Scabies
Definition
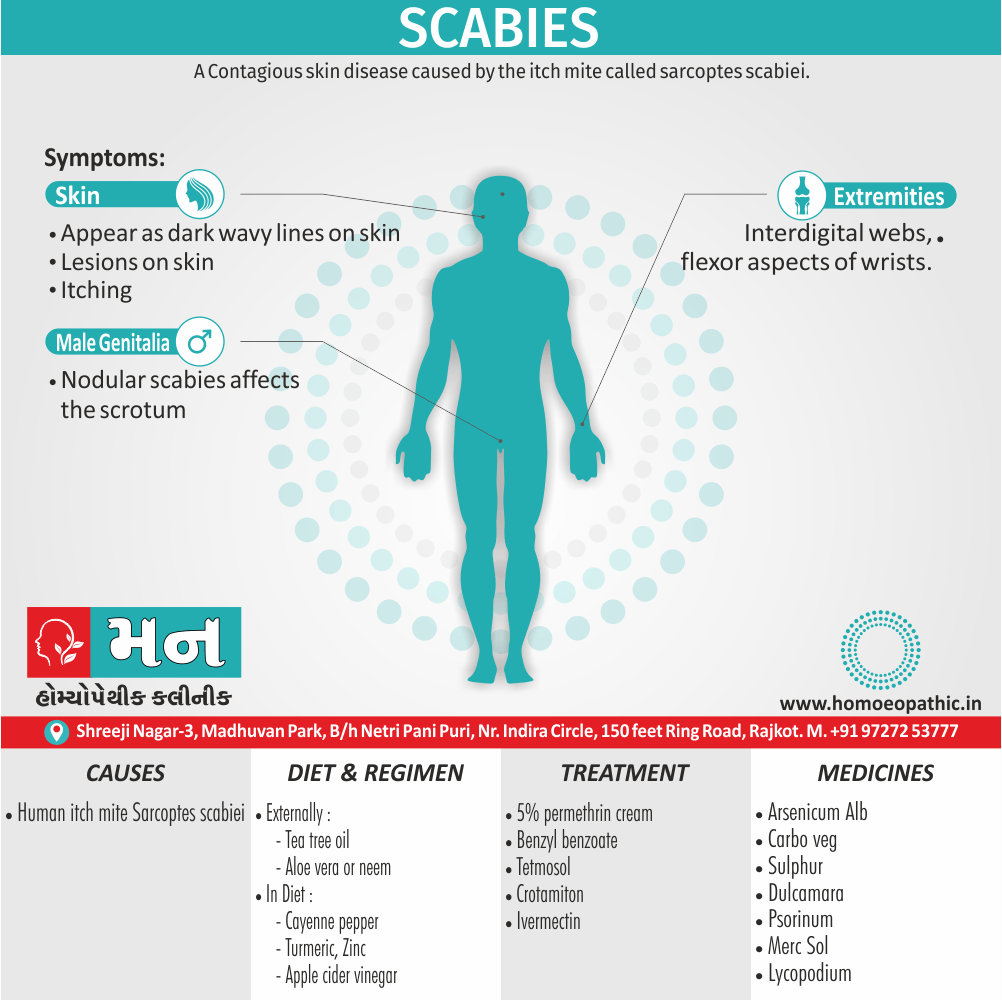
Scabies is a contagious skin Disease marked by itching and small raised red spots, caused by the itch mite. [1][2][3]
There aren’t any perfect synonyms for scabies since it’s a specific medical condition caused by the itch mite, Sarcoptes scabiei. However, here are some related terms you might encounter:
- Acarian itch: This term refers to itching caused by mites in general, not just scabies specifically.
- Sarcoptic mange: This is a skin condition in animals caused by a similar mite.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Scabies
- Generally, Scabies is an itchy skin condition by a tiny mite called Sarcoptes scabiei.
- Moreover, Intense itching occurring where the mite burrows.
- Scabies is an itchy skin condition caused by a tiny burrowing mite called Sarcoptes scabiei. Additionally, Intense itching occurs in the area where the mite burrows. The urge to scratch may be especially strong at night.
