Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
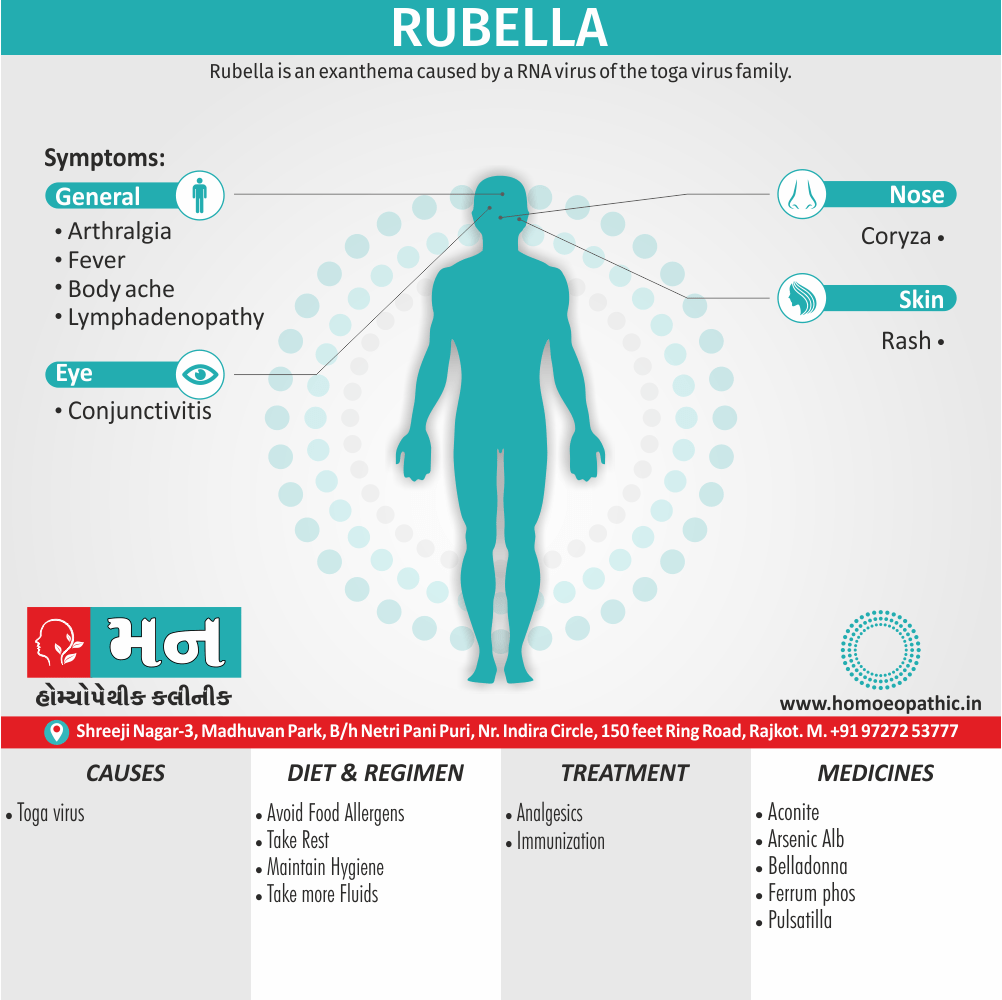
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
It is also known as German Measles or 3-Day measles,[2]
Transmission – Droplet inhalation from an infected person. Neonates with congenital infection are prominent shedders of the virus, which may found, often as long as 6 months. Incubation period – 14–21 days. Period of infectivity – from 7 days before to 2 weeks after onset.
Epidemiology
Epidemiology
Recent Trends (2017-2021)
- Incidence: The incidence of rubella declined 48%, from 2.3 to 1.2 cases per million population. (Progress Toward Measles and Rubella Elimination — India, 2005–2021 | MMWR – CDC, 2022)
- Age Group: In 2021, among the laboratory-confirmed and epidemiologically linked cases, 58% of rubella cases were reported in children aged 9 months–4 years. (Progress Toward Measles and Rubella Elimination — India, 2005–2021 | MMWR – CDC, 2022)
- Genotype: Rubella virus genotype 2B was detected and reported from 43 patients during 2017–2021. However, genotype information is available for a small proportion of rubella cases (0.4%) during this period. (Progress Toward Measles and Rubella Elimination — India, 2005–2021 | MMWR – CDC, 2022) .
