Sexual Dysfunction in Female
Definition
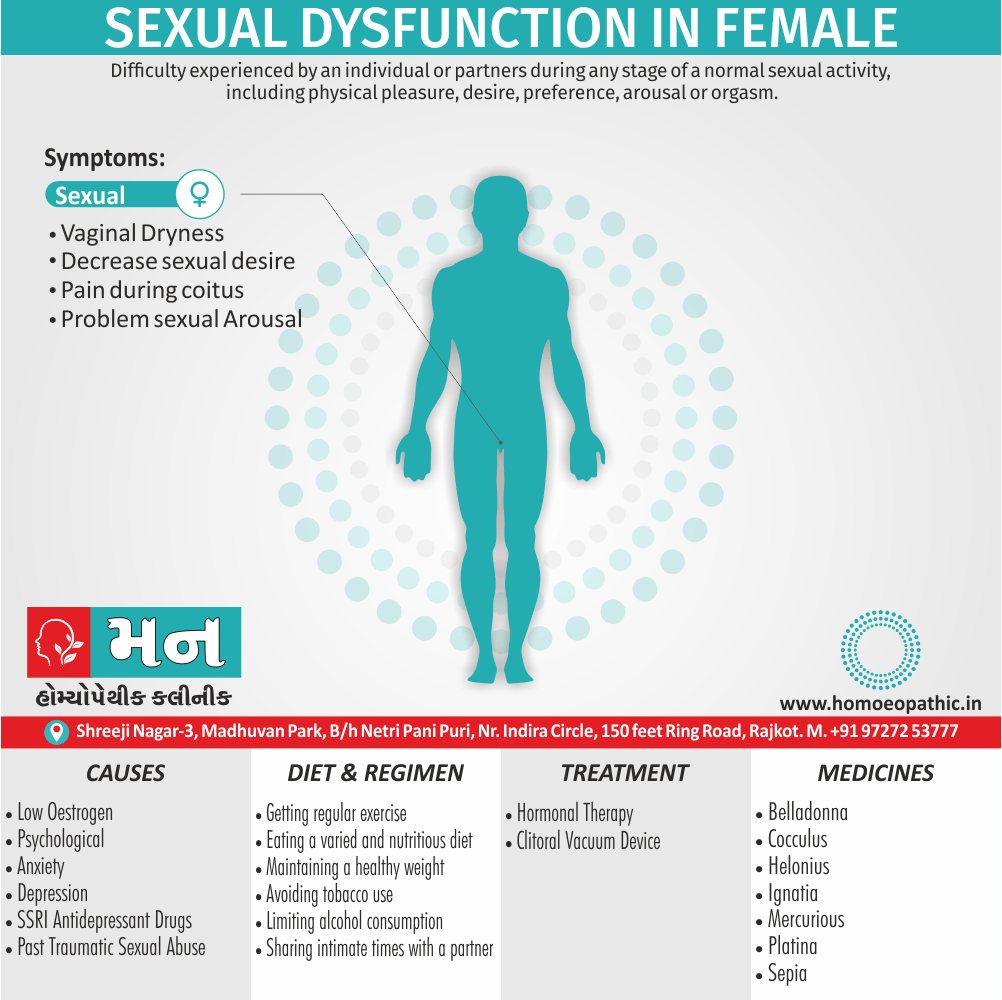
Sexual dysfunction in female is difficulty experienced by an individual or partners during any stage of a normal sexual activity, including physical pleasure, desire, preference, arousal or orgasm. The World Health Organization defines sexual dysfunction as a "person’s" inability to participate in a sexual relationship as they would wish". This definition is broad and gives way too many interpretations. Additionally, A diagnosis of sexual dysfunction under DSM-5 requires a person to feel extreme distress and interpersonal strain for a minimum of six months (except for substance- or medication-induced sexual dysfunction). Besides this, Sexual dysfunctions can have a profound impact on an individual’s perceived quality of sexual life.[1][3]
Female sexual dysfunction (FSD) can be referred to using several different terms, including:
- Female sexual arousal disorder (FSAD): This focuses on the difficulty or inability to become aroused or maintain arousal during sexual activity.
- Hypoactive sexual desire disorder (HSDD): This refers to a persistent lack of sexual thoughts, fantasies, or desire for sexual activity.
- Female orgasmic disorder (FOD): This refers to difficulty reaching orgasm, delay in reaching orgasm, or a reduced intensity of orgasm during sexual activity.
- Sexual pain disorders: This covers conditions like vaginismus (muscle spasms that make penetration painful) or dyspareunia (painful intercourse).
- Sexual dissatisfaction: This is a broader term that can encompass any dissatisfaction with sexual experiences or function.
Additionally, some more general terms might be used:
- Sexual dysfunction in women
- Sexual problems in women
- Sexual health problems in women
It’s important to note that while these terms are often used interchangeably, they might have slightly different meanings in specific medical contexts.
Please let me know if you’d like more information on any of these terms.
Overview
Physiology
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
Female sexual dysfunction (in other words, FSD) has traditionally included disorders of desire, arousal, pain, and muted orgasm. The associated risk factors for FSD are similar to those in males i.e.: cardiovascular disease, endocrine disorders, hypertension, neurologic disorders, and smoking.
Epidemiologic data are limited, but the available estimates suggest that as many as 43% of women complain of at least one sexual problem. Despite the recent interest in organic causes of FSD, desire also arousal phase disorders remain the most common presenting problems when surveyed in a community-based population.
Physiology
Physiology
The female sexual response requires the presence of estrogens. A role for androgens is also likely but less well established. In the CNS, estrogens and androgens work synergistically to enhance sexual arousal and response.
A number of studies reports enhanced libido in women during preovulatory phases of the menstrual cycle, suggesting that hormones involved in the ovulatory surge (e.g., estrogens) increase desire. Sexual motivation is heavily influenced by context, including the environment and partner factors.
