Septic Arthritis
Definition
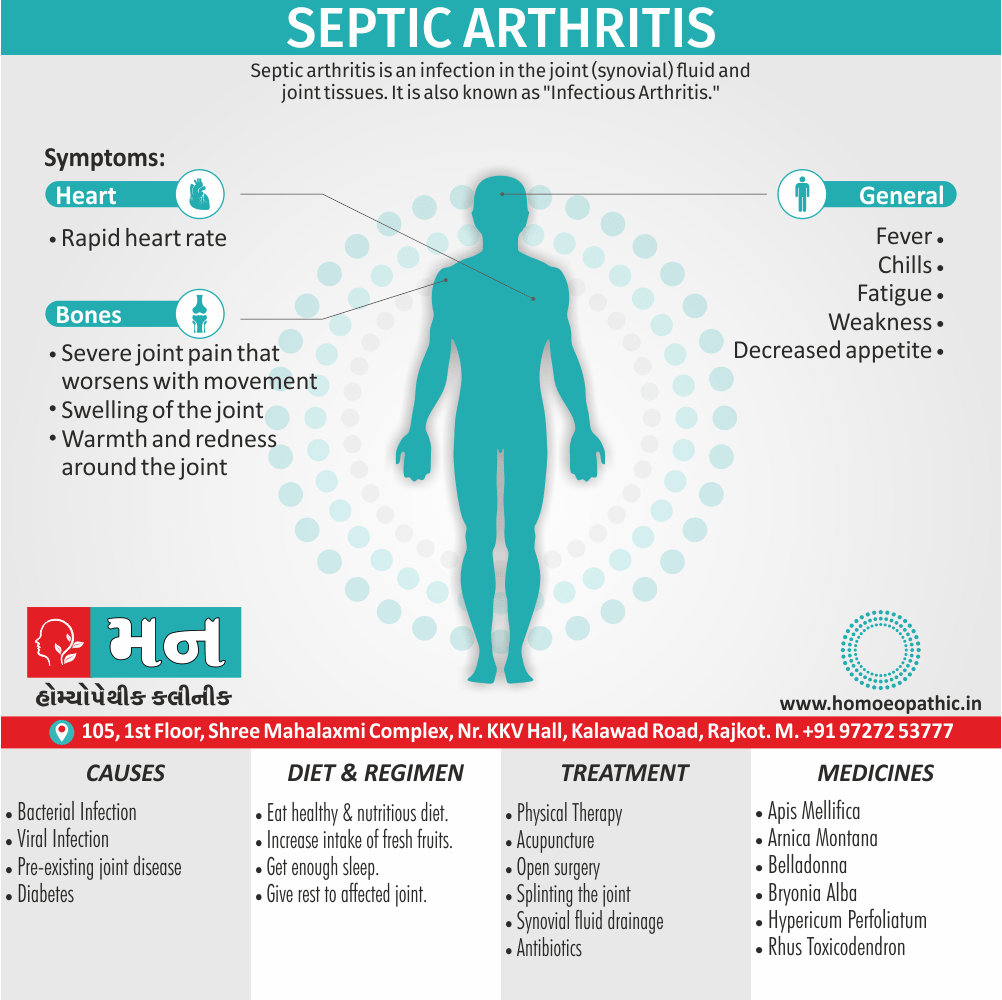
Septic arthritis is an infection in the joint (synovial) fluid and joint tissues. It is also known as “Infectious Arthritis.” [1]
Septic arthritis, also known as infectious arthritis or pyogenic arthritis, is a painful infection in a joint.
While there are no direct synonyms for septic arthritis, the following terms are often used interchangeably:
- Infectious arthritis: This broad term encompasses all forms of arthritis caused by an infection, including septic arthritis.
- Pyogenic arthritis: This term specifically refers to septic arthritis caused by bacteria that form pus.
- Bacterial arthritis: This term highlights the bacterial origin of the infection, which is the most common cause of septic arthritis.
Please note that while these terms are often used synonymously with septic arthritis, they can also refer to other types of joint infections. It’s always best to consult with a healthcare professional for an accurate diagnosis and treatment plan.
Overview
Epidemiology
Causes
Types
Joint & Bone Infections
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
Septic arthritis is the most rapid and destructive joint disease, and is associated with significant morbidity and a mortality of 10%.
This has not improved over the last 20 years, despite advances in antimicrobial therapy.
The incidence is 2–10 per 100,000 in the general population, and 30–70 per 100,000 in those with preexisting joint disease or joint replacement.
Septic arthritis is usually due to haematogenous spread from either skin or upper respiratory tract; infection from direct puncture wounds or secondary to joint aspiration is uncommon.
Risk factors include;
- Increasing age,
- Pre existing joint disease (principally RA),
- Diabetes mellitus,
- Immunosuppression (by drugs or disease),
- Intravenous drug misuse.
In RA, the skin is a frequent portal of entry because of maceration of skin between the toes due to joint deformity and difficulties with foot hygiene due to hand deformity. [1]
Infants and older adults are most likely to develop septic arthritis.
Knees are most commonly affected, but septic arthritis also can affect hips, shoulders and other joints.
