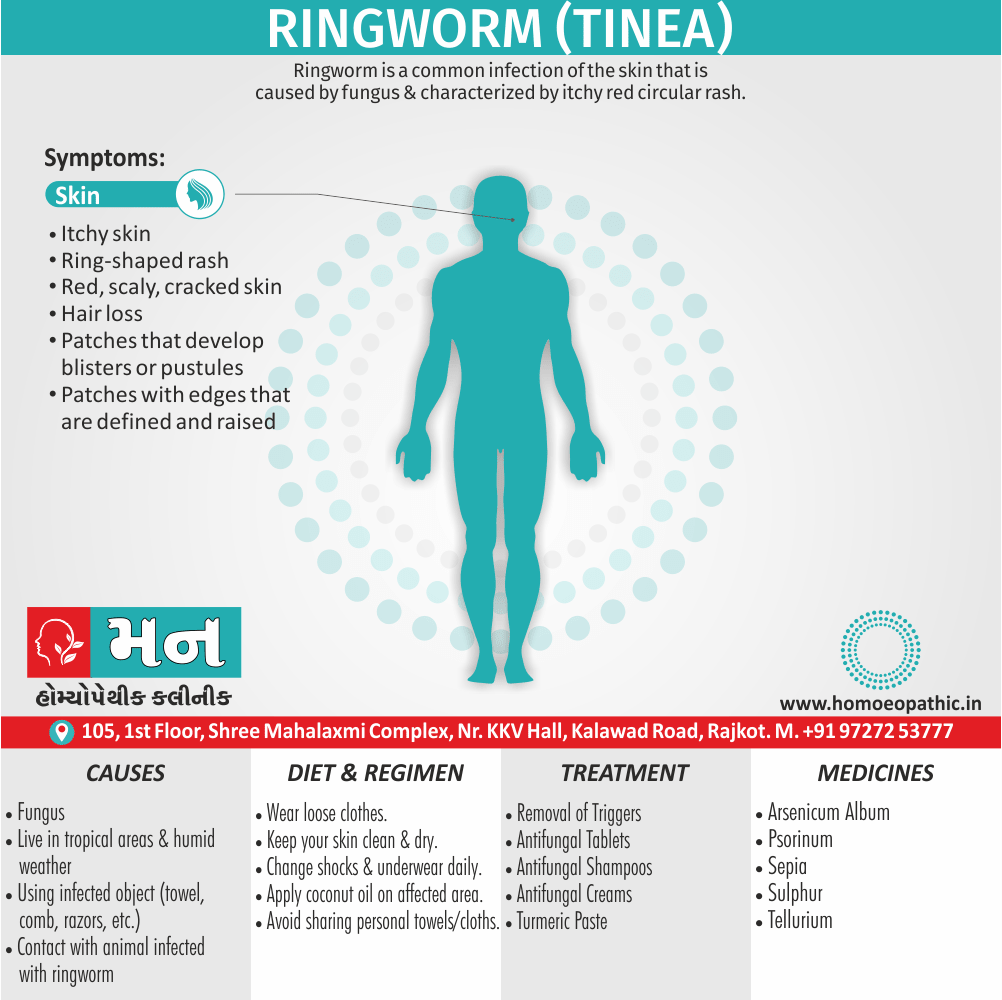
Ringworm (Tinea)
Definition
Ringworm is a common infection of the skin that is caused by fungus & characterised by itchy red circular rash.
It is also called “tinea” or “dermatophytosis.”
Ringworm has two main options for synonyms, depending on how technical you want to get:
Technical Medical Term:
Tinea – This is the genus name for the fungus that causes ringworm. There are different types of tinea depending on the body part affected (e.g., tinea capitis for scalp ringworm).
Informal Synonyms:
- Dermatophytosis – This is a broader term for any fungal infection of the skin, hair, or nails.
- Body ringworm, scalp ringworm, etc. – You can describe the specific area affected with "ringworm" after it (e.g., scalp ringworm).
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Ringworm (Tinea)
Dermatophyte infections (ringworm) are extremely common also usually caused by fungi of the Microsporum, Trichophyton and Epidermophyton species.
Furthermore, The fungi can originate from soil (geophilic) or animals (zoophilic), or be confined to human skin (anthropophilic).
In detail, Dermatophyte infections usually present with skin(tinea corporis), scalp (tinea capitis), groin (tinea cruris), foot (tinea pedis) also nail (onychomycosis) involvement. [1]
Besides this, It is called ringworm because the itchy, red rash has a ring-like appearance.
However, ringworm is nothing to do with worms.
It can affect different parts of the body.
Epidemiology
Epidemiology
The epidemiology of ringworm (dermatophytosis) in India presents a complex picture with varying prevalence rates across different regions and age groups.
- A study by Noronha et al. (2023) revealed a wide range of prevalence, from 6.09% to 61.5%, with higher rates reported in North India compared to South India, contrary to expectations based on climate.
- The study also highlighted an increasing trend of dermatophytosis across India in the last 5-7 years, affecting individuals of all ages, including infants and children.
