Recurrent abortion or Habitual Abortion
Definition
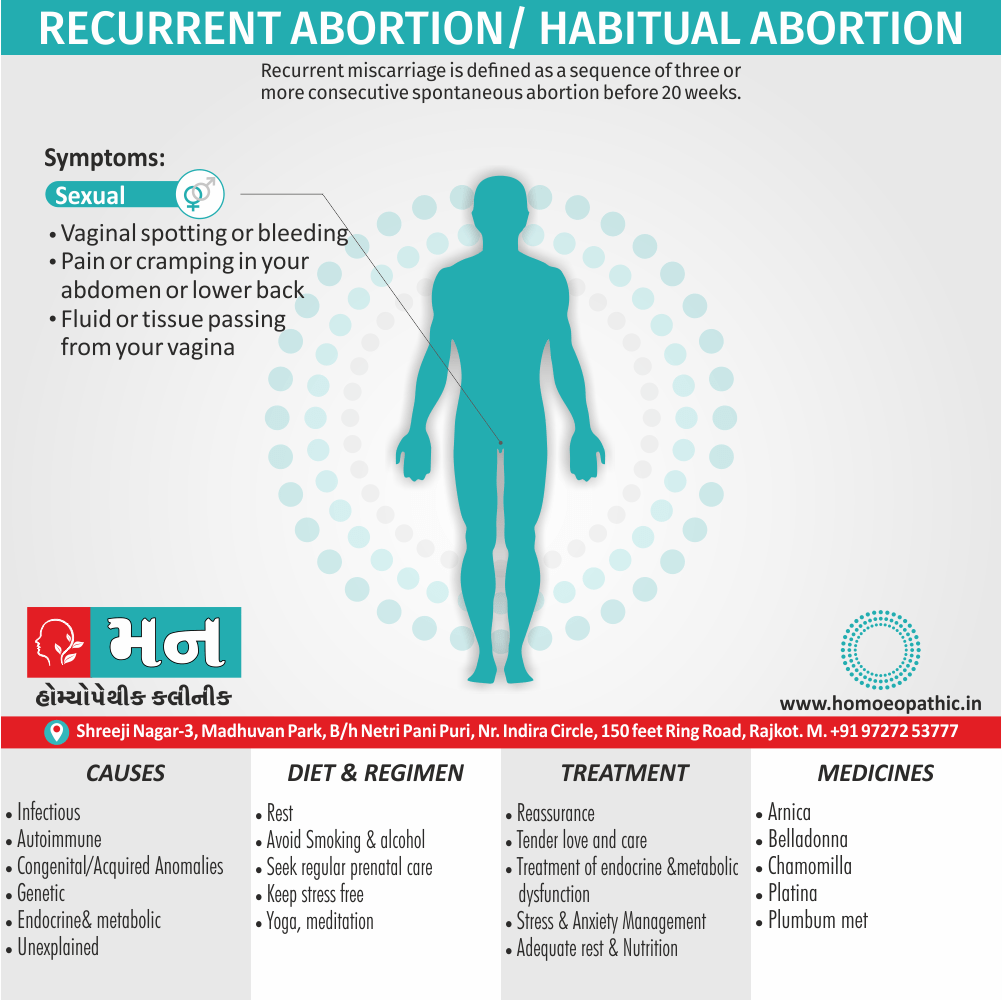
Recurrent miscarriage is defined as a sequence of three or more consecutive spontaneous abortion before 20 weeks. Some, however, consider two or more as a standard. It may be primary or secondary (having previous viable birth). A woman procuring three consecutive induced abortions is not a habitual abortion.
There are several synonyms for recurrent abortion/habitual abortion, all conveying the same meaning:
- Recurrent miscarriage – This is the most common synonym used in everyday language.
- Recurrent pregnancy loss (RPL) – This is a more technical term used in the medical field.
- Habitual miscarriages – While grammatically correct, "miscarriage" is often preferred over "abortion" in non-medical contexts due to its less clinical connotation.
All of these terms refer to experiencing three or more consecutive pregnancy losses.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prognosis
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Recurrent abortion
It is also known as recurrent pregnancy loss or habitual abortion, is a distressing condition defined as the occurrence of three or more consecutive spontaneous abortions before 20 weeks of gestation. It affects approximately 1% of couples trying to conceive.
Key Points:
- Emotional Impact: Recurrent abortion can have a profound emotional and psychological impact on couples, leading to anxiety, depression, and feelings of loss.
- Causes: The causes of recurrent abortion are diverse and can include genetic abnormalities, uterine anomalies, immunologic factors, endocrine disorders, infections, and thrombophilias.
- Diagnosis: A thorough evaluation is essential to identify any underlying causes. This may include a detailed medical history, physical examination, blood tests, imaging studies, and genetic testing.
- Treatment: The appropriate treatment approach depends on the identified cause. Options may include medical management, surgical interventions, or assisted reproductive technologies.
- Prognosis: Although recurrent abortion can be challenging, many couples with this condition go on to have successful pregnancies. The prognosis depends on the underlying cause and the available treatment options.
Remember: If you or someone you know is experiencing recurrent abortion, seeking support from healthcare professionals and mental health specialists is crucial. With appropriate care and guidance, many couples can overcome this difficult experience and achieve their dream of parenthood.[2]
Epidemiology
Epidemiology
The prevalence of recurrent spontaneous miscarriage (RSM) in India is reported to be around 7.46%. This finding comes from a study published in 2015 titled "An Epidemiology Study to Determine the Prevalence and Risk Factors Associated with Recurrent Spontaneous Miscarriage in India."