Overall Burden
- Congenital Rubella Syndrome (CRS): It is estimated that over 2 lakh babies are born with birth defects because of Rubella infection during pregnancy in the Indian sub-continent.
- Susceptibility: Around 40-45% of women in the childbearing age are susceptible to Rubella.
Key Points
- India has made significant progress in reducing the incidence of rubella through nationwide vaccination campaigns.
- However, rubella remains a public health concern, particularly due to the risk of CRS.
- Continued efforts are needed to improve vaccination coverage and surveillance to achieve rubella elimination.
Causes
Causes
- It is caused by a virus that’s passed from person to person. It can spread when an infected person coughs or sneezes. It can also spread by direct contact with infected mucus from the nose and throat.
- It can also passed on from pregnant women to their unborn children through the bloodstream.
- A person who has infected with the virus that causes rubella is contagious for about one week before the onset of the rash until about one week after the rash disappears.
- An infected person can spread the illness before the person realizes they has it.[4]
Types
Types
According to Togaviruses: Rubella Virus in Medical Microbiology (4th edition) by Samuel Baron (editor), published in 1996 by the University of Texas Medical Branch at Galveston, there is only one serotype of rubella virus. However, the book also notes that phylogenetic analysis suggests there may be at least three distinct genetic lineages of the virus.[5]
Risk Factors
Risk Factors
According to Rubella (German measles) in Medical Microbiology (4th edition), edited by Samuel Baron and published in 1996 by the University of Texas Medical Branch at Galveston, the primary risk factors for contracting rubella include:
- Being unvaccinated or undervaccinated: The most significant risk factor is not having received the MMR (measles, mumps, rubella) vaccine or not having completed the full vaccination series.
- Traveling to areas where rubella is endemic: Rubella remains prevalent in some parts of the world. Traveling to these regions increases the risk of exposure, particularly for unvaccinated individuals.
- Being a healthcare worker: Healthcare professionals who work with potentially infected patients have an increased risk of exposure.
- Being pregnant: While rubella is generally mild in children and adults, it poses a severe risk to developing fetuses. Pregnant women who contract rubella, especially during the first trimester, can pass the virus to their unborn child, leading to congenital rubella syndrome (CRS), which can cause serious birth defects or even fetal death.[5]
Pathogenesis
Pathogenesis
According to Rubella (German measles) in Medical Microbiology (4th edition), edited by Samuel Baron and published in 1996 by the University of Texas Medical Branch at Galveston, the pathogenesis of rubella unfolds as follows:
- Transmission and Initial Infection: The rubella virus is primarily transmitted via respiratory droplets. Following inhalation, the virus replicates in the nasopharynx and regional lymph nodes.
- Viremia and Systemic Spread: The virus subsequently enters the bloodstream, leading to viremia. This systemic spread allows the virus to reach various organs and tissues, including the skin and joints.
- Rash and Immune Response: The characteristic rash of rubella is believed to be an immune-mediated response to the virus in the skin.
- Congenital Rubella Syndrome (CRS): In pregnant women, the virus can cross the placenta and infect the developing fetus. The timing of infection during pregnancy significantly impacts the severity of CRS. Infection during the first trimester poses the highest risk of severe birth defects, affecting the eyes, ears, heart, and brain.[5]
Pathophysiology
Pathophysiology of Rubella
According to Rubella (German measles) in Medical Microbiology (4th edition), edited by Samuel Baron and published in 1996 by the University of Texas Medical Branch at Galveston, the pathophysiology of rubella involves:
- Cellular Infection and Replication: The rubella virus primarily infects cells of the respiratory tract. The virus attaches to host cell receptors and enters the cell via endocytosis. Once inside, the virus uncoats, and its RNA genome is released into the cytoplasm. The viral RNA is translated into viral proteins, and new viral RNA is synthesized. The new viral particles then assemble and bud from the infected cell, ready to infect other cells.