- Another study mentioned in Forbes India (2023) estimated that 1-12 cases out of every 1,000 patients in India are affected by fungal infections, emphasizing the significant burden of this disease.
These references underscore the substantial prevalence and evolving nature of ringworm in India, highlighting the need for continued research and effective public health interventions to address this significant health concern.
Causes
Causes of Ringworm (Tinea)
- Certain types of fungi (plural of fungus) cause ringworm.These fungi thrive where it’s warm and humid.
- Ringworm is common in tropical areas and during hot, humid summers.
- It flourishes in warm, moist locker rooms and indoor pools.
- You can also get ringworm when the weather is cool because ringworm is extremely contagious.
It’s possible to get ringworm from:
- Having skin-to-skin contact with someone who have ringworm.
- Petting an animal like a dog, cat, or farm animal infected with ringworm.
- Touching soil infected with ringworm.
- Using an infected object like a phone, comb, or towel.
Risk Factors:
- Live in a tropical area
- Spend time in hot, humid weather
- Sweat heavily
- Wrestle, play football, or participate in another contact sport
- Live in close contact with others, such as in military housing
- Share towels, clothes, razors, and other things without disinfecting (razors) or washing (clothes and towels) them
- Head-to-head contact can spread scalp ringworm
- Wearing tight clothing
- Obesity
- Have diabetes
The fungi that cause ringworm can live on any infected object, including clothing, brushes, and sports equipment for a long time. [5]
Types
Types of Ringworm (Tinea)
Areas of the body that can be affected by ringworm include:
- Feet (i.e. tinea pedis, commonly called “athlete’s foot”)
- Groin, inner thighs, or buttocks (i.e. tinea cruris, commonly called “jock itch”)
- Scalp (i.e. tinea capitis)
- Beard (i.e. tinea barbae)
- Hands (i.e. tinea manuum)
- Toenails or fingernails (i.e. tinea unguium, also called “onychomycosis”)
- Other parts of the body such as arms or legs (i.e. tinea corporis) [4]
Risk Factors
Risk Factors of Ringworm (Tinea)
- Live in a tropical area
- Spend time in hot, humid weather
- Sweat heavily
- Wrestle, play football, or participate in another contact sport
- Live in close contact with others, such as in military housing
- Share towels, clothes, razors, and other things without disinfecting (razors) or washing (clothes and towels) them
- Head-to-head contact can spread scalp ringworm
- Wearing tight clothing
- Obesity
- Have diabetes [5]
Pathogenesis
Pathogenesis of Ringworm
Ringworm, or dermatophytosis, is primarily caused by dermatophyte fungi, which have the unique ability to invade and thrive in keratinized tissues like skin, hair, and nails. The pathogenesis involves several steps:
Adherence: Fungal spores adhere to the skin surface, facilitated by factors like moisture, warmth, and minor skin abrasions.
Invasion: Dermatophytes produce enzymes, such as keratinases, that break down keratin, allowing the fungus to penetrate the stratum corneum (outermost skin layer).
Growth and Spread: The fungus grows within the keratinized tissue, forming hyphae (thread-like structures) that spread radially, leading to the characteristic ring-shaped lesion.
Inflammation: The host’s immune system responds to the fungal invasion, triggering inflammation, which manifests as redness, itching, and scaling.
Hair and Nail Involvement: In some cases, the fungus may invade hair follicles or nail beds, causing hair loss or nail discoloration and thickening.[7]
This comprehensive dermatology textbook provides detailed information on the pathogenesis, clinical presentation, diagnosis, and treatment of various skin diseases, including ringworm. It serves as a valuable resource for healthcare professionals and researchers in the field of dermatology.
Pathophysiology
Pathophysiology of Ringworm
Ringworm, or dermatophytosis, is a superficial fungal infection that targets keratinized tissues such as skin, hair, and nails. The pathophysiology unfolds through a series of key steps:
Adherence & Invasion: Dermatophyte fungal spores land on the skin, attaching themselves with the aid of factors like moisture, warmth, and minor skin injuries. They then use enzymes like keratinases to break down keratin, a structural protein, enabling their penetration into the stratum corneum (outermost skin layer).
Hyphal Growth & Spread: The fungus thrives within the keratin-rich environment, growing hyphae (thread-like structures) that radiate outward. This radial expansion creates the characteristic circular or ring-shaped lesion often associated with ringworm.
Host Immune Response: The body’s defense system reacts to the fungal invasion, triggering an inflammatory response. This manifests as redness, itching, and scaling at the infection site.
Hair & Nail Involvement: In certain cases, the dermatophytes may extend their invasion into hair follicles or nail beds. This can result in hair loss, brittle nails, or discoloration and thickening of the nails.[8]
This acclaimed dermatology textbook delivers an in-depth exploration of the pathophysiology, clinical manifestations, diagnosis, and treatment of various skin disorders, including ringworm. It serves as an invaluable resource for both healthcare practitioners and researchers specializing in dermatology.
