Snoring
Definition:
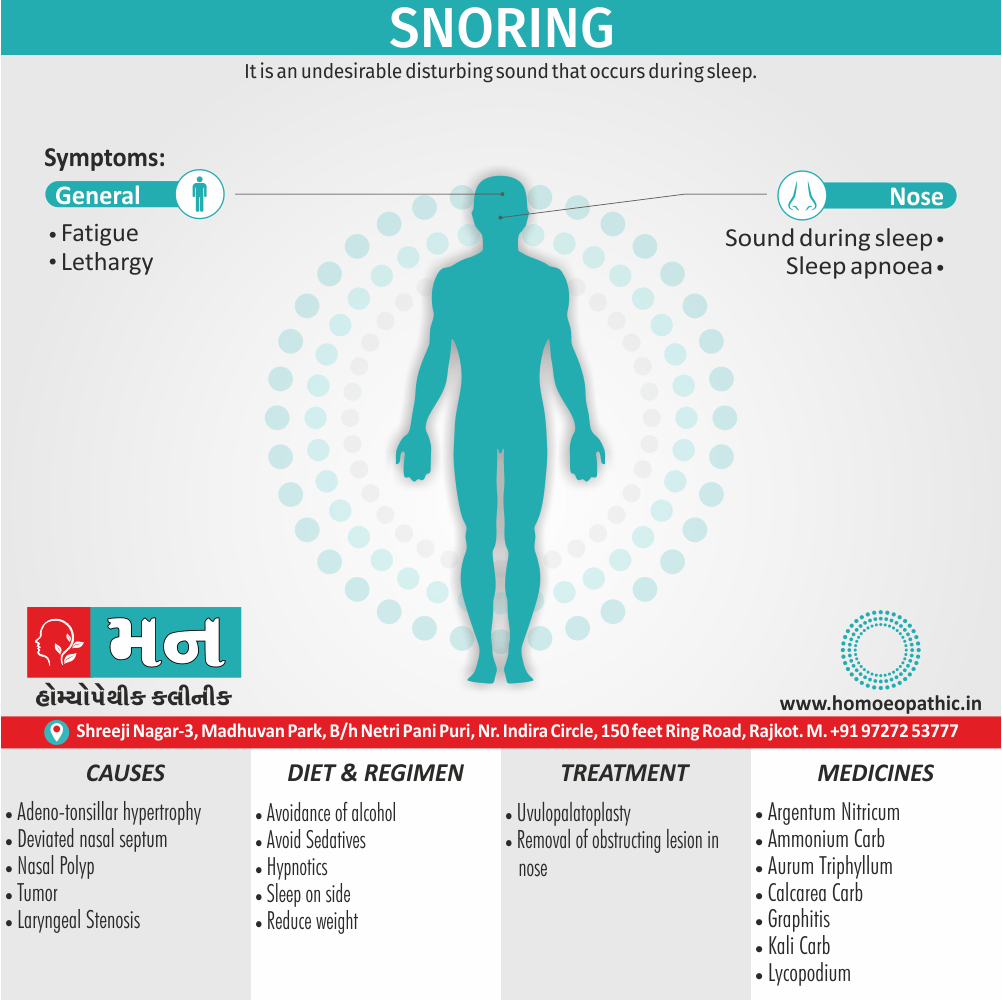
Snoring is an undesirable disturbing sound that occurs during sleep [1]
Snoring refers to the hoarse or harsh sound that occurs when someone is breathing during sleep. Here are some synonyms or related terms:
- Sawing logs: A colloquial term for snoring loudly.
- Snorting: Breathing noisily through the nose, often associated with snoring.
- Rattling: A harsh, shaking sound similar to snoring.
- Snuffling: Breathing noisily through the nose, usually with a congested sound.
- Heavy breathing: Loud or labored breathing during sleep, which may or may not include snoring.
Additionally, here are some verbs related to snoring:
- Saw wood: A slang term meaning to snore.
- Snort: To make a snorting sound while sleeping.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Snoring:
Snoring is estimated that 25% of adult males and 15% of adult females snore. Its prevalence increases with age
- Sleep apnea. It is cessation of breathing that lasts for 10 s or more during sleep. Less than five such episodes is normal.
- Apnea index. It is number of episodes of apnea in 1 h.
- Hypopnea. It is reduction of airflow. Some define it as drop of 50% of airflow from the base line associated with an EEG defined arousal or 4% drop in oxygen saturation.
- Respiratory disturbance index (in other words, RDI). Also called apnea– hypopnea index. It is the number of apnea and hypopnea events per hour. Normally RDI is less than five. Based on RDI, severity of apnea has been classified as mild, 5–14; moderate, 15–29; and severe ≥ 30.