It’s important to note that prevalence rates can vary depending on the study population and the specific definition of recurrent miscarriage used. However, this figure provides a general understanding of the frequency of RSM in the Indian context.[1]
Causes
Causes
It can be multifactorial and complex. Below are some of the main categories of causes, supported by a reputable medical source:
Genetic Factors
Chromosomal Abnormalities: The most common cause, particularly in the first trimester, is aneuploidy (abnormal number of chromosomes) in the embryo.
Parental Chromosomal Abnormalities: Balanced translocations in one or both parents can also lead to recurrent miscarriages.
Anatomical Factors
Uterine Anomalies: Congenital or acquired structural abnormalities of the uterus, such as a septate uterus, bicornuate uterus, or fibroids, can affect implantation or fetal growth.
Cervical Incompetence: A weakened cervix may dilate prematurely, leading to second-trimester miscarriages.
Immunologic Factors
Antiphospholipid Syndrome (APS): An autoimmune disorder that can lead to blood clots in the placenta, disrupting its function.
Alloimmune Factors: In some cases, the mother’s immune system may react against the fetus, leading to rejection.
Endocrine Factors
Hormonal Imbalances: Conditions like uncontrolled diabetes, thyroid disease, or polycystic ovary syndrome (PCOS) can affect hormonal balance and impact pregnancy.
Luteal Phase Defect: Insufficient progesterone production after ovulation may hinder implantation and early pregnancy development.
Infections
Certain Infections: Some infections, particularly those affecting the reproductive system, can increase the risk of miscarriage.
Thrombophilias
Inherited or Acquired Thrombophilias: These conditions increase the risk of blood clots, potentially affecting placental blood flow and leading to miscarriage.
Environmental and Lifestyle Factors
- Smoking, Alcohol, Drug Use: These can adversely affect fertility and increase the risk of miscarriage.
- Exposure to Environmental Toxins: Certain chemicals and toxins may impact reproductive health and contribute to pregnancy loss.
Remember:
- It’s essential to consult with a healthcare professional for a thorough evaluation and personalized management plan if you are experiencing recurrent miscarriages.
- In some cases, the cause of recurrent abortion remains unexplained even after extensive investigation.[2]
Types
Types
Primary Recurrent Miscarriage
This type of recurrent abortion refers to cases where a woman has experienced multiple miscarriages and has never had a successful live birth.
Secondary Recurrent Miscarriage
This type refers to cases where a woman experiences multiple miscarriages after having had at least one successful live birth.
Please let me know if you have any other questions![2]
Risk Factors
Risk factors
Several factors can increase the risk of recurrent abortions. Here are some key risk factors with references from a reputable medical source.
1. Advanced Maternal Age
Women over the age of 35 have a higher risk of recurrent miscarriages compared to younger women.
2. Uterine Anomalies
Structural abnormalities of the uterus, such as a septate uterus or fibroids, can increase the risk of recurrent pregnancy loss.
3. Parental Chromosomal Abnormalities
Genetic abnormalities in either parent can increase the risk of miscarriage.
4. Antiphospholipid Syndrome
This autoimmune disorder can increase the risk of blood clots, which can interfere with placental function and lead to miscarriage.
5. Endocrine Disorders
Conditions like uncontrolled diabetes or thyroid disease can affect hormonal balance and increase the risk of miscarriage.
6. Lifestyle Factors
Smoking, excessive alcohol consumption, and drug use can increase the risk of recurrent miscarriage.
Please note: It is crucial to consult a healthcare professional for personalized advice and management if you are concerned about recurrent abortions.[2]
Pathogenesis
Pathogenesis
It is complex and multifactorial, often involving a combination of factors that contribute to pregnancy loss. Here are some of the key mechanisms involved, supported by a reputable medical reference.
Genetic Abnormalities
Aneuploidy: The most common cause of early miscarriages, particularly in the first trimester, is aneuploidy – an abnormal number of chromosomes in the embryo.
Uterine Anomalies
Structural Abnormalities: Uterine anomalies like septate uterus or fibroids can impact implantation or the growth of the fetus, leading to miscarriage.
Immunologic Factors
Antiphospholipid Syndrome: This autoimmune disorder can lead to blood clots in the placenta, affecting its function and causing miscarriage.
Alloimmune Factors: In some cases, the mother’s immune system may react against the fetus, leading to pregnancy loss.
Endocrine Factors
Hormonal Imbalances: Conditions like uncontrolled diabetes or thyroid disease can disrupt the hormonal environment necessary for a healthy pregnancy.
Luteal Phase Defect: Inadequate progesterone production after ovulation can impair implantation and early pregnancy development.
Infections
Certain Infections: Some infections, like Listeria or Toxoplasma, can cross the placenta and harm the fetus, increasing the risk of miscarriage.
Note:
It’s crucial to remember that the cause of recurrent miscarriage often remains unexplained even after extensive investigation. Understanding the potential mechanisms involved helps guide the diagnostic process and inform potential treatment options. If you have concerns about recurrent pregnancy loss, consulting a healthcare professional is essential.[2]
Pathophysiology
Pathophysiology
It is multifaceted and often involves an interplay of various factors. Here are some of the main mechanisms that can lead to recurrent pregnancy loss, supported by a reputable medical reference.
Genetic Factors
Chromosomal Abnormalities: The leading cause of early pregnancy loss, particularly in the first trimester, is aneuploidy. It occurs when an embryo has an abnormal number of chromosomes, often leading to developmental issues and miscarriage.
Parental Chromosomal Abnormalities: Balanced translocations or other structural rearrangements in parental chromosomes can also increase the risk of recurrent miscarriages.
Anatomical Factors
Uterine Anomalies: Structural abnormalities in the uterus, such as a septate uterus, bicornuate uterus, or the presence of fibroids, can impair implantation or disrupt the growth of the developing fetus.
