Pruritus Vulva
Definition
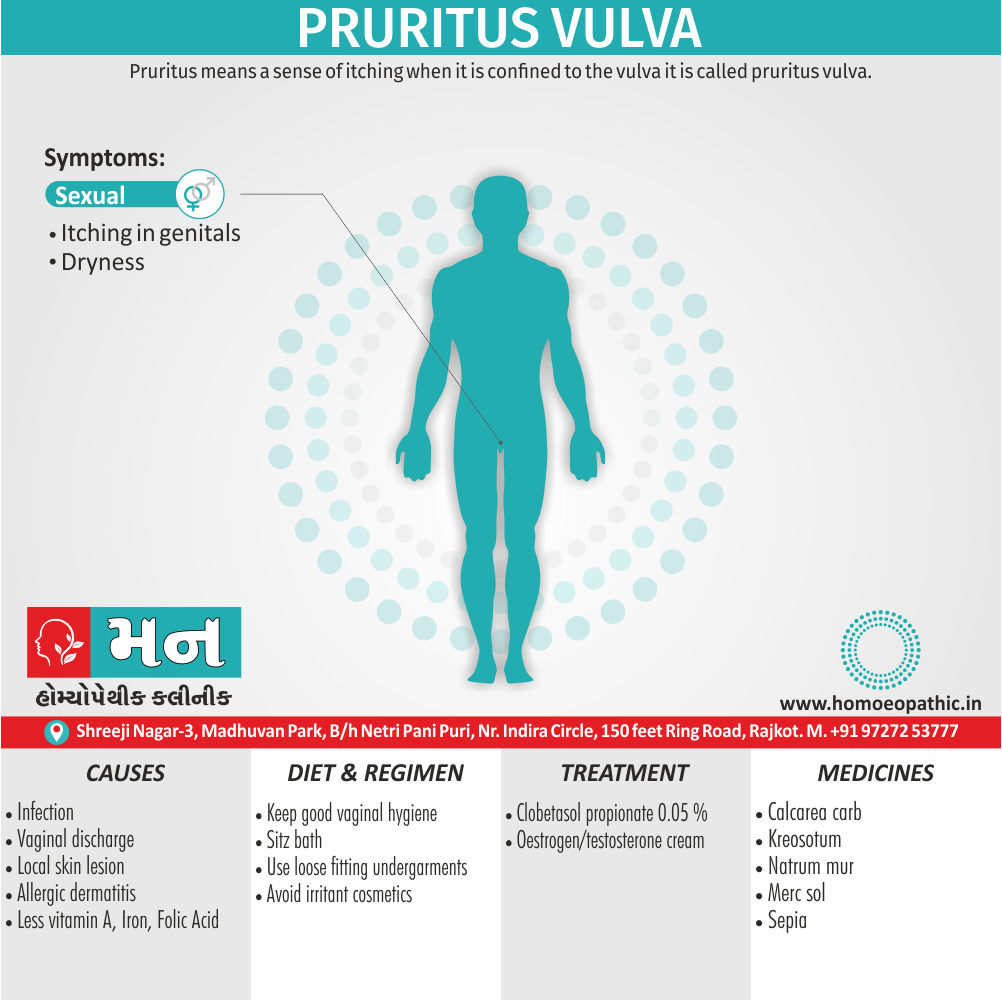
Pruritus means sense of itching, when it is confined to the vulva, it is called pruritus vulvae. It should not be confused with pain.[3]
Here are some synonyms for Pruritis Vulvae, ranging from informal to medical terms:
- Informal: Itchy vulva
- Patient-friendly: Vulval itching
- Medical: Pruritus of vulva, Vulvar pruritus
- Diagnostic Codes: L29.2 (ICD-10-CM)
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
Pruritus vulvae, commonly known as vulvar itching, is a distressing symptom affecting the external female genitalia (vulva). It can significantly impact a woman’s quality of life, leading to discomfort, sleep disturbances, and emotional distress. While it can occur at any age, it is more prevalent in postmenopausal women.
Causes:
The causes of pruritus vulvae are diverse and can be broadly categorized into:
- Infectious: Vulvovaginal candidiasis (most common), bacterial vaginosis, sexually transmitted infections, etc.
- Inflammatory/Dermatologic: Irritant or allergic contact dermatitis, lichen sclerosus, eczema, psoriasis, etc.
- Neoplastic: Vulvar intraepithelial neoplasia (VIN), vulvar cancer.
- Other: Atrophic vaginitis, diabetes mellitus, neurogenic pruritus, psychogenic pruritus, etc.
Clinical Features:
- Itching: The primary symptom, varying in intensity and duration
- Skin changes: Redness, swelling, excoriations, fissures, lichenification, dryness, etc.
- Associated symptoms: Burning, stinging, dyspareunia, vaginal discharge, urinary symptoms
Diagnosis:
- Detailed history and physical examination
- Laboratory tests: Wet mount, cultures, blood tests, allergy testing
- Additional tests: Biopsy, colposcopy, patch testing
Treatment:
- Addressing the underlying cause (e.g., antifungal for candidiasis, corticosteroids for dermatitis)
- Symptomatic relief: Cool compresses, antihistamines, topical anesthetics
- Lifestyle modifications: Avoiding irritants, wearing cotton underwear, practicing good hygiene
- Psychological support if needed
Prevention:
- Avoiding douching and harsh soaps
- Wearing breathable clothing
- Managing underlying medical conditions
- Practicing good hygiene[7]
Epidemiology
Epidemiology
Unfortunately, I could not find any specific epidemiological studies on Pruritus Vulva conducted exclusively in India with the year of publication. However, I can share some relevant information that may be helpful:
A study titled "Pruritus Vulvae: A Clinicomycological Study" published in the Indian Journal of Dermatology, Venereology and Leprology in 2007, investigated the causes of pruritus vulvae in 100 women attending a dermatology outpatient department. The study found that the most common causes were fungal infections (58%), followed by irritant or allergic contact dermatitis (22%) and bacterial infections (10%).[4]
Another study, "Clinical and Etiological Profile of Pruritus Vulvae" published in the Indian Journal of Sexually Transmitted Diseases and AIDS in 2015, examined 100 women with pruritus vulvae. This study reported similar findings, with fungal infections being the most common cause (52%), followed by bacterial vaginosis (20%) and irritant or allergic contact dermatitis (14%).[5]
While these studies do not provide specific epidemiological data such as prevalence or incidence rates, they offer valuable insights into the common causes of pruritus vulvae in Indian women.