- Arousal. Transient awakening from sleep as a result of apnea or respiratory efforts.
- Arousal index. In detail, It is number of arousal events in 1 h. Less than four is normal.
- Sleep efficiency. Minutes of sleep divided by minutes in bed after lights are turned off.
- Multiple either sleep latency test or nap study. Patient is given four or five scheduled naps usually in the daytime. Latency period from wakefulness to the onset of sleep and rolling eye movement (in other words, REM) sleep are measured. It is performed when narcolepsy is suspected or daytime sleepiness is evaluated objectively.
Epidemiology
Epidemiology:
The epidemiology of snoring in India varies considerably depending on the specific population studied and the definition of snoring used. However, some general trends can be observed from available research.
- A study published in 1997 ("Prevalence of snoring and sleep breathing-related disorders in Chinese, Malay and Indian adults in Singapore") found a snoring prevalence of 10.9% among Indian adults in Singapore.
- A 2006 study ("Prevalence and risk factors of obstructive sleep apnea syndrome in a population of Delhi, India") reported that 45% of the 2150 participants reported habitual snoring.
- In a 2019 review article ("Obstructive Sleep Apnea Hypopnea Syndrome – Indian scenario"), the authors noted that the prevalence of snoring in Indian studies ranged from 16% to 84%, with males generally having higher rates than females.
These figures highlight the wide range of snoring prevalence estimates in India. Several factors contribute to this variability, including differences in study populations (e.g., urban vs. rural, age groups), definitions of snoring (e.g., self-reported vs. observed), and methodological approaches.
Overall, while snoring is a common phenomenon in India, more research is needed to establish precise prevalence rates and identify specific risk factors within the Indian population.[4][5][6]
Causes
Causes of Snoring:
In children most common cause is adeno-tonsillar hypertrophy. In adults cause of snoring could be in [1]
The nose or nasopharynx such as
- Septal deviation,
- Turbinate hypertrophy,
- Nasal valve collapse,
- Nasal polypi or
- Tumors;
In oral cavity and oropharynx such as
- Elongated soft palate and uvula,
- Tonsillar enlargement,
- Macroglossia,
- Retrognathia,
- Large base of tongue; or
- Its tumor;
In the larynx and laryngopharynx such as
- Laryngeal stenosis or
- Omega-shaped epiglottis.
Other causes include obesity and thick neck with collar size exceeding 42 cm. Use of alcohol, sedatives and hypnotics aggravates snoring due to muscle relaxation.[1]
Types
Types:
snoring occurs when the flow of air through the mouth and nose is obstructed during sleep, causing the surrounding tissues to vibrate and produce the characteristic sound. This obstruction can be caused by various factors, including:
- Anatomical abnormalities: such as a deviated septum, enlarged tonsils, or a long soft palate.
- Obesity: excess weight can lead to fat deposition around the neck, narrowing the airway.
- Alcohol consumption: alcohol relaxes the muscles in the throat, increasing the likelihood of airway collapse.
- Sleeping position: sleeping on the back can cause the tongue to fall back and obstruct the airway.
- Weight loss: shedding excess pounds can significantly reduce snoring severity.
- Avoiding alcohol before bed: limiting alcohol intake in the evening can improve sleep quality and reduce snoring.
- Sleeping on your side: this position helps keep the airway open and prevents the tongue from blocking it.
- Nasal devices: such as nasal strips or dilators, can help improve airflow through the nose and reduce snoring.
- Oral appliances: custom-fitted devices worn in the mouth can reposition the jaw and tongue, preventing airway obstruction.
- Continuous positive airway pressure (CPAP) therapy: this involves wearing a mask that delivers pressurized air to keep the airway open during sleep.
- Surgery: in some cases, surgical procedures may be necessary to correct anatomical abnormalities that contribute to snoring.[7]
Risk Factors
Risk factors:
Obesity: Excess weight, especially around the neck, can lead to fat deposition in the throat area, narrowing the airway and increasing the likelihood of snoring.
Gender: Men are more likely to snore than women due to anatomical differences in the upper airway.
Age: As we age, the muscles in the throat relax, making airway collapse more likely during sleep, leading to snoring.
Alcohol and Sedative Use: Alcohol and certain medications can relax the muscles in the throat, increasing the risk of airway obstruction and snoring.
Nasal Congestion: Allergies, colds, or structural abnormalities in the nose can obstruct airflow, forcing you to breathe through your mouth and increasing the chances of snoring.