Once sufficient sexual desire is reached, sexual arousal is mediated by the central and autonomic nervous systems. Cerebral sympathetic outflow is thought to increase desire, and peripheral parasympathetic activity results in clitoral Vaso congestion and vaginal secretion (lubrication).
The neurotransmitters for clitoral corporal engorgement are similar to those in the male, with a prominent role for neural, smooth-muscle, and endothelial released nitric oxide (NO).
Other Factors
A fine network of vaginal nerves and arterioles promotes a vaginal transudate. The major transmitters of this complex vaginal response are not certain, but roles for NO and Vaso intestinal polypeptide (VIP) are suspected.
Investigators studying the normal female sexual response have challenged the long-held construct of a linear and unmitigated relationship between initial desire, arousal, Vaso congestion, lubrication, and eventual orgasm.
Caregivers should consider a paradigm of a positive emotional and physical outcome with one, many, or no orgasmic peak and release.
Although there are anatomic differences as well as variation in the density of vascular and neural beds in males and females, the primary effectors of sexual response are strikingly similar. Intact sensation is important for arousal.
Thus, reduced levels of sexual functioning are more common in women with peripheral neuropathies (e.g., diabetes). Vaginal Lubrication is a transudate of serum that results from the increased pelvic blood flow associated with arousal.
Vascular insufficiency from a variety of causes may compromise adequate lubrication and result in dyspareunia. Cavernosal and arteriole smooth-muscle relaxation occurs via increased nitric oxide synthase (NOS) activity and produces engorgement in the clitoris and the surrounding vestibule.
Orgasm requires an intact sympathetic outflow tract; hence, orgasmic disorders are common in female patients with spinal cord injuries.
Epidemiology
Epidemiology
The epidemiology of female sexual dysfunction (FSD) in India reveals a significant prevalence, although estimates vary across studies due to methodological differences and diverse populations.
Key Findings:
- Prevalence: FSD estimates range from 14% to 73.2%, with a majority of studies reporting rates exceeding 50%. These variations highlight the influence of sociocultural factors, study designs, and assessment tools.
- Common Dysfunctions: Difficulties with desire, arousal, lubrication, orgasm, and satisfaction are frequently reported. Pain during intercourse (dyspareunia) is also prevalent.
- Risk Factors: Age, lower education levels, physical health issues, relationship problems, and cultural taboos have been identified as contributing factors.
- Underreporting and Help-Seeking: Despite the high prevalence, FSD remains largely underreported and undertreated due to stigma, lack of awareness, and limited access to healthcare.[5][6][7].
Causes
Causes
[1] Sexual Desire Disorder or Hypoactive sexual desire disorder
- Decreased libido is characterized by a lack of or absence for some time of sexual desire or libido for sexual activity or of sexual fantasies.
Causes:
- Decrease in the production of normal estrogen in women.
- Ageing,
- Fatigue,
- Pregnancy,
- Medications (such as the SSRIs) or psychiatric conditions, such as depression and anxiety.
[2] Sexual Arousal Disorder
- Sexual arousal disorders were previously known as frigidity in women.
- Frigidity has been replaced with a number of terms describing specific problems that can be broken down into four categories as described by the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders: lack of desire, lack of arousal, pain during intercourse, and lack of orgasm.
- For people of all genders, these conditions can manifest themselves as an aversion to and avoidance of sexual contact with a partner.
- In men, there may be partial or complete failure to attain or maintain an erection, or a lack of sexual excitement and pleasure in sexual activity.
- There may be physiological origins to these disorders, such as decreased blood flow or lack of vaginal lubrication. Chronic disease can also contribute, as well as the nature of the relationship between the partners.
[3] Orgasm Disorder
Anorgasmia
It is classified as persistent delays or absence of orgasm following a normal sexual excitement phase in at least 75% of sexual encounters. The disorder can have physical, psychological, or pharmacological origins. SSRI antidepressants are a common pharmaceutical culprit, as they can delay orgasm or eliminate it entirely. A common physiological culprit of anorgasmia is menopause; one in three women report problems obtaining an orgasm during sexual stimulation following menopause.
It is when ejaculation occurs before the partner achieves orgasm, or a mutually satisfactory length of time has passed during intercourse. There is no correct length of time for intercourse to last, but generally, premature ejaculation is thought to occur when ejaculation occurs in under two minutes from the time of the insertion of the penis. For a diagnosis, the patient must have a chronic history of premature ejaculation, poor ejaculatory control, and the problem must cause feelings of dissatisfaction as well as distress the patient, the partner or both.
- Historically attributed to psychological causes, new theories suggest that premature ejaculation may have an underlying neurobiological cause which may lead to rapid ejaculation.
- Post-orgasmic Disorder
It symptoms shortly after orgasm or ejaculation. Post-coital tristesse (PCT) is a feeling of melancholy and anxiety after sexual intercourse that lasts for up to two hours.
- POIS may involve adrenergic symptoms: rapid breathing, paranesthesia, palpitations, headaches, aphasia, nausea, itchy eyes, fever, muscle pain and weakness and fatigue.
- The etiology of this condition is unknown; but it may present as anxiety relating to coital activities and thus may be incorrectly diagnosed as such. There is no known cure or treatment.
[4] Sexual pain Disorder
Sexual pain disorders in women include dyspareunia and vaginismus .
Causes:
- Insufficient lubrication in women. Poor lubrication may result from insufficient excitement and stimulation, or from hormonal changes caused by menopause, pregnancy, or breastfeeding.
- Irritation from contraceptive creams and foams can also cause dryness, as can fear and anxiety about sex.
- It is unclear exactly what causes vaginismus, but it is thought that past sexual trauma may play a role.
- Another female sexual pain disorder is called vulvodynia or vulvar vestibuli is. In this condition, women experience burning pain during sex which seems to be related to problems with the skin in the vulvar and vaginal areas. The cause is unknown.
Types
Classification of Sexual Dysfunction in Female
It may Classified in to 4 categories i.e.