It is important to note that further research is needed to establish the true epidemiological picture of pruritus vulvae in India.
Causes
Causes of Pruritus Vulva
Vaginal discharge i.e.
- The most common cause of pruritus vulvae is vaginal discharges either due to Trichomonas vaginalis or Candida albicans or both.
Local skin lesions i.e.
- The lesions may be either localized in the vulva or part of generalized lesions. Such lesions include — psoriasis, seborrheic dermatitis, intertrigo, etc.
Infections of the vulva i.e.
- Fungal—Candida
- Viral—Herpes genitals, genital warts.
- Parasitic—Threadworm may migrate to the area (especially in children), scabies, pediculosis.
- STD—Gonorrhoea, Trichomoniasis
Allergy or contact dermatitis i.e.
Use of nylon undergarments or washing those with certain soaps or detergents, idiosyncrasy to chemical contraceptives or condom is often related.[3]
Non neoplastic epithelial disorders of the vulva i.e.
- Squamous hyperplasia.
- Lichen sclerosis.
Neoplastic epithelial disorders i.e.
- Paget’s disease
- Invasive carcinoma of the vulva
Pruritus vulvae due to some systemic diseases i.e.
- Medical disorders: Glycosuria causes local changes in the skin and pruritus. Additionally, It favors the growth of Candida. Others: Thyroid disorders, Chronic liver disease.
- Dermatological causes: Contact dermatitis, drug allergy.
- Deficiency state: Deficiencies of iron, folic acid, vitamin B12 also vitamin A are all implicated.
- Psychosomatic causes: When no cause detect, Psychic factor is to exclude. Mental Anxiety or sexual frustration may be responsible for scratching.
Types
Types
Pruritus Vulva can broadly be categorized into several types based on underlying causes:
Infectious:
- Fungal infections: Candidal vulvovaginitis is the most common cause
- Bacterial infections: Bacterial vaginosis, though less frequent, can also contribute
- Viral infections: Herpes simplex virus can cause recurrent outbreaks with associated pruritus
- Parasitic infestations: Scabies or pubic lice can infrequently cause vulvar itch
Inflammatory/ Dermatological:
- Irritant or allergic contact dermatitis: Reaction to soaps, detergents, feminine hygiene products, etc.
- Lichen sclerosus: Chronic inflammatory condition causing thinning and whitening of vulvar skin
- Eczema/ Atopic dermatitis: Chronic skin condition with red, itchy patches
- Psoriasis: Autoimmune condition causing thick, scaly patches on skin
Neoplastic:
- Vulvar Intraepithelial Neoplasia (VIN): Precancerous changes in vulvar skin can sometimes present with itch
- Vulvar cancer: Though rare, can cause persistent pruritus
Other:
- Hormonal changes: Atrophic vaginitis due to estrogen deficiency in menopause
- Neurogenic pruritus: Itch originating from nerve dysfunction
- Psychogenic pruritus: Itch linked to psychological factors
- Idiopathic pruritus: Itch with no identifiable cause
Note: This categorization is based on the information presented in the reference book. Other classifications or subtypes might exist in different literature or clinical practices.[6]
Risk Factors
Risk factors
Several factors can increase the risk of developing Pruritus Vulva:
Personal Hygiene and Lifestyle:
- Frequent douching: Disrupts the natural vaginal flora, increasing the risk of infections
- Use of harsh soaps, detergents, or feminine hygiene products: Can cause irritation and allergic reactions
- Wearing tight-fitting or synthetic clothing: Creates a warm, moist environment favorable for fungal and bacterial growth
- Excessive sweating: Can contribute to irritation and maceration of the vulvar skin
Medical Conditions:
- Diabetes mellitus: High blood sugar levels can promote fungal growth and impair the immune system
- Immunosuppression: Weakened immune system increases susceptibility to infections
- Urinary or fecal incontinence: Chronic moisture and irritation can predispose to skin breakdown and infections
- Sexually transmitted infections (STIs): Can cause vulvar lesions and inflammation
Hormonal Factors:
- Menopause: Estrogen deficiency leads to atrophic changes in the vulvar skin, making it more prone to irritation and infections
- Pregnancy: Hormonal fluctuations and increased vaginal discharge can increase the risk of vulvovaginal candidiasis
Other Factors:
- History of atopic dermatitis or other allergic conditions: Increases the likelihood of developing allergic contact dermatitis
- Psychological stress: Can exacerbate existing pruritus or trigger psychogenic pruritus
- Certain medications: Some medications can cause dryness or allergic reactions in the vulvar area
Note: This list of risk factors is not exhaustive. Other factors might also contribute to the development of Pruritus Vulva.[8]
Pathogenesis
Pathogenesis
The pathogenesis of Pruritus Vulva is complex and multifactorial, often involving an interplay of various factors:
Inflammation:
- Infectious agents: Bacteria, fungi, viruses, or parasites can trigger an inflammatory response in the vulvar skin, leading to the release of inflammatory mediators (histamine, prostaglandins, cytokines) that stimulate itch receptors.
- Irritant or allergic contact dermatitis: Exposure to irritants or allergens can initiate an inflammatory cascade, causing pruritus.
- Chronic inflammatory conditions: Lichen sclerosus and other dermatological conditions can result in chronic inflammation and persistent itch.
