for visual disturbances or scotomas.
Additional Assessments:
- Urine Dipstick: Check for proteinuria.
- Weight: Monitor for sudden weight gain, which may suggest fluid retention.
This comprehensive textbook provides detailed guidance on the clinical examination of women with preeclampsia, emphasizing the importance of a systematic and thorough assessment to identify potential complications and guide appropriate management.[7]
Diagnosis
Diagnosis
A diagnosis of preeclampsia happens if you have high blood pressure after 20 weeks of pregnancy and at least one of the following findings:
- Protein in your urine (proteinuria), indicating an impaired kidney
- Other signs of kidney problems
- A low blood platelet count
- Elevated liver enzymes showing an impaired liver
- Fluid in the lungs (pulmonary edema)
- New headaches that don’t go away after taking pain medication
- New vision disturbances
High blood pressure
- A blood pressure reading has two numbers. The first number is the systolic pressure, a measure of blood pressure when the heart is contracting.
- The second number is the diastolic pressure, a measure of blood pressure when the heart is relaxed.
- In pregnancy, high blood pressure is diagnosed if the systolic pressure is 140 millimeters of mercury (mm Hg) or higher or if the diastolic pressure is 90 mm Hg or higher.
- A number of factors can affect your blood pressure. If you have a high blood pressure reading during an appointment, your health care provider will likely take a second reading four hours later to confirm a diagnosis of high blood pressure.
Additional tests
- If you have high blood pressure, your health care provider will order additional tests to check for other signs of preeclampsia:
- Blood tests- A blood sample analyzed in a lab can show how well the liver and kidneys are working. Blood tests can also measure the amount of blood platelets, the cells that help blood clot.
- Urine analysis- Your health care provider will ask you for a 24-hour urine sample or a single urine sample to determine how well the kidneys are working.
- Foetal ultrasound- Your primary care provider will likely recommend close monitoring of your baby’s growth, typically through ultrasound. The images of your baby created during the ultrasound exam allow for estimates of the baby’s weight and the amount of fluid in the uterus (amniotic fluid).
- Nonstress test or biophysical profile- A nonstress test is a simple procedure that checks how your baby’s heart rate reacts when your baby moves. A biophysical profile uses an ultrasound to measure your baby’s breathing, muscle tone, movement and the volume of amniotic fluid in your uterus.[4]
Differential Diagnosis
Differential Diagnosis
- Lupus nephritis
- Superimposed preeclampsia
- Hemolysis
- Elevated liver enzymes, low platelets syndrome
- Catastrophic APS
- Hepatorenal syndrome
Complications
Complications
The Complications of preeclampsia may include:
- Fetal growth restriction
- Abruptio placenta
- DIC
- Acute renal failure
- Severe ascites
- Pulmonary edema
- Pleural effusions
- Cerebral edema
- Laryngeal edema
- Retinal detachment
- Subcapsular liver hematoma
- ARDS
- Sepsis, and death
- Preterm birth
- Placental abruption
- Eclampsia
Other Complications
- HELLP syndrome- HELLP stands for hemolysis (the destruction of red blood cells), elevated liver enzymes and low platelet count. This severe form of preeclampsia affects several organ systems. HELLP syndrome is life-threatening to the mother and baby, and it may cause lifelong health problems for the mother.
- Other organ damage- Preeclampsia may result in damage to the kidneys, liver, lung, heart, or eyes, and may cause a stroke or other brain injury. The amount of injury to other organs depends on how severe the preeclampsia is.
- Cardiovascular disease-Having preeclampsia may increase your risk of future heart and blood vessel (cardiovascular) disease. The risk is even greater if you’ve had preeclampsia more than once or you’ve had a preterm delivery.[1][4]
Investigations
Investigations :
Blood Pressure Monitoring:
Regular blood pressure measurements are crucial for identifying hypertension and assessing its severity.
Ambulatory blood pressure monitoring may be helpful in certain cases to evaluate blood pressure variability and nocturnal dipping.
Urine Analysis:
Proteinuria Assessment:
24-hour urine collection for protein quantification is considered the gold standard.
Spot urine protein/creatinine ratio can provide a rapid assessment.
Other Urine Tests:
Dipstick analysis for blood, nitrites, and leukocytes to rule out urinary tract infection.