[1] Firstly, Hypoactive sexual desire disorder
[2] Secondly, Sexual Arousal Disorder
[3] Thirdly, Orgasm Disorder
[4] Fourthly, Sexual pain Disorder
Risk Factors
Risk factor of Sexual Dysfunction in Female
- Neurologic disease: stroke, spinal cord injury, parkinsonism Trauma, genital surgery, radiation
- Endocrinopathies: diabetes, hyperprolactinemia Liver and/or renal failure
- Cardiovascular disease
- Psychological factors and interpersonal relationship disorders: sexual abuse, life stressors
- Medications: Antiandrogens, Antidepressants, Antioestrogens or GnRH antagonists,Antihistamines,Antihypertensives,diuretics, Alkylating agents, Anticholinergics
Pathogenesis
Pathogenesis of Sexual Dysfunction in Females
Key Points:
The pathogenesis of female sexual dysfunction (FSD) is complex and multifactorial, involving an intricate interplay of biological, psychological, and sociocultural factors. It often involves a combination of predisposing, precipitating, and maintaining factors that contribute to the development and persistence of sexual difficulties.
Biological Factors:
- Hormonal Imbalance: Fluctuations in estrogen, testosterone, and other hormones can affect sexual desire, arousal, and orgasm. Menopause, postpartum period, and certain medical conditions can disrupt hormonal balance.
- Vascular Insufficiency: Reduced blood flow to the genitals can impair arousal and lubrication. Cardiovascular disease, diabetes, and smoking can contribute to vascular problems.
- Neurological Disorders: Conditions affecting the nervous system, such as multiple sclerosis or spinal cord injury, can interfere with sexual function.
- Medications: Certain drugs, including antidepressants, antihypertensives, and hormonal contraceptives, can have sexual side effects.
- Chronic Illnesses: Conditions like diabetes, cancer, and chronic pain can impact sexual desire and response.
- Genital Pain: Conditions like endometriosis, vulvodynia, or vaginal infections can cause pain during intercourse, leading to avoidance and decreased sexual desire.
Psychological Factors:
- Mental Health Issues: Depression, anxiety, and stress can significantly affect sexual function.
- Negative Body Image: Feeling self-conscious or dissatisfied with one’s body can lead to low self-esteem and decreased sexual desire.
- Past Trauma: Sexual abuse or other traumatic experiences can create psychological barriers to intimacy and sexual pleasure.
- Relationship Issues: Poor communication, conflict, or lack of trust in a relationship can contribute to sexual dysfunction.
- Performance Anxiety: Worrying about sexual performance can create a cycle of anxiety and decreased arousal.
Sociocultural Factors:
- Cultural and Religious Beliefs: Restrictive attitudes toward sexuality can lead to guilt, shame, and decreased sexual expression.
- Gender Inequality: In societies where women have limited power and autonomy, they may experience sexual difficulties due to lack of control over their bodies and sexual experiences.
- Lack of Education: Inadequate sex education can lead to misinformation and anxiety about sex.
Maintaining Factors:
- Avoidance: Fear of pain or negative experiences can lead to avoidance of sexual activity, perpetuating dysfunction.
- Negative Cognitions: Negative thoughts and beliefs about sex can interfere with arousal and pleasure.
- Relationship Problems: Ongoing conflict or lack of intimacy in a relationship can maintain sexual difficulties.[8]
Pathophysiology
Pathophysiology of Sexual Dysfunction in Females
Key Points:
The pathophysiology of female sexual dysfunction (FSD) involves intricate interactions between physiological and psychological processes, often influenced by contextual factors. It underscores the interconnectedness of mind and body in sexual response.
Physiological Mechanisms:
- Neuroendocrine System: Hypothalamic-pituitary-gonadal axis dysfunction can impact libido, arousal, and orgasm. Hormonal fluctuations (e.g., menopause, postpartum) disrupt neurotransmitter balance, affecting desire and response.
- Vascular System: Impaired blood flow to genital tissues hampers arousal and lubrication. Endothelial dysfunction, atherosclerosis, and microvascular disease contribute to decreased engorgement and sensitivity.
- Nervous System: Central and peripheral nervous system disruptions hinder sexual function. Spinal cord injuries, neuropathy, and neurodegenerative diseases impair sensory input, motor output, and subjective arousal.
- Genitopelvic Tissues: Atrophy, inflammation, and structural changes affect sensitivity and comfort. Menopausal changes, surgeries, and chronic conditions (e.g., lichen sclerosus) contribute to dyspareunia and decreased lubrication.
Psychological Mechanisms:
- Cognitive Processes: Negative thoughts, beliefs, and expectations surrounding sex interfere with arousal and pleasure. Anxiety, depression, and body image concerns can diminish sexual desire and inhibit orgasm.
- Emotional Regulation: Difficulty managing emotions, especially anxiety and stress, hinders sexual responsiveness. Trauma, relationship issues, and life stressors can negatively impact sexual function.
- Behavioral Patterns: Avoidance of sexual activity due to pain, fear, or negative experiences perpetuates dysfunction. Learned behaviors and negative associations can reinforce sexual difficulties.
Contextual Factors:
- Sociocultural Influences: Cultural norms, religious beliefs, and gender roles shape sexual attitudes and behaviors. Internalized stigma, restrictive norms, and lack of sexual autonomy can contribute to FSD.
- Relationship Dynamics: Communication problems, power imbalances, and emotional disconnect within a relationship affect sexual satisfaction. Intimacy and trust are essential for healthy sexual functioning.
- Medical and Psychological Comorbidities: Chronic illnesses, medications, and mental health conditions can impact sexual response. Addressing these factors is crucial for managing FSD effectively.[8]
Clinical Features
Clinical Features of Sexual Dysfunction in Females
Key Points:
Female sexual dysfunction (FSD) manifests in a variety of clinical features that can significantly impact a woman’s quality of life and intimate relationships. These features often cluster into distinct categories:
Desire Disorders:
- Hypoactive Sexual Desire Disorder (HSDD): Persistent or recurrent lack of or significantly reduced sexual interest/arousal, accompanied by distress.