The infection can quickly and severely damage the cartilage and bone within the joint, so prompt treatment is crucial. [2]
Epidemiology
Epidemiology
The epidemiology of septic arthritis in India varies depending on the population studied and the year of publication:
Adults:
- The reported incidence ranges from 4 to 12 cases per 100,000 person-years. Incidence increases with age and socioeconomic deprivation. [6]
(Epidemiology, Management, and Outcomes of Large and Small Native Joint Septic Arthritis in Adults | Clinical Infectious Diseases| Oxford Academic, 2020)
Children:
- The annual incidence of septic arthritis in children varies between 5 and 12 cases/100,000 persons. It can be as high as 5-20 cases/100,000 persons in the developing world. In India, its reported incidence is 1 per 1500 persons. [7]
(Article_3- Septic Arthritis-IJPO 2022.cdr – International Journal of Paediatric Orthopaedics, 2022)
Overall:
- The rate of septic arthritis varies from 4 to 29 cases per 100,000 persons per year, depending on underlying medical conditions and joint characteristics. [8]
(A Study on Prevalence, Complications and Management of Septic Arthritis, 2021)
Causes
Causes
Infectious arthritis is a type of arthritis that occurs when bacteria or viruses, or other organisms get into the fluid between joints and multiply.
In adults, the most likely organism is Staphylococcus aureus, particularly in patients with RA and diabetes.
In young, sexually active adults, disseminated gonococcal infection occurs in up to 3% of untreated gonorrhoea, usually presenting with migratory arthralgia, low grade fever and tenosynovitis, which may precede the development of oligo or monoarthritis.
other factors
Painful pustular skin lesions may also be present.
Amongst the older people and intravenous drug users, Gram Negative bacilli or group B, C and G streptococci are important causes.
Group A streptococci, pneumococci, meningococci and Haemophilus influenzae are occasionally isolated. [1]
Types
Types:
Septic arthritis can be broadly classified into the following types:
Nongonococcal Arthritis:
- This type accounts for over 80% of septic arthritis cases.
- The most common causative agents are Staphylococcus and Streptococcus species.
- The infection can originate from various sources, including drug abuse, cellulitis, abscesses, endocarditis, and chronic osteomyelitis.
- Methicillin-resistant Staphylococcus aureus (MRSA)is a growing concern, affecting 5 to 25% of cases.
Gonococcal Arthritis:
- Caused by Neisseria gonorrhoeae, a sexually transmitted infection.
- It can manifest as localized septic arthritis or an arthritis-dermatitis syndrome characterized by malaise, polyarthralgias, tenosynovitis, and dermatitis.
- Gonococcal arthritis can affect any joint, presenting as monoarthritis, oligoarthritis, or polyarthritis.
- It is more common in young, sexually active individuals.
Other Types:
- Less common causes of septic arthritis include fungal infections (e.g., Candida), mycobacterial infections (e.g., tuberculosis), and viral infections (e.g., parvovirus B19).
- These infections are often seen in immunocompromised individuals or those with specific risk factors.[9]
Joint & Bone Infections
Joint and bone infection in old age:
Vertebral infection i.e.:
- More common.
- Recognition may be delayed, as symptoms may be attributed to compression fractures caused by osteoporosis.
Peripheral vascular disease i.e.:
- Leads to more frequent involvement of the bones of the feet, and diabetic foot ulcers are also commonly complicated by osteomyelitis.
Prosthetic joint infections i.e.:
- Now more common because of the increased frequency of prosthetic joint insertion in older people.
Gram-negative bacilli i.e.:
- More frequent pathogens than in younger people. [1]
Risk Factors
Risk factors for septic arthritis include:
Existing joint problems i.e.:
- Chronic diseases and conditions that affect your joints such as osteoarthritis, gout, rheumatoid arthritis or lupus can increase your risk of septic arthritis, as can an artificial joint, previous joint surgery and joint injury.
Taking medications for rheumatoid arthritis i.e.:
- People with rheumatoid arthritis have a further increase in risk because of medications they take that can suppress the immune system, making infections more likely to occur.
- Diagnosing septic arthritis in people with rheumatoid arthritis is difficult because many of the signs and symptoms are similar.
Skin fragility i.e.:
- Skin that breaks easily and heals poorly can give bacteria access to your body.
- Some skin conditions such as psoriasis and eczema increase your risk of septic arthritis, as do infected skin wounds.
- People who regularly inject drugs also have a higher risk of infection at the site of injection.
Weak immune system i.e.:
- People with a weak immune system are at greater risk of septic arthritis.
- This includes people with diabetes, kidney and liver problems, and those taking drugs that suppress their immune systems.
Joint trauma i.e.:
- Animal bites, puncture wounds or cuts over a joint can put you at risk of septic arthritis.
- Having a combination of risk factors puts you at greater risk than having just one risk factor does. [2]
Pathogenesis
Pathogenesis
The pathogenesis of septic arthritis involves the following steps:
Microbial Invasion:
- The most common route of infection is hematogenous spread, where bacteria enter the bloodstream from a distant site of infection like skin, respiratory tract, or urinary tract.
- Less frequently, the infection can spread directly from adjacent tissues like osteomyelitis or through penetrating trauma.