- Scabies is contagious and can spread quickly through close physical contact in a family, child care group, school class, nursing home or prison. In detail, Because scabies is so contagious, doctors often recommend treatment for entire families or contact groups.
Epidemiology
Epidemiology
Scabies remains a significant public health concern in India, particularly affecting vulnerable populations and resource-limited communities. Several epidemiological studies have provided valuable insights into the prevalence and risk factors associated with scabies in the Indian context.
Rural community
A study conducted in a rural community in India in 1984 reported a prevalence rate of 13% by population and 30.9% by household, highlighting the substantial burden of scabies in rural areas (An epidemiological study of scabies in a rural community in India, 1984).[9]
Prevalence
A more recent study assessing a scabies outbreak in a known Indian population in 2023 found a prevalence of 39%, further emphasizing the ongoing challenge of scabies control in the country (Assessing the outbreak of scabies in a known Indian population: a prospective clinical study, 2023).[10]
Other key factors
- Additional research has explored specific populations and risk factors. A study among school adolescents in urban Lucknow in 2022 identified a prevalence of 11.6%, with overcrowding and low socioeconomic status being significant risk factors (Prevalence and risk factors of scabies among school adolescents in urban Lucknow, India, 2022).[11]
- Another study focusing on primary schoolchildren in a Kolkata slum in 2017 reported an alarming prevalence of 39.42%, underscoring the heightened vulnerability of children in impoverished settings (Epidemiology of Scabies, 2017).[12]
These studies, along with others, demonstrate the persistent challenge of scabies in India, particularly affecting vulnerable populations and resource-limited communities. Continued efforts in surveillance, prevention, and control are crucial to reduce the burden of this neglected tropical disease in the country.
Causes
Causes of Scabies
- Scabies is caused by the human itch mite Sarcoptes scabiei. [2][3]
- The eight-legged mite that causes scabies in humans is microscopic. In detail, The female mite burrows just beneath your skin and makes a tunnel where it deposits eggs.
- The eggs hatch, and the mite larvae work their way to the surface of your skin, where they mature and can spread to other areas of your skin or to the skin of other people. Besides this, The itching of scabies results from your body’s allergic reaction to the mites, their eggs and their waste.
- Close physical contact and, less often, the sharing of clothing or bedding with an infected person can spread the mites.
- Animals and humans all are affected by their own distinct species of mites. Each species prefers one specific type of host and doesn’t live long away from that preferred host.
- Humans may have a temporary skin reaction from contact with the animal scabies mite. But people generally can’t develop full-blown scabies from this source, as they might from contact with the human scabies mite.
Life cycle of Mite:
- Adult mite laid her egg on blood sucking vector
- Larva enter the host after the vector takes a blood meal
- The eggs become adult in the host body so the host become infected.
- After that mite comes out in the soil through stool.
- Again, this cycle repeatedly occurs.[4]
Types
Types
Classic Scabies:
This is the most common type, characterized by itchy burrows, papules, and nodules, often located on the wrists, hands, and between fingers.
Crusted Scabies (Norwegian Scabies):
A severe form with thick, crusted lesions containing a high number of mites. It’s more common in immunocompromised individuals and can be highly contagious.
Nodular Scabies:
This type presents with persistent itchy nodules, even after treatment, and may require additional therapy.
Bullous Scabies:
Characterized by fluid-filled blisters, it’s more common in infants and young children.
Scabies incognito:
This occurs when scabies is masked or altered by prior treatment or steroid use, making diagnosis challenging.
Note: It’s important to consult a healthcare professional for accurate diagnosis and treatment of any suspected skin condition.
I hope this information is helpful![13]
Risk Factors
Risk factor of Scabies
- Sometimes with complications, such as glomerulonephritis due to nephritogenic streptococci.
- It spreads in households and environments where there is intimate personal contact. [1]
Pathogenesis
Pathogenesis
Mite Infestation:
The female scabies mite, Sarcoptes scabiei var. hominis, burrows into the epidermis, laying eggs and feces along the way.