- Spread and Tissue Damage: The virus spreads from the respiratory tract to the lymph nodes and then to the bloodstream (viremia). This viremia allows the virus to disseminate to various organs and tissues, including the skin, joints, and, in pregnant women, the placenta and fetus. The exact mechanisms by which the virus causes tissue damage are not fully understood but likely involve a combination of direct viral damage to cells and immune-mediated responses.
- Congenital Rubella Syndrome: In the developing fetus, the virus can infect a wide range of cells, leading to a variety of birth defects. The mechanisms behind these defects are complex and involve disruption of normal fetal development, including cell death, impaired cell growth, and chromosomal abnormalities.[5]
Clinical Features
Clinical Features
Prodromal Phase (Before Rash):
- Low-grade fever
- Malaise
- Headache
- Sore throat
- Conjunctivitis
- Lymphadenopathy (especially postauricular, suboccipital, and posterior cervical nodes)
- Forchheimer spots (small, red spots on the soft palate) in some cases
Rash:
- Maculopapular (flat, red spots that may feel slightly raised)
- Begins on the face and spreads rapidly to the trunk and extremities
- Typically lasts 3 days and fades in the same order it appeared
- Can be accompanied by mild pruritus (itching)
Other Possible Symptoms:
- Arthralgia (joint pain) or arthritis, more common in adolescents and adults, particularly women
- Encephalitis (inflammation of the brain), a rare but serious complication
Important Considerations
- Congenital Rubella Syndrome (CRS): Rubella infection during pregnancy can lead to serious birth defects, including hearing loss, cataracts, heart defects, and intellectual disability.
- Asymptomatic Infections: Approximately 25-50% of rubella infections are asymptomatic, especially in young children.
- Differential Diagnosis: The rash of rubella can resemble other viral exanthems (rashes), such as measles, scarlet fever, and drug eruptions. Laboratory testing is necessary to confirm the diagnosis.[6]
Sign & Symptoms
Sign & Symptoms of Rubella
- Exanthem – Rash occurs more often in older children and adults on first or second day of illness, first on face and behind the ears, and then spreads downwards to trunk and limbs.
- The rash is variable but commonly starts as discrete, pink, punctate, erythematous, perifollicular macules that rapidly become confluent.
- Alternatively, there may blotchy pink rash or confluent blush. The rash seldom persists for more than 4 days and is not followed by staining or desquamation.
- Rubella without rash is common in young children. In a dark-skinned patient all that may seen is prominence of hair follicles giving a goose pimpled appearance.
- Arthralgia is common and occasionally arthritis. Distribution is usually symmetrical polysynovitis involving the small joints of hands, knees, hips and intervertebral joints, which occasionally may not remit promptly.
- Lymphadenopathy – Slight enlargement of lymph nodes, particularly of sub occipital and posterior auricular groups.
- Buccal mucous membranes – are inflamed, with blotchy erythema and prominent follicles on soft palate, accompanied by mild conjunctivitis and coryza.[1]
Clinical Examination
Clinical Examination of Rubella
Prodromal Phase
- General: Mild fever, malaise, headache
- Eyes: Conjunctivitis with redness and tearing
- Mouth and Throat: Mild pharyngitis, possible Forchheimer spots (small, red petechiae on the soft palate)
- Lymph Nodes: Tender enlargement of posterior auricular, suboccipital, and posterior cervical nodes
Rash
- Appearance: Maculopapular, pink-red rash
- Distribution: Begins on face, spreads rapidly to trunk and extremities, fades in same order it appeared
- Duration: Typically 3 days
Other Findings
- Arthralgia/Arthritis: May be present, more common in adolescents and adults, particularly women
- Neurologic: Rarely, encephalitis may occur
Important Considerations
- Congenital Rubella Syndrome (CRS): In pregnant women, assess for possible exposure and fetal risk
- Differential Diagnosis: Consider other viral exanthems (measles, scarlet fever, roseola, etc.), drug eruptions, and other causes of rash
- Laboratory Testing: Confirm diagnosis with serology or viral detection.[7]
Diagnosis
Diagnosis of Rubella
- The rubella rash can look like many other viral rashes. So health care providers usually confirm rubella with the help of lab tests.