Joint Colonization:
- Once in the bloodstream, the bacteria adhere to the synovial membrane, the lining of the joint capsule.
- The synovial membrane is highly vascularized and lacks a basement membrane, making it susceptible to bacterial colonization.
- Factors like prior joint damage or inflammation, as well as the virulence of the bacteria, can further facilitate colonization.
Inflammatory Response:
- The presence of bacteria triggers an intense inflammatory response in the joint.
- The synovial membrane becomes swollen and hyperemic, producing excessive synovial fluid with high white blood cell count.
- The release of inflammatory mediators leads to cartilage damage and bone erosion.
Joint Destruction:
- If left untreated, the ongoing inflammation can lead to irreversible joint damage.
- The articular cartilage, which provides a smooth surface for joint movement, gets degraded.The underlying bone can also be eroded, leading to joint instability and deformity. [10]
Pathophysiology
Pathophysiology
The pathophysiology of septic arthritis involves a complex interplay of host and microbial factors:
Microbial Invasion and Proliferation:
- The causative microorganism gains access to the joint space, primarily through hematogenous spread from a distant infection site.
- Once within the joint, the microbe adheres to the synovial membrane and proliferates rapidly.
- The synovial fluid, rich in nutrients and low in antimicrobial factors, provides a favorable environment for bacterial growth.
Inflammatory Cascade:
- The presence of bacteria triggers a robust inflammatory response in the synovium.
- The host immune system releases various cytokines and chemokines, attracting neutrophils and other inflammatory cells to the joint.
- Neutrophils attempt to phagocytose and kill the bacteria, but their action also contributes to tissue damage.
Synovial Membrane Changes:
- The synovial membrane undergoes significant changes due to inflammation.
- It becomes hyperemic, edematous, and infiltrated with inflammatory cells.
- The synovial lining proliferates, forming pannus tissue that can erode cartilage and bone.
Joint Effusion and Cartilage Destruction:
- The inflamed synovium produces excessive synovial fluid, leading to joint effusion and pain.
- The synovial fluid contains high levels of inflammatory mediators and proteolytic enzymes that degrade cartilage.
- The articular cartilage, which provides a smooth surface for joint movement, is progressively destroyed.
Bone Erosion and Joint Destruction:
- If left untreated, the inflammatory process can extend to the subchondral bone, leading to bone erosion.
- The loss of cartilage and bone support can result in joint instability, deformity, and functional impairment. [11]
Clinical Features
Clinical Features
The clinical presentation of septic arthritis is typically characterized by the following features:
Cardinal Symptoms:
- Acute Joint Pain: The pain is usually severe, constant, and aggravated by movement. The patient may be unable to bear weight on the affected joint.
- Joint Swelling: The joint is often swollen, warm, and tender to touch. The swelling may be accompanied by erythema (redness) and increased local temperature.
- Limited Range of Motion: The patient may have difficulty moving the affected joint due to pain and swelling.
- Fever: Fever is common, especially in cases of hematogenous spread. However, it may be absent in immunocompromised individuals.
Additional Symptoms:
- Chills: Chills may accompany fever in some cases.
- Malaise: The patient may feel generally unwell, fatigued, and have a decreased appetite.
- Systemic Symptoms: In severe cases, septic arthritis can lead to systemic symptoms like hypotension, tachycardia, and confusion.
- Specific Findings: Certain infections may have specific manifestations. For instance, gonococcal arthritis can be associated with a rash or tenosynovitis. [11]
Sign & Symptoms
Sign & Symptoms
- Severe pain that worsens with movement
- Swelling of the joint
- Warmth and redness around the joint
- Fever
- Chills
- Fatigue
- Weakness
- Decreased appetite
- Rapid heart rate
- Irritability [3]
Any joint can be affected, lower limb joints, such as the knee and hip, are commonly targeted. [1]
Clinical Examination
Clinical Examination
The clinical examination of a patient with suspected septic arthritis should focus on the affected joint and include a thorough systemic assessment:
Local Examination of the Joint:
- Inspection: Look for signs of swelling, erythema (redness), warmth, and any open wounds or skin lesions near the joint.
- Palpation: Gently palpate the joint to assess tenderness, warmth, and the presence of effusion (fluid within the joint).
- Range of Motion: Evaluate the active and passive range of motion of the joint, noting any limitations or pain with movement.
- Stability: Assess joint stability, especially in weight-bearing joints, to rule out ligamentous injury or subluxation.
Systemic Examination:
- Vital Signs: Monitor temperature, heart rate, blood pressure, and respiratory rate.
- Skin: Examine the skin for rashes, petechiae (small red spots), or any signs of infection elsewhere in the body.
- Lymph Nodes: Palpate regional lymph nodes for enlargement or tenderness.
- Cardiovascular: Auscultate the heart for murmurs, which may suggest endocarditis as a source of infection.
- Respiratory: Listen to the lungs for any signs of pneumonia or other respiratory infection.
- Abdomen: Palpate the abdomen for tenderness or organomegaly.
- Neurological: Assess neurological function to rule out any complications like spinal epidural abscess. [9]
Diagnosis
Diagnosis
Prompt diagnosis of septic arthritis is necessary to prevent permanent damage to the joint.