Immune Response:
The presence of mites, eggs, and feces triggers an immune response, leading to intense itching, inflammation, and skin lesions.
Delayed Hypersensitivity:
The delayed type IV hypersensitivity reaction is the primary driver of the itch and inflammation seen in scabies.
Sensitization:
Repeated exposure to mite antigens can lead to sensitization, making individuals more prone to severe reactions in subsequent infestations.
Secondary Infections:
Scratching can damage the skin, providing an entry point for bacteria, leading to secondary bacterial infections like impetigo.
Note: For accurate diagnosis and treatment of any skin condition, please consult a qualified healthcare professional.[14]
Pathophysiology
Pathophysiology of Scabies
- The symptoms are caused by an allergic reaction of the host’s body to mite proteins, though exactly which proteins remains a topic of study. The mite proteins are also present from the gut, in mite feces, which are de
- posited under the skin. The allergic reaction is both of the delayed (cell-mediated) and immediate (antibody-mediated) type, and involves IgE (antibodies are presumed to mediate the very rapid symptoms on reinfection).
- The allergy-type symptoms (itching) continue for some days, and even several weeks, after all mites are killed. New lesions may appear for a few days after mites are eradicated.
- Nodular lesions from scabies may continue to be symptomatic for weeks after the mites have been killed.
- Rates of scabies are negatively related to temperature and positively related to humidity. [8]
Clinical Features
Clinical Features
Intense Itching:
The hallmark of scabies, often worse at night due to increased mite activity.
Burrows:
Tiny, wavy, thread-like lines on the skin created by the burrowing female mites.
Papules and Nodules:
Small, red bumps or larger, firm bumps that may develop due to the body’s immune response to the mites.
Vesicles and Bullae:
Small, fluid-filled blisters or larger blisters, particularly common in infants and young children.
Excoriations:
Scratch marks and open sores resulting from scratching, which can lead to secondary bacterial infections.
Distribution:
Commonly affects the wrists, hands, finger webs, elbows, armpits, waistline, buttocks, and genitals. In infants and young children, the face, scalp, palms, and soles may also be involved.
Crusted Scabies (Norwegian Scabies):
A severe form with thick, crusted lesions containing a large number of mites, often seen in immunocompromised individuals.
Note: Accurate diagnosis and treatment of scabies require evaluation by a healthcare professional.[15]
Sign & Symptoms
Sign & Symptoms of Scabies
- Intense Pruritus
- Additionally, Itching Worse at night also after a hot shower.
- Burrows – seen most commonly on interdigital webs, flexor aspects of wrists.
- Moreover, Appear as dark wavy lines that end in a pearly bleb containing the female mite
- Most lesions are between the fingers or on the volar wrists, elbows, and penis.Besides this,
- Bacterial superinfection can occur.
- Site: the face, scalp, neck, palms also soles are spread except in children.
- Nodular scabies – affects the scrotum.
- Norwegian scabies – hyper infestation with thousands of mites, seen in steroid therapy, either immunodeficiency or AIDS.[2][3]
Clinical Examination
Clinical Examination
Thorough Skin Inspection:
A comprehensive examination of the entire skin surface is essential, paying close attention to typical areas of involvement (wrists, hands, finger webs, elbows, armpits, waistline, buttocks, genitals).
Burrow Identification:
Careful search for burrows, which may appear as thin, wavy, thread-like lines. A hand lens or dermatoscope can aid in visualization.
Lesion Assessment:
Note the type, distribution, and extent of lesions (papules, nodules, vesicles, bullae, excoriations).
Secondary Infection Evaluation:
Look for signs of bacterial infection, such as pus, crusting, or surrounding erythema.
Crusted Scabies Assessment:
In suspected cases, examine for thick, crusted lesions, especially in immunocompromised individuals.
Nail Examination:
Inspect nails for signs of nail dystrophy, which can sometimes be associated with scabies.
Family and Close Contact Screening:
It’s crucial to examine close contacts for signs of scabies, as it is highly contagious.