Nerve Sensitization:
- Peripheral nerve sensitization: Chronic inflammation or nerve injury can lead to heightened sensitivity of peripheral nerves, resulting in increased itch perception.
- Central sensitization: Persistent pruritus can lead to changes in the central nervous system, amplifying the itch sensation and making it more difficult to control.
Dryness and Atrophy:
- Menopausal changes: Estrogen deficiency can lead to vulvar atrophy, causing dryness, thinning of the skin, and increased susceptibility to irritation and pruritus.
- Other causes of dryness: Certain medications, soaps, and environmental factors can contribute to dryness and exacerbate itch.
Psychological Factors:
- Psychogenic pruritus: Psychological stress, anxiety, or depression can trigger or worsen pruritus in some individuals.
- Itch-scratch cycle: The act of scratching can provide temporary relief but can also further damage the skin, leading to more inflammation and pruritus, perpetuating the cycle.
Other Factors:
- Neoplastic processes: Vulvar intraepithelial neoplasia (VIN) or vulvar cancer can sometimes present with pruritus as an early symptom.
- Hormonal fluctuations: Changes in hormone levels during pregnancy or menstruation can sometimes contribute to pruritus.
- Idiopathic pruritus: In some cases, no specific underlying cause can be identified.
Note: This overview of pathogenesis is based on the information presented in the reference book. Further research is ongoing to fully elucidate the complex mechanisms involved in Pruritus Vulva.[7]
Pathophysiology
Pathophysiology
The pathophysiology of Pruritus Vulva involves a complex interplay of various factors, leading to the sensation of itch:
Sensory Nerve Stimulation:
- Itch Receptors: The vulvar skin is richly innervated with sensory nerve fibers containing specialized itch receptors (pruriceptors). These receptors can be activated by various stimuli, including inflammatory mediators, histamine, neuropeptides, and other pruritogens.
- Neurogenic Inflammation: In some cases, the itch sensation itself can trigger the release of additional inflammatory mediators from nerve endings, further amplifying the itch response.
Inflammatory Mediators:
- Histamine: Released from mast cells and basophils in response to allergens, irritants, or infections, histamine is a potent pruritogen that directly activates itch receptors.
- Prostaglandins and Leukotrienes: These inflammatory mediators, produced by various cells in response to tissue injury or inflammation, can sensitize nerve endings and contribute to itch.
- Cytokines: Released by immune cells during inflammation, cytokines can modulate the itch response and contribute to chronic pruritus.
Skin Barrier Disruption:
- Dryness and Atrophy: Estrogen deficiency in menopause or other conditions can lead to vulvar atrophy, causing dryness, thinning of the skin, and increased susceptibility to irritation and pruritus.
- Irritants and Allergens: Exposure to harsh soaps, detergents, feminine hygiene products, or other irritants can disrupt the skin barrier, allowing penetration of pruritogens and triggering inflammation.
Central Sensitization:
- Chronic Itch: Persistent pruritus can lead to changes in the central nervous system, resulting in increased sensitivity to itch stimuli and a lower threshold for itch perception.
- Psychogenic Factors: Stress, anxiety, and depression can modulate the central processing of itch and contribute to chronic pruritus.
Other Factors:
- Infections: Vulvovaginal candidiasis, bacterial vaginosis, and other infections can trigger inflammation and pruritus.
- Hormonal Fluctuations: Changes in hormone levels during pregnancy or menstruation can sometimes contribute to pruritus.
- Neoplastic Processes: Vulvar intraepithelial neoplasia (VIN) or vulvar cancer can sometimes present with pruritus.
Note: The pathophysiology of Pruritus Vulva is complex and not fully understood. Further research is ongoing to elucidate the precise mechanisms involved.[9]
Clinical Features
Clinical Features
The clinical features of Pruritus Vulva can vary depending on the underlying cause, but typically include:
Itching:
- The hallmark symptom, often described as intense, burning, or stinging
- Can be localized to the vulva or extend to the perineum, anus, or inner thighs
- May be intermittent or continuous, and can worsen at night or with certain triggers (heat, moisture, friction)
Skin Changes:
- Redness, swelling, and inflammation of the vulvar skin
- Excoriations, fissures, or lichenification (thickening of the skin with accentuated skin markings) due to scratching
- Dryness, scaling, or cracking of the skin, particularly in atrophic vulvitis
- White patches or plaques in lichen sclerosus
- Vesicles or ulcers in herpes simplex virus infection
Associated Symptoms:
- Burning or stinging sensation
- Pain or discomfort during sexual intercourse (dyspareunia)
- Vaginal discharge (abnormal color, odor, or consistency)
- Urinary symptoms (frequency, urgency, dysuria) in cases of concomitant urinary tract infection
Psychological Impact:
- Frustration, anxiety, and embarrassment due to persistent itch
- Sleep disturbances due to nighttime itching
- Reduced quality of life and sexual dysfunction
Note: The specific clinical features can vary depending on the underlying cause of Pruritus Vulva. A thorough history and physical examination are essential for accurate diagnosis and management.[10]
Sign & Symptoms
Sign & Symptoms of Pruritus Vulva
- Extreme also constant itching.
- A burning sensation in the vulvar area.
- Vaginal discharge.
- Small cracks on the skin of the vulva.
- Redness and swelling on the vulva also labia (lips of the vagina)
- Blisters on the vulva.
- Scaly, thick, whitish patches on the vulva.
Clinical Examination
Clinical Examination
The clinical examination for Pruritus Vulva should be comprehensive and include the following components:
Inspection:
- Careful visual examination of the entire vulvar region, including the mons pubis, labia majora and minora, clitoris, vestibule, and perineum.
- Note any skin changes such as redness, swelling, excoriations, fissures, lichenification, dryness, scaling, white patches, vesicles, or ulcers.
- Assess for signs of infection (discharge, odor, lesions) or atrophy (thinning of the skin, loss of rugal folds).