Clinical Features
Clinical Features of Ringworm
Ringworm, also known as dermatophytosis, presents with a range of clinical manifestations depending on the site of infection and the specific dermatophyte species involved. Common clinical features include:
Skin:
- Annular or circular lesions with a well-defined, raised border and central clearing
- Redness, scaling, and itching at the affected site
- May present as multiple lesions or coalesce into larger patches
Scalp (Tinea capitis):
- Scaly patches with hair loss
- Broken hairs or black dots (representing broken hair shafts)
- May be accompanied by inflammation, pustules, or kerion (severe inflammatory reaction)
Nails (Tinea unguium):
- Thickened, discolored, and brittle nails
- White or yellow discoloration
- Separation of the nail from the nail bed (onycholysis)
Feet (Tinea pedis):
- Itching, burning, and scaling between the toes or on the soles of the feet
- Blisters or fissures may also be present
- Foul odor in severe cases
Groin (Tinea cruris):
- Red, itchy rash in the groin folds
- Well-defined border with central clearing
- May extend to the inner thighs or buttocks[9]
Rook’s Textbook of Dermatology is a comprehensive resource that provides in-depth information on the clinical features, diagnosis, and management of various skin diseases, including ringworm. It is an invaluable reference for dermatologists and other healthcare professionals involved in the care of patients with skin conditions.
Sign & Symptoms
The Sign & Symptoms
Symptoms typically appear between 4 and 14 days after the skin comes in contact with the fungi that cause ringworm.
The symptoms of ringworm often depend on which part of the body is infected, but they generally include:
- Itchy skin
- Ring-shaped rash
- Red, scaly, cracked skin
- Hair loss [3]
Body or skin ringworm (Tinea Corporis):

Corporis
Symptoms include i.e.:
- A rash with a ring-like appearance.
- The skin may be red and inflamed around the outside of the ring, but look fine in the middle.
- Patches can grow slowly, increasing in size and appearing on more areas of the body.
- Merging rings.
- Rings feel slightly raised.
- Itchiness, especially under the rash.
Groin infection (Tinea Cruris/ “Jock Itch”):

Tinea Cruris
There may be:
- Itchiness, especially in and around the groin.
- Redness and a burning sensation in the affected area.
- Flaky and scaly skin on the inner thighs.
- Symptoms worsen when walking, running, or exercising.
- Tight clothing makes symptoms worse.
Beard area (Tinea Barbae):

Barbae
This can involve:
- Redness, swelling, and pus-filled bumps on the cheeks, chin, and upper neck.
- Hair loss, which usually resolves after treatment.
- Swollen glands.
- Raw, open skin and raised, soft, spongy patches that weep.
- Tiredness. [2]
Feet with ringworm infection (Tinea Pedis / Athlete’s Foot):

Tinea Pedis

Athlete’s Foot
- Itching, burning, and stinging on your soles also between your toes.
- Dry, scaly skin that usually begins between the toes also can spread to the bottom of the feet, sides, or both.
- Peeling skin
- Blisters, painful cracking skin, bleeding, also thick patches of red and scaly skin.
- Besides this, Skin between the toes turns white, becoming soft and mushy.
- Foul odor.
- Rash on one or both hands because touching the infected foot can spread the infection to your hands.
Nails with ringworm infection (Tinea Unguium / “Onychomycosis”):

Tinea Unguium
- Can infect 1 or several nails
- Begins with thickening of the tissue under the nail (nail bed).
- Nails discolor and thicken.
- Thickened nails may start to lift away from the nail bed.
- Crumbling nails.
- Disappearing nails (In time, you see less of the nails.)
- Toenails more likely than fingernails to become infected.
- Often develops in people who have athlete’s foot for a long time.
Scalp ringworm (Tinea Capitis):
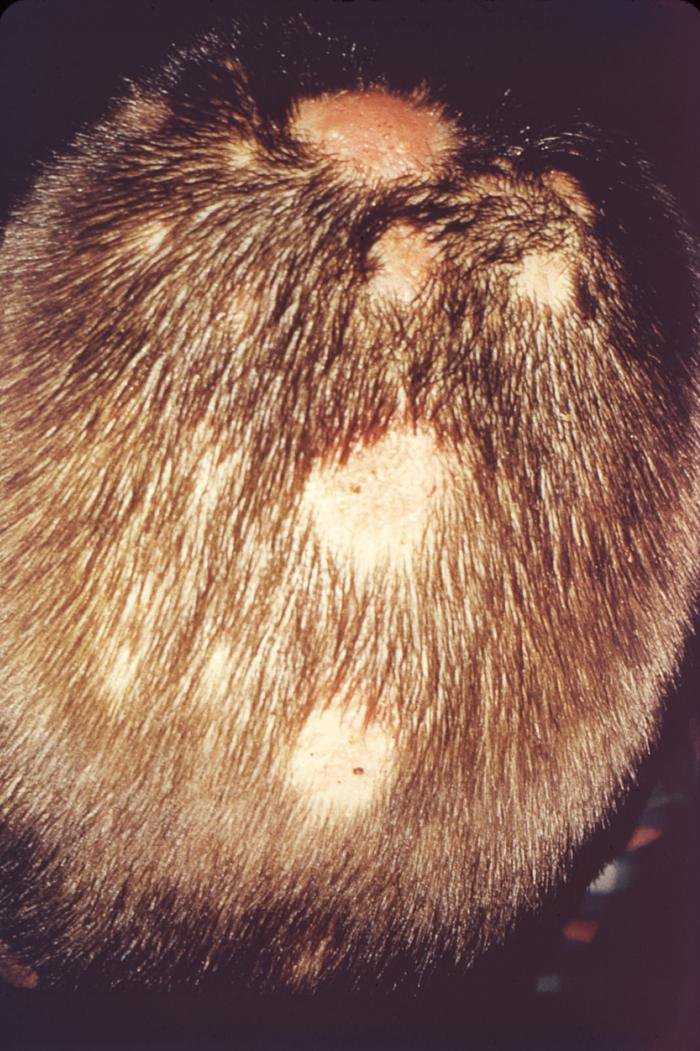
Tinea Capitis
- A scaly bald patch.