Note: Clinical examination alone may not be sufficient for diagnosis. Further tests, such as skin scrapings for microscopic identification of mites or eggs, may be required. Always seek evaluation by a healthcare professional for accurate diagnosis and management.[16]
Diagnosis
Diagnosis of Scabies
- Scrapings from unroofed burrows reveal the mite, its eggs, or fecal pellets also examine it under the microscope.[2]
Differential Diagnosis
Complications
Complications
Secondary Bacterial Infections:
The most common complication, arising from scratching and skin damage. These infections can lead to impetigo, folliculitis, cellulitis, and even more severe systemic infections.
Post-Scabies Eczema:
Persistent itching and inflammation can continue even after successful treatment, requiring further management.
Glomerulonephritis:
A rare but serious complication, particularly associated with streptococcal skin infections secondary to scabies. It can lead to kidney damage.
Rheumatic Fever:
Another rare complication linked to streptococcal infections, potentially affecting the heart and joints.
Sepsis:
In severe cases, especially in immunocompromised individuals, overwhelming infection can lead to sepsis, a life-threatening condition.
Crusted Scabies Complications:
This severe form can lead to extensive skin damage, pain, and systemic complications due to the high mite burden.
Psychological Impact:
The intense itching and social stigma associated with scabies can significantly affect quality of life and mental well-being.
Note: Prompt diagnosis and treatment of scabies are essential to prevent complications. It is crucial to seek medical attention for any concerns about skin health.[17]
Investigations
Investigation
Skin Scrapings:
The gold standard for diagnosis, involving scraping the skin with a scalpel blade and examining the sample under a microscope to identify mites, eggs, or feces.
Dermoscopy:
A non-invasive technique using a handheld dermatoscope to magnify the skin surface and visualize burrows and other characteristic features.
Ink Test:
Applying ink to the skin and wiping it off can help highlight burrows, making them easier to identify.
Polymerase Chain Reaction (PCR):
A molecular test that detects scabies DNA, offering high sensitivity and specificity, especially in cases where microscopy is inconclusive.
Blood Tests:
May be helpful in ruling out other conditions or assessing for complications like secondary infections.
Skin Biopsy:
Rarely needed, but may be considered in atypical presentations or for research purposes.
Note: Scabies investigation should be conducted by a healthcare professional. The choice of diagnostic method may vary depending on the clinical presentation, available resources, and patient factors.[18]
Treatment
Treatment of Scabies
- Gamma-Benzene hemachloride (lindane) 1% solution (side effects – seizures and aplastic anemia)
- 5% permethrin cream – drug of choice
- Benzyl benzoate
- Tetmosol
- Crotamiton [3]
Prevention
Prevention of Scabies
Personal Hygiene:
Regular handwashing and bathing can reduce the risk of transmission.
Avoid Close Contact:
Minimize skin-to-skin contact with infected individuals.
Wash Clothing and Linens:
Wash all clothing, bedding, and towels used by an infected person in hot water and dry them on high heat.
Treat Close Contacts:
Simultaneous treatment of household members and close contacts is crucial to prevent re-infestation.
Environmental Cleaning:
Vacuuming and cleaning surfaces can help remove mites from the environment.
Education and Awareness:
Raising awareness about scabies transmission and prevention is vital, especially in communities with high prevalence.
Note: These preventive measures can significantly reduce the spread of scabies. However, consulting a healthcare professional for specific guidance and timely treatment is crucial in managing outbreaks.[19]
Homeopathic Treatment
Homeopathic Treatment of Scabies
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Scabies:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Medicines:
Arsenicum Alb:
- Inveterate cases; additionally eruption in the bends of the knees.
- Pustular eruption, burning also itching.
- Better from external warmth.
- Furthermore, Scabies with violent itching along with great restlessness is treated well with medicine Arsenic Album.
- The skin peels off in large scales also is very sore to touch in such cases.
- Besides this, Dry, rough, scaly, dirty skin like parchment burns intensely.
- Over-sensitiveness of the skin with acute itching and burning is observed in cases where Arsenic Album will prove the most effective among medicines for scabies.
- All in all, The person is unable to sleep due to violent itching in the affected areas.