Sleeping Position: Sleeping on your back can cause the tongue and soft palate to collapse toward the back of the throat, obstructing the airway and causing snoring.
Family History: If you have a family history of snoring or sleep apnea, you may be genetically predisposed to these conditions.
Smoking: Smoking irritates the lining of the airway, leading to inflammation and swelling, which can contribute to snoring.
Understanding these risk factors can help you take proactive steps to reduce your risk of snoring and its associated complications. By maintaining a healthy weight, avoiding alcohol and sedatives before bed, managing nasal congestion, and adopting healthy sleep habits, you can improve your sleep quality and overall well-being.[7]
Pathogenesis
Pathogenesis:
Anatomic Factors:
- Nasal Obstruction: Deviations of the nasal septum, enlarged turbinates, or nasal polyps can impede airflow, leading to increased airflow velocity and tissue vibration.
- Soft Palate and Uvula: Elongation or excessive laxity of the soft palate and uvula can cause them to flutter during breathing, producing snoring sounds.
- Tongue Base: In some individuals, the tongue base may fall back during sleep, obstructing the airway and contributing to snoring.
- Large Tonsils and Adenoids: Enlarged tonsils and adenoids, particularly in children, can narrow the airway and predispose to snoring.
Functional Factors:
- Muscle Relaxation: During sleep, the muscles of the upper airway relax, leading to decreased airway caliber and increased collapsibility. This is particularly pronounced during REM sleep.
- Obesity: Excess weight, particularly around the neck, can increase the amount of fat tissue surrounding the airway, contributing to narrowing and snoring.
- Alcohol and Sedatives: These substances can further relax the muscles of the upper airway, exacerbating snoring.
- Hormonal Changes: Pregnancy and menopause can lead to changes in the upper airway tissues, potentially increasing the risk of snoring.
Other Factors:
Pathophysiology
Pathophysiology of Snoring:
Muscles of pharynx are relaxed during sleep and cause partial obstruction. Breathing against obstruction causes vibrations of soft palate, tonsillar pillars and base of tongue producing sound. Sound as loud as 90 dB has been recorded during snoring. Snoring may be primary, i.e., without association with obstructive sleep apnea (OSA) or complicated, i.e., associated with OSA. Primary snoring is not associated with excessive daytime sleepiness and has apnea–hypopnea index of less than five.[1]
Clinical Features
Clinical Feature:
Snoring article Clinicle Feature:
Snoring, a common sleep-related breathing disorder characterized by noisy breathing during sleep, affects millions worldwide. It can range from mild, occasional snoring to loud, disruptive snoring associated with more serious health conditions like obstructive sleep apnea (OSA).
Common clinical features associated with snoring include:
- Loud, disruptive snoring that disturbs bed partners or roommates
- Frequent gasping or choking during sleep
- Witnessed apneas (temporary cessation of breathing)
- Excessive daytime sleepiness
- Morning headaches
- Difficulty concentrating
- Irritability[9]
Sign & Symptoms
Sign & Symptoms:
Excessive loud snoring is socially disruptive and forms snoring-spouse syndrome and is the cause of marital discord sometimes leading to divorce. In addition, a snorer with obstructive sleep apnea may manifest with:
- Excessive daytime sleepiness
- Morning headaches
- General fatigue
- Memory loss
- Irritability and depression
- Decreased libido
- Increased risk of road accidents[8]
Clinical Examination
Clinical Examination:
Medical History:
- Detailed history of snoring, including its frequency, duration, severity, and associated symptoms like daytime sleepiness, witnessed apneas, choking or gasping during sleep, morning headaches, and impaired concentration or memory.
- Past medical history, focusing on conditions like hypertension, heart disease, diabetes, and any prior sleep studies or treatments.
- Medications, including any over-the-counter or herbal supplements.
- Social history, assessing alcohol consumption, smoking habits, and illicit drug use.
- Family history of snoring, sleep apnea, or other sleep disorders.
Physical Examination:
- General appearance, noting body mass index (BMI), neck circumference, and any facial or craniofacial abnormalities.
- Airway assessment, including evaluation of nasal patency, presence of nasal polyps or septal deviation, size and position of tonsils and adenoids, and tongue size and position.
- Cardiovascular and respiratory examination, including blood pressure measurement, heart and lung auscultation.
- Neurological examination, assessing for any signs of neurological dysfunction.
Additional Diagnostic Tests:
- Polysomnography (sleep study) to confirm the diagnosis of sleep apnea and assess its severity.
- Home sleep apnea testing (HSAT) as a potential alternative to in-lab polysomnography for patients with a high pre-test probability of moderate to severe obstructive sleep apnea.