Cervical Incompetence: A weakened or prematurely dilated cervix may lead to second-trimester miscarriages due to the inability to retain the pregnancy.
Immunologic Factors
Antiphospholipid Syndrome (APS): This autoimmune disorder promotes the formation of blood clots, potentially affecting placental blood flow and leading to fetal demise.
Alloimmune Dysfunction: In some cases, the maternal immune system might inappropriately recognize the fetus as foreign, triggering an immune response that can result in pregnancy loss.
Endocrine Factors
Hormonal Imbalances: Conditions like uncontrolled diabetes, thyroid dysfunction, or polycystic ovary syndrome (PCOS) can disrupt the delicate hormonal balance required for a successful pregnancy.
Luteal Phase Defect: Inadequate progesterone production after ovulation can impair endometrial receptivity and hinder implantation, leading to early pregnancy loss.
Infections
Certain Infections: Infections like bacterial vaginosis, certain sexually transmitted infections, and some viral infections can increase the risk of miscarriage, potentially by triggering inflammation or directly affecting the fetus.
Thrombophilias
Inherited or Acquired Thrombophilias: These conditions predispose individuals to blood clot formation. In the context of pregnancy, this can impact placental circulation and contribute to miscarriage.
Please Note:
- The exact cause of recurrent miscarriages might remain unidentified even after a thorough evaluation.
- If you are experiencing recurrent pregnancy loss, it’s important to consult with a healthcare professional for personalized guidance and management.[2]
Clinical Features
Clinical Features
Recurrent abortion, although primarily defined by the occurrence of multiple consecutive miscarriages, often presents with additional clinical features that can aid in diagnosis and understanding the underlying causes. Here are some of the clinical features commonly associated with recurrent abortion, supported by a reputable medical reference.
History of Multiple Miscarriages
The primary characteristic of recurrent abortion is a history of three or more consecutive spontaneous pregnancy losses before 20 weeks of gestation.
Timing of Miscarriages
The timing of miscarriages can offer clues to the underlying cause.
- Early miscarriages (before 12 weeks) are often associated with chromosomal abnormalities or implantation issues.
- Second-trimester miscarriages (12-20 weeks) may be linked to uterine anomalies, cervical incompetence, or maternal medical conditions.
Symptoms of Miscarriage
Women experiencing recurrent miscarriages may present with typical symptoms of miscarriage, such as:
- Vaginal bleeding
- Cramping or abdominal pain
- Passage of tissue or clots
Associated Medical Conditions
Certain medical conditions may coexist with recurrent abortion, including:
- Antiphospholipid syndrome
- Thyroid disorders
- Diabetes
- Uterine anomalies
- Thrombophilias
Psychological Impact
- Recurrent miscarriages can take a significant emotional toll, leading to anxiety, depression, and grief.
Please Note:
- The specific clinical features can vary depending on the underlying cause of the recurrent miscarriages.
- If you have concerns about recurrent pregnancy loss, seeking evaluation and guidance from a healthcare professional is essential.[2]
Sign & Symptoms
Sign & Symptoms of Recurrent abortion
Recurrent abortion often manifests through signs and symptoms typical of a single miscarriage. However, experiencing these repeatedly can be a significant indicator of recurrent pregnancy loss. Here are the common signs and symptoms associated with recurrent abortion, supported by a reputable medical reference.
1. Vaginal Bleeding
- Bleeding can range from light spotting to heavy bleeding with clots.
- It may occur at any stage of pregnancy but is often seen in the first trimester.
2. Cramping or Abdominal Pain
- Pain can range from mild discomfort to severe cramping, similar to menstrual cramps.
- It may be localized to the lower abdomen or radiate to the back.
3. Passage of Tissue or Clots
- In some cases, women may notice the passage of tissue or blood clots from the vagina.
Additional Signs and Symptoms
- Loss of pregnancy symptoms: This may include decreased nausea, breast tenderness, or fatigue.
- Backache: Lower back pain may be present.
- Brownish discharge: This may be a sign of old blood from an impending or ongoing miscarriage.
Note:
- It’s important to remember that not all women experiencing recurrent abortion will exhibit these symptoms.
- If you have concerns about recurrent pregnancy loss or experience any of these symptoms, seeking immediate medical attention is crucial.[2]
Clinical Examination
Clinical Examination
A thorough clinical examination is essential in the evaluation of recurrent abortion. This examination aims to identify any potential underlying causes and guide further investigations. Here are some key aspects of the clinical examination, supported by a reputable medical reference.
General Physical Examination:
- Assessment of overall health and well-being
- Vital signs measurement (blood pressure, heart rate, respiratory rate, temperature)
- Evaluation for signs of systemic illness or endocrine disorders (e.g., thyroid enlargement, hirsutism)
Pelvic Examination:
- Careful inspection of the external genitalia for any abnormalities
- Speculum examination to assess the cervix for any signs of incompetence or infection
- Bimanual examination to evaluate the size, shape, and position of the uterus and ovaries, and to identify any masses or tenderness
Additional Examinations (if indicated):
- Ultrasound: To visualize the uterus and ovaries, identify any structural abnormalities, and assess for any retained products of conception
- Hysteroscopy: To directly visualize the uterine cavity and identify any abnormalities like polyps, fibroids, or adhesions
- Laparoscopy: To visualize the pelvic organs and identify any endometriosis, adhesions, or other abnormalities
Note:
- The extent of the clinical examination may vary depending on the individual’s medical history and the suspected underlying causes of recurrent abortion.
- It is crucial to consult with a healthcare professional for a comprehensive evaluation and personalized management plan if you are experiencing recurrent pregnancy loss.[2]
Diagnosis
Diagnosis of Recurrent abortion
Diagnosing recurrent abortion involves a comprehensive evaluation to identify any underlying causes that may be contributing to the pregnancy losses. This typically includes a combination of detailed history taking, physical examinations, and various laboratory and imaging tests.