- Sexual Aversion Disorder: Persistent or recurrent extreme aversion to and avoidance of all (or almost all) genital sexual contact with a sexual partner, accompanied by distress.
Arousal Disorders:
- Female Sexual Arousal Disorder (FSAD): Persistent or recurrent inability to attain, or to maintain until completion of the sexual activity, an adequate lubrication-swelling response of sexual excitement, accompanied by distress.
Orgasm Disorders:
- Female Orgasmic Disorder (FOD): Persistent or recurrent delay in, or absence of, orgasm following a normal sexual excitement phase, accompanied by distress.
Sexual Pain Disorders:
- Genito-Pelvic Pain/Penetration Disorder (GPPPD): Persistent or recurrent difficulties with one or more of the following: vaginal penetration during intercourse, marked vulvovaginal or pelvic pain during vaginal intercourse or penetration attempts, marked fear or anxiety about vulvovaginal or pelvic pain in anticipation of, during, or as a result of vaginal penetration, marked tensing or tightening of the pelvic floor muscles during attempted vaginal penetration.
Additional Features:
- Decreased Sexual Satisfaction: Dissatisfaction with the frequency, quality, or overall experience of sexual activity.
- Reduced Sexual Frequency: Reduced initiation of or receptivity to sexual activity.
- Difficulty Communicating Sexual Needs: Difficulty expressing sexual desires or concerns to a partner.
- Emotional Distress: Feelings of frustration, anxiety, guilt, or shame related to sexual difficulties.
- Relationship Problems: Sexual dysfunction can strain intimate relationships, leading to conflict, decreased intimacy, and emotional distance.
- Impact on Quality of Life: FSD can negatively affect self-esteem, body image, and overall well-being.[8]
Sign & Symptoms
Signs & Symptoms of Sexual Dysfunction in Females
Key Points:
The signs and symptoms of female sexual dysfunction (FSD) can vary widely and often overlap, reflecting the complex nature of this condition. However, some common indicators include:
Desire Disorders:
- Lack of sexual interest or desire: Reduced or absent thoughts, fantasies, or urges for sexual activity.
- Aversion to sexual activity: Avoidance of sexual encounters, including physical intimacy and genital contact.
- Difficulty initiating sexual activity: Feeling hesitant or reluctant to engage in sexual interactions.
Arousal Disorders:
- Difficulty getting or staying aroused: Inability to become physically or mentally excited during sexual activity.
- Lack of vaginal lubrication or swelling: Insufficient natural lubrication, leading to discomfort or pain during intercourse.
- Reduced sensation in the genitals: Decreased sensitivity or numbness in the clitoris, vulva, or vagina.
Orgasm Disorders:
- Delayed or absent orgasm: Difficulty reaching orgasm or experiencing a significantly reduced intensity of orgasm.
- Infrequent or never experiencing orgasm: Rarely or never experiencing orgasm, even with adequate stimulation.
Sexual Pain Disorders:
- Pain during intercourse (dyspareunia): Discomfort or pain in the vulva, vagina, or pelvis during penetration or thrusting.
- Painful muscle spasms (vaginismus): Involuntary contractions of the pelvic floor muscles, making penetration difficult or impossible.
- Burning or stinging sensation in the genitals: Discomfort or pain in the vulva or vagina, even without sexual activity.
Additional Signs & Symptoms:
- Decreased sexual satisfaction: Feeling unfulfilled or dissatisfied with sexual experiences.
- Anxiety or fear related to sex: Experiencing worry, tension, or apprehension about sexual encounters.
- Negative body image: Feeling self-conscious or uncomfortable about one’s physical appearance during sexual activity.
- Difficulty communicating sexual needs: Struggling to express desires or concerns to a partner.[8]
Clinical Examination
Clinical Examination of Sexual Dysfunction in Females
Key Points:
A comprehensive clinical examination is crucial for accurate diagnosis and effective management of female sexual dysfunction (FSD). It involves a combination of physical, psychological, and relational assessments to identify underlying causes and contributing factors.
Physical Examination:
- General Physical Examination: Assess overall health, including cardiovascular, endocrine, and neurological systems.
- Pelvic Examination: Evaluate for signs of atrophy, inflammation, infection, or structural abnormalities.
- External genitalia: Inspect for lesions, irritation, or signs of trauma.
- Internal genitalia: Perform a speculum examination to assess vaginal health and a bimanual examination to assess the uterus and ovaries.
- Pelvic floor muscles: Evaluate for muscle tone, tenderness, or trigger points.
Psychological Assessment:
- Detailed Sexual History: Inquire about sexual concerns, symptoms, onset, duration, and impact on quality of life.
- Psychosocial History: Explore relationship dynamics, emotional well-being, past trauma, and cultural or religious beliefs that may influence sexual function.
- Mental Health Screening: Assess for anxiety, depression, or other psychological conditions that may contribute to sexual difficulties.
Relational Assessment:
- Partner Involvement (if applicable): If the patient is in a relationship, consider involving the partner in the assessment to understand their perspective and identify any relational factors contributing to FSD.
Additional Considerations:
- Laboratory Tests: May include hormonal assays, blood glucose, and lipid profile to rule out underlying medical conditions.
- Specialized Tests: May include pelvic floor muscle function testing or vaginal sensory testing in specific cases.
Importance of Sensitivity and Empathy:
- Create a safe and comfortable environment for the patient to discuss sensitive topics.
- Use open-ended questions and active listening to encourage communication.
- Validate the patient’s concerns and avoid judgment or assumptions.[8]
Diagnosis
Diagnosis of Sexual Dysfunction in Female
- History medical, surgical, obstetric, psychological, gynecologic, sexual, and social information. Past experiences, intimacy, knowledge, and partner availability should also be ascertained.