- Imaging studies (e.g., cephalometry, computed tomography, magnetic resonance imaging) may be considered to evaluate upper airway anatomy in selected cases.[9]
Diagnosis
Diagnosis:
Polysomnography (PSG)
remains the gold standard for diagnosing snoring and associated sleep disorders. PSG comprehensively records various physiological parameters during sleep, including:
- Respiratory effort: Chest and abdominal movements to assess breathing patterns.
- Airflow: Nasal and oral airflow to detect obstructions.
- Oxygen saturation: Blood oxygen levels to identify drops associated with sleep apnea.
- Electroencephalogram (EEG): Brain activity to determine sleep stages.
- Electrooculogram (EOG): Eye movements to monitor sleep stages.
- Electromyogram (EMG): Muscle activity to assess muscle tone during sleep.
Home Sleep Apnea Testing (HSAT)
is an alternative for individuals with a high pre-test probability of obstructive sleep apnea (OSA). HSAT devices typically record:
- Respiratory effort.
- Airflow.
- Oxygen saturation.
- Pulse rate.
HSAT is less comprehensive than PSG but offers a more convenient and cost-effective option for screening OSA.
Additional diagnostic tools
may include:
- Epworth Sleepiness Scale (ESS): A questionnaire to assess daytime sleepiness.
- Imaging studies: Such as X-rays or computed tomography (CT) scans to evaluate the upper airway anatomy.
- Drug-induced sleep endoscopy (DISE): To visualize upper airway collapse during sleep.[9]
Differential Diagnosis
Differential Diagnosis:
- Obstructive Sleep Apnea (OSA): The most common cause, OSA involves repeated airway collapse during sleep, leading to snoring, gasping, and daytime fatigue.
- Nasal Obstruction: Allergies, deviated septum, or nasal polyps can obstruct airflow, causing mouth breathing and snoring.
- Obesity: Excess weight around the neck can narrow the airway, contributing to snoring.
- Alcohol & Sedatives: These relax throat muscles, increasing the likelihood of snoring.
- Hypothyroidism: An underactive thyroid can cause tissue swelling, potentially obstructing the airway and leading to snoring.
- Large Tonsils or Adenoids: These can obstruct the airway, especially in children, causing snoring.
- Neuromuscular Disorders: Conditions affecting muscle tone can contribute to airway collapse and snoring.[9]
Complications
Complications :
- Obstructive Sleep Apnea (OSA): This is the most concerning complication of snoring. OSA occurs when the airway becomes partially or completely blocked during sleep, leading to repeated pauses in breathing. This can result in daytime sleepiness, fatigue, high blood pressure, heart problems.
- Cardiovascular Problems: Snoring, especially when associated with OSA, can put a strain on the cardiovascular system. The repeated drops in oxygen levels and surges in blood pressure can lead to hypertension, heart arrhythmias, heart failure, and an increased risk of heart attack.
- Daytime Impairment: The fragmented sleep caused by snoring and OSA can lead to excessive daytime sleepiness, fatigue, difficulty concentrating, impaired memory, and decreased productivity. This can affect work, school, and relationships.[9][10]
Investigations
Investigations:
- Snoring‘s spectrum: From benign vibrations to obstructive sleep apnea, the book dissects snoring‘s varied manifestations.
- Root causes: Anatomical factors, lifestyle choices, and medical conditions contributing to snoring are examined in detail.
- Diagnostic tools: The book outlines diagnostic procedures to identify the specific cause of an individual’s snoring.
- Treatment options: Lifestyle modifications, dental appliances, surgical interventions, and innovative therapies are discussed.[11]
Treatment
Treatment:
- Avoidance of alcohol, sedatives also hypnotics.
- Reduction of weight.
- Sleeping on the side rather than on the back.
- Removal of obstructing lesion in nose, nasopharynx, oral cavity, hypopharynx and larynx. Radiofrequency has been used for volumetric reduction of tissues of turbinates, soft palate and base of tongue.
- Performing uvulopalatoplasty (UPP) surgically with cold knife or assisted with radiofrequency (RAUP) or laser (LAUP).[1]
Prevention
Prevention:
Key Snoring Prevention Strategies:
Maintain a Healthy Weight: Excess weight can contribute to snoring by increasing tissue around the neck and throat, obstructing airflow. Losing even a small amount of weight can make a significant difference.
Sleep on Your Side: Sleeping on your back can cause the tongue and soft palate to collapse to the back of the throat, leading to snoring. Sleeping on your side helps keep your airways open.
Avoid Alcohol and Sedatives Before Bed: Alcohol and sedatives relax the muscles in the throat, increasing the likelihood of snoring. Avoiding these substances before bed can help prevent snoring.
