Psychoactive Substance Use Disorders
Definition
Psychoactive Substance Use Disorders caused by psychoactive drugs. It is also one that is capable of altering the mental functioning. [2]
Here are some synonyms for Psychoactive Substance Use Disorders:
- Substance Use Disorders (SUDs)
- Addiction
- Substance dependence
- Substance abuse
- Chemical dependence
- Drug abuse
- Substance misuse
- Problematic substance use
- Harmful substance use
It’s important to note that some of these terms have slightly different meanings. For example, "substance abuse" is often used to refer to a less severe form of substance use disorder than "addiction."
Overview
Acute Intoxication
Withdrawal State
Dependence Syndrome
Harmful Use
Epidemiology
Causes
Psychoactive Substances
Why do people use substances ?
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Psychoactive Substance Use Disorders:
The use of alcohol and other psychoactive substances has recorded throughout history, often with the primary aim of changing an individual’s mood or relieving the distress of harsh circumstances.
Early examples include the chewing of tobacco leaves or coca (cocaine) in North America and Peru, respectively.
Humans are clearly vulnerable to the desire to use substances; this is illustrate by the fact that alcohol and other psychoactive substances remain a leading cause of medical and social problems worldwide and cause psychoactive substance use disorders.
World Health Organization (WHO) statistics report that alcohol is the primary causative factor in 4 percent of the global burden of disease. [1]
Drug:
A drug is defined (by WHO) as any substance that, when taken into the living organism, may modify one or more of its functions. This definition conceptualises ‘drug’ in a very broad way, including not only the medic at ions but also the other pharmacologically active substances.
The words ‘drug addiction’ and ‘drug person with substance abuse disorder’ were dropped from scientific use due to their derogatory connotation. Instead ‘ drug abuse’, ‘ drug dependence’, ‘ harmful use’, ‘misuse’, and ‘psychoactive substance use disorders’ are the terms used in the current nomenclature.
A psychoactive drug is one that is capable of altering the mental functioning.
There are four important patterns of psychoactive substance use disorders, which may overlap with each other:
1. Acute intoxication
2. Withdrawal state
3. Dependence syndrome
4. Harmful use.
The other syndromes associated with the psychoactive substance use in ICD-10 include psychotic disorder, amnesic syndrome, and residual and late-onset (delayed onset) psychotic disorder.
Acute Intoxication
Acute Intoxication In psychoactive Substance Use Disorder:
According to ICD-10, acute intoxication is a transient condition following the administration of alcohol or other psychoactive substance, resulting in disturbances in level of consciousness, cognition, perception, affect or behaviour, or other psychophysiological functions and responses. This is usually associated with high blood levels of the drug. [2]
The disturbances are directly related to the acute pharmacological effects of the substance and resolve with time, with complete recovery, except where tissue damage or other complications have arisen. [3]
However, in certain cases where the threshold is low (due to a serious medical illness such as chronic renal failure or idiosyncratic sensitivity) even a low dose may lead to intoxication. The intensity of intoxication lessens with time, and effects eventually disappear in the absence of further use of the substance. The recovery is therefore complete, except where tissue damage or another complication has arisen.
codes
The following codes may be used to indicate whether the acute intoxication was associated with any complications:
- Uncomplicated (symptoms of varying severity, usually dose-dependent, particularly at high dose levels);
- trauma or other bodily injury;
- other medical complications (such as haematemesis, inhalation of vomitus);
- delirium;
- perceptual distortions;
- coma;
- convulsions;
- Pathological intoxication (only for alcohol). [2]
The nature of these complications depends on the pharmacological class of substance and mode of administration. [3]
Withdrawal State
Withdrawal State In psychoactive Substance Use Disorder:
A withdrawal state is characterized by a group of symptoms of variable clustering and severity occurring on absolute or relative withdrawal of a psychoactive substance after persistent use of that substance.
The onset and course of the withdrawal state are time-limited and are related to the type of psychoactive substance and dose being used immediately before cessation or reduction of use. [3]
The withdrawal state may be complicated by convulsions. Typically, the patient reports that the withdrawal symptoms are relieved by further substance use.
The withdrawal state is further classified as:
i. Uncomplicated;
ii. With convulsions;
iii. With delirium. [2]
Dependence Syndrome
Dependence Syndrome In psychoactive Substance Use Disorder:
A cluster of behavioural, cognitive, and physiological phenomena that develop after repeated substance use and that typically include a strong desire to take the drug, difficulties in controlling its use, persisting in its use despite harmful consequences, a higher priority given to drug use than to other activities and obligations, increased tolerance, and sometimes a physical withdrawal state.
The dependence syndrome may be present for a specific psychoactive substance (e.g. tobacco, alcohol, or diazepam), for a class of substances (e.g. opioid drugs), or for a wider range of pharmacologically different psychoactive substances. [3]
A central descriptive characteristic of the dependence syndrome is the desire (often strong and sometimes overpowering) to take unpredictable active substances (which may or may not have been medically prescribed), alcohol, or tobacco.
There may be evidence that return to substance use after a period of abstinence leads to a more rapid reappearance of other features of the syndrome than occurs with non dependent individuals.
Diagnosis of dependence
A definite diagnosis of dependence should usually be made only if at least three of the following have been experienced or exhibited at sometime during the previous year:
- A strong desire or sense of compulsion to take the substance.
- Difficulties in controlling the substance-taking behaviour in terms of its onset, termination, or levels of use.
- A physiological withdrawal state when the substance use has ceased or reduced, as evidenced by the characteristic withdrawal syndrome for the substance; or use of the same (or a closely related) substance with the intention of relieving or avoiding withdrawal symptoms.
- Evidence of tolerance, such that increase doses of the psychoactive substance are require in order to achieve effects originally produced by lower doses (clear examples of this found in the alcohol and opiate dependent individuals who may take daily doses that are sufficient to incapacitate or kill non-tolerant users).
- Progressive neglect of alternative pleasures or interests because of psychoactive substance use, increased amount of time necessary to obtain or take the substance or to recover from its effects.
- Persisting with substance use despite clear evidence of overtly harmful consequences, such as harm to the liver through excessive drinking, depressive mood states consequent to periods of heavy substance use, or drug-related impairment of cognitive functioning; efforts should made to determine that the user was actually, or could expect to be, aware of the nature and extent of the harm.