- Medical disorders that may affect sexual health should be delineated. They include diabetes, cardiovascular disease, gynecologic conditions, obstetric history, depression, anxiety disorders, and neurologic disease.
- Medications should be reviewed as they may affect arousal, libido, and orgasm.
- The need for counselling and recognizing life stresses should be identified.
- The physical examination should Assess the genitalia, including the clitoris, Pelvic floor examination may identify prolapse or other disorders.
- Laboratory studies are needed, especially if menopausal status is uncertain. Estradiol, follicle-stimulating hormone (FSH), and luteinizing hormone (LH) are usually obtained, and dehydroepiandrosterone (DHEA) should be considered as it reflects adrenal androgen secretion.
- Liver function assessment, and Lipid studies may be useful, if not otherwise obtained. Complicated diagnostic Evaluations such as clitoral Doppler Ultrasonography and biothesiometry require expensive equipment and are of uncertain utility. It is Important for the patient to identify which symptoms Are most distressing.
- The Evaluation of FSD previously occurred mainly in a psychosocial context. However, inconsistencies between diagnostic categories based only on psychosocial Considerations and the emerging Recognition of organic.
Differential Diagnosis
Differential Diagnosis of Sexual Dysfunction in Females
Key Points:
Accurate diagnosis of female sexual dysfunction (FSD) requires careful consideration of various differential diagnoses that may mimic or contribute to sexual difficulties. These include:
Medical Conditions:
- Endocrine disorders:
- Hypothyroidism, hyperthyroidism, diabetes mellitus, hyperprolactinemia
- Cardiovascular diseases:
- Hypertension, coronary artery disease, peripheral vascular disease
- Neurological disorders:
- Multiple sclerosis, Parkinson’s disease, spinal cord injury
- Chronic pain conditions:
- Fibromyalgia, arthritis, chronic pelvic pain
- Genitourinary conditions:
- Lichen sclerosus, vulvodynia, endometriosis, pelvic organ prolapse, urinary incontinence
- Medications:
- Antidepressants, antipsychotics, antihypertensives, hormonal contraceptives
Psychological Conditions:
- Mood disorders:
- Major depressive disorder, bipolar disorder
- Anxiety disorders:
- Generalized anxiety disorder, panic disorder, social anxiety disorder
- Trauma-related disorders:
- Post-traumatic stress disorder (PTSD)
- Body image concerns:
- Eating disorders, body dysmorphic disorder
Relationship Factors:
- Poor communication:
- Difficulty expressing needs and desires to a partner
- Conflict or lack of intimacy:
- Unresolved issues or emotional distance in the relationship
- Discrepancy in sexual desire:
- Mismatched levels of sexual interest between partners
Sociocultural Factors:
- Cultural or religious beliefs:
- Restrictive attitudes toward sexuality
- Negative sexual experiences:
- History of sexual abuse or trauma
- Lack of sexual knowledge or education:
- Misconceptions or anxiety about sex
Substance Use:
- Alcohol or drug abuse:
- Can impair sexual function and contribute to relationship problems
Age-Related Changes:
- Menopause:
- Hormonal fluctuations and physical changes can affect sexual function.[8]
Complications
Complications of Sexual Dysfunction in Females
Key Points:
Untreated or poorly managed female sexual dysfunction (FSD) can lead to various complications that affect a woman’s overall well-being and quality of life. These complications can be physical, psychological, and relational.
Physical Complications:
- Chronic Pain: Persistent pain during intercourse (dyspareunia) can lead to increased muscle tension, inflammation, and further discomfort.
- Pelvic Floor Dysfunction: Vaginismus, characterized by involuntary muscle spasms, can worsen if not addressed, leading to chronic pain and difficulty with gynecological examinations or tampon insertion.
- Sexual Avoidance: Fear of pain or negative experiences can lead to avoidance of sexual activity, perpetuating dysfunction and potentially causing further physical discomfort due to lack of use.
Psychological Complications:
- Decreased Self-Esteem: Sexual difficulties can lead to feelings of inadequacy, shame, and low self-worth.
- Anxiety and Depression: Frustration, guilt, and the inability to enjoy sexual intimacy can contribute to the development or exacerbation of anxiety and depression.
- Relationship Problems: FSD can strain intimate relationships, leading to communication breakdowns, decreased intimacy, and potential infidelity or separation.
Relational Complications:
- Reduced Intimacy: Lack of sexual satisfaction can create emotional distance between partners, leading to decreased overall intimacy and connection.
- Communication Difficulties: FSD can make it challenging for couples to discuss their sexual needs and concerns openly, hindering problem-solving and mutual understanding.
- Conflict and Resentment: Unresolved sexual issues can breed frustration, resentment, and conflict within the relationship.
Impact on Quality of Life:
- Reduced Overall Well-being: FSD can significantly diminish a woman’s overall quality of life, affecting her happiness, self-confidence, and sense of fulfillment.
- Social Isolation: Shame and embarrassment about sexual difficulties can lead to social withdrawal and avoidance of intimate situations.
- Decreased Productivity: Emotional distress and relationship problems associated with FSD can impact work performance and daily functioning.[8]
Investigations
Investigation of Sexual Dysfunction in Female
- Serum Prolactin
- Serum Oestrogen
- Gonadotropins
- CBC
- Blood sugar level
- Lipid Profile
- Thyroid profile
Treatment
Treatment of Sexual Dysfunction in Female
GENERAL
- An open discussion with the patient is important as couples may need to educate about normal anatomy and physiologic responses, including the role of orgasm, in sexual encounters.
- Physiologic changes associated with aging and/or disease should explain. Couples may need to remind that clitoral stimulation rather than coital intromission may more beneficial. Behavioral modification and nonpharmacologic therapies should be a first step.
- Patient and partner counselling may improve communication and relationship strains. Lifestyle changes involving known risk factors can an important part of the treatment process.
- Emphasis on maximizing physical health and avoiding lifestyles (e.g., smoking, alcohol abuse) and medications likely to produce FSD is important.