Microscopic examination for red blood cells and casts.
Blood Tests:
Complete Blood Count (CBC): Assess for anemia, thrombocytopenia (low platelet count), and signs of infection.
Liver Function Tests: Evaluate for elevated liver enzymes, which may indicate hepatic involvement.
Renal Function Tests: Assess serum creatinine and blood urea nitrogen (BUN) levels to evaluate kidney function.
Coagulation Studies: Assess for abnormalities in coagulation parameters, which may suggest increased risk of bleeding or clotting.
Uric Acid: Elevated levels may be associated with preeclampsia and increased risk of adverse outcomes.
Other Biomarkers: Research is ongoing to identify additional biomarkers that may aid in the diagnosis and prediction of preeclampsia severity.
Fetal Assessment:
Ultrasound: Evaluate fetal growth, amniotic fluid volume, and placental morphology.
Doppler Studies: Assess blood flow in the umbilical artery and other fetal vessels to evaluate placental function and fetal well-being.
Fetal Monitoring: Non-stress test and biophysical profile may be used to assess fetal health and identify any signs of distress.
This comprehensive textbook provides a thorough overview of the various investigations used in the diagnosis and management of preeclampsia. It highlights the importance of a multidisciplinary approach and individualized assessment to optimize maternal and fetal outcomes.[7]
Prevention
Prevention
Medication
- The best clinical evidence for prevention of preeclampsia is the use of low-dose aspirin.
- Your primary care provider may recommend taking an 81-milligram aspirin tablet daily after 12 weeks of pregnancy if you have one high-risk factor for preeclampsia or more than one moderate-risk factor.
- It’s important that you talk with your provider before taking any medications, vitamins or supplements to make sure it’s safe for you.
Lifestyle and healthy choices
- Before you become pregnant, especially if you’ve had preeclampsia before, it’s a good idea to be as healthy as you can be.
- Talk to your provider about managing any conditions that increase the risk of preeclampsia.[4]
Homeopathic Treatment
Homeopathic Treatment
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
The Homeopathic Medicines for Pregnancy induced hypertension (Preeclampsia)
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Aconite
- Intense anxiety, fear, restlessness and tossing about.
- Sudden, violent acute conditions, due to fright, shock, cold dry winds; getting chilled whilst sweating.
- Hyperpyrexia with burning thirst, hot dry skin and rapid pounding pulse. Profuse arterial hemorrhages.
- Numbness and tingling of affected parts.
- Congestions and inflammations with sweating, redness and burning.
- Better – warmth and after sweating.
Glonoine
- Confusion with dizziness.
- Head heavy but cannot lie it on a pillow, can’t bear anything about the head.
- Surging of blood to heart and head. Severe congestions to the head.
- Tendency to sudden and violent irregularities of the circulation.
- Any exertion brings rush of blood to heart and fainting spells. Pulsating sensation through’ body.
- Face flushed hot, livid; sweaty.
- Worse – in the sun, exposure to sun rays, gas open fire: jar, stooping, having hair out; peaches, stimulants, from 6am to noon, L side.[2]
Strophanthus Hispidus:
- Acts on the heart; diminishes the rapidity. Arteriosclerosis, rigid arteries of the old age person.
- Restores tone to a brittle tissue, esp. heart muscle and valves.
Sepia:
- Irritable, easily offended. Sad, indifferent to those loved best. Averse to occupation, to family.
- Weakness, yellow complexion.
- Pulsating headache in cerebellum.
- Violent intermittent palpitation, Beating in all arteries.
- Tremulous feeling with flushes. Feet hot and hands cold and vice versa.
- Worse – standing. cold air, Forenoon, evenings, washing, dampness, L side, before thunderstorm.
- Better – exercise, press., warmth of bed, hot applications, after sleep.
Veratrum viride:
- Quarrelsome and delirious. Especially adapted to full blooded, plethoric persons. Additionally, Controls action of heart and pulse.
- Paroxysms of auricular fibrillation.
- Valvular diseases, Beating of pulse throughout especially in R thigh. Bloated livid face.
- Bloodshot eyes. Great prostration. Lastly, Narrow well developed streak right through the middle of the tongue.
Crataegus:
- Apprehensiveness and despondency.
- Heart tonic, Acts on heart muscle, Irregularity of heart.