In addition to a complete medical history and physical examination, diagnostic procedures for septic arthritis may include:
Removal of joint fluid:
- This is done to examine for white blood cells also bacteria.
Blood tests:
- In brief, These tests are done to detect bacteria.
Phlegm, spinal fluid, and urine tests:
- These tests are done to detect bacteria also find the source of infection.
X-ray:
- A diagnostic test that uses invisible electromagnetic energy beams to produce images of internal tissues, bones, also organs onto film.
Bone scan:
- A nuclear imaging method to evaluate any degenerative and/or arthritic changes in the joints to detect bone diseases also tumors to determine the cause of bone pain or inflammation.
Magnetic resonance imaging (MRI):
- A diagnostic procedure that uses a combination of large magnets, radio frequencies, additionally a computer to produce detailed images of organs and structures within the body.
Radionuclide scans:
- Generally, Nuclear scans of various organs to determine blood flow to the organs. [4]
Differential Diagnosis
Differential Diagnosis
When evaluating a patient with acute joint pain and swelling, several conditions can mimic septic arthritis. It is crucial to consider the following differential diagnoses:
Crystal-Induced Arthritis:
- Gout and pseudogout can present with acute monoarthritis, often with intense pain and inflammation. The presence of crystals in the synovial fluid helps differentiate these conditions.
Rheumatoid Arthritis:
- Although typically a chronic polyarthritis, rheumatoid arthritis can occasionally present with acute monoarthritis or oligoarthritis. Serological tests for rheumatoid factor and anti-cyclic citrullinated peptide antibodies can aid in diagnosis.
Reactive Arthritis:
- This inflammatory arthritis often follows an infection, particularly in the gastrointestinal or genitourinary tract. It can affect multiple joints and may be accompanied by extra-articular manifestations like conjunctivitis and urethritis.
Psoriatic Arthritis:
- This inflammatory arthritis is associated with psoriasis and can affect peripheral joints, spine, and entheses (tendon insertions). Skin and nail changes typical of psoriasis can help distinguish this condition.
Lyme Arthritis:
- Caused by Borrelia burgdorferi infection, Lyme arthritis often affects large joints, particularly the knee. A history of tick bite or erythema migrans rash can suggest this diagnosis.
Viral Arthritis:
Several viruses can cause acute arthritis, including parvovirus B19, rubella, and hepatitis B. These infections are usually self-limiting and resolve without specific treatment.
Osteomyelitis:
- Infection of the bone can sometimes present with adjacent joint involvement, making it difficult to differentiate from septic arthritis. Imaging studies like MRI can help distinguish these conditions. [11]
Complications
Complications
Untreated or inadequately treated septic arthritis can lead to several serious complications
Local Complications:
- Joint Destruction: The ongoing inflammation and cartilage degradation can result in irreversible joint damage, leading to pain, stiffness, and loss of function.
- Osteomyelitis: The infection can spread from the joint to the adjacent bone, causing osteomyelitis, a serious bone infection that requires prolonged antibiotic therapy and sometimes surgery.
- Abscess Formation: An abscess, a collection of pus within the joint or surrounding tissues, may develop, requiring drainage and debridement.
- Septic Bursitis: The infection can extend to nearby bursae (fluid-filled sacs that cushion joints), causing septic bursitis.
- Joint Ankylosis: In severe cases, the joint may become fused or stiff due to fibrosis and bony overgrowth, leading to complete loss of motion.
Systemic Complications:
- Sepsis: The infection can spread throughout the body, causing sepsis, a life-threatening condition characterized by organ dysfunction.
- Endocarditis: Bacteria from the joint can seed the heart valves, leading to endocarditis, an infection of the heart’s inner lining.
- Meningitis: In rare cases, the infection can spread to the meninges (membranes surrounding the brain and spinal cord), causing meningitis.
- Death: Although rare with prompt treatment, septic arthritis can be fatal, especially in immunocompromised individuals or those with delayed diagnosis. [9]
Investigations
Investigations
The investigation of septic arthritis aims to confirm the diagnosis, identify the causative organism, and assess the extent of joint involvement. The following investigations are commonly performed:
Laboratory Investigations:
- Synovial Fluid Analysis: This is the most crucial investigation. Arthrocentesis (joint aspiration) is performed to obtain synovial fluid, which is then analyzed for:
- Appearance: Typically, the fluid is turbid or purulent in septic arthritis.
- Cell Count: The white blood cell count is markedly elevated, often exceeding 50,000 cells/µL, with a predominance of neutrophils.
- Gram Stain and Culture: These tests help identify the causative organism. Gram stain provides rapid preliminary information, while culture confirms the diagnosis and guides antibiotic therapy.
- Other Tests: Glucose and protein levels may be measured. Crystal analysis is performed to rule out crystal-induced arthritis.
Blood Tests:
- Complete Blood Count: Leukocytosis (elevated white blood cell count) is common.
- Erythrocyte Sedimentation Rate (ESR) and C-reactive Protein (CRP): These inflammatory markers are usually elevated.
- Blood Cultures: Positive blood cultures may identify the causative organism, especially in cases of hematogenous spread.
Imaging Studies:
- X-rays: Initial X-rays may show soft tissue swelling and joint effusion. Later, they may reveal joint space narrowing, cartilage destruction, and bone erosion.