- The use of topical lubricants may address complaints of dyspareunia and dryness. Contributing medications such as antidepressants may need to be altered, including the use of medications with less impact on sexual function, dose reduction, medication switching, or drug holidays.
HORMONAL THERAPY
- In postmenopausal women, estrogen replacement therapy may be helpful in treating vaginal atrophy, decreasing coital pain, and improving clitoral sensitivity.
- Estrogen replacement in the form of local cream is the preferred method, as it avoids systemic side effects.
- Androgen levels in women decline substantially before menopause.
- However, low levels of testosterone or DHEA are not effective predictors of a positive therapeutic outcome with androgen therapy.
- The widespread use of exogenous androgens is not supported by the literature except in select circumstances and in secondary arousal disorders.
ORAL AGENTS
- The efficacy of PDE-5i in FSD has been a marked disappointment in light of the proposed role of nitric oxide–dependent physiology in the normal female sexual response.
- The use of PDE-5i for FSD should be discouraged pending proof that it is effective.
CLITORAL VACUUM DEVICE
- In patients with arousal and orgasmic difficulties, the option of using a clitoral vacuum device may be explored.
- This handheld battery-operated device has a small soft plastic cup that applies a vacuum over the stimulated clitoris.
- This causes increased cavernosal blood flow, engorgement, and vaginal lubrication.
Prevention
Prevention of Sexual Dysfunction in Females:
- Regular Exercise: Engaging in regular physical activity can help improve cardiovascular health, increase blood flow, and enhance overall well-being, contributing to healthy sexual function.[9]
Stress Management: Effective stress management techniques, such as mindfulness meditation, yoga, or deep breathing exercises, can help reduce anxiety and tension, promoting sexual well-being.[10]
Open Communication: Maintaining open and honest communication with your partner about your sexual needs, desires, and concerns can foster intimacy and enhance sexual satisfaction.[11]
- Healthy Lifestyle Choices: Adopting a healthy lifestyle, including a balanced diet, adequate sleep, and avoiding smoking and excessive alcohol consumption, can support overall health and contribute to sexual well-being.[12]
Homeopathic Treatment
Homeopathic Treatment of Sexual Dysfunction in Female
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Sexual Dysfunction in Female:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Medicines:
SEPIA:
- It is a good remedy for FSD.
- Sepia woman is highly irritable, sensitive, and angry, easily offended and miserable due to weak uterine problems.
- Low sex drive is due to the relaxation of pelvic muscles, and there is a bearing down sensation as if everything would escape through the vagina.
- Aversion to coition due to prolapsed of uterus and vagina wall.
- Frigidity from childbirth after weaning or hormone pills.
- Nausea and irritability on thought of sex.
- Great weakness after sex. Aversion to whom she loved best and other family members.
AGNUS CASTUS:
- Sexual desire almost absent.
- Sexual thrill absent due to excessive masturbation.
- Aversion to sex.
- Relaxation of genitals with leucorrhoea.
- Great sadness, depression and sexual melancholy.
- Diminished sexual desire with complete prostration and general debility.
BERBERIS VULGARIS:
- Berberis vulgaris is suitable to listless, apathetic also indifferent woman.
- Sexual desire absent due to pain during coition.
- Cutting, stitching pains during coition. In detail, Vaginismus.
- Vagina very sensitive, pinching constriction in mons veneris, contraction also tenderness of vagina.
- Burning and soreness in vagina after intercourse.
- Enjoyment absents during sex. Besides this, Great prostration after sex.
- Neuralgia of ovaries and vagina are other factors for low sex drive.
ONOSMODIUM:
- Onosmodium is another effective medicine for low sex drive in woman.
- Sexual desire completely absent due to uterine pain and bearing down pains.
- Soreness of ovaries with rectum.
- The woman has low power of concentration and co-ordination.
- She has early and prolonged menses, Great prostration, weak, timid. Often suffers from migraine headache.
- Sexual neurasthenia, weariness, tiredness in legs.
STAPHYSAGRIA:
- Aversion to sex due to past history of rape or sexual abuse.
- Vaginismus, vagina is very sensitive to touch.
- Ovarian pain, going into thighs, worse pressure or sex.
- Prolapse with sinking feeling in the abdomen.
- Staphysagria patient often prefers solitude.
- Frequent urinary infection, which is worse from intercourse.
IGNATIA MARA :
- Best indicated medicine in FSD.
- Sexual desire absent, especially in vehement woman.
- They are moody, emotional, sensitive and easily excited.
- Aversion to sex due to vaginismus, vagina very sensitive.
- Intense pain at the entrance of vagina during coition with burning heat.
- Sexual desire absents after grief, shock, disappointment, frustration, and worry. Patient is worse after coition.
HELONIU
- Tendency to inflammation of vulva also vagina, with formation of pus.
- Persistent itching of genitals either with or without formation of blisters or sores.
- Foul smelling leucorrhea.
PLATINA
- Nervous, spasmodic women; great tenderness of vulva.
- Nymphomania. Additionally, Excessive sexual development.
- Pruritus vulvae. Ovaritis with sterility.
- Abnormal sexual appetite also melancholia
Diet & Regimen
Diet & Regimen
For Sexual Dysfunction in Female
Diet:
Importance: A balanced diet contributes to hormonal balance, healthy blood flow, and overall well-being, all essential for sexual function.
Focus on:
Phytoestrogen-rich foods: These plant compounds can mimic the effects of estrogen in the body, potentially helping with vaginal dryness and low libido. Good sources include soybeans, tofu, tempeh, flaxseeds, and sesame seeds.
Iron-rich foods: Iron is crucial for energy levels and red blood cell production, which can impact sexual desire and arousal. Include lean red meat, poultry, beans, lentils, spinach, and fortified cereals in your diet.
Foods high in omega-3 fatty acids: These healthy fats support cardiovascular health and may improve mood, which can positively influence sexual function. Good sources include fatty fish (salmon, tuna, mackerel), flaxseeds, chia seeds, and walnuts.