1. Detailed History and Physical Examination
A thorough medical and reproductive history is crucial, including details about previous pregnancies, miscarriages, and any associated symptoms.
A physical examination will be performed to assess overall health and identify any potential contributing factors, such as uterine anomalies or signs of endocrine disorders.
2. Laboratory Investigations
Blood tests may be ordered to assess various factors, including:
- Chromosomal analysis (karyotyping) of both partners to identify any genetic abnormalities
- Thyroid function tests to rule out thyroid disorders
- Blood glucose levels to assess for diabetes
- Antiphospholipid antibodies to detect antiphospholipid syndrome
- Thrombophilia screening to identify blood clotting disorders
3. Imaging Studies
Ultrasound: To assess the uterus and ovaries for any structural abnormalities, such as fibroids or polyps
Hysterosalpingogram (HSG): To evaluate the shape of the uterine cavity and the patency of the fallopian tubes
Sonohysterogram (SHG): To provide a more detailed view of the uterine cavity
Magnetic Resonance Imaging (MRI): May be used in specific cases to further evaluate uterine or pelvic anatomy
4. Additional Tests
Depending on the clinical suspicion, other tests may be recommended, such as:
- Endometrial biopsy to assess the lining of the uterus
- Immunologic testing to evaluate for alloimmune factors
- Infectious disease screening to rule out infections
Note:
- The diagnostic process should be tailored to the individual’s specific situation and may involve collaboration between various specialists, including obstetricians, reproductive endocrinologists, and geneticists.
- It’s essential to remember that in some cases, despite extensive testing, a definitive cause for recurrent abortion may not be identified.[2]
Differential Diagnosis
Differential Diagnosis
When a woman experiences recurrent pregnancy loss, it is crucial to conduct a thorough differential diagnosis to identify the underlying cause. Several conditions can mimic or contribute to recurrent abortion, necessitating careful evaluation. Here are some key differential diagnoses, supported by a reputable medical reference.
Chromosomal Abnormalities
Aneuploidy (abnormal number of chromosomes) in the embryo is the most common cause of early miscarriage.
Parental chromosomal abnormalities, like balanced translocations, can also contribute to recurrent loss.
Uterine Anomalies
Structural abnormalities of the uterus, like septate uterus, bicornuate uterus, or fibroids, can affect implantation or fetal growth.
Cervical incompetence, where the cervix dilates prematurely, can lead to second-trimester losses.
Immunologic Factors
Antiphospholipid syndrome (APS) can increase the risk of blood clots, affecting placental blood flow.
Alloimmune factors, where the maternal immune system reacts against the fetus, can also contribute.
Endocrine Disorders
Uncontrolled diabetes, thyroid disorders, and polycystic ovary syndrome (PCOS) can disrupt hormonal balance, impacting pregnancy.
Luteal phase defect, characterized by insufficient progesterone production, can affect implantation.
Infections
Certain infections, particularly those affecting the reproductive system, like bacterial vaginosis or some sexually transmitted infections, can increase the risk of miscarriage.
Thrombophilias
Inherited or acquired thrombophilias increase the risk of blood clot formation, which can affect placental blood flow and lead to pregnancy loss.
Note:
- It’s important to consider other potential causes like environmental factors, lifestyle factors (smoking, alcohol, drug use), and in some cases, unexplained recurrent pregnancy loss.
- A thorough evaluation by a healthcare professional is essential to differentiate between these possibilities and determine the most appropriate management approach.[2]
Complications
Complications
While the primary concern in recurrent abortion is the repeated pregnancy losses, there are additional potential complications that can impact a woman’s physical and emotional well-being. It is important to be aware of these potential complications, supported by a reputable medical reference.
Psychological Impact:
Recurrent miscarriages can have a profound emotional and psychological impact, leading to:
- Anxiety and depression
- Grief and loss
- Relationship strain
- Difficulty conceiving in the future due to fear of further loss
Physical Complications:
Although rare, some physical complications can arise from recurrent miscarriages or their underlying causes, such as:
- Asherman’s syndrome (scarring within the uterus)
- Cervical incompetence (weakening of the cervix)
- Complications related to surgical interventions for uterine anomalies
Complications Related to Underlying Causes:
- Certain underlying causes of recurrent abortion can have their own associated complications, including:
- Antiphospholipid syndrome: Increased risk of blood clots, stroke, and other thromboembolic events
- Uncontrolled diabetes: Increased risk of complications affecting various organ systems
- Thyroid disorders: Impact on overall health and well-being
Note:
- The specific complications can vary depending on the individual’s situation and the identified cause of recurrent abortion.
- Seeking appropriate medical and psychological support is crucial to address both the physical and emotional aspects of recurrent pregnancy loss.
- Early diagnosis and management of underlying conditions can help minimize the risk of complications.
Remember:
- If you’re experiencing recurrent miscarriages, don’t hesitate to seek help. With proper care and support, many women with a history of recurrent abortion can go on to have successful pregnancies.[2]
Investigations
Investigations
It involves a comprehensive approach to identify potential underlying causes. This usually involves a combination of medical history review, physical examination, and various laboratory and imaging tests. Here are some key areas of investigation, supported by a reputable medical reference.