- Ultrasound: Ultrasound can help visualize joint effusion and guide arthrocentesis.
- MRI: MRI provides detailed images of the joint and surrounding tissues, helping assess the extent of inflammation, cartilage damage, and bone involvement. It is particularly useful in evaluating the hip and spine.
Other Investigations:
- Additional cultures: Cultures of blood, urine, or other potential sources of infection may be obtained to identify the primary site of infection.
- Echocardiogram: An echocardiogram may be performed if endocarditis is suspected. [11]
Treatment
Treatment
A full recovery can take several weeks, but the infection should disappear entirely.
The best treatment for infectious arthritis depends on the cause.
- The patient should admit to hospital for pain relief and administration of parenteral antibiotics.
- Flucloxacillin (2 g IV 4 times daily) is the antibiotic of first choice pending the results of cultures, since it will cover most staphylococcal and streptococcal infections.
- If there is reason to suspect a Gram Negative infection, then a cephalosporin or gentamicin should add.
- Microbiology advice should sought in complicated situations such as intravenous drug users, patients in intensive care and those who might colonise by resistant organisms.
- It is traditional to continue intravenous antibiotics for 2 weeks and to follow this with oral treatment for another 4 weeks, but there is no evidence to support the optimal duration of treatment.
- Joint aspiration should perform using a large bore needle once or twice daily.
- If this is not possible, arthroscopic or open surgical drainage may need to be undertaken.
- Regular passive movement should undertake from the outset, and active movements encouraged once the condition has stabilised.
Other Treatment
- Infected prosthetic joints require management by the orthopaedic team, but often prolonged antibiotic treatment on its own is ineffective and removal of the prosthesis is required for eradication of the infection.
- Arthritis may be a feature of Lyme disease caused by members of the Borrelia species of microorganisms.
- It is generally a late manifestation, which usually affects large joints.
- Brucellosis presents with an acute febrile illness, followed in some cases by the development of localised infection, which can result in arthritis, bursitis, osteomyelitis, sacroiliitis also paravertebral or psoas abscesses.
- If bacteria are responsible for the infection, additionally doctors will usually prescribe antibiotics.
- Moreover, People should take antibiotics as early as possible to reduce the risk of permanent damage.
- People can take antibiotics as an oral treatment over several weeks.
- In detail, A full course of treatment can take up to 6–8 weeks to complete.
- Besides this, Some people may need to spend some time in the hospital to allow continuous administration of antibiotics also to drain fluids through an IV.
- This treatment can last a few either days or weeks, depending on the severity of the condition.
- All in all, If a fungus causes the infection, doctors will treat it with an antifungal medication instead of antibiotics. [1]
Other treatment methods to reduce pain may be used along with treatment for the infection.
These methods include:
- Using nonsteroidal anti-inflammatory drugs
- Resting the joint
- Splinting the affected joint
- Going to physical therapy [3]
Emergency management of suspected septic arthritis:
Admit patient to hospital i.e.: |
Perform urgent investigations
|
Commence intravenous antibiotic i.e.: |
|
Relieve pain i.e.: |
|
Aspirate joint i.e.: |
|
Arrange physiotherapy i.e.: |
|
Prevention
Prevention
Preventing septic arthritis involves a combination of strategies aimed at reducing the risk of infection and prompt management of potential sources of infection. The following preventive measures are recommended:
Prompt Treatment of Infections:
- Early and appropriate treatment of skin infections, respiratory tract infections, urinary tract infections, and other potential sources of bacteremia can reduce the risk of hematogenous spread to the joints.
Vaccination:
- Vaccination against common pathogens like Streptococcus pneumoniae and Haemophilus influenzae type b can help prevent septic arthritis caused by these organisms.
Prophylactic Antibiotics:
- In certain high-risk situations, such as prosthetic joint replacement or individuals with compromised immunity, prophylactic antibiotics may be considered before invasive procedures like dental work or surgery.
Joint Hygiene:
- Proper wound care and hygiene around joints, especially in individuals with pre-existing joint damage or arthritis, can minimize the risk of direct inoculation of bacteria into the joint.
Immunization:
- Keeping immunizations up-to-date is important, especially for those at higher risk, such as individuals with chronic diseases or weakened immune systems.
Safe Sex Practices:
- Practicing safe sex can reduce the risk of sexually transmitted infections like gonorrhea, which can lead to septic arthritis.
Early Recognition and Treatment of Joint Pain:
- Prompt medical attention for any unexplained joint pain or swelling can lead to early diagnosis and treatment of septic arthritis, minimizing the risk of complications. [9]
Homeopathic Treatment
Homoeopathic Treatment
Homeopathic treatment for septic arthritis is natural, safe and without any side-effects, and one can enjoy immense relief from these frustrating symptoms.
It is a patient-oriented science and medicines are prescribed on the characteristics of the individual rather than just the symptoms of the disease.
Apis Mellifica:
- Used for swelling of joint with synovitis also synovial effusion, septic arthritis, red hot swollen joint , pain on slightest either pressure or motion, gout , rheumatoid arthritis , post viral arthritis and arthralgia.