Palpation:
- Gently palpate the vulvar skin to assess for tenderness, induration, or masses.
- Examine the inguinal lymph nodes for enlargement or tenderness.
Speculum Examination:
- If indicated, perform a speculum examination to visualize the vaginal walls and cervix.
- Obtain samples for microbiological testing (wet mount, cultures) if infection is suspected.
Additional Assessments:
- Assess for signs of urinary or fecal incontinence, which can contribute to vulvar irritation.
- Evaluate for psychological distress or anxiety, which can exacerbate pruritus.
Note: A thorough clinical examination is essential for identifying the underlying cause of Pruritus Vulva and guiding appropriate management.[11]
Diagnosis
Diagnosis of Pruritus Vulva
It should be borne in mind that pruritus vulvae are a manifestation of some underlying pathology either located at the site or elsewhere in the body.
The investigations should include i.e.:
Detailed history regarding
age of onset, intensity of itching, duration, associated vaginal discharge, contraceptive practice, relation with psychologic upset or neurosis, allergy to nylon, either soap or particular detergents.
General examination
Thorough systemic examination need.
Examination for diabetes mellitus, liver also thyroid disorders, hematological diseases to made
Local examination
The extent of the lesion is to note.[3]
Special investigations
- Microscopic examination of the vaginal discharge or vulval scraping to detect Candida or Trichomonas vaginalis.
- Urine for sugar, protein and pus cells.
- Blood—Complete blood count, postprandial glucose. Detailed hematological workup (polycythemia, leukaemia), thyroid profile, liver function and renal function tests carry out.
- Stool—Ova, parasites and cysts are to look for.
- In long-standing cases especially with vulval epithelial disorders, biopsy either random or colposcopy directed, is to take to note the type of skin changes and exclude malignancy.[3]
Differential Diagnosis
Differential Diagnosis
Pruritus Vulva can have a wide range of differential diagnoses, including:
Infectious Causes:
- Vulvovaginal candidiasis (most common)
- Bacterial vaginosis
- Trichomoniasis
- Herpes simplex virus infection
- Genital warts (human papillomavirus infection)
- Scabies
- Pubic lice
Inflammatory/ Dermatological Conditions:
- Irritant or allergic contact dermatitis
- Lichen sclerosus
- Eczema/ Atopic dermatitis
- Psoriasis
- Lichen planus
- Seborrheic dermatitis
- Intertrigo
Neoplastic Conditions:
- Vulvar intraepithelial neoplasia (VIN)
- Vulvar cancer
- Paget’s disease of the vulva
Other Causes:
- Atrophic vaginitis (due to estrogen deficiency)
- Diabetes mellitus
- Neurogenic pruritus
- Psychogenic pruritus
- Drug reactions
- Systemic diseases (e.g., liver disease, kidney disease, thyroid disease)
- Idiopathic pruritus
Note: The differential diagnosis of Pruritus Vulva can be extensive. A careful history, physical examination, and appropriate investigations are necessary to arrive at the correct diagnosis and guide management.[12]
Complications
Complications
Pruritus Vulva is often a benign and self-limiting condition, it can lead to several complications if left untreated or inadequately managed:
Skin Changes:
- Lichenification: Chronic scratching can lead to thickening and leathery changes in the vulvar skin, making it more prone to irritation and infection.
- Excoriations and Fissures: Persistent scratching can cause breaks in the skin, increasing the risk of secondary bacterial or fungal infections.
- Hyperpigmentation: Chronic inflammation can lead to darkening of the vulvar skin.
Infections:
- Secondary bacterial or fungal infections: Breaks in the skin from scratching can provide an entry point for pathogens, leading to cellulitis, abscesses, or impetigo.
- Recurrent vulvovaginal infections: Chronic inflammation and disruption of the normal vaginal flora can predispose to recurrent infections, such as candidiasis or bacterial vaginosis.
Psychological Impact:
- Anxiety and Depression: Chronic pruritus can significantly impact a woman’s quality of life, leading to anxiety, depression, and social isolation.
- Sleep Disturbances: Nighttime itching can disrupt sleep patterns, leading to fatigue and impaired concentration.
- Sexual Dysfunction: Pain and discomfort during intercourse can lead to decreased sexual desire and avoidance of intimacy.
Rarely:
- Vulvar Cancer: In rare cases, persistent pruritus can be a presenting symptom of vulvar cancer, particularly in older women.
Note: Early diagnosis and effective management of Pruritus Vulva are crucial to prevent these potential complications.[13]
Investigations
Investigation
The investigation of Pruritus Vulva aims to identify the underlying cause and guide appropriate management. It typically involves the following:
Detailed History:
- Onset, duration, and characteristics of the itch (location, severity, timing, triggers)
- Associated symptoms (vaginal discharge, urinary symptoms, skin changes)
- Medical history (diabetes, allergies, STIs, medications)
- Sexual history
- Personal hygiene practices
Physical Examination:
- Careful inspection of the vulva, perineum, and perianal area
- Assessment for skin changes, discharge, lesions, or signs of infection
- Speculum examination if indicated
Laboratory Investigations:
- Wet mount preparation of vaginal discharge to identify Candida, Trichomonas, or bacterial vaginosis
- Vaginal pH measurement
- Cultures for bacteria, fungi, or viruses if indicated
- Blood glucose test if diabetes is suspected
- Allergy testing if allergic contact dermatitis is suspected
Additional Investigations (if indicated):
- Biopsy of vulvar skin lesions to rule out malignancy or other dermatological conditions
- Colposcopy to evaluate for cervical or vaginal pathology
- Patch testing to identify allergens
- Nerve conduction studies or imaging if neurogenic pruritus is suspected
Note: The specific investigations will depend on the clinical presentation and suspected etiology.[14]
Treatment
Treatment of Pruritus Vulva
- Appropriate local hygiene is to be taken care of.