Medical and Reproductive History
A detailed history will be taken, including information about:
- Previous pregnancies, miscarriages, and their timing
- Any associated symptoms during pregnancy or miscarriage
- Past medical and surgical history
- Family history of recurrent miscarriages or genetic disorders
Physical Examination
A thorough physical examination will be conducted to assess overall health and identify potential contributing factors, including:
- General physical examination to evaluate for signs of systemic illness or endocrine disorders
- Pelvic examination to assess the uterus and ovaries for any abnormalities
Laboratory Tests
Several laboratory tests may be ordered to evaluate various potential causes:
- Chromosomal analysis (karyotyping) of both partners
- Thyroid function tests
- Blood glucose levels
- Antiphospholipid antibodies
- Thrombophilia screening
- Progesterone levels
- Infectious disease screening
Imaging Studies
Imaging studies can help visualize the reproductive organs and identify any structural abnormalities:
- Ultrasound (transvaginal or abdominal)
- Hysterosalpingogram (HSG)
- Sonohysterogram (SHG)
- Magnetic Resonance Imaging (MRI)
Additional Investigations
Depending on clinical suspicion, other investigations may be considered:
- Endometrial biopsy
- Immunologic testing
- Consultation with specialists (e.g., geneticist, reproductive immunologist)
Remember:
- The investigation process should be tailored to the individual’s specific needs and may involve multiple healthcare professionals.
- If you’re experiencing recurrent miscarriages, don’t hesitate to seek help. A comprehensive investigation can increase the chances of identifying the underlying cause and finding appropriate solutions to increase the likelihood of a successful pregnancy.[2]
Treatment
Treatment
It is highly individualized and depends on the underlying cause identified through thorough investigation. Here are some potential treatment approaches, supported by a reputable medical reference.
Treatment of Underlying Causes
Genetic Abnormalities: If a parental chromosomal abnormality is identified, genetic counseling and options such as preimplantation genetic testing (PGT) may be discussed.
Uterine Anomalies: Surgical correction of uterine abnormalities like septate uterus or removal of fibroids may improve pregnancy outcomes. Cervical cerclage may be considered for cervical incompetence.
Immunologic Factors: Antiphospholipid syndrome may be treated with low-dose aspirin and heparin. Other immunologic factors may necessitate further investigation and potential immunotherapy.
Endocrine Disorders: Management of conditions like diabetes or thyroid disorders is crucial for improving pregnancy outcomes. Progesterone supplementation might be considered in cases of luteal phase defect.
Infections: Appropriate treatment of any identified infections is necessary.
Thrombophilias: Depending on the specific thrombophilia, anticoagulation therapy may be recommended.
Supportive Measures
Psychological Support: Counseling and support groups can help couples cope with the emotional challenges of recurrent abortion.
Lifestyle Modifications: Adopting healthy lifestyle habits, such as maintaining a healthy weight, avoiding smoking and alcohol, and managing stress, can improve overall health and potentially enhance fertility.
- Empirical Treatments
In cases where no specific cause is identified, empirical treatments might be considered:
- Progesterone supplementation in early pregnancy
- Low-dose aspirin
- Baby aspirin
Assisted Reproductive Technologies (ART)
- In certain situations, ART, such as in vitro fertilization (IVF), may be considered to increase the chances of a successful pregnancy.
Note:
- It’s essential to consult with a healthcare professional for a personalized treatment plan tailored to your specific needs and underlying causes.
- With proper evaluation and management, many couples with a history of recurrent abortion can go on to have healthy pregnancies.[2]
Prognosis
Prognosis of Recurrent abortion
It is generally favorable, even without any specific treatment. The majority of couples with a history of recurrent miscarriages will eventually achieve a successful pregnancy and deliver a healthy baby.
Key Points on Prognosis:
- Spontaneous Success: Even without intervention, approximately 65-75% of couples with unexplained recurrent abortion will have a successful subsequent pregnancy.
- Impact of Identified Causes: The prognosis can be significantly improved if an underlying cause is identified and treated effectively.
- Individual Factors: The prognosis may vary depending on factors like the woman’s age, the number of previous miscarriages, and the presence of any underlying medical conditions.
- Psychological Support: Addressing the emotional impact of recurrent miscarriage is essential for overall well-being and can positively influence future pregnancy outcomes.
Remember:
- While experiencing recurrent abortion can be emotionally challenging, it’s crucial to remain hopeful and seek appropriate medical care.
- With advances in medical understanding and treatment options, the outlook for couples facing recurrent pregnancy loss is increasingly optimistic.[2]
Prevention
Prevention
It can be a challenging and emotionally distressing experience, there are steps that can be taken to potentially reduce the risk of further pregnancy loss. These preventive measures focus on addressing modifiable risk factors and optimizing overall health. Here are some key strategies, supported by a reputable medical reference.
Addressing Underlying Medical Conditions:
If an underlying cause of recurrent abortion is identified, treating it appropriately can significantly improve the chances of a successful pregnancy.
This may involve managing conditions like diabetes, thyroid disorders, or antiphospholipid syndrome.
Surgical correction of uterine anomalies or cervical cerclage for cervical incompetence might also be necessary.
Lifestyle Modifications:
Adopting healthy lifestyle habits can positively impact overall health and reproductive function.
These modifications may include:
- Maintaining a healthy weight
- Avoiding smoking and excessive alcohol consumption
- Eating a balanced diet rich in fruits, vegetables, and whole grains
- Engaging in regular exercise
- Managing stress through relaxation techniques.
Preconception Counseling and Care:
Seeking preconception counseling can help identify any potential risks and optimize health before attempting pregnancy.
This may include:
- Reviewing medical and reproductive history
- Addressing any existing medical conditions
- Discussing genetic testing if relevant
- Optimizing medications and supplements
- Providing guidance on healthy lifestyle practices
Prenatal Care:
- Early and regular prenatal care is essential for monitoring the pregnancy and identifying any potential complications.
- This includes regular checkups, ultrasounds, and appropriate screenings.
Remember:
- While these measures can help reduce the risk of recurrent abortion, they do not guarantee a successful pregnancy.