Arnica Montana:
- Use in blunt injury also trauma, sore unimpressive bruised sensation with swelling concussion and contusion call for this remedy.
Bryonia Alba:
- Generally, Stiffness and pain with hot swelling, redness of joints with stitching and tearing pain aggravation on least motion every spot is painful on slightest pressure.
Hypericum Perfoliatum:
- This is the remedy for degenerative changes of joints involving nerves, sciatica, coccygodynia, cervical and lumbar spondylosis with nerve compression, additionally tingling burning and numb sensation with lancinating pain calls for the remedy, darting pain of shoulders , cramps in calf muscles, pain in tips of toes also fingers, sensation of pressure along the ulnar side if arm.
Other remedies:
- Rhus Toxicodendron
- Ledum Palustre
- Bellis Perennis
- Belladonna [5]
Diet & Regimen
The Diet & Regimen
Diet:
- No specific dietary restrictions: There are no specific dietary restrictions for patients with septic arthritis.
- Focus on a healthy diet: A balanced diet rich in fruits, vegetables, and whole grains is recommended to promote overall health and support the immune system.
- Adequate hydration: Adequate fluid intake is important to maintain hydration and support joint health.
Regimen:
- Rest: The affected joint should be rested to allow for healing and reduce pain.
- Immobilization: The joint may need to be immobilized with a splint or brace to protect it and promote healing.
- Physical therapy: Physical therapy exercises may be recommended to improve range of motion and strengthen the muscles around the affected joint.
- Pain management: Pain medications may be prescribed to manage pain and discomfort.
- Antibiotics: Antibiotics are the primary treatment for septic arthritis. The specific type and duration of antibiotic therapy will depend on the type of bacteria causing the infection.
- Joint aspiration or drainage: In some cases, the infected joint may need to be aspirated (fluid removed) or drained to relieve pressure and remove infected fluid.
- Surgery: In rare cases, surgery may be necessary to drain the joint, remove infected tissue, or repair joint damage.
Do’s and Don'ts
The Do’s & Don’ts
Do’s:
Seek medical attention immediately:
- If you experience symptoms of septic arthritis, such as joint pain, swelling, redness, warmth, or fever, seek medical attention immediately. Early diagnosis and treatment are essential to prevent joint damage and other complications.
Take antibiotics as prescribed:
- Antibiotics are the primary treatment for septic arthritis. It is crucial to take the full course of antibiotics as prescribed by your doctor, even if you start to feel better.
Rest the affected joint:
- Resting the affected joint is essential to allow for healing and reduce pain. Avoid activities that put stress on the joint.
Follow your doctor’s instructions regarding immobilization:
- Your doctor may recommend immobilizing the joint with a splint or brace to protect it and promote healing.
Attend physical therapy sessions as recommended:
- Physical therapy exercises can help improve range of motion and strengthen the muscles around the affected joint.
Manage pain with prescribed medications:
- Your doctor may prescribe pain medications to manage pain and discomfort. Take them as directed.
Maintain a healthy lifestyle:
- A balanced diet, regular exercise, and adequate sleep can help support your immune system and promote healing.
Don’ts:
Delay seeking medical attention:
- Septic arthritis is a medical emergency. Delaying treatment can lead to serious complications, including joint damage, sepsis, and even death.
Stop taking antibiotics prematurely:
- Even if you start to feel better, it is essential to complete the full course of antibiotics as prescribed by your doctor. Stopping antibiotics early can lead to the infection returning or becoming resistant to treatment.
Overuse the affected joint:
- Avoid activities that put stress on the affected joint, as this can delay healing and increase the risk of complications.
Ignore pain:
- If you experience pain in the affected joint, rest it and take pain medication as prescribed. Do not try to "push through" the pain.
Neglect physical therapy:
- Physical therapy is essential for regaining range of motion and strength in the affected joint. Attend all recommended sessions and follow your therapist’s instructions.
Engage in unhealthy behaviors:
- Smoking, excessive alcohol consumption, and drug use can weaken your immune system and make it harder for your body to fight infection.
Terminology
Terminology:
Septic Arthritis:
- Meaning: Inflammation of a joint caused by a bacterial or fungal infection.
Arthritis:
- Meaning: Inflammation of one or more joints, causing pain and stiffness.
Synovial Fluid:
- Meaning: A thick liquid found in the cavities of synovial joints that reduces friction between the articular cartilage of synovial joints during movement.
Synovial Joint:
- Meaning: A freely movable joint, also known as a diarthrosis. This kind of joint has a joint cavity filled with synovial fluid.
Arthrocentesis:
- Meaning: A procedure where a needle is inserted into a joint to remove synovial fluid for examination.
Gram Stain:
- Meaning: A laboratory staining method used to differentiate bacterial species into two large groups: gram-positive bacteria and gram-negative bacteria.
Culture:
- Meaning: The process of growing microorganisms in a controlled environment, typically for the purpose of identification or study.
Antibiotics:
- Meaning: Medications that fight bacterial infections.
Joint Aspiration/Drainage:
- Meaning: The removal of fluid from a joint, often done to relieve pressure or remove infected fluid.
Immobilization:
- Meaning: Restricting movement of a joint, often with a splint or brace, to promote healing.