- Insomnia of aortic sufferers; Oedema. High arterial tension.
- Sedative to cross, irritable patients.
- Arteriosclerosis; said to have a solvent power upon crustaceous deposits in arteries.
- Extreme Dyspnoea on least exertion, without much increase in pulse.
- Worse – warm room. Better – fresh air, quiet and rest.[2]
Diet & Regimen
Diet & Regimen
Recommendations for PIH
Dietary
- Reduce Sodium Intake: Limit processed foods, salty snacks, and added salt to reduce fluid retention and lower blood pressure.
- Increase Potassium Intake: Foods rich in potassium like bananas, sweet potatoes, and leafy greens can help counter the effects of sodium.
- Focus on Calcium: Adequate calcium intake is essential for blood pressure regulation. Include dairy products, fortified plant milk, or calcium supplements as advised by your doctor.
- Healthy Protein Sources: Choose lean protein like fish, poultry, beans, and lentils.
- Complex Carbohydrates: Opt for whole grains, fruits, and vegetables for sustained energy and fiber.
- Hydration: Drink plenty of water throughout the day to help your body flush out toxins.
Regimen for PIH
- Regular Prenatal Care: Frequent checkups are crucial to monitor blood pressure and overall health.
- Blood Pressure Monitoring: Home blood pressure monitoring may be recommended to track your levels between appointments.
- Medications: In some cases, your doctor may prescribe medication to manage blood pressure.
- Rest and Relaxation: Adequate rest and stress management techniques are important.
- Weight Management: Maintaining a healthy weight gain during pregnancy can help reduce the risk of complications.
- Regular Exercise: Light to moderate exercise, as approved by your doctor, can improve circulation and overall health.
Do’s and Don'ts
The Do’s & Don’ts
Do’s:
Attend Regular Prenatal Checkups:
- Consistent monitoring of blood pressure and other vital signs is crucial for early detection and management of PIH.
Monitor Blood Pressure at Home:
- If advised by your healthcare provider, invest in a reliable blood pressure monitor and track your readings regularly.
Maintain a Healthy Diet:
- Focus on a balanced diet rich in fruits, vegetables, whole grains, and lean protein.
- Limit sodium intake to reduce fluid retention and manage blood pressure.
- Consult a registered dietitian for personalized meal planning.
Stay Active:
- Engage in regular, moderate-intensity exercise as approved by your healthcare provider.
- Activities like walking, swimming, and prenatal yoga can help maintain healthy blood pressure and overall well-being.
Get Adequate Rest:
- Aim for 7-8 hours of sleep each night.
- Resting on your left side can improve blood flow to the placenta and kidneys.
Manage Stress:
- Practice relaxation techniques like deep breathing, meditation, and prenatal yoga.
- Seek support from friends, family, or a therapist if needed.
Report Any Concerning Symptoms:
- Immediately contact your healthcare provider if you experience severe headaches, visual disturbances, upper abdominal pain, nausea, vomiting, decreased urine output, or sudden swelling.
Don’ts:
Smoke or Use Tobacco Products:
- Smoking increases the risk of PIH and other complications.
- Seek support from healthcare professionals or smoking cessation programs to quit.
Consume Alcohol or Use Recreational Drugs:
- These substances can harm both you and your baby and may worsen PIH.
- Avoid them completely during pregnancy.
Take Over-the-Counter Medications Without Consulting Your Doctor:
- Some medications can interact with medications used to manage PIH or worsen its symptoms.
- Always consult your healthcare provider before taking any medications, even those deemed safe during pregnancy.
Ignore Your Doctor’s Advice:
- Follow your healthcare provider’s recommendations regarding diet, exercise, medications, and follow-up appointments.
- Promptly address any concerns or questions you may have.
Stress or Overexert Yourself:
- While staying active is important, avoid strenuous activities or heavy lifting.
- Delegate tasks and prioritize rest whenever possible.
Remember:
- PIH, including preeclampsia, can be a serious condition but with early detection and appropriate management, most women experience healthy pregnancies and deliveries.
- Don’t hesitate to reach out to your healthcare provider with any questions or concerns.
- By taking proactive steps and adhering to medical advice, you can significantly reduce your risk of complications and ensure the well-being of both you and your baby.