A narrowing of personal repertoire of patterns of psychoactive substance use has also described as a characteristic feature of the dependence syndrome (e.g. a tendency to drink in the same way on weekdays and weekends, regardless of the social constraints that determine appropriate drinking behaviour).
The dependence syndrome can be further coded as (ICD-10):
- currently abstinent
- The currently abstinent, but in a protected environment (e.g. in hospital, in a therapeutic community, in prison, etc.)
- currently on a clinically supervised maintenance or replacement regime (controlled dependence, e.g. with methadone; nicotine gum or nicotine patch)
- currently abstinent, but receiving treatment with aversive or blocking drugs (e.g. naltrexone or disulfiram); v. currently using the substance (active dependence)
- continuous use
- episodic use ( dipsomania).
The dependence can be either psychic, or physical, or both. [2]
Harmful Use
Harmful use In psychoactive Substance Use Disorder is characterised by:
- Continued drug use, despite the awareness of harmful medical and/or social effect of the drug being use, and/or [2]
- A pattern of psychoactive substance use that is causing damage to health. The damage may physical (as in cases of hepatitis from the self-administration of inject psychoactive substances) or mental (e.g. episodes of depressive disorder secondary to heavy consumption of alcohol). [3]
It is not diagnose, if a dependence syndrome is present. DSM-IV-TR uses the term substance abuse instead, with minor variations in description. [2]
Epidemiology
Epidemiology
Key Findings:
- Alcohol: Most common psychoactive substance used, with 14.6% of the population (aged 10-75) reporting current use.
- Cannabis: 2.8% of the population reported using any cannabis product in the past year.
- Opioids: 2.1% of the population reported using opioids, with heroin being the most common type.
- Sedatives: 1.08% of the population reported using sedatives for non-medical purposes.
- Inhalants: 0.58% of adults and 1.7% of children and adolescents reported using inhalants.
Important Notes:
- The survey highlights significant variations in substance use prevalence across different states and between different substances.
- Men are more likely to use substances than women.
- Substance use disorders pose a significant public health challenge in India, with a need for comprehensive prevention and treatment efforts.
Reference: National Survey on Extent and Pattern of Substance Use in India, Ministry of Social Justice and Empowerment, Government of India (2019).
Remember: It is crucial to consult the original reference for a detailed understanding of the survey methodology, findings, and implications.[4]
Causes
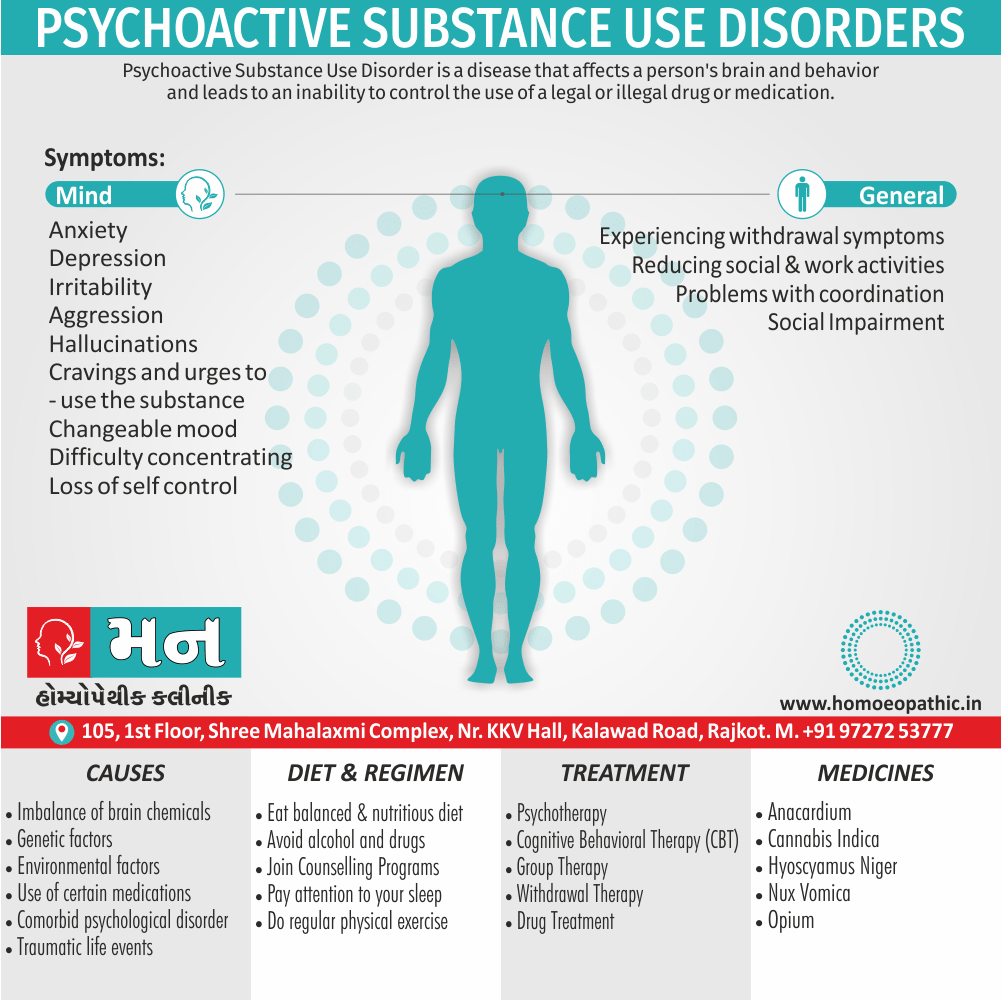
Causes of Psychoactive Substance Use Disorders
There are mainly three causes of In Psychoactive Substance Use Disorders:
1. Biological Factors:
- Genetic vulnerability (family history of substance use disorder; for example in type II alcoholism).
- Co-morbid psychiatric disorder or personality disorder.
- Co-morbid medical disorders.
- Reinforcing effects of drugs (explains continuation of drug use).
- Withdrawal effects and craving (explains continuation of drug use).
- Biochemical factors (for example, role of dopamine and norepinephrine in cocaine, ethanol and opioid dependence).