- It’s important to maintain open communication with your healthcare provider throughout the process and address any concerns or questions.
- With proper care and support, many couples with a history of recurrent miscarriages can go on to have healthy pregnancies and welcome their babies into the world.[2]
Homeopathic Treatment
Homeopathic Treatment of Recurrent abortion:
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Recurrent abortion:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Medicines:
Arnica
- Traumatism of grief. Hemorrhages. Additionally, Tendency to hemorrhage.
- Furthermore, Tendency to tissue degeneration, septic conditions, bruised parts after labor. In detail, Violent after pains.
- Uterine hemorrhage – feeling as if foetus were lying cross-wise.
- Worse – especially least touch, motion, rest, damp, cold. On the other hand, Better – lying down or with head low.
Belladonna
- For violence of attack also suddenness of onset.
- Female – sensitive forcing downwards as if all the viscera would protrude at genitals.
- Dryness also heat of vagina. In detail, Dragging around loins, Pain in sacrum.
- Hemorrhage hot, Cutting pain from hip to hip, Labor pains come and go suddenly.
- Besides this, Badly smelling hemorrhages, hot gushes of blood.
- Worse – touch, noise, specifically lying down. Whereas, Better – semi-erect.
Chamomilla
- Chief guiding symptoms mental/emotional group.
- Moreover, Female – uterine hemorrhages.
- Profuse discharge of clotted, dark blood, with labour-like pains.
- Labour pains spasmodic; additionally press upward.
- Patient intolerant of pain. Worse – heat, anger, especially open air, night.
Sabina
- Sabina has a special action on the uterus.
- Pain from sacrum to the pubis. Additionally; Hemorrhages, where blood is fluid and clots together.
- Recurrent abortion, especially at third month. Violent pulsations; wants windows open.
- Female – Uterine pains extend into thighs. In detail, Threatened miscarriage. Retained placenta; intense after pains.
- Besides this, Menorrhagia in women who aborted easily. Inflammation of ovaries and uterus after abortion. Hemorrhage partly clotted.
- Worse – from least motion, atony of uterus, heat, warm air. On the other hand; Better – cool, fresh air.
Platina
- Generally, It is pre-eminently a woman’s remedy. intense spasms.
- Pains increase and decease gradually. Additionally; Tremulousness.
- Abdomen – pain in umbilical region; extending through to back.
- Pressing also bearing down in abdomen, extending to pelvis.
- Female – parts hyper-sensitive. Tingling internally also externally. Ovaries sensitive also burn.
- Spasms and painful bearing down. Ovaritis with sterility. Abnormal sexual melancholia.
- Worse – specifically; sitting and standing; evening. Whereas; Better – walking.
Plumbum
- Tendency to abortion from non-development of uterus.
- Muscular fibers of uterus do not develop proportionally as the foetus increases in size in uterus also Recurrent abortion. [3]
Diet & Regimen
Diet & Regimen
While there is no single "recurrent abortion diet," adopting a healthy lifestyle and balanced diet before and during pregnancy can contribute to overall well-being and potentially improve pregnancy outcomes. Here are some recommended dietary and lifestyle practices, supported by a reputable medical reference.
Dietary Recommendations:
Focus on Nutrient-Rich Foods: Prioritize whole foods, including:
- Fruits and vegetables: Aim for a variety of colorful options to ensure adequate intake of vitamins, minerals, and antioxidants.
- Whole grains: Choose whole-wheat bread, brown rice, quinoa, and oats for sustained energy and fiber.
- Lean proteins: Opt for fish, poultry, beans, lentils, and nuts for essential amino acids.
- Healthy fats: Include sources like avocados, nuts, seeds, and olive oil for essential fatty acids.
- Dairy or dairy alternatives: Ensure adequate calcium intake for bone health.
Prenatal Vitamins: Take a high-quality prenatal vitamin as recommended by your healthcare provider to supplement any potential nutrient deficiencies.
Hydration: Stay well-hydrated by drinking plenty of water throughout the day.
Limit Processed Foods: Minimize intake of processed foods, sugary drinks, and excessive caffeine.
Food Safety: Practice safe food handling and avoid foods that may pose a risk of foodborne illness, such as raw or undercooked meat, fish, and eggs.
Lifestyle Recommendations:
- Maintain a Healthy Weight: Strive for a healthy body mass index (BMI) before conception and during pregnancy.
- Regular Exercise: Engage in moderate-intensity exercise as approved by your healthcare provider.
- Stress Management: Practice relaxation techniques like yoga, meditation, or deep breathing to manage stress.
- Avoid Smoking, Alcohol, and Drugs: These substances can negatively impact fertility and increase the risk of miscarriage.
Note:
- It is essential to consult with your healthcare provider or a registered dietitian for personalized dietary and lifestyle recommendations, particularly if you have any underlying medical conditions or specific nutritional needs.
- Remember, a healthy lifestyle is just one aspect of managing recurrent abortion. Addressing any identified underlying causes and seeking comprehensive medical care are equally important.[2]
Do’s and Don'ts
Do’s & Don’ts
Recurrent Abortion Do’s & Don’ts
It can be emotionally and physically challenging. While seeking professional medical advice is crucial, here are some general do’s and don’ts that may help support you during this difficult time.
Do’s:
- Seek Professional Help: Consult with a healthcare provider specializing in recurrent pregnancy loss for a thorough evaluation and personalized treatment plan.
- Prioritize Emotional Well-being: Allow yourself to grieve and process your emotions. Consider seeking counseling or joining a support group to connect with others who understand your experience.
- Maintain a Healthy Lifestyle: Eat a balanced diet, exercise regularly, get enough sleep, and manage stress to promote overall health and well-being.