Terminology
Terminology
- Pregnancy-Induced Hypertension (PIH): A broad term encompassing various hypertensive disorders that develop during pregnancy, including gestational hypertension, preeclampsia, and eclampsia.
- Preeclampsia: A serious condition characterized by high blood pressure and proteinuria (excess protein in the urine) after 20 weeks of gestation. It can affect multiple organ systems and lead to complications for both mother and baby.
- Eclampsia: The most severe form of preeclampsia, involving seizures or coma in a pregnant woman with preeclampsia.
- Gestational Hypertension: High blood pressure that develops after 20 weeks of gestation without proteinuria or other signs of organ damage.
- Chronic Hypertension: High blood pressure that exists before pregnancy or develops before 20 weeks of gestation.
- Superimposed Preeclampsia: The development of preeclampsia in a woman with pre-existing chronic hypertension.
Other Terminology
- Proteinuria: The presence of excess protein in the urine, often indicative of kidney damage.
- Hypertension: High blood pressure, typically defined as a systolic blood pressure of 140 mmHg or higher or a diastolic blood pressure of 90 mmHg or higher.
- Endothelial Dysfunction: Damage to the inner lining of blood vessels, leading to impaired blood flow and organ dysfunction.
- HELLP Syndrome: A severe form of preeclampsia involving Hemolysis (breakdown of red blood cells), Elevated Liver enzymes, and Low Platelet count.
- Fetal Growth Restriction (FGR): A condition where the fetus is smaller than expected for its gestational age due to insufficient placental blood flow.
- Preterm Birth: Birth before 37 weeks of gestation.
- Maternal Morbidity and Mortality: Illness or death related to pregnancy or childbirth.
Related To Homoeopathy
Totality of Symptoms:
- Preeclampsia: This refers to the complete clinical picture of the patient, encompassing the physical signs and symptoms (e.g., hypertension, proteinuria, edema), as well as the mental and emotional state.
- In Homeopathy: The cornerstone of homeopathic prescribing, it emphasizes considering all the patient’s symptoms, modalities (factors that make symptoms better or worse), and individual characteristics to select the most appropriate remedy.
Individualization:
- Preeclampsia: While there are standard guidelines for managing preeclampsia, treatment may need to be individualized based on the severity of the condition, maternal and fetal well-being, and other factors.
- In Homeopathy: A core principle that highlights the unique nature of each patient and their illness. Homeopathic treatment aims to address the individual’s specific needs rather than solely focusing on the disease diagnosis.
Vital Force:
- In Preeclampsia: Though not explicitly used in conventional medicine, this concept may relate to the body’s inherent ability to maintain homeostasis and resist disease. Preeclampsia could be seen as a disruption of this vital force.
- In Homeopathy: A central concept referring to the dynamic energy that animates the living organism and maintains health. Homeopathic remedies are believed to stimulate the vital force to initiate healing.
Miasm:
- In Preeclampsia: Not directly applicable, but certain predispositions or inherited tendencies might be considered in the context of susceptibility to preeclampsia.
- In Homeopathy: Refers to inherited or acquired predispositions to certain disease patterns. Miasmatic understanding helps homeopaths identify deeper underlying tendencies and select remedies accordingly.
Proving:
- In Preeclampsia: Clinical trials and research studies play a role in understanding the pathophysiology and treatment of preeclampsia.
- In Homeopathy: A systematic process of observing the effects of a substance on healthy individuals to determine its potential therapeutic applications.
References
References
- DC Dutta’s Text Book of OBSTETRICS
- Homoeopathic Body-System Prescribing – A Practical Workbook of Sector Remedies
- https://www.fernandezhospital.com/ Uploads/Document/189/dietary_guidelines _for_pregnancy_induced_hypertension.pdf
- https://www.mayoclinic.org/diseases-conditions/preeclampsia/diagnosis-treatment/drc-20355751.
- Prevalence and Risk Factors of Pregnancy Induced Hypertension Including Preeclampsia/Eclampsia in Women of Odisha, an Eastern I – Acta Scientific (2019).
- Prevalence of pregnancy induced hypertension and associated factors in Kashmiri women attending a tertiary care hospital at Srinagar: a cross-sectional study | International Journal of Reproduction, Contraception, Obstetrics and Gynecology (2023).