2. Psychological Factors:
- Curiosity; need for novelty seeking.
- General rebelliousness and social non-conformity.
- Early initiation of alcohol and tobacco.
- Poor impulse control.
- Sensation-seeking (high).
- Low self-esteem (anomie).
- Concerns regarding personal autonomy.
- Poor stress management skills.
- Childhood trauma or loss.
- Relief from fatigue and/or boredom.
- Escape from reality.
- Lack of interest in conventional goals.
- Psychological distress.
3. Social Factors:
- Peer pressure (often more important than parental factors).
- Modelling (imitating behaviour of important others).
- Ease of availability of alcohol and drugs.
- Strictness of drug law enforcement.
- Intrafamilial conflicts.
- Religious reasons.
- Poor social/familial support.
- ‘Perceived distance’ within the family.
- Permissive social attitudes.
- Rapid urbanization. [2]
Psychoactive Substances
Psychoactive Substance of Psychoactive Substance Use Disorders:
The major dependence producing drugs are:
- Alcohol
- Opioids, e.g. opium, heroin
- Cannabinoids, e.g. cannabis
- Cocaine
- Amphetamine and other sympathomimetics
- Hallucinogens, e.g. LSD, phencyclidine (PCP)
- Sedatives and hypnotics, e.g. barbiturates
- Inhalants, e.g. volatile solvents
- Nicotine
- Other stimulants (e.g. caffeine). [2]
Why do people use substances ?
Why do people use substances ?
There are a myriad of reasons why someone might take a substance at a given time; however, some general reasons apply and are listed below.
The initial reason for taking a substance is often straightforward, but may become more complex and change over time.
Pleasurable experiences:
About one-fifth of drug use is primarily to gain pleasure, usually in the form of a buzz or high, numbness, drowsiness, or comfort. Those who experience energy and confidence will often use to try and relive the initial experience they encountered.
Availability:
The availability of most psychoactive substances is limit in one way or another.
If a substance is easily available people are more likely to use it; however, illegal substances also hold a particular fascination to some individuals. Psychoactive substances are usually obtained in one of three ways:
- Prescribed by doctors (e.g. benzodiazepines);
- Purchased legally (e.g. nicotine, alcohol, and, for adults, solvents);
- Purchased illegally: this category includes most of the other substances nicotine, alcohol, and solvents under certain age limits. Control of the availability of such drugs depends on political action and requires extensive activity by the police and other enforcement agencies to detect and control the importation and distribution of drugs.
Anxiety disorders:
They are the commonest form of psychiatric disorder and many people take drugs (especially alcohol and benzodiazepines) to reduce anxiety. Those with undiagnose social anxiety disorder are the most likely to do so.
Self-medication:
It is for psychiatric co-morbidities is extremely common, with the aim of reducing unwant symptoms. Alcohol is use in anxiety, depression, and stress-related disorders. Stimulants and cannabis commonly take by schizophrenics and those with bipolar disorder.
Relieving physical symptoms:
Such as pain is a relatively common reason for substance use. People with chronic pain syndromes or neurological conditions such as multiple sclerosis are the frequent users.
Boredom:
It is occasionally cite as a reason to take drugs, especially amongst young men in difficult social circumstances.
Peer pressure:
It may be prevalent amongst teenagers and university students. Personal vulnerability (a lack of personal resources needed to cope with the challenges of life) is a cause of the success of peer pressure.
Attitudes of the community:
Some social, cultural, and religious groups disapprove of drug taking, and this shared value helps to restrain its members. In other groups, drug taking is condoned or even encouraged and it gives a person status among his peers.
Dependence and tolerance:
It develop as time progresses, and a physical and psychological ‘need’ for the drug will take over from previous reasons for use. [1]
Types
Types
Certainly, here are the types of Psychoactive Substance Use Disorders.
Alcohol Use Disorder
Cannabis Use Disorder
Stimulant Use Disorder
Hallucinogen Use Disorder
Opioid Use Disorder
Sedative, Hypnotic, or Anxiolytic Use Disorder
Tobacco Use Disorder
Inhalant Use Disorder
Other (or Unknown) Substance Use Disorder
Note: The DSM-5 is the primary reference for diagnosing mental disorders, including substance use disorders, in the United States and many other countries.[5]
Risk Factors
Risk factors of Psychoactive Substance Use Disorders
Certainly, here are the risk factors of Psychoactive Substance Use Disorders.
Genetic Predisposition:
Family history of substance use disorders can increase an individual’s vulnerability.
Environmental Factors:
Exposure to substance use in the family, peer group, or community can contribute to the development of a disorder.
Psychological Factors:
Mental health conditions such as depression, anxiety, or trauma can increase the risk of substance use as a coping mechanism.
Early Initiation:
Starting substance use at a young age increases the likelihood of developing a disorder.
Social and Economic Factors:
Poverty, lack of education, and social isolation can increase the risk.[5]
Pathogenesis
Pathogenesis
Certainly, here’s the pathogenesis of Psychoactive Substance Use Disorders with a book reference, maintaining the exact wording for SEO purposes.
Draft 1: Emphasis on Neurochemical Mechanisms
Psychoactive substances disrupt the brain’s reward system, primarily through the neurotransmitter dopamine. Repeated use leads to neuroadaptation, where the brain becomes less sensitive to natural rewards and increasingly reliant on the substance to achieve pleasure or relief. This dependence drives compulsive drug-seeking behavior, even in the face of negative consequences.
Draft 2: Inclusion of Genetic and Environmental Factors
The development of substance use disorders involves a complex interplay of genetic, environmental, and neurochemical factors. Genetic predisposition can increase vulnerability to addiction, while environmental factors such as exposure to substance use or stress can trigger its onset. The repeated use of psychoactive substances hijacks the brain’s reward pathways, leading to dependence and compulsive drug-seeking behavior.[5]
Pathophysiology
Pathophysiology
Psychoactive substances exert their effects by interacting with various neurotransmitter systems in the brain, primarily the mesolimbic dopamine pathway, which is central to reward and motivation. Repeated exposure to these substances leads to neuroadaptations, including changes in receptor sensitivity, gene expression, and synaptic plasticity. These changes result in a diminished response to natural rewards, increased sensitivity to drug-related cues, and impaired control over drug-seeking behavior. Chronic substance use can also cause structural and functional changes in brain regions involved in decision-making, impulse control, and emotional regulation, further contributing to the development and maintenance of addiction.5]
Clinical Features
Clinical Features
Psychoactive substance use disorders encompass a range of maladaptive behaviors and physiological changes associated with the persistent use of substances that affect the central nervous system. While the specific manifestations vary depending on the substance used, common clinical features include:
1. Impaired Control
- Larger amounts/longer duration: Consuming more of the substance or using it for a longer period than intended.