- Widespread baldness with thick, crusty patches on the scalp
- Black dots in the bald area.
- Open sores oozing pus.
- Raised soft, spongy, inflamed area.
- Swollen lymph nodes.
- Intense itch. [5]
Clinical Examination
Clinical Examination
The clinical examination of ringworm, or dermatophytosis, involves a thorough assessment of the affected area to identify characteristic features and confirm the diagnosis. The following steps are typically involved:
Visual Inspection: The physician will carefully examine the affected area, noting the presence of annular or circular lesions with a well-defined, raised border and central clearing. They will also assess the extent of the infection, the presence of scaling, redness, or inflammation, and any associated symptoms such as itching or pain.
Wood’s Lamp Examination: A Wood’s lamp, which emits ultraviolet light, may be used to examine the affected area. Some dermatophyte species fluoresce under Wood’s lamp, emitting a characteristic green or yellow color, aiding in the diagnosis.
Microscopic Examination: Skin scrapings or hair samples may be collected from the affected area and examined under a microscope. The presence of fungal hyphae or spores confirms the diagnosis of ringworm.
Fungal Culture: In some cases, a fungal culture may be performed to identify the specific dermatophyte species causing the infection. This information can be helpful in guiding treatment decisions.
Bolognia’s Dermatology is a comprehensive textbook that provides detailed information on the clinical examination, diagnosis, and management of various skin diseases, including ringworm. It is an essential resource for dermatologists and other healthcare professionals involved in the care of patients with skin conditions.
Remember:
- The clinical examination is a crucial step in diagnosing ringworm and differentiating it from other skin conditions.
- A combination of visual inspection, Wood’s lamp examination, microscopic examination, and fungal culture may be used to confirm the diagnosis.
- Early diagnosis and treatment are essential to prevent the spread of infection and complications.
Diagnosis
Diagnosis
- Your doctor will diagnose ringworm by examining your skin and possibly using a black light to view your skin in the affected area.
- Depending on the type of fungus, it may sometimes fluoresce (glow) under black light.
Your doctor may confirm a suspected diagnosis of ringworm by requesting certain tests:
- If you’re getting either a skin biopsy or fungal culture, your doctor will take a sample of your skin or discharge from a blister and send it to a lab to test it for the presence of fungus.
- If you’re getting a KOH exam, your doctor will scrape off a small area of infected skin onto a slide and place drops of a liquid called potassium hydroxide (KOH) on it. The KOH breaks apart normal skin cells, making the fungal elements easier to see under a microscope. [3]
Differential Diagnosis
Differential Diagnosis of Ringworm
Ringworm, also known as dermatophytosis, can mimic various other skin conditions. Therefore, a careful differential diagnosis is crucial to ensure accurate diagnosis and appropriate treatment. Some common differential diagnoses for ringworm include:
- Eczema: This inflammatory skin condition can present with redness, scaling, and itching, which may resemble ringworm. However, eczema typically lacks the well-defined border and central clearing seen in ringworm.
- Psoriasis: This chronic autoimmune condition causes thick, silvery scales on the skin, which can sometimes be confused with ringworm. However, psoriasis lesions are often thicker and more widespread than ringworm lesions.
- Pityriasis rosea: This self-limiting skin condition causes a herald patch followed by a widespread rash with oval-shaped lesions. The rash in pityriasis rosea may resemble ringworm, but it usually has a characteristic "Christmas tree" distribution pattern.
- Granuloma annulare: This inflammatory skin condition causes red or skin-colored bumps that often form a ring shape. It can be difficult to distinguish from ringworm, but granuloma annulare typically lacks scaling and itching.
- Erythema annulare centrifugum: This rare skin condition causes expanding circular or oval lesions with a trailing scale. It can resemble ringworm, but erythema annulare centrifugum lesions tend to be larger and less scaly.[11]
Habif’s Clinical Dermatology is a comprehensive textbook that provides in-depth information on the differential diagnosis of various skin diseases, including ringworm. It is a valuable resource for dermatologists and other healthcare professionals involved in the care of patients with skin conditions.