Carbo veg:
- Eruption dry and fine, almost over the whole body, worst on extremities.
- Itching worse especially after undressing.
- Dyspeptic symptoms, belching of wind also passing flatus; after abuse of mercurial salves.
Sulphur:
- One of the leading medicines for scabies.
- Main remedy; voluptuous tingling itching in the bends of joints and between fingers, as soon as he gets warm in bed, with burning and soreness after scratching.
- Skin rough and scaly, with formation of little vesicles and pustules; glandular swellings.
- One of the most prescribed medicines for scabies is Sulphur.
- The symptoms to look out for include intense itching and scratching which worsen with washing and heat, especially during the night. The condition is characterized by unhealthy skin with pimply eruptions which are painfully sensitive to air, wind, and washing. [5]
Dulcamara:
- Scabies with red edges, painfully sensitive to touch also to cold water.
- Itching pustules which pass into suppuration also become covered with scabs.
Psorinum:
- Body of the patient has a filthy odor. Violent itching, worse from warmth of bed.
- Warmth of bed excites itching like anything, but again, on uncovering feels chilly.
- Sleepless from intolerable itching. "Inveterate cases with symptoms of tuberculosis.”
- Psorinum is another of the most prescribed medicines for scabies.
- It has shown the most remarkable results in case of unhealthy skin with an abnormal tendency to skin diseases.
- In such cases, the person complains of intolerable itching which gets worse from lying in bed.
- In fact, so severe is the itching that the person scratches until the skin starts to bleed.
- Psorinum is the best treatment option among medicines for scabies with dirty, rough, scabby, greasy skin along with violent itching.
Merc Sol:
- Fat itch, esp. in bends of elbows, when some of the vesicles become pustular.
- Itching all over, worse at night when warm in bed.
Croton Tig:
- Intense itching but the parts are so tender that the patient is practically unable to scratch.
- This itching is of a tingling character.
Lycopodium:
- Humid suppurating eruption, full of deep fissures; itching violently when becoming warm during the day.[6]
9. Causticum
- Scabies, especially in the folds of the skin and between the thighs, responds well to Causticum.
- Causticum is also one of the best medicines for scabies with intense itching and scratching in the finger webs, leading to great soreness.
- Burning, rawness and soreness are the key symptoms to look out for in scabies cases where Causticum will prove effective.
10. Sepia
- Sepia is one of the most effective medicines for scabies cases where a person complains of itching vesicles not relieved by scratching.
- The skin turns pinkish from scratching.
- The condition gets worse in the open air while the person feels better in a warm room.
- Scabies which is present mostly at the bends of the elbows and knees and where scratching does not provide any relief is also treated well with Sepia, making it a popular prescription among Homeopathic medicines for scabies.[6]
Diet & Regimen
Diet & Regimen
For Scabies
Diet
While no specific diet can cure scabies, focusing on foods that promote skin health and reduce inflammation can support healing and alleviate discomfort.
Foods to Include:
- Omega-3 Fatty Acids: Found in fatty fish (salmon, tuna, mackerel), flaxseeds, and walnuts, these healthy fats help reduce inflammation and support skin regeneration.
- Vitamin A: Essential for skin health, vitamin A is found in sweet potatoes, carrots, spinach, and kale.
- Vitamin C: A powerful antioxidant that aids in collagen production and wound healing. Citrus fruits, berries, and bell peppers are excellent sources.
- Zinc: Supports skin repair and immune function. Include zinc-rich foods like beef, pumpkin seeds, and chickpeas in your diet.
- Probiotics: Yogurt, kefir, and sauerkraut promote gut health, which can positively impact skin health.
Foods to Avoid:
- Inflammatory Foods: Processed foods, sugary drinks, and excessive saturated and trans fats can worsen inflammation.
- Allergenic Foods: If you have any known food allergies or sensitivities, avoiding these foods can help reduce skin irritation.
- Medical Treatment: The most crucial step in managing scabies is seeking professional medical advice and following the prescribed treatment plan. This typically involves topical scabicides or oral medications.