- In detail; To use loose fitting undergarments preferably made of cotton to keep the area aerated.
- To prevent the vicious cycle of ‘itch-scratch’.
- Local application of either antibiotics or Clobetasol propionate 0.05 percent ointment may be helpful. Additionally, If the skin is atrophic, oestrogen or testosterone cream may be helpful.
- To treat the specific etiological factor causing pruritus by appropriate therapy—local or systemic.
Surgery: Surgery may be needed when biopsy is confirms features of neoplasia (VIN or invasion).[3]
Prevention
Prevention
Although not all cases of Pruritus Vulva are preventable, certain measures can help reduce the risk and recurrence:
Hygiene and Lifestyle:
- Avoid douching: It disrupts the natural vaginal flora, increasing susceptibility to infections.
- Use mild, unscented soaps and detergents: Harsh soaps can irritate the delicate vulvar skin.
- Wear cotton underwear and loose-fitting clothing: This allows for better air circulation and reduces moisture buildup.
- Change out of wet clothing promptly: Dampness can promote fungal and bacterial growth.
- Practice good toilet hygiene: Wipe from front to back after using the toilet to prevent contamination of the vulva with fecal bacteria.
Manage Underlying Medical Conditions:
- Control diabetes: Maintain good blood sugar control to reduce the risk of fungal infections.
- Treat infections promptly: Seek medical attention for any signs of vaginal or vulvar infection.
- Manage incontinence: Use appropriate products and techniques to minimize moisture and irritation.
Hormonal Management:
- Consider topical estrogen for atrophic vaginitis: This can help restore the vulvar skin’s health and reduce dryness.
- Discuss hormonal contraceptives with your doctor: Some contraceptives can alter the vaginal environment and increase the risk of infections.
Other Measures:
- Avoid irritants and allergens: Identify and avoid potential triggers, such as certain soaps, detergents, fabrics, or feminine hygiene products.
- Manage stress: Practice relaxation techniques or seek professional help to manage stress and anxiety.
- Avoid scratching: Scratching can further damage the skin and worsen the itch. Use cool compresses or topical medications to relieve itching.
Note: These preventive measures can help reduce the risk of Pruritus Vulva. However, if symptoms persist or recur, it is important to seek medical evaluation to identify and address the underlying cause.[15]
Homeopathic Treatment
Homeopathic Treatment of Pruritus Vulva:
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Pruritus Vulva:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Kreasote
For Managing Violent Itching of the Vagina Kreasote is a very beneficial medicine for managing violent itching in the vagina. Itching is intolerable, making the person rub the area compulsively. Itching is worse during the evening, and the soreness and burning in the vagina is felt after scratching. A smarting and stitching sensation is present in the vagina. Vaginal pain is felt after urinating. Burning in the vagina may be present during intercourse. Acrid, corrosive, gushing and highly offensive discharge from the vagina may be present. The vagina may be highly inflamed in cases requiring Kreasote.[1]
Sepia
For Itching attended with Discharges Sepia is highly recommended for treating vaginal itching with prominent vaginal discharges. The vaginal discharges vary in nature – they may be yellow or greenish or milky. Excessive vaginal itching is accompanied by a lumpy discharge. The discharge is excoriating and also cause burning. Sepia is also indicated in cases of severe itching of the vulva with the presence of pimples/vesicular eruptions. It is also a top-listed medicine used for the treatment of vaginitis and vaginal infections.
Merc Sol
For Vaginal Itching with Marked Burning Merc Sol is useful for managing vaginal itching when accompanied by marked burning. Smarting, corroding and biting sensation is also felt in the vagina. Itching in vagina worsens from contact of urine in most cases needing Merc Sol. Vaginal discharges may be there that are worse at night time. The discharge from the vagina tends to be green in color. The discharge may be sticky.[1]
Natrum Mur
To Manage Vaginal Dryness and Itching Natrum Mur is a significant medicine for treating vaginal dryness and itching. Itching usually occurs after menses. There is burning and soreness felt in the vagina that appears mainly after urinating. Natrum Mur is also indicated for pimples on the external genitals with marked itching. In such cases, sometimes falling of hair from the genital may be noticed. Apart from the above, Natrum Mur is a prominent medicine to treat itching in cases of genital herpes.
Calcarea Carb
For Vaginal Itching that Worsens in Evening Calcarea Carb is a well-indicated medicine to manage vaginal itching that worsens during the evening. The itching worse after going to bed. Along with this, vaginal discharges of white milky character may be present. Itching on the vulva may be present along with soreness. Stitching pains are also felt on the vulva along with excessive sweat on the genitalia. Itching and burning in the vagina before and after menses is also indicates towards the use of Calcarea Carb.[1]
Graphites
To Relieve Vaginal Itching before Menses Graphites is a well-indicated homeopathic medicine for relieving vaginal itching before menses. Along with this biting or smarting in the vagina may be present. Vesicular eruptions or excoriations in the vagina may be present. Acrid, excoriating, profuse, gushing leucorrhea may be present. In most cases, the leucorrhea is yellowish-white in color that excoriates the skin. Itching pimples on the vulva and the labia that may cause a smarting sensation and be painful also suggest the use of Graphites.
Lycopodium
For Vaginal Itching during, Menses,Lycopodium is prepared from the spores of a plant Lycopodium Clavatum commonly known by the name of Club Moss or Wolf’s-Claw. This plant belongs to natural order Lycopodiaceae. Lycopodium is helpful to manage vaginal itching experienced during menses. Dryness and burning sensation in the vagina may also be complained of. In some cases, a milky, acrid vaginal discharge with burning in the vagina may be present.[1]
Conium
For Vaginal Itching felt after Menses Conium is beneficial to manage vaginal itching experienced after menses. The itching is violent in nature. It is felt deep in the vagina. Stitching pain in the vagina may also be present. White or yellow, acrid vaginal discharge with burning or smarting sensation in the vagina may be present.