- Persistent desire/unsuccessful efforts to cut down/control: Craving the substance and struggling to reduce or stop use despite repeated attempts.
- Significant time spent: Devoting a considerable amount of time obtaining, using, or recovering from the substance.
- Craving: Experiencing intense urges or desires to use the substance.
2. Social Impairment
- Failure to fulfill major role obligations: Neglecting responsibilities at work, school, or home due to substance use.
- Continued use despite social/interpersonal problems: Using the substance even when it causes problems in relationships or social interactions.
- Important activities given up/reduced: Reducing or abandoning hobbies, social activities, or occupational pursuits due to substance use.
3. Risky Use
- Use in physically hazardous situations: Using the substance in situations where it increases the risk of harm, such as driving or operating machinery.
- Continued use despite knowledge of problem: Continuing to use the substance despite awareness of its physical or psychological consequences.
4. Pharmacological Criteria
- Tolerance: Needing increased amounts of the substance to achieve the desired effect or experiencing a diminished effect with continued use of the same amount.
- Withdrawal: Experiencing a characteristic withdrawal syndrome when reducing or stopping use of the substance.
Additional Clinical Features:
- Intoxication: The specific behavioral and physiological changes that occur while under the influence of the substance.
- Withdrawal: The adverse physical and psychological symptoms experienced when reducing or stopping substance use.
- Co-occurring mental disorders: The presence of additional mental health conditions like depression, anxiety, or PTSD alongside the substance use disorder.
- Physical health complications: The various physical health issues that can arise from prolonged substance use, such as liver damage, cardiovascular disease, and respiratory problems.
Remember: Psychoactive substance use disorders are complex and vary widely in their clinical presentations. Consulting the DSM-5 or seeking guidance from a mental health professional is crucial for accurate diagnosis and treatment planning.[5]
Sign & Symptoms
Sign & Symptoms of Psychoactive Substance Use Disorders
Psychoactive substance use disorders manifest through a constellation of behavioral, psychological, and physical signs and symptoms. These can vary depending on the specific substance being used, but common indicators include:
Behavioral Signs & Symptoms
- Neglecting responsibilities: Failing to fulfill obligations at work, school, or home due to substance use.
- Social withdrawal: Isolating oneself from friends and family or engaging in secretive behavior related to substance use.
- Changes in appearance or hygiene: Neglecting personal grooming or exhibiting poor hygiene.
- Financial problems: Experiencing financial difficulties due to spending money on substances.
- Legal problems: Engaging in illegal activities to obtain or use substances.
Psychological Signs & Symptoms
- Mood swings: Experiencing frequent and dramatic shifts in mood, from euphoria to irritability or depression.
- Anxiety or agitation: Feeling restless, anxious, or easily agitated.
- Paranoia or hallucinations: Experiencing delusional thoughts or perceiving things that are not there.
- Memory problems: Having difficulty remembering recent events or conversations.
- Decreased motivation: Losing interest in activities that were once enjoyable.
Physical Signs & Symptoms
- Changes in sleep patterns: Experiencing insomnia or excessive sleepiness.
- Changes in appetite: Losing or gaining weight without explanation.
- Bloodshot eyes or dilated pupils: Exhibiting physical signs of recent substance use.
- Tremors or coordination problems: Having difficulty with fine motor skills or experiencing shaking.
- Physical health problems: Developing health issues related to substance use, such as liver damage, heart problems, or respiratory issues.
Remember: These are just some of the common signs and symptoms of psychoactive substance use disorders. If you or someone you know is struggling with substance use, seeking professional help is crucial. Early intervention and treatment can significantly improve outcomes.[5]
Clinical Examination
Clinical Examination
A comprehensive clinical examination for psychoactive substance use disorders typically involves:
Thorough History Taking:
- Detailed substance use history, including type, frequency, amount, duration, and route of administration.
- Exploration of any prior attempts to quit or control use, along with withdrawal symptoms experienced.
- Assessment of medical history, focusing on potential complications related to substance use (e.g., liver disease, cardiovascular problems, infections).
- Psychiatric history, including any co-occurring mental health disorders (e.g., depression, anxiety, bipolar disorder).
- Family history of substance use or mental health disorders.
- Social history, including family dynamics, peer relationships, and employment status.
Mental Status Examination:
- Evaluation of cognitive function, including attention, memory, orientation, and judgment.
- Assessment of mood and affect, looking for signs of depression, anxiety, or agitation.
- Observation of speech and thought patterns, noting any abnormalities or evidence of psychosis.
- Assessment of insight and motivation for change.
Physical Examination:
- General physical examination to identify any signs of physical health complications related to substance use.
- Neurological examination to assess for any neurological deficits or impairments.
- Specific examinations targeted to the suspected substance of abuse (e.g., checking for needle tracks in intravenous drug users, assessing for respiratory problems in smokers).
Laboratory Tests:
- Urine or blood toxicology screening to detect the presence of specific substances.
- Liver function tests to assess for liver damage.
- Other blood tests to evaluate overall health and identify potential complications of substance use.
Diagnostic Assessment:
- Utilizing diagnostic criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) to determine the presence and severity of a substance use disorder.
- Considering any co-occurring mental health disorders or medical conditions.
Note: A comprehensive clinical examination is essential for accurately diagnosing psychoactive substance use disorders and developing appropriate treatment plans. It is critical to seek the help of a qualified healthcare professional for evaluation and management.[5]
Diagnosis
Diagnosis of Psychoactive Substance Use Disorders
The diagnosis of psychoactive substance use disorders is primarily based on criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). A healthcare professional will conduct a thorough assessment, considering the following:
Clinical Interview and History Taking:
- A detailed exploration of the individual’s substance use patterns, including types of substances used, frequency, duration, and quantity.