- You may have a virus culture or a blood test, which can detect the presence of different types of rubella antibodies in your blood.
- These antibodies show whether you’ve had a recent or past infection or a rubella vaccine.[4]
Differential Diagnosis
Differential Diagnosis of Rubella
Conditions to Consider:
- Measles: Can present with similar prodromal symptoms and rash, but measles typically has a higher fever, cough, coryza, Koplik spots, and a more extensive rash that lasts longer.
- Scarlet Fever: May have a similar rash, but typically presents with a sore throat, fever, strawberry tongue, and sandpaper-like rash.
- Roseola Infantum: Characterized by high fever followed by a rash that appears as the fever subsides. The rash is typically rose-colored and less extensive than rubella.
- Parvovirus B19 Infection (Fifth Disease): Presents with a slapped-cheek rash on the face and a lacy rash on the trunk and extremities.
- Enterovirus Infections: Can cause a variety of rashes, including maculopapular eruptions.
- Drug Eruptions: Certain medications can cause rashes that mimic rubella.
- Other Viral Exanthems: Several other viruses can cause rashes, including adenovirus, Epstein-Barr virus, and cytomegalovirus.
Key Points:
- Clinical Presentation: The clinical presentation of rubella can be nonspecific, especially in mild cases.
- Laboratory Testing: Confirmation of rubella requires laboratory testing, such as serology or viral detection.
- Consideration of Exposure: Recent travel or exposure to individuals with rubella should be considered in the differential diagnosis.[6]
Complications
Complications of Rubella
- Encephalitis
- G-B syndrome
- Thrombocytopenia
- Hepatitis
Investigations
Investigations of Rubella
Serology:
- IgM Antibody: Detection of rubella-specific IgM antibody indicates recent infection.
- IgG Antibody: Presence of IgG antibody indicates past infection or immunity due to vaccination. A fourfold rise in IgG titer between acute and convalescent sera also confirms recent infection.
Viral Detection:
- Viral Culture: Isolation of rubella virus from throat swab, urine, or other clinical specimens can confirm the diagnosis, but it is less commonly used due to the need for specialized laboratory facilities.
- Nucleic Acid Amplification Tests (NAATs): Polymerase chain reaction (PCR) or other NAATs can detect rubella virus RNA in clinical specimens, providing a rapid and sensitive diagnosis.
Other Tests:
- Complete Blood Count (CBC): May show mild leukopenia or thrombocytopenia.
- Liver Function Tests: May show mild elevation in liver enzymes.
Important Considerations
- Timing of Testing: Collect specimens during the acute phase of illness, ideally within the first few days of rash onset.
- Prenatal Testing: In pregnant women with suspected rubella exposure, serologic testing is crucial to assess immunity and fetal risk.
- Congenital Rubella Syndrome (CRS): In infants with suspected CRS, testing for rubella-specific IgM and IgG antibodies, as well as viral detection, is necessary to confirm the diagnosis.[7]
Treatment
Treatment of Rubella
- Bed rest
- Analgesics suffice for the uncomplicated attack. Rubella proven by antibody estimation in first 4 months of pregnancy is a strong indication for termination.
- Acetaminophen and ibuprofen can be given to control fever.[2]
- Ibuprofen reduce joint and muscle pain.
Strategies for Immunization
- Combined MMR vaccine give routinely to all children in the second year of life, with a booster in the second decade.
- All women screen when they reach childbearing age and immunize with monovalent rubella vaccine, if non-immune. It is necessary to maintain adequate contraceptive measures for 3 months.
- Routine screening and immunization undertake in the immediate postnatal period. Immunized mothers excrete the vaccine virus in breast milk for up to 1 month; this is not a contraindication to vaccination or breastfeeding.