- Williams Obstetrics, 26th Edition, F. Gary Cunningham, Kenneth J. Leveno, Steven L. Bloom, Jodi S. Dashe, Barbara L. Hoffman, Brian M. Casey, Catherine Y. Spong, 2020, McGraw-Hill Education.
Also Search As
Pregnancy Induced Hypertension Also Search As
Specific Search Terms
Combining Keywords:
- "homeopathy preeclampsia"
- "homeopathic treatment for PIH"
- "homeopathic remedies for high blood pressure in pregnancy"
- "homeopathy and gestational hypertension"
Including Specific Remedies:
- "Belladonna for preeclampsia"
- "Aconite in pregnancy-induced hypertension"
- "Gelsemium for high blood pressure during pregnancy"
Adding Location (if relevant):
- "homeopathy for preeclampsia in India"
- "homeopathic treatment PIH UK"
Search Platforms
- Search Engines (Google, Bing, DuckDuckGo): Start with general searches using the keywords above. Consider adding "article" or "research" to narrow results.
- Homeopathic Websites and Forums: Search within websites of homeopathic organizations, clinics, or practitioners. Look for dedicated blogs or article sections.
- Homeopathic Journals and Databases: Access online homeopathic journals or specialized databases like HomBRex or Hompath.
Tips for Effective Searching
- Use Quotation Marks: Enclose phrases in quotation marks to search for exact matches.
- Use Boolean Operators: Utilize "AND", "OR", and "NOT" to refine searches and combine terms.
- Filter by Date: If looking for recent information, filter results by publication date.
- Check Credibility: Prioritize articles from reputable sources, like homeopathic journals or experienced practitioners.
Additional Resources
- Consult a Homeopathic Practitioner: Discuss your interest with a qualified homeopath. They can provide personalized recommendations and information on relevant research.
- Homeopathic Libraries: Visit libraries with specialized collections on homeopathy.
- Online Homeopathic Communities: Participate in online forums or groups to connect with others interested in homeopathy and pregnancy.
Important Considerations:
- Evidence: Remember that the evidence base for homeopathy in treating preeclampsia is limited. Approach information with a critical eye.
- Consult a Doctor: Always seek advice from a qualified medical professional for the diagnosis and management of preeclampsia. Homeopathy should only be considered as a complementary therapy alongside conventional medical care.
Frequently Asked Questions (FAQ)
How is PIH diagnosed?
Diagnosis
- PIH is diagnosed through regular blood pressure checks during prenatal visits. If your blood pressure is consistently high (140/90 mm Hg or higher), your doctor may conduct further tests to assess your health and the baby’s well-being.
Can homeopathy help manage PIH?
- Homeopathy may offer supportive care for PIH by addressing associated symptoms and promoting overall well-being. However, it’s crucial to note that PIH requires close medical supervision and conventional treatment.
What is Pregnancy induced hypertension?
Definition
Preeclampsia is a multisystem disorder of unknown etiology characterized by development of hypertension to the extent of 140/90 mm Hg or more with proteinuria after the 20th week in a previously normotensive and nonproteinuric woman.
What causes Pregnancy induced hypertension?
- Other high blood pressure disorders during pregnancy
- Gestational hypertension
- Chronic hypertension
- Chronic hypertension with superimposed preeclampsia
How does a homeopath select the right remedy for PIH?
- A skilled homeopath will conduct a thorough case analysis, considering the pregnant woman’s physical, mental, and emotional symptoms, along with her medical history, to find the most suitable remedy.
What are the symptoms of Pregnancy induced hypertension?
Symptoms
- Excess protein in urine (proteinuria)
- Decreased levels of platelets in blood
- Increased liver enzymes
- Severe headaches
- Changes in vision
- Shortness of breath
Can homeopathy be used alongside conventional treatment for PIH?
- Yes, homeopathy can potentially be used as a complementary therapy alongside conventional medical treatment for PIH, but only under the guidance of a qualified healthcare professional.
How long does it take to see improvement with homeopathy for PIH symptoms?
- The response to homeopathic treatment varies depending on the individual and the specific symptoms. It’s crucial to prioritize conventional medical care for managing PIH itself.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Pregnancy induced hypertension?
Homoeopathic Medicines for pregnancy induced hypertension
- Aconite
- Glonoine
- Strophanthus Hispidus
- Sepia
- Veratrum viride
- Crataegus