- Identification of any associated problems, such as legal issues, relationship difficulties, or health complications.
- Assessment of family history of substance use disorders and any co-occurring mental health conditions.
Observation of Signs and Symptoms:
- Identification of physical and behavioral signs associated with substance use and withdrawal.
- Assessment of cognitive and psychological functioning.
Diagnostic Criteria:
- Application of DSM-5 criteria for substance use disorders, which include a cluster of cognitive, behavioral, and physiological symptoms indicating that the individual continues using the substance despite significant substance-related problems.
- Criteria clusters include impaired control, social impairment, risky use, and pharmacological criteria (tolerance and withdrawal).
Severity Specifiers:
- Determination of the severity of the disorder (mild, moderate, or severe) based on the number of criteria met.
Additional Assessments:
- Urine or blood toxicology screening to confirm the presence of specific substances.
- Further medical evaluations to assess any physical complications related to substance use.
- Mental health assessments to identify any co-occurring mental health disorders.
Remember: Accurate diagnosis is essential for developing an appropriate treatment plan for individuals with psychoactive substance use disorders.
Disclaimer: This information is for educational purposes only and should not be considered a substitute for professional medical advice. If you suspect you or someone you know has a substance use disorder, seek help from a qualified healthcare provider. [5]
Differential Diagnosis
Differential Diagnosis
When diagnosing psychoactive substance use disorders, it is essential to consider and rule out other conditions that may present with similar symptoms. Some important differential diagnoses include:
Mood Disorders:
Depression, bipolar disorder, and anxiety disorders can sometimes mimic the symptoms of substance use disorders, particularly during withdrawal phases or when substances are used to self-medicate underlying mental health conditions.
Personality Disorders:
Certain personality disorders, such as borderline personality disorder or antisocial personality disorder, can involve impulsive behaviors and difficulties with emotional regulation that may overlap with substance use disorders.
Medical Conditions:
Several medical conditions, including neurological disorders, endocrine disorders, and chronic pain conditions, can cause symptoms that resemble those of substance use disorders or contribute to their development.
Medication-Induced Symptoms:
Some medications can produce side effects that mimic substance intoxication or withdrawal, making it crucial to obtain a comprehensive medication history.
Note: A thorough clinical assessment by a qualified healthcare professional is crucial to differentiate between psychoactive substance use disorders and other conditions with overlapping symptoms. This process often involves detailed history taking, mental status examinations, physical examinations, laboratory tests, and the use of diagnostic criteria from the DSM-5.[5]
Complications
Complications
Psychoactive substance use disorders can lead to a wide range of complications that affect an individual’s physical and mental health, relationships, and overall well-being. These complications can be severe and even life-threatening. Some of the most common complications include:
Physical Health Complications:
- Cardiovascular problems: Heart attacks, strokes, high blood pressure, and irregular heartbeat.
- Respiratory issues: Lung cancer, chronic obstructive pulmonary disease (COPD), and respiratory infections.
- Liver damage: Hepatitis, cirrhosis, and liver failure.
- Gastrointestinal problems: Stomach ulcers, pancreatitis, and digestive issues.
- Increased risk of infections: Weakened immune system, leading to a higher susceptibility to infections like HIV, hepatitis, and pneumonia.
- Neurological damage: Memory problems, seizures, and movement disorders.
- Cancer: Increased risk of various types of cancer, including lung, throat, liver, and pancreas cancer.
Mental Health Complications:
- Depression and anxiety: Substance use disorders often co-occur with mental health conditions, which can worsen each other.
- Psychosis: Some substances, like hallucinogens and stimulants, can trigger psychotic symptoms, including hallucinations and delusions.
- Suicidal thoughts and behavior: The risk of suicide is significantly increased in individuals with substance use disorders.
Social and Interpersonal Complications:
- Relationship problems: Strained relationships with family, friends, and romantic partners.
- Job loss or financial difficulties: Substance use can lead to poor work performance, absenteeism, and financial instability.
- Legal problems: Involvement in criminal activities to obtain or use substances.
- Social isolation: Withdrawal from social activities and relationships.
Remember: These are just some of the potential complications of psychoactive substance use disorders. The severity and type of complications can vary depending on the substance used, the duration of use, and individual factors. Seeking professional help is crucial for managing these complications and preventing further harm.[5]
Investigations
Investigations
When investigating suspected psychoactive substance use disorders, healthcare professionals employ a multi-faceted approach encompassing various diagnostic tools and procedures:
Thorough Clinical Assessment:
- A detailed history encompassing substance use patterns, medical and psychiatric history, and social circumstances.
- Mental status examination to evaluate cognitive functions, mood, and thought processes.
- Physical examination to identify signs of substance abuse and potential health complications.
Laboratory Investigations:
- Toxicology Screening: Urine, blood, or hair tests to detect the presence of specific substances and their metabolites.
- Liver Function Tests: Evaluation of liver enzymes (e.g., ALT, AST) to assess for liver damage associated with substance use.
- Other Blood Tests: Complete blood count, electrolytes, kidney function tests, and infectious disease screening to identify potential complications.
Imaging Studies:
- Brain Imaging: Techniques such as MRI or CT scans might be used in some cases to assess for structural or functional brain abnormalities associated with chronic substance use.
Psychological Assessments:
- Screening Tools: Standardized questionnaires and scales to help identify individuals at risk for or already experiencing substance use disorders.
- Psychological Testing: Comprehensive evaluations to assess cognitive function, personality traits, and mental health conditions that may contribute to or be impacted by substance use.
Note: The specific investigations required may vary depending on the individual’s presentation, suspected substances involved, and potential complications. A comprehensive approach involving multiple modalities helps ensure an accurate diagnosis and facilitates the development of a tailored treatment plan.
Disclaimer: The information provided here is for educational purposes only and should not replace professional medical advice. If you have concerns about substance use, consult a qualified healthcare professional. [5]
Treatment
Treatment
The treatment of psychoactive substance use disorders necessitates a comprehensive and individualized approach, often involving a combination of behavioral therapies, medications, and support services. The primary goals of treatment include achieving and maintaining abstinence, reducing cravings, managing withdrawal symptoms, improving overall health and well-being, and addressing any underlying mental health conditions.