Physical Therapy:
- Meaning: Treatment to restore movement and function after an injury or illness, often involving exercises and stretches.
Sepsis:
- Meaning: A life-threatening condition that arises when the body’s response to an infection injures its tissues and organs.
Osteomyelitis:
- Meaning: Inflammation of bone or bone marrow, usually due to infection.
Immunocompromised:
- Meaning: Having a weakened immune system, making one more susceptible to infections.
Other terminologies :
Septic Arthritis:
- Meaning: Inflammation of a joint caused by a bacterial or fungal infection.
Arthritis:
- Meaning: Inflammation of one or more joints, leading to pain, stiffness, and swelling.
Vital Force:
- Meaning: The fundamental energy or life force that animates and sustains the body, according to homeopathic philosophy. Imbalance or disturbance of this force is believed to be the root cause of illness.
Miasm:
- Meaning: In homeopathy, a miasm refers to a predisposing, inherited weakness or susceptibility to certain types of diseases.
Totality of Symptoms:
- Meaning: The complete picture of the patient’s physical, mental, and emotional symptoms, which is considered essential for selecting the appropriate homeopathic remedy.
Similia Similibus Curentur:
- Meaning: The Latin phrase "like cures like," which is the central principle of homeopathy. It suggests that a substance that can produce symptoms in a healthy person can cure similar symptoms in a sick person.
Potentization:
- Meaning: The process of diluting and succussing (vigorously shaking) a homeopathic remedy to increase its therapeutic power while reducing its toxicity.
Repertory:
- Meaning: A reference book used by homeopaths to find remedies based on the specific symptoms presented by a patient.
Materia Medica:
- Meaning: A collection of descriptions of the therapeutic properties and symptom pictures of various homeopathic remedies.
Aggravation:
- Meaning: A temporary worsening of existing symptoms after taking a homeopathic remedy, often considered a sign that the remedy is working.
Proving:
- Meaning: A process in which healthy volunteers take a homeopathic remedy to record the symptoms it produces, helping to understand its therapeutic potential.
Constitutional Remedy:
- Meaning: A homeopathic remedy chosen based on the patient’s overall physical and mental constitution, rather than just specific symptoms.
Nosode:
- Meaning: A homeopathic remedy prepared from diseased tissue or bodily fluids.
References
Reference
- Davidson’s Principles and Practice of Medicine (22nd edition) Ch. 25
- https://www.mayoclinic.org/diseases-conditions/bone-and-joint-infections/diagnosis-treatment/drc-20350760
- https://www.healthline.com/health/septic-arthritis#treatments
- https://www.stanfordchildrens.org/en/topic/default?id=septic-infectious-arthritis-90-P01730
- https://atomictherapy.org/arthritis/
Epidemiology, Management, and Outcomes of Large and Small Native Joint Septic Arthritis in Adults Clinical Infectious Diseases Oxford Academic, 2020
- Article_3- Septic Arthritis-IJPO 2022.cdr – International Journal of Paediatric Orthopaedics, 2022
- A Study on Prevalence, Complications and Management of Septic Arthritis, 2021
- Hochberg MC, et al. Bacterial arthritis. In: Rheumatology. 7th ed. Elsevier; 2019.
- Firestein GS, et al. Infectious arthritis. In: Kelley’s Textbook of Rheumatology. 10th ed. Elsevier; 2019.
- Jameson JL, et al. Infectious arthritis. In: Harrison’s Principles of Internal Medicine. 21st ed. McGraw-Hill Education; 2022.
- Book: Kelly’s Textbook of Rheumatology
Edition: 11th Edition
Editors: Gary S. Firestein, et al.
Year of Publication: 2021
Publisher: Elsevier
Also Search As
Also Search As
People can search for homeopathic articles on septic arthritis using a variety of methods and resources:
Online Search Engines:
- Specific keywords: Use precise terms like "homeopathic treatment septic arthritis," "homeopathy for septic arthritis," or "homeopathic remedies septic arthritis" in search engines like Google, Bing, or DuckDuckGo.
- Homeopathic journals and databases: Explore online databases and journals specializing in homeopathy, such as the National Center for Homeopathy (NCH) website or the Homeopathy Research Institute (HRI) website.
- Homeopathic organizations: Check the websites of reputable homeopathic organizations like the North American Society of Homeopaths (NASH) or the European Committee for Homeopathy (ECH) for articles and resources.
Online Libraries and Databases:
- PubMed: Search for articles related to homeopathy and septic arthritis on PubMed, a database of medical literature. While it may not have many articles specifically on homeopathic treatment for septic arthritis, it can provide insights into the condition itself.
- Google Scholar: Use Google Scholar to search for scholarly articles and research papers on homeopathy and septic arthritis.
Homeopathic Practitioners and Libraries:
- Consult a homeopathic practitioner: A qualified homeopath can provide personalized recommendations and resources based on your specific needs.
- Visit a homeopathic library: Many homeopathic schools and organizations have libraries with extensive collections of books and journals.
Additional Tips:
- Use a variety of search terms: Try different combinations of keywords to broaden your search.
- Refine your search: Use filters to narrow down your results by date, publication type, or author.