- Hygiene:
- Wash all bedding, clothing, and towels in hot water and dry them on high heat to kill mites.
- Vacuum carpets and furniture regularly.
- Avoid close physical contact with others until the infestation is cleared.
- Wash all bedding, clothing, and towels in hot water and dry them on high heat to kill mites.
- Itch Relief:
- Cool compresses and calamine lotion can soothe itchy skin.
- Oatmeal baths can provide relief.
- Over-the-counter antihistamines may help reduce itching.
- Cool compresses and calamine lotion can soothe itchy skin.
- Omega-3 Fatty Acids: Found in fatty fish (salmon, tuna, mackerel), flaxseeds, and walnuts, these healthy fats help reduce inflammation and support skin regeneration.
Do’s and Don'ts
Do’s and Don’ts
Certainly, here are the Do’s and Don’ts of Scabies:
Do’s:
- Seek Professional Help: If you suspect you have scabies, consult a doctor or dermatologist for diagnosis and proper treatment.
- Follow Treatment Instructions: Use prescribed medications exactly as directed, even if symptoms improve before completing the full course.
- Treat All Close Contacts: Ensure that everyone in close contact with the infected person, including household members and sexual partners, receives treatment simultaneously.
- Wash and Dry Items: Wash all clothing, bedding, and towels used by the infected person in hot water and dry them on high heat. Items that can’t be washed should be sealed in a plastic bag for at least 72 hours.
- Clean the Environment: Vacuum and clean surfaces in areas where the infected person has been, especially in shared spaces.
- Maintain Personal Hygiene: Wash hands frequently with soap and water, especially after contact with the infected person or their belongings.
- Inform Close Contacts: Let people you’ve had close contact with know about your scabies so they can seek treatment if necessary.
Don’ts:
- Don’t Self-Diagnose or Self-Treat: Scabies can be easily mistaken for other skin conditions. Consult a healthcare professional for proper diagnosis and treatment.
- Don’t Scratch: Scratching can worsen symptoms and increase the risk of secondary infections.
- Don’t Share Personal Items: Avoid sharing clothing, bedding, towels, or other personal items with the infected person.
- Don’t Delay Treatment: Prompt treatment can prevent complications and further spread of the infestation.
- Don’t Assume It’s Gone Too Soon: Itching may persist for some time even after successful treatment. Follow up with your doctor if symptoms persist or worsen.
Remember, scabies is a highly contagious skin condition, but with proper treatment and preventive measures, it can be effectively managed and cured.
Terminology
Terminology
Scabies:
A contagious skin infestation caused by the parasitic mite Sarcoptes scabiei.
Mite:
A tiny, eight-legged arachnid that burrows into the skin to lay eggs.
Burrows:
The tunnels created by the female mites as they lay eggs under the skin, often appearing as thin, wavy lines.
Papules:
Small, solid, raised bumps on the skin, often itchy, caused by the body’s immune response to the mites.
Nodules:
Larger, firm bumps that may persist even after treatment, often found in areas like the armpits and groin.
Vesicles:
Small, fluid-filled blisters on the skin.
Bullae:
Larger blisters, often seen in infants and young children.
Excoriations:
Scratch marks or open sores caused by intense itching.
Crusted Scabies (Norwegian Scabies):
A severe form of scabies with thick, crusted skin lesions containing a large number of mites. It’s often seen in people with weakened immune systems.
Pruritus:
Medical term for itching.
Hypersensitivity:
An exaggerated immune response to an allergen or irritant.
Secondary Infection:
A bacterial infection that occurs on top of another existing condition, often due to scratching and skin damage.
Impetigo:
A common bacterial skin infection characterized by red sores that quickly rupture, ooze, and develop a honey-colored crust.
Topical Medications:
Medications applied directly to the skin, often used to treat scabies.
Oral Medications:
Medications taken by mouth, sometimes used in severe cases of scabies or for people who cannot tolerate topical medications.
Contact Tracing:
Identifying and notifying people who may have been exposed to an infectious disease.
Incubation Period:
The time between exposure to an infection and the appearance of symptoms.