Practice Good Sleep Hygiene: Establishing a regular sleep schedule, creating a relaxing bedtime routine, and ensuring your bedroom is dark, quiet, and cool can all contribute to better sleep and reduced snoring.
Keep Nasal Passages Open: If nasal congestion is contributing to your snoring, try using nasal strips, decongestants, or a neti pot to clear your nasal passages.
Consider an Oral Appliance: An oral appliance can help reposition your jaw and tongue, keeping your airways open and reducing snoring. Consult with a dentist or sleep specialist to determine if an oral appliance is right for you.
Address Underlying Medical Conditions: Certain medical conditions, such as sleep apnea or allergies, can contribute to snoring. Treating these underlying conditions can help alleviate snoring.[11]
Homeopathic Treatment
Homoeopathic Treatment for Snoring:
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines are selected after a full individualizing examination and case-analysis, which includes the medical history of the patient, physical and mental constitution, family history, presenting symptoms, underlying pathology, possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) is also often taken into account for the treatment of chronic conditions.
What does homeopathic doctor do ?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’. The disease diagnosis is important but in homeopathy, the cause of disease is not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness are also looked for.
Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition. The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology is not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can be greatly improved with homeopathic medicines.
Homeopathic medicines for Snoring
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications are also taken into account for selecting a remedy.
Amm-c.—
*Stoppage of nose mostly at night; must breathe through mouth (Nux-v.). Without any cold. Starts up every time the child tries to go to sleep.
Argentum nitricum
Coryza at first dry, then moist, discharging thick, yellow, purulent mucus, mingled with clots to blood; chilliness, lachrymation, sneezing [3]
Arum Triphyllum
Profuse coryza, discharge burning and ichorous, making nostrils and lips sore; feverishness and hot, dried skin; child picks at his skin, even producing raw places
Calcarea Carb
Nose dry and of offensive smell, nostrils sore and ulcerated, discharge thick and pus-like, or thin and watery; moist during day and dry at night; enlargement of glands; profuse sweat, especially about head and feet; hoarseness; very susceptible to external influence, currents of air, cold, heat, noise, excitement.
Cham.
Nose runs, yet stuffed; one cheek red, the other pale; characteristic irritability. [3]
Graphites
Herpetic children, catching cold easily; dryness of nostrils, or alternate flowing and dryness; cracked also ulcerated nostrils; bloody mucus or thick foetid discharge; frequent sneezing. [3]
Kali Carb
Anemic children of cachectic appearance, with puffy swelling over upper eyelids, especially mornings; cannot breathe through nostrils in a warm room, (>) in open air; nostrils raw also bleeding; profuse, fetid, yellow-green discharge.[3]
Lycopodium
Dry from of chronic coryza, with much sneezing during the day and complete closure at night, so that child breathes with mouth open (Elaps) and protruding tongue; constipation, flatulency; coryza extending down air-passages; causing with loose expectoration; child starts out of sleep; rubbing its nose.
Nux-v
Coryza fluent during day; stopped at night; nose dry and stuffed; breathes through mouth. "Coryza prevents infants from breathing while nursing; worse especially at night and towards morning."[3]
Samb.
"Child suddenly awakens nearly suffocated, sits up in bed and turns blue; grasps for breath, which it finally gets, then lies down again in bed, to be aroused again sooner or later by another spell." "Nose perfectly dry and completely obstructed, preventing breathing also nursing; constant snuffles." Child *inspires but cannot expire (Chlorine, Mephitis). Lastly, Edematous swelling in nose giving rise to snuffles.
Sticta.
Nose stuffed up. Constant need or inclination to blow nose, but nothing is discharged; excessive dryness of nose. (Tertiary syphilis.)
Diet & Regimen
Diet And Regimen:
1. Lose weight if you are higher-weight person.
Generally, This will help reduce the amount of tissue in the throat that might be causing your snoring. You can lose weight by reducing your overall caloric intake by eating smaller portions and more healthy foods. Additionally, Make sure you get regular exercise daily. You may also consider seeing your doctor or a nutritionist for help.[2]
2. Sleep on your side.
Sleeping on your back sometimes causes the tongue to move to the back of the throat, which partly blocks airflow through your throat. Furthermore, Sleeping on your side may be all you need to do to allow air to flow easily and reduce or stop your snoring.
3. Raise up the head of your bed.
Elevating the head of your bed by four inches may help reduce your snoring by keeping your airways open.
4. Use nasal strips or an external nasal dilator.
Stick-on nasal strips can be placed on the bridge of the nose to help increase the space in the nasal passage. This can make your breathing more effective also reduce or eliminate your snoring.