Complications
Complications of Ringworm (Tinea)
Although ringworm is typically a self-limiting condition, it can sometimes lead to complications, especially if left untreated or in individuals with weakened immune systems. Some potential complications of ringworm include:
Secondary bacterial infection: The breakdown of the skin barrier due to ringworm can create an entry point for bacteria, leading to secondary bacterial infections. These infections can cause increased redness, swelling, pain, and pus formation.
Scarring: Severe or chronic ringworm infections, particularly those involving the scalp or nails, can sometimes result in scarring. Scarring can lead to permanent hair loss or nail deformities.
Cellulitis: In rare cases, ringworm can spread to deeper layers of the skin, causing cellulitis, a serious bacterial infection of the skin and underlying tissues. Cellulitis requires prompt medical attention and antibiotic treatment.
Tinea incognito: The use of topical corticosteroids on ringworm lesions can alter the appearance of the infection, making it more difficult to diagnose. This condition is known as tinea incognito and can lead to delayed treatment and increased risk of complications.
Psychological impact: The visible nature of ringworm, especially on exposed areas of the body, can cause embarrassment, anxiety, and social isolation. This can negatively impact a person’s quality of life.[12]
Dermatology: An Illustrated Colour Text provides comprehensive information on various skin diseases, including ringworm. It discusses the potential complications associated with ringworm and emphasizes the importance of early diagnosis and treatment to prevent these complications.
Investigations
Investigations of Ringworm
Ringworm, also known as dermatophytosis, is typically diagnosed based on clinical presentation. However, several investigations can be employed to confirm the diagnosis and identify the causative fungal species:
Potassium hydroxide (KOH) preparation: Skin scrapings or hair samples are treated with KOH, which dissolves keratin and makes fungal elements more visible under a microscope. The presence of hyphae or spores confirms the diagnosis of ringworm.
Fungal culture: Skin scrapings or hair samples are inoculated onto culture media to isolate and identify the specific dermatophyte species. This helps guide treatment decisions, especially in cases of treatment failure or recurrent infections.
Wood’s lamp examination: A Wood’s lamp, which emits ultraviolet light, can be used to examine the affected area. Some dermatophyte species fluoresce under Wood’s lamp, aiding in the diagnosis, especially in cases of scalp ringworm.
Dermoscopy: This non-invasive technique uses a handheld microscope to magnify the skin surface, allowing for a closer examination of the lesion. Dermoscopy can help differentiate ringworm from other skin conditions and identify specific patterns suggestive of different dermatophyte species.
Skin biopsy: In rare cases, a skin biopsy may be performed to confirm the diagnosis, especially when the clinical presentation is atypical or other investigations are inconclusive.[13]
Clinical Dermatology provides comprehensive information on the diagnosis and management of various skin diseases, including ringworm. It discusses the different investigations used to confirm the diagnosis of ringworm and their clinical significance.
Treatment
Treatment depends on the type of ringworm:
Scalp ringworm:
The most common treatments for scalp ringworm are oral antifungals tablets.
However, the choice of medication will depend on the type of fungi involved.
Terbinafine (Lamisil) i.e.:
- The side effects are normally mild and do not last long.
- They may include diarrhea and nausea.
- People with a history of liver disease should not take terbinafine.
Griseofulvin (Grisovin) i.e.:
- The side effects, which usually go away fairly quickly, may include headache, indigestion, and nausea.
Anti-fungal shampoos i.e.:
- These help prevent the spread of ringworm and may speed up recovery, but they do not cure it.
Shaving a child’s head i.e.:
- There is no evidence that this reduces ringworm infection or accelerates recovery time.
Skin ringworm and groin infection:
- Generally, Most cases are treated with antifungal creams.
- Moreover, If symptoms are severe, or if they cover a large area of the body and do not respond to OTC (Over the Counter) medications, the doctor may prescribe a prescription-strength topical medication.
- Besides this, The doctor may prescribe an oral medication (taken by mouth).
- Lastly, Oral medications can have some side effects, including stomach upset, rash, or abnormal liver function.
Caring for the skin during infection:
Care for the skin properly can help speed recovery.
- Wash the skin gently.
- Dry the skin thoroughly but gently.
- Pat the skin with a towel in tender areas, but do not rub.
- Make sure any folds also areas between the toes are dried thoroughly.
- Change either sock or underwear more often than usual if they cover an infected area.
- Always treat the feet and groin at the same time, as infection often spreads from one area to another.
- Where possible, wear loose-fitting clothing also undergarments, such as boxers.
- People have used home remedies for ringworm for many years before researchers invented antifungal treatments.
Home Remedies:
These treatments include:
Apple cider vinegar i.e.:
- Basically, Some people apply apple cider vinegar-soaked cotton balls over affected areas of skin three times a day to treat ringworm.
Coconut oil i.e.:
- Coconut oil isn’t just for cooking people apply it to their skin to reduce the incidence of ringworm infections.
- Additionally, If you want to try this remedy, apply coconut oil one to three times a day.
Turmeric i.e.
- First of all, Turmeric is a spice you can mix with water to make an antifungal paste.