Contagious:
Easily spread from one person to another.
Zoonotic:
A disease that can be transmitted from animals to humans.
Fomite:
An inanimate object that can carry and transmit infectious agents (e.g., clothing, bedding).
Understanding these terms can help you better comprehend information about scabies and make informed decisions about prevention and treatment.
Miasm:
A fundamental concept in homeopathy referring to a predisposing disease tendency or underlying susceptibility. Scabies is often associated with the psoric miasm.
Constitutional Remedy:
A homeopathic remedy chosen based on the individual’s overall physical, mental, and emotional characteristics, aiming to treat the underlying susceptibility and promote healing.
Repertory:
A comprehensive index of homeopathic symptoms and the remedies associated with them, used to guide remedy selection.
Materia Medica:
A collection of detailed descriptions of the symptoms and characteristics associated with different homeopathic remedies.
Potency:
The degree of dilution and succussion of a homeopathic remedy, believed to influence its strength and depth of action.
Aggravation:
A temporary worsening of symptoms after taking a remedy, often considered a positive sign of healing.
Suppression:
The suppression of symptoms by conventional medications or other means, potentially leading to deeper health issues in homeopathic philosophy.
Proving:
A systematic process of observing and recording symptoms experienced by healthy individuals after taking a homeopathic remedy, used to understand the remedy’s action.
Specific Remedies for Scabies
Sulphur:
Often indicated for intense itching, burning, and skin eruptions.
Mercurius solubilis:
May be helpful for moist, itchy eruptions with a tendency to suppurate.
Psorinum:
Considered for cases with a history of suppressed skin conditions or chronic skin problems.
Causticum:
May be indicated for dry, cracked skin with intense itching, worse at night and in cold air.
Arsenicum album:
Often used for burning, restless itching with anxiety and fear.
Remember:
- Homeopathic treatment for scabies should be individualized based on the specific symptoms and characteristics of the individual.
- Consulting a qualified homeopath is essential for proper diagnosis and selection of the most appropriate remedy.
References
References use for Article Scabies
- Davidsons Principles and Practice of Medicine
- Harrison Manual of Medicine, 19e (May 22, 2016) _ (0071828524) _ (McGraw-Hill)
- Pradip Kumar Das –A Systematic review of Subjects for PG Medical Entrance Examination
- https://www.google.com/url?sa=i&url=https%3A%2F%2Fwww.uv.es%2Fderma%2FCLindex%2FCLinfest%2Fcycles001.htm&psig=AOvVaw1j9FulWwNxtFtP3qjpEbgD&ust=1651661539754000&source=images&cd=vfe&ved=0CAkQjRxqFwoTCMipye-Uw_cCFQAAAAAdAAAAABAl
- Homoeopathic Therapeutics by Lilienthal
- The Homoeopathic Prescriber by K. C. Bhanja
- https://www.medicalnewstoday.com/articles/321335
- https://en.wikipedia.org/wiki/Scabies#Differential_diagnosis
- An epidemiological study of scabies in a rural community in India, 1984
- Assessing the outbreak of scabies in a known Indian population: a prospective clinical study, 2023
- Prevalence and risk factors of scabies among school adolescents in urban Lucknow, India, 2022
- Epidemiology of Scabies, 2017,Kolkata
- Andrews’ Diseases of the Skin: Clinical Dermatology
Edition: 13th Edition
Writers: William D. James, Timothy G. Berger, Dirk M. Elston,(2020),Publication: Elsevier. - Rook’s Textbook of Dermatology
Edition: 9th Edition
Writers: Christopher Griffiths, Jonathan Barker, Tanya Bleiker, Richard Chalmers, Fiona Creamer, et al. - Fitzpatrick’s Dermatology in General Medicine
Edition: 9th Edition
Writers: Lowell A. Goldsmith, Stephen I. Katz, Barbara A. Gilchrest, Amy S. Paller, David J. Leffell, Klaus Wolff, (2019, Publication: McGraw Hill
(2016), Publication: Wiley Blackwell - Bolognia JL, Schaffer JV, Cerroni L. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018.