- Take Prenatal Vitamins: Ensure adequate intake of essential nutrients like folic acid by taking prenatal vitamins as recommended by your healthcare provider.
- Stay Informed: Educate yourself about recurrent abortion, its causes, and available treatment options.
- Follow Medical Advice: Adhere to any treatment plans or recommendations provided by your healthcare provider.
- Be Patient: Healing takes time. Be kind to yourself and allow yourself the time and space you need to recover emotionally and physically.
Don’ts:
- Blame Yourself: Recurrent abortion is not your fault. It’s often a result of complex medical factors beyond your control.
- Isolate Yourself: Reach out to loved ones and support networks. Sharing your feelings can be cathartic and help you navigate this challenging experience.
- Neglect Your Health: Prioritize your physical and emotional well-being. Take care of yourself by eating nutritious meals, exercising regularly, and getting enough rest.
- Give Up Hope: Many women with a history of recurrent abortion go on to have successful pregnancies. With appropriate care and support, you may be able to achieve your dream of parenthood.
- Compare Your Journey: Every woman’s experience with recurrent abortion is unique. Avoid comparing your journey to others, as this can lead to unnecessary stress and anxiety.
Remember:
- The most important step is to seek guidance from a qualified healthcare professional. They can assess your individual situation, provide appropriate testing and treatment, and offer emotional support.
- Don’t lose hope. With advancements in medical knowledge and treatment options, many women with recurrent abortion are able to experience successful pregnancies.
Please let me know if you have any other questions.
Terminology
Terminology
Understanding the specific terms used in the context of recurrent abortion is essential for clear communication and comprehension of medical information. Here are some key terminologies and their definitions:
Recurrent Abortion/Recurrent Pregnancy Loss (RPL):
The loss of three or more consecutive pregnancies before 20 weeks of gestation.
Miscarriage:
The spontaneous loss of a pregnancy before 20 weeks of gestation.
Spontaneous Abortion:
Another term for miscarriage, indicating that the pregnancy loss occurred naturally without medical or surgical intervention.
Primary Recurrent Abortion:
Recurrent miscarriages in a woman who has never had a live birth.
Secondary Recurrent Abortion:
Recurrent miscarriages in a woman who has had at least one live birth.
Clinical Pregnancy:
A pregnancy that has been confirmed by ultrasound or histopathological examination.
Biochemical Pregnancy:
A very early pregnancy that is detected by a positive pregnancy test but is lost before it can be visualized on ultrasound.
Aneuploidy:
An abnormal number of chromosomes in the embryo, a common cause of early miscarriage.
Uterine Anomalies:
Structural abnormalities of the uterus that can contribute to recurrent miscarriages.
Antiphospholipid Syndrome (APS):
An autoimmune disorder associated with an increased risk of blood clots, which can affect pregnancy.
Thrombophilia:
A condition that increases the risk of blood clot formation.
Cervical Incompetence:
A condition where the cervix weakens and dilates prematurely, potentially leading to miscarriage.
Luteal Phase Defect:
Inadequate progesterone production after ovulation, which can impair implantation and early pregnancy development.
How these terms are used in the context of recurrent abortion:
Describing the condition:
The terms "recurrent abortion" and "recurrent pregnancy loss" are used interchangeably to refer to the clinical scenario of multiple consecutive pregnancy losses.
Classifying types of recurrent abortion:
The terms "primary" and "secondary" recurrent abortion distinguish between cases where a woman has never had a live birth versus those where she has had at least one.
Identifying potential causes:
Terminologies like "aneuploidy," "uterine anomalies," "APS," and "thrombophilia" are used to describe specific factors that can contribute to recurrent miscarriages.
Discussing diagnostic procedures:
Terms like "clinical pregnancy," "biochemical pregnancy," and various imaging techniques (ultrasound, HSG, MRI) are used when explaining the diagnostic process.
Explaining treatment options:
Medical terms may be used to describe medications or procedures aimed at addressing the underlying cause of recurrent abortion, such as "progesterone supplementation," "cervical cerclage," or "anticoagulation therapy."
Understanding these key terms empowers individuals to better comprehend medical information and actively participate in discussions about their reproductive health.
Here are some terminologies commonly used in homeopathic articles discussing recurrent abortion and their meanings:
Recurrent Abortion/Recurrent Miscarriage:
The loss of three or more consecutive pregnancies before 20 weeks of gestation.
Habitual Abortion:
An older term, sometimes still used, for recurrent abortion.
Miasm:
A fundamental concept in homeopathy referring to a predisposing disease tendency or inherited susceptibility. Psoric, sycotic, and syphilitic are the three primary miasms.
Constitutional Remedy:
A homeopathic medicine chosen based on the totality of a person’s physical, mental, and emotional symptoms, aiming to address their underlying susceptibility and strengthen their overall health.
Totality of Symptoms:
The complete picture of a person’s physical, mental, and emotional symptoms, which forms the basis for homeopathic prescription.
Repertory:
A reference book listing symptoms and the homeopathic remedies associated with them, used to aid in remedy selection.
Materia Medica:
A reference book detailing the symptoms and characteristics of homeopathic remedies.
Potency:
The strength or dilution of a homeopathic remedy.
Aggravation:
A temporary worsening of symptoms after taking a homeopathic remedy, often considered a positive sign indicating that the remedy is working.
Proving:
A systematic process of observing the effects of a homeopathic remedy on healthy individuals to identify its characteristic symptoms.
How these terms are used in the context of homeopathic articles on recurrent abortion:
Understanding the cause:
Homeopaths may consider recurrent abortion as a manifestation of an underlying miasmatic disturbance, and seek to identify the predominant miasm in order to select a suitable constitutional remedy.
Individualized treatment:
The focus is on treating the whole person, considering their unique physical, mental, and emotional characteristics, rather than just the recurrent miscarriages.