Sulphur
For Itching, Burning, Soreness Sulphur is a useful medicine to treat vaginal itching, burning, and soreness. This tends to worsen by sitting. Intense itching of the vulva with pimples also indicates for using Sulphur. Chronic thin and profuse vaginal discharge causing burning and smarting sensation in the vulva is also treated well with Sulphur.
Nitric Acid
For Itching attended with Stitching Pains Nitric Acid is a suitable medicine for managing vaginal itching when attended with stitching pains. Itching in the vagina may worsen after intercourse. Burning in the vagina is also felt and vagina may be swollen too. Nitric Acid also offers help in cases of ulcers in the vagina with burning and itching.[1]
Diet & Regimen
Diet & Regimen
Although there is no specific "Pruritus Vulva Diet," certain dietary and lifestyle modifications can help manage symptoms and promote vulvar health:
Diet:
- Probiotics: Consuming foods rich in probiotics or taking probiotic supplements can help maintain a healthy balance of vaginal flora and reduce the risk of infections. Yogurt, kefir, sauerkraut, and kimchi are good sources of probiotics.
- Anti-inflammatory foods: Incorporate foods with anti-inflammatory properties into your diet. These include fruits, vegetables, whole grains, fatty fish, nuts, and seeds.
- Limit sugar and processed foods: High sugar intake can promote fungal growth and inflammation.
Regimen:
- Maintain good hygiene: Practice gentle cleansing of the vulva with mild, unscented soap and water. Avoid douching and harsh soaps.
- Wear breathable clothing: Opt for cotton underwear and loose-fitting clothing to reduce moisture and friction.
- Manage stress: Stress can exacerbate pruritus. Practice relaxation techniques like yoga, meditation, or deep breathing exercises.
- Avoid scratching: Scratching can worsen inflammation and lead to skin damage. Use cool compresses or topical medications to relieve itching.
- Consider Sitz baths: Soaking in a warm Sitz bath with baking soda or oatmeal can soothe irritated skin and reduce itching.
Note: These dietary and lifestyle recommendations can be beneficial for overall vulvar health and may help manage Pruritus Vulva symptoms. However, it is essential to address the underlying cause of pruritus for effective treatment.[16]
Do’s and Don'ts
Do’s & Don’ts
Pruritus Vulva Do’s and Don’ts
Do’s:
- Seek medical evaluation: If you experience persistent or recurrent vulvar itching, consult a healthcare professional for proper diagnosis and treatment.
- Practice good hygiene: Gently cleanse the vulva with mild, unscented soap and water once or twice daily. Pat dry thoroughly after washing.
- Wear breathable clothing: Choose cotton underwear and loose-fitting clothing to allow air circulation and reduce moisture buildup.
- Avoid irritants: Identify and avoid potential triggers such as harsh soaps, detergents, feminine hygiene products, scented toilet paper, and tight-fitting clothing.
- Apply cool compresses: Cool compresses or ice packs wrapped in a towel can help soothe itching and reduce inflammation.
- Use over-the-counter anti-itch creams or ointments: Hydrocortisone cream or other antihistamine creams can provide temporary relief from itching.
- Take prescribed medications as directed: If your doctor prescribes medication for an underlying condition, take it as instructed to manage the itching.
- Manage stress: Practice relaxation techniques such as yoga, meditation, or deep breathing exercises to reduce stress, which can worsen itching.
- Maintain a healthy lifestyle: Eat a balanced diet, exercise regularly, and get enough sleep to support overall health and immune function.
Don’ts:
- Scratch the affected area: Scratching can damage the skin, worsen inflammation, and lead to secondary infections.
- Use douches or feminine hygiene sprays: These products can disrupt the natural balance of vaginal flora and increase the risk of infections.
- Wear tight-fitting or synthetic clothing: These materials can trap moisture and heat, creating an environment conducive to fungal and bacterial growth.
- Use scented soaps, bubble baths, or bath oils: These products can irritate the delicate vulvar skin.
- Engage in sexual activity if you have an active infection: This can spread the infection to your partner or worsen your symptoms.
- Self-diagnose or self-treat: Consult a healthcare professional for proper diagnosis and treatment.
- Ignore persistent or recurrent itching: Seek medical attention if the itching does not improve with self-care measures or if you develop other symptoms.
Remember, early diagnosis and appropriate management are crucial for effectively addressing Pruritus Vulva and preventing complications. If you have any concerns about vulvar itching, consult your healthcare professional for guidance.
Terminology
Terminology
Pruritus Vulva:
Meaning: Itching of the vulva, the external female genitalia.
Vulva:
Meaning: The external female genitalia, including the labia majora, labia minora, clitoris, and vaginal opening.
Pruriceptors:
Meaning: Specialized sensory nerve endings that detect itch stimuli.
Pathogenesis:
Meaning: The biological mechanism(s) that lead to the development of a disease or condition, in this case, pruritus vulva.
Pathophysiology:
Meaning: The functional changes that occur in the body as a result of a disease or condition, specifically focusing on the physiological processes involved in pruritus vulva.
Inflammatory Mediators:
Meaning: Signaling molecules released by cells during inflammation, such as histamine, prostaglandins, and cytokines, that contribute to the sensation of itch.
Lichenification:
Meaning: Thickening and hardening of the skin with accentuated skin markings, often caused by chronic scratching.
Excoriation:
Meaning: Abrasion or scratch on the skin surface, usually caused by scratching.
Fissures:
Meaning: Linear cracks or breaks in the skin, often associated with dryness and inflammation.
Atrophic Vaginitis:
Meaning: Thinning, drying, and inflammation of the vaginal walls due to decreased estrogen levels, often occurring after menopause.
Lichen Sclerosus:
Meaning: A chronic inflammatory skin condition that causes thinning, whitening, and cracking of the vulvar skin.
Vulvar Intraepithelial Neoplasia (VIN):
Meaning: Precancerous changes in the vulvar skin that can sometimes present with itching.