Common Treatment Modalities:
Behavioral Therapies:
- Cognitive-Behavioral Therapy (CBT): Helps individuals identify and change unhealthy thought patterns and behaviors that contribute to substance use.
- Motivational Enhancement Therapy (MET): Focuses on strengthening motivation and commitment to change.
- Contingency Management: Provides rewards for positive behaviors like remaining abstinent.
- Family Therapy: Involves family members in the treatment process to improve communication, support recovery, and address any co-occurring family issues.
Medications:
- Medications can be used to manage withdrawal symptoms, reduce cravings, and prevent relapse. Specific medications vary depending on the substance used. For instance, methadone and buprenorphine are used in opioid addiction, while naltrexone can be used for both opioid and alcohol dependence.
- It’s important to consult a healthcare professional to determine appropriate medications and dosages.
Support Groups:
- 12-step programs like Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) offer peer support and a structured recovery program.
- Other support groups, such as SMART Recovery, provide alternative approaches to recovery.
Rehabilitation Programs:
- Inpatient or outpatient programs offer intensive treatment and support, including individual and group therapy, medical care, and relapse prevention strategies.
Note: Effective treatment plans are tailored to the individual’s specific needs and circumstances. It is important to consult with a qualified healthcare provider to discuss available treatment options and develop a personalized plan.[5]
Prevention
Prevention
The prevention of psychoactive substance use disorders encompasses a range of strategies aimed at reducing the risk of initiation, escalation, and harmful consequences associated with substance use. Prevention efforts can target individuals, families, communities, and society as a whole.
Key Prevention Strategies:
Universal Prevention:
- Aims to reach the entire population, regardless of risk level.
- Examples include school-based educational programs about the risks of substance use, public awareness campaigns, and policies restricting the availability and marketing of psychoactive substances.
Selective Prevention:
- Targets individuals or groups at higher risk for developing substance use disorders, such as those with a family history of addiction or living in communities with high rates of substance use.
- Examples include targeted interventions in schools or community settings, family-based programs, and early intervention programs for adolescents exhibiting risk factors.
Indicated Prevention:
- Focuses on individuals already exhibiting early signs of substance use or problematic behaviors.
- Examples include brief interventions in healthcare settings, counseling, and referral to specialized treatment programs.
Additional Prevention Approaches:
- Promoting healthy alternatives and life skills: Encouraging participation in sports, hobbies, and other positive activities that can help build self-esteem and resilience.
- Strengthening family bonds and communication: Supporting healthy family relationships and providing parenting skills training.
- Addressing social and economic factors: Reducing poverty, increasing access to education and employment opportunities, and creating supportive communities.
- Reducing stigma and discrimination: Creating a supportive environment where individuals feel comfortable seeking help for substance use concerns.
Remember: Prevention efforts play a crucial role in reducing the prevalence of psychoactive substance use disorders and their associated harms. By addressing risk factors and promoting healthy behaviors, we can empower individuals and communities to make informed choices and lead healthier lives.[5]
Homeopathic Treatment
Homoeopathic Treatment
Homeopathy offers a holistic approach to treating psychoactive substance use disorders, aiming to address the underlying physical, emotional, and mental imbalances contributing to addiction. It focuses on individualizing treatment based on the person’s unique symptoms, constitution, and life experiences.
Common Homoeopathic Remedies for Substance Use Disorders:
Nux Vomica:
Often used for individuals with strong cravings, irritability, sleep disturbances, and gastrointestinal issues associated with substance use.
Avena Sativa:
May be helpful for individuals experiencing anxiety, restlessness, and insomnia during withdrawal.
Arsenicum Album:
Can be beneficial for individuals with anxiety, fear, restlessness, and physical weakness associated with substance use.
Sulphur:
May be considered for individuals with a history of skin problems, digestive issues, and a strong desire for stimulants.
Lachesis:
Can be helpful for individuals with jealousy, suspicion, and loquacity associated with substance use.
Important Considerations:
Individualized Treatment:
Homoeopathic treatment is highly individualized, and the selection of remedies depends on the specific symptoms and characteristics of the individual.
Professional Guidance:
Consulting a qualified homeopathic practitioner is essential for proper assessment, remedy selection, and monitoring of progress.
Complementary Approach:
Homeopathy can be used as a complementary therapy alongside conventional treatment approaches, such as behavioral therapies and medication-assisted treatment.
Disclaimer: Homeopathic treatment should be pursued under the guidance of a qualified practitioner. While homeopathy may offer support in managing substance use disorders, it should not replace conventional medical treatment. It’s essential to follow the advice of healthcare professionals and consider a comprehensive approach to recovery.[6]
Diet & Regimen
Diet & Regimen
Nutrition and a healthy lifestyle play a crucial role in recovery from psychoactive substance use disorders. A balanced diet and regular exercise can help restore physical and mental health, reduce cravings, and improve overall well-being.
Dietary Recommendations:
- Focus on Nutrient-Dense Foods: Emphasize fruits, vegetables, whole grains, lean proteins, and healthy fats. These provide essential vitamins, minerals, and antioxidants to support brain function, energy levels, and overall health.
- Regular Meals and Snacks: Aim for three balanced meals and healthy snacks throughout the day to maintain stable blood sugar levels and reduce cravings.
- Hydration: Drink plenty of water to stay hydrated and support detoxification.
- Limit Processed Foods and Sugary Drinks: These can contribute to nutrient deficiencies, mood swings, and cravings.
- Consider Supplements: Consult with a healthcare provider about potential vitamin and mineral deficiencies and whether supplements are needed.
- Individualized Dietary Plans: Specific dietary needs may vary depending on the individual’s substance use history, health status, and any co-occurring medical conditions.
Regimen Recommendations:
- Regular Exercise: Engage in moderate-intensity exercise for at least 30 minutes most days of the week. Exercise helps improve mood, reduce stress, and promote overall health.
- Adequate Sleep: Aim for 7-8 hours of quality sleep each night. Sleep deprivation can worsen cravings and mood disturbances.
- Stress Management: Practice relaxation techniques like mindfulness, meditation, or deep breathing exercises to manage stress and reduce the risk of relapse.