Remedy selection:
The totality of the woman’s symptoms, including her past medical history, family history, and current complaints, is considered when selecting a homeopathic remedy.
Monitoring progress:
Homeopaths observe changes in the woman’s overall health and well-being, as well as any changes in the pattern of miscarriages, to assess the effectiveness of the remedy.
Emphasis on prevention:
Homeopathy aims not only to treat existing recurrent miscarriages but also to prevent future ones by strengthening the woman’s overall health and addressing any underlying predispositions.
It is important to note that homeopathy remains a controversial form of treatment, and its effectiveness for recurrent abortion has not been scientifically proven. If you are considering homeopathic treatment, it is crucial to consult with a qualified homeopathic practitioner and inform your primary healthcare provider about any complementary or alternative therapies you are using.
References
References
- "An Epidemiology Study to Determine the Prevalence and Risk Factors Associated with Recurrent Spontaneous Miscarriage in India."(2015).
- Book: Williams Obstetrics
Edition: 26th Edition
Writer: F. Gary Cunningham, Kenneth J. Leveno, Steven L. Bloom, Jodi S. Dashe, Barbara L. Hoffman, Brian M. Casey, Catherine Y. Spong, (2020)
Publication: McGraw Hill Medical - Homoeopathic Body-System Prescribing – A Practical Workbook of Sector Remedies.
Also Search As
Also Search As
People can search for homeopathic articles on recurrent abortion using various online resources and strategies. Here are some effective ways:
Search Engines:
- Use specific keywords: Start with basic search terms like "homeopathy recurrent abortion" or "homeopathic treatment for recurrent miscarriage."
- Include additional keywords: Refine your search by adding terms like "causes," "remedies," "case studies," or "success stories."
- Use quotation marks: Enclose phrases in quotation marks to search for exact matches, like "homeopathic approach to recurrent pregnancy loss."
Homeopathic Websites and Resources:
- Explore homeopathic organizations: Visit websites of reputable homeopathic organizations, such as the National Center for Homeopathy or the American Institute of Homeopathy, as they may have articles or resources on recurrent abortion.
- Search homeopathic journals and publications: Look for online databases or archives of homeopathic journals, where you can often find research articles or case studies related to recurrent abortion.
- Check homeopathic blogs and forums: Many homeopathic practitioners and enthusiasts maintain blogs or participate in online forums where they may discuss recurrent abortion and related topics.
Other Tips:
- Consult with a homeopathic practitioner: Ask your homeopath for recommendations on reliable sources of information.
- Utilize social media: Follow homeopathic groups or pages on social media platforms to stay updated on the latest research and discussions.
- Be mindful of source credibility: Always evaluate the credibility of the information you find. Look for articles written by qualified homeopathic practitioners or published in reputable journals.
Specific Search Examples:
- "Homeopathic remedies for recurrent miscarriage"
- "Case studies of successful homeopathic treatment for recurrent abortion"
- "Homeopathic approach to unexplained recurrent pregnancy loss"
- "Miasmatic treatment of recurrent abortion"
- "Constitutional remedies for recurrent miscarriage"
There are numerous ways to search for information on recurrent abortion, using both general and specialized resources:
General Search Engines
- Use Broad Search Terms: Start with basic search terms like:
- "recurrent abortion"
- "recurrent miscarriage"
- "habitual abortion"
- Refine with Specific Questions: Add details to narrow results, such as:
- "causes of recurrent abortion"
- "treatment for recurrent miscarriage"
- "support groups for recurrent pregnancy loss"
- Include Location: Add your location to find local resources and statistics:
- "recurrent abortion India"
- "recurrent miscarriage clinics near me"
Medical Websites & Databases
- Reputable Health Organizations:
- Mayo Clinic, American Pregnancy Association, National Institutes of Health, etc.
- Often provide reliable, evidence-based information.
- Medical Journals:
- PubMed, Google Scholar
- Access to scientific studies and research articles.
- Patient Support Groups:
- Search for online or local support groups specific to recurrent pregnancy loss.
Other Search Strategies
- Social Media: Follow relevant hashtags or groups on platforms like Facebook or Instagram.
- Books & eBooks: Search for medical textbooks or patient-friendly books on the topic.
- Consult a Healthcare Provider: They can provide personalized guidance and recommend resources.
Key Points to Remember:
- Reliable Sources: Focus on reputable medical websites, organizations, and healthcare professionals.
- Specific Keywords: Use clear search terms, be specific with your questions, and consider your location when searching.
- Diverse Resources: Utilize a variety of sources, including medical websites, databases, patient support groups, and books.
- Consult Your Doctor: Always discuss any information you find with your healthcare provider for personalized advice.
By using these strategies, you can access a wide range of information about recurrent abortion, empowering yourself with knowledge and connecting with resources for support.
Frequently Asked Questions (FAQ)
What is Recurrent abortion/ Habitual Abortion?
Recurrent abortion/ Habitual Abortion is defined as a sequence of three or more consecutive spontaneous abortion before 20 weeks.
What causes Recurrent abortion/ Habitual Abortion?
Homoeopathic Medicine For Recurrent Abortion
- Genetic factors
- Endocrine and metabolic
- Infection
- Inherited thrombophilia
- Immune factors Autoimmunity
What are the symptoms of Recurrent abortion/ Habitual Abortion?
- Vaginal spotting or bleeding
- Pain or cramping in your abdomen or lower back
- Fluid or tissue passing from your vagina
Homeopathic Medicines used by Homeopathic Doctors in treatment of Recurrent abortion/ Habitual Abortion?
- Arnica
- Belladonna
- Chamomilla
- Sabina
- Platina
- Plumbum