- Evaluate the source: Ensure the information comes from a reliable and reputable source.
- Consult with a healthcare professional: Always discuss any homeopathic treatment with your doctor, especially for serious conditions like septic arthritis.
Important Note:
It’s important to be clear that searching for information about septic arthritis online should never replace seeking advice from a qualified medical professional. Septic arthritis is a serious condition and requires prompt diagnosis and treatment.
That being said, here are ways to search for information about septic arthritis online:
Using Search Engines:
- Specific Keywords: Start with broad terms like "septic arthritis" and then narrow down your search with more specific keywords, such as:
- "septic arthritis symptoms"
- "septic arthritis causes"
- "septic arthritis treatment"
- "septic arthritis diagnosis"
- "septic arthritis knee" (or other affected joint)
- Reliable Sources: Focus on websites from reputable organizations like:
- Mayo Clinic: mayoclinic.org
- Cleveland Clinic: my.clevelandclinic.org
- Johns Hopkins Medicine: hopkinsmedicine.org
- National Institutes of Health (NIH): nih.gov
- Centers for Disease Control and Prevention (CDC): cdc.gov
Medical Websites and Databases:
- PubMed: This is a free resource provided by the National Institutes of Health. It contains a vast database of medical literature, including research articles and clinical studies on septic arthritis.
- Google Scholar: This search engine specifically indexes scholarly literature, including articles, theses, books, and abstracts from academic publishers, professional societies, online repositories, and universities.
Online Encyclopedias and Health Portals:
- WebMD: This website provides comprehensive information about various health conditions, including septic arthritis.
- MedlinePlus: This service from the National Library of Medicine offers information about diseases, conditions, and wellness in language that is easy to understand.
Tips for Effective Searching:
- Use multiple search terms: Try different combinations of keywords to get a broader range of results.
- Refine your search: Use filters to narrow down your results by date, publication type, or source.
- Evaluate the source: Make sure the information you find is from a credible and trustworthy source. Look for websites with medical credentials, author information, and citations.
- Cross-reference information: Don’t rely on a single source. Compare information from multiple websites to ensure accuracy.
Remember, while online resources can be helpful for learning about septic arthritis, it’s crucial to consult a healthcare professional for diagnosis and treatment.
Frequently Asked Questions (FAQ)
What is Septic Arthritis?
Definition
Septic arthritis is a serious infection of a joint. It occurs when bacteria or other microorganisms invade the joint space, causing inflammation, pain, and swelling.
What are the Symptoms of Septic Arthritis?
The most common symptoms of septic arthritis are:
- Intense joint pain
- Swelling in the affected joint
- Redness and warmth over the joint
- Limited range of motion in the joint
- Fever
What Causes Septic Arthritis?
Septic arthritis is usually caused by bacteria, but it can also be caused by fungi or viruses. The bacteria can enter the joint through:
- An open wound or injury near the joint
- A bloodstream infection that spreads to the joint
- An infection in another part of the body that spreads to the joint
Who is at Risk for Septic Arthritis?
Anyone can develop septic arthritis, but certain factors can increase the risk, including:
- Older age
- Weakened immune system
- Chronic illnesses like diabetes or rheumatoid arthritis
- Recent joint surgery or injury
- Intravenous drug use
How is Septic Arthritis Diagnosed?
Septic arthritis is diagnosed based on a combination of:
- Medical history and physical exam
- Blood tests to check for signs of infection
- Joint aspiration (removal of fluid from the joint) for analysis
- Imaging tests like X-rays or MRI to rule out other conditions
Can homeopathy help with septic arthritis?
Homeopathy can be considered as a complementary therapy for septic arthritis, aiming to support the body’s natural healing process and address the underlying susceptibility to infection.
How does a homeopath choose the right remedy for septic arthritis?
A homeopath will conduct a detailed case-taking, considering the patient’s entire symptom picture, including physical, mental, and emotional symptoms, as well as modalities (factors that make symptoms better or worse). This information helps them select the most appropriate remedy.
Is it safe to use homeopathy for septic arthritis?
Yes,
Homeopathic remedies are generally considered safe when used under the guidance of a qualified homeopathic practitioner. However, it is essential to consult with your doctor before starting any new treatment, especially if you have a serious condition like septic arthritis.
Can homeopathy replace conventional medical treatment for septic arthritis?
No,
homeopathy should not be used as a replacement for conventional medical treatment for septic arthritis. Septic arthritis is a serious condition that requires prompt medical attention, including antibiotics and drainage of the infected joint. Homeopathy can be used as a complementary therapy alongside conventional treatment to support the body’s healing process and address any underlying susceptibility to infection.
What are some homeopathic remedies commonly used for septic arthritis?
Some commonly used homeopathic remedies for septic arthritis include:
- Bryonia: For joints that are hot, swollen, and painful, with stitching pains worse from motion.
- Apis mellifica: For joints that are red, swollen, and stinging, with a sensation of heat and burning.
- Rhus toxicodendron: For joints that are stiff and painful, with pain worse on initial movement but better with continued motion.
- Hepar sulph: For joints that are very sensitive to touch and cold, with sharp, splinter-like pains.
- Belladonna: For sudden, intense joint pain with redness, heat, and throbbing.