- In detail, Apply the paste directly to your skin and allow it to dry. [3]
Prevention
Prevention of Ringworm
Ringworm, also known as dermatophytosis, is a contagious fungal infection that can be prevented by adopting certain hygiene practices and lifestyle modifications. Some effective preventive measures include:
Maintaining good personal hygiene:
- Wash hands frequently with soap and water, especially after touching pets or other potentially infected individuals.
- Shower regularly and dry the skin thoroughly, paying particular attention to areas prone to moisture, such as the feet and groin.
- Avoid sharing personal items like towels, combs, and clothing with others.
Protecting feet:
- Wear shower shoes or sandals in public showers, locker rooms, and swimming pools.
- Change socks and shoes regularly, especially if they become damp or sweaty.
- Choose breathable footwear made of natural materials.
Caring for pets:
- Take pets to the veterinarian regularly for check-ups and treatment of any skin conditions.
- Avoid close contact with pets that have visible skin lesions.
- Wash hands thoroughly after handling pets.
Avoiding close contact with infected individuals:
- Refrain from sharing personal items with people who have ringworm.
- Avoid direct skin-to-skin contact with infected individuals.
Boosting immunity:
- Maintain a healthy lifestyle with a balanced diet, regular exercise, and adequate sleep.
- Manage stress levels, as stress can weaken the immune system and increase susceptibility to infections.
Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology provides a concise overview of various skin diseases, including ringworm. It emphasizes the importance of preventive measures in reducing the risk of ringworm infection.[8]
Homeopathic Treatment
Homoeopathic Treatment
Homeopathic treatment for Ringworm is natural, safe and without any side-effects, and one can enjoy immense relief from these frustrating symptoms.
It is a patient-oriented science and medicines are prescribed on the characteristics of the individual rather than just the symptoms of the disease.
Sepia – for ringworm in isolated spots:
- It is the top natural remedy especially for ringworm infection appearing in isolated spots.
- Although the ringworm lesion for using sepia can be noticed on any part of the body, additionally the common location is the bends of the knee and elbow.
- The eruptions are accompanied by itching and scratching, though scratching does not provide any relief.
- Apart from these symptoms, increased sweating with or without a bad smell may be noticed in persons requiring Sepia.
- Another peculiar symptom for using sepia is the recurrence of ringworm infection in every spring season.
- Sepia can help in eradicating the tendency to have a ringworm infection every time the spring season approaches.
- High sensitivity towards cold air may be found with these symptoms.
- The mental symptoms of utmost importance while recommending sepia are irritability and indifferent behavior towards family, friends, and life.
Tellurium – for ringworm infection with lesions on large part of body:
- Tellurium is the best natural medicine when ringworm eruptions cover a large part of the body.
- Here, the ringworm lesions join one another and eventually cover a large area of skin.
- Moreover, The body is densely covered with intersecting ring lesions.
- In detail, The ringworm eruptions with clear margins are easily detectable on an increased surface of the skin for using tellurium.
- Eruptions are marked by excessive itching and stinging sensation.
- The itching remains present throughout day also night.
- Besides this, Cold air seems to worsen the itching.
- All in all, An offensive smell from the area covered with ringworm eruptions is frequently noticed.
Sulphur – for intense itching and burning:
- In treating ringworm lesions also, sulphur is quite successful.
- The main complaint described by ringworm patients that helps in selecting sulphur is intense itching also burning in eruptions.
- The person goes on scratching the lesions but it does not seem to provide any relief.
- Only the intense burning sensation follows scratching.
- Additionally, The itching is heightened at night in most patients who can benefit from sulphur.
- It is also of great help in all cases of ringworm appearing on limbs, scalp, trunk, and face when accompanied by intense itching and burning.
- This remedy specifically helps to soothe the itching and burning, followed by the disappearance of eruptions.
- Sulphur is a deep acting natural remedy that can help in root extraction of ringworm lesions if used for some time.
- Lastly, It should always be the first Homeopathic choice in those cases of ringworm that have been suppressed with local medications of varying kinds.
Psorinum – for Ringworm (Tinea) on scalp and bends of joints:
- Psorinum is an excellent skin remedy used for the treatment of ringworm.
- It is mainly used for ringworm infection of scalp also bends of joints.
- Furthermore, The eruptions are excessively itching.
- In most cases, the itching is enhanced in bed due to warmth.
- Hair loss is the key noticeable feature for using natural remedy psorinum for ringworm of the scalp (Tinea Capitis).
- In a few cases, the hair appears dry, rough also lustreless.
- Another key symptom is profuse sweating with bad odour throughout the body.
- High sensitivity to cold air is another prominent symptom to be noted for using Psorinum.
- The persons needing psorinum cannot tolerate cold air even in summer weather.
Arsenic Album – for scalp Ringworm (Tinea):
- It is a very beneficial natural remedy for ringworm of scalp.
- The scalp shows bald spots with intolerable itching.
- The scalp is rough and dry.
- Along with itching, there is an intense burning sensation.
- The symptoms of itching and burning are most markedly disturbing at night.
- Arsenic Album helps in all spheres to reduce itching, burning and also helps in regrowth of hair on bald spots.