- Habif TP. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 7th ed. Philadelphia, PA: Elsevier; 2021.
- Wolff K, Johnson RA, Saavedra AP. Fitzpatrick’s Color Atlas and Synopsis of Clinical Dermatology. 8th ed. New York, NY: McGraw-Hill Education; 2017.
- Kumar B, Gupta S. Sexually Transmitted Infections. 6th ed. New Delhi: Elsevier India; 2018
Also Search As
Also Search As
Here are some effective ways people can search for homeopathic articles on scabies:
Specific Search Terms:
Use targeted keywords and phrases:
Add modifiers to refine the search:
Search Engines:
- Utilize major search engines like Google, DuckDuckGo, Bing, etc.
- Use advanced search options to filter by date, language, or file type (e.g., PDF).
Homeopathic Resources:
Explore online databases and journals dedicated to homeopathy:
- The National Center for Homeopathy (NCH): Offers a searchable database of articles and publications.
- Homeopathy Plus: Provides access to various homeopathic journals and articles.
- Similia: A digital library of homeopathic literature.
Check websites of homeopathic organizations and institutions:
- The American Institute of Homeopathy (AIH)
- The British Homeopathic Association (BHA)
- The Faculty of Homeopathy (UK)
Other Tips:
- Look for articles written by qualified homeopaths or published in reputable homeopathic journals.
- Pay attention to the date of publication to ensure the information is current.
- Consider using a VPN if access to certain resources is restricted in your region.
There are several ways to search for information about scabies:
Online Search Engines:
- Use major search engines like Google, Bing, DuckDuckGo, etc.
- Employ specific search terms like:
Reputable Health Websites:
Consult websites of trusted health organizations:
- World Health Organization (WHO)
- Centers for Disease Control and Prevention (CDC)
- Mayo Clinic
- National Institutes of Health (NIH)
- American Academy of Dermatology (AAD)
Look for articles, FAQs, and patient education resources on these websites.
Medical Databases:
- Access medical literature databases like PubMed or Google Scholar for research articles and clinical studies on scabies.
- Use relevant keywords and filters to refine your search.
Libraries:
- Visit your local library or university library to access medical textbooks, journals, and other resources on scabies.
- Ask a librarian for assistance in finding relevant materials.
Healthcare Professionals:
- Consult a doctor, dermatologist, or other healthcare professional for personalized information and advice on scabies.
- They can answer your specific questions, diagnose the condition, and recommend appropriate treatment options.
Additional Tips:
- When searching online, be critical of the information you find. Stick to reputable sources and avoid websites that promote unproven treatments or make exaggerated claims.
- Pay attention to the date of publication, especially for online resources, to ensure the information is current.
- Consider using a variety of search methods to gather a comprehensive understanding of scabies.
Remember, accurate information is essential for proper diagnosis and treatment of scabies. If you suspect you or someone you know has scabies, it’s important to seek professional medical advice.
Frequently Asked Questions (FAQ)
What is Scabies?
Scabies is a contagious skin Disease marked by itching and small raised red spots, caused by the itch mite.
How is scabies diagnosed?
- A doctor can diagnose scabies by examining the skin and looking for burrows or taking a skin scraping to identify the mites under a microscope.
Can scabies be prevented?
- Avoiding close contact with infected individuals is the best way to prevent scabies. Additionally, washing clothes, bedding, and towels in hot water and drying them on high heat can help kill mites.
What are the symptoms of Scabies?
Symptoms
- Intense Pruritus
- Itching Worse at night also after a hot shower.
- Burrows
- Appear as dark wavy lines that end in a pearly bleb
- Most lesions are between the fingers or on the volar wrists, elbows, and penis.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Scabies?
Homoeopathic Medicines For Scabies
- Arsenicum Alb
- Carbo veg
- Sulphur
- Dulcamara
- Psorinum
- Merc Sol
- Croton Tig
- Lycopodium
Is homeopathic treatment safe for scabies, especially for children and pregnant women?
- Homeopathic remedies are generally considered safe for all age groups, including children and pregnant women, when prescribed by a qualified practitioner.