Limit:
Sugar and refined carbohydrates: These can lead to energy crashes, mood swings, and weight gain, which can negatively impact libido and sexual function.
Excessive alcohol: Can interfere with arousal and lubrication.
Regimen:
Pelvic floor exercises: Strengthening the pelvic floor muscles can improve blood flow to the genitals and enhance sensation. Kegel exercises are a common recommendation.
Mind-body practices: Yoga, tai chi, and meditation can help reduce stress, improve body awareness, and increase mindfulness, all of which can benefit sexual function.
Hormone therapy: If hormonal imbalances are contributing to sexual dysfunction, hormone therapy may be an option. Consult with your doctor to discuss the risks and benefits.
Cognitive behavioral therapy (CBT): Can help address negative thoughts and beliefs that may be contributing to sexual difficulties.
Relationship counseling: If relationship issues are playing a role, couples therapy can help improve communication and intimacy.
Important considerations:
Menopause: Hormonal changes during menopause can significantly impact sexual function. Discuss hormone replacement therapy (HRT) or other options with your doctor.
Underlying medical conditions: Conditions like diabetes, heart disease, and depression can contribute to sexual dysfunction. Managing these conditions is essential.
Medications: Certain medications can have side effects that affect sexual function. Talk to your doctor about possible alternatives
Do’s and Don'ts
Do’s & Don’ts
Sexual Dysfunction in Female do’s & don’ts
Do’s:
- Seek professional help: If you experience persistent or distressing sexual difficulties, consult a healthcare professional or a qualified sex therapist. They can provide accurate diagnosis, personalized treatment options, and support.
- Communicate openly with your partner: Talk to your partner about your concerns, desires, and needs. Open communication can help foster understanding, intimacy, and mutual support.
- Practice self-care: Prioritize stress management, healthy eating, regular exercise, and adequate sleep. Taking care of your physical and emotional well-being contributes to healthy sexual function.
- Explore different forms of intimacy: Intimacy is not just about sexual intercourse. Explore other ways to connect with your partner, such as cuddling, kissing, or sensual touch.
- Be patient and understanding: Addressing sexual dysfunction can take time and effort. Be patient with yourself and your partner, and remember that setbacks are normal.
Don’ts:
- Ignore the problem: Avoiding or denying sexual difficulties can worsen the issue and strain your relationship.
- Self-blame or feel shame: Sexual dysfunction is common and treatable. It’s not your fault, and there’s no need to feel ashamed.
- Rely on quick fixes or unproven remedies: Avoid self-medicating or using untested products without professional guidance.
- Compare yourself to others: Everyone’s sexual experience is unique. Avoid comparing yourself to others or unrealistic expectations.
- Give up on intimacy: Even if you’re experiencing sexual difficulties, maintain emotional and physical connection with your partner.
Remember:
- Every woman is different: What works for one person may not work for another.
- Professional guidance is key: Consult a healthcare professional for personalized advice and support.
- Open communication and patience are essential: Talk to your partner and be patient with yourself during the process.
Terminology
Terminologies
- Sexual Dysfunction: A persistent or recurrent problem that causes distress or impairs a person’s ability to enjoy sexual activity. In females, it can manifest in various ways, including:
- Low Sexual Desire/Interest: Lack of interest in sex or a decreased frequency of sexual thoughts or fantasies.
- Sexual Arousal Disorder: Difficulty becoming aroused or maintaining arousal during sexual activity, which might include insufficient lubrication or lack of sensation.
- Orgasmic Disorder: Difficulty achieving orgasm or a significant delay or absence of orgasm despite adequate sexual stimulation.
- Sexual Pain Disorder: Pain during intercourse (dyspareunia) or involuntary muscle contractions that make penetration painful or impossible (vaginismus).
Libido: A person’s overall sexual drive or desire.
- Hypoactive Sexual Desire Disorder (HSDD): A specific type of sexual dysfunction characterized by a persistent or recurrent lack of sexual fantasies or desire for sexual activity.
Female Sexual Arousal Disorder (FSAD): A persistent or recurrent inability to attain or maintain adequate lubrication-swelling response of sexual excitement until the completion of sexual activity.
Anorgasmia: The persistent or recurrent difficulty or inability to achieve orgasm after sufficient sexual stimulation and arousal.
Other Terminologies
Dyspareunia: Painful sexual intercourse, which can occur in the vulva, vagina, or deeper within the pelvis.
Vaginismus: Involuntary muscle spasms in the muscles surrounding the vagina that make penetration painful or impossible.
Hormones: Chemical messengers that regulate various bodily functions, including sexual desire and response. Estrogen, progesterone, and testosterone play crucial roles in female sexual health.
Menopause: The natural cessation of menstruation, typically occurring around age 50, which can lead to hormonal changes and potentially impact sexual function.
Pelvic Floor Muscles: The group of muscles that support the pelvic organs, including the bladder, uterus, and rectum. Weakness or dysfunction in these muscles can contribute to sexual difficulties.
Psychological Factors: Mental and emotional factors that can influence sexual function, including stress, anxiety, depression, relationship problems, and past trauma.
Body Image: A person’s perception of their physical appearance, which can impact their sexual confidence and satisfaction.
Sex Therapy: A specialized form of therapy that addresses sexual difficulties and helps individuals and couples improve their sexual communication, intimacy, and satisfaction.
Additionally, a homeopathic article on sexual dysfunction in females might include specific terms related to female reproductive health and sexual function, such as:
- Dysmenorrhea: Painful menstruation.
- Amenorrhea: Absence of menstruation.
- Menopause: The natural cessation of menstruation.
- Libido: Sexual desire.
- Anorgasmia: Inability to achieve orgasm.
- Vaginismus: Painful muscle spasms in the vagina.