- Adverse reactions – to vaccine limit and include transient arthralgia, and egg and neomycin hypersensitive reactions.[1]
Prevention
Prevention of Rubella
MMR Vaccine: The most effective way to prevent rubella is through vaccination with the measles, mumps, and rubella (MMR) vaccine.
Recommended Schedule:
- First dose: 12-15 months of age
- Second dose: 4-6 years of age
Catch-up Vaccination: Adolescents and adults without evidence of immunity should receive at least one dose of MMR vaccine.
Pregnant Women: Women of childbearing age should ensure they are immune to rubella before becoming pregnant. If not immune, they should receive the MMR vaccine postpartum.
Healthcare Workers: Healthcare personnel should be immune to rubella to prevent transmission to vulnerable patients.
Secondary Prevention: Outbreak Control
Case Isolation: Individuals with confirmed or suspected rubella should be isolated to prevent further transmission.
Contact Tracing: Identify and assess contacts of infected individuals for possible exposure and need for vaccination or post-exposure prophylaxis.
Post-exposure Prophylaxis: In certain situations, MMR vaccine or immunoglobulin may be offered to susceptible contacts to prevent or modify illness.
Key Points:
High Vaccination Coverage: Maintaining high vaccination coverage is crucial to achieve herd immunity and prevent rubella outbreaks.
Prenatal Counseling: Educate women of childbearing age about the importance of rubella immunity and vaccination before pregnancy.
Public Health Surveillance: Monitor rubella cases and outbreaks to guide prevention and control efforts.
Remember: Vaccination is the cornerstone of rubella prevention. By ensuring widespread vaccination coverage, we can protect individuals from rubella and its serious complications, including congenital rubella syndrome.[6]
Homeopathic Treatment
Homeopathic Treatment of Rubella
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Rubella:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Medicines:
Aconitum napellus
- Sudden high fever with hot dry skin, pain in the eyes, strong thirst, and a fearful or panicky feeling are indications for this remedy.
- Symptoms often start near midnight, and may wake the person up.
Bryonia
- This remedy can be indicated when the rash is slow to appear, and the chest is congested with a painful cough.
- The person’s head hurts when coughing.
- Everything feels worse from motion, making the person want to stay completely still.
- Chills and shivering often come with fever, but warmth can make things worse.
- The person’s mouth may be very dry, with a thirst for long cold drinks.
Euphrasia
- When this remedy is indicated during German Measles, the eyes are swollen, streaming, and very sensitive to light.
- The tears can irritate the face, and the person’s nose may run with a bland and watery discharge.
- Headache may intensify with fever.
- The person has chills, feels worse from warmth, and prefers to stay in a darkened room.\
Pulsatilla
- This remedy is often indicated when the rash is slow to develop and the symptoms of a cold are prominent.
- A stuffy nose producing yellowish mucus, a gagging cough (most often dry at night and loose in the morning), and plugging or inflammation in the ears are common.
- The person does not feel very thirsty, is worse from warmth and stuffy rooms, and improves in open air.
- People who need this remedy often want a lot of comforting and attention.
Belladonna
- Fever that comes on rapidly, with a red flushed face, hot skin, dilated eyes that are sensitive to light.
- Throbbing headache that is worse from jarring are all indications for this remedy.
- The rash is red and may be hot to touch.
- Many children needing Belladonna have nightmares during fever and talk or cry out when apparently asleep.
Gelsemium
- A drowsy, lethargic feeling with fever, droopy eyes, and shaking chills running up and down the spine are strong indications for this remedy.
- The rash is itchy, hot, and dry.
- A headache that begins in the back of the head and neck often seen when Gelsemium is needed.
Kali bichromicum
- When this remedy indicate in German Measles, cold symptoms worsen over time.
- Hoarseness, coughing up of stringy yellow mucus, earache, and sticky eyes may be seen.
- Symptoms can worse in the morning, and the person feels best from staying in bed and keeping warm.
Rhus Toxicodendron
- An extremely itchy rash that feels better from applying heat may indicate a need for this remedy.