You could also try a nasal dilator, which is a stiffened adhesive strip that’s applied on top of the nose across the nostrils. This can decrease airflow resistance, making it easier to breath.
Try nasal strips to help reduce snoring.
5. Treat chronic allergies.
Allergies can reduce airflow through your nose, which forces you to breathe through your mouth. Additionally, this increases the likelihood that you’ll snore. Talk to your doctor about what kind of over-the-counter or prescription allergy medications may improve your condition.
Buy over-the-counter allergy medication now.
6. Correct structural problems in your nose.
Some people are born with or experience an injury that gives them a deviated septum. Additionally, This is the misalignment of the wall that separates both sides of the nose, which restricts airflow. In detail, It may cause mouth breathing during sleep, causing snoring. It may be necessary to get surgery to correct this condition. Talk to your doctor.
7. Limit or avoid alcohol before bed.
Try not to consume alcohol for at least two hours leading up to your bedtime. Alcohol can relax the throat muscles, causing snoring.
8. Avoid taking sedatives before bed.
If you snore and take sedatives, talk to your doctor to see what your options are. Stopping sedative use before bed may ease your snoring.
9. Stop smoking.
Smoking is an unhealthy habit that can worsen your snoring. Talk to your doctor about therapies such as gum or patches that can help you quit.[2]
10. Get enough sleep.
In Brief, Make sure you get the recommended seven to eight hours of sleep you need each night.
11. Use an oral appliance.
Dental mouthpieces called “oral appliances” can help keep your air passages open, making it easier for you to breathe. This prevents snoring. Lastly, You need to see your dentist to get one of these devices made.
12. Use a CPAP (continuous positive airway pressure) machine.
If medically appropriate, wearing a pressurized air mask over your nose when you sleep can help keep your airway open. In detail, this treatment is often recommended to treat obstructive sleep apnoea.
13. Wear palatal implants.
Also called the “pillar procedure,” this treatment involves injecting braided strands of polyester filament into your mouth’s soft palate. Lastly, This stiffens it to reduce snoring.
14. Get UPPP (uvulo-palato-pharyngo-plasty).
This type of surgery tightens throat tissue in the hopes it will reduce snoring. Laser-assisted uvulo-palato-pharyngo-plasty (LAUPPP), which is sometimes more effective than UPPP, is also available.
15. Radiofrequency tissue ablation (somno-plasty).
This new treatment uses low-intensity radio waves to shrink the tissue on your soft palate to reduce snoring.[2]
Do’s and Don'ts
Do’s & Don’ts
Snoring Do’s & Don’ts
Do’s:
Maintain a healthy weight: Excess weight can lead to increased tissue around your neck and throat, which can obstruct your airway and cause snoring. Losing even a small amount of weight can make a big difference.
- Sleep on your side: Sleeping on your back can cause your tongue and soft palate to collapse to the back of your throat, narrowing your airway and causing snoring. Sleeping on your side helps keep your airways open.
- Elevate your head: Elevating the head of your bed by a few inches can help keep your airways open and reduce snoring. You can use a wedge pillow or elevate the entire head of your bed.
- Keep your nasal passages open: If nasal congestion is contributing to your snoring, try using nasal strips, a neti pot, or a humidifier to keep your nasal passages open.
Also Including:
- Avoid alcohol and sedatives before bed: Alcohol and sedatives relax the muscles in your throat, making snoring more likely. Avoiding these substances before bed can help prevent snoring.
- Practice good sleep hygiene: Establishing a regular sleep schedule, creating a relaxing bedtime routine, and ensuring your bedroom is dark, quiet, and cool can all contribute to better sleep and reduced snoring.
- Stay hydrated: Drinking plenty of water throughout the day can help keep your nasal passages and throat moist, reducing the likelihood of snoring.
Don’ts:
Don’t sleep on your back: Sleeping on your back can cause your tongue and soft palate to collapse to the back of your throat, narrowing your airway.
Shouln’t consume alcohol or sedatives before bed: Alcohol and sedatives relax the muscles in your throat, making snoring more likely. Avoid these substances before bed to help prevent snoring.
Don’t smoke: Smoking irritates the lining of your throat and nasal passages, which can contribute to snoring. Quitting smoking can help reduce snoring and improve your overall health.
Don’t eat a heavy meal before bed: Eating a large meal before bed can cause your stomach to push up against your diaphragm, making it harder to breathe and increasing the likelihood of snoring.