References
References
- Harrisons_Principles_of_Internal_Medicine-_19th_Edition-_2_Volume_Set
- Homoeopathic Therapeutics by Lilienthal
- https://www.healthline.com/health/erectile-dysfunction/foods-diet#cocoa
- https://www.rajeevclinic.com/disease/gynaecology
- Prevalence and risk factors for female sexual dysfunction in women attending a medical clinic in South India. Latha KS, Bhat PS, Kotian MS, Kamath A. J Sex Med. 2010 May;7(5):1767-75. doi: 10.1111/j.1743-6109.2009.01710.x. Epub 2010 Feb 1.
- Female Sexual Dysfunction: Indian Perspective and Role of Indian Gynecologists. Shaveta Jain, Rekha Sachan, Archana Rani, and Shashi Alok. Journal of Mid-life Health. 2020 Jul-Sep; 11(3): 108–112. doi: 10.4103/jmh.JMH_70_19
- Development of Hindi-Translated Version of the Female Sexual Function Index for Evaluating Sexual Dysfunctions among Individuals with Anxiety, Depression, and Other Common Mental Health Conditions: Experiential Account and Preliminary Findings from India. Kumar, N; Vohra, A; Sharma, N; Prakash, O; Singh, TB; Grov er, S. Journal of Clinical Medicine. 2023; 12(14):4623.
- Textbook of Female Sexual Function and Dysfunction: Diagnosis and Treatment, Irwin Goldstein, Cindy M. Meston, Andrew T. Goldstein, Lori A. Brotto, 2nd Edition, 2023, Wiley-Blackwell.
The Female Brain, 2nd Edition, Louann Brizendine, M.D., 2017, Harmony Books.
Come As You Are: The Surprising New Science That Will Transform Your Sex Life, 1st Edition, Emily Nagoski, Ph.D., 2015, Simon & Schuster.
Mating in Captivity: Unlocking Erotic Intelligence,1st Edition, Esther Perel, 2006, Harper.
Our Bodies, Ourselves, 9th Edition, The Boston Women’s Health Book Collective, 2011,Touchstone.
Also Search As
Also search as
1. Online Search Engines:
- Specific Keywords: Use search terms such as "homeopathy for female sexual dysfunction," "homeopathic remedies for low libido," "homeopathic treatment for anorgasmia," or "homeopathy for vaginismus."
- Combining Keywords: Combine general terms like "homeopathy" or "homeopathic medicine" with specific symptoms or conditions like "low sexual desire," "painful intercourse," or "difficulty achieving orgasm."
- Reputable Sources: Focus on websites of homeopathic organizations, professional homeopaths, or reputable health information platforms to ensure reliable information.
2. Homeopathic Resources:
- Homeopathic Libraries: Visit libraries that specialize in homeopathy or alternative medicine for books and journals on the topic.
- Homeopathic Organizations: Check the websites and publications of national or international homeopathic organizations for articles and resources.
- Homeopathic Practitioners: Consult with a qualified homeopathic practitioner who can provide information and guidance on relevant literature.
3. Academic Databases:
- Search Engines: Use academic search engines like PubMed, Google Scholar, or ScienceDirect to find peer-reviewed research articles on homeopathy and female sexual dysfunction.
- Keywords: Use keywords like "homeopathy," "female sexual dysfunction," "clinical trials," or specific homeopathic remedies.
- Filters: Filter search results by publication date, language, or article type to find the most relevant and up-to-date information.
4. Social Media & Online Communities:
- Homeopathic Groups: Join online groups or forums dedicated to homeopathy or women’s health to connect with individuals who have experience with homeopathic treatment for sexual dysfunction.
- Social Media Hashtags: Follow relevant hashtags on social media platforms to discover articles, discussions, and insights related to homeopathy and female sexual health.
Additional Tips:
- Specify the type of sexual dysfunction: If you are looking for information about a specific issue, include it in your search terms (e.g., "homeopathy for low libido after menopause").
- Consider the source’s credibility: Be critical of the information you find online and assess the credibility of the source before relying on it.
- Consult a professional: If you’re considering homeopathic treatment, consult with a qualified homeopathic practitioner for personalized advice and guidance.
Frequently Asked Questions (FAQ)
What is Sexual Dysfunction in Female?
Definition
The World Health Organization defines sexual dysfunction as a "person’s" inability to participate in a sexual relationship as they would wish".
How common is sexual dysfunction in females?
Sexual dysfunction is quite common, with estimates suggesting that up to 43% of women experience some form of sexual difficulty at some point in their lives.
What are the types of Sexual Dysfunction in Female?
Types
- Sexual Desire Disorder
- Orgasm Disorder
- Sexual pain Disorder
What are the signs and symptoms of sexual dysfunction?
Sign & Symptoms
- Lack of interest in sex
- Difficulty getting aroused or maintaining arousal
- Inability to achieve orgasm
- Pain during intercourse
- Vaginal dryness
What causes Sexual Dysfunction in Female?
Causes
- Decrease in the production of normal estrogen in women.
- Ageing
- Fatigue
- Pregnancy
- Medications
- Psychiatric conditions (depression and anxiety)
How is sexual dysfunction in females diagnosed?
Diagnosis typically involves a comprehensive evaluation that includes:
- Detailed medical and sexual history
- Physical examination
- Psychological assessment
- Laboratory tests
Can homeopathy help with female sexual dysfunction?
Yes, homeopathy offers a holistic approach to address female sexual dysfunction by considering the individual’s unique physical, mental, and emotional symptoms. Homeopathic remedies aim to stimulate the body’s self-healing abilities and restore balance, which can improve sexual function.
Are homeopathic remedies safe for female sexual dysfunction?
Homeopathic remedies are generally considered safe when prescribed by a qualified practitioner.They are prepared from natural substances and undergo extensive dilution and potentization, making them non-toxic and suitable for most individuals.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Sexual Dysfunction in Female?
Homoeopathic Medicines for Sexual dysfunction in females
- Sepia
- Agnus Castus
- Berberis Vulgaris
- Onosmodium
- Staphysagria
- Ignatia Amara