Dyspareunia:
Meaning: Painful or difficult sexual intercourse.
Wet Mount Preparation:
Meaning: A microscopic examination of a sample of vaginal discharge to identify microorganisms such as bacteria, yeast, or parasites.
Colposcopy:
Meaning: A procedure to examine the cervix, vagina, and vulva using a magnifying instrument called a colposcope.
Biopsy:
Meaning: The removal of a small sample of tissue for microscopic examination to diagnose a disease or condition.
Idiopathic:
Meaning: Of unknown cause or origin.
Remember, this is not an exhaustive list of all terminologies used in articles on pruritus vulva, but it covers some of the key terms you are likely to encounter.
Terminologies and Their Meanings Used in Homeopathic Articles on Pruritus Vulva
In addition to the common medical terms already discussed, homeopathic articles on Pruritus Vulva may also utilize specific terminologies related to homeopathic principles and practice. Here are some examples:
Miasm:
Meaning: In homeopathy, a miasm is a predisposing factor or inherited taint that underlies chronic disease. Understanding the miasm is believed to help select the most appropriate homeopathic remedy.
Repertory:
Meaning: A reference book listing symptoms and the homeopathic remedies associated with them, used to aid in remedy selection.
Materia Medica:
Meaning: A collection of detailed descriptions of the properties and effects of homeopathic remedies.
Potency:
Meaning: The degree of dilution and succussion (vigorous shaking) a homeopathic remedy has undergone. Higher potencies are believed to have a deeper and longer-lasting action.
Aggravation:
Meaning: A temporary worsening of symptoms after taking a homeopathic remedy, often considered a positive sign indicating the remedy is working.
Amelioration:
Meaning: An improvement in symptoms after taking a homeopathic remedy.
Constitutional Remedy:
Meaning: A remedy chosen based on the individual’s overall physical, mental, and emotional characteristics, rather than just the specific symptoms of Pruritus Vulva.
Totality of Symptoms:
Meaning: The complete picture of the patient’s symptoms, including physical, mental, and emotional aspects, used to guide the selection of the most appropriate remedy.
Proving:
Meaning: A systematic process in homeopathy where healthy individuals take a substance and record their symptoms, helping to establish the remedy’s picture.
Similia Similibus Curentur:
Meaning: "Like cures like," the fundamental principle of homeopathy, stating that a substance that can cause symptoms in a healthy person can cure similar symptoms in a sick person.
Nosode:
Meaning: A homeopathic remedy prepared from diseased tissue or secretions.
Sarcode:
Meaning: A homeopathic remedy prepared from healthy tissue or secretions.
These terminologies reflect the unique approach of homeopathy in understanding and treating Pruritus Vulva. Homeopathic articles may discuss the selection of remedies based on the totality of symptoms, miasmatic considerations, and individual characteristics of the patient.
References
Reference:
- https://www.drhomeo.com/homeopathic-treatment/homeopathic-medicines-for-vaginal-itching/
- https://www.msdmanuals.com/home/women-s-health-issues/symptoms-of-gynecologic-disorders/genital-itching
- DC Dutta Text Book of Gynaecology
- A Clinicomycological Study" published in the Indian Journal of Dermatology, Venereology and Leprology in 2007.
- "Clinical and Etiological Profile of Pruritus Vulvae" published in the Indian Journal of Sexually Transmitted Diseases and AIDS in 2015.
- Comprehensive Gynecology
Edition: 7th Edition
Authors: D. Ashley Hillard, Gretchen M. Lentz (2017), Publisher: Elsevier. - Fitzpatrick’s Dermatology in General Medicine Edition: 9th Edition
Authors: Klaus Wolff, Lowell A. Goldsmith, Stephen I. Katz, Barbara A. Gilchrest, Amy S. Paller, David J. Leffell, (2019)
Publisher: McGraw Hill Professional. - Williams Gynecology
Edition: 4th Edition
Authors: Barbara L. Hoffman, John O. Schorge, Joseph I. Schaffer, Lisa M. Halvorson, Karen D. Bradshaw, F. Gary Cunningham, (2020)
Publisher: McGraw Hill Professional. - Clinical Gynecologic Endocrinology and Infertility, Edition: 9th Edition
Authors: Marc A. Fritz, Leon Speroff
(2019), Publisher: Lippincott Williams & Wilkins. - Yen & Jaffe’s Reproductive Endocrinology
Edition: 8th Edition
Authors: Jerome F. Strauss III, Robert L. Barbieri, (2019)
Publisher: Elsevier - Novak’s Gynecology
Edition: 16th Edition
Authors: Jonathan S. Berek, Evelyn Nicole Fessler,(2020)
Publisher: Wolters Kluwer - Danforth’s Obstetrics and Gynecology
Edition: 11th Edition
Authors: Ronald S. Gibbs, Arthur F. Haney, Joe Leigh Simpson, (2016)
Publisher: Lippincott Williams & Wilkins - Te Linde’s Operative Gynecology
Edition: 13th Edition
Authors: John O. Schorge, F. Gary Cunningham, Karen D. Bradshaw, Joseph I. Schaffer, Lisa M. Halvorson, Barbara L. Hoffman, (2020), Publisher: Wolters Kluwer - Berek & Novak’s Gynecology
Edition: 16th Edition
Authors: Jonathan S. Berek, Neville F. Hacker
Year of Publication: 2020
Publisher: Wolters Kluwer - Practical Gynecologic Oncology
Edition: 7th Edition
Authors: Neville F. Hacker, Michael J. Birrer, Andrew Berchuck, Gloria C. Huang, Robert E. Bristow, Pedro T. Ramirez, Dennis S. Chi
(2018),Publisher: Wolters Kluwer - Integrative Women’s Health
Edition: 1st Edition
Authors: Victoria Maizes, Tieraona Low Dog, Felice Gersh, Janet Carpenter
Year of Publication: 2015
Publisher: Oxford University Press
Also Search As
Also Search As
People can search for homeopathic articles on Pruritus Vulva using various online search methods:
Specific Search Queries:
- "Homeopathic treatment for Pruritus Vulva"
- "Homeopathy and Vulvar itching"
- "Remedies for Pruritus Vulva in homeopathy"
- "Homeopathic approach to Pruritus Vulva"
- "Pruritus Vulva: A homeopathic perspective"
Using Specific Homeopathic Terminology:
- "Pruritus Vulva: Repertory and Materia Medica"
- "Miasmatic treatment for Pruritus Vulva"
- "Constitutional remedies for Pruritus Vulva"
- "Homeopathic case studies on Pruritus Vulva"
General Search Strategies:
- Use search engines like Google, DuckDuckGo, or Ecosia.