Must not ignore chronic snoring: If you snore regularly and experience excessive daytime sleepiness, talk to your doctor. Snoring can sometimes be a symptom of a more serious underlying medical condition, such as sleep apnea.
Terminology
Terminology:
- Snoring: The harsh or hoarse sound that occurs when breathing is partially obstructed during sleep, causing the tissues in the throat to vibrate.
- Obstructive Sleep Apnea (OSA): A serious sleep disorder where breathing repeatedly stops and starts during sleep due to complete or partial blockage of the upper airway. Snoring is a common symptom of OSA.
- Upper Airway: The passage that allows air to flow from the nose and mouth to the lungs. It includes the nasal passages, throat, and voice box.
- Soft Palate: The fleshy part at the back of the roof of the mouth. It can vibrate during sleep and contribute to snoring.
- Uvula: The small, fleshy projection hanging down at the back of the soft palate. It can also vibrate and contribute to snoring.
- Nasal Congestion: Blockage or narrowing of the nasal passages, often caused by allergies, colds, or sinus infections. It can make breathing through the nose difficult and lead to mouth breathing and snoring.
- Polysomnography (PSG): A sleep study that monitors various bodily functions during sleep, such as brain activity, eye movements, heart rate, and breathing patterns. It’s used to diagnose sleep disorders like sleep apnea.
- Epiglottis: A flap of cartilage at the base of the tongue that prevents food or liquid from entering the trachea (windpipe) during swallowing. It can sometimes contribute to snoring if it becomes floppy or relaxed during sleep.
- Tonsils and Adenoids: Masses of lymphatic tissue at the back of the throat and behind the nasal cavity, respectively. Enlarged tonsils or adenoids can obstruct the airway and contribute to snoring, especially in children.
Homeopathic articles about snoring, along with their meanings:
Snoring: As in general medical literature, this refers to the harsh or hoarse sound produced during sleep due to partial obstruction of the airway, causing the tissues in the throat to vibrate.
Constitutional Remedy: A central concept in homeopathy, it’s a remedy chosen based on the individual’s overall physical, mental, and emotional characteristics, rather than just the specific symptoms. In the context of snoring, a homeopath would consider the person’s entire constitution to find the most suitable remedy.
Miasm: Another fundamental homeopathic idea, it refers to a predisposing disease tendency or inherited weakness. Homeopaths believe that certain remedies are particularly effective for individuals with specific miasmatic backgrounds, which might also contribute to snoring.
Potency: This denotes the strength or dilution of a homeopathic remedy. It’s expressed in Roman numerals (e.g., 6C, 30C, 200C), with higher numbers indicating greater dilution and, theoretically, deeper action on the body’s vital force.
Other Terminology Are:
Aggravation: A temporary worsening of symptoms after taking a remedy, which homeopaths often consider a positive sign that the remedy is working and stimulating the body’s healing response.
Modalities: These are factors that make a symptom better or worse. In the context of snoring, modalities could include the position of sleep, time of night, temperature, or emotional states that influence the snoring.
Repertory: A reference book used by homeopaths to find remedies based on specific symptoms and their modalities. It lists various symptoms and the remedies known to be associated with them.
Materia Medica: A comprehensive collection of information about homeopathic remedies, including their sources, preparation, and the symptoms they’re known to produce and cure.
Vital Force: A core principle in homeopathy, it’s the inherent energy or life force that animates the body and maintains health. Homeopaths believe that disease arises from disturbances in the vital force, and remedies act by stimulating its self-healing capacity.
Provings: A method used in homeopathy to determine the effects of a remedy on healthy individuals. Volunteers take the remedy and meticulously record any physical, mental, or emotional symptoms they experience. This information helps build the materia medica.
References
Reference use in Article Snoring:
- Diseases_of_Ear_Nose_and_Throat_6E
- https://www.healthline.com/health/snoring-remedies#_noHeaderPrefixedContent
- Homoeopathic Therapeutics by Lilienthal
- "Prevalence of snoring and sleep breathing-related disorders in Chinese, Malay and Indian adults in Singapore"
- ("Prevalence and risk factors of obstructive sleep apnea syndrome in a population of Delhi, India")
- 2019 review article ("Obstructive Sleep Apnea Hypopnea Syndrome – Indian scenario")
- Sleep: The Mysteries, the Problems, and the Solutions,First Edition.
- Principles and Practice of Sleep Medicine,7th Edition
- Kryger, M.H., Roth, T., & Dement, W.C.. Principles and Practice of Sleep Medicine. 6th ed. Elsevier.