- Apart from these local symptoms, a few general symptoms are also to be taken into account in selecting Arsenic Album for Tinea Capitis.
- The first is acute anxiety.
- The second is extreme restlessness.
- The next is fastidiousness with a desire for clean surroundings and objects to be placed at a proper place.
- Thirst for a small quantity of water at very short intervals is another important symptom which is significant for selecting arsenic album. [6]
Diet & Regimen
Diet & Regimen for Ringworm
- Include immune-boosting foods: Focus on foods rich in vitamins and minerals, particularly vitamin C, vitamin D, and zinc, which play a crucial role in immune function. Good sources include citrus fruits, leafy green vegetables, nuts, seeds, and whole grains.
- Limit processed foods and sugar: Processed foods and sugary drinks can negatively impact immune function and gut health, potentially hindering the healing process.
- Stay hydrated: Adequate hydration is essential for skin health and overall well-being. Aim to drink plenty of water throughout the day.
- Consider probiotics: Probiotics, found in fermented foods like yogurt and sauerkraut or as supplements, can support gut health and indirectly boost immunity.
Regimen:
In addition to dietary measures, adopting certain lifestyle practices can also help manage ringworm and prevent its recurrence:
- Maintain good hygiene: Wash hands frequently, especially after touching affected areas or pets. Shower regularly and dry the skin thoroughly.
- Avoid scratching: Scratching can worsen the infection and increase the risk of secondary bacterial infections.
- Keep the affected area clean and dry: Gently wash the affected area with mild soap and water, and pat it dry completely.
- Avoid sharing personal items: Do not share towels, clothing, or other personal items with others to prevent the spread of infection.
- Follow the prescribed treatment plan: Adhere to the medications and topical treatments prescribed by your healthcare provider.
Integrative Dermatology provides a holistic approach to skin health, including the management of ringworm. It discusses the role of diet and lifestyle modifications in supporting the body’s natural healing processes and preventing recurrence of infections.[14]
Do’s and Don'ts
The Do’s & Don’ts
Do’s:
- Take medical advice: Consult a doctor or dermatologist for proper diagnosis and treatment recommendations.
- Do keep the affected area clean and dry: Wash the affected area with mild soap and water twice daily. Pat it dry thoroughly.
- Do apply prescribed medications: Use antifungal creams, lotions, or powders as directed by your doctor.
- Complete the full course of treatment: Even if symptoms improve, continue the treatment for the prescribed duration to ensure complete eradication of the fungus.
- Do wash hands frequently: Wash hands thoroughly after touching the affected area or applying medication.
- Do wash clothing, bedding, and towels in hot water: This will help kill any fungal spores and prevent reinfection.
- Keep your skin cool and dry: Avoid excessive sweating and wear loose-fitting clothes made of breathable fabrics.
- Do avoid sharing personal items: Do not share towels, combs, clothing, or other personal items with others.
- Do inform close contacts: If you have ringworm, inform close contacts so they can be aware of the risk and take preventive measures.
- Be patient: Ringworm treatment can take several weeks or even months. Be patient and consistent with your treatment plan.
Don’ts:
- Don’t scratch: Scratching can worsen the infection and increase the risk of secondary bacterial infections.
- Avoid sharing personal items: Avoid sharing towels, combs, clothing, or other personal items with others to prevent the spread of infection.
- Don’t cover the affected area with tight bandages or clothing: This can create a warm, moist environment that favors fungal growth.
- Don’t stop treatment prematurely: Even if symptoms improve, complete the full course of treatment as directed by your doctor.
- Not ignore symptoms: If you suspect you have ringworm, seek medical attention promptly. Early diagnosis and treatment can prevent complications and reduce the risk of spreading the infection to others.
Terminology
Terminology
- Dermatophytosis: The medical term for ringworm, encompassing all fungal infections of the skin, hair, and nails caused by dermatophytes.
- Dermatophytes: A group of fungi that thrive on keratin, a protein found in skin, hair, and nails.
- Tinea: The general term used to describe any dermatophyte infection, followed by a Latin term indicating the affected body part.
- Tinea capitis: Ringworm of the scalp
- Tinea corporis: Ringworm of the body
- groin (jock itch)
- Tinea pedis: Ringworm of the feet (athlete’s foot)
- Tinea unguium: Ringworm of the nails
- Hyphae: Thread-like structures that make up the body of a fungus.
- Spores: Reproductive units of fungi that can spread the infection.
- KOH preparation: A diagnostic test where skin scrapings are treated with potassium hydroxide to dissolve skin cells and make fungal elements more visible under a microscope.
- Fungal culture: A laboratory test where a sample from the infected area is placed on a special medium to grow and identify the specific type of fungus.
- Antifungal medications: Medications used to treat fungal infections, available in topical (creams, lotions, powders) or oral forms.
- Zoonotic transmission: Transmission of an infection from animals to humans. Some types of ringworm can be spread from pets to people.
- Anthropophilic: Dermatophytes that primarily infect humans.
- Zoophilic: Dermatophytes that primarily infect animals but can also infect humans.