- The person is very restless, and may feel driven to get up and pace.
- Stiffness may felt in all the muscles of the body, worse at night, from lying still in bed, and on waking in the morning.
- The person may have chills along with fever, and all symptoms improve by warmth and motion.[3]
Diet & Regimen
Diet & Regimen of Rubella
- Eliminate all suspected food allergens, including dairy (milk, cheese, eggs, and ice cream), wheat (gluten), soy, corn, preservatives, and chemical food additives. Your health care provider may want to test you for food allergies.
- Eat foods high in B-vitamins and iron, such as whole grains (if no allergy), dark leafy greens (such as spinach and kale), and sea vegetables.
- Eat antioxidant foods, including fruits (such as blueberries, cherries, and tomatoes), and vegetables (such as squash and bell pepper).
- Avoid refined foods, such as white breads, pastas, and sugar.
- Eat fewer red meats and more lean meats, cold-water fish, tofu (soy, if no allergy), or beans for protein.
- Use healthy oils for cooking, such as olive oil.
- Reduce significantly or eliminate trans-fatty acids, found in commercially-baked foods, such as cookies, crackers, cakes, and donuts. Also avoid French fries, onion rings, processed foods, and margarine.
- Avoid coffee and other stimulants, alcohol, and tobacco.
- Drink 6 to 8 glasses of filtered water daily.
- Exercise moderately for 30 minutes daily, 5 days a week.[2]
Do’s and Don'ts
The Do’s & Don’ts
Do’s:
- Get vaccinated: The MMR vaccine is the most effective way to prevent rubella. Ensure you and your children are up-to-date on vaccinations.
- Isolate if infected: If you or your child has rubella, stay home for at least 7 days after the rash appears to prevent spreading the virus.
- Practice good hygiene: Wash hands frequently with soap and water, especially after using the bathroom or being in public places. Cover coughs and sneezes with a tissue or your elbow.
- Seek medical advice if pregnant and exposed: If you’re pregnant and suspect you’ve been exposed to rubella, contact your healthcare provider immediately. Early diagnosis and management are crucial.
- Educate others: Spread awareness about the importance of rubella vaccination and prevention measures.
Don’ts:
- Don’t expose others if infected: Avoid contact with pregnant women and other susceptible individuals if you have rubella.
- Not ignore symptoms: If you experience symptoms like fever, rash, or swollen lymph nodes, consult a healthcare professional for diagnosis and advice.
- Don’t self-medicate: Avoid taking any medications without consulting a doctor, especially during pregnancy.
- Don’t panic: While rubella can be serious, especially during pregnancy, most people recover fully with supportive care.
- Not delay vaccination: Ensure timely vaccination for yourself and your children to prevent the spread of rubella and protect vulnerable populations.
Remember: Rubella is a preventable disease. By following these do’s and don’ts, you can contribute to its eradication and protect yourself and others from its complications.
Terminology
Terminologies Of Rubella
Rubella: Also known as German measles, it is a contagious viral infection that causes a mild rash and fever.
Congenital Rubella Syndrome (CRS): A serious condition that can occur when a pregnant woman contracts rubella, leading to birth defects in the baby, such as hearing loss, heart problems, and intellectual disability.
MMR Vaccine: A combination vaccine that protects against measles, mumps, and rubella.
Maculopapular Rash: A type of rash characterized by flat, red spots (macules) that may also have slightly raised bumps (papules).
Prodrome: The initial period of an illness, characterized by general symptoms such as fever, malaise, and headache, before the onset of more specific symptoms.
Postauricular Lymphadenopathy: Swelling of the lymph nodes located behind the ears, a common symptom of rubella.
Forchheimer Spots: Small, red spots on the soft palate that may be seen in some cases of rubella.
Encephalitis: Inflammation of the brain, a rare but serious complication of rubella.
Other Terminologies
Serology: The study of blood serum, particularly for the detection of antibodies.
IgM Antibody: An antibody produced early in the immune response to an infection, indicating a recent or current infection.
IgG Antibody: An antibody produced later in the immune response and providing long-term immunity.