- Include relevant keywords like "Pruritus Vulva," "homeopathy," "treatment," "remedies," and "causes."
- Search for articles on reputable homeopathic websites, blogs, and journals.
- Consider using specific search operators like quotation marks to search for exact phrases or the minus sign to exclude certain terms.
- Use image search to find visual representations or infographics related to homeopathic treatment of Pruritus Vulva.
Additional Tips:
- Consult a qualified homeopathic practitioner for personalized advice and treatment recommendations.
- Join online homeopathic forums or groups to connect with other individuals seeking information about Pruritus Vulva and homeopathy.
- Read books or publications on homeopathy and women’s health for in-depth information.
Remember, while searching for information online, be sure to critically evaluate the source’s credibility and consult a healthcare professional for proper diagnosis and treatment. Homeopathy should be considered a complementary therapy and used in conjunction with conventional medical approaches for managing Pruritus Vulva.
There are several ways to search for information on Pruritus Vulva, catering to different needs and preferences:
Online Search Engines:
- Keywords: "Pruritus Vulva," "vulvar itching," "itchy vulva," "female genital itching"
- Search engines: Google, Bing, DuckDuckGo, etc.
- Search operators: Use quotation marks for exact phrases, add "+" to include specific terms, use "-" to exclude terms.
- Image search: Find visual representations or diagrams of conditions.
Medical Websites and Databases:
- Reputable sources: Mayo Clinic, Cleveland Clinic, National Institutes of Health (NIH), etc.
- Medical databases: PubMed, MedlinePlus, etc.
- Search by symptoms, condition, or specific questions.
Health Forums and Communities:
- Online forums: Search for forums dedicated to women’s health or specific conditions.
- Social media groups: Find support groups or communities on platforms like Facebook or Reddit.
- Caution: Information on forums can be unreliable, always verify with a healthcare professional.
Books and Publications:
- Medical textbooks: Search for gynecology or dermatology textbooks.
- Patient education materials: Look for brochures or pamphlets at healthcare facilities.
- Online libraries: Access e-books or articles through your local library or university.
Consult a Healthcare Professional:
- Gynecologist: The primary specialist for female reproductive health.
- Dermatologist: If the cause is suspected to be skin-related.
- Primary care physician: Can provide initial assessment and referral if needed.
Additional Tips for Searching:
- Use specific terminology: Include medical terms like "vulvitis," "vaginitis," "lichen sclerosus," etc., for more targeted results.
- Specify your search: If you’re looking for causes, treatment options, or home remedies, include those terms in your search query.
- Consider your location: Add your country or region to find locally relevant information, especially for statistics or available treatments.
- Refine your search over time: If initial results are too broad, try adding more specific keywords or using search operators.
Remember, information found online should not replace professional medical advice. Always consult a healthcare provider for diagnosis and treatment recommendations for Pruritus Vulva.
Frequently Asked Questions (FAQ)
What is Pruritus Vulva?
Pruritus means sense of itching, when it is confined to the vulva, it is called pruritus vulvae. It should not be confused with pain.
What causes Pruritus Vulva?
Causes
- Vaginal discharge
- Local skin lesions
- Infections of the vulva
- Allergy or contact dermatitis
- Non neoplastic epithelial disorders of the vulva
How is pruritis vulvae treated?
- Lifestyle changes: Avoiding irritants, wearing loose-fitting cotton underwear, and practicing good hygiene can help relieve symptoms.
- Medications: Antifungal creams, antibiotics, or corticosteroids may be prescribed to treat infections or inflammation.
- Hormone therapy: Estrogen creams or oral medications can be used to address dryness associated with menopause.
- Other therapies: In some cases, light therapy or other procedures may be recommended.
How is pruritis vulvae diagnosed?
Diagnosis
A healthcare provider will conduct a thorough medical history and physical examination, including a pelvic exam. They may also take swabs or perform a biopsy to rule out infections or other conditions.
What are the symptoms of Pruritus Vulva?
Symptoms
- Extreme and constant itching.
- A burning sensation in the vulvar area.
- Vaginal discharge.
- Small cracks on the skin of the vulva.
- Redness and swelling on the vulva and labia (lips of the vagina)
- Blisters on the vulva.
How does homeopathy treat pruritis vulvae?
Homeopathic treatment involves a detailed consultation to understand your specific symptoms, medical history, and overall health. Based on this information, a qualified homeopath will prescribe a personalized remedy to stimulate your body’s natural healing response and reduce itching.
Can homeopathy prevent pruritis vulvae from recurring?
By addressing the root cause and strengthening the body’s defenses, homeopathy can help reduce the frequency and intensity of future episodes of pruritis vulvae
How long does it take to see results with homeopathic treatment?
The response time varies depending on the individual, the underlying cause of the itching, and other factors. Some may experience relief within a few days, while others might require a longer duration of treatment.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Pruritus Vulva?
Homoeopathic Medicine For Pruritus Vulva
- Calcarea carbonica
- Kreosotum
- Natrum muriaticum
- Sepia
- Borax
- Kali bichromicum
- Pulsatilla
- Sulphur