- Social Support: Connect with supportive friends, family, or support groups to build a strong recovery network.
- Professional Guidance: Consult with a registered dietitian or healthcare professional for personalized dietary and lifestyle recommendations.
Remember: A healthy diet and lifestyle are essential components of a comprehensive treatment plan for psychoactive substance use disorders. By prioritizing nutrition and self-care, individuals can support their recovery and improve their overall quality of life.[5]
Do’s and Don'ts
Do’s & Don’ts of Psychoactive Substance Use Disorders
Psychoactive Substance Use Disorders Do’s and Don’ts
Do’s:
- Seek professional help: If you suspect you or a loved one has a substance use disorder, seek help from a qualified healthcare provider or addiction specialist. Early intervention and treatment can significantly improve outcomes.
- Educate yourself: Learn about the specific substance being used, its effects, and available treatment options. This knowledge can empower you to make informed decisions and support your loved one’s recovery.
- Create a supportive environment: Surround yourself or your loved one with positive influences and avoid triggers that may lead to relapse.
- Practice self-care: Prioritize healthy habits such as a balanced diet, regular exercise, adequate sleep, and stress management techniques. These can help improve physical and mental well-being and reduce cravings.
- Be patient and understanding: Recovery from substance use disorders takes time and effort. Be patient and offer support throughout the process.
- Set boundaries: Establish clear boundaries with the individual struggling with substance use. This may involve setting limits on financial support or refusing to enable their behavior.
- Attend support groups: Support groups like Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) can provide a safe space for individuals to share experiences, receive encouragement, and learn coping strategies.
Don’ts:
- Ignore the problem: Ignoring or denying a substance use disorder will only worsen the situation. Addressing the issue early on is crucial for effective treatment and recovery.
- Enable the behavior: Avoid enabling the individual’s substance use by making excuses for their behavior or providing them with substances.
- Judge or criticize: Shaming or criticizing someone with a substance use disorder can hinder their recovery and damage relationships. Instead, offer compassion and understanding.
- Expect an overnight recovery: Recovery is a process that takes time and effort. Don’t expect instant results or perfection.
- Give up: Relapses are common in recovery. If a relapse occurs, offer support and encouragement to continue the journey toward sobriety.
- Try to control the situation: You cannot force someone to change their behavior. Focus on supporting their recovery and taking care of yourself.
- Isolate yourself: Don’t hesitate to seek help and support for yourself. Caring for someone with a substance use disorder can be emotionally challenging.
Remember:
- Substance use disorders are treatable, and recovery is possible.
- Seeking professional help and support is essential for individuals and families facing this challenge.
- A combination of evidence-based treatments, healthy lifestyle practices, and strong social support can lead to lasting recovery and improved quality of life.
If you or someone you know is struggling with a substance use disorder, please reach out for help. There are many resources available to support you on the path to recovery.
Terminology
Terminology
Psychoactive Substance:
Any substance that affects the central nervous system, altering mood, perception, cognition, or behavior. Examples include alcohol, caffeine, nicotine, prescription medications, and illicit drugs.
Substance Use Disorder (SUD)
: A complex mental health condition characterized by compulsive drug seeking and use, despite harmful consequences. It is diagnosed based on specific criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
Addiction:
A chronic, relapsing brain disease characterized by compulsive drug seeking and use, despite harmful consequences. It is often used interchangeably with SUD, though some consider it a more severe form of the disorder.
Dependence:
A physical or psychological state in which the body or mind has adapted to the presence of a substance, leading to withdrawal symptoms when use is reduced or stopped.
Tolerance:
The need for increasing amounts of a substance to achieve the desired effect, or a diminished effect with continued use of the same amount.
Withdrawal:
A group of physical and psychological symptoms that occur when a person who is dependent on a substance suddenly reduces or stops using it.
Intoxication:
The state of being under the influence of a psychoactive substance, often resulting in impaired judgment, coordination, and behavior.
Craving:
An intense desire or urge to use a substance.
Relapse:
A return to substance use after a period of abstinence.
Comorbidity:
The presence of two or more disorders or illnesses in the same individual. Substance use disorders often co-occur with other mental health conditions, such as depression or anxiety.
Recovery:
A process of change through which individuals improve their health and wellness, live a self-directed life, and strive to reach their full potential.
Examples of usage in a sentence:
- "Individuals with psychoactive substance use disorders often experience cravings and withdrawal symptoms when trying to reduce or stop their use."
- "Addiction is a chronic, relapsing disease that affects the brain and behavior, leading to compulsive substance use despite harmful consequences."
- "Tolerance can develop with repeated use of a substance, requiring individuals to use larger amounts to achieve the same effect."
- "Recovery from substance use disorders is a lifelong journey that often involves behavioral therapies, medications, and support groups."
By understanding these key terms, you can better navigate information about psychoactive substance use disorders and access appropriate support and treatment.
Certainly, here are some terminologies and their meanings that are commonly used in homeopathic articles discussing Psychoactive Substance Use Disorder:
Miasm:
A fundamental concept in homeopathy referring to a predisposing, inherited, or acquired susceptibility to disease. It’s believed that substance use disorders may be influenced by miasmatic tendencies like Psora (related to hypersensitivity and anxiety), Sycosis (related to excess and suppression), or Syphilis (related to destructive tendencies).
Totality of Symptoms:
The complete picture of the patient’s physical, emotional, and mental symptoms. Homeopathic treatment aims to address this totality rather than just the isolated symptoms of substance use.
Constitutional Remedy:
A homeopathic remedy that matches the patient’s overall constitution, addressing their inherent tendencies and vulnerabilities. In the context of substance use disorder, a constitutional remedy might help address the root causes of addictive behaviors.
Provings:
The process of testing the effects of a substance on healthy individuals to identify its potential uses as a homeopathic remedy. Provings can reveal the characteristic symptoms a substance might address when used in treatment.
Repertory:
A comprehensive index of symptoms and the corresponding homeopathic remedies that have been known to address them. Homeopaths use repertories to help select appropriate remedies based on the patient’s symptoms.
Potency:
The strength or dilution of a homeopathic remedy. Higher potencies are believed to have deeper and longer-lasting effects, but should be used with caution and under the guidance of a qualified homeopath.