Herd Immunity: A form of indirect protection from infectious disease that occurs when a large percentage of a population has become immune to an infection, thereby providing a measure of protection for individuals who are not immune.
Post-Exposure Prophylaxis: Preventive measures taken after exposure to an infectious disease to reduce the risk of developing the disease.
Viral Exanthem: A rash caused by a viral infection.
Teratogenic: Capable of causing birth defects.
Conjunctivitis: Inflammation of the conjunctiva, the thin, clear membrane that covers the white part of the eye and the inner surface of the eyelids.
Specific Remedies Potentially Relevant to Rubella:
- Pulsatilla: Often used for mild cases with a changeable rash, tearfulness, and a desire for company.
- Belladonna: May be helpful for high fever, red face, and throbbing headache.
- Mercurius Solubilis: Considered when there is swollen glands, sore throat, and increased salivation.
References
References use for Rubella
- Harrison-s_Principles_of_Internal_Medicine-_19th_Edition-_2_Volume_Set
- https://www.stlukes-stl.com/health-content/medicine/33/000145.htm
- https://www.peacehealth.org/medical-topics/id/hn-2239004
- www.mayoclinic.org
- Rubella Virus in Medical Microbiology (4th edition) by Samuel Baron (editor), published in 1996 by the University of Texas Medical Branch at Galveston.
- Nelson Textbook of Pediatrics, 21st Edition, by Kliegman, St. Geme, Blum, Shah, Tasker, Wilson, Behrman; published in 2020 by Elsevier.
- Feigin and Cherry’s Textbook of Pediatric Infectious Diseases, 8th Edition, by Cherry, Demmler-Harrison, Kaplan, Steinbach, Hotez; published in 2019 by Elsevier.
Also Search As
Rubella Also Search As
Online Search Engines:
Use specific keywords:
- "homeopathy rubella"
- "homeopathic treatment for rubella"
- "rubella remedies homeopathy"
- "homeopathic approach to rubella"
Include additional terms for targeted results:
Homeopathic Websites and Forums:
Visit websites of homeopathic organizations or practitioners:
- National Center for Homeopathy
- American Institute of Homeopathy
- Homeopathic Educational Services
Search within online forums dedicated to homeopathy:
- ABC Homeopathy Forum
- Homeopathy World Community Forum
Homeopathic Libraries and Bookstores:
Consult homeopathic libraries or bookstores:
- Local homeopathic clinics or schools might have libraries
- Online bookstores specializing in homeopathy
Consult a Homeopathic Practitioner:
Directly ask a homeopathic practitioner for relevant articles or resources.
They may have access to professional journals or publications.
Tips:
Use quotation marks for exact phrases to refine searches.
Filter search results by date to find recent articles.
Be critical of the information found, as homeopathy lacks scientific evidence.
Always consult with a qualified healthcare professional for any health concerns, especially during pregnancy.
Vaccination remains the most reliable way to prevent rubella and its complications.
Pregnant women should seek professional medical advice regarding any potential exposure to rubella.
Frequently Asked Questions (FAQ)
What are the symptoms of Rubella?
- Exanthem – Rash occurs more often in older children and adults on first or second day of illness, first on face and behind the ears, and then spreads downwards to trunk and limbs.
Is rubella serious?
- Rubella is usually mild in children and adults. However, it can be serious if contracted during pregnancy, potentially causing birth defects.
What is the treatment for rubella?
- There is no specific treatment for rubella. The focus is on managing symptoms with rest, fluids, and over-the-counter pain relievers.
Can homeopathy help with Rubella?
- Homeopathy offers a gentle and supportive approach to managing Rubella symptoms and aiding the body’s natural healing process.
Can homeopathy help prevent Rubella?
- While there is no specific homeopathic preventive for Rubella, constitutional treatment aims to strengthen the immune system and enhance overall well-being, potentially reducing susceptibility to infections.
How long does it take to see results with homeopathy for Rubella?
- The response time varies depending on the individual and the severity of symptoms. Some may experience relief within a few days, while others may require longer-term treatment.