American Academy of Sleep Medicine. International Classification of Sleep Disorders, 3rd Edition (ICSD-3)
Prevention & Treatment of Snoring by Prof. Dr. Ninad Moon
Also Search As
Also Search As
Online Search Engines
Use specific keywords:
Try different search engines:
While Google is popular, explore other search engines like DuckDuckGo or Bing to see if they yield different results.
Refine your search:
Use advanced search operators like quotation marks for exact phrases, or the minus sign to exclude specific terms. Example: "homeopathy snoring" -surgery
Homeopathic Websites and Forums
Visit dedicated homeopathy sites:
- Many websites specialize in homeopathy and may have articles or resources on snoring.
Search within homeopathic forums
- : Online communities and forums dedicated to homeopathy can be valuable sources of information and personal experiences.
Check homeopathic associations’ websites:
- National or regional homeopathic associations often have online resources and may publish articles on specific conditions like snoring.
Homeopathic Libraries and Practitioners
Visit a local homeopathic library:
- Some cities or towns have libraries dedicated to homeopathy, where you can find books and articles on the subject.
Consult a homeopathic practitioner:
- They can provide personalized recommendations and may have access to articles or research on homeopathy and snoring.
There are several ways to search for information about snoring, each with its own advantages:
Online Search Engines
- Simple keyword searches: Start with general terms like "snoring" or "causes of snoring".
- Specific queries: To narrow down your search, use more specific keywords like "snoring remedies", "snoring and sleep apnea", or "snoring in children".
- Medical websites: Search on reputable health websites like Mayo Clinic, WebMD, or the Cleveland Clinic.
- Image search: Look for visual aids like diagrams of the respiratory system or photos of snoring treatments.
Medical Databases
- PubMed: This free database provides access to medical literature and research articles. Search using medical terms like "sleep-disordered breathing" or "obstructive sleep apnea".
- Google Scholar: Another option for finding scholarly articles and research papers on snoring and related topics.
Libraries and Bookstores
- Books on sleep disorders: Visit your local library or bookstore and browse the health section for books on sleep disorders, which will likely include information on snoring.
- Medical textbooks: If you have access to a medical library, consult textbooks on otolaryngology (ear, nose, and throat) or sleep medicine.
Healthcare Professionals
- Consult your doctor: If you’re concerned about your snoring or suspect it might be a symptom of a more serious condition, talk to your doctor.
- Seek a sleep specialist: For in-depth evaluation and treatment options, consider seeing a sleep specialist.
Additional Tips
- Use reliable sources: Stick to information from reputable healthcare organizations, medical professionals, and peer-reviewed research articles.
- Be specific in your search: If you’re looking for information on a particular aspect of snoring (e.g., causes, treatments, or its connection to sleep apnea), include those terms in your search.
- Check the date of publication: Ensure the information you’re reading is up-to-date, as medical knowledge and treatment options can evolve.
By utilizing these diverse search methods, you can access a wide range of reliable information about snoring, its causes, potential health implications, and available treatment options.
Frequently Asked Questions (FAQ)
Is snoring harmful?
Snoring itself may not be harmful, but it can be a sign of a more serious condition called obstructive sleep apnea (OSA). OSA is characterized by repeated pauses in breathing during sleep, which can lead to a number of health problems, including high blood pressure, heart disease, stroke, and diabetes.
How is snoring treated?
The treatment for snoring depends on the underlying cause. Some common treatment options include:
- Lifestyle changes: Losing weight, avoiding alcohol and sedatives before bed, and sleeping on your side can help reduce snoring.
- Nasal devices: Nasal strips or dilators can help open up the nasal passages, making it easier to breathe through your nose.
- Oral appliances: These devices help keep the airway open by repositioning the jaw or tongue.
- Continuous positive airway pressure (CPAP): This therapy involves wearing a mask that delivers air pressure to keep the airway open during sleep. It is the most effective treatment for OSA.
- Surgery: In some cases, surgery may be recommended to remove excess tissue in the throat or correct structural abnormalities that contribute to snoring.
Can homeopathy cure snoring?
Yes, homeopathy offers remedies that can address the root cause of snoring, leading to significant improvement or even complete cessation.
What are the reasons of Snoring?
- Adeno-tonsillar hypertrophy
- Septal deviation
- Turbinate hypertrophy
- Nasal valve collapse
- Elongated soft palate and uvula
- Tonsillar enlargement
- Laryngeal stenosis
- Omega-shaped epiglottis
What are the symptoms of Snoring?
- Excessive daytime sleepiness
- Morning headaches
- General fatigue
- Memory loss
- Irritability and depression
How long does it take to see results with homeopathy for snoring?
The response time varies. Some individuals experience relief within days or weeks, while others may require a longer duration of treatment.