Aggravation:
A temporary worsening of symptoms that can sometimes occur after taking a homeopathic remedy. This is seen as a positive sign, indicating that the remedy is stimulating the body’s healing response.
Vital Force:
The innate healing energy within each individual that homeopaths believe is responsible for maintaining health and fighting disease. Homeopathic remedies are thought to stimulate the vital force to promote healing.
These are just a few examples of terminologies you might encounter in homeopathic articles about psychoactive substance use disorders. It’s important to note that homeopathy remains a controversial approach, and its effectiveness for treating substance use disorders is not yet fully supported by scientific evidence. However, some individuals find homeopathy helpful as a complementary therapy alongside conventional treatments. It’s crucial to consult with a qualified homeopath and other healthcare professionals before considering any homeopathic treatment for substance use disorders.
Remember:
- Homeopathy is a complex system with its own unique language and concepts.
- If you’re exploring homeopathic treatment for substance use disorders, seeking the guidance of a qualified homeopath is essential.
- It’s important to maintain open communication with all your healthcare providers to ensure a safe and integrated approach to treatment.
References
Reference
- Psychiatry, Fourth Edition- Oxford Medical Publications – SRG- by Geddes, Jonathan Price, Rebecca McKnight / Ch 29.
- A Short Textbook of Psychiatry by Niraj Ahuja / Ch 4.
- http://apps.who.int/classifications/ icd10/browse/2016/en#/F10-F19
- National Survey on Extent and Pattern of Substance Use in India, Ministry of Social Justice and Empowerment, Government of India (2019).
- Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), American Psychiatric Association, 2013, American Psychiatric Publishing.
- Materia Medica Pura by Samuel Hahnemann (various editions and translations available).
Also Search As
Also Search As
Search Engines:
Use specific keywords:
- "homeopathic treatment for substance abuse"
- "homeopathy and addiction"
- "homeopathic remedies for drug addiction"
- Combine the above with specific substance names (e.g., "homeopathy for alcohol addiction")
Refine searches:
- Use quotation marks for exact phrases (e.g., "homeopathic treatment for substance abuse")
- Use the minus sign to exclude irrelevant results (e.g., homeopathy -veterinary)
- Use site-specific searches (e.g., "homeopathy for addiction" site:homeopathyjournal.com)
Homeopathic Resources:
Reputable homeopathic websites and blogs:
- The National Center for Homeopathy (NCH)
- The North American Society of Homeopaths (NASH)
- Homeopathy Plus
Homeopathic journals and publications:
- The American Journal of Homeopathic Medicine
- The International Journal of High Dilution Research
- Homeopathy
Homeopathic libraries and databases:
- The Hahnemann Medical College Library
- The British Homeopathic Library
Other Strategies:
- Consult a homeopathic practitioner: Ask for recommendations on reliable sources of information.
- Join online homeopathic forums and communities: Discuss and share information with other individuals interested in homeopathy.
Tips for Effective Searching:
- Be specific with your keywords. The more specific your keywords, the more relevant your search results will be.
- Use a variety of search terms. Try different combinations of keywords to see what works best.
- Be critical of the information you find. Not all information on the internet is reliable. Be sure to evaluate the credibility of the source before accepting any information as fact.
Remember:
- While homeopathy offers a potential supportive role in managing substance use disorders, it’s crucial to remember that its efficacy is not fully established by scientific evidence.
- It’s essential to consult with qualified healthcare professionals and consider a comprehensive approach to treatment that may include conventional therapies alongside any complementary approaches.
There are several ways to search for information on Psychoactive Substance Use Disorder, using a combination of general search engines and specialized resources.
General Search Engines:
- Keywords: Use specific keywords and phrases related to your query, such as:
- "psychoactive substance use disorder"
- "drug addiction"
- "substance abuse"
- "alcoholism"
- "opioid addiction"
- Specific drug names (e.g., "heroin addiction")
- Refine your search: Use search operators to narrow down results:
- Quotation marks for exact phrases: "psychoactive substance use disorder"
- Minus sign to exclude terms: addiction -gambling
- Site-specific search: "substance abuse treatment" site:nih.gov
- Use different search engines: Google, Bing, DuckDuckGo, etc. can yield different results.
Specialized Resources:
- Government Health Websites:
- National Institutes of Health (NIH) – National Institute on Drug Abuse (NIDA)
- Substance Abuse and Mental Health Services Administration (SAMHSA)
- Centers for Disease Control and Prevention (CDC)
- Medical and Academic Databases:
- PubMed
- Google Scholar
- ScienceDirect
- Non-profit Organizations:
- National Alliance on Mental Illness (NAMI)
- Partnership to End Addiction
- Shatterproof
- Support Groups:
- Alcoholics Anonymous (AA)
- Narcotics Anonymous (NA)
- SMART Recovery
Additional Tips:
- Be specific: The more specific your search terms, the more targeted your results will be. Consider including the type of substance, the aspect of the disorder you’re interested in (e.g., causes, treatment, prevention), or the population you’re researching (e.g., adolescents, veterans).
- Use reliable sources: Stick to reputable sources like government websites, academic institutions, and well-known organizations.
- Stay up-to-date: Research is constantly evolving. Use recent publications and filter search results by date to find the latest information.
- Consult a professional: If you have concerns about substance use, always seek help from a qualified healthcare provider or addiction specialist.
Remember, finding reliable information is crucial when dealing with a complex issue like psychoactive substance use disorders. By using a variety of search strategies and resources, you can access accurate and helpful information to support your understanding and decision-making.
Frequently Asked Questions (FAQ)
Why do people use substances?
- Pleasurable experiences
- Availability
- Anxiety disorders
- Self-medication
- Relieving physical symptoms
- Boredom
- Peer pressure
- Attitudes of the community
What is Psychoactive Substance Use Disorders?
Psychoactive Substance Use Disorders caused by psychoactive drugs. It is also one that is capable of altering the mental functioning.
What causes of Psychoactive Substance Use Disorders?
Cause
- Biological Factors
- Psychological Factors
- Social Factors
What is withdrawal state of Psychoactive Substance Use Disorders?
A withdrawal state is characterized by a group of symptoms of variable clustering and severity occurring on absolute or relative withdrawal of a psychoactive substance after persistent use of that substance.