- Geophilic: Dermatophytes that live in the soil but can occasionally infect humans.
- Immunocompromised: Having a weakened immune system, which can increase the risk of severe or recurrent ringworm infections.
References
References
- Davidson’s Principles and Practice of Medicine (22nd edition) Ch. 28
- https://www.medicalnewstoday.com/articles/158004.php
- https://www.healthline.com/health/ringworm#pictures
- https://www.cdc.gov/fungal/diseases/ringworm/diagnosis.html
- https://www.aad.org/public/diseases/contagious-skin-diseases/ringworm#treatment
- https://www.drhomeo.com/homeopathic-treatment/homeopathic-medicine-ringworms/
- Andrews’ Diseases of the Skin: Clinical Dermatology, 13th Edition, William D. James, Timothy G. Berger, Dirk M. Elston, 2020, Elsevier.
- Fitzpatrick’s Dermatology in General Medicine, 9th Edition, Klaus Wolff, Lowell A. Goldsmith, Stephen I. Katz, Barbara A. Gilchrest, Amy S. Paller, David J. Leffell, 2019, McGraw Hill Professional.
- Rook’s Textbook of Dermatology, 9th Edition, Christopher Griffiths, Jonathan Barker, Tanya Bleiker, Richard Chalmers, Fiona Creamer, 2016, Wiley Blackwell.
- Bolognia JL, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
- Habif’s Clinical Dermatology, 7th Edition, James G. H. Dinulos, 2021, Elsevier.
- Dermatology: An Illustrated Colour Text, 6th Edition, David J. Gawkrodger, 2016, Churchill Livingstone.
- Clinical Dermatology, 6th Edition, Thomas P. Habif, James G. H. Dinulos, Michael J. Chapman, Sarah C. Hurley, 2016, Mosby.
- Integrative Dermatology, Second Edition, Elizabeth L. Hale, Adam I. Rubin, 2018, Elsevier.
Also Search As
Ringworm Also search as
Online Search Engines:
- Use specific keywords:
- "homeopathic treatment for ringworm"
- "homeopathy and ringworm"
- "ringworm remedies in homeopathy"
- "homeopathic approach to dermatophytosis"
- Include the specific type of ringworm (e.g., "tinea capitis homeopathy") for more targeted results.
- Utilize advanced search options:
- Filter results by date to find recent articles.
- Use quotation marks to search for exact phrases.
- Exclude certain words with the minus sign (e.g., "ringworm homeopathy -conventional treatment").
Homeopathic Websites and Journals:
- Visit websites of reputable homeopathic organizations and institutions:
- The National Center for Homeopathy (NCH)
- The American Institute of Homeopathy (AIH)
- The Faculty of Homeopathy (UK)
- Search for articles within online homeopathic journals:
- The Journal of the American Institute of Homeopathy
- Homeopathy
- The International Journal of High Dilution Research
Homeopathic Libraries and Databases:
- Visit local homeopathic libraries or clinics to access books and journals.
- Search online databases dedicated to homeopathic research:
- HomBRex
- The American Homeopath
Additional Tips:
- Consult a qualified homeopath: They can provide valuable information and recommend reliable resources.
- Look for articles written by experienced homeopaths or researchers.
- Check the credibility of the source and the date of publication.
- Cross-reference information from multiple sources to ensure accuracy.
Frequently Asked Questions (FAQ)
What is Ringworm?
Ringworm is a common infection of the skin that is caused by fungus & characterised by itchy red circular rash. Ringworm is also called “tinea” or “dermatophytosis.”
What causes Ringworm?
- Fungi
- Skin-to-skin contact
- Animal infected with ringworm
- Touching soil infected
- Using an infected object
What are the symptoms of Ringworm?
- Itchy skin
- Ring-shaped rash
- Red, scaly, cracked skin
- Hair loss
Give the types of Ringworm ?
- Tinea pedis
- Tinea cruris
- Tinea capitis
- Tinea barbae
- Tinea manuum
- Tinea unguium
- Tinea corporis
How is ringworm spread?
- Ringworm is highly contagious and spreads through direct skin-to-skin contact with an infected person or animal. It can also be transmitted indirectly through contaminated objects like towels, clothing, or combs.
How is ringworm diagnosed?
- A doctor can often diagnose ringworm based on its appearance. Sometimes, they may take a skin scraping or sample to confirm the diagnosis under a microscope.
Can homeopathy effectively treat ringworm?
- Homeopathy offers a holistic approach to address the underlying causes of ringworm and stimulate the body’s natural healing abilities to combat the fungal infection.
How does a homeopath select the right remedy for ringworm?
- A detailed case analysis, considering the location, appearance of the lesions, itching intensity, and overall health, is crucial in selecting the most suitable remedy.
How long does it take to see results with homeopathy for ringworm?
- The response time varies depending on the individual and the severity of the infection. Some may experience improvement within a few weeks, while others may require longer-term treatment.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Ringworm?
Homoeopathic medicines for ringworm
- Sepia
- Tellurium
- Sulphur
- Psorinum
- Arsenic Album
